Abstract
Introduction
Aging brings with an increased risk of chronic diseases among older adults, which could affect health outcomes. Evidence has showed that health literacy is associated with health outcomes. However, limited studies explore the underlying mechanism between health literacy and health outcomes. Hence, this study aimed to determine whether self-efficacy for managing chronic disease mediates the relationship between health literacy and health outcomes among older patients with chronic diseases, and to explore whether disease duration moderates the relationship between health literacy, self-efficacy for managing chronic disease, and health outcomes.
Methods
Participants were recruited from tertiary hospitals in Zhejiang Province, China from May 2019 to June 2020 using a convenience sampling method. A total of 471 older patients with chronic diseases completed questionnaires measuring demographics, disease-related information, health literacy, self-efficacy for managing chronic disease, and health outcomes. The mediation effect was examined using the structural equation model method, based on the bias-corrected bootstrapping method. The moderation effect was tested by the multiple-group analysis.
Results
A good fit model suggested that self-efficacy for managing chronic disease partially mediated the relationships between health literacy and health outcomes. In addition, disease duration moderated the relationships between health literacy, self-efficacy for managing chronic disease, and health outcomes.
Discussion
The findings highlight that adequate health literacy improved health outcomes among older patients with chronic diseases, which was further promoted by self-efficacy for managing chronic diseases. Moreover, a long disease duration could enhance the effect.
Keywords: health literacy (MeSH), self-efficacy, health outcomes, chronic disease, aged
Introduction
Chronic disease is increasingly recognized as a serious, worldwide public health concern. Every year, 41 million people die from chronic diseases, which is equivalent to 71% of all deaths globally (1). In China, the prevalence of chronic diseases is increasing. A report from a nationwide survey showed that more than 20% of people aged 18 years and above suffer from at least one chronic disease (2). More concerning, chronic diseases accounted for four-fifth of total deaths, and continue to become the predominant disease burden (3). With the aging population and the globalization of unhealthy lifestyles, older people are particularly at risk of chronic diseases. Chronic diseases tend to be of long duration, imposing physical and mental burdens on the elderly and affecting their health outcomes.
Health literacy is defined as the extent to which individuals possess the knowledge, motivation, and competencies to access, understand, appraise, and apply health information (4). Researchers have found that adequate health literacy generally contributes to improving health outcomes. For example, a meta-analysis showed that health literacy is significantly associated with better diabetes outcomes, such as glycemic control, knowledge, and self-care (5). Severaleveral studies indicated that adequate health literacy is more likely associated with greater health-related quality of life and self-rated health (6). Conversely, limited health literacy is strongly associated with worse health outcomes, which leads to a higher risk of mortality, hospitalizations, and healthcare cost (7–11). Solid evidence has confirmed that there is a significantly positive association between health literacy and health outcomes, but how and when it affects health outcomes in older adults with chronic diseases needs to be further explored. Answering these questions will help healthcare professionals conduct targeted and effective interventions to promote older patients' health outcomes.
According to Bandura's self-efficacy theory, self-efficacy is one's belief in the ability to organize and execute actions required to produce given levels of attainments (12). A high sense of self-efficacy will bring stronger intentions to complete a behavior. Specifically, patients with strong self-efficacy tend to complete health-related behaviors and ultimately get better health outcomes. In a conceptual framework for explaining health outcomes, Ussher proposed the association between health literacy, self-efficacy, and health outcomes. They predicted that individuals with higher health literacy would have stronger self-efficacy (13). A number of studies also have found a positive association between health literacy and self-efficacy (14–17). In addition, the association between self-efficacy and health outcomes has also been identified. Previous research showed that higher self-efficacy is significantly associated with better blood pressure control, glycemic control, and medication adherence (18, 19). Evidence has found support for the potential mediating role of self-efficacy on health outcomes. A study found that self-efficacy played a partial mediating effect on the relationship between medication literacy and medication adherence (20). Accordingly, we speculated that health literacy could enhance health outcomes by improving the patients' self-efficacy for managing chronic disease. Therefore, we proposed the first hypothesis: self-efficacy for managing chronic disease plays a mediating role between health literacy and health outcomes.
High health literacy may result in good health outcomes through the mediating role of self-efficacy, but not all individuals with high health literacy homogeneously experience high levels of self-efficacy and have good health outcomes. Though lack of direct evidence, indirect evidence suggested that disease duration may moderate the relationship between health literacy and health outcomes. A study found that diabetes duration was associated with diabetic health literacy (21). Patients with inadequate health literacy were attained with shorter diabetes duration. Inversely, research has shown that long disease duration was negatively related to good glycemic control among patients with type 2 diabetes mellitus (22, 23). Therefore, we proposed the second hypothesis: disease duration plays a moderating role between health literacy and health outcomes.
Disease duration may moderate not only the direct relationship between health literacy and health outcomes but also the mediating effect of self-efficacy. According to the previous evidence, disease duration was an important influencing factor for both health literacy and self-efficacy. A study on patients with hypertension showed that patients with long duration of hypertension have better medication literacy comparing those with short duration (20). Studies also found that disease duration was positively associated with self-efficacy among patients with type 2 diabetes mellitus. Patients with long disease duration had stronger self-efficacy than those with shorter duration (24, 25). In this study, we speculated that the positive association between health literacy and self-efficacy was stronger in individuals with longer disease duration and weaker in individuals with shorter disease duration. Therefore, we proposed the third hypothesis: disease duration plays a moderating role between health literacy and self-efficacy in managing chronic disease. Moreover, disease duration may also moderate the relationship between self-efficacy and health outcomes. A meta-analysis found that pain duration had a significant moderating effect on the association between self-efficacy and chronic pain outcomes (26). Additionally, the moderating effect of pain duration had a larger effect on the patients having a longer duration than those having a shorter duration. Thus, we speculated that patients with long disease duration could strengthen the positive effect of self-efficacy on health outcomes. Therefore, we proposed the fourth hypothesis: disease duration plays a moderating role between self-efficacy for managing chronic disease and health outcomes.
In summary, this study aimed to further explore the relationship between health literacy and health outcomes among older patients with chronic diseases. Specifically, it included the following: first, whether self-efficacy for managing chronic disease plays a mediating role between health literacy and health outcomes; second, whether disease duration moderates the first and second half and direct path of the mediating relationship. Our hypothesized model can be seen in Figure 1.
Figure 1.
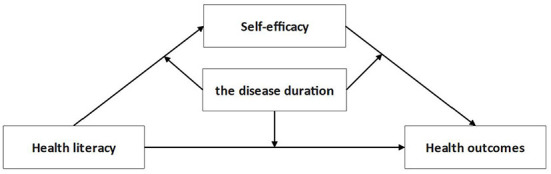
The proposed moderated mediation model.
Materials and methods
Study design and participants
A cross-sectional study was conducted in tertiary hospitals in Zhejiang Province, China, which was from May 2019 to June 2020. In this study, a total of 520 patients were recruited using the convenience sampling method. The inclusion criteria for the participants were as follows: (a) aged 60 years and older; (b) have confirmed at least one diagnosis of chronic diseases. The exclusion criteria for the participants were patients who had been diagnosed with: (a) mental disorders (e.g., Schizophrenia, Alzheimer's disease, Bipolar disorder); (b) malignancy. Before data collection, the investigators would explain the purpose of the study to patients and obtain informed consent from each patient. Then, the investigators used article questionnaires to conduct face-to-face surveys. After removing invalid questionnaires, 471 valid questionnaires were included in the analysis ultimately.
The study sample size was calculated using G*Power 3.1.9.7 with 50% effect, 5% precision, and 90% power, giving a sample size of 298. In addition, structural equation modeling was used to test the moderated mediation effect in this study. According to previous studies, structural equation modeling requires the sample size to be 10–15 times the number of variables (27). This study contained a total of 23 variables (10 demographic items, four health literacy dimensions, one self-efficacy variable, and eight health outcomes domains). Considering 10% non-responders, the final sample size was set at 256–383. The actual sample is 471 which size is satisfactory for analysis.
Measurements
The questionnaire included demographic information, disease-related information, and three scales selected according to the purpose of the study. Demographic information included age, gender, marital status, occupation before retirement, the number of children, living arrangements, education attainment, and monthly household income. Disease-related information was regarding the number of chronic diseases and disease duration. The basic information of the three scales is as follows.
Health literacy
Health literacy was measured by a health literacy scale for chronic patients. The scale was developed by Jordan et al. (28) and translated by Sun (29). It consists of 24 items about the patients' information acquisition ability, communication and interaction ability, health improvement willingness, and economic support willingness. Each item is rated on a 5-point scale from 1 (with great difficulty or reluctance) to 5 (without any difficulty or strongly willing). The total score ranges from 24 to 120, with higher scores implying greater health literacy. The scale showed acceptable internal consistency (Cronbach's α = 0.815) that was in line with prior research (Cronbach's α = 0.894) (30).
Self-efficacy for managing chronic disease
Self-efficacy for managing chronic disease was assessed by the Chinese version of the Self-efficacy for Managing Chronic Disease scale (SEMCD) (31). The scale includes six items on a 10-point scale from 1 (not at all confident) to 10 (totally confident). The score is computed as the mean of the six items. Higher scores indicate greater self-efficacy. The instrument demonstrated high reliability and validity. The Cronbach's α value of 0.938 obtained in the current study indicated acceptable internal consistency (31).
Health outcomes
Health outcomes were measured by the Chinese version of the 12-item Short-Form Health Survey (SF-12). The scale includes the following eight domains: general health, physical functioning, role-physical, bodily pain, vitality, social functioning, role-emotional, and mental health. The physical and mental health of the older persons was investigated through the physical component summary (PCS) and mental component summary (MCS) of the scale, respectively. The scores were calculated by summing items and then transforming these raw scores to a 0–100 scale using norm-based methods with a mean of 50 and a standard deviation of 10. Higher scores indicate better health. The SF-12 PCS and MCS scales demonstrated good internal consistency, with Cronbach's α ≥ 0.82 and 0.75, respectively (32). In this study, Cronbach's α coefficient of the questionnaire was 0.915.
Ethical considerations
The study was approved by the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University (KY2021-104). Before the interviews, informed consent was obtained. All participants were informed that this study was anonymous and did not pose any harm to them.
Data analysis
Data management and analysis were performed using SPSS 26.0 and AMOS 22.0. Continuous variables were described with means and standard deviation. Categorical data were presented as numbers and percentages. Participants were divided into two groups according to their disease duration, which was < 10 years. This grading standard was mainly based on the previous evidence (33). First, descriptive statistics were generated for all variables. Second, univariate analysis was undertaken to compare the differences between the two groups. Continuous data were analyzed with the independent-sample t-test or the Kruskal–Wallis test. Categorical data were performed with Chi-square for nominal distribution and the Kruskal–Wallis test for ordinal distribution as appropriate. Then, a structural equation model was carried out to determine the direct effect of health literacy on health outcomes and the role of self-efficacy in managing chronic disease as a mediator in this relationship. Given the statistically significant variables in univariate analysis, variables including age, gender, occupation, and the number of chronic diseases were taken as covariates. A bias-corrected bootstrap confidence interval was employed to test the indirect mediation effects. Next, the multiple-group analysis was used to assess the moderating effect of the disease duration. A p < 0.05 was accepted to be statistically significant.
Results
Descriptive statistics
In total, 471 participants were enrolled in this study, of whom 231 (49%) were men and 240 (51%) were women. Of the 417 participants, 219 were with disease duration of ≥10 years, and 252 were with disease duration of < 10 years. The demographic characteristics of participants are presented in Table 1. There was no difference between the two groups in the with respect to the marital status, the number of children, living arrangements, education attainment, and monthly household income of the participants. Only four demographic variables including age, gender, occupation before retirement, and the number of chronic diseases were significantly different between the two groups.
Table 1.
Descriptive statistic of the participants (N = 471).
| Classification | Total (N = 471) | Disease duration < 10 years (N = 252) | Disease duration ≥10 years (N = 219) | Test statistic | P | |
|---|---|---|---|---|---|---|
| M (SD) or N (%) | ||||||
| Age | 60–69 | 183 (38.9) | 111 (44.0) | 72 (32.9) | 12.753a | <0.001 |
| 70–79 | 195 (41.4) | 108 (42.9) | 87 (39.7) | |||
| ≥80 | 93 (19.7) | 33 (13.1) | 60 (27.4) | |||
| Gender | Male | 231 (49.0) | 108 (42.9) | 123 (56.2) | 8.303b | 0.004 |
| Female | 240 (51.0) | 144 (57.1) | 96 (43.8) | |||
| Marital status | Married | 399 (84.7) | 213 (84.5) | 186 (84.9) | 0.015b | 0.902 |
| Divorced or widowed | 72 (15.3) | 39 (15.5) | 33 (15.1) | |||
| Occupation before retirement | Self-employment | 60 (12.7) | 36 (14.3) | 24 (10.9) | 9.690b | 0.046 |
| Freelance | 42 (8.9) | 30 (11.9) | 12 (5.5) | |||
| Farmer | 216 (45.9) | 114 (45.2) | 102 (46.6) | |||
| Staff of government agencies or public sector | 84 (17.8) | 42 (16.7) | 42 (19.2) | |||
| Worker | 69 (14.7) | 30 (11.9) | 39 (17.8) | |||
| No. of children | 0–2 | 162 (34.4) | 93 (36.9) | 69 (31.5) | 1.513b | 0.219 |
| ≥3 | 309 (65.6) | 159 (63.1) | 150 (68.5) | |||
| Live alone | No | 399 (84.7) | 210 (83.3) | 189 (86.3) | 0.797b | 0.372 |
| Yes | 72 (15.3) | 42 (16.7) | 30 (13.7) | |||
| Educational attainment | None | 165 (35.0) | 75 (29.8) | 90 (41.1) | 2.112a | 0.146 |
| Primary school | 189 (40.1) | 114 (45.3) | 75 (34.2) | |||
| Middle school | 42 (8.9) | 27 (10.7) | 15 (6.9) | |||
| High school or secondary vocational school | 30 (6.4) | 18 (7.1) | 12 (5.5) | |||
| Undergraduate or junior college above | 45 (9.6) | 18 (7.1) | 27 (12.3) | |||
| Monthly household income (RMB) | ≤1,500 | 54 (11.5) | 24 (9.5) | 30 (13.7) | 0.238a | 0.625 |
| 1,501–3,000 | 168 (35.7) | 90 (35.7) | 78 (35.6) | |||
| 3,001–5,000 | 171 (36.3) | 102 (40.5) | 69 (31.5) | |||
| 5,001–10,000 | 48 (10.2) | 21 (8.3) | 27 (12.3) | |||
| >10,000 | 30 (6.4) | 15 (6.0) | 15 (6.9) | |||
| No. of chronic disease | 1 | 198 (42.0) | 135 (53.6) | 63 (28.8) | 29.586b | <0.001 |
| ≥2 | 273 (58.1) | 117 (46.4) | 156 (71.2) | |||
| Health literacy | 81.7 (22.8) | 83.6 (20.8) | 79.6 (24.7) | 1.874c | 0.062 | |
| Self-efficacy | 45.2(12.7) | 45.7 (11.5) | 44.7 (13.9) | 0.854c | 0.394 | |
| PCS | 52.5 (25.9) | 54.3 (23.2) | 50.3 (28.7) | 1.673c | 0.095 | |
| MCS | 64.1 (18.2) | 66.5 (17.2) | 61.3 (18.9) | 3.166c | 0.002 | |
PCS, physical component summary; MCS, mental component summary;
Z;
χ2;
t.
Mediation analysis
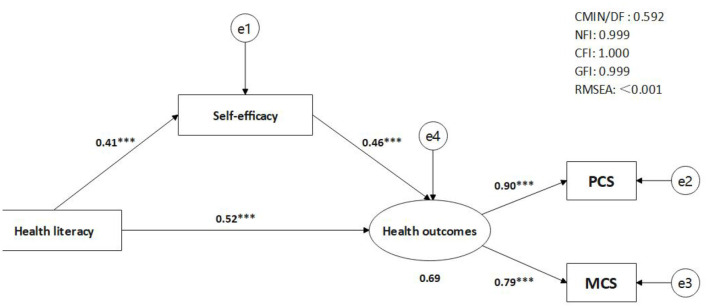
The proposed mediation model revealed a good fit to the data (χ2/df = 0.59, CFI = 1.00, NFI = 0.99, GFI = 0.99, RMSEA < 0.001, see Figure 2). Health literacy was significantly and positively associated with self-efficacy for managing chronic disease (β = 0.41, p < 0.001), and the latter was also significantly and positively associated with health outcomes (β = 0.46, p < 0.001). As expected, the direct effect of health literacy on health outcomes was significant [β = 0.52, 95% CI = (0.446, 0.591), p < 0.001]. The results of bootstrapping test revealed that self-efficacy for managing chronic disease partially mediated the relationship between health literacy and health outcomes, and the indirect effect was 0.192 [95% CI = (0.147, 0.242)]. The mediated effect accounted for 26.9% of the total effect (see Table 2).
Figure 2.
The mediation model. PCS, physical component summary; MCS, mental component summary. ***p < 0.001.
Table 2.
The mediating effect of self-efficacy on health literacy and health outcomes.
| Effect | 95% BCI | |
|---|---|---|
| Direct effect | 0.522*** | 0.446–0.591 |
| Indirect effect | 0.192*** | 0.147–0.242 |
| Total effect | 0.714*** | 0.655–0.808 |
BCI, Bootstrapped confidence interval;
p < 0.001.
Moderated mediation analysis
The results showed that the moderated mediation model fit the data well (see Appendix A). Disease duration moderated the above mediation model (see Table 3, Appendix B). The results revealed that disease duration moderated the direct effect of health literacy on health outcomes. The path from health literacy to health outcomes was significantly stronger among the participants with disease duration ≥10 years [β = 0.551, 95% BCI = (0.473, 0.625)] than those with disease duration < 10 years [β = 0.496, 95% BCI = (0.379, 0.601)] (Δχ2/df = 31.919, Δdf = 9, p < 0.001). Besides, the results confirmed our hypothesis explaining that disease duration moderated the association between health literacy and self-efficacy for managing chronic disease (β = 0.475, p < 0.001 for disease duration ≥10 years vs. β = 0.336, p < 0.001 for disease duration < 10 years), as well as the path between self-efficacy for managing chronic disease and health outcome (β = 0.490, p < 0.001 for disease duration ≥10 years vs. β = 0.401, p < 0.001 for disease duration < 10 years). It illustrated the indirect effect of health literacy on health outcomes was more obvious in individuals with a duration of ≥10 years.
Table 3.
The moderating effect of disease duration.
| Dependent variable | Independent variable | Disease duration<10 years | Disease duration ≥10 years | ||
|---|---|---|---|---|---|
| β | 95% BCI | β | 95% BCI | ||
| Self-efficacy | Health literacy | 0.336 | 0.223–0.447 | 0.475 | 0.357–0.571 |
| Health outcomes | Self-efficacy | 0.401 | 0.255–0.524 | 0.490 | 0.390–0.588 |
| Health outcomes | Health literacy | 0.496 | 0.379–0.601 | 0.551 | 0.473–0.625 |
Discussion
This study revealed that health literacy was significantly and positively associated with health outcomes among older patients with chronic diseases. This finding was consistent with previous research results (5, 6). The results further indicated that self-efficacy for managing chronic disease played a mediation role between health literacy and health outcomes, which verified the first hypothesis. Moreover, it verified the conceptual framework of mechanisms linking health literacy to health outcomes. The framework considers that individuals with higher health literacy would have stronger self-efficacy and could obtain better health outcomes. Bandura believed that self-efficacy is an important determinant of intention and behaviors (12). When patients are convinced that they were capable of managing their own diseases, they would have a high sense of self-efficacy to participate in disease management activities, which would affect both physical and mental health (18, 19). In other words, older patients who experience strong self-efficacy for managing chronic diseases are more likely to perform health behaviors using their health-related knowledge. Thus, with an increase in health literacy, the older would be more confident in managing their health-related behaviors, which would affect health outcomes including physical and mental. This study confirmed that health literacy could affect health outcomes by strengthening the self-efficacy of older adults for managing chronic diseases. Therefore, healthcare professionals should enhance older adults' self-efficacy for managing chronic diseases and help them equip with adequate health literacy to achieve better physical and mental health through self-managing behaviors.
This study found that disease duration moderated the relationship between health literacy and health outcomes, and the first and second half of the mediating effect of self-efficacy for managing chronic disease. Thus, the results supported the previous hypothesis. As known, chronic diseases tend to be of long duration and people with chronic diseases need long-term care. Previous evidence showed that the disease duration could influence chronic disease management (34). First, in this study, the positive relationship between health literacy and health outcomes was more significant in patients with long disease duration. The results revealed that disease duration played a positive role at this time, which was in line with previous results (23, 35). This could be because patients with long disease duration might increase the probability of health-related stimulus to strengthen the positive relationship between health literacy and health outcomes. Therefore, these results supported the second hypothesis. Second, the results demonstrated that disease duration had a significant moderating effect on the relationship between health literacy and self-efficacy for managing chronic disease. In individuals with long disease duration, the promoting effect on self-efficacy for managing chronic disease was more evident with an increased health literacy. That is, patients with long disease duration might be exposed to more health-related knowledge and have more opportunities to put it into practice. With more successful experience, patients would experience more confidence in self-management. So the long disease duration played a positive effect on the relationship between health literacy and self-efficacy for managing chronic disease. Therefore, the third hypothesis was verified. Finally, the result indicated that disease duration plays a moderating role in self-efficacy for managing chronic disease and health outcomes. In this study, the impact of self-efficacy for managing the chronic disease on health outcomes in the long duration patients is more significant than those with short duration. The possible reason was that patients with long disease duration had more successful experience in self-management and maintaining calmness to cope with their diseases.
This study explored the relationship between self-efficacy for managing chronic disease and disease duration in health literacy and health outcomes. The study validated the mediation model, emphasizing the mediating effect of self-efficacy for managing chronic disease between health literacy and health outcomes among older patients with chronic disease. The mediation-moderated model proposed suggested that disease duration also affects the health outcomes of patients. The research enriches previous results and provides guidance for healthcare professionals. to improve older patients' health outcomes. Professionals could conduct self-efficacy-oriented inventions (e.g., peer support groups) interventions to enhance older adults' self-efficacy. Moreover, we recommend that professionals could consider the disease duration in patients when conducting interventions. We should strengthen the evaluation of health literacy and self-efficacy among the older with chronic diseases, especially those with short disease duration.
Limitations
The findings in this study are subject to three limitations. First, it is a cross-sectional design that could not reveal the causes and effects of the relationship. Second, this study used a convenience sample from four hospitals in Zhejiang which limits generalizability. Third, the study just tested single mediating and moderating variables. Accordingly, longitudinal studies could be conducted in the future. In addition, future research could use a larger random sample. Furthermore, it will be important to explore the multiple moderating roles on health outcomes among older adults with chronic diseases, such as socioeconomic status.
Conclusion
In conclusion, this study found that health literacy had a significantly positive association with health outcomes among older patients with chronic disease; self-efficacy for managing chronic disease mediated the relationship between health literacy and health outcomes; disease duration moderated the direct relationship between health literacy and health outcomes, as well as the second half of the mediating effect of self-efficacy for managing chronic disease.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
JL: data collection, data interpretation, and manuscript drafting. SS and YG: data collection and data interpretation. HL: data collection and data analysis. LF: data collection. XZ: study design and manuscript reviewing. HX: study design, conceptual interpretation, and manuscript reviewing. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors want to express sincere gratitude to all the participants.
Funding Statement
This study was supported by the Science and Technology Plan Project of Wenzhou (Grant Number Y20220105), the General Scientific Research Foundation of the Education Department of Zhejiang Province (Grant Number Y202250198), and the Natural Science Foundation of Zhejiang Province (Grant Number LGF20H250003).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Appendix A
Table A1.
The multiple group analysis.
| CMIN | DF | CMIN/DF | NFI | CFI | GFI | RMSEA | |
|---|---|---|---|---|---|---|---|
| Unconstrained model | 11.457 | 2 | 5.728 | 0.986 | 0.989 | 0.988 | 0.100 |
| Measurement weight model | 15.593 | 3 | 5.198 | 0.981 | 0.985 | 0.984 | 0.095 |
| Structural weight model | 27.217 | 6 | 4.536 | 0.968 | 0.974 | 0.973 | 0.087 |
| Structural covariance model | 33.810 | 7 | 4.830 | 0.960 | 0.968 | 0.966 | 0.09 |
| Structural association error model | 40.426 | 9 | 4.492 | 0.952 | 0.962 | 0.959 | 0.086 |
| Measurement error model | 43.376 | 11 | 3.943 | 0.948 | 0.961 | 0.956 | 0.079 |
Appendix B
Table B1.
Model difference test.
| Δ-CMIN | Δ-DF | P | Δ-NFI | Δ-CFI | Δ-GFI | |
|---|---|---|---|---|---|---|
| Measurement weight model | 4.136 | 1 | 0.042 | –0.005 | –0.004 | –0.004 |
| Structural weight model | 15.760 | 4 | 0.003 | –0.018 | –0.015 | –0.015 |
| Structural covariance model | 22.353 | 5 | <0.001 | –0.026 | –0.021 | –0.022 |
| Structural association error model | 28.969 | 7 | <0.001 | –0.034 | –0.027 | –0.029 |
| Measurement error model | 31.919 | 9 | <0.001 | –0.038 | –0.028 | –0.032 |
References
- 1.World Health Organization . Noncommunicable Diseases. WHO (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed October 11, 2022).
- 2.China's State Council . The State Council Information Office Held a Press Conference on the “Report on Nutrition Chronic Disease Status of Chinese Residents 2020.” China's State Council (2020). Available online at: http://www.gov.cn/xinwen/2020-12/24/content_5572983.htm (accessed October 11, 2022).
- 3.Chinese Center for Disease Control and Prevention . Chinese National Death Cause Surveillance Dataset. Beijing: Science and Technology of China Press; (2020). [Google Scholar]
- 4.Sørensen K, Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marciano L, Camerini AL, Schulz PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med. (2019) 34:1007–17. 10.1007/s11606-019-04832-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marques S, Escarce AG, Lemos S, Marques S, Escarce AG, Lemos S. Health literacy and self-rated health in adults primary care patients. Codas. (2018) 30:e20170127. 10.1590/2317-1782/20182017127 [DOI] [PubMed] [Google Scholar]
- 7.Fabbri M, Yost K, Rutten LF, Manemann SM, Boyd CM, Jensen D, et al. Health literacy and outcomes in patients with heart failure: a prospective community study. Mayo Clin Proc. (2018) 93:9–15. 10.1016/j.mayocp.2017.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mcnaughton C, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. (2015) 4:e001799. 10.1161/JAHA.115.001799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan P, Allen LA, et al. Health literacy and outcomes among patients with heart failure. JAMA. (2011) 305:1695–701. 10.1001/jama.2011.512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palumbo R. Examining the impacts of health literacy on healthcare costs. An evidence synthesis. Health Serv Manage Res. (2017) 30:197–212. 10.1177/0951484817733366 [DOI] [PubMed] [Google Scholar]
- 11.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 12.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1997) 84:191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 13.Ussher M, Ibrahim S, Reid F, Shaw A, Gillian R. Psychosocial correlates of health literacy among older patients with coronary heart disease. J Health Commun. (2010) 15:788–804. 10.1080/10810730.2010.514030 [DOI] [PubMed] [Google Scholar]
- 14.Zuercher E, Diatta ID, Burnand B, Peytremann-Bridevaux I. Health literacy and quality of care of patients with diabetes: a cross-sectional analysis. Prim Care Diabetes. (2017) 11:233–40. 10.1016/j.pcd.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 15.Ishikawa H, Yano E. The relationship of patient participation and diabetes outcomes for patients with high vs. low health literacy. Patient Educ Couns. (2011) 84:393–7. 10.1016/j.pec.2011.01.029 [DOI] [PubMed] [Google Scholar]
- 16.Bohanny W, Wu SF, Liu CY, Yeh SH, Tsay SL, Wang TJ. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Pract. (2013) 25:495–502. 10.1111/1745-7599.12017 [DOI] [PubMed] [Google Scholar]
- 17.Le YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Pat Educ Counsel. (2016) 99:287–94. 10.1016/j.pec.2015.08.021 [DOI] [PubMed] [Google Scholar]
- 18.Ghadiri R, Alimohammadi M, Majdabadi HA. Determination of the psychometric properties of the patients' self-efficacy scale in blood pressure patients. Interv Med Appl Sci. (2018) 10:87–94. 10.1556/1646.10.2018.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ji M, Ren D, Dunbar-Jacob J, Gary-Webb TL, Erlen JA. Correlates of self-management behaviors, glycemic control and metabolic syndrome in patients with type 2 diabetes. Nurs Res. (2019) 69:e9–17. 10.1097/NNR.0000000000000401 [DOI] [PubMed] [Google Scholar]
- 20.Shen Z, Shi S, Ding S, Zhong Z. Mediating effect of self-efficacy on the relationship between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. (2020) 11:569092. 10.3389/fphar.2020.569092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashim SA, Barakatun-Nisak MY, Abu Saad H, Ismail S, Hamdy O, Mansour AA. Association of health literacy and nutritional status assessment with glycemic control in adults with type 2 diabetes mellitus. Nutrients. (2020) 12:3152. 10.3390/nu12103152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radwan M, Elsous A, Al-Sharif H, Mustafa AA. Glycemic control among primary care patients with type 2 diabetes mellitus in the gaza strip, palestine. Ther Adv Endocrinol Metab. (2018) 9:3–14. 10.1177/2042018817742070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Souza JG, Apolinario D, Magaldi RM, Busse AL, Campora F, Jacob-Filho W. Functional health literacy and glycaemic control in older adults with type 2 diabetes: a cross-sectional study. BMJ Open. (2014) 4:e004180. 10.1136/bmjopen-2013-004180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D'Souza MS, Karkada SN, Parahoo K, Venkatesaperumal R, Achora S, Cayaban ARR. Self-efficacy and self-care behaviours among adults with type 2 diabetes. Appl Nurs Res. (2017) 36:25–32. 10.1016/j.apnr.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 25.Tharek Z, Ramli AS, Whitford DL, Imail Z, Mohd Zulkifli M, Sharoni SKA, et al. Relationship between self-efficacy, self-care behaviour and glycaemic control among patients with type 2 diabetes mellitus in the Malaysian primary care setting. BMC Fam Pract. (2018) 19:39. 10.1186/s12875-018-0725-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson T, Wang YL, Wang Yang, Fan HY. Self-efficacy and chronic pain outcomes: a meta-analytic review. J Pain. (2014) 15:800–14. 10.1016/j.jpain.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 27.Thompson B. Ten commandments of structural equation modeling. In:Grimm LG, Yarnold PR, editors. Reading and Understanding More Multivariate Statistics. Washington, DC: American Psychological Association; (2000). [Google Scholar]
- 28.Jordan JE, Buchbinder R, Osborne RH. Conceptualising health literacy from the patient perspective. Patient Educ Couns. (2010) 79:36–42. 10.1016/j.pec.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 29.Sun H. Development and preliminary application of scale on health literacy for patients with chronic disease. (Master's thesis), Fudan University, Shanghai (China) (2012). [Google Scholar]
- 30.Sun H, Peng H, Fu H. The reliability and consistency of health literacy scale for chronic patients. Fudan Univ J Med Sci. (2012) 39:268–72. 10.3969/j.issn.1672-8467.2012.03.009 [DOI] [Google Scholar]
- 31.Ritter PL, Lorig K. The English and Spanish self-efficacy to manage chronic disease scale measures were validated using multiple studies. J Clin Epidemiol. (2014) 67:1265–73. 10.1016/j.jclinepi.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 32.Busija L, Ackerman IN, Haas R, Wallis J, Buchbinder R. Adult measures of general health and health related quality of life. Arthritis Care Res. (2020) 72:522–64. 10.1002/acr.24216 [DOI] [PubMed] [Google Scholar]
- 33.Kong L. Clinical analysis of complication of senile diabetic: a report of 150 cases. Chin J Gen Pract. (2012) 10:847–9. 10.16766/j.cnki.issn.1674-4152.2012.06.050 [DOI] [Google Scholar]
- 34.Qu Z, Parry M, Liu F, Wen X, Li J, Zhang Y, et al. Self-management and blood pressure control in China: a community-based multicentre cross-setional study. BMJ Open. (2019) 9:e025819. 10.1136/bmjopen-2018-025819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salim H, Ghazali SS, Lee PY, Cheong AT, Pinnock H. Health literacy levels and its determinants among people with asthma in Malaysian primary healthcare settings: a cross-sectional study. BMC Public Health. (2021) 21:1186. 10.1186/s12889-021-11194-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.