Abstract
To assess factors influencing acceptability of COVID-19 vaccine in a population of predominantly indigent, minority, pregnant and non-pregnant people of reproductive age. Cross-sectional survey using a modified Health Belief model administered between January 2021 and January 2022 at four hospitals in Brooklyn. Participants included English-speaking reproductive aged persons attending clinics at the participating sites. Descriptive and univariate data analyses were used for analysis. 283 eligible reproductive persons were approached of whom 272 completed the survey (96%). Three quarters said they would take the vaccine under certain circumstances (“as soon as it is ready” [28.6%], “when my doctor recommends it” [21.3%] or “when enough people have received it to know if it works” [25%]), while 25% said they would never take the vaccine. When comparing persons that would take it under certain circumstances to those that never would, the “never” group was significantly more likely to note that, “they would not trust any COVID vaccine” (71.4% vs. 28.5%; p ≤ 0.0001). This greater level of distrust extended to greater distrust of doctors, government, family, newspapers, and media. However, 36% said they would be influenced by their doctor’s recommendation. Pregnant participants were significantly more likely to wait until their doctor recommended it (17.6% of pregnant persons compared to 3.7% of non-pregnant p < 0.0001). Despite mistrust and other discouraging factors, many persons, under appropriate circumstances (e.g., reassurance about vaccine safety) may be motivated to take the vaccine. Even those who claimed that they wouldn’t take the vaccine under any circumstance may be influenced by their health care providers.
Keywords: COVID-19, Vaccine hesitancy, Vaccine, Pregnant, Health-Belief Model
Introduction
Low rates of vaccination have been a persistent problem in obstetrics, with rates of influenza vaccination and Tdap failing to achieve national goals. This failure is also seen among non-pregnant reproductive aged persons, which is a concern for pregnancy as well since vaccinations even outside of pregnancy could reduce risks should the person conceive shortly thereafter (e.g., influenza vaccination early in flu season, pregnancy shortly thereafter) [1]. COVID vaccination rates have also failed to achieve desirable rates in the pregnant, as well as in the general United States (US) population. As of October 2022, only 68.1% had completed the primary COVID-19 vaccine series [2], with similar numbers found among reproductive age females (69.3% of females between ages of 18–24 years-old completed the primary vaccine series as did 73.2% of females between ages of 25–49 years-old). The race and ethnicity of COVID-19 vaccine recipients is only known for 78.5% of persons who completed the primary series. Among those, persons who identify as black, non-Hispanic constitute a smaller percentage of vaccinated peoples than they do of the general population [2]. In addition, COVID-19 vaccination to a greater extent than other vaccines, has become freighted with more political meaning than other vaccines, and in the view of some, has been linked to people’s distrust of the government [3].
To achieve better COVID vaccination rates, it is important to understand factors that influence decisions made by high-risk groups, e.g. pregnant and non-pregnant people of reproductive age, particularly people of color. Groups that have been reported to have lower rates of vaccination include women, people who identify as Black, people who are unemployed, those with lower income and lower education, and people who are younger [3–6]. To capture those voices, we performed a survey to assess factors that might influence the acceptability of a COVID-19 vaccine in a population consisting predominantly of indigent, minority pregnant and non-pregnant people of reproductive age. An instrument was used that included questions based on the Health Belief Model (HBM). HBM is a tool used to identify psychological factors that may influence an individual’s health-related behaviors. The model assesses an individual’s perception of susceptibility and perception of severity of a disease, and the perceived benefits and perceived barriers of an intervention; in this case a vaccine [7]. The model can be used to predict an individual’s health behavior in different clinical situations. In addition, given the hardening of positions regarding vaccinations, we sought to distinguish women who expressed a willingness to be vaccinated under certain circumstances from those who stated that they would “never” be vaccinated. Through this analysis, we hope to better understand which strategies might motivate the former to act, and to try to understand factors that undergirded the hesitancy of the latter.
Methods
This was a cross-sectional study administered between January 2021 and January 2022 at four hospitals in Brooklyn, New York. The study was approved by the Maimonides and Downstate IRBs (2021-01-02-MMC, 1700502-7). Participants were reproductive age women attending clinics at the participating sites. The inclusion criterion was reproductive aged persons between ages of 15 years-old and 49 years-old receiving care at any of the four clinical sites, and English speaking. The exclusion criteria consisted of being non-English speaking, and being aged < 15 years-old or > 49 years old.
The survey included demographics such as age, zip code, self-reported race, languages spoken, and education, as well as health-related questions like pregnancy status, breastfeeding status, flu shot history, and COVID-19 history. Questions about comfort with the COVID-19 vaccine, concerns, and ideal administration site (e.g., hospital vs. pharmacy) were also asked.
Participants were then asked questions based on the Health Belief Model. Participants were asked about factors that either motivated or discouraged vaccination using a three-point effect scale (a lot, a little, not at all). Variables included cost of vaccine, side effects, effectiveness, fear of passing vaccine via breastmilk, health care professional’s recommendation, and federal agency recommendation. Participants were also asked about their trust in various sources of vaccine information including health care providers, family or friends, newspaper or magazines, radio, internet, television, government health agencies, charitable organizations, religious organizations or leaders, and social media.
Pregnant participants were asked a few additional questions regarding factors that influenced their willingness to be vaccinated in the setting of pregnancy, such as whether they believed COVID-19 posed a particular risk to pregnant women, the risk of COVID-19 for unborn child, and the risk to other children. Vaccine-related questions included their trust in their obstetrician, vaccine safety for unborn child, side effects for unborn child, and side effects for the mother. The study was designed before vaccines were available, hence questions about whether the women had been vaccinated were not added until the study was already underway.
Descriptive and univariate data analyses were used to analyze the demographic characteristics of the respondents. Following Skewness and Kurtosis test to analyze for normality, Kruskall–Wallis test was used to compare the difference in vaccine acceptability. Chi-Square and Fisher Exact tests at a p-value of < 0.05 were used to analyze other variables of interest. All statistical analyses were performed with Stata/IC 16.1 (StataCorp LLC, Texas).
Results
Participant Characteristics
Study personnel approached 283 individuals of whom 272 completed the survey (96%). Among those, 170 (62.5%) were pregnant. Table 1 shows the demographics of the study population. The majority were people of color (Black 53.8%, Latina 20.3%, Asian 12.2%, White 12.2%, Native American 1.5%). Slightly more than half of participants had gone beyond high school (54%). As noted above, questions about receipt of vaccine were added after the study had begun approximately 3–4 months (03/2021) after the initial survey was created. Vaccine status was not collected for 185 respondents (43% of who were pregnant). Vaccine status was known for 87 respondents of which 50 respondents did not receive the vaccine. Amongst this non-vaccinated group, 6 (12%) respondents were pregnant vs. 44 (88%) were non-pregnant women. 37 respondents did receive the vaccine of which 3 (8%) respondents were pregnant vs. 34 (92%) were non-pregnant women (Table 2).
Table 1.
Demographics and characteristics of participants
| Variables | Yes/Maybe* | No** | p-value |
|---|---|---|---|
| Age N = 270 (IQR) | 0.0001 | ||
| 32 [27–37] | 27 [22–33.5] | ||
| Racial Identity N = 272 | 0.205 | ||
| Blacks | 133 (65.20%) | 50 (73.53%) | |
| Non-blacks | 71 (34.80%) | 18 (26.47%) | |
| Education N = 272 | 0.002 | ||
| < HS + HS diploma | 77 (37.75%) | 40 (58.82%) | |
| > HS | 127 (62.25%) | 28(41.18%) | |
| Pregnancy status N = 272 | 0.193 | ||
| No | 81 (39.71%) | 21 (30.88%) | |
| Yes | 123 (60.29%) | 47 (69.12%) |
Data represented as median [IQR] or N (%)
HS high school
*Yes or Maybe will take the vaccine
**No, will not take the vaccine
Table 2.
Pregnant status and vaccine status
| Pregnant respondents | Non-pregnant respondent | p-value | |
|---|---|---|---|
| Took C19 Vaccine | 3 (33.3%) | 34 (43.6%) | 0.72 |
| Did not take C19 Vaccine | 6 (66.7%) | 44 (56.4%) |
Data represented as (%)
*The number of respondents with known vaccine status is too small to ascertain any relationship between vaccine status, pregnancy status and any attitudinal questions. Data collection for the variable, vaccine status, was not started until approximately 3–4 months (03/2021) after the initial survey was created
Concerns About Vaccination
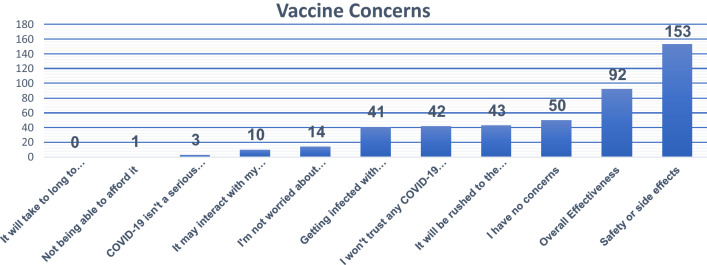
Participants were then asked about their concerns about vaccination, and were able to indicate as many factors as they thought relevant (Fig. 1). The most common concern was safety (n = 153, 56%) followed by vaccine effectiveness (n = 92, 33.8%). Relatively few respondents felt that the disease wasn’t serious (n = 3, 1.1%) or that they were not worried about contracting it (n = 14, 5.1%).
Fig. 1.
Study population’s concerns about COVID-19 vaccine
Overall, three quarters of women said they would take the vaccine under certain circumstances (“as soon as it is ready” [28.6%], “when my doctor recommends it” [21.3%] or “when enough people have received it to know if it works” [25%]). The other 25% said they would never take a COVID-19 vaccination (Table 3).
Table 3.
Vaccine acceptability among respondents
| Answer N = 272 | % |
|---|---|
| Yes, as soon as it's available to me | 28.6 |
| I'll wait until my doctor recommends it | 21.3 |
| I'll wait until enough people have received it to know if it works | 25 |
| I'll never get any COVID-19 vaccine | 25 |
Data represented as (%)
Comparison of “Under the Certain Circumstances” Versus “Never” Group
We then assessed factors that distinguished those who might take the vaccine (under the circumstances listed above) from those who said they never would (Table 1). The “never” group was younger 27 (vs. 32 years old; p = 0.0001) and less educated (greater than HS 58.8% vs. 41.2%; p = 0.002) than the group who would accept vaccine under certain circumstances. When contrasting their responses to concerns about the vaccine, the “never” group were significantly more likely to note that, “they would not trust any COVID vaccine” (71.4% vs. 28.5%; p ≤ 0.0001). This level of distrust among the “never” vaccination group extended to greater distrust of doctors (n = 15, 23.4%), government (n = 32, 50%), family (n = 30, 48.3%), and newspapers (n = 38, 58.4%). The only platform in which their trust was not lower than the “maybe” group was social media (Table 4). Participants who were pregnant were not more likely to be in the never vaccination group, but among those who might take the vaccine, the pregnant participants were significantly more likely to say they would wait until their doctor recommended it (17.6% of pregnant women compared to 3.7% of non-pregnant women; p ≤ 0.0001).
Table 4.
Areas of trust and vaccine acceptability among respondents
| In general, how much would you trust information about COVID-19 from each of the following? | |||
|---|---|---|---|
| Yes/Maybe* | No** | p-value | |
| Doctor/Health-care provider N = 262 | < 0.0001 | ||
| No | 10 (5.05%) | 15 (23.44%) | |
| Yes | 188 (94.95%) | 49 (76.56%) | |
| Family or friends N = 252 | < 0.0001 | ||
| No | 35 (18.42%) | 30 (48.39%) | |
| Yes | 155 (81.58%) | 32 (51.6%) | |
| Newspapers or magazines N = 261 | < 0.0001 | ||
| No | 56 (28.47%) | 38 (58.46%) | |
| Yes | 140 (71.42%) | 27 (41.54%) | |
| Radio N = 260 | 0.019 | ||
| No | 70 (35.90%) | 34 (52.31%) | |
| Yes | 125 (64.10%) | 31 (47.69%) | |
| Internet N = 260 | 0.01 | ||
| No | 36 (18.46%) | 22 (33.85%) | |
| Yes | 159 (81.54%) | 43 (66.15%) | |
| TV N = 257 | < 0.001 | ||
| No | 38 (19.59%) | 29 (46.03%) | |
| Yes | 156 (80.41%) | 34 (53.97%) | |
| Government N = 256 | < 0.001 | ||
| No | 27 (14.06%) | 32 (50.0%) | |
| Yes | 165 (85.94%) | 32 (50.0%) | |
| Charitable Groups N = 252 | < 0.001 | ||
| No | 61 (32.28%) | 40 (63.49%) | |
| Yes | 128 (67.72%) | 23 (36.51%) | |
| Social media N = 253 | 0.138 | ||
| No | 89 (47.09%) | 37 (57.81%) | |
| Yes | 100 (52.91%) | 27 (42.19%) | |
Data represented at (%)
*Yes or maybe will take vaccine
**No will not take vaccine
Importantly, despite saying globally that they would never get vaccinated, the “never” vaccine group did acknowledge some factors that could affect that position (Table 5). For example, a large minority of those women said they would be influenced by evidence of effectiveness (n = 30, 47%) or evidence of safety (n = 29, 44%). This was in contrast to the smaller percentage (n = 17, 26%) who said they would be influenced by CDC or FDA recommendations. A slightly higher percent said they would be influenced by the recommendation of their doctor (n = 23, 36%). When responding to factors that might discourage vaccination, the “never” group cited learning that lots of people were getting side effects (n = 38, 60%) or that effectiveness was less than 60% (n = 43, 69%) (Table 6). Both factors were cited significantly more often by the “never” group than the “maybe group” (p = 0.01 and p = 0.05 respectively). Conversely, women in the “maybe” group were significantly more likely to cite cost (54% v. 29%; p = 0.001) as a potentially discouraging factor.
Table 5.
Motivating factors and vaccine acceptability
| Motivating factors | Yes/Maybe | No | p-value |
|---|---|---|---|
| Vaccine free and readily available N = 260 | < 0.0001 | ||
| No | 45 (23.08%) | 51 (78.46%) | |
| Yes | 150 (76.92%) | 14 (21.54%) | |
| 90% Effective N = 256 | < 0.0001 | ||
| No | 22 (11.46%) | 34 (53.13%) | |
| Yes | 170 (88.54%) | 30 (46.88%) | |
| Few people experience side effects N = 262 | < 0.0001 | ||
| No | 29 (14.72%) | 36 (55.38%) | |
| Yes | 168 (85.28%) | 29 (44.62%) | |
| Only single vaccine dose needed N = 256 | < 0.001 | ||
| No | 48 (25.14%) | 38 (58.46%) | |
| Yes | 143 (74.87%) | 27 (41.54%) | |
| Your doctor or health care professional recommended it N = 257 | < 0.0001 | ||
| No | 31 (16.06%) | 41 (64.06%) | |
| Yes | 162 (83.94%) | 23 (35.94%) | |
| The CDC or FDA recommended it N = 254 | < 0.0001 | ||
| No | 34 (17.89%) | 47 (73.44%) | |
| Yes | 156 (82.11%) | 17 (26.56%) |
Data represented as (%)
*Yes or maybe will take vaccine
**No will not take vaccine
Table 6.
Discouraging factors and vaccine acceptability
| Discouraging factors | Yes/Maybe* | No** | p-value |
|---|---|---|---|
| Pay-out-of-pocket N = 256 | 0.001 | ||
| No | 90 (46.15%) | 46 (70.77%) | |
| Yes | 105 (53.85%) | 19 (29.23%) | |
| Minor side effects N = 257 | 0.011 | ||
| No | 45 (23.20%) | 25 (39.68%) | |
| Yes | 149 (76.80%) | 38 (60.32%) | |
| Vaccine 60% effective N = 256 | 0.05 | ||
| No | 37 (19.07%) | 19 (30.65%) | |
| Yes | 157 (80.93%) | 43 (69.35%) | |
| Annual vaccine requirement N = 257 | 0.446 | ||
| No | 87 (45.31%) | 33 (50.77%) | |
| Yes | 105 (54.69%) | 32 (49.23%) |
Data represented as (%)
*Yes or maybe will take vaccine
**No will not take vaccine
Discussion
In a study of people from a demographic group that has previously been described as vaccine hesitant, we have found that concerns about the vaccine (effectiveness and safety) were greater drivers of behaviors, than were misconceptions about the disease (i.e., people did not discount the seriousness of their disease or their likelihood of acquiring it.) Importantly, we also found that while about one quarter of respondents said they would never take the vaccine, when asked about specific factors that might motivate them, they did acknowledge some, such as effectiveness of vaccine and recommendations from their health care providers.
The fact that people who said they would never take a COVID vaccine, in subsequent questioning were able to acknowledge factors that could motivate them is not entirely illogical. It is possible that those respondents were saying they would never take the vaccine given the current set of facts (or their misapprehension of those facts). The respondents who said they would never accept the vaccine were younger, less educated, and a large minority of them said they would be motivated to take the vaccine if their doctor recommended it. These factors suggest that if physicians educate and encourage, then some otherwise recalcitrant people might be swayed toward vaccination.
Our understanding of the driving factors in respondent’s decisions, (i.e., vaccine related factors were more salient than virus related factors, as described above), were based on responses to a modified Heath Belief Model. The Health Belief Model is designed to identify psychological factors that may influence an individual’s health-related behaviors. The framework is built upon an individual’s perception of susceptibility, perception of severity, perceived benefits, and perceived barriers [7]. In our study the first two factors were not paramount, whereas the latter two were more dispositive. The model can be used to predict an individual’s health behavior in different clinical situations. This has been shown in previous studies involving breast self-examination, smoking cessation, cervical cancer screening, and influenza vaccination among the elderly [8–10]. In a previous cross-sectional study that we performed to assess predictors of H1N1 vaccination, we found, similarly to what we found here, that addressing perceived barriers to the vaccine, such as fear of side-effects, safety of the vaccine for the fetus, and risk of infection during the pregnancy, might be the most effective means to increase vaccination rates among pregnant women [11].
Distrust in the government, is often used as an explanation by people with various political leanings for their skepticism about vaccination and even masking. However, for the population that we studied, America’s past history of medical misconduct may be more of a driver of mistrust. There is strong evidence that mistrust stemming from institutional racism contributes to vaccine hesitancy among this group, and can partially explain high vaccine hesitancy rates [12–16]. Padamsee et al., found that overall vaccine hesitancy decreased more rapidly among Black Americans compared to White Americans since the first available vaccine [12]. They attributed this change to the perceived belief that vaccines are necessary to protect the Black communities from institutional racism [12]. The fact that our study population, which consisted mostly of Black Americans and people of color, fell into the “maybe” group, comports with this theory.
One important message for providers that emerged from this survey is that they still have a critical role to play, particularly in pregnancy. They have the power of suasion that many women said would determine how they would act. However, “physician hesitancy,” when physicians and/or their respective organizations do not recommend COVID-19 vaccination, is a major contributor to low vaccination rates especially among pregnant persons. Recently Chervenak et al., attributed this unaddressed problem to three root causes related to misapplication of clinical practices: therapeutic nihilism, shared decision making, and respect for patient autonomy [17]. Rather than offering sound recommendations, physicians are misguided by the application of these principles and defer their recommendations. Our data shows how recommendations from health care providers can be motivating towards vaccine acceptability. As such, efforts must be made to reversing physician hesitancy along with vaccine hesitancy.
Our study had several strengths. It focused on a population of particular interest at a moment in time when vaccines were first becoming available. In addition, we had sufficient power to discern differences in factors that motivated participants who said they were willing to consider vaccination in some circumstances from those who said they would never be vaccinated. These insights may be useful in framing public health messages.
We also had limitations. The answers reflect a time when vaccines were relatively new, and attitudes may change as more information is made available by access to enlarging data sets. However, even subsequent to our data collection, vaccination rates remain suboptimal. We also cannot comment on factors influencing vaccine hesitancy in other sub-populations, such as rural or southern communities. However, given health disparities in the US, the population we did asses remains one of high interest.
Conclusion
In conclusion, vaccine hesitancy remains an unresolved issue particularly in marginalized groups such as, the persons in our study population. To date, vaccine rates in this population remain suboptimal. Our study, demonstrates that despite mistrust and other discouraging factors, many persons under appropriate circumstances may be motivated to take the vaccine. As such, continued efforts to dispel safety concerns are still needed. More importantly, many persons are still influenced to take the vaccine if recommendations come from their health care providers. Therefore, stronger efforts and future research is needed to combat “physician hesitancy” so that those that are in the “maybe” group could be motivated to take the vaccine.
Funding
The authors have not disclosed any funding.
Declarations
Conflict of interest
The authors have not disclosed any competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beigi RH, Switzer GE, Meyn LA. Acceptance of a pandemic avian influenza vaccine in pregnancy. Journal of Reproductive Medicine. 2009;54:341–346. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC; Retrieved 18 October, 2022 from https://covid.cdc.gov/covid-data-tracker
- 3.Toth-Manikowski SM, Swirsky ES, Gandhi R, Piscitello G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. American Journal of Infection Control. 2022;50(1):20–25. doi: 10.1016/j.ajic.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Du M, Tao L, Liu J. The association between risk perception and COVID-19 vaccine hesitancy for children among reproductive women in China: An online survey. Frontiers in Medicine (Lausanne) 2021;8:741298. doi: 10.3389/fmed.2021.741298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Limbu YB, Gautam RK, Pham L. The health belief model applied to COVID-19 vaccine hesitancy: A systematic review. Vaccines. 2022;10(6):973. doi: 10.3390/vaccines10060973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ndugga N, Pham O, Hill L, Artiga S, Parker N. Latest data on COVID-19 vaccinations by race/ethnicity. San Francisco, California: Kaiser Family Foundation; 2021. Retrieved June 15, 2021, from https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/
- 7.Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2(4):328–335. doi: 10.1177/109019817400200403. [DOI] [PubMed] [Google Scholar]
- 8.Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: an application of the Health Belief Model. BMC Womens Health. 2009;9:37. doi: 10.1186/1472-6874-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson CE, Mues KE, Mayne SL, Kiblawi AN. Cervical cancer screening among immigrants and ethnic minorities: A systematic review using the Health Belief Model. Journal of Lower Genital Tract Disease. 2008;12(3):232–241. doi: 10.1097/LGT.0b013e31815d8d88. [DOI] [PubMed] [Google Scholar]
- 10.Nexøe J, Kragstrup J, Søgaard J. Decision on influenza vaccination among the elderly. A questionnaire study based on the health belief model and the multidimensional locus of control theory. Scandinavian Journal of Primary Health Care. 1999;17(2):105–110. doi: 10.1080/028134399750002737. [DOI] [PubMed] [Google Scholar]
- 11.Friedman D, Steinberg E, Azhar E, Weedon J, Wilson TE, Minkoff H. Predictors of H1N1 vaccination in pregnancy. American Journal of Obstetrics and Gynecology. 2011;204(6 Suppl 1):S124–S127. doi: 10.1016/j.ajog.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Hovick SR, Na K, Nisbet EC, Wegener DT, Kelly Garrett R. Changes in COVID-19 vaccine hesitancy among Black and White individuals in the US. JAMA Netw Open. 2022;5(1):e2144470. doi: 10.1001/jamanetworkopen.2021.44470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abedi V, Olulana O, Avula V, et al. Racial, economic and health inequality and COVID-19 infection in the United States. medRxiv. Preprint posted online May 1, 2020. 10.1101/2020.04.26.20079756 [DOI] [PMC free article] [PubMed]
- 14.Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M. Racial and ethnic disparities in population-level Covid-19 mortality. Journal of General Internal Medicine. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy BL, Logan TD. Racial economic inequality amid the COVID-19 crisis. The Hamilton Project. Published August 13, 2020. Retrieved August 29, 2022, from https://www.hamiltonproject.org/assets/files/EA_HardyLogan_LO_8.12.pdf
- 16.Pummerer L, Böhm R, Lilleholt L, Winter K, Zettler I, Sassenberg K. Conspiracy theories and their societal effects during the COVID-19 pandemic. Social Psychological and Personality Science. 2022;13(1):49–59. doi: 10.1177/19485506211000217. [DOI] [Google Scholar]
- 17.Chervenak FA, McCullough LB, Grunebaum A. Reversing physician hesitancy to recommend COVID-19 vaccination for pregnant patients. American Journal of Obstetrics and Gynecology. 2021;226(6):805–812. doi: 10.1016/j.ajog.2021.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]