Background:
Breast augmentation is one of the most frequently performed aesthetic procedures in the United States. Online information is often used by patients to make decisions when undergoing cosmetic procedures. It is vital that online medical information includes relevant decision-making factors and uses language that is understandable to broad patient audiences. Ideally, online resources should aid patient decisions in aesthetic surgical planning, especially implant size selection for breast augmentation. We describe patient decision-making factors and readability of breast implant size selection recommended by private practice plastic surgery webpages.
Methods:
Using a depersonalized, anonymous query to Google search engine, the terms “breast implant size factors” and “breast implant size decision” were searched, and 52 plastic surgery private practice webpages were identified. Webpages were analyzed for reported decision-making factors of implant size selection. Readability analyses of webpages were performed with Readability Studio and Hemingway Editor.
Results:
The two major decision-making factors for implant size selection reported by webpages were body/tissue-based measurements and surgeon input. Ten factors related to patient lifestyle, surgical goals, and procedural options were also identified. Average webpage scores for five readability measures exceeded recommended levels for medical information.
Conclusions:
Reported decision-making factors for implant size selection emphasize a plastic surgeon’s expertise but may enhance the patient’s role in preoperative planning. Webpages describing breast implant size selection exceed the sixth and eighth grade reading levels recommended by the AMA and NIH, respectively. Improving the readability of webpages will refine the role of online medical information in preoperative planning of breast augmentation.
Takeaways
Question: How well do practice webpages inform patients on preoperative breast implant size selection?
Findings: We identified 12 reported decision-making factors related to implant size selection, with webpages discussing a median of six factors. Surgeon input and tissue-based measurements were the most commonly reported factors. Readability scores of webpages exceeded recommended reading levels for online medical information.
Meaning: Practice webpages are invaluable to patients and offer a depth of information related to procedural details, but greater attention is needed to ensure webpages are comprehensive and digestible to broad patient audiences.
INTRODUCTION
Breast augmentation is one of the most popular aesthetic surgical procedures performed by plastic surgeons in the United States.1,2 However, the surgery is often subject to reoperation and is a major source of medical litigation.3–7 Preoperative planning, shared decision-making, and level-setting patient expectations can help address these issues. Therefore, it is vital that patients’ expectations are shaped by accurate and comprehensive information to optimize preoperative consultation communication and avoid medical and legal complications.8–11 Today, most preoperative approaches include five features: patient education and informed consent,4,12–15communication of patient goals,4,14,16 tissue-based measurements,4,12,13,15,16 patient decision support devices,4,12–14,16 and review of implant and surgical options.13
Online medical information is a key element of patient planning, utilized by 95% of aesthetic surgery patients before in-office consultation.10 Despite the growing prevalence of plastic surgery content on social media platforms, practice websites remain a popular and heavily utilized information source for patients. Over 50% of plastic surgery patients indicate utilization of plastic surgery practice websites.17,18 Aside from before and after photographs, medical information related to procedures of interest is the most popular form of practice website content.17 The internet also guides how patients select their plastic surgeon. Half of breast augmentation patients find their plastic surgeon on the internet, and reported that a plastic surgeon’s website influenced their decision to undergo surgery.3 Unfortunately, the quality and readability of online medical information related to aesthetic procedures is not always appropriate.1,9,10,19–22 Prior research has also found that breast reconstruction content on plastic surgery society and academic websites is less readable than nonacademic sites, signaling a barrier to patient access of high-quality information.23,24
There is a continual need to improve patient resources in aesthetic surgery. The aim of our study was to assess content and readability of webpages discussing preoperative breast implant size selection to determine how well they inform patients before in-office consultation. Our team hypothesized that the content and poor readability of online information regarding breast augmentation may be contributing to inappropriate levels of expectation and possible dissatisfaction with outcomes. We detail 52 webpages representing 50 plastic surgery practices in the United States. Prior studies have analyzed the readability of breast augmentation websites, but ours is the first to also examine reported decision-making factors for implant size selection. By characterizing both content and readability, their role as a patient resource in preoperative planning is better understood.
METHODS
Webpage Identification
The terms “breast implant size factors” and “breast implant size decision” were searched using Google search engine, on December 6, 2021 and updated on August 20, 2022. To depersonalize search results, Startpage.com was utilized to send anonymous, depersonalized searches to Google’s search engine that are not shaped by user settings, location, IP address, search history, or cookies.25 The first 30 results from each search term were analyzed at both time points. Inclusion criteria were US plastic surgery practice webpages related to implant size selection. Exclusion criteria were (1) advertisements, (2) webpages unrelated to implant size selection, and (3) nonpractice webpages, such as those belonging to informational sites, companies, academic institutions, or plastic surgery organizations. Private practice surgeon gender and US state location details were extracted from included webpages.
Webpage Text Qualitative Analysis
Webpage texts were extracted and analyzed independently for stated decision-making factors of breast implant size selection by two authors (J.E.F. and E.C.L.). Coding and identification of factors was completed to establish decision-making categories. Discrepancies between authors’ coding were resolved by shared analysis and discussion. Webpages were also assessed for surgeon gender and US state location. Decision-making factors were tabulated by webpage for descriptive statistical analysis and comparison. One-way ANOVA was run to analyze differences in reported decision-making factors by gender of practice surgeon(s) (man, woman, or both) and practice location (geographic regions: Northeast, Southeast, Midwest, Southwest, or West).
Webpage Text Readability Analyses
Webpage texts were batch imported into Readability Professional Studio software.26 Flesch-Kincaid, Flesch Reading Ease, Fry, Gunning Fog, Raygor Estimate, and SMOG readability test measures were run by batch calculation, on August 20, 2022. (See table, Supplemental Digital Content 1, which displays the scale, equation, and assessed qualities of six readability measures utilized in this study. http://links.lww.com/PRSGO/C370.) In addition, webpage texts were imported into the Hemingway Editor webtool.27 Readability results and text metrics were extracted for analysis. One-way ANOVA was run to analyze differences in readability scores by gender of practice surgeon(s) (man, woman, or both) and practice location (geographic regions: Northeast, Southeast, Midwest, Southwest, or West).
RESULTS
Private Practice Breakdown
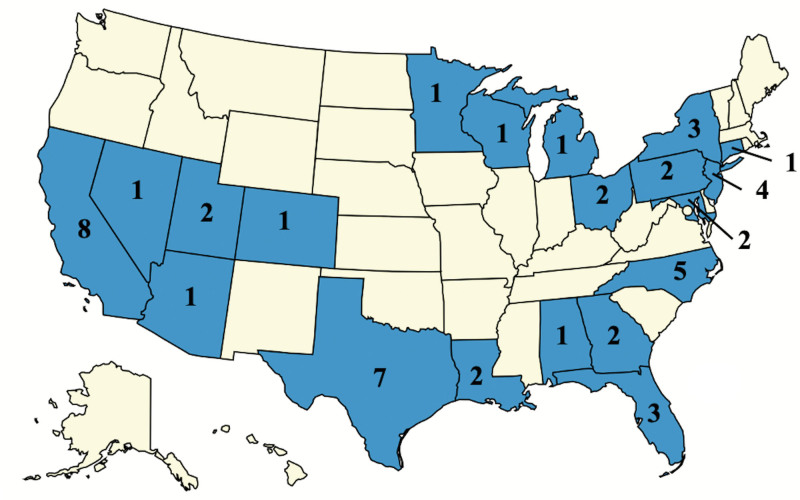
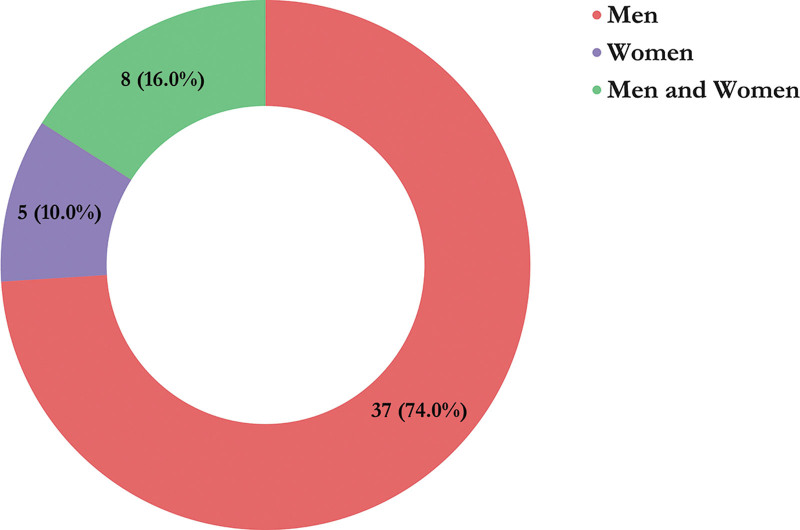
A total of 52 unique webpages representing 50 plastic surgery private practices met the inclusion criteria: 30 webpages from “breast implant size factors” and 30 webpages from “breast implant size decision” searches were included, with eight overlapping webpage results. Two practices each had two unique webpages dedicated to breast implant size selection. Practices were distributed across 20 US states, with California, Texas, North Carolina, and New Jersey being most represented. Figure 1 maps the distribution of included practices across individual states. The majority of practices were represented by male surgeons (74%), whereas 10% were represented by women and 16% by both men and women. Figure 2 provides a visual breakdown of plastic surgeon gender among included practices.
Fig. 1.
A US map showing the number of included practices in each state.
Fig. 2.
A pie chart demonstrating the breakdown of included practices’ surgeon genders.
Decision-making Factor Analysis
We identified 12 decision-making factors for breast implant sizing reported by practice webpages. These factors were reflective of the five core elements of preoperative planning in breast augmentation that have been developed over the past 20 years. The number of decision-making factors ranged from two to 10, with a mean of 5.73 factors and median of six factors. The proportion of webpages reporting each decision-making factor varied, ranging from 15.38% (consultation with loved ones) to 86.54% (body and tissue-based measurements, surgeon input). No significant differences in average number of reported decision-making factors were found between webpages when analyzed by geographic region or surgeon gender (one-way ANOVA tests). Table 1 provides an overview of the 12 identified decision-making factors and their prevalence among webpages.
Table 1.
Decision-making Factors for Implant Size Selection in 52 Webpages
| Elements of Preoperative Planning | Decision-making Factors Identified | Percentage of Webpages | Example Considerations |
|---|---|---|---|
| Patient education and informed consent | Surgeon input | 86.54% | Share goals during consult, trust physician authority |
| Lifestyle | 51.92% | Exercise, career, clothing | |
| Complications and adverse outcomes | 30.77% | Back pain, future implant removal, infection | |
| Fertility and aging | 21.15% | Future pregnancy, breastfeeding, and breast growth | |
| Family/friend input | 15.38% | Bring someone to consultation, discuss options with others | |
| Communication of patient goals | Conception of goal size | 61.54% | Do not reference bra sizes, over/underestimate implant size |
| Surgical motivation | 57.69% | Restore shape after breastfeeding, increase size | |
| Correct breast asymmetry | 19.23% | Correct incongruous breast sizes or breast deformity | |
| Tissue-based measurements | Body and tissue-based measurements | 86.54% | Height, weight, skin elasticity, breast dimensions, breast size |
| Patient decision support Devices | 3D imaging, photography, wearable sizers | 61.54% | 3D simulation, reference photos, wearable implant sizers |
| Review of implant and surgical options | Other features of implant | 55.77% | Implant profile, type, and shape |
| Procedural considerations | 25% | Concurrent breast lift, implant placement |
Readability
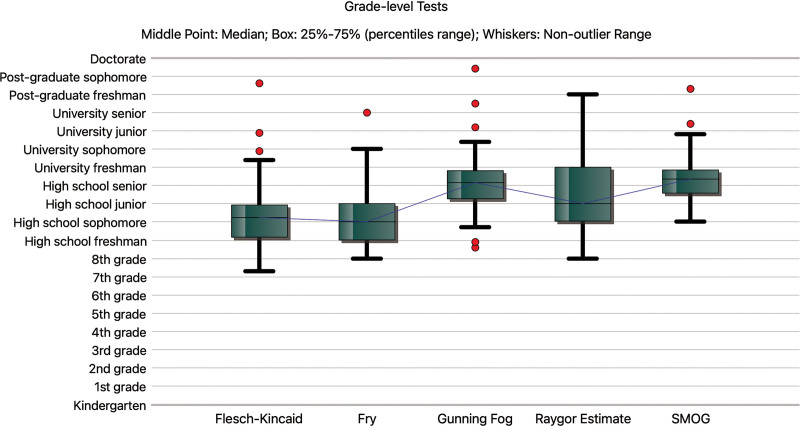
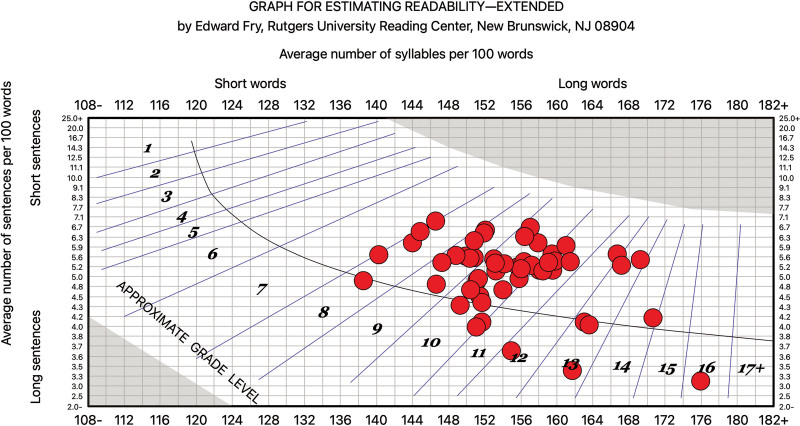
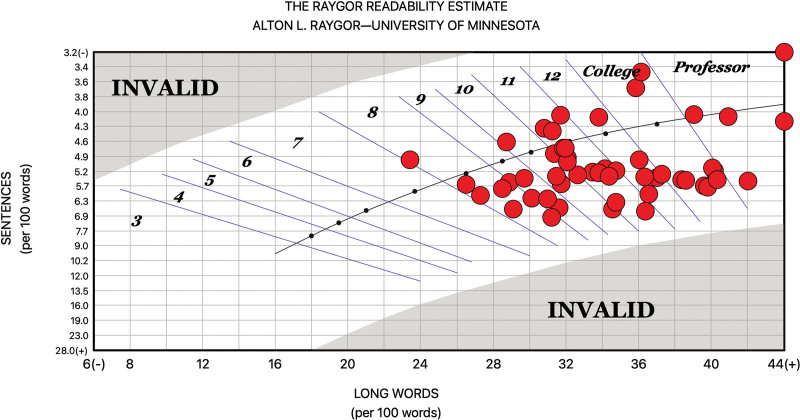
Across all readability measures, mean readability scores exceeded the sixth grade and eighth grade reading levels recommended by the American Medical Association and National Institutes of Health, respectively.28,29 Average readability scores of webpages spanned high school to college level for all readability measures, with five readability scores ranging from 10 to 12.3 grade levels. Table 2 lists average webpage scores for all six readability measures utilized in this study. Several webpage readability scores extended beyond college level. Figure 3 provides readability score box plots for five readability measures scored on a grade-level scale. Figure 4 provides the distribution of individual webpage Fry Readability scores. Figure 5 provides the distribution of individual Raygor Estimate Readability scores. The average Hemingway Editor readability score for webpages was 9.44 grade level. The average time to read each webpage was 2 minutes and 57 seconds. Webpages had an average of 5.06 complex phrases, 9.81 sentences that are hard to read, and 9.98 sentences that are very hard to read. Table 3 provides the full report of average webpage readability scores from Hemingway Editor. Average Fry readability scores differed by geographic region (P < 0.03, one-way ANOVA) but average scores did not differ by other readability measures or surgeon gender. Table 4 provides all one-way ANOVA P values analyzing the association between practice location and surgeon gender with the number of reported decision-making factors and six readability scores.
Table 2.
Average Readability Scores of Webpages Guiding Breast Implant Size Selection
| Readability Professional Studio Software | ||
|---|---|---|
| Readability Measure | Average Readability Score | Scale |
| Flesch-Kincaid score | 10.4 | Grade level |
| Flesch Reading Ease score | 58 | 0–100 (100 = easiest) |
| Fry score | 10 | Grade level |
| Gunning Fog score | 12.2 | Grade level |
| Raygor Estimate score | 11 | Grade level |
| SMOG score | 12.3 | Grade level |
Fig. 3.
Box and whisker plot of scores of five readability measures on grade-level scale.
Fig. 4.
A labeled scatter plot of individual webpage Fry Readability scores.
Fig. 5.
A labeled scatter plot of individual webpage Raygor Estimate Readability scores.
Table 3.
Hemingway Editor Analysis of Webpages Guiding Breast Implant Size Selection
| Hemingway Editor Writing Analysis Webtool | |
|---|---|
| Textual Analysis Elements | Average Score |
| Education required to read (grade level) | 9.44 |
| Reading time | 2 minutes and 57 seconds |
| Number of words | 743.08 words |
| Number of sentences | 44.40 sentences |
| Number of uses of passive voice | 4.04 uses of passive voice |
| Number of phrases with simpler alternatives | 5.06 phrases with simpler alternatives |
| Number of sentences that are hard to read | 9.81 sentences that are hard to read |
| Number of sentences that are very hard to read | 9.98 sentences that are very hard to read |
Table 4.
One-way ANOVA P Values Analyzing Differences in Number of Implant Size Decision-making Factors and Readability Scores
| Groups | Decision-making Factors | Flesch-Kincaid | Flesch Reading Ease | Fry | Gunning Fog | Raygor Estimate | SMOG |
|---|---|---|---|---|---|---|---|
| Geographic regions | 0.32117568 | 0.08033026 | 0.0530873 | 0.02962899 | 0.2906447 | 0.13217852 | 0.05845738 |
| Surgeon gender | 0.12228598 | 0.7198601 | 0.44977633 | 0.18622791 | 0.76931349 | 0.34550834 | 0.74086001 |
Boldface indicates statistically significant difference in Fry readability scores between private practice websites when grouping websites by the practice’s U.S. geographic location (Northeast, Southeast, Midwest, Southwest, and West).
DISCUSSION
To our knowledge, this study is the first to analyze US plastic surgery practice webpages for decision-making factors of implant size selection. Our findings indicate that discussion of implant sizing is not significantly shaped by surgeons’ geographic location or gender. However, websites frequently omitted core elements of preoperative planning. Correlating our 12 identified factors to five common features of preoperative planning in breast augmentation, we established that approximately 38% (20/52) of webpages omitted any discussion of either reviewing implant/surgical options or patient decision support devices. Only 27% (14/52) of webpages reported decision-making factors representing all five elements of preoperative planning.
The most prevalent decision-making factors were tissue-based measurements and surgeon input (both 86.54%). Webpages varied in their discussion of biometric considerations, with some mentioning broad, poorly-defined characteristics such as body size and proportion, while other webpages offered implant size selection algorithms based on a series of specific body and tissue-based measurements. Patient measurements included height, weight, shoulder width, baseline breast tissue, chest dimensions, breast dimensions, and breast envelope size. Tissue-based measurements were emphasized as a constraint on implant size to maintain overall body proportionality and reduce complications.
The second most prevalent decision-making factor discussed was surgeon input. The tone of surgeon input varied, with some webpages only stating that patients should contact the surgeon. In contrast, others explicitly convey the surgeon’s final authority in implant size. Webpages frequently reminded readers that in-person consultation with a plastic surgeon is required before implant size selection. Management of patient expectations continues to be a vital aspect of preoperative planning in plastic surgery. Emphasizing physician expertise and tissue-based measurements as an integral part of preoperative planning manages expectations from the beginning of patients’ self-directed online searching.
Unhappiness with breast implant size and involvement of family/friends in the postoperative period are two major sources of patient dissatisfaction with breast augmentation results.7 We identified several decision-making factors in webpages that address these complaints. Discussions of patient lifestyle, fertility and aging, and conception of breast size reflect elements of patient education that minimize patient dissatisfaction and surgical complications. The discordance between how plastic surgeons and patients conceptualize breast size (cubic centiliters versus bra cup size) is a major obstacle to patient education and preoperative planning.14,15 In over 60% of webpages, patients were directed to consider goal breast size in terms of implant size volume. Additionally, 15% of webpages recommended that patients consult with loved ones during the preoperative period. This suggestion can reduce the risk of patients being influenced by negative opinions from family and friends after surgery.
Prior review of plastic surgery health literacy research suggests that plastic surgeons should dedicate a greater proportion of patient education to discussion of risks and outline surgical details.8,23 With only 31% and 25% of webpages discussing complications/adverse outcomes and procedural considerations, respectively, our analysis reflects the importance of these recommendations. Of note, only one webpage discussed the risk of breast implant associated anaplastic large cell lymphoma.
Our findings demonstrate that the readability of webpages focused on implant selection was poor, as mean reading grade levels (10–12.3) ranged from high school to college levels, exceeding current guidelines. This is in agreement with prior analyses of plastic surgery breast resources, reflecting an unresolved need for online resources that are inclusive and accessible to broad patient audiences.23 With the exception of average Fry readability scores, readability scores of practice webpages did not significantly differ by surgeons’ geographic location and none significantly differed by gender. Efforts to improve online medical writing are thus concrete and can be facilitated by use of freely accessible resources, such as the Hemingway Editor webtool.27 Our results from Hemingway Editor clarified that increasing the use of simple phrasing and shorter sentence-structures represent two concrete steps toward improving readability for patients. Tiourin et al’s scoping review of health literacy in plastic surgery proposed key steps for improving readability and also recommended increasing the use of short, simple words and sentences in medical information.23 Additionally, Patel et al recently published on the readability of online information related to cosmetic injectables and propose an iterative algorithm for improving readability, quality, and technical aspects of websites containing medical information.8,9 The wide scope of information contained in practice websites makes them an invaluable resource to patients.17 Plastic surgeons offering online advice to patients for preoperative planning of breast augmentation have a vested interest in ensuring that this medical information is comprehensive and readable.
Although the present study expands the literature on readability of online information related to breast augmentation, only 60 total Google webpage results were examined at each time point for inclusion and exclusion criteria. It is unclear whether aesthetic surgery patients prioritize practice websites over other online sources of medical information, such as academic websites and social media. Future studies should seek input from patients on the role of online medical information in preoperative planning and should assess whether utilization translates to satisfaction with surgical results.
CONCLUSIONS
The chief priority in plastic surgery must always be patient safety and desirable, sustainable outcomes. These concerns are particularly relevant in aesthetic surgical procedures with increasing exposure and popularization online. Online medical information that is accessible and readable to broad patient audiences is crucial to achieving this goal. By reporting elements of preoperative planning online, plastic surgeons manage patient expectations, optimize in-person consultation, and frame breast augmentation results as an outcome of shared decision-making. Emphasis on tissue-based measurements and surgeon input for implant size selection ensure that patients know implant sizing will not exceed what can be safely accommodated. Still, reported decision-making factors are oriented to patient satisfaction. Carefully curated webpages that prepare a patient for their first in-person consultation and serve as a patient decision aid can enhance the physician–patient relationship in preoperative planning. However, our findings reveal that these webpages exceed recommended readability levels, which limit their utility to patients. Though online guides for implant size selection are well-intentioned, plastic surgeons must ensure that their online writing can be grasped by patients to empower their decision-making capacity.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.American Society of Plastic Surgeons. Plastic surgery statistics report 2020. April 27, 2022. Available at https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf. Accessed August 20, 2022
- 2.Mehta S, Farhadi J, Atrey A. A review of litigation in plastic surgery in England. Lessons learned. J Plast Reconstr Aesthet Surg. 2010;63:1747–1748. [DOI] [PubMed] [Google Scholar]
- 3.Didie ER, Sarwer DB. Factors that influence the decision to undergo cosmetic breast augmentation surgery. J Womens Health (Larchmt). 2003;12:241–253. [DOI] [PubMed] [Google Scholar]
- 4.Nava MB, Rocco N, Tunesi G, et al. Decisional pathways in breast augmentation: how to improve outcomes through accurate pre-operative planning. Gland Surg. 2017;6:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spear SL, Dayan JH, West J. The anatomy of revisions after primary breast augmentation: one surgeon’s perspective. Clin Plast Surg. 2009;36:157–65, viii.. [DOI] [PubMed] [Google Scholar]
- 6.Spear SL, Murphy DK, Slicton A, et al. ; Inamed Silicone Breast Implant U.S. Study Group. Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;120:8S–16S. [DOI] [PubMed] [Google Scholar]
- 7.Tebbetts JB, Tebbetts TB. An approach that integrates patient education and informed consent in breast augmentation. Plast Reconstr Surg. 2002;110:971–978; discussion 979. [DOI] [PubMed] [Google Scholar]
- 8.Patel AA, Joshi C, Varghese J, et al. Do websites serve our patients well? A comparative analysis of online information on cosmetic injectables. Plast Reconstr Surg. 2022;149:655e–668e. [DOI] [PubMed] [Google Scholar]
- 9.Patel AA, Mulvihill L, Jin A, et al. Websites or videos: which offer better information for patients? A comparative analysis of the quality of youtube videos and websites for cosmetic injectables. Plast Reconstr Surg. 2022;149:596–606. [DOI] [PubMed] [Google Scholar]
- 10.Montemurro P, Porcnik A, Hedén P, et al. The influence of social media and easily accessible online information on the aesthetic plastic surgery practice: literature review and our own experience. Aesthetic Plast Surg. 2015;39:270–277. [DOI] [PubMed] [Google Scholar]
- 11.Svider PF, Jiron J, Zuliani G, et al. Unattractive consequences: litigation from facial dermabrasion and chemical peels. Aesthet Surg J. 2014;34:1244–1249. [DOI] [PubMed] [Google Scholar]
- 12.Diaz JF. Review of 494 consecutive breast augmentation patients: system to improve patient outcomes and satisfaction. Plast Reconstr Surg Glob Open. 2017;5:e1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams WP, Jr, Small KH. The process of breast augmentation with special focus on patient education, patient selection and implant selection. Clin Plast Surg. 2015;42:413–426. [DOI] [PubMed] [Google Scholar]
- 14.Berry MG, Cucchiara V, Davies DM. Breast augmentation: part III—preoperative considerations and planning. J Plast Reconstr Aesthet Surg. 2011;64:1401–1409. [DOI] [PubMed] [Google Scholar]
- 15.Wan D, Rohrich RJ. Modern primary breast augmentation: best recommendations for best results. Plast Reconstr Surg. 2018;142:933e–946e. [DOI] [PubMed] [Google Scholar]
- 16.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2005;116:2005–2016. [PubMed] [Google Scholar]
- 17.Sorice SC, Li AY, Gilstrap J, et al. Social media and the plastic surgery patient. Plast Reconstr Surg. 2017;140:1047–1056. [DOI] [PubMed] [Google Scholar]
- 18.Janik PE, Charytonowicz M, Szczyt M, et al. Internet and social media as a source of information about plastic surgery: comparison between public and private sector, a 2-center study. Plast Reconstr Surg Glob Open. 2019;7:e2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gould DJ, Leland HA, Ho AL, et al. Emerging trends in social media and plastic surgery. Ann Transl Med. 2016;4:455455–4554455.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rayess H, Zuliani GF, Gupta A, et al. Critical analysis of the quality, readability, and technical aspects of online information provided for neck-lifts [published correction appears in JAMA Facial Plast Surg. 2017 Mar 1;19(2):161]. JAMA Facial Plast Surg. 2017;19:115–120. [DOI] [PubMed] [Google Scholar]
- 21.Barton N, Janis JE. Missing the mark: the state of healthcare literacy in plastic surgery. Plast Reconstr Surg Glob Open. 2020;8:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tiourin E, Barton N, Janis JE. Health literacy in plastic surgery: a scoping review. Plast Reconstr Surg Glob Open. 2022;10:e4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Powell LE, Andersen ES, Pozez AL. Assessing readability of patient education materials on breast reconstruction by major US academic hospitals as compared with nonacademic sites. Ann Plast Surg. 2021;86:610–614. [DOI] [PubMed] [Google Scholar]
- 24.Aliu O, Chung KC. Readability of ASPS and ASAPS educational web sites: an analysis of consumer impact. Plast Reconstr Surg. 2010;125:1271–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Startpage Private Search Engine. 2022. Available at http://www.startpage.com. Accessed August 20, 2022.
- 26.Readability Studio Professional Edition 2019.4, Oleander Software. 2019. Accessed August 20, 2022.
- 27.Hemingway Editor. 2021. Available at https://hemingwayapp.com. Accessed August 20, 2022.
- 28.American Medical Association. Health literacy: a manual for clinicians with contributions 2003. 2006. Available at http://lib.ncfh.org/pdfs/6617.pdf. Accessed August 20, 2022.
- 29.National Institutes of Health. Clear Communication. 2020. Available at https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/clear-simple. Accessed August 20, 2022.