Abstract
Objective:
Through a systematic review and mixed-methods meta-synthesis of the existing literature on surgeon well-being, we sought to identify the specific elements of surgeon well-being, examine factors associated with suboptimal well-being, and highlight opportunities to promote well-being.
Background:
Suboptimal surgeon well-being has lasting and substantial impacts to the individual surgeon, patients, and to society as a whole. However, most of the existing literature focuses on only 1 aspect of well-being—burnout. While undoubtedly a crucial component of overall well-being, the mere absence of burnout does not fully consider the complexities of being a surgeon.
Methods:
We performed a literature search within Ovid Medline, Elsevier Excerpta Medica dataBASE, EBSCOhost Cumulative Index to Nursing and Allied Health Literature, and Clarivate Web of Science from inception to May 7, 2020, in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Studies with primary data examining surgeon well-being were included. Using a predetermined instrument, data were abstracted from each study and compared using thematic analysis.
Results:
A total of 5369 abstracts were identified and screened, with 184 full articles (172 quantitative, 3 qualitative, 9 mixed methods) selected for analysis. Among these, 91 articles measured burnout, 82 examined career satisfaction, 95 examined work-related stressors, 44 explored relationships and families, and 85 assessed emotional and physical health. Thematic analysis revealed 4 themes: professional components, personal components, work-life balance, and impacts to well-being.
Conclusions:
Surgeon well-being is complex and multifaceted. This nuanced examination of surgeon well-being highlights the critical need to develop and provide more long-term support to surgeons—with interventions being tailored based on individual, institutional, and systemic factors.
Keywords: surgeon burnout, surgeon career satisfaction, surgeon well-being
Mini-abstract: A meta-analysis of surgeon well-being revealed 4 domains to be most prevalent in the existing literature: professional components, personal components, work-life balance, and impacts to well-being. Despite the existing literature lacking a cohesive definition, studies were consistent with regard to reporting the multitude of variables that constitute surgeon well-being, its impacts, and the potential implications. The complex and multifaceted nature of this topic highlights the critical need to develop and provide more long-term support to surgeons—with interventions being tailored based on individual, institutional, and systemic factors.
Supplemental Digital Content is available in the text.
INTRODUCTION
According to The National Academy of Medicine, “physician or surgeon well-being is a state of personal fulfillment and engagement that leads to joy in one’s practice and connection to why one entered health care and surgery as a profession in the first place.”1 When this has not been achieved, the individual, their patients, and society as a whole are subject to substantial and lasting impacts. Physicians’ physical and emotional health are at risk with numerous studies demonstrating an association between distress and cardiovascular disease, obesity and related comorbidities, as well as substance use disorders, depression, and suicidality.2 Physicians with suboptimal well-being also report lower patient satisfaction and feel they may be more susceptible to medical error and providing poorer quality care.3,4 Surgeons, specifically, may experience negative impacts to both their technical and cognitive intraoperative performance, with serious consequences to their patients.5 Suboptimal physician well-being may also lead to interpersonal relationship issues, diminished productivity, and ultimately, the decision to leave medicine and surgery.6,7 From a societal standpoint, this threat to the physician workforce represents a significant potential loss due to the public health advantage of having individuals who are driven to accomplish work that goes beyond fulfilling personal circumstance.8
The last 2 decades have demonstrated increased attention to surgeon wellness with the overwhelming majority of the literature focused on burnout. Burnout was first coined in the 1970s by American psychologist Herbert Freudenberger as “the extinction of motivation or incentive, especially where one’s devotion to a cause or relationship fails to produce the desired results.”9 Physicians exhibit higher burnout rates than the general working population, with surgeons among the highest.10,11 Studies among surgeon populations, specifically, identify burnout risk factors to include being a woman, younger age, subspecialty choice, and greater work hours and nights on call per week.12 While burnout undoubtedly contributes to overall surgeon well-being, the absence of burnout does not fully consider the intricate and multifaceted nature of being a surgeon.13 This is particularly evident when reflecting on the dissonance between such high burnout rates and equally high rates of career satisfaction and well-being.14,15
In this context, we sought to systematically review the existing literature regarding surgeon well-being. Our objective was to identify the specific elements of surgeon well-being, examine the factors contributing to suboptimal surgeon well-being, and highlight potential opportunities to promote and support surgeon well-being.
METHODS
Review Design, Data Sources, and Search Strategy
We engaged a research librarian to initiate a search of the published literature within Ovid Medline, Elsevier Excerpta Medica dataBASE, EBSCOhost Cumulative Index to Nursing and Allied Health Literature, and Clarivate Web of Science from inception to May 7, 2020, in accordance with systematic review guidelines established by the Institute of Medicine.16 Search terms included data-specific combinations of the following index terms and text words: surgeon, surgery, wellness, well-being, burnout, and distress. Supplement 1 (see http://links.lww.com/AOSO/A6) provides reproducible searches for all databases.
Inclusion and Exclusion Criteria
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses schema, we developed inclusion criteria for relevant articles.17 Surgeon subspecialties included breast, cardiothoracic, colorectal, general, neurologic, orthopedic, otolaryngology/head and neck, pediatric, plastic, surgical oncology, transplant, trauma, urologic, and vascular. Only peer-reviewed studies based on primary data examining surgeon well-being were included. As such, we excluded reviews or guidelines, book chapters, and opinion pieces or letters. Due to concerns of quality of data and inability to verify peer review, we excluded studies from the gray literature (eg, abstract or conference proceedings). Finally, we excluded studies based outside the United States due to differences in practice patterns, reimbursement, and legal and regulatory issues specific to the United States, and studies with fewer than 20% surgeon subjects to ensure adequate surgeon representation.
Study Selection and Data Extraction
Article selection occurred in 3 phases. First, 5369 titles and abstracts (including duplicates) were screened using the inclusion and exclusion criteria. Consensus discussions regularly took place to resolve disagreements. We excluded 5246 total abstracts, yielding 123 remaining articles for full review. In the second phase (in-depth review), we excluded an additional 32 articles that did not pertain to surgeons and well-being (n = 19), were not surgeon-specific (n = 6), were not United States based (n = 4), or otherwise did not fulfill inclusion criteria (n = 3). In the third phase, we then performed a hand search of the references from the 91 remaining articles (n = 63) and an updated search (May 7, 2020, n = 30), which yielded a total of 184 articles for full review (Fig. 1).
FIGURE 1.
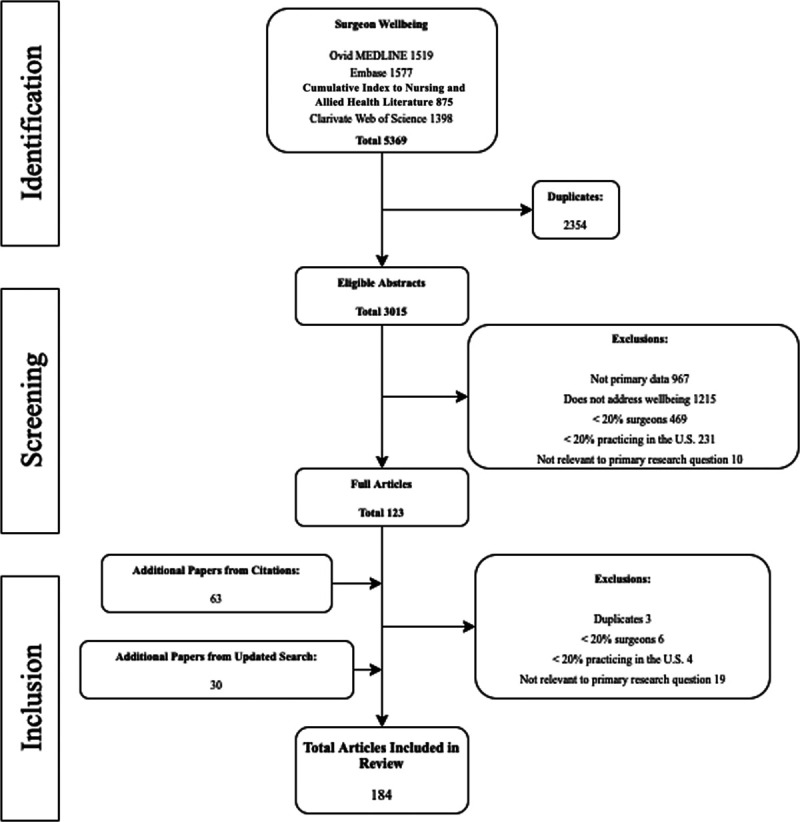
PRISMA diagram. CINAHL indicates Cumulative Index to Nursing and Allied Health Literature; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; U.S., United States.
We employed a modified data abstraction tool, which had been previously used for systematic review and meta-synthesis studies.18–21 Detailed data, including sample population, methods, results, and conclusions, were extracted from each article and independently assessed by at least 2 reviewers (D.Q.D., O.M.B.) for methodologic quality. Similar to the screening phase, consensus discussions were utilized to resolve disagreements. Final adjudication was made by the lead author.
Assessment of Methodologic Quality and Risk of Bias
Methodologic quality was assessed according to predefined criteria for reliability and validity, and quality.22 We evaluated quantitative studies based on selection and minimization of attrition bias, minimization of confounding and measurement bias, appropriateness of statistical tests, and whether the results supported the conclusions. To evaluate qualitative studies, we utilized an explicit sampling strategy and description of data analysis, statement of final themes with definitions, validation of findings, and strategies to achieve consensus among coders.19–21 None of the included studies demonstrated major issues in methodologic quality.
Data Analysis
We selected a mixed-methods meta-synthesis for this study due to (1) the heterogeneity of methodology and outcome measures of the included studies and (2) the ability to synthesize and provide overviews of both quantitative and qualitative studies based on themes, interventions, and results.23,24 Employing thematic analysis, we organized and synthesized the data into coherent themes using a 5-step inductive approach: (1) in-depth reading of each article by at least 2 independent reviewers (familiarization with the data); (2) independent coding of each article by the reviewers; (3) search for themes related to surgeon-specific well-being; (4) group discussion to review, compare, and contrast themes across studies for further refinement; and (5) final set of data-driven themes based on consensus regarding definitions, validation of results through triangulation, and predetermined strategies for adjudication of any discrepancies. All investigators reviewed the categorization of the themes and agreed on the final results of the data analysis. Emergent themes crossed both qualitative and quantitative methodologies.19,21
RESULTS
In total, the database searches retrieved 6370 citations, of which 2813 were identified as duplicates by Endnote X8. The remaining 3557 unique citations screened in DistillerSR (Evidence Partners Inc., Ottawa, Ontario, Canada). A total of 3015 citations were excluded during title/abstract review. We included 184 full articles (172 quantitative, 3 qualitative, 9 mixed methods) in this analysis (Appendix 1, see http://links.lww.com/AOSO/A7). Thematic analysis revealed 4 major themes, which defined well-being: professional components, personal components, work-life balance, and impacts to well-being (Appendix 2, see http://links.lww.com/AOSO/A8 and Fig. 2).
FIGURE 2.

Aspects of surgeon well-being.
PROFESSIONAL COMPONENTS
Connections to profession was the first broad theme, which encompassed career satisfaction, burnout, and work-related stressors (Appendix 3, see http://links.lww.com/AOSO/A9).
Career Satisfaction
Career satisfaction was often associated with surgeon burnout (R1–10). While some studies focused on surgeons collectively, others focused on differences based on subspecialty (R3, 5, 7, 10–36), gender (R13, 19, 22, 23, 30, 33, 37–47), personality (R12, 48, 49), and career position (R1, 6, 10, 19, 31, 50–57). For example, one study found emotional stability and extraversion to predict job satisfaction among trauma surgeons, with no significant gender-based differences (R12). Three additional studies examined career satisfaction based on institution setting, with surgeons reporting similar levels of satisfaction across rural, academic, and private practice settings (R58–60). Career satisfaction was also measured in relation to job turnover and employment patterns (R37, 40, 61–70). Nearly all studies found surgeons to exhibit high levels of career satisfaction, despite certain stressors specific to the work environment described in the section on work-related stressors below.
Burnout
While some studies focused on prevalence and factors associated with burnout among surgeons as a group (R37, 71–82), others focused on surgical subspecialties (R1–3, 7, 10, 14, 17, 20, 21, 29, 83–100). Studies consider factors like the relationship between burnout and residency class size (R101), differences between career stage (R54, 102, 103), practice settings (R31, 58, 104), frequency of call nights (R2), and work hours (R2, 105–110) among others. Seven studies explored more personal characteristics, such as the role of gender (R38, 81, 111, 112) as well as the influence of qualities such as grit and resilience (R113–115). Finally, 9 studies examined methods to mitigate burnout, including evaluations of programs to promote well-being (R116–120), the impacts of adequate support (R50, 121, 122), personal habits (R8), and modifiable factors such as fitness programs, nutrition consultation, and increased socialization with colleagues (R123).
Work-Related Stressors
Among work stressors, practice setting (R31), administrative load (R85, 94, 95, 104), caseload (R65, 85, 96, 104), hours worked (R2, 18, 29, 53, 70, 105, 108–110, 117, 124–131), call conditions (R2, 132), and the lack of collegial relationships (R28, 63, 65, 81, 133–136) were frequently cited as concerns. Additionally, 7 studies focused on clinical and perioperative aspects including disclosing adverse events (R137), medical error (R82, 138, 139), patient complications (R140), uncertainty (R141), and intraoperative stress (R142). Uncertainty surrounding the impacts of health care reform (R20, 143) and involvement in recent malpractice lawsuits (R31, 123, 144, 145) were also cited as important sources of concern. Others described worries over career trajectory including perceived lack of opportunity for career growth (R40, 59, 65, 123), lack of meaning in work (R8), poor perception of control over professional life (R85), and pressure to succeed in research (R123). For example, one study found that discontent in these areas primarily drove recent pediatric surgery fellowship graduates to change jobs early in their careers (R65). Psychological job demands including (R91, 146–147) emotional exhaustion (R65, 139), imposter syndrome (R77), ability to cope with suffering and death (R123), impacts of mass casualty events (R148), depersonalization (R142), and stress (R39, 143, 149, 150) were commonly identified as sources of work-related tensions. Several studies explored issues of discrimination, harassment, and abuse, with a significant focus on impacts of gender bias among women surgeons (R81, 111, 151–153). Finally, fourteen studies described finances (R1, 20, 52, 57, 60, 96, 106, 134, 135, 154) and included anxiety over future earnings (R20, 143), inadequate salary or income (R11, 21, 60, 134, 135, 143) high debt levels (R96), and low collections or billing (R143).
PERSONAL COMPONENTS
Connection to personal aspects was the second broad theme, which included relationships and family, emotional health, and physical health (Appendix 4, see http://links.lww.com/AOSO/A10).
Relationships and Family
Work-life balance was commonly assessed as a factor contributing to career satisfaction (R1, 20, 33, 129, 133) and burnout (R47, 58, 85, 96, 123, 153). Five studies explicitly focused on relationship health and stability (R14, 28, 41, 95, 136). While other studies explored the connection between career satisfaction and marital status (R40, 59, 153, 155), marital satisfaction (R106, 156), spousal support (R94, 144), the impact of educational debt on personal relationships (R57), and the impacts of dual-physician households (R157). Five studies explored the impacts of having children (R40, 134, 153, 155, 156) on overall surgeon well-being, while 1 assessed the impacts of having an older adult (R156) in the home. Additional factors considered included secondhand stress experienced by family and friends (R123, 143), the impacts on relationships and family as a reason for attrition (R22, 45, 52, 67, 68, 158), the role of medical specialty and incidence of divorce (R159), satisfaction with maternity leave (R112), and the need for more work-life integration (R160) for new mothers. For example, a recent study found that pregnancy remains a significant challenge during residency, with greater collegial and institutional support needed both pre- and post-pregnancy (R160).
Emotional Health
Fourteen studies examined psychiatric levels of distress (R29, 81, 85, 89, 94, 123) in surgeons, including the prevalence of post-traumatic stress disorder (R37, 161, 162) effects of mass casualty (R148) and adverse events (R82, 137, 138, 140) and the stress of caring for trauma patients (R163). Studies commonly explored depression and suicidal ideation (R31, 74, 139, 143, 164, 165), with some focusing explicitly on related factors such as recent malpractice suits (R166), hours on call (R2), and implications on workforce (R66, 167). Six studies assessed methods to mitigate negative impacts to emotional health during training and after, including wellness promotion practices (R7, 8, 96, 150, 168) and time off policies (R169). Other aspects related to emotional health included the relationship between grit and well-being (R170), the consequences of shame on residents (R72, 171), and the impact of anxiety on achievement (R146). For example, one study found grit to be positively correlated with general psychological well-being (R114). Conversely, other studies found that a higher number of shame events was a predictor of depersonalization (R72, 171). Two studies demonstrated the perceived stigma and fear of loss of reputation related with pregnancy and motherhood (R112, 160). Finally, 1 study examined the lack of access to mental health services (R18).
Physical Health
Seven studies explored the positive impacts of certain health habits, such as exercise and having a primary care provider, among surgeons (R8, 16, 85, 89, 154, 172, 173). Three additional studies investigated the impacts of physical education and nutrition initiatives on surgeons and found those programs to improve physical activity and quality of life of participants versus nonparticipants in those programs (R120, 123, 174). Conversely, alcohol and substance abuse and dependence were found to be critical problems among surgeons (R123, 140, 143, 145). Several studies examining surgeon sleep practices found disrupted or shortened sleep to be associated with suboptimal surgeon well-being (R18, 29, 58, 68, 105, 108, 109, 124, 126, 127, 130, 154). Two studies examined pregnancy-related health concerns, finding connections between rigorous rotations and impacts to maternal and fetal health (R112, 160). One study explored personal health issues as a reason for retirement among plastic surgeons (R52). Finally, 1 study evaluated the effectiveness of a time off policy to address health needs (R169).
WORK-LIFE BALANCE
Work-life balance was often considered in relation to burnout (R1,8, 14, 18, 20, 38, 47, 71, 80, 85, 88, 93–96, 167, 175) and career satisfaction (4, 20, 25, 33, 36, 42, 50, 54, 59, 60, 167, 175). Six studies explored the role of work-life balance and overall well-being (R7, 50, 102, 113, 123, 176). Three focused on the stress caused by lack of work-life balance, emphasizing child rearing and impacts on marriage (R104, 142, 177). Eight studies examined gender-based differences (R13, 22, 23, 30, 39, 40, 133, 153), with 2 additional focusing explicitly on motherhood, demonstrating greater family life strain on women than on men (R155, 160). Four studies focused on career stage differences, specifically on risk of attrition earlier in career (R54, 63, 68, 134). Eight studies assessed the impact of resident duty hour regulations, predominantly finding a positive impact on resident perceptions of work-life balance (R70, 79, 105, 106, 110, 124, 125, 129). One study evaluated an initiative aimed at improving work-life balance (R116). Finally, 1 study examined the connection between work-life balance and the use of psychoactive substances (R145).
IMPACTS TO WELL-BEING
General impacts to well-being was the third broad theme, which included work environment, home life, and personal factors (Appendix 5, see http://links.lww.com/AOSO/A11).
Work Environment
Factors related to having a supportive institution (R38, 51, 100) were found to positively impact well-being and included the presence of collegial relationships (R6, 96, 160), resident or fellow support (R132), clerical or administrative support (R9, 112), the presence of a structured mentoring program (R118, 24, 75), protected research time (R6), adequate maternity leave (R112), and being appreciated by patients (R100). Certain institutional settings (R24, 34, 139), such as larger group practices (R92), and professional growth opportunities (R6, 21, 34, 44, 100) were found to be beneficial to surgeon well-being. Finally, 4 studies focused on the benefits of the 80-hour work week restrictions (R109, 128, 129, 131, 146) and 1 on the role of predictable schedules (R44) as they relate to surgeon welfare.
Several factors related to the environment of the institution were found to have a negative impact on well-being: relationships and family, including practice setting (R42, 73, 92), hospital culture (R37, 160, 178, 179), hospital support (R37, 58), lack of mentorship (R65, 90, 160), inadequate referrals (R86), and perception of limited autonomy over delivery of medical services (R71, 85, 100). Adverse peer relationships (R1, 96), poor mentor interactions (R1, 96, 142) personal conflict with partners (R65), perception of being bullied (R37), and issues with operating room (OR) staff (R65, 96, 142) were also found to negatively impact well-being. A significant number of studies reported the consequences of excessive case load, including having large trauma volumes (R86) and work hours (R2, 5, 6, 14, 18, 29, 31, 34, 35, 37, 47, 70, 73, 75, 87, 92, 93, 96, 99, 105, 117, 130, 162, 174, 178) on surgeon well-being. However, inadequate OR exposure among trainees (R1) and complex and rarely performed procedures among attending surgeons (R142) were also assessed and found to have negative impacts on surgeon well-being. Additional studies focused on the impacts of inadequate research and administrative time and spending time on nonclinical activities (R88, 172). Frustration with work (R6, 78, 90), including missed educational opportunities (R17, 31, 35, 37, 42, 93, 175), and a lack of opportunity for career advancement (R65) were associated with dissatisfaction. Three studies found the role of medical error (R82) and recent malpractice lawsuits (R31, 123) to be strongly related to a surgeon’s level of distress. Additional factors contributing to suboptimal well-being included lack of career satisfaction (R71), difficulty communicating with patients (R21, 58, 123), and shame exposure (R72).
Home Life
Satisfaction with work-life balance was found to positively impact well-being (R8, 18, 20, 44, 58). Four studies identified having children (R10, 96, 139, 155), in 1 additional study older children (R31), as having a positive impact. Additionally, having a partner (R6), greater number of years married (R87), and social support (R21) were found to be beneficial to the well-being of surgeons. Finally, social networks (R44), and spending time with those networks (R96), were identified as being advantageous to surgeons.
Tension between work and family were often considered in relation to well-being (R47, 71, 85, 86, 88, 94, 96, 123, 167, 177). Converse to the studies that focused on the positive impacts of having children described above, 3 additional studies focused on the negative impacts of having children at home (R87, 175), with a specific focus on childcare issues (R156). Similarly, 1 study identified having an older adult at home as a source of additional stress (R156). Social and personal stressors (R1, 14), a lack of recreational time (R162), and a lack of personal growth (R71, 177) were all negatively associated with well-being. Finally, several studies explored the impact of stress from strained spousal or partner relationships (R85, 94, 95, 123, 157).
Personal
Both male and female identity were identified as having the potential to positively impact well-being (R9, 31, 139). Two studies identified lower experience level (R9, 104) to positively impact well-being while several identified greater experience level (R29, 60, 87, 141, 180) to be beneficial. Similarly, 1 study found younger age (R9) to be advantageous, while 1 identified older age (R31) as having a positive impact on well-being. Pediatric, cardiothoracic, and neurosurgery were identified as having surgeons with higher levels of well-being (R31, 97). Personal practices, such as making time for hobbies (R7), limiting alcohol use (R7), dispositional mindfulness (R118), and health maintenance (R8), were found to be constructive. Finally, individual characteristics including emotional stability (R12), extraversion (R12), emotional intelligence (R79), positive outlook (R8), grit (R115), and resilience (R163) were found to enhance surgeon well-being.
Negative gender-related attitudes and behaviors were identified as having consequences to surgeons (R19, 25, 30, 37, 75, 99, 123, 155, 157, 162, 181–183). Trauma, vascular, and urology surgical subspecialties (R9, 31, 82, 92, 181, 183, 184) were found to negatively impact surgeon well-being, as were junior academic rank (R37, 53, 93, 183) and younger age (R37, 71, 92, 93, 172, 175). Two studies addressed the impacts of the inability to discuss personal distress (R123) and lack of access to mental health services (R18). Low efficacy (R88) and questioning career choice (R100) were also identified as having a negative impact on well-being.
DISCUSSION
This systematic review is the first to comprehensively examine the critical elements of surgeon well-being, highlighting important and much-needed opportunities for improvement and further investigation. We found that overall, despite the lack of a cohesive definition of well-being, the existing literature was consistent with regard to reporting the multitude of variables that constitute surgeon well-being, its impacts, and the implications of suboptimal well-being. As such, we take this opportunity to present best practices to optimize surgeon well-being using the reviewed literature and framed by a wellness model proposed by the American College of Emergency Physicians, which encompasses occupational, emotional, physical, financial, spiritual, social, and intellectual components (Fig. 3).25
FIGURE 3.

Surgeon well-being components.
The occupation of surgery is characterized by demanding, high-risk work with unique burdens that can contribute to suboptimal well-being.26 The pressure of mastering medical and surgical knowledge, navigating the technical aspects of each case, and hospital logistics may lead to higher rates of burnout and career dissatisfaction among other aspects of well-being. Such negative effects have been associated with a higher likelihood of leaving the surgical field altogether.27 Multiple opportunities exist to help prevent these unfortunate events. Broadly, greater focus should be made on better aligning surgeon skillset with responsibility and authority.28 Meaning, a surgeon who has dedicated substantial time to developing and refining their skills should use their skills and time in the most meaningful and productive ways.29 For example, rather than collecting and sharing health information in an effort to reduce medical error and improve the quality of medical care, electronic health records have led to greater administrative and clerical duties among providers at the expense of direct patient contact and in some cases, physician perceptions of poorer care.30 Redistribution of electronic medical record tasks and other less meaningful administrative duties to nonsurgeons can offload some of this work and allow surgeons to better align their skillset with their responsibilities.31 Excessive caseload, hours worked, and call duties were an important stressor among surgeons in the reviewed studies.32,33 Rather than incentivizing surgeons to focus only on productivity, which has been found to increase the risk of burnout, institutions should offer creative compensation models depending on surgeon need.34 From the resident trainee perspective, attrition rates have been reported to be highest during internship year and among underrepresented minorities and women, and often occur while on certain rotations that inherently require exhaustive work or sleep deprivation.35 This may represent an opportunity to redesign the surgical training curricula to moderate workload as needed and provide meaningful mentorship and support for residents. Finally, institutions must make efforts to reduce barriers for advancement including transparent salary and promotion procedures, opportunities for leadership especially among underrepresented minorities and women, and creating and maintaining a culture where inclusion is a priority and discrimination, harassment, and bullying are not tolerated.
The surgeons’ natural inclination to develop their own practices and mold their respective niches is often challenged when surgeons are forced to balance work with other facets of life.10 Surgeons demonstrate a strong desire to procure protected time in both personal and professional spaces.36 Limiting administrative duties and supporting work that is meaningful to surgeons, as mentioned above, would allow surgeons to develop their own professional interests. Departments may also consider professional development and leadership programs and support collaboration both within and between their disciplines to foster intellectual growth and enhance departmental culture.37,38 Multiple studies have indicated a need for structured mentorship programs to provide both professional guidance and social support with current programs clearly showing improved quality of life measures.39–41 Further, surgeons and institutions may consider promoting opportunities for difficult conversations where individuals are safe to experience vulnerability in discussing patient complications and personal distress.42,43 Such activities may facilitate a cultural shift from one focused on productivity to one that promotes self-care and resilience as well as a space that ensures psychological safety.38,44,45 Surgeons overseeing resident trainees have the unique opportunity of supporting well-being by intentionally refusing to participate in either shaming events or public humiliation, thereby deconstructing the unrealistic idea of the “perfect surgeon.”46,47
Social belonging and constructive, meaningful relationships are known to positively impact surgeon well-being; with interactions taking the form of strong mentorship, affirmative relationships with a spouse or partner, and supportive colleagues.48,49 Through our review, however, the inverse also held true with social stressors, lack of available mentors, and marital distress and work-home conflict contributing to burnout, career dissatisfaction, and decreased overall well-being.48,50,51 Although many studies focus on social support outside of work, our review as well as recent reports examining physician coworker support suggest that stronger collegial support and more robust mentorship also prove beneficial to well-being.52,53 Systems promoting these relationships could include programming activities separate from work duties and locations to bring peers together socially, formal mentor pairing, and peer-to-peer debrief opportunities following emotionally challenging situations among others.54,55
Across studies, surgeons demonstrated high levels of emotional exhaustion and depersonalization, consistent with recent studies of physicians across different specialties.56 Complicating this picture, surgeons often report high rates of alcohol and substance abuse while also reporting low rates of seeking psychologic or psychiatric health due to fear of diminished reputation, loss of respect, and shame or embarrassment in seeking help.57–59 With stigma surrounding mental health being particularly prevalent within surgical subspecialties, there is a need to provide surgeons with stress-management training and to develop systems to identify and intervene in cases of emotional exhaustion.60 Individual factors such as emotional stability, emotional intelligence, coping mechanisms, and personal fulfillment were found to have a positive impact on well-being, although their ability to mitigate more significant anxiety, post-traumatic stress disorder, and the emotional impact of negative outcomes or mass casualty incidents warrants further research.61–64
As a career, surgery is physically demanding and exhausting, requiring surgeons to work long hours and maintain poor and rigid postures for prolonged periods.65 Surgical careers have also been found to impact other areas of physical health—including poor rates of preventative health screenings66 and more issues with female infertility compared to the general population.67 Institutions must actively provide resources that promote surgeon well-being through efforts such as establishing comfortable call rooms where surgeons can rest during night shifts, limiting the number of consecutive hours that a surgeon works,68 introducing more ergonomically favorable ORs and work,42 and providing access to fitness equipment and places.69 Additionally, practical duty hour regulations must be considered for both practicing surgeons and residents. Current Accreditation Council for Graduate Medical Education guidelines only restrict resident duty hours, and even then, they unreasonably allow residents to work 24 consecutive hours,70 which is in direct contrast to Centers for Disease Control and Prevention recommendations for individuals to sleep at least 7 hours every 24 hours.71 Most importantly, it is imperative that institutions and surgical departments cultivate and promote a culture that encourages surgeons to take personal time to address and maintain their physical health needs at their own discretion.
A significant disadvantage of the nature of surgical training is the accrual of large financial debt—through the costs of medical education, examinations, and post-graduate training—upwards of $350,000, which surgeons continue to repay even 30 years post-graduation.72 This problem is exacerbated by the lack of support available to surgeons, specifically when trying to navigate financial matters such as financial planning, contract negotiations, and loan repayment. Moreover, a significant salary inequity exists between men and women physicians, with women physicians of all specialties being compensated about $51,000 less than their male colleagues.73 Additionally, despite surgeons increasingly caring and operating on more complicated, older patients, compensations have remained the same for 20 years, despite a significant increase in the cost of goods.74 In other words, surgeons are not being incentivized to do more work for less pay. The constant anxiety regarding these financial concerns has been shown to negatively impact physician well-being.73 In order to address this burden at an institutional level, more focus should be placed on providing equitable support and guidance when navigating contract negotiations and establishing and disseminating information that promotes financial well-being. At a broader level, however, significant opportunities exist to reevaluate the financial debt of surgeons, with significant need to provide greater access to loan forgiveness and repayment options to surgeons through both federally supported programs, such as the National Institutes of Health Loan Repayment Program, and institution-specific programs.
Our search has several limitations inherent to systematic reviews. First, we recognize that well-being measurement has yet to reach consensus.75 However, we were intentionally broad in our definition of well-being in an effort to be as inclusive as possible when conducting our search. Further, although publication and search biases were possible, we strived to minimize these through broad capture of surgeon well-being, specifically by searching 5 large databases with the assistance of a research librarian and performing a hand search of all the references from the included studies. Although we recognize that there are other elements that may impact surgical well-being (eg, physical and emotional stress in OR specifically), we chose to focus our study on the less technical elements of surgery. Furthermore, despite our focus on studies in the United States, our findings may plausibly be extrapolated across different countries. Previous literature has demonstrated shared concerns in surgeon well-being across multiple countries including optimal strategies for intervention at various phases during a surgeon’s career. Finally, we recognize the limitations of the solutions offered and acknowledge that this was not meant to be a comprehensive review of interventions. Despite these limitations, our findings are consistent with the attitudes and practices of physicians in other nonsurgical specialties.
CONCLUSIONS
To our knowledge, this is the first systematic review to comprehensively characterize surgeon well-being and potential interventions that promote and support both practicing surgeons and surgical trainees. Beyond burnout and career satisfaction, we provide a more nuanced examination of surgeon well-being, systematically evaluating its components, influential factors, and the subsequent consequences of suboptimal well-being. Importantly, the numerous negative effects of suboptimal well-being highlight the critical need to develop and implement effective interventions that encompass both the personal and professional domains such that lasting and meaningful change occurs.
ACKNOWLEDGMENTS
The authors would like to thank Elayna Sabelhaus for assistance with this study.
Supplementary Material
Footnotes
P.A.S. receives funding through the National Institute on Aging Grants for Early Medical/Surgical Specialists’ Transition to Aging Research (R03 AG056588) and the Agency for Healthcare Research and Quality (K08 HS026772).
Disclosure: The authors declare that they have nothing to disclose.
C.A.V. and P.A.S. participated in the research design. All authors participated in the writing of the article, performance of the research, and data analysis. All authors contributed new reagents or analytic tools.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Brigham T, Barden C, Legreid Dopp A, et al. A Journey to Construct an All-Encompassing Conceptual Model of Factors Affecting Clinician Well-Being and Resilience. 2018. National Academy of Medicine. Available at: https://nam.edu/journey-construct-encompassing-conceptual-model-factors-affecting-clinician-well-resilience/. Accessed September 5, 2020 [Google Scholar]
- 2.Sargent MC, Sotile W, Sotile MO, et al. Quality of life during orthopaedic training and academic practice. Part 1: orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009; 91:2395–2405 [DOI] [PubMed] [Google Scholar]
- 3.Firth-Cozens J, Greenhalgh J.Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997; 44:1017–1022 [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002; 136:358–367 [DOI] [PubMed] [Google Scholar]
- 5.Maher Z, Milner R, Cripe J, et al. Stress training for the surgical resident. Am J Surg. 2013; 205:169–174 [DOI] [PubMed] [Google Scholar]
- 6.Dodson TF, Webb AL.Why do residents leave general surgery? The hidden problem in today’s programs. Curr Surg. 2005; 62:128–131 [DOI] [PubMed] [Google Scholar]
- 7.Gifford E, Galante J, Kaji AH, et al. Factors associated with general surgery residents’ desire to leave residency programs: a multi-institutional study. JAMA Surg. 2014; 149:948–953 [DOI] [PubMed] [Google Scholar]
- 8.Jager AJ, Tutty MA, Kao AC.Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017; 92:415–422 [DOI] [PubMed] [Google Scholar]
- 9.Freudenberger HJ.Staff burn-out. J Soc Issues. 1974; 30:159–165 [Google Scholar]
- 10.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009; 250:463–471 [DOI] [PubMed] [Google Scholar]
- 11.Balch CM, Shanafelt TD, Sloan JA, et al. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011; 254:558–568 [DOI] [PubMed] [Google Scholar]
- 12.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012; 147:168–174 [DOI] [PubMed] [Google Scholar]
- 13.Siedsma M, Emlet L.Physician burnout: can we make a difference together? Crit Care. 2015; 19:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanafelt TD, Kaups KL, Nelson H, et al. An interactive individualized intervention to promote behavioral change to increase personal well-being in US surgeons. Ann Surg. 2014; 259:82–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dimou FM, Eckelbarger D, Riall TS.Surgeon burnout: a systematic review. J Am Coll Surg. 2016; 222:1230–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eden J, Levit L, Berg A, et al.Institute of Medicine (US) Committee on Standards for Systematic Reviews of Comparative Effectiveness Research. Finding What Works in Health Care: Standards for Systematic Reviews. 2011. National Academies Press (US) [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62:e1–34 [DOI] [PubMed] [Google Scholar]
- 18.Guetterman TC, Fetters MD, Creswell JW.Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann Fam Med. 2015; 13:554–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suwanabol PA, Kanters AE, Reichstein AC, et al. Characterizing the role of U.S. surgeons in the provision of palliative care: a systematic review and mixed-methods meta-synthesis. J Pain Symptom Manage. 2018; 55:1196–1215.e5 [DOI] [PubMed] [Google Scholar]
- 20.Mouch CA, Regenbogen SE, Revels SL, et al. The quality of surgical care in safety net hospitals: a systematic review. Surgery. 2014; 155:826–838 [DOI] [PubMed] [Google Scholar]
- 21.Dossett LA, Hudson JN, Morris AM, et al. The primary care provider (PCP)-cancer specialist relationship: a systematic review and mixed-methods meta-synthesis. CA Cancer J Clin. 2017; 67:156–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stroup DF, Berlin JA, Morton SC, et al. MOOSE guidelines for meta-analyses and systematic reviews of observational studies. JAMA. 2000; 283:2008–2012 [DOI] [PubMed] [Google Scholar]
- 23.Dixon-woods M, Agarwal S, Young B, et al. Integrative Approaches to Qualitative and Quantitative Evidence. Health Development Agency; 2004 [Google Scholar]
- 24.Sandelowski M, Voils CI, Barroso J.Defining and Designing Mixed Research Synthesis Studies. Res Sch. 2006; 13:29. [PMC free article] [PubMed] [Google Scholar]
- 25.Manfredi RA, Huber JM.Being Well in Emergency Medicine: ACEP’s Guide to Investing in Yourself. 2017. American College of Emergency Physicians [Google Scholar]
- 26.Campbell DA, Sonnad SS, Eckhauser FE, et al. Burnout among American surgeons. Surgery. 2001; 130:695–696 [DOI] [PubMed] [Google Scholar]
- 27.Antiel RM, Reed DA, Van Arendonk KJ, et al. Effects of duty hour restrictions on core competencies, education, quality of life, and burnout among general surgery interns. JAMA Surg. 2013; 148:448–455 [DOI] [PubMed] [Google Scholar]
- 28.Johnson CA, Corey BL.Kao L, Chen H.Healthcare role. Success in Academic Surgery: Wellbeing. 2020. Springer; 41–52 [Google Scholar]
- 29.Rothenberger DA.Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017; 60:567–576 [DOI] [PubMed] [Google Scholar]
- 30.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016; 91:422–431 [DOI] [PubMed] [Google Scholar]
- 31.DiAngi YT, Longhurst CA, Payne TH.Taming the EHR (electronic health record) - there is hope. J Fam Med. 2016; 3:1072. [PMC free article] [PubMed] [Google Scholar]
- 32.Sawyer RG, Tribble CG, Newberg DS, et al. Intern call schedules and their relationship to sleep, operating room participation, stress, and satisfaction. Surgery. 1999; 126:337–342 [PubMed] [Google Scholar]
- 33.Lind A, Latz K, Sinclair MR, et al. Pediatric orthopaedic surgeons dissatisfied in on-call practices despite improving call conditions. The 2015 POSNA Membership Survey Regarding Trauma Care. J Pediatr Orthop. 2018; 38:e33–e37 [DOI] [PubMed] [Google Scholar]
- 34.Shanafelt TD, Noseworthy JH.Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017; 92:129–146 [DOI] [PubMed] [Google Scholar]
- 35.Sullivan MC, Yeo H, Roman SA, et al. Surgical residency and attrition: defining the individual and programmatic factors predictive of trainee losses. J Am Coll Surg. 2013; 216:461–471 [DOI] [PubMed] [Google Scholar]
- 36.Balch CM, Shanafelt TD, Sloan J, et al. Burnout and career satisfaction among surgical oncologists compared with other surgical specialties. Ann Surg Oncol. 2011; 18:16–25 [DOI] [PubMed] [Google Scholar]
- 37.Vitous CA, Shubeck S, Kanters A, et al. Reflections on a leadership development program: impacts on culture in a surgical environment. Surgery. 2019; 166:721–725 [DOI] [PubMed] [Google Scholar]
- 38.Patel AM, Ingalls NK, Mansour MA, et al. Collateral damage: the effect of patient complications on the surgeon’s psyche. Surgery. 2010; 148:824–828; discussion 828–830 [DOI] [PubMed] [Google Scholar]
- 39.Attenello FJ, Buchanan IA, Wen T, et al. Factors associated with burnout among US neurosurgery residents: a nationwide survey. J Neurosurg. 2018; 129:1349–1363 [DOI] [PubMed] [Google Scholar]
- 40.Jackson TN, Morgan JP, Jackson DL, et al. The crossroads of posttraumatic stress disorder and physician burnout: a national review of United States trauma and nontrauma surgeons. Am Surg. 2019; 85:127–135 [PubMed] [Google Scholar]
- 41.Salles A, Liebert CA, Esquivel M, et al. Perceived value of a program to promote surgical resident well-being. J Surg Educ. 2017; 74:921–927 [DOI] [PubMed] [Google Scholar]
- 42.Han K, Bohnen JD, Peponis T, et al. The surgeon as the second victim? Results of the Boston Intraoperative Adverse Events Surgeons’ Attitude (BISA) Study. J Am Coll Surg. 2017; 224:1048–1056 [DOI] [PubMed] [Google Scholar]
- 43.Pinto A, Faiz O, Bicknell C, et al. Acute traumatic stress among surgeons after major surgical complications. Am J Surg. 2014; 208:642–647 [DOI] [PubMed] [Google Scholar]
- 44.Guest RS, Baser R, Li Y, et al. Cancer surgeons’ distress and well-being, I: the tension between a culture of productivity and the need for self-care. Ann Surg Oncol. 2011; 18:1229–1235 [DOI] [PubMed] [Google Scholar]
- 45.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010; 251:995–1000 [DOI] [PubMed] [Google Scholar]
- 46.Shapiro MC, Rao SR, Dean J, et al. What a shame: increased rates of OMS resident burnout may be related to the frequency of shamed events during training. J Oral Maxillofac Surg. 2017; 75:449–457 [DOI] [PubMed] [Google Scholar]
- 47.Al Atassi H, Shapiro MC, Rao SR, et al. Oral and maxillofacial surgery resident perception of personal achievement and anxiety: a cross-sectional analysis. J Oral Maxillofac Surg. 2018; 76:2532–2539 [DOI] [PubMed] [Google Scholar]
- 48.Crafts TD, Bell TM, Srisuwananukorn A, et al. Accounting for early job turnover in recent pediatric surgery fellowship graduates: an American Pediatric Surgical Association Membership and Credentials Committee study. J Pediatr Surg. 2018; 53:2273–2278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wai PY, Dandar V, Radosevich DM, et al. Engagement, workplace satisfaction, and retention of surgical specialists in academic medicine in the United States. J Am Coll Surg. 2014; 219:31–42 [DOI] [PubMed] [Google Scholar]
- 50.Martini S, Arfken CL, Churchill A, et al. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004; 28:240–242 [DOI] [PubMed] [Google Scholar]
- 51.Cyr-Taro AE, Kotwall CA, Menon RP, et al. Employment and satisfaction trends among general surgery residents from a community hospital. J Surg Educ. 2008; 65:43–49 [DOI] [PubMed] [Google Scholar]
- 52.Mikkola L, Suutala E, Parviainen H.Social support in the workplace for physicians in specialization training. Med Educ Online. 2018; 23:1435114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamama L, Hamama-Raz Y, Stokar YN, et al. Burnout and perceived social support: the mediating role of secondary traumatization in nurses vs. physicians. J Adv Nurs. 2019; 75:2742–2752 [DOI] [PubMed] [Google Scholar]
- 54.Scott SD, Hirschinger LE, Cox KR, et al. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009; 18:325–330 [DOI] [PubMed] [Google Scholar]
- 55.Taylor C, Xyrichis A, Leamy MC, et al. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open. 2018; 8:e024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee RT, Seo B, Hladkyj S, et al. Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resour Health. 2013; 11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011; 146:54–62 [DOI] [PubMed] [Google Scholar]
- 58.Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012; 147:212–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tschuor C, Raptis DA, Morf MC, et al. Job satisfaction among chairs of surgery from Europe and North America. Surgery. 2014; 156:1069–1077 [DOI] [PubMed] [Google Scholar]
- 60.Hendin H, Reynolds C, Fox D, et al. Licensing and physician mental health: problems and possibilities. J Med Licens Discip. 2007; 93:6–11 [Google Scholar]
- 61.Foulkrod KH, Field C, Brown CVR.Trauma surgeon personality and job satisfaction: results from a national survey. Am Surg. 2010; 76:422–427 [DOI] [PubMed] [Google Scholar]
- 62.Hollis RH, Theiss LM, Gullick AA, et al. Emotional intelligence in surgery is associated with resident job satisfaction. J Surg Res. 2017; 209:178–183 [DOI] [PubMed] [Google Scholar]
- 63.Anton NE, Montero PN, Howley LD, et al. What stress coping strategies are surgeons relying upon during surgery? Am J Surg. 2015; 210:846–851 [DOI] [PubMed] [Google Scholar]
- 64.Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg. 2012; 255:625–633 [DOI] [PubMed] [Google Scholar]
- 65.Kant IJ, de Jong LC, van Rijssen-Moll M, et al. A survey of static and dynamic work postures of operating room staff. Int Arch Occup Environ Health. 1992; 63:423–428 [DOI] [PubMed] [Google Scholar]
- 66.Brandt ML.Sustaining a career in surgery. Am J Surg. 2017; 214:707–714 [DOI] [PubMed] [Google Scholar]
- 67.Phillips EA, Nimeh T, Braga J, et al. Does a surgical career affect a woman’s childbearing and fertility? A report on pregnancy and fertility trends among female surgeons. J Am Coll Surg. 2014; 219:944–950 [DOI] [PubMed] [Google Scholar]
- 68.Park AE, Zahiri HR, Hallbeck MS, et al. Intraoperative “Micro Breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg. 2017; 265:340–346 [DOI] [PubMed] [Google Scholar]
- 69.Fargen KM, Spiotta AM, Turner RD, et al. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016; 90:380–384 [DOI] [PubMed] [Google Scholar]
- 70.Accreditation Council for Graduate Medical Education.. Resident duty hours in the learning and working environment: comparison of 2003 and 2011 standards. Available at: http://www.acgme.org/Portals/0/PDFs/dh-ComparisonTable2003v2011.pdf. Accessed September 1, 2020
- 71.Centers for Disease Control and Prevention. Are You Getting Enough Sleep? 2020. Available at: https://www.cdc.gov/sleep/features/getting-enough-sleep.html. Accessed September 1, 2020
- 72.Jolly P.Medical school tuition and young physicians’ indebtedness. If tuition continues its rapid increase, young physicians may find it difficult to repay their medical school debts, and some students may be deterred from attempting a career in medicine. Health Aff. 2005; 24:527–535 [DOI] [PubMed] [Google Scholar]
- 73.Arnold MW, Dibrito SR.Kim E, Lindeman B.Personal factors. Wellbeing. 2020. Springer:53–61 [Google Scholar]
- 74.Rekman JF, Alseidi A.Kim E, Lindeman B.Regulatory, business, and payer environment. Wellbeing. 2020. Springer International Publishing:103–117 [Google Scholar]
- 75.Raj KS.Well-being in residency: a systematic review. J Grad Med Educ. 2016; 8:674–684 [DOI] [PMC free article] [PubMed] [Google Scholar]


