Abstract
Objective
Emergency service workers are at risk of experiencing poor mental health due to repeated exposure to potentially traumatic events. Promoting healthy lifestyle factors may help improve health outcomes and quality of life among this population. This study aimed to evaluate the efficacy of a 10-week physical activity (PA) and diet programme delivered via Facebook for sedentary emergency service workers and their support partners on levels of psychological distress.
Methods
We delivered a 10-week intervention via a private Facebook group facilitated by exercise physiologists, a dietitian and peer-facilitators. Weekly education modules and telehealth calls were delivered, and participants were provided with a PA tracking device (Fitbit accelerometer). A stepped-wedge design was applied to compare levels of psychological distress (K6) during baseline, to intervention by comparing slopes of change. Secondary pre–post outcomes included mental health symptoms, PA, quality of life, social support to exercise, sleep quality and suicidal ideation.
Results
In total, N=90 participants (n=47 emergency service workers and n=43 support partners) were recruited in 4 cohorts (aged 42.3±11.5 years, 51% male). Levels of psychological distress did not change significantly during the baseline (control) slope and reduced significantly during the first 6 weeks of intervention (intervention slope 1). The slopes were significantly different, b=−0.351, p = 0.003 (i.e. the trajectories of change) and improvements plateaued until follow up. Retention was high (92%) and improvements in mental health symptoms, minutes of PA, sedentary time and quality of life were significant.
Conclusions
Our intervention delivered via social media is feasible and associated with reduced levels of psychological distress among emergency service workers and support partners.
Trial registration
Australian New Zealand Clinical Trials Registry (ACTRN): 12619000877189.
Keywords: first-responders, exercise, lifestyle behaviours, mental health, social media
Introduction
There are currently over 115,000 full time and 235,000 volunteer emergency service workers in Australia, including paramedics, fire fighters, police officers and state emergency service workers.1 People in these occupations work to ensure public health and safety and in doing so are regularly exposed to significant occupational stressors and potentially traumatic events including violence, natural disasters and death.2 Emergency service workers are subsequently at increased risk of developing mental health disorders including depression, anxiety and post-traumatic stress disorder (PTSD).3 A 2018 national survey of emergency services personnel across Australia found that approximately 25% of people currently employed were experiencing high levels of psychological distress and 10% met diagnostic criteria for PTSD,1 compared to 4% in the general population.4 The rates of mental disorders among former employees were even higher,5 with rates of PTSD estimated to be 23%.1 A potential consequence of these mental health issues is high rates of suicidal thoughts and behaviours.1 In Australia, one emergency service worker dies by suicide approximately every 4 weeks.6 Maintaining and promoting the mental health of this workforce is essential, not only for employees but for the broader community who rely on their services.
In addition to trauma exposure, emergency service workers face other occupational risks including shift work and highly stressful work environments. Common consequences associated with shift work include poor sleep,7 poor diet8 and low levels of physical activity.9 In addition, the emergency service worker's role typically involves primarily sedentary tasks (e.g. desk work or sitting in a vehicle), with only occasional periods of intense physical exertion.10 Sedentary behaviour and physical inactivity are modifiable behaviours associated with an increased risk of poor mental health.11 These occupational risk factors also lead to poor physical health outcomes including high rates of hypertension and obesity which are commonly seen in emergency service workers.12–14
There is increasing academic and clinical interest in the role of lifestyle interventions targeting physical activity and nutrition behaviours to simultaneously improve physical and mental health.15,16 Physical activity and its structured subset, exercise, can improve mood and reduce psychiatric symptoms among people with diagnosed mental disorders as well as sub-clinical populations experiencing mental health symptoms.17,18 A study among paramedics found that sleep and physical activity explained a significant level of variance in trauma response (35%), indicating likely protective effects of such behaviours and the role of lifestyle interventions as a potentially feasible first-line mental health strategy.19,20 Another study found that exercise participation and high cardiorespiratory fitness can help police officers to better cope with chronic stress and subsequently take less sick leave.21
Emergency service workers therefore require tailored interventions to help overcome some of the adverse health consequences of their work. Some evidence demonstrates that emergency workers may be more likely to engage in tailored lifestyle interventions compared to traditional mental health therapies as perceived stigma still exists amongst this population regarding psychotherapeutic and pharmaceutical interventions.22 Despite the known mental health and cardioprotective benefits of exercise, there is limited research investigating the role and ways of engaging emergency service workers in such interventions.20
Social support is a protective factor against PTSD, yet social connections are often lost when people experience mental health issues.23 This also includes the families of emergency service workers who share the burden and impacts of trauma exposure and workplace stress.24 Enhancing social resources can therefore help buffer the effects of loss-related events and is an important health behaviour change strategy.25 Social resources can be proximal including family members and spouses, and distal including friendships with peers. Therefore, group health promotion interventions and the inclusion of already established social networks may be a useful strategy to maximise physical activity adherence.
Over a third of the world's population (38%) use social media sites such as Facebook, Instagram and WhatsApp.26 Given the rapid growth in the use and availability of social media, it may be a scalable and potentially cost-effective opportunity to deliver health promotion interventions to Australia's geographically dispersed emergency service workforce.27 Online delivery offers flexibility for emergency workers and families to access the intervention in their own time, and based on findings among other populations, can provide social resources through interactions and support between peers.28
Strategies to help mitigate the mental and physical health consequences of emergency service work and trauma exposure are needed. Physical activity and diet are modifiable risk factors, yet to date there have been no studies delivered online targeting these health behaviours among emergency service workers. The aim of this study was therefore to evaluate the efficacy of a mental health informed 10-week physical activity and diet programme delivered via Facebook for sedentary emergency service workers and their chosen support partners. The effect of the programme on psychological distress (primary outcome), depression, anxiety and stress, physical activity levels, sleep quality, quality of life, social support to exercise and suicidal ideation were assessed. We hypothesised that participation in the intervention would be associated with reduced levels of psychological distress.
Methods
Study design
This study applied a stepped-wedge cluster design to test the impact of the intervention on emergency service worker and support partner outcomes. This involved the sequential roll out of the intervention to four closed cohort clusters over time. While randomised controlled trials (RCTs) are considered the ‘gold standard’ methodology for evaluating clinical effectiveness by establishing a cause–effect relationship,29 there are situations where they may not be the most appropriate study design, for example, if there is a prior belief that that the intervention will do more good than harm, then it may be unethical to withhold the intervention from participants.30 Based on the extant literature on lifestyle interventions improving physical and mental health outcomes15,17 we therefore used the stepped-wedge design as an alternative. This allowed all participants to have timely access to the lifestyle intervention while maintaining the research strengths associated with an RCT.
The trial was registered with the Australian and New Zealand Clinical Trails registry (ACTRN12619000877189) and approved by the UNSW Human Research Ethics Committee HC180561. The study is reported in line with the CONSORT 2010 checklist extension for stepped-wedge cluster randomised trials.31 The study protocol has been published elsewhere32 and was informed by pilot work.33
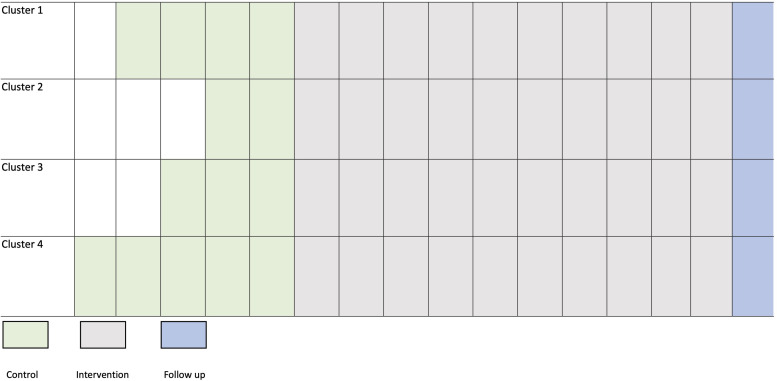
Data were collected on multiple occasions before the intervention (baseline) to detect whether the intervention had an effect significantly greater than the underlying secular trend during baseline. Consecutive observations were interrupted by the intervention to see if the slope (rate of change over time) or level (mean starting point) of the time series changed following the intervention. Participants were recruited into successive clusters and the baseline lengths of each cluster were randomised between 2 and 5 weeks with treatment introduced at different times for each cluster to control for the effects of time as shown in Figure 1. A random number generator in excel was used to allocate the baseline length of each cluster in random order.
Figure 1.
Stepped-wedge cluster design with 4 clusters and baseline lengths randomised between 2 and 5 weeks, followed by a 10-week intervention and 1-month follow up. Each square represents 1 week.
Participants
Participants were recruited between August 2019 and July 2021 through Behind the Seen, a not-for-profit, ex-service organisation that aims to increase awareness and reduce stigma towards mental health issues faced by emergency service workers and their families.34 The Behind the Seen facilitators posted the study advertisement on their Facebook page. Interested participants contacted the research team who provided information about the study and a link to the online screening questionnaires. The screening questionnaires including the Exercise and Sports Science Australia (ESSA) exercise pre-screening tool,35 the Physical Activity Vital Sign (PAVS),36 the Kessler-6 (K6)37 and the Suicidal Ideation Attributes Scale (SIDAS).38 A member of the research team then checked the questionnaire responses to determine eligibility based on the following criteria: (i) former or current emergency service worker; (ii) aged 18–65 years; (iii) currently physically inactive based on World Health Organisation guidelines and defined as engaging in <150 minutes of moderate to vigorous physical activity (MVPA) per week; (iv) absence of any absolute contraindications to exercise as per the ESSA exercise pre-screening tool; (v) English speaking and (vi) internet and Facebook access.
Participants were excluded if they: (i) scored >25 in the K6 (indicative of very high levels of psychological distress) and were not receiving treatment and/or medication had changed in the previous 4 weeks, (ii) scored ≥21 in the SIDAS (indicative of a high risk of suicidal behaviour) and determined ineligible based on a suicide risk assessment conducted by a clinical psychologist on the research team. The suicide risk assessment guide to determine high, medium and low risk to determine their suitability of taking part and the most appropriate response. Participants of high risk would be immediately referred to the acute care team and excluded from the study. Participants with medium risk would be referred for appropriate mental health support and their participation in the study will be discussed with the medical or psychological practitioner. Participants of low risk could take part.
Eligible emergency service workers were required to nominate a support partner to participate in the programme with them. This was defined as any person with a close personal relationship to the emergency service worker (e.g. spouse, family member, caregiver or close friend). The support partner was required to be (i) aged between 18 and 65 years; (ii) absence of any absolute contraindications to exercise as per the ESSA exercise pre-screening tool; (iii) English speaking and (iv) internet and Facebook access. The same exclusion criteria for support partners were used. Monte Carlo simulations conducted in Mplus8 using our pilot data (psychological distress (K6)) showed that a sample size of n=80 would be sufficient to achieve power of 80% with the p-value set at 0.05.33
Intervention
Participants were enrolled in a 10-week physical activity programme delivered via a private Facebook group. The programme was delivered in separate Facebook groups to four clusters. The Facebook group was co-facilitated by exercise physiologists and a dietitian with mental health expertise39 and peer-facilitators.40 The same staff were used for each cohort.
Exercise physiologists and dietitian
The exercise physiologists provided education and encouraged discussions on different predetermined weekly topics including goal setting, overcoming barriers, reducing sedentary behaviour and nutrition. A detailed description of the weekly content has been previously published.32 The intervention content was designed in accordance with mental health and trauma-informed principles for physical activity.41 For example, the intervention considered the specific barriers to engaging in physical activity and healthy lifestyle behaviours health often experienced by people living with poor mental health including low motivation, mood and fatigue. The intervention was tailored around individual choices and preferences and involved encouraging participants to participate in meaningful activity which they enjoy. In addition, the facilitators focused on building self-efficacy and empowerment, helping participants to identify individual strengths and support networks to improve their lifestyle behaviours. The content was informed by the qualitative feedback from our pilot study and based on behaviour change techniques including fostering social support, self-monitoring and shaping knowledge.42 All aspects of the programme were co-developed with the facilitators of the community organisation (Behind the Seen), who have lived experience of both working as an emergency service worker, living with PTSD and being a spouse of an emergency worker. In addition, the facilitators had both research and clinical experience in mental health.
The exercise physiologists posted 3 to 4 times per week and monitored the Facebook group daily from Monday to Friday. The dietitian led 1 week of the intervention which focused on nutrition. The group aims and rules were pinned to the Facebook group so that they were always accessible for participants. Rules included being respectful of other people's opinions, zero tolerance of rude or hurtful comments, ensuring confidentiality of participants of the group and no sharing of personally identifiable information of others without their permission. Any harmful content which did not align with the aims of the group would be deleted.
Peer-facilitators
The peer-facilitators were participants from previous clusters of the programme who expressed interest to volunteer to take part in a subsequent cluster to help motivate and support other participants. Peer-facilitators in the first cluster were recruited from our pilot study.33 Participants who expressed interest were ‘graduated’ into the role of peer-facilitator for the subsequent cluster of the programme and co-delivered the succeeding programme with the exercise physiologists. The peer-facilitators were selected based on their engagement with the programme, rather than their physical activity levels or experience. The peers were encouraged to post on the Facebook group, participate in weekly group video calls with the facilitators and self-disclose their journey with participants in the group where they were comfortable doing so. No formal training was provided, however the study exercise physiologists had regular meetings with the peer-facilitators to check in, discuss any concerns and review the progress of the programme. The peer-facilitators helped to establish trust and collaboration, two key trauma informed principles.
The exercise physiologists and peer-facilitators co-hosted two weekly group video calls via Zoom which lasted approximately 30 minutes. Participants were encouraged to call into a single session per week. The study exercise physiologists led the video call focusing on the weekly topic and giving participants an opportunity to reflect on the content posted on the Facebook group, ask questions and share their experiences with each other and also the peers and facilitators. The telehealth calls also provided an opportunity for face-to-face social connection. All participants were given a physical activity tracking device (Fitbit Inspire) and the facilitators set up step count challenges using the Fitbit app which involved competing for the highest overall team step count over 4 weeks between emergency workers versus support partners.
Outcomes
Data collection
Data were collected from both the emergency service workers and their support partner via self-report questionnaires. We compared emergency service workers and support partners on key baseline demographics including psychological distress and physical activity levels. All pre-screening and outcome measure data were collected and managed using REDCap electronic data capture tool hosted and managed by Research Technology Services (UNSW Sydney).
Multiple baseline data
Primary outcome
The primary outcome was psychological distress. This was measured using the K6 which is a reliable and valid, 6-item self-report questionnaire.37 The K6 uses a 5-point Likert scale with total scores ranging from 6 to 30. Total scores between 6 and 18 are classified as not having a probable serious mental illness and >18 as having a probable serious mental illness.43 Psychometric properties include good internal consistency (α=0.83) and acceptable discriminative validity.44 The K6 was assessed every week throughout the intervention including the baseline period and at the 4-week follow up.
Secondary outcomes
Physical activity (multiple baseline)
Physical activity levels were assessed weekly using the PAVS.36 The PAVS assesses weekly levels of MVPA and takes <1 minute to complete. This was assessed weekly throughout the baseline and intervention phase and again at the 4-week follow up. All other secondary outcomes were assessed prior to the 10-week intervention (baseline), at the end of 10 weeks (post-intervention) and again 4 weeks later (follow up).
Physical activity (pre, post, follow up)
The simple physical activity questionnaire (SIMPAQ) is a five-item clinical tool designed to assess physical activity among populations at high risk of sedentary behaviour.45 The SIMPAQ was adapted to an online version using REDCap. The SIMPAQ traditionally requires an interviewer to form simple calculations to account for hours left in the day based on previous answers, and our online version uses basic formulas to still allow participants to crosscheck responses based on how many hours they need to account for. Total time per week of walking, MVPA and sedentary time were assessed.
Depression, anxiety and stress
The Depression Anxiety and Stress Scale (DASS-21) is a 21-item self-report instrument that measures the related negative emotional states of depression, anxiety and stress.46 A total score and 3 separate subscales, each with 7 items, were calculated to identify severity ratings for depression, anxiety and stress. Higher scores represented more severe symptoms. For the depression domain, scores of 0 to 4 are considered normal, 5 to 6 mild, 7 to 10 moderate, 11 to 13 severe and >14 extremely severe. For anxiety, 0 to 3 is considered normal, 4 to 5 mild, 6 to 7 moderate, 8 to 9 severe, and >10 extremely severe. For stress, 0 to 7 is normal, 8 to 9 mild, 10 to 12 moderate, 13 to 16 severe, and >17 extremely severe.
PTSD symptoms
The PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5), (PCL-5) is a 20-item self-report measure that assesses symptoms of PTSD. Symptom severity scores range from 0 to 80, with a cut-off score of 33 indicating a provisional diagnosis of PTSD.47 A decrease in scores of >10 points indicates a clinically significant change; >5 points indicates a reliable change.47 The PCL-5 was only completed by the emergency service workers and not their nominated support partners.
Sleep quality
The Pittsburgh Sleep Quality Index was used to assess the quality and patterns of sleep in the past month.48 A total of 7 sub-scores were calculated to yield a global score ranging from 0 to 21. A sum of 5 or greater indicates poor sleep quality.
Quality of life
The AQoL-6D quality of life questionnaire has six separately scored dimensions and provides a summary global ‘utility’ score to describe health-related quality of life.49 Dimensions include pain, relationships, independent living, mental health, coping and senses. Total scores range from 20 to 99 with higher numbers representing better quality of life.
Social support to exercise
The social support and exercise survey was used as an assessment of the level of support individuals making health behaviour changes (exercise) felt they were receiving from family and friends.50 Two separate scores; one for friends and one for family were calculated whereby higher scores represent greater perceived support.50 It was adapted for the purpose of this study to assess the past month instead of the past 3 months.
Suicidal ideation
The SIDAS was used to assess the presence and severity of suicidal thoughts.38 It is specifically developed for online use and consists of five items, each targeting an attribute of suicidal thoughts: frequency, controllability, closeness to attempt, level of distress and impact on daily functioning. The sum of the five items is the overall score (0–50) and higher scores indicate more severe suicidal ideation. A score of >21 indicates a high risk of suicidal behaviour.
Feasibility and acceptability
Feasibility was assessed via retention which was defined as: (i) retention in the Facebook group for full duration of the 10-week study, (ii) participation in the group by actively viewing at least one post over the previous 2 weeks and (iii) not missing greater than two consecutive assessment time points. Feasibility and acceptability were also assessed at post-intervention using the 14-item feasibility and acceptability questionnaire that has been used previously to measure participant responses to a private Facebook group.51 Responses are answered on a 7-point Likert scale (strongly disagree–strongly agree).
Statistical analysis
Demographics
Descriptive baseline statistics were calculated. Comparisons between groups (emergency workers vs support partners) were assessed for the K6 (primary outcome) and physical activity levels. The chi square tests were used for categorical variables and two sample t-tests for continuous variables.
Comparing multiple baselines to intervention
To examine the effect of the intervention on the primary outcome (K6), data from each cluster was combined and an interrupted time series design was used to compare the rate of change in K6 on multiple occasions (between 2 and 5 times depending on cohort) before intervention, to the rate of change during, and following the intervention period. A piecewise latent growth curve model (LGCM) was fitted in Mplus 8 base package using the complex analysis function.52 LGCM extends traditional repeated measures analysis of variance by modelling changes in the mean and the variance of initial status (intercept) and the growth rate (slope) simultaneously. We controlled for baseline DASS-21 scores and position (emergency service worker or support partner) on the intercept. The analysis was clustered by pair (emergency service worker and support partner) to account for non-independence of observations within pairs. We note that the length of the baseline was considerably shorter than the intervention so we used the methodology outlined by Rioux et al.53 to address two key factors in modelling the intervention slope. Firstly, change may not be linear over the duration of the intervention. That is, the slope may change direction or magnitude, so there may need to be additional turning points or ‘knots’ in the slope to appropriately model changes over time. Second, there may also be a change in level at the knot point. That is, the new slope created at the knot point may have a different mean starting point (intercept) than the end of the previous slope. We used the following steps. First, visual inspection of the data was used to identify the location for a knot point. Then separate slopes were modelled for (a) baseline; (b) intervention slope 1; (c) intervention slope 2 and (d) change in level of knot points. Model constraints were used to test for significant differences between slope estimates between baseline and intervention.
Model fit was evaluated using χ2 with a scaling correction factor for multiple linear regression (MLR), comparative fit index (CFI), Tucker–Lewis index (TLI), root mean-square error of approximation (RMSEA) and standardised root mean-square residual (SRMR). Models are considered good fit if CFI > 0.95, TLI > 0.95, RMSEA < 0.05 and SRMR < 0.05, with a χ2 p-value or its scaling correction factor for MLR >0.05. The models were estimated under missing data theory using all available information.54
Pre–post intervention tests
To test for differences between pre-intervention and post-intervention in secondary outcomes, we used a multivariate omnibus test in mixed models clustered by pair (emergency service and support partnership) with cohort as a random effect, to test whether, across all five dependent variables (depression, anxiety, stress, sleep quality and quality of life) there was a significant effect. This was used to control for type 1 error. We report the Cohen's d effect sizes for all pre–post outcomes. Given a significant multivariate test, individual mixed models were then run for each dependent variable. All analyses for the pre–post tests were conducted on SPSS version 27.
Results
We recruited n=47 emergency service workers and n=43 support partners across 4 separate clusters (total N=90). The mean age across all clusters was 42.3 ±11.5 years. In total, 29 of 47 (62%) of the emergency service workers and n=17 of 43 (40%) of the support partners were male. The sample size in each cluster ranged from n=19 to n=28. In total, 37 of 47 (79%) of the emergency service workers are currently serving while 21% were retired or medically discharged. Of the total sample, 61% of emergency service/support partner pairs were spouses, 26% were friends, 9% were family members and 4% other (e.g. carer). There was no significant difference in age between emergency service workers and support partners (p = 0.08). The baseline demographics for the four clusters are shown in Table 1.
Table 1.
Participant demographics from four clusters.
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First-responder N=11 | Support partners N=11 | Total N=22 | First-responder N=11 | Support partners N=8 | Total N=19 | First-responder N=11 | Support partners N=10 | Total N=21 | First-responder N=14 | Support partners N=14 | Total N=28 | First-responder n=47 | Support partners N=43 | Total N=90 | |
| Age, mean(SD) | 40.6(13.1) | 40.2(11.1) | 40.1(11.8) | 43.7(14.4) | 46.4(12.4) | 44.8(13.3) | 48.4(10.5) | 44.0(13.0) | 46.3(11.6) | 43.2(9.2) | 35.1(6.8) | 39.2(8.9) | 43.9(11.7) | 40.8(11.3) | 42.3(11.5) |
| Sex, n(%) | |||||||||||||||
| Male | 8(73) | 4(36) | 12(55) | 6(65) | 2(25) | 8(42) | 7(64) | 5(50) | 12(57) | 8(57) | 6(43) | 14(50) | 29(62) | 17(40) | 46(51) |
| Female | 3(27) | 7(64) | 10(45) | 5(45) | 6(75) | 11(58) | 4(36) | 5(50) | 9(43) | 5(36) | 8(57) | 13(46) | 17(36) | 26(60) | 43(48) |
| Other | - | - | - | - | - | - | - | - | - | 1(7) | - | 1(4) | 1(2) | - | 1(1) |
| Smoking status, n(%) | |||||||||||||||
| No | 8(73) | 9(82) | 17(77) | 11(100) | 7(88) | 18(95) | 10(91) | 9(90) | 19(91) | 13(93) | 12(86) | 25(89) | 42(89) | 37(86) | 79(88) |
| Yes | 3(27) | 2(18) | 5(23) | - | 1(12) | 1(5) | 1(9) | 1(10) | 2(9) | 1(7) | 2(14) | 3(11) | 5(11) | 6(14) | 11(12) |
| Marital status, n(%) | |||||||||||||||
| Married | 7(64) | 7(64) | 14(63) | 4(36) | 1(13) | 5(26) | 4(36) | 4(40) | 8(38) | 6(43) | 6(43) | 12(43) | 21(45) | 18(42) | 39(43) |
| Single | 1(9) | - | 1(5) | 3(27) | 2(25) | 5(26) | 2(18) | 4(40) | 6(29) | 3(21) | 2(14) | 5(18) | 9(19) | 8(19) | 17(19) |
| De-facto | 3(27) | 3(27) | 6(27) | 2(18) | 1(13) | 3(16) | 4(36) | 2(20) | 6(20) | 5(36) | 6(42) | 11(39) | 14(30) | 12(28) | 26(29) |
| Other/prefer not say | - | 1(9) | 1(5) | 2(18) | 4(50) | 6(32) | 1(9) | - | - | - | - | 3(6) | 5(11) | 8(9) | |
| Education, n(%) | |||||||||||||||
| Primary school | - | - | - | - | - | - | 1(9) | - | 1(5) | - | 2(7) | 2(7) | 1(2) | 2(5) | 3(3) |
| High school | 1(9) | 4(36) | 5(23) | - | - | - | 1(9) | 1(10) | 2(9) | 1(8) | 3(21) | 4(14) | 3(6) | 8(19) | 11(12) |
| Diploma/certificate | 7(64) | 6(55) | 13(59) | 7(64) | 4(50) | 11(58) | 4(36) | 4(40) | 8(38) | 7(50) | 6(43) | 13(46) | 25(53) | 20(47) | 45(50) |
| Bachelor degree | 3(27) | 1(9) | 4(18) | 4(36) | 4(5) | 8(42) | 4(36) | 5(50) | 9(43) | 3(21) | 2(14) | 5(18) | 14(30) | 12(30) | 26(29) |
| Post-graduate degree | - | - | - | - | - | - | 1(9) | - | 1(5) | 3(21) | 1(7) | 4(14) | 4(14) | 1(2) | 5(5) |
| Occupation, n(%) | |||||||||||||||
| Fire | 4(36) | - | 4(18) | 5(45) | - | 5(26) | 4(36) | 1(10) | 5(24) | 7(50) | 4(29) | 11(39) | 20(43) | 5(11) | 25(28) |
| Paramedic | 4(36) | - | 4(18) | 5(45) | 1(13) | 6(32) | 4(36) | - | 4(19) | 3(22) | - | 3(11) | 16(34) | 1(2) | 17(19) |
| Police | 3(28) | 1(9) | 4(18) | 1(10) | 1(13) | 2(11) | 1(10) | - | 1(5) | 2(14) | 1(7) | 3(11) | 7(15) | 3(7) | 10(11) |
| Other ESW | - | - | - | - | 1(13) | 1(5) | 2(18) | - | 2(9) | 2(14) | 0 | 2(7) | 4(9) | 1(2) | 5(6) |
| Other (non-ESW) | - | 8(45) | 5(23) | - | - | 2(10) | - | 5(50) | 5(24) | - | 4(29) | 4(14) | - | 14(33) | 15(15) |
| Business/finance | - | 4(26) | 4(18) | - | 2(25) | 2(10) | - | 2(20) | 2(9) | - | 3(21) | 3(11) | - | 11(26) | 11(12) |
| Health professional | - | - | - | - | 1(13) | 1(5) | - | 2(20) | 2(9) | - | 2(14) | 2(7) | - | 5(12) | 5(6) |
| Home duties | - | 1(9) | 1(5) | - | 2(25) | 2(11) | - | - | - | - | - | - | - | 3(7) | 3(3) |
| Job status, n(%) | |||||||||||||||
| Current serving | 8(73) | - | - | 9(82) | - | - | 8(73) | - | - | 12(86) | - | - | 37(79) | - | 37(79) |
| Retired/discharged | 3(27) | - | - | 2(18) | - | - | 3(27) | - | - | 2(14) | - | - | 10(21) | - | 10(21) |
| Facebook use/week, n(%) | |||||||||||||||
| >3 hours | 8(73) | 6(55) | 14(64) | 6(55) | 4(57) | 10(56) | 3(27) | 4(40) | 7(33) | 7(50) | 5(36) | 12(43) | 24(51) | 19(45) | 43(48) |
| 1–2 hours | 2(18) | 2(18) | 4(18) | 3(27) | 2(29) | 5(28) | 5(46) | 2(20) | 7(33) | 5(36) | 6(43) | 11(39) | 15(32) | 12(29) | 27(30) |
| <1 hour | 1(9) | 3(27) | 4(18) | 2(18) | 1(14) | 3(17) | 3(27) | 4(40) | 7(33) | 2(14) | 3(21) | 5(18) | 8(17) | 11(26) | 19(21) |
| Relationship between pairs, n(%) | |||||||||||||||
| Spouse | - | 10(91) | 10(91) | - | 3(38) | 3(38) | - | 4(40) | 4(40) | 9(64) | 9(64) | - | 26(61) | 26(61) | |
| Friend | - | 1(9) | 1(9) | - | 3(38) | 3(38) | - | 5(50) | 5(50) | 2(14) | 2(14) | - | 11(26) | 11(26) | |
| Family member | - | - | - | - | 2(25) | 2(25) | - | 1(10) | 1(10) | 2(14) | 2(14) | - | 4(9) | 4(9) | |
| Other | - | - | - | - | - | - | - | 1(7) | 1(7) | - | 2(4) | 2(4) | |||
Note: Some percentages might not add to 100% due to rounding. ESW: emergency service worker.
At baseline, n=15 (17%) of the total sample met the cut-off score of >18 on the K6, indicating probable serious mental illness. There was no significant difference between the number of emergency service workers versus support partners meeting the cut-off (22% vs 11%, χ2 =1.74, N=90, p=0.19). Under half (n=19, 40%) of the emergency service workers met diagnostic cut-off for PTSD at baseline. Mean levels of moderate to vigorous activity were 62.3± 75.1 minutes per week among the emergency service workers and 176.7± 261.8 among the support partners. Significantly more support partners versus emergency service workers met the physical activity guidelines at baseline (37% vs 9%, (χ2 =10.31 (1, N=86), p = 0.001)).
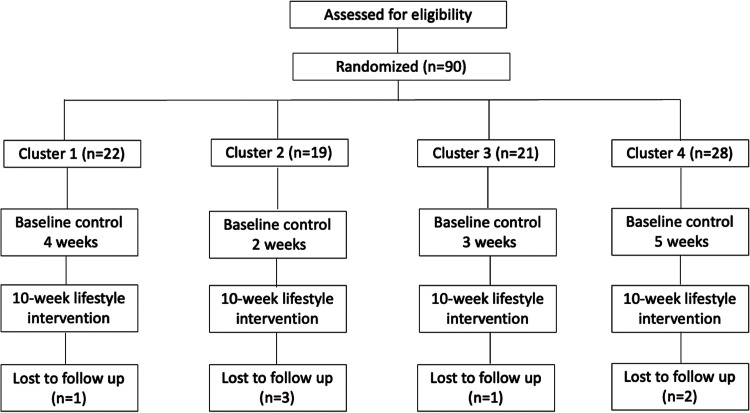
Retention was high with 83 of 90 (92%) completing the intervention. Total dropouts were n=7. Of these, n=2 dropped out during the baseline phase, n=3 before week 5 and n=2 between weeks 6 and 10. N=53 (59%) completed the 1-month follow up. The flow of participants through the trial is shown in Figure 2.
Figure 2.
Flow of participants through trial in each cluster.
Adverse events
There were no adverse events related to the study reported during the conduct of the intervention, nor was there any inappropriate behaviour, online harassment or privacy concerns in the group which needed to be removed by the facilitators.
Psychological distress
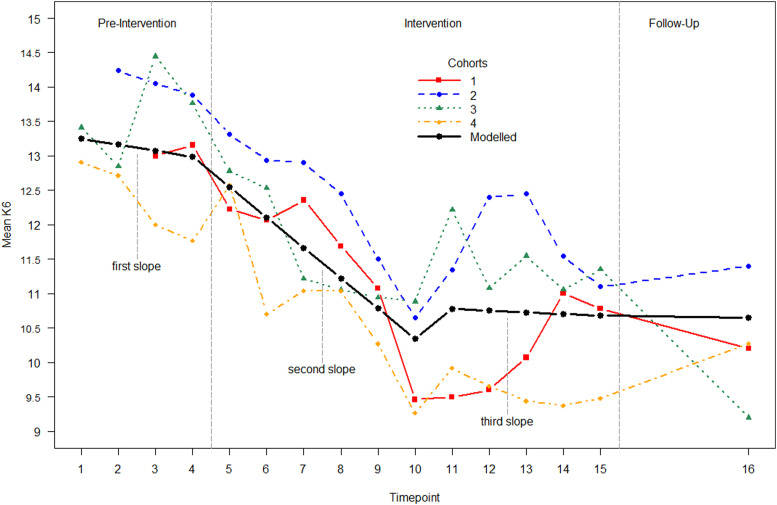
Visual inspection of the cluster means revealed a reduction in psychological distress in the first 6 weeks of the intervention, followed by a floor effect whereby the symptom improvements were maintained at the lower level compared to baseline. That is, there was a change in direction of the intervention slope with a turning or ‘knot’ point approximately halfway through the intervention. We thus modelled the intervention as two slopes, with a knot for a change in direction at week 6 to better represent data. The length of the baseline (4 weeks) was more comparable in time course to the two intervention slopes (6 weeks each). We therefore had three slopes comprised of four baseline time points, followed by six time points and another six (including the 1-month follow up). The first week of the baseline only included cluster 4 (the only cluster with 5 weeks of baseline) so the slope was unduly influenced by this cluster, biasing the slopes. This first week was removed so that only weeks with two or more clusters were modelled.
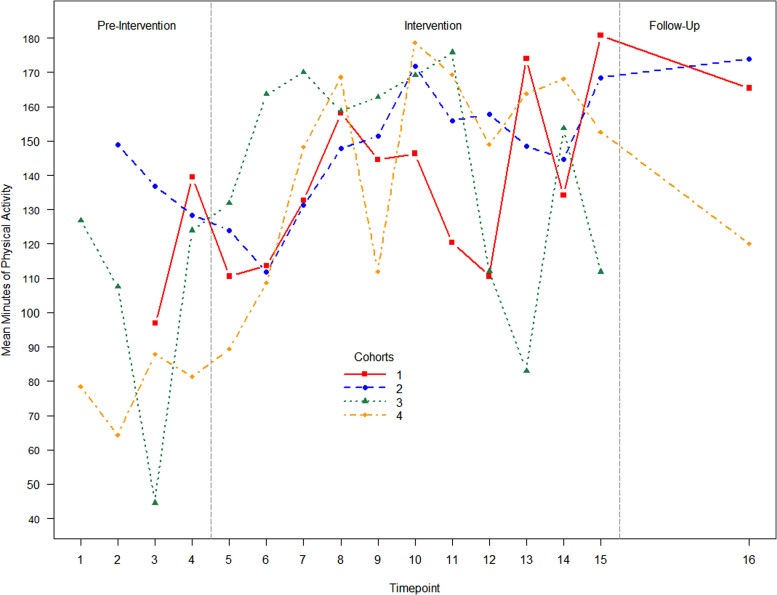
The baseline slope (slope 1) was not significant, b = −0.09, p = 0.379, as shown in Table 2. The intervention slope 2 (intervention time points 1–5) showed a significant decrease in psychological distress across the intervention period, b = −0.441, p = <0.001. That is, participants decreased by 0.441 of a point on the K6 per week during the first 6 weeks. The intervention slope 3 (time point 11–16 (follow up)) did not decrease significantly, b = −0.009, p = 0.883 (i.e. improvements in K6 were maintained). The difference between baseline and intervention slope 1 was significant, b=−0.351, p = 0.003, (i.e. the trajectories of change were significantly different), while slope 2 was not significantly different to baseline b=0.081, p = 0.533). That is, participants continually reduced their levels of psychological distress compared to baseline until week 6 (i.e. improvements were greater in the first part of the intervention) and then improvements plateaued. The model showed mediocre fit (chi square = 264.24, p < 0.001 RMSEA = 0.097; CFI = 0.918; TLI = 0.913, SRMR = 0.114). Clustering by cohort revealed that no cluster variables were significant and adding it to the model caused estimation problems, making it unstable. We therefore did not cluster by cohort. The estimated marginal means for K6 scores at each time point are shown below in Figure 3. Due to large amounts of variance in reporting of physical activity (see Figure 4 for weekly means), physical activity could not be added to the latent growth curve model.
Table 2.
Latent growth curve models for psychological distress.
| Coefficient | SE | t-score | p-value | |
|---|---|---|---|---|
| Position on intercept | 0.658 | 0.553 | 1.190 | 0.234 |
| DASS-21 on intercept | 0.277 | 0.030 | 9.148 | <0.001 |
| Baseline | −0.090 | 0.102 | −0.880 | 0.379 |
| Intervention 1 | −0.441 | 0.062 | −7.098 | <0.001 |
| Intervention 2 | −0.009 | 0.064 | −0.147 | 0.883 |
| Intervention 1 vs baseline | −0.351 | 0.116 | −3.018 | 0.003 |
| Intervention 2 vs baseline | 0.081 | 0.129 | 0.624 | 0.533 |
| Intervention 1 vs 2 | −0.432 | 0.089 | −4.861 | <0.001 |
Note: Baseline= slope 1, Intervention 1=slope 2, Intervention 2= slope 3. Bold font indicates statistical significance. DASS: Depression Anxiety and Stress Scale.
Figure 3.
Estimated marginal means for weekly K6 scores per cluster. Note: The coloured points show the mean of each cluster at each weekly assessment. The black line shows the modelled slope across clusters with knot points at week 4 (end of baseline) and week 10 (6 weeks into the intervention). There is also a change in level modelled between weeks 10 and 11.
Figure 4.
Mean weekly physical activity scores per cluster.
Pre–post tests
The results for all secondary outcomes at baseline and post-intervention are shown in Table 3. The multivariate omnibus test across all variables was significant, that is, time was significantly associated with the multivariate outcome F (822) = 4.912, p < 0.001. Individual mixed models analysis of the secondary outcomes revealed a significant effect of time for anxiety (p = 0.02, Cohen d = 0.30), stress (p = 0.003, Cohen d = 0.22), quality of life (p = 0.001, Cohen d = 0.26), MVPA (p = 0.03, Cohen d = 0.29), walking time (p = 0.002, Cohen d = 0.43), sedentary behaviour (p = 0.045, Cohen d = 0.25), support to exercise from family (p = 0.004, Coehn d = 0.45) and PTSD symptoms (p = 0.001, Cohen d = 0.23). There was no significant effect of time for sleep quality (p = 0.07, Cohen d = 0.16), depression (p = 0.15, Cohen d = 0.14), suicidal ideation (p = 0.45, Cohen d = 0.09) and support to exercise from friends (p = 0.19, Cohen d = 0.14). The effect of position (i.e. emergency service worker vs support partner) was significant across time points for depression, stress, quality of life and sleep quality. However, there was no interaction between time and position (i.e. change from pre, post to follow up) between the two groups in any outcome except friends support to exercise.
Table 3.
Mixed models pre, post and follow-up data.
| Variable | n | Baseline- estimate (SE) | 95% Confidence interval | n | Post-estimate (SE) | 95% Confidence interval | n | Follow-up estimate (SE) | 95% Confidence interval | Time | Position | Time x position | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F test | p-value | F test | p-value | F test | p-value | ||||||||||
| DASS depression | |||||||||||||||
| Total | 90 | 6.0(0.5) | [4.91, 7.08] | 73 | 5.3(0.6) | [4.20, 6.44] | 50 | 5.3(0.6) | [4.09, 6.56] | 1.90 | 0.15 | 10.02 | 0.002 | 0.53 | 0.59 |
| ESW | 7.6(0.8) | [6.12, 9.12] | 7.2(0.8) | [5.63, 8.72] | 6.8(0.8) | [5.17, 8.48] | |||||||||
| Partner | 4.4(0.8) | [2.90, 5.94] | 3.5(0.8) | [1.84, 5.10] | 3.8(0.9) | [2.00, 5.65] | |||||||||
| DASS anxiety | |||||||||||||||
| Total | 90 | 4.5(0.4) | [3.64, 5.32] | 73 | 3.3(0.5) | [2.82, 4.58] | 50 | 5.3(0.6) | [2.35, 4.32] | 4.10 | 0.02 | 1.39 | 0.24 | 0.46 | 0.63 |
| ESW | 5.2(0.6) | [4.01, 6.34] | 4.1(0.6) | [2.94, 5.35] | 3.6(0.7) | [2.30, 4.94] | |||||||||
| Partner | 3.8(0.6) | [2.57, 5.01] | 3.3(0.6) | [1.98, 4.53] | 3.1(0.7) | [1.59, 4.52] | |||||||||
| DASS stress | |||||||||||||||
| Total | 90 | 4.5(0.4) | [6.76, 8.89] | 73 | 3.7(0.4) | [5.34, 7.57] | 50 | 3.3(0.5) | [4.90, 7.43] | 5.90 | 0.003 | 4.80 | 0.03 | 0.04 | 0.96 |
| ESW | 9.0(0.7) | [7.53, 10.47] | 7.5(0.8) | [5.99, 9.05] | 7.2(0.9) | [5.53, 7.01] | |||||||||
| Partner | 6.7(0.8) | [5.12, 8.19] | 5.4(0.8) | [3.77, 7.02] | 5.1(1.0) | [3.23, 7.01] | |||||||||
| Quality of life | |||||||||||||||
| Total | 88 | 75.0(1.5) | [72.14, 77.92] | 72 | 78.5(1.5) | [75.54, 81.52] | 49 | 77.9(1.6) | [74.61, 81.18] | 7.38 | 0.001 | 8.90 | 0.004 | 1.40 | 0.26 |
| ESW | 69.73(2.0) | [65.74, 73.73] | 74.6(2.1) | [70.48, 78.70] | 74.6(2.2) | [70.48, 78.70] | |||||||||
| Partner | 80.4(2.1) | [76.14, 84.56] | 82.5(2.2) | [78.13, 86.80] | 81.2(2.5) | [76.33, 86.04] | |||||||||
| MVPA, minutes/week | |||||||||||||||
| Total | 89 | 103.7(17.4) | [69.38, 137.94] | 77 | 151.2(18.3) | [114.98, 187.46] | 46 | 135.5(23.4) | [89.37, 181.57] | 3.50 | 0.03 | 2.70 | 0.11 | 2.11 | 0.13 |
| ESW | 59.9(24.1) | [12.47, 107.57] | 114.72(25.0) | [65.54, 163.90] | 142.4(29.0) | [85.18, 199.63] | |||||||||
| Partner | 147.33(24.9) | [97.97, 196.68] | 187.72(27.0) | [134.48, 240.96] | 128.53(36.7) | [56.24, 200.83] | |||||||||
| Sleep quality | |||||||||||||||
| Total | 89 | 9.3(0.5) | [8.44, 10.25] | 71 | 8.6(0.5) | [7.67, 9.55] | 44 | 8.8(0.5) | [7.75, 9.89] | 2.72 | 0.07 | 7.77 | 0.006 | 1.09 | 0.34 |
| ESW | 10.35(0.6) | [9.10, 11.61] | 9.63(0.7) | [8.33, 10.92] | 10.42(0.7) | [8.95, 11.90] | |||||||||
| Partner | 8.32(0.7) | [7.02, 9.63] | 7.59(0.7) | [6.23, 8.96] | 7.22(0.7) | [5.66, 8.77] | |||||||||
| Sedentary hours/day | |||||||||||||||
| Total | 89 | 8.6(0.4) | [7.85, 9.47] | 72 | 7.7(0.4) | [6.85, 8.61] | 46 | 7.3(0.6) | [6.17, 8.36] | 3.17 | 0.045 | 1.09 | 0.30 | 0.67 | 0.51 |
| ESW | 9.37(0.6) | [8.24, 10.50] | 8.14(0.6) | [6.94, 9.35] | 7.25(0.7) | [5.89, 8.62] | |||||||||
| Partner | 7.95(0.6) | [6.79, 9.12] | 7.31(0.6) | [6.04, 8.58] | 7.28(0.9) | [5.56, 9.0] | |||||||||
| Walking minutes/day | |||||||||||||||
| Total | 89 | 41.6(5.2) | [31.26, 51.95] | 74 | 63.0(5.7) | [51.76, 74.16] | 46 | 64.6(7.3) | [50.15, 78.97] | 6.59 | 0.002 | 0.57 | 0.45 | 2.20 | 0.12 |
| ESW | 34.2(7.3) | [19.85, 48.61] | 53.6(7.8) | [38.21, 69.10] | 71.5(9.0) | [53.80, 89.24] | |||||||||
| Partner | 48.9(7.54) | [34.10, 63.85] | 72.3(8.2) | [56.03, 88.54] | 57.6(11.5) | [34.88, 80.32] | |||||||||
| Social support to exercise (family) | |||||||||||||||
| Total | 69 | 18.4(1.0) | [16.32, 20.45] | 54 | 22.1(1.1) | [19.87, 24.40] | 37 | 19.9(1.4) | [17.24, 22.63] | 5.90 | 0.004 | 0.819 | 0.369 | 0.01 | 0.99 |
| ESW | 17.6(1.4) | [14.73, 20.44] | 21.4(1.6) | [18.28, 24.55] | 19.0(1.8) | [15.43, 22.59] | |||||||||
| Partner | 19.2(1.5) | [16.20, 22.16] | 22.9(1.6) | [19.59, 26.12] | 20.9(2.0) | [16.84, 24.89] | |||||||||
| Social support to exercise (friend) | |||||||||||||||
| Total | 69 | 14.8(0.9) | [13.15, 16.53] | 54 | 15.8(0.9) | [13.97, 17.56] | 37 | 14.5(1.0) | [12.48, 16.59] | 1.68 | 0.19 | 1.496 | 0.225 | 2.71 | 0.07 |
| ESW | 14.5(1.2) | [12.17, 16.83] | 13.94(1.3) | [11.46, 16.43] | 13.8(1.4) | [11.03, 16.57] | |||||||||
| Partner | 15.2(1.2) | [12.74, 17.62] | 17.6(1.3) | [15.00, 20.17] | 15.3(1.5) | [12.22, 18.32] | |||||||||
| SIDAS | |||||||||||||||
| Total | 89 | 11.4(0.6) | [10.18, 12,66] | 75 | 11.9(0.6) | [10.61, 13.19] | 11.2(0.7) | [9.83, 12.78] | 0.80 | 0.45 | 1.372 | 0.245 | 0.658 | 0.52 | |
| ESW | 12.35(0.8) | [10.61, 14.03] | 12.6(0.8) | [10.84, 14.40] | 11.36(0.9) | [9.44, 13.36] | |||||||||
| Partner | 10.5(0.8) | [8.73, 12.33] | 11.1(0.9) | [9.32, 13.06] | 11.1(1.1.0) | [9.01, 13.41] | |||||||||
| PCL-5 | |||||||||||||||
| ESW | 47 | 28.1(2.7) | [22.60, 33.51] | 40 | 24.0 (2.7) | [18.51, 29.53] | 31 | 22.1(2.8) | [16.42, 27.78] | 7.81 | 0.001 | - | - | - | - |
Note: Position indicates emergency service worker or support partners. Bold font indicates statistical significance.
DASS: Depression, Anxiety and Stress Scale; Estimate: estimated marginal means; ESW: emergency service worker; MVPA: moderate to vigorous physical activity; PCL-5: PTSD checklist for DSM-5; PTSD: post-traumatic stress disorder; SE: standard error; SIDAS: Suicidal Ideation Attributes Scale.
Acceptability
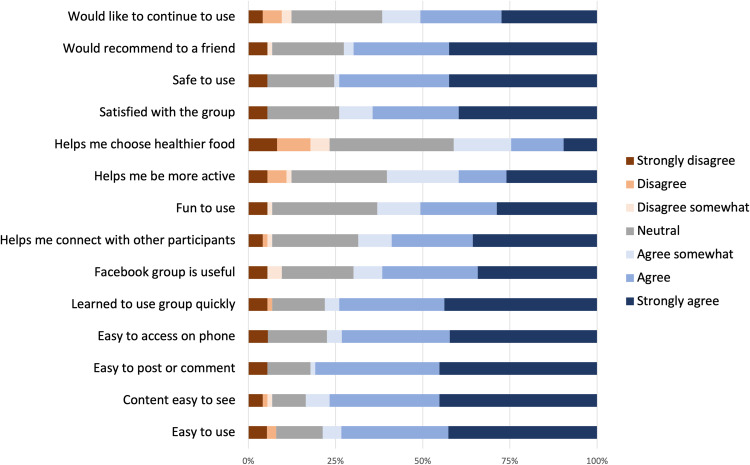
The results from the feasibility and acceptability questionnaire are shown in Figure 5. Most participants (>75%) agreed that the Facebook group was easy to use. The majority found that it was easy to view the content, post or comment on the group and access via a smartphone. There was some disagreement regarding satisfaction, the desire to continue using the group and whether the group was fun to use.
Figure 5.
Feasibility and acceptability responses.
Discussion
The results of this study showed that an online physical activity intervention is a feasible strategy that can help to reduce levels of psychological distress among emergency service workers and their support partners. Levels of psychological distress did not change significantly during the baseline period yet reduced significantly during the first 6 weeks of the intervention, compared to baseline. Improvements then plateaued and were maintained until the end of the intervention and to the 1-month follow up. This finding is consistent with a previous exercise intervention conducted in police officers which found that the greatest improvements in levels of PTSD were made in the first 6 weeks of the intervention and then maintained until the end of the programme at week 12.55 Therefore, by helping emergency service workers to maintain social and personal resources associated with lifestyle behaviours, this may help to protect their mental health and prevent resource loss spirals, as explained by the conservation of resources theory.56
In addition to reductions in psychological distress, participation in the intervention was also associated with improved levels of anxiety, stress, quality of life and PTSD symptoms in line with previous studies.57,58 The active components of the intervention mediating the improvements in mental health symptoms however are not clear. Given the existing exercise and mental health treatment and prevention literature,17,59 and the target of the intervention, the observed significant changes in physical activity levels and sedentary behaviour are likely contributing factors. While mean weekly physical activity levels could not be added to the latent growth curve model because of the large variability in self-reported data, Figure 4 appears to show a trend of increasing physical activity levels throughout the intervention compared to baseline. Our findings therefore suggest that increasing physical activity levels and reducing sedentary behaviour may be a useful strategy for improving mental health in a primarily sub-clinical population. Core components of the intervention included the supervision by exercise physiologists, as recommended to increase adherence among people with poor mental health,60 and the focus on enjoyment and the emphasis on sustainable, incremental lifestyle change tailored to individual preferences, rather than specific exercise prescription.41
The study also aimed to facilitate social support, which has been found among other populations including veterans to drive the relationship between increased exercise and improved mental health.61 Further investigation into the role of social support including the dyad relationship (i.e. emergency service and support partner) in moderating health behaviours is warranted. For example, it would be helpful to understand the interactions between the physical activity behaviours of emergency service workers and their support partners and the factors mediating this relationship to understand the design of dyad interventions. While support from friends to exercise did not change significantly, changes in family support, which is not surprising given 70% of dyads, were spouses or family members rather than friends. Lastly, retention was high (91%) compared to previous social media delivered physical activity and diet intervention studies among the general population62 and physical activity interventions among people with anxiety disorders.63 This is an important finding given the barriers such as stigma and accessibility often associated with other preventative and treatment-based mental health initiatives.64
Limitations
Several limitations should be considered. Firstly, the online recruitment via social media introduces a bias toward those who are already active online and technologically literate. Future studies using digital platforms to target physical activity and diet among this population should consider assessing the usability of the platforms to truly understand the acceptance of these technologies. This includes assessing the separate constructs of usefulness, satisfaction and ease of use.
Secondly, it is difficult to dismantle the intervention components (e.g. Fitbit, Facebook group, telehealth calls), to inform which component is having the greatest effect and inform future initiatives. The authors will however conduct a secondary analysis to regress changes in symptom scores on changes in Fitbit measured physical activity levels to better understand possible associations.
In addition, this study involved a relatively small sample (n=90) with large heterogeneity regarding employment and mental health symptomology. The sampling from a specific organisation (Behind the Seen) introduces another bias. Confounding variables such as engagement levels, major life events or medication changes were not monitored or controlled for due to high participant questionnaire burden; however, future research should consider assessing these. While we recruited participants with and without a diagnosed mental illness, we excluded people who were experiencing high levels of symptomatology and were not engaged in other mental health support. Since the present study is not mental health treatment it may therefore not be suitable for people experiencing very high levels of psychiatric symptomatology. In addition, the follow-up period of 1 month may not be long enough to detect sustained changes and future research should consider longer follow-up period to determine maintenance of behaviour change and reasons for dropout.
A strength of this study is the stepped-wedge design whereby everyone had access to the intervention, however importantly while the primary outcome (K6) had a control, the pre–post–follow up data did not and therefore caution should be taken not to overinterpret these findings. Finally, our sample size calculation determined that we would need n=80 participants, and so in our protocol we reported that would recruit 5 clusters to account for drop out.32 Given our low dropout rate (n=7), we terminated recruitment after 4 trials (n=90) since this exceeded the required n=80 participants.
Conclusion
Emergency service workers are regularly exposed to trauma as part of their work. We therefore need to equip emergency workers with resources to help buffer the effects of stress and trauma exposure. Results add to the small yet increasing body of evidence showing the impact of targeting modifiable lifestyle behaviours, known predictors of mental health, for populations exposed to trauma. Our stepped-wedge evaluation of a 10-week online lifestyle intervention resulted in significant improvements in levels of psychological distress and may be associated with other health outcomes including quality of life among emergency service workers and their support partners. Future research should consider evaluating the mechanistic factors (e.g. levels of physical activity, social support) as mediators of improvements in levels of psychological distress.
Acknowledgments
We would like to thank and acknowledge the contribution of Veronique Moseley and Ross Beckley from Behind the Seen to the co-design of this study.
Footnotes
Contributorship: GM and SR researched the literature and conceived the study. GM, SR, RW, ZS and DV were involved in the protocol development. GM and SR recruited all participants and GM, SR and ST conducted the study. GM, RW, ZS and DH conducted the data analysis. GM wrote the first draft of the manuscript and all authors reviewed and edited the manuscript and approved the final version.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study was approved by the UNSW Human Research Ethics Committee HC180561.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: GM is funded by a Suicide Prevention Australia Scholarshipe and funding from the Elderslee Foundation
Guarantor: GM.
ORCID iDs: Grace McKeon https://orcid.org/0000-0003-4722-1639
Simon Rosenbaum https://orcid.org/0000-0002-8984-4941
References
- 1.Lawrence D, Kyron M, Rikkers W, et al. Answering the call: national survey: beyond Blue's National Mental Health and Wellbeing Study of Police and Emergency Services-Final report. 2018.
- 2.Carleton RN, Afifi TO, Taillieu T, et al. Exposures to potentially traumatic events among public safety personnel in Canada. Can J Behav Sci 2019; 51: 37–52. [Google Scholar]
- 3.Jones S. Describing the mental health profile of first responders: a systematic review. J Am Psychiatr Nurses Assoc 2017; 23: 200–214. [DOI] [PubMed] [Google Scholar]
- 4.Creamer M, Burgess P, McFarlane AC. Post-traumatic stress disorder: findings from the Australian National Survey of Mental Health and Well-being. Psychol Med 2001; 31: 1237–1247. [DOI] [PubMed] [Google Scholar]
- 5.Cloitre M. The “one size fits all” approach to trauma treatment: should we be satisfied? Eur J Psychotraumatol 2015; 6: 27344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Coronial Information System. Intentional self-harm among emergency services personnel in Australia. 2019.
- 7.Fekedulegn D, Burchfiel CM, Charles LE, et al. Shift work and sleep quality among urban police officers: the BCOPS study. J Occup Environ Med 2016; 58: e66–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LdC A, Levandovski R, Dantas G, et al. Obesity and shift work: chronobiological aspects. Nutr Res Rev 2010; 23: 155–168. [DOI] [PubMed] [Google Scholar]
- 9.Atkinson G, Fullick S, Grindey C, et al. Exercise, energy balance and the shift worker. Sports Med 2008; 38: 671–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sörensen L, Smolander J, Louhevaara V, et al. Physical activity, fitness and body composition of Finnish police officers: a 15-year follow-up study. Occup Med (Lond) 2000; 50: 3–10. [DOI] [PubMed] [Google Scholar]
- 11.Allen MS, Walter EE, Swann C. Sedentary behaviour and risk of anxiety: a systematic review and meta-analysis. J Affect Disord 2019; 242: 5–13. [DOI] [PubMed] [Google Scholar]
- 12.Takemoto E, Van Oss KR, Chamany S, et al. Post-traumatic stress disorder and the association with overweight, obesity, and weight change among individuals exposed to the World Trade Center disaster, 2003–2016. Psychol Med 2021; 51: 2647–2656. [DOI] [PubMed] [Google Scholar]
- 13.Ferri P, Guadi M, Marcheselli L, et al. The impact of shift work on the psychological and physical health of nurses in a general hospital: a comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy 2016; 9: 203–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hegg-Deloye S, Brassard P, Jauvin N, et al. Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emerg Med J 2014; 31: 242–247. [DOI] [PubMed] [Google Scholar]
- 15.Firth J, Solmi M, Wootton RE, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry 2020; 19: 360–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 2019; 6: 675–712. [DOI] [PubMed] [Google Scholar]
- 17.Ashdown-Franks G, Firth J, Carney R, et al. Exercise as medicine for mental and substance use disorders: a meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med 2020; 50(1), 151-170. [DOI] [PubMed] [Google Scholar]
- 18.Schuch F, Stubbs B, Meyer J, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety 2019; 36: 846–858. [DOI] [PubMed] [Google Scholar]
- 19.Hutchinson LC, Forshaw MJ, McIlroy D, et al. The role of lifestyle on NHS ambulance workers’ wellbeing. J Workplace Behav Health 2021; 36: 159–171. [Google Scholar]
- 20.McKeon G, Steel Z, Wells R. Exercise and PTSD symptoms in emergency service and frontline medical workers: a systematic review. Transl J Am Coll Sports Med 2021; 7: e000189. [Google Scholar]
- 21.Gerber M, Kellmann M, Hartmann T, et al. Do exercise and fitness buffer against stress among Swiss police and emergency response service officers? Psychol Sport Exerc 2010; 11: 286–294. [Google Scholar]
- 22.Deady M, Peters D, Lang H, et al. Designing smartphone mental health applications for emergency service workers. Occup Med 2017; 67: 425–428. [DOI] [PubMed] [Google Scholar]
- 23.Lee J-S. Perceived social support functions as a resilience in buffering the impact of trauma exposure on PTSD symptoms via intrusive rumination and entrapment in firefighters. PLoS One 2019; 14: e0220454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Casas JB, Benuto LT. Work-related traumatic stress spillover in first responder families: a systematic review of the literature. Psychol Trauma Theory Res Pract Pol 2021; 14: 209–217. [DOI] [PubMed] [Google Scholar]
- 25.Firth J, Rosenbaum S, Stubbs B, et al. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med 2016; 46: 2869–2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Auxier B, Anderson M. Social media use in 2021. Pew Research Center. 2021.
- 27.Giustini D, Ali SM, Fraser M, et al. Effective uses of social media in public health and medicine: a systematic review of systematic reviews. Online J Public Health Inform 2018; 10: e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodyear VA, Wood G, Skinner B, et al. The effect of social media interventions on physical activity and dietary behaviours in young people and adults: a systematic review. Int J Behav Nutr Phys Act 2021; 18: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell DT, Stanley JC. Experimental and quasi-experimental designs for research. Ravenio Books, 2015. [Google Scholar]
- 30.Organization WH. Health promotion evaluation: recommendations to policy-makers: report of the WHO European Working Group on Health Promotion Evaluation. Copenhagen: WHO Regional Office for Europe, 1998. [Google Scholar]
- 31.Hemming K, Taljaard M, McKenzie JE, et al. Reporting of stepped wedge cluster randomised trials: extension of the CONSORT 2010 statement with explanation and elaboration. Br Med J 2018; 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKeon G, Steel Z, Wells R, et al. Mental health informed physical activity for first responders and their support partner: a protocol for a stepped-wedge evaluation of an online, codesigned intervention. BMJ Open 2019; 9: e030668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKeon G, Steel Z, Wells R, et al. A mental health–informed physical activity intervention for first responders and their partners delivered using Facebook: mixed methods pilot study. JMIR Form Res 2021; 5: e23432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fogarty A, Steel Z, Ward PB, et al. Trauma and mental health awareness in emergency service workers: a qualitative evaluation of the behind the seen education workshops. Int J Environ Res Public Health 2021; 18: 4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norton K CJ, Parker R, Williams A, et al. New Australian standard for adult pre-exercise screening. Sport Health 2012; 30: 12–18. [Google Scholar]
- 36.Greenwood JL, Joy EA, Stanford JB. The physical activity vital sign: a primary care tool to guide counseling for obesity. J Phys Act Health 2010; 7: 571–576. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32: 959–976. [DOI] [PubMed] [Google Scholar]
- 38.Van Spijker BA, Batterham PJ, Calear AL, et al. The Suicidal Ideation Attributes Scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav 2014; 44: 408–419. [DOI] [PubMed] [Google Scholar]
- 39.Rosenbaum S, McKeon G, Stubbs B, et al. Redefining mental healthcare: going multidisciplinary to manage multimorbidity. Br J Sports Med 2021; 55: 7–8. [DOI] [PubMed] [Google Scholar]
- 40.McKeon G, Mastrogiovanni C, Chapman J, et al. The experiences of peer-facilitators delivering a physical activity intervention for emergency service workers and their families. Ment Health Phys Act 2021; 21: 100414. [Google Scholar]
- 41.Teychenne M, White RL, Richards J, et al. Do we need physical activity guidelines for mental health: what does the evidence tell us? Ment Health Phys Act 2020; 18: 100315. [Google Scholar]
- 42.Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011; 26: 1479–1498. [DOI] [PubMed] [Google Scholar]
- 43.Kessler RC, Green JG, Gruber MJ, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res 2010; 19: 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Staples LG, Dear BF, Gandy M, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: the PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry 2019; 56: 13–18. [DOI] [PubMed] [Google Scholar]
- 45.Rosenbaum S, Morell R, Abdel-Baki A, et al. Assessing physical activity in people with mental illness: 23-country reliability and validity of the simple physical activity questionnaire (SIMPAQ). BMC Psychiatry 2020; 20: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995; 33: 335–343. [DOI] [PubMed] [Google Scholar]
- 47.Blevins CA, Weathers FW, Davis MT, et al. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015; 28: 489–498. [DOI] [PubMed] [Google Scholar]
- 48.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213. [DOI] [PubMed] [Google Scholar]
- 49.Richardson JRJ, Peacock SJ, Hawthorne G, et al. Construction of the descriptive system for the Assessment of Quality of Life AQoL-6D utility instrument. Health Qual Life Outcomes 2012; 10: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sallis JF, Grossman RM, Pinski RB, et al. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987; 16: 825–836. [DOI] [PubMed] [Google Scholar]
- 51.Naslund JA, Aschbrenner KA, Marsch LA, et al. Feasibility and acceptability of Facebook for health promotion among people with serious mental illness. Digit Health 2016; 2: 2055207616654822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Duncan TE, Duncan SC. An introduction to latent growth curve modeling. Behav Ther 2004; 35: 333–363. [Google Scholar]
- 53.Rioux C, Stickley ZL, Little TD. Solutions for latent growth modeling following COVID-19-related discontinuities in change and disruptions in longitudinal data collection. Int J Behav Dev 2021; 45: 463–473. [Google Scholar]
- 54.Muthén LK, Muthén B. Mplus user’s guide: statistical analysis with latent variables, user’s guide. Muthén & Muthén, 2017. [Google Scholar]
- 55.Rosenbaum S, Stierli M, McCullagh S, et al. An open trial of the RECONNECT exercise program for NSW Police Officers with posttraumatic stress disorder or psychological injury. Health Promot J Austr 2020; 33: 28-33. [DOI] [PubMed] [Google Scholar]
- 56.Hobfoll SE, Shirom A, Golembiewski R. Conservation of resources theory. Handb Organ Behav 2000: 57–81. [Google Scholar]
- 57.Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand 2015; 131: 350–359. [DOI] [PubMed] [Google Scholar]
- 58.Hegberg NJ, Hayes JP, Hayes SM. Exercise intervention in PTSD: a narrative review and rationale for implementation. Front Psychiatry 2019; 10: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosenbaum S, Vancampfort D, Steel Z, et al. Physical activity in the treatment of post-traumatic stress disorder: a systematic review and meta-analysis. Psychiatry Res 2015; 230: 130–136. [DOI] [PubMed] [Google Scholar]
- 60.Stubbs B, Vancampfort D, Rosenbaum S, et al. Dropout from exercise randomized controlled trials among people with depression: a meta-analysis and meta regression. J Affect Disord 2016; 190: 457–466. [DOI] [PubMed] [Google Scholar]
- 61.Wilkins SS, Melrose RJ, Hall KS, et al. PTSD improvement associated with social connectedness in Gerofit veterans exercise program. J Am Geriatr Soc 2021; 69: 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williams G, Hamm MP, Shulhan J, et al. Social media interventions for diet and exercise behaviours: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 2014; 4: e003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vancampfort D, Sanchez CPR, Hallgren M, et al. Dropout from exercise randomized controlled trials among people with anxiety and stress-related disorders: a meta-analysis and meta-regression. J Affect Disord 2021; 282: 996–1004. [DOI] [PubMed] [Google Scholar]
- 64.Jones S, Agud K, McSweeney J. Barriers and facilitators to seeking mental health care among first responders: “Removing the Darkness”. J Am Psychiatr Nurses Assoc 2020; 26: 43–54. [DOI] [PubMed] [Google Scholar]