Abstract
Background
Evidence indicates that medical students have had high rates of mental health problems, especially during the COVID-19 pandemic, which could be affected by alexithymia—a marked dysfunction in emotional awareness, social attachment and interpersonal relationships—and stress. However, psychological resilience might relieve alexithymia and stress levels.
Aims
This study aimed to investigate the role of resilience in alexithymia and stress in medical students.
Methods
A total of 470 medical students completed online and offline surveys, including the Toronto Alexithymia Scale-20 (TAS-20), the Connor-Davidson Resilience Scale (CD-RISC) and the College Student Stress Questionnaire (CSSQ). The data of five participants were excluded because of a lack of integrity. Mann-Whitney U test or Kruskal-Wallis test was used to compare group differences in the CD-RISC scores among categorical variables. Spearman correlation analysis was employed to evaluate the associations between resilience and alexithymia and between resilience and stress. Mediation analysis was used to test the mediating effect of resilience between alexithymia and stress.
Results
Of the medical students considered in the analysis, 382 (81.28%) were female and 88 (18.72%) were male. There was a significant negative correlation between the TAS-20 scores and the total and subtotal CD-RISC scores (p<0.001). The CSSQ scores also significantly negatively correlated with the total and subtotal CD-RISC scores (p<0.001). Resilience mediated the relationship between alexithymia and stress (total effect=1.044 7, p<0.001). The indirect effect of alexithymia significantly impacted stress through resilience (effect=0.167 0, 95% CI: 0.069 to 0.281).
Conclusions
Our findings suggest that resilience might effectively reduce alexithymia and stress. They also contributed to a better understanding of the mediating effects of resilience on alexithymia and stress during the COVID-19 pandemic. The evidence from these results encourages universities to focus on improving students’ resilience.
Keywords: resilience, psychological; mental health; COVID-19; psychosomatic medicine
WHAT IS ALREADY KNOWN ON THIS TOPIC
Medical students have been shown to have high rates of negative mental health symptoms. The COVID-19 pandemic has magnified the stressors these students usually encounter during their studies. Alexithymia, a personality trait that negatively affects mental health, appears to increase perceived stress. Resilience has been found to play a positive role in decreasing stress and alexithymia. However, how resilience has influenced medical students’ alexithymia and stress during the recent pandemic remains unclear.
WHAT THIS STUDY ADDS
This study explored the relationships between resilience and alexithymia and resilience and stress. Mediation analysis was used to investigate how resilience mediates the associations between alexithymia and stress.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
As the COVID-19 pandemic continues, universities should pay close attention to students with pronounced alexithymia because their perceptions of stress may be severe. At the same time, universities could enhance all students’ resilience through specific interventions, such as well-being and cognitive behaviour therapies.
Introduction
Evidence indicates that medical students have high rates of psychiatric disorders and mental stress worldwide and are at high risk for suicidal ideation.1 Burnout of medical students increases after clinical rotations in which they are exposed to patients with debilitating illnesses, life-threatening diseases and death.2 Medical students also experience a variety of other stressors, such as examinations, living away from family and financial hardships—all making them more prone to mental disorders.3 Not surprisingly, the high prevalence of emotional disorders among medical students may increase their risk for other problems, such as low levels of life satisfaction, school incompletion and suicide.
Starting soon after the onset of the COVID-19 pandemic, universities closed their doors, and digital learning replaced in-person lectures. However, the clinical aspects of medical training are ill-suited for E-learning. Unfortunately, the pandemic continuously disrupted medical education and training throughout this period.4 An epidemiological study of 746 217 college students showed that acute stress, anxiety and depressive symptoms were prevalent during the COVID-19 pandemic.5 Moreover, COVID-related psychological stress in medical students was found to significantly increase the risk of negative impact on their health, academic performance, professional identity and future medical service quality.6
A novel study suggested that students who experienced psychological problems during the COVID-19 pandemic would more likely be affected by deficiencies in emotional identification and expression or, in other words, alexithymia.7 The disorder is a multifaceted personality construct, including difficulties identifying and describing feelings and poor externally-oriented thinking,8 that is more common in younger populations (24.1%), especially among college students.9
Furthermore, alexithymia is a sign of negative emotions and a significant risk factor for other medical and psychiatric problems.10 Thus, individuals with alexithymia are prone to reporting mental health–related concerns. In our previous research, nursing students showed significantly positive correlations between alexithymia and health anxiety.10 However, during the COVID-19 pandemic, the relationships between alexithymia and different aspects of stress in medical students were not evident and, thus, are worthy of attention.
A previous study found resilience plays a positive role in the mental health of medical students.11 For example, students with higher resilience scores exhibited better adaptive coping strategies when facing academic stress.11 Nevertheless, compared with non-medical students, medical students may have lower resilience levels.12 Many factors can influence students’ resilience, such as workplace and training stress, interpersonal relationships and alexithymia.13 14 Resilience and positive coping have also been shown to be protective factors for developing stress symptoms and decreasing the risks of pandemic-related distress.15 Therefore, we hypothesised that resilience could be a mediator for reducing stress and alexithymia in medical students. However, more research is needed to determine the relationships among resilience, stress and alexithymia, which is the aim of this study.
Methods
Procedures and participants
This cross-sectional study conducted from 18 March to 21 April 2021 was based on online and offline surveys. College students in China were invited to participate in this survey via the Wenjuanxing platform (https://www.wjx.cn/report/110598159.aspx), distributed on the Internet, WeChat and the Tencent QQ platform, or by completing a printed version of the scales. Students who had failed to complete the online survey received a notification about unanswered questions; the survey could be submitted online only after all questions were answered. Online and offline questionnaires were checked to reject invalid surveys.
In total, 475 students (18 to 26 years old) volunteered to participate in this survey; five incomplete questionnaires were rejected. Gender, academic performance (ie, good, average or poor), home location (ie, city/town or countryside), only-child family (ie, yes or no) and family income (ie, high, average or low) were collected via ad hoc questions. Students were also asked questions about alexithymia, resilience and stress.
Measurements
Clinimetric evaluation of alexithymia
Alexithymia assessment was performed using the 20-item Toronto Alexithymia Scale (TAS-20), a 5-point Likert-type questionnaire that assesses the degree of difficulty in identifying and describing emotions. TAS-20 has three factors, including difficulty identifying feelings (DIF), difficulty describing feelings to others (DDF) and an externally oriented style of thinking (EOT).8 The Chinese version of TAS-20 has fair internal consistency (Cronbach’s α=0.645, 0.630 and 0.581, respectively) and test–retest reliability (r=0.782, 0.687 and 0.893, respectively).8
Clinimetric assessment of resilience
A clinimetric evaluation of resilience was determined by the Connor-Davidson Resilience Scale (CD-RISC), a 5-point scale (0–4) with higher scores reflecting greater resilience.16 The Chinese version of CD-RISC is a 25-item instrument with three factors (ie, tenacity, strength and optimism), which shows a good reliability coefficient (0.91).17 Tenacity encompasses 13 items (ie, items 11–23) describing an individual’s equanimity, promptness, perseverance, and sense of control when facing situations of hardship and challenge. Strength includes eight items (ie, items 1, 5, 7–10, 24 and 25) assessing an individual’s capacity to recover and become strong after setbacks and overcome past experiences. The optimism factor consists of items 2, 3, 4 and 6, which measure an individual’s confidence in resisting adverse events.
Stress assessment
The students’ stress was assessed by the College Student Stress Questionnaire (CSSQ), a 30-item scale.18 CSSQ measures seven aspects of stress (ie, seven subscales): economy, adaption, love, self-abasement, interpersonal relationships, employment and academic performance. Each item encompasses five statements, rated from ‘no stress’ (1) to ‘extreme stress’ (5), with total scores ranging from 0 to 150. The Cronbach’s α coefficient of CSSQ is 0.959, showing a good reliability.
Statistical analysis
A Mann-Whitney U test or a Kruskal-Wallis test was used to compare group differences in the CD-RISC scores among the categorical variables. Spearman correlation analysis was employed to evaluate the associations between resilience and alexithymia and between resilience and stress (Bonferroni correction).
PROCESS was applied to test the mediating effect of resilience between alexithymia and stress. We used an exploratory parallel multiple mediator model to evaluate the associations of the three factors of CD-RISC between alexithymia and stress.
Results
Demographic information of students
Table 1 shows the demographics of students. Approximately 81.28% of the students were female, and 64.68% indicated average academic performance. About 45.96% of the students came from the countryside or 53.19% came from only-child families. In addition, 72.34% of students came from homes with an average family income, and 32.98% were first-year college students.
Table 1.
Demographics of college students in the survey
| Demographic characteristics | Number (n) | Percentage (%) | |
| Gender (n=470) |
Male | 88 | 18.72 |
| Female | 382 | 81.28 | |
| Academic performance (n=470) |
Good | 84 | 17.87 |
| Average | 304 | 64.68 | |
| Poor | 82 | 17.45 | |
| Home location (n=470) |
City or town | 254 | 54.04 |
| Countryside | 216 | 45.96 | |
| Only-child family (n=470) |
Yes | 250 | 53.19 |
| No | 220 | 46.81 | |
| Family income (n=470) |
High | 95 | 20.21 |
| Average | 340 | 72.34 | |
| Low | 35 | 7.45 | |
| College grade level (n=470) |
Grade 1 | 155 | 32.98 |
| Grade 2 | 113 | 24.04 | |
| Grade 3 | 95 | 20.21 | |
| Grade 4 | 56 | 11.91 | |
| Grade 5 | 51 | 10.85 | |
Comparisons of resilience between different groups
In this study, we divided the students into various groups according to demographic information. As shown in table 2, no significant differences in the total CD-RISC and its subscales were found between different genders, academic performance, home location, only-child family status, family income and college grade level (all p>0.05).
Table 2.
Comparisons of resilience in college students by demographics
| Items | CD-RISC | Tenacity | Self-improvement | Optimism | |
| Gender | Male (n=88) | 56 (50, 69.50) | 28 (24, 33.75) | 20 (17, 24) | 9 (8, 11) |
| Female (n=382) | 56 (49, 65) | 28 (24, 33) | 20 (17, 23) | 9 (8, 11) | |
| Z value* | −0.375 | −0.218 | −0.643 | −0.021 | |
| P value | 0.707 | 0.828 | 0.520 | 0.984 | |
| Home location | City or town (n=254) | 56.50 (49, 67) | 28 (24, 34) | 20 (17, 23) | 9 (8, 11) |
| Countryside (n=216) | 56 (50, 63.75) | 28 (25, 31.75) | 20 (17, 23) | 9 (8, 11) | |
| Z value* | −0.745 | −1.050 | −0.216 | −1.291 | |
| P value | 0.456 | 0.294 | 0.829 | 0.197 | |
| Only-child family | Yes (n=250) | 56 (49, 65) | 28 (25, 33) | 20 (17, 23) | 9 (8, 11) |
| No (n=220) | 56 (49, 65.50) | 27 (24, 33) | 20 (17, 23) | 9 (8, 11) | |
| Z value | −0.414 | −0.766 | −0.167 | −0.309 | |
| P value | 0.679 | 0.444 | 0.868 | 0.757 | |
| Academic performance | Good (n=84) | 56 (50, 65) | 27 (24, 32.25) | 18 (17, 23) | 10 (8, 11) |
| Average (n=304) | 56 (49.25, 64.75) | 28 (24, 33) | 20 (17, 23) | 9 (8, 11) | |
| Poor (n=82) | 57 (48, 68) | 28 (23, 34) | 20 (17, 23) | 9 (7, 11) | |
| χ2† | 0.006 | 0.059 | 0.525 | 0.776 | |
| P value | 0.997 | 0.971 | 0.769 | 0.678 | |
| Family income | High (n=95) | 59 (51, 69) | 29 (26, 35) | 20 (17, 23) | 10 (8, 11) |
| Average (n=340) | 56 (49, 64) | 27.5 (24, 33) | 20 (17, 23) | 9 (8, 11) | |
| Low (n=35) | 55 (50, 71.75) | 27 (24, 37.25) | 20 (17, 23.75) | 9 (8, 11) | |
| χ2† | 2.752 | 4.151 | 0.700 | 2.289 | |
| P value | 0.253 | 0.126 | 0.705 | 0.318 | |
| College grade level | Grade 1 (n=155) | 56 (48, 64) | 27 (24, 32) | 20 (16, 23) | 9 (8, 11) |
| Grade 2 (n=113) | 56 (50, 64) | 28 (24, 32) | 20 (16.50, 23) | 9 (7, 11) | |
| Grade 3 (n=95) | 56 (51, 67) | 28 (24, 34) | 20 (17, 23) | 10 (8, 11) | |
| Grade 4 (n=56) | 56.50 (49, 66) | 28 (25, 33) | 19.50 (17, 22.75) | 9 (8, 11) | |
| Grade 5 (n=51) | 56 (50, 67) | 28 (25, 35) | 20 (17, 23) | 9 (8, 10) | |
| χ2† | 0.845 | 1.028 | 0.244 | 3.465 | |
| P value | 0.932 | 0.905 | 0.993 | 0.483 | |
Data are expressed as median (quartile 1, quartile 3).
*Mann-Whitney U test.
†Kruskal-Wallis test.
CD-RISC, Connor-Davidson Resilience Scale.
Correlations of resilience, alexithymia and stress
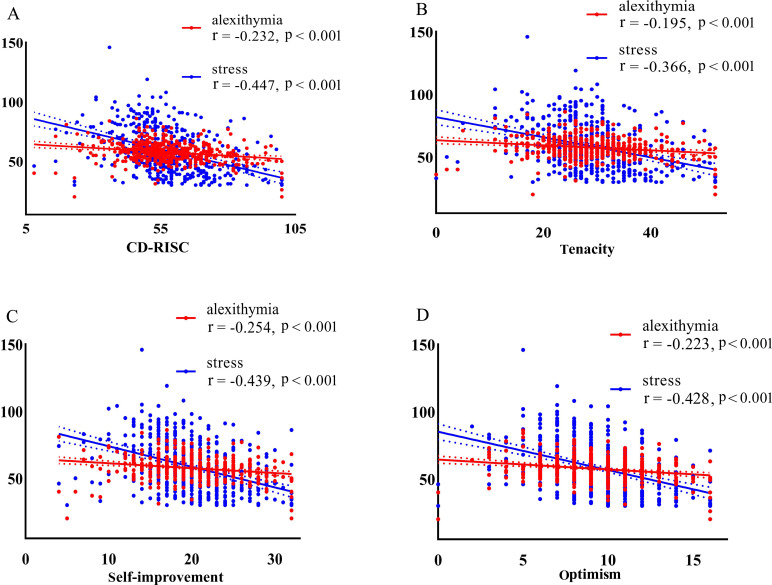
Figure 1 illustrates significant associations (uncorrected) between CD-RISC and other scales. CD-RISC (r=−0.232, p<0.001, figure 1A), tenacity (r=−0.195, p<0.001, figure 1B), self-improvement (r=−0.254, p<0.001, figure 1C) and optimism (r=−0.223, p<0.001, figure 1D) were all negatively correlated with TAS-20, and also negatively correlated with stress (r=−0.447, p<0.001; r=−0.366, p<0.001; r=−0.439, p<0.001; r=−0.428, p<0.001, respectively).
Figure 1.
Correlations between (A) CD-RISC and TAS-20, stress, respectively; (B) tenacity and TAS-20, stress; (C) self-improvement and TAS-20, stress; (D) optimism and TAS-20, stress, respectively. CD-RISC, Connor-Davidson Resilience Scale; TAS-20, Toronto Alexithymia Scale-20.
Mediating effect of resilience between alexithymia and stress
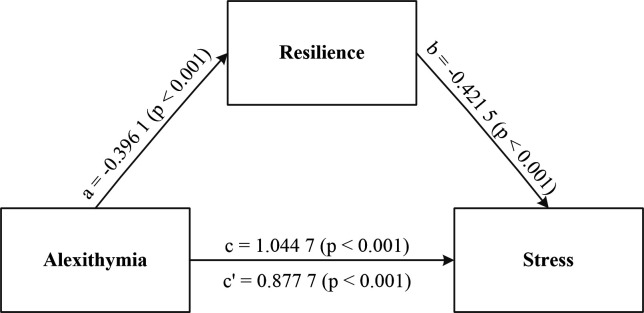
The current study found that alexithymia influenced stress in direct and indirect ways (see figure 2).
Figure 2.
Unstandardised regression coefficients for the relationship between alexithymia and stress as mediated by resilience. a, b, c and c′ are standardised path coefficients.
The direct effect of alexithymia on stress was significant when controlling for resilience (c’=0.877 7; 95% CI: 0.697 to 1.058). Meanwhile, the indirect effect also showed statistical significance (effect=0.167 0, 95% CI: 0.069 to 0.281). Moreover, the total effect of alexithymia on stress was 1.044 7 (c=1.044 7, 95% CI: 0.858 to 1.231).
A multiple mediator model test was employed to explain which aspect of resilience could mediate alexithymia and stress. A bootstrapped 95% CI confirmed that the indirect effect of alexithymia had an impact of 0.167 0 that was produced by resilience as a mediator on stress (95% CI: 0.069 to 0.281). Alexithymia significantly affected all three factors of resilience (all p<0.001, table 3). However, only two factors of resilience (ie, self-improvement and optimism) significantly affected stress. For the indirect paths, alexithymia could affect stress through self-improvement and optimism (ie, the CI did not straddle 0). The indirect pathway via tenacity had no statistical significance (95% CI: −0.077 to 0.052). Therefore, self-improvement and optimism mediate the relationship between alexithymia and stress in medical students.
Table 3.
Mediating effect of resilience subscales between alexithymia and stress
| Coefficient | SE | t value | P value | |
| Alexithymia → resilience (mediator) | ||||
| Alexithymia → tenacity | −0.193 | 0.044 | −4.358 | <0.001 |
| Alexithymia → self-improvement | −0.129 | 0.027 | −4.804 | <0.001 |
| Alexithymia → optimism | −0.074 | 0.014 | −5.175 | <0.001 |
| Resilience → stress (after controlling for Alexithymia) | ||||
| Tenacity → stress | 0.034 | 0.160 | 0.214 | 0.831 |
| Self-improvement → stress | −0.825 | 0.273 | −3.028 | 0.003 |
| Optimism → stress | −1.324 | 0.369 | −3.594 | 0.004 |
| Effect | Boot SE | Boot lower limit CI | Boot upper limit CI | |
| Indirect path of alexithymia to stress | ||||
| Alexithymia → tenacity → stress | −0.007 | 0.032 | −0.077 | 0.052 |
| Alexithymia → self-improvement → stress | 0.106 | 0.054 | 0.024 | 0.231 |
| Alexithymia → optimism → stress | 0.098 | 0.042 | 0.030 | 0.191 |
CI, confidence interval; SE, standard error.
Discussion
Main findings
As the relationship between alexithymia and stress in medical students during the COVID-19 pandemic has been largely unexplored, this study examined whether resilience can explain this association. It was the first study to investigate the role of resilience as a mediator between alexithymia and stress in medical students during the recent pandemic lockdown. The current study indicated that students who reported stress or alexithymia exhibited lower resilience. It was found that tenacity, self-improvement and optimism were strongly negatively correlated with stress and alexithymia. Mediation analysis revealed that resilience was a mediator between alexithymia and stress.
A moderate correlation was found between alexithymia and resilience total and subscale scores. This finding was consistent with several previous studies that explored the relationship between alexithymia and resilience in general populations,14 depressive patients19 and patients after kidney transplantation.20 The negative correlation between alexithymia and resilience is very easy to understand, especially during the COVID-19 pandemic. Alexithymia is a defence mechanism when an individual experiences a traumatic event, such as the COVID-19 outbreak and the ensuing lockdown. Resilience is the ability to withstand and recover from mental hardship effectively.21 However, individuals with higher alexithymia use avoidance as a coping strategy rather than problem-solving and positive thinking, and they have less social support.22 For example, emotion-focused coping was more common than problem-focused coping in individuals with alexithymia, as it aimed to regulate the emotional experience of the stressful event.23 As a matter of fact, positive coping strategies are to some extent consistent with resilience, both of which are positive attempts when people face unpleasant situations. For example, individuals with alexithymia might find it more challenging to cope with stressful events and find it more difficult to use positive coping strategies. Furthermore, they will more likely feel less emotional support from families or friends.
We found negative correlations between resilience and stress in medical students; similar results had been supported by other studies about students.21 24 One epidemiological investigation found that the number of students accessing university counselling services grew by 50% from 2010 to 2015.24 To some degree, the lowered resilience of students could explain this increase in help-seeking, as it could also affect their academic performance, sense of coherence and quality of life.13 Seemingly, the COVID-19 pandemic has made the negative relationship between resilience and stress stronger. Medical students’ stressors, such as class interruptions, concerns about personal or family health, and social isolation from peers, resulted in undesirable changes in behaviour, difficulty concentrating and increased use of negative coping strategies.25 This implies that students may have had higher levels of resilience before the pandemic.
Our finding that resilience was a mediator between alexithymia and stress supports results from previous studies that reported resilience mediated the associations between interpersonal relationships and depression,26 as well as loneliness and depression.27 In this study, the first critical path in the mediation model was that alexithymia was a forerunner to severe stress, consistent with findings from a cross-sectional study indicating that alexithymia was the strongest predictor of social stress.28 As evidenced, individuals with high alexithymia exhibited elevated subjective negative affect.29 Furthermore, negative emotions resulted in various types of stress, including impaired interpersonal relationships, academic performance and romantic relationships.30 During the COVID-19 pandemic, limited social activity may have passively increased students’ perceived stress, especially for those with high alexithymia. Another important path in this mediation model was resilience indirectly accounted for the link between alexithymia and stress. Although serious alexithymia could increase medical students’ pressure, resilience was found to effectively relieve it, as supported by Romano et al.30 According to the authors, resilience mediated the relationship between alexithymia and academic burnout. Therefore, our study indicated that resilience played a vital role in relieving stress and alexithymia in medical students.
Limitations
Our study has a few limitations. First, while the sample size studied was relatively large, the complex relationships between resilience, alexithymia and stress warrant larger sample sizes for study. Second, all data were obtained through self-report scales, which could induce response bias; the associations between variables may be under-or-over-estimated by participants. Furthermore, the generalisation of our results should be taken with caution because the results obtained from our study sample may be not applicable to other populations.
Implications
Although we cannot make a definitive conclusion on the causal links based on the present investigation, our findings showed that resilience could relieve the negative effect of alexithymia on stress in medical students during the COVID-19 pandemic. These results provide helpful evidence for universities to attend to students’ psychological resilience. Psychotherapy is one means of improving levels of resilience.
Biography
Yuqun Zhang, graduated from the School of Medicine at Southeast University in Nanjing, China in June 2017 with a PhD in neurology. She has worked as a lecturer at the Nanjing University of Chinese Medicine in the School of Nursing in China since 2017. She has authored more than 40 refereed research papers and presided over five research projects, including the National Natural Science Foundation of China, the Qinglan Project from Jiangsu Province, the Natural Science Foundation of Jiangsu Province, the Natural Science Foundation of Jiangsu Higher Education Institutions and Philosophy, and the Social Science Foundation of Jiangsu Higher Education Institutions in China. She was awarded a second prize of the Science and Technology Progress Award of the Ministry of Education and a first prize of Jiangsu Province Medical New Technology Introduction Award. In addition, she has contributed to three books and two sets of teaching materials for undergraduate medical students. Her main research interests include neuroimaging mechanisms of postpartum depression and the psychotherapeutic mechanisms of cognitive behaviour therapy for psychosomatic disorders.

Footnotes
YZ and TW contributed equally.
Contributors: YZ as the guarantor, also designed this study, analysed data and wrote the manuscript. TW collected the data and wrote the manuscript. SJ, HZ, LC and SD modified the manuscript.
Funding: This work was funded by Qing Lan Project of Jiangsu Higher Education Institutions, National Natural Science Foundation of China (grant number 82001426) and School-based Youth Project Funding (grant number NZY82001426).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the recommendations of the ethics committee (Zhongda Hospital, Southeast University, Nanjing, China, No. 2021ZDSYLL142-Y01) with written informed consent from all subjects. It is in accordance with the declaration of Helsinki. Participants gave informed consent to participate in the study before taking part.
References
- 1. Wilkes C, Lewis T, Brager N, et al. Wellbeing and mental health amongst medical students in Canada. Int Rev Psychiatry 2019;31:584–7. 10.1080/09540261.2019.1675927 [DOI] [PubMed] [Google Scholar]
- 2. Zis P, Artemiadis A, Bargiotas P, et al. Medical studies during the COVID-19 pandemic: the impact of digital learning on medical students' burnout and mental health. Int J Environ Res Public Health 2021;18:349. 10.3390/ijerph18010349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Karyotaki E, Klein AM, Riper H, et al. Examining the effectiveness of a web-based intervention for symptoms of depression and anxiety in college students: study protocol of a randomised controlled trial. BMJ Open 2019;9:e028739. 10.1136/bmjopen-2018-028739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mahapatra A, Sharma P. Case series associated with COVID-19 pandemic in causing psychiatric morbidity. Gen Psychiatr 2021;34:e100343. 10.1136/gpsych-2020-100343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ma Z, Zhao J, Li Y, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci 2020;29:e181. 10.1017/S2045796020000931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu M, Xu W, Yao Y, et al. Mental health status of students' parents during COVID-19 pandemic and its influence factors. Gen Psychiatr 2020;33:e100250. 10.1136/gpsych-2020-100250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tang W, Hu T, Yang L, et al. The role of alexithymia in the mental health problems of home-quarantined university students during the COVID-19 pandemic in China. Pers Individ Dif 2020;165:110131. 10.1016/j.paid.2020.110131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yuan Y, Shen X, Zhang X, et al. The reliability and validity of Toronto Alexithymia Scale (TAS-20). Sichuan Ment Health 2003;16:25–7. [Google Scholar]
- 9. Mei S, Xu G, Gao T, et al. The relationship between college students' alexithymia and mobile phone addiction: testing mediation and moderation effects. BMC Psychiatry 2018;18:329. 10.1186/s12888-018-1891-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang Y, Zhao Y, Mao S, et al. Investigation of health anxiety and its related factors in nursing students. Neuropsychiatr Dis Treat 2014;10:1223–34. 10.2147/NDT.S61568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van der Merwe LJ, Botha A, Joubert G. Resilience and coping strategies of undergraduate medical students at the University of the Free State. S Afr J Psychiatr 2020;26:1471. 10.4102/sajpsychiatry.v26i0.1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Noreen A, Iqbal N, Hassan B, et al. Relationship between psychological distress, quality of life and resilience among medical and non-medical students. J Pak Med Assoc 2021;71:2181–5. 10.47391/JPMA.04-611 [DOI] [PubMed] [Google Scholar]
- 13. Lin YK, Lin C-D, Lin BY-J, et al. Medical students' resilience: a protective role on stress and quality of life in clerkship. BMC Med Educ 2019;19:473. 10.1186/s12909-019-1912-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Osimo SA, Aiello M, Gentili C, et al. The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front Psychol 2021;12:630751. 10.3389/fpsyg.2021.630751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang C, Ye M, Fu Y, et al. The psychological impact of the COVID-19 pandemic on teenagers in China. J Adolesc Health 2020;67:747–55. 10.1016/j.jadohealth.2020.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 17. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Pers 2007;35:19–30. 10.2224/sbp.2007.35.1.19 [DOI] [Google Scholar]
- 18. Zhu J. A study on the influencing factors of college students’ pressure—a case study of university in Nanchang. Nanchang, China: M.S. Jiangxi University of Finance and Economics, 2017. [Google Scholar]
- 19. De Berardis D, Fornaro M, Valchera A, et al. Alexithymia, resilience, somatic sensations and their relationships with suicide ideation in drug naïve patients with first-episode major depression: an exploratory study in the "real world" everyday clinical practice. Early Interv Psychiatry 2020;14:336–42. 10.1111/eip.12863 [DOI] [PubMed] [Google Scholar]
- 20. Tomaszek A, Wróblewska A, Zdankiewicz-Ścigała E, et al. Post-traumatic growth among patients after living and cadaveric donor kidney transplantation: the role of resilience and alexithymia. Int J Environ Res Public Health 2021;18:2164 10.3390/ijerph18042164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bacchi S, Licinio J. Resilience and psychological distress in psychology and medical students. Acad Psychiatry 2017;41:185–8. 10.1007/s40596-016-0488-0 [DOI] [PubMed] [Google Scholar]
- 22. Polloni L, DunnGalvin A, Ferruzza E, et al. Coping strategies, alexithymia and anxiety in young patients with food allergy. Allergy 2017;72:1054–60. 10.1111/all.13097 [DOI] [PubMed] [Google Scholar]
- 23. Di Tella M, Tesio V, Ghiggia A, et al. Coping strategies and perceived social support in fibromyalgia syndrome: relationship with alexithymia. Scand J Psychol 2018;59:167–76. 10.1111/sjop.12405 [DOI] [PubMed] [Google Scholar]
- 24. Galante J, Dufour G, Vainre M, et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet Public Health 2018;3:e72–81. 10.1016/S2468-2667(17)30231-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fuentes AV, Jacobs RJ, Ip E, et al. Coping, resilience, and emotional well-being in pharmacy students during the COVID-19 pandemic. Ment Health Clin 2021;11:274–8. 10.9740/mhc.2021.09.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee TS-H, Wu Y-J, Chao E, et al. Resilience as a mediator of interpersonal relationships and depressive symptoms amongst 10th to 12th grade students. J Affect Disord 2021;278:107–13. 10.1016/j.jad.2020.09.033 [DOI] [PubMed] [Google Scholar]
- 27. Zhao X, Zhang D, Wu M, et al. Loneliness and depression symptoms among the elderly in nursing homes: a moderated mediation model of resilience and social support. Psychiatry Res 2018;268:143–51. 10.1016/j.psychres.2018.07.011 [DOI] [PubMed] [Google Scholar]
- 28. Popa-Velea O, Diaconescu L, Mihăilescu A, et al. Burnout and its relationships with alexithymia, stress, and social support among Romanian medical students: a cross-sectional study. Int J Environ Res Public Health 2017;14:560. 10.3390/ijerph14060560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Connelly M, Denney DR. Regulation of emotions during experimental stress in alexithymia. J Psychosom Res 2007;62:649–56. 10.1016/j.jpsychores.2006.12.008 [DOI] [PubMed] [Google Scholar]
- 30. Romano L, Buonomo I, Callea A, et al. Alexithymia in young people's academic career: the mediating role of anxiety and resilience. J Genet Psychol 2019;180:157–69. 10.1080/00221325.2019.1620675 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.