Abstract
Emerging data suggest that few veterans are initiating prolonged exposure (PE) and cognitive processing therapy (CPT) and dropout levels are high among those who do start the therapies. The goal of this study was to use a large sample of veterans seen in routine clinical care to 1) report the percent of eligible and referred veterans who (a) initiated PE/CPT, (b) dropped out of PE/CPT, (c) were early PE/CPT dropouts, 2) examine predictors of PE/CPT initiation, and 3) examine predictors of early and late PE/CPT dropout. We extracted data from the medical records of 427 veterans who were offered PE/CPT following an intake at a Veterans Health Administration (VHA) PTSD Clinical Team. Eighty-two percent (n = 351) of veterans initiated treatment by attending Session 1 of PE/CPT; among those veterans, 38.5% (n = 135) dropped out of treatment. About one quarter of veterans who dropped out were categorized as early dropouts (dropout before Session 3). No significant predictors of initiation were identified. Age was a significant predictor of treatment dropout; younger veterans were more likely to drop out of treatment than older veterans. Therapy type was also a significant predictor of dropout; veterans receiving PE were more likely to drop out late than veterans receiving CPT. Findings demonstrate that dropout from PE/CPT is a serious problem and highlight the need for additional research that can guide the development of interventions to improve PE/CPT engagement and adherence.
Keywords: evidence-based practice, patient adherence, posttraumatic, stress disorders, veterans
Posttraumatic stress disorder (PTSD) is a prevalent, debilitating, and costly condition (Hermes, Rosenheck, Desai, & Fontana, 2012; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Schnurr, Hayes, Lunney, McFall, & Uddo, 2006). The lifetime prevalence of PTSD among Vietnam veterans is 17%, and the postdeployment prevalence among Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF)/Operation New Dawn (OND) combat veterans is estimated to be 13% (Dohrenwend et al., 2006; Kok, Herrell, Thomas, & Hoge, 2012). Left untreated, PTSD fails to remit in one third of cases (Kessler et al., 1995); fortunately, efficacious treatments for PTSD exist. Prolonged exposure (PE) and cognitive processing therapy (CPT) have larger evidence bases than any other treatments for PTSD and are considered preferred first-line therapies in the VHA and Department of Defense PTSD Clinical Practice Guidelines (Veterans Health Administration & Department of Defense, 2010). PE and CPT result in large reductions in PTSD and associated symptoms across a wide range of veteran populations (Chard, Schumm, Owens, & Cottingham, 2010; Monson et al., 2006; Schnurr et al., 2007; Suris, Link-Malcolm, Chard, Ahn, & North, 2013; Thorp, Stein, Jeste, Patterson, & Wetherell, 2012; Tuerk, Yoder, Ruggiero, Gros, & Acierno, 2010). Further, completion of PE/CPT has a positive impact on physical health, functioning, health care utilization, and PTSD-related health care costs (Meyers et al., 2013; Rauch et al., 2009; Tuerk et al., 2013). Given the strength of evidence for these treatments, VHA mandated that either CPT or PE be available to all veterans with PTSD (U.S. Department of Veterans Affairs, 2008). To achieve this goal, VHA launched the Mental Health Dissemination Initiative to train their workforce to administer the treatments and implemented system-level changes (e.g., modified scheduling procedures to accommodate 90-min sessions) to encourage implementation (Karlin et al., 2010). Yet, emerging data suggest that few veterans with PTSD initiate PE/CPT, and those who do often complete an insufficient number of sessions (Shiner et al., 2013).
It is unclear how many veterans who are offered PE/CPT chose to initiate treatment. Two studies using retrospective clinic data examined this issue (Chard et al., 2010; Mott, Mondragon, et al., 2014). Mott and colleagues found that only 11.4% of veterans who attended an individual psychotherapy session with a PE/CPT trained provider initiated PE/CPT; however, the number of veterans who were offered one of the treatments and did not initiate (as opposed to those who were not offered PE/CPT) was not reported. Conversely, Chard et al. found that 94% of veterans who attended a screening and were offered CPT chose to initiate the treatment. The data are more consistent in demonstrating that among those who initiate the treatments, dropout is common. Three clinic-based studies of PE demonstrated that 31% to 44% of veterans dropped out of treatment (Gros, Yoder, Tuerk, Lozano, & Acierno, 2011; Jeffreys et al., 2014; Mott, Mondragon, et al., 2014); further, 28% of veterans who received PE through the Mental Health Dissemination Initiative did not receive an adequate dose of treatment (i.e., fewer than eight sessions; Eftekhari et al., 2013). Four VHA clinic-based studies of CPT with veterans yielded dropout rates of 31% to 50% (Chard et al., 2010; Davis, Walter, Chard, Parkinson, & Houston, 2013; Jeffreys et al., 2014; Mott, Mondragon, et al., 2014). However, conclusions regarding the specific rate of dropout from PE/CPT in VHA clinical care must be tempered given that the majority of existing studies have relied on small or unique samples (e.g., veterans who received PE during clinicians’ supervised training period) and have used differing definitions of dropout.
Little is known about why so few veterans initiate and complete PE/CPT. The recent study by Mott, Mondragon, et al. (2014) described above is the only published report that examined differences between veterans who did and did not initiate PE/CPT. Although a number of demographic, disease-related (e.g., diagnosis of PTSD), and utilization variables (e.g., history of group psychotherapy) were associated with initiation in bivariate analyses, only service era and service connection emerged as significant predictors of initiation in the competitive model. Specifically, OEF/OIF/OND veterans and those without PTSD service connection were significantly less likely to initiate PE/CPT than veterans from other eras and those who were service connected for PTSD. However, as noted above, the noninitiator group was a mix of veterans who were not offered PE/CPT by their therapists and veterans who declined the treatment, thereby limiting the conclusions the can be drawn regarding characteristics of veterans who chose to initiate. Many studies have examined predictors of dropout from PE/CPT; however, consistent associations have failed to emerge. Approximately one third of such studies failed to find any significant predictors (Chard et al., 2010; Taylor, 2003; van Minnen & Hagenaars, 2002; Zoellner, Feeny, Fitzgibbons, & Foa, 1999). Demographic variables such as age, gender, race/ethnicity, level of education, marital status, and service-connected disability status were most often examined (Chard et al., 2010; Garcia, Kelley, Rentz, & Lee, 2011; Gros et al., 2011; Jeffreys et al., 2014; Mott, Mondragon, et al., 2014; Rizvi, Vogt, & Resick, 2009; Taylor, 2003; van Minnen, Arntz, & Keijsers, 2002; Zoellner et al., 1999). Younger age is the only demographic variable that predicted dropout in more than one trial (Garcia et al., 2011; Gros et al., 2011; Jeffreys et al., 2014; Rizvi et al., 2009). Affective variables, such as total PTSD symptomology, PTSD symptom clusters, depression, and other comorbid conditions were also evaluated (Chard et al., 2010; Garcia et al., 2011; Gros et al., 2011; Mott, Mondragon, et al., 2014; Rizvi et al., 2009; Taylor, 2003; van Minnen & Hagenaars, 2002; van Minnen et al., 2002; Zayfert et al., 2005; Zoellner et al., 1999). The results were equivocal; some trials reported increased rates of PTSD symptomology, particularly avoidance symptoms, and elevated symptoms of depression were associated with dropout, whereas others failed to find an association. The difficulty in identifying consistent predictors may be attributable to the relatively small sample sizes used in many prior studies, which left studies underpowered to detect differences.
Finally, several investigators have examined when during the course of PE/CPT veterans are most likely to drop out of treatment. Mott, Mondragon, et al. (2014) reported that veterans receiving PE were most likely to drop out after completing two sessions; Garcia and colleagues (2011) found that all veterans who dropped out of PE did so before session four. Approximately two thirds of veterans who received CPT in a clinic-based study dropped out before session four (Davis et al., 2013); similarly, Mott et al. found that veterans receiving CPT most often dropped out after session three. These findings suggest that many, if not most, veterans who drop out do so early in the course of treatment, before engaging in the active components of PE/CPT (exposure to trauma-specific content and challenging of trauma-related thoughts). To date, no studies have examined predictors of early versus later dropout from PE/CPT. Such a comparison may improve our understanding of the reasons that veterans drop out of these therapies.
The goal of this study was to use a large sample of veterans seen in routine clinical care to 1) report the percent of eligible and referred veterans who (a) initiated PE/CPT, (b) dropped out of PE/CPT, (c) were early PE/CPT dropouts (before Session 3), 2) examine predictors of PE/CPT initiation, 3) examine predictors of early and late PE/CPT dropout. Given the limited and often mixed findings regarding PE/CPT initiation and dropout as reviewed above, these aims were considered to be exploratory.
Method
Participants and Procedure
We examined initiation and dropout from PE/CPT within an outpatient VHA PTSD Clinical Team (PCT) from January 2010 to December 2012. We used an administrative database maintained by the PCT to identify the sample; all veterans referred for PE/CPT during the study time period were tracked in the database. Veterans who were referred but did not attend an initial assessment of their eligibility for and interest in PE/CPT (Session 0) were excluded, as were those who were deemed inappropriate for PE/CPT during this assessment. Outcome variables, demographic characteristics, and pretreatment symptomology were extracted through review of PE/CPT progress notes in the electronic medical record (EMR). All procedures were approved by the local Institutional Review Board.
Referral and assessment process.
Referrals for PE/CPT were made by veterans’ treating mental health providers. There were no specific criteria for referral other than suspicion of full or subthreshold PTSD and an interest in weekly psychotherapy for PTSD. Following referral, the PCT program manager conducted a chart review; if ongoing substance dependence, current high levels of suicidality or frequent self harm, current psychotic symptoms, or a recent evaluation showing a lack of PTSD symptoms were noted in the chart, the referral was not accepted. Following the chart review, veterans were assigned a therapist and scheduled to undergo an intake to determine eligibility (Session 0) that included assessment of PTSD symptomology and treatment contraindications (substance dependence, high levels of suicidality/self harm, psychosis). The therapist had discretion as to whether or not to offer PE/CPT as a treatment option. We reviewed the charts of 512 veterans who attended Session 0; 85 veterans (16.6%) were not offered a course of PE/CPT. The most common reason for exclusion (49.4% of those excluded) was a lack of PTSD symptoms, particularly reexperiencing and avoidance symptoms. An additional 9.4% of veterans were excluded because of substance dependence, 4.7% because of high levels of suicidal ideation or self-injurious behavior, and 3.5% because of current psychotic symptoms.
Delivery of PE/CPT.
If the therapist determined that PE/CPT was an appropriate treatment, they provided a brief overview of the treatment rationale and anticipated course of treatment. The treatment offered (PE vs. CPT) was typically determined by which treatment the therapist was trained to deliver. Within the PCT, adherence to the treatment manuals was encouraged, although flexibility in number of sessions was allowed (e.g., early responders did not need to complete all sessions). The primary components of PE are in vivo exposure (real-life exposure to avoided trauma-related triggers) and imaginal exposure (exposure to the trauma memory; Foa, Hembree, & Rothbaum, 2007). PE was delivered in 90-min individual weekly sessions and was expected to last 10 to 12 sessions, although therapists and veterans mutually decided when to end treatment based on habituation to the trauma memory (or memories) and progression through the in vivo hierarchy. The CPT protocol outlines a 12-session treatment that consists of writing a statement about the impact of the trauma on one’s life, writing and reading an account of one’s trauma, and the identification, evaluation, and modification of trauma-related cognitions (Resick, Monson, & Chard, 2006). CPT-C was not offered in the clinic. CPT was most often delivered in individual 60-min weekly sessions, although a minority of veterans received the combined group/individual format (7.7% of those who received CPT). Those who received the group/individual format attended one 60-min individual and one 90-min group session per week; the individual and group sessions were typically delivered on the same day.
Clinicians.
PE and CPT were delivered by clinicians from a variety of disciplines (psychologists, social workers, psychiatrists, and nurses) and psychology and social work trainees. All therapists received VHA roll-out or roll-out equivalent (e.g., local training conducted by certified trainers) didactic training. All veterans who received PE/CPT during the study time frame were included in our sample, including those seen as practice cases by clinicians who were working toward completing the training requirements.
Measures
Outcome variables.
We extracted data regarding treatment initiation and dropout from the EMR. The PCT used templated progress notes for PE/CPT, which eased data extraction and ensured that session notes were well labeled. Veterans were considered treatment initiators if they completed Session 1 of either PE/CPT. If a veteran either no-showed or presented to the session and told their therapist they did not want to participate in PE/CPT, they were coded as noninitiators. Veterans were characterized as dropouts if they did not complete the final session of PE or CPT as outlined in the respective treatment manual (e.g., no final session note) and there was not a note by the provider stating that PE/CPT was no longer an appropriate or needed treatment, regardless of the number of sessions completed. Veterans did not need to attend a certain number of sessions to be classified as completers, but they must have had a final session note. Final PE sessions involved discussing current levels of distress related to items on the in vivo hierarchy, conducting the final imaginal exposure, reviewing the course of treatment, and planning related to relapse prevention. Final CPT sessions involved identifying and challenging thoughts related to intimacy, reading and discussing the rewritten impact statement, reviewing treatment, and identifying goals for the future. We also extracted the number of PE/CPT sessions that each veteran attended. When calculating number of sessions attended for those in the combined individual/Group CPT format, veterans were credited with attending one session if they attended any portion of the week’s session (group only, individual only, or both). Sessions that occurred during the course of the treatment but did not include PE/CPT content were not included in the count. Finally, we characterized veterans as early dropouts if they dropped out before session three of PE/CPT; late dropout was operationalized as termination after session three but before completion.
Predictor variables.
We extracted the demographic variables of gender, age, and military service era from the EMR. We also recorded whether the veteran was seen in person or via telemedicine, the therapist who delivered the treatment, and which treatment (PE or CPT) the therapist recommended (for Veterans who did not initiate treatment) or provided (for Veterans who initiated treatment). Finally, when available embedded in patient notes, we obtained pretreatment PTSD Checklist (PCL; n = 354) scores as an index of the severity of PTSD symptoms from the Session 0 or Session 1 progress note (Weathers, Litz, Herman, Huska, & Keane, 1993).
Data extraction.
Data were extracted from the charts by the lead author (S.K.F.), a project coordinator with knowledge of PE/CPT and familiarity with EMRs, and a clinician with roll-out training in both PE and CPT. To evaluate the reliability of the data extraction, 10% of included cases (n = 43) were independently coded by a second rater; Cohen’s kappa (κ) and intraclass correlation coefficients (ICC) were calculated as measures of interrater reliability. The interrater reliability was excellent (κ = 0.88–0.95; ICC = 0.99–1.00).
Data Analysis
We calculated the proportion of veterans who were referred and deemed appropriate for PE/CPT, who initiated treatment. We then calculated the proportion of treatment initiators who dropped out of treatment and the percent of early dropouts. Because veterans were nested within therapists (e.g., multiple veterans were treated by the same therapist), we calculated ICCs to examine correlations in outcomes among veterans treated by the same therapist. Low and non-significant ICCs indicate that it is not necessary to treat the data as nested (e.g., therapist does not need to be included in models). For the main analyses, we first conducted a binary logistic regression to examine the association between the predictor variables and treatment initiation. The fit of the final model was evaluated using the Hosmer-and-Lemeshow goodness-of-fit statistic, for which a good model fit is evidenced by a low chi-square statistic and a high p value (Hosmer & Lemeshow, 2000). We then conducted a multinomial logistic regression to evaluate how the predictor variables were related to dropout status (early dropout, late dropout, completer) among veterans who initiated treatment. As multinomial regression compares each group to a single reference group, two multinomial regressions were performed to allow for comparisons across all dropout categories. Specifically, the model was first run with “completer” as the reference group, then rerun with “late dropout” as the reference group. The fit of the model was assessed using the deviance goodness-of-fit test, in which a high p value reflects a good model fit. Predictor variables were entered in one block for both regressions. For entry in the regression models, we categorized PCL score and age. A median split was used to dichotomize PCL scores into high and low PTSD symptomology; age was grouped into three categories (under 35 years, 35 to 54 years, and 55 years and over). Age and service era could not be simultaneously entered into the regression models due to problems with multicollinearity. Thus, the models were run twice: once with age and once with service era. The models that used age as a predictor are presented. The pattern of findings did not differ when the models were run using service era; odds ratios (ORs) are presented for the service era categories found to be significant predictors in the service era models. Participants without complete data were excluded from both regressions. All analyses were conducted using SPSS Version 19.
Results
The sample consisted of 427 veterans; see Table 1 for sample characteristics. The veterans were seen by 72 unique therapists, each of whom treated an average of 5.93 (SD = 11.37) veterans (range = 1–77). PCL scores were (M = 62.31, SD = 10.58) similar to those observed in other samples of veterans initiating PE and CPT (e.g., Eftekhari et al., 2013; Chard et al., 2010). Veterans who were seen via telemedicine were significantly more likely to be offered CPT than PE, χ2(1, N = 419) = 15.88, p < .001; therapy type was not significantly associated with age, service era, gender, or pretreatment PCL.
Table 1.
Sample Characteristics and Rates of Treatment Initiation and Dropout by Predictor Variables
| Total |
Treatment initiators |
Treatment dropouts among initiators |
||||
|---|---|---|---|---|---|---|
| Variable | N or M | % or SD | n or M | % or SD | n or M | % or SD |
| Telemedicine (N, %) | ||||||
| No | 348 | 81.5 | 293 | 84.5 | 116 | 40.0 |
| Yes | 79 | 18.5 | 58 | 73.4 | 19 | 32.8 |
| Gender (N, %) | ||||||
| Male | 359 | 84.1 | 291 | 81.1 | 111 | 38.1 |
| Female | 68 | 15.9 | 60 | 88.2 | 24 | 40.0 |
| Therapy (N, %) | ||||||
| CPT | 231 | 54.1 | 195 | 84.4 | 65 | 33.3 |
| PE | 188 | 44.0 | 156 | 82.9 | 70 | 44.9 |
| Era (N, %) | ||||||
| OEF/OIF/OND | 186 | 43.6 | 150 | 80.6 | 76 | 50.7 |
| Gulf War I/Post-Vietnam | 87 | 20.4 | 72 | 82.8 | 26 | 36.1 |
| Vietnam | 154 | 36.1 | 129 | 83.8 | 33 | 25.5 |
| PCL (M, SD) | 62.31 | 10.58 | 62.28 | 10.54 | 62.56 | 10.68 |
| Age (M, SD) | 46.39 | 14.56 | 46.62 | 14.58 | 42.67 | 14.42 |
Note. Data regarding therapy type was not available for eight veterans who did not initiate treatment. OEF/OIF/OND = Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn; CPT = cognitive processing therapy; PE = prolonged exposure.
Rates of Treatment Initiation and Dropout
Of the 427 veterans who attended Session 0 of PE/CPT and were evaluated as appropriate for the treatment, 82.2% (n = 351) initiated treatment by attending Session 1. Veterans attended an average of 8.87 (SD = 4.40) sessions; veterans who received PE attended an average of 8.11 (SD = 4.82) sessions, while those who received CPT attended an average of 9.49 (SD = 3.99) sessions. Of the 351 veterans who initiated PE/CPT, 38.5% (n = 135) dropped out of treatment. Thus, only 50.6% (n = 216) of veterans who attended Session 0 and were appropriate for PE/CPT completed treatment. The mean number of sessions attended by veterans who dropped out was 4.47 (SD = 3.06). Of those who dropped out, 25.9% (n = 35) did so before Session 3. Veterans who dropout out early completed an average of 1.29 (SD = 0.80) sessions, whereas those who dropped out late attended 5.70 (SD = 2.74) sessions. The mean number of sessions attended by treatment completers was 11.71 (SD = 2.52; range = 5–25). See Figure 1 for the percent of veterans who dropped out of PE/CPT at each treatment session.
Figure 1.
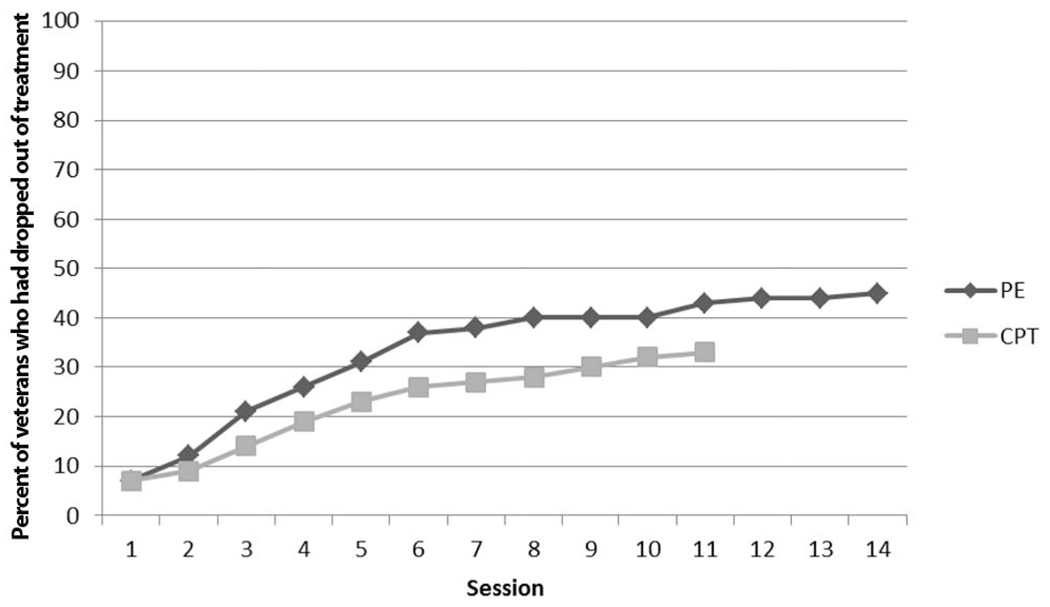
Percent of veterans who had dropped out of prolonged exposure and cognitive processing therapy following each treatment session. PE = prolonged exposure; CPT = cognitive processing therapy.
Predictors of Treatment Initiation
We examined the relative contribution of demographic variables (age, gender), pretreatment PTSD symptom severity, type of therapy, and location of therapy (telemedicine) in the prediction of treatment initiation (see Table 2). Therapist assignment did not account for a significant amount of variance (ICC = 0.04, p = .099), indicating that it was not necessary to include therapist as a nesting variable within the regression model. The Hosmer and Lemeshow test indicated that the model was a good fit for the data, χ2(8, N = 334) = 4.14, p = .844. There were no significant predictors of PE/CPT initiation. There was a trend suggesting that veterans aged 35–54 years initiated at a lower rate than veterans 55 years and older. When service era, rather than age, was included in the model, there was a trend for OEF/OIF/OND veterans to be less likely to initiate treatment than Vietnam veterans (OR = 0.42, p = .50).
Table 2.
Binary Logistic Regression of Predictors of Prolonged Exposure and Cognitive Processing Therapy Initiation Among Veterans (N = 334)
| Predictor | OR | 95% CI | p |
|---|---|---|---|
| Telemedicine (reference: yes) | 1.10 | 0.39–3.12 | ns |
| Gender (reference: female) | 0.71 | 0.25–1.99 | ns |
| Therapy (reference: CPT) | 0.70 | 0.32–1.43 | ns |
| Age (reference: 55+ years) | |||
| Under 35 years | 0.48 | 0.18–1.26 | ns |
| 35 to 54 years | 0.40 | 0.16–1.02 | .056 |
| PTSD Checklist Score (reference: high) | 0.99 | 0.95–1.03 | ns |
Note. PE = prolonged exposure; PTSD = posttraumatic stress disorder.
Predictors of Treatment Dropout
The same predictors as described above were examined in a multinomial regression examining prediction of treatment dropout (see Table 3). Therapist assignment did not account for a significant amount of variance in dropout (ICC = 0.03, p = .527), therefore therapist was not included in the model. The deviance goodness-of-fit test indicated that the model was a good fit for the data, χ2(566, N = 301) = 69.22, p = .247. Age was a significant predictor of dropout. Veterans under 35 years of age were significantly more likely to drop out early or late (as compared to completing PE/CPT) than veterans over 55 years. Veterans in the middle age range were more likely than older veterans to drop out of treatment early (as compared to dropping out late or completing PE/CPT). Therapy type was also a significant predictor; those who received PE were significantly more likely to be late dropouts than those who received CPT. When service era, rather than age, was included in the model, OEF/OIF/OND veterans were more likely to drop out early than complete (OR = 9.35, p = .001), drop out late than complete (OR = 2.10, p = .015), and drop out early than late (OR = 4.46, p = .026) as compared with Vietnam veterans.
Table 3.
Predictors of Prolonged Exposure and Cognitive Processing Therapy Dropout Status Among Veterans (N = 301)
| Early dropout vs. late dropout (reference) |
Early dropout vs. completion (reference) |
|||||
|---|---|---|---|---|---|---|
| Predictor | OR | 95% CI | p | OR | 95% CI | p |
|
| ||||||
| Telemedicine (reference: yes) | 0.77 | 0.21–2.82 | ns | 0.96 | 0.29–3.18 | ns |
| Gender (reference: female) | 1.85 | 0.54–6.41 | ns | 1.56 | 0.48–5.08 | ns |
| Therapy (reference: CPT) | 0.99 | 0.40–2.46 | ns | 1.75 | 0.74–4.14 | ns |
| Age (reference: 55+ years) | ||||||
| Under 35 years | 3.50 | 0.84–14.18 | ns | 6.93 | 1.79–26.84 | .005 |
| 35 to 54 years | 5.03 | 1.26–20.14 | .022 | 8.41 | 2.25–31.46 | .002 |
| PTSD Checklist score (reference: high) | 1.32 | 0.53–3.27 | ns | 1.34 | 0.57–3.16 | ns |
| Late dropout vs. completion (reference) |
||||||
| Telemedicine (reference: yes) | — | — | — | 1.29 | 0.58–2.69 | ns |
| Gender (reference: female) | — | — | — | 0.84 | 0.41–1.73 | ns |
| Therapy (reference: CPT) | — | — | — | 1.77 | 1.03–3.05 | .038 |
| Age (reference: 55+ years) | ||||||
| Under 35 years | — | — | — | 2.00 | 1.04–3.86 | .038 |
| 35 to 54 years | — | — | — | 1.67 | 0.86–3.25 | .129 |
| PTSD Checklist score (reference: high) | — | — | — | 1.02 | 0.59–1.73 | ns |
Note. PE = prolonged exposure; PTSD = posttraumatic stress disorder.
Discussion
Of veterans who were deemed appropriate and offered PE/CPT, only about one half completed the treatment. Approximately 18% failed to initiate the treatment, and about one third of those who initiated dropped out before completion. The proportion of veterans who failed to initiate PE/CPT was approximately twice as large as was reported by Chard et al. (2010), but much smaller than the 89% reported by Mott, Mondragon, and colleagues (2014). As discussed above, the composition of Mott et al.’s noninitiator group makes comparisons difficult; however, it is unclear why our rate of initiation was lower than Chard et al.’s. It is possible that differences in how veterans are referred to PE/CPT or the intake process could contribute to differing rates of initiation across clinics. In their examination of VHA PTSD residential programs, Cook et al. found that programs varied in terms of which veterans were offered PE/CPT; some programs offered the treatments to all veterans with PTSD, while others were more discerning (Cook et al., 2013). This may also be true for outpatient clinics, and differing entry requirements may impact rates of initiation. Future research should also examine methods of presenting the treatments that may facilitate initiation. For example, Mott and colleagues recently piloted a shared decision-making tool that showed promise in increasing interest and participation in PE/CPT (Mott, Stanley, et al., 2014).
The rate of dropout among those who initiated treatment is higher than has been demonstrated in reviews of PE/CPT in civilian populations (Hembree et al., 2003). However, it was similar to what has been reported in prior studies of veteran populations (e.g., Chard et al., 2010; Jeffreys et al., 2014; Schnurr et al., 2007; Suris et al., 2013). Regarding the timing of dropout, consistent with the prior research conducted within VHA, we found that early dropout was common; about one-quarter of veterans who dropped out did so before session three and a majority did so during the first two thirds of the protocol. This pattern of early dropout is particularly concerning given prior research suggesting that PE/CPT treatment gains do not begin to emerge until session six (Nishith, Resick, & Griffin, 2002). Thus, it is likely that the majority of veterans who dropped out continued to suffer from high levels of PTSD symptomology.
Age and service era were significant predictors of treatment dropout; younger veterans and OEF/OIF/OND veterans were significantly more likely to drop out of PE/CPT. There was also a trend toward OEF/OIF/OND veterans initiating treatment at a lower rate than Vietnam veterans. This finding is consistent with prior studies that have found age and service era to predict PE/CPT dropout (Eftekhari et al., 2013; Garcia et al., 2011; Gros et al., 2011; Jeffreys et al., 2014; Mott, Mondragon, et al., 2014; Rizvi et al., 2009). Unfortunately, because of a strong correlation between the two variables we were unable to examine the unique contributions of age and service era; prior work that included both variables yielded mixed findings (Jeffreys et al., 2014; Mott, Mondragon, et al., 2014). Regardless of whether age or factors associated with service era (e.g., time since trauma, cohort culture) are driving higher dropout rates, approximately 60% of eligible OEF/OIF/OND veterans either failed to initiate or dropped out of PE/CPT. Understanding their reasons for not completing treatment must be a research priority. Eftekhari et al. (2013) took a first step in examining this issue among more than 1900 veterans who received PE as part of the Mental Health Dissemination Initiative. For veterans who dropped out of PE before session eight, their clinicians were asked to report whether they dropped out because of symptom improvement, symptom worsening, “other” (in which the most often cited reasons were avoidance and scheduling conflicts), or unknown reasons. “Other” and symptom worsening were the most common reasons overall; OEF/OIF/OND veterans were more likely than other eras to drop out due to symptom improvement or unknown reasons. Research examining veterans’ perceptions of their reasons for dropout and examinations of outcomes following dropout, particularly among OEF/OIF/OND veterans would further this line of inquiry.
Therapy type was the other significant predictor of dropout; those who received PE were more likely to be late dropouts, and thus less likely to be completers, than those who received CPT. In interpreting these findings, it is important to remember that veterans were not randomly assigned to therapy type; thus this finding may be attributable to differential assignment to PE or CPT based on a veteran characteristic that is also associated with dropout, rather than a true difference between the two treatments. Findings from the three prior studies that compared dropout rates in PE and CPT are equivocal. In the one randomized trial, conducted with civilian female sexual assault survivors, there was no difference in dropout between PE and CPT (Resick, Nishith, Weaver, Astin, & Feuer, 2002). The two nonrandomized, VHA clinic-based studies yielded conflicting findings; one found higher rates of dropout for PE, whereas the other reported that more veterans with CPT dropped out of treatment (Jeffreys et al., 2014; Mott, Mondragon, et al., 2014). A trial that randomizes veterans to either PE or CPT, such as the ongoing VA-funded study entitled Comparative Effectiveness Research in Veterans with PTSD, is needed to definitively answer the question of whether PE and CPT have differing dropout rates among veterans.
In interpreting these findings, it is important to consider the limitations of the study. The primary limitation is that the data were collected from one PCT; although rates of dropout are consistent with prior studies, findings may not generalize to other clinics or the larger veteran population. Clinic-specific variables such as referral processes, selection of PE/CPT candidates (including a lack of specific inclusion/exclusion criteria), other available treatment options, and clinic culture may impact initiation and dropout. A related limitation is that we only examined a subset of potential predictors. Factors such as veterans’ perceived reasons for dropout, fidelity and competence in delivering the treatments, comorbidities, and engagement in concurrent treatments should be examined in future studies. Finally, the lack of data regarding PTSD symptomology before dropout prevents us from examining outcomes (both symptom exacerbation and remission) that may have contributed to dropout.
Despite these limitations, this study used a large, clinical sample of veterans to contribute to the emerging literature regarding dropout from PE/CPT. Findings demonstrate that dropout from PE/CPT is a serious problem; only one half of the veterans who presented for Session 0 and were deemed eligible finished treatment. The findings are even more alarming for younger and returning OEF/OIF/OND veterans; only 40% of OEF/OIF/OND veterans completed treatment. Prior studies suggest that a majority of the treatment dropouts will continue to struggle with high levels of symptomology (Nishith et al., 2002; Tuerk et al., 2011), which left untreated may lead to a course of chronic disability and diminished quality of life similar to the pattern documented among many Vietnam veterans (Schnurr, Lunney, Bovin, & Marx, 2009). Thus, increasing the rate of PE/CPT completion among veterans, especially among younger and returning veterans, must be a priority for researchers and clinicians. Although this study identified two significant predictors of dropout, the findings highlight the need for additional research. A comprehensive understanding of reasons for dropout will likely be needed to develop interventions to improve rates of completion. We recommend that future studies of dropout employ study designs that include veteran perspectives and provide data will facilitate the development of explanatory models of dropout that can guide intervention development.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. This material is based on work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development. Drs Shannon M. Kehle-Forbes and Laura A. Meis are supported by VA Health Services Research & Development Career Development Awards.
Contributor Information
Shannon M. Kehle-Forbes, Center for Chronic Disease Outcomes Research, Minneapolis VA Healthcare System, Minneapolis, Minnesota, and Department of Medicine, University of Minnesota
Laura A. Meis, Center for Chronic Disease Outcomes Research, Minneapolis VA Healthcare System, Minneapolis, Minnesota, and Department of Medicine, University of Minnesota
Melissa A. Polusny, Center for Chronic Disease Outcomes Research, Minneapolis VA Healthcare System, and Department of Psychiatry, University of Minnesota
Michele R. Spoont, Center for Chronic Disease Outcomes Research, Minneapolis VA Healthcare System, and National Center for PTSD, Honolulu, Hawaii
References
- Chard KM, Schumm JA, Owens GP, & Cottingham SM (2010). A comparison of OEF and OIF veterans and Vietnam veterans receiving cognitive processing therapy. Journal of Traumatic Stress, 23, 25–32. [DOI] [PubMed] [Google Scholar]
- Cook JM, O’Donnell C, Dinnen S, Bernardy N, Rosenheck R, & Hoff R (2013). A formative evaluation of two evidence-based psychotherapies for PTSD in VA residential treatment programs. Journal of Traumatic Stress, 26, 56–63. 10.1002/jts.21769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JJ, Walter KH, Chard KM, Parkinson RB, & Houston WS (2013). Treatment adherence in cognitive processing therapy for combat-related PTSD with history of mild TBI. Rehabilitation Psychology, 58, 36–42. 10.1037/a0031525 [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, & Marshall R (2006). The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science, 313, 979–982. 10.1126/science.1128944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, & Karlin BE (2013). Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. Journal of the American Medical Association Psychiatry, 70, 949–955. 10.1001/jamapsychiatry.2013.36 [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. New York, NY: Oxford University Press. [Google Scholar]
- Garcia HA, Kelley LP, Rentz TO, & Lee S (2011). Pretreatment predictors of dropout from cognitive behavioral therapy for PTSD in Iraq and Afghanistan war veterans. Psychological Services, 8, 1–11. 10.1037/a0022705 [DOI] [Google Scholar]
- Gros DF, Yoder M, Tuerk PW, Lozano BE, & Acierno R (2011). Exposure therapy for PTSD delivered to veterans via telehealth: Predictors of treatment completion and outcome and comparison to treatment delivered in person. Behavior Therapy, 42, 276–283. 10.1016/j.beth.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, & Tu X (2003). Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress, 16, 555–562. 10.1023/B:JOTS.0000004078.93012.7d [DOI] [PubMed] [Google Scholar]
- Hermes ED, Rosenheck RA, Desai R, & Fontana AF (2012). Recent trends in the treatment of posttraumatic stress disorder and other mental disorders in the VHA. Psychiatric Services, 63, 471–476. 10.1176/appi.ps.201100432 [DOI] [PubMed] [Google Scholar]
- Hosmer DW, & Lemeshow S (2000). Applied logistic regression (2nd ed.). New York, NY: Wiley-Interscience. 10.1002/0471722146 [DOI] [Google Scholar]
- Jeffreys MD, Reinfeld C, Nair PV, Garcia HA, Mata-Galan E, & Rentz TO (2014). Evaluating treatment of posttraumatic stress disorder with cognitive processing therapy and prolonged exposure therapy in a VHA specialty clinic. Journal of Anxiety Disorders, 28, 108–114. 10.1016/j.janxdis.2013.04.010 [DOI] [PubMed] [Google Scholar]
- Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, … Foa EB (2010). Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of Traumatic Stress, 23, 663–673. 10.1002/jts.20588 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, & Hoge CW (2012). Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: Reconciling prevalence differences between studies. Journal of Nervous and Mental Disease, 200, 444–450. 10.1097/NMD.0b013e3182532312 [DOI] [PubMed] [Google Scholar]
- Meyers LL, Strom TQ, Leskela J, Thuras P, Kehle-Forbes SM, & Curry KT (2013). Service utilization following participation in cognitive processing therapy or prolonged exposure therapy for posttraumatic stress disorder. Military Medicine, 178, 95–99. 10.7205/MILMED-D-12-00302 [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, & Stevens SP (2006). Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 898–907. 10.1037/0022-006X.74.5.898 [DOI] [PubMed] [Google Scholar]
- Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, & Teng EJ (2014). Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. Journal of Traumatic Stress, 27, 265–273. 10.1002/jts.21927 [DOI] [PubMed] [Google Scholar]
- Mott JM, Stanley MA, Street RL Jr., Grady RH, & Teng EJ (2014). Increasing engagement in evidence-based PTSD treatment through shared decision-making: A pilot study. Military Medicine, 179, 143–149. 10.7205/MILMED-D-13-00363 [DOI] [PubMed] [Google Scholar]
- Nishith P, Resick PA, & Griffin MG (2002). Pattern of change in prolonged exposure and cognitive-processing therapy for female rape victims with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 70, 880–886. 10.1037/0022-006X.70.4.880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SA, Grunfeld TE, Yadin E, Cahill SP, Hembree E, & Foa EB (2009). Changes in reported physical health symptoms and social function with prolonged exposure therapy for chronic posttraumatic stress disorder. Depression and Anxiety, 26, 732–738. 10.1002/da.20518 [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2006). Cognitive processing therapy: Veteran/military version. Boston, MA: VA Boston Healthcare System. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, & Feuer CA (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, & Resick PA (2009). Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy, 47, 737–743. 10.1016/j.brat.2009.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, … Bernardy N (2007). Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA: Journal of the American Medical Association, 297, 820–830. 10.1001/jama.297.8.820 [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Hayes AF, Lunney CA, McFall M, & Uddo M (2006). Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 707–713. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, & Marx BP (2009). Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review, 29, 727–735. 10.1016/j.cpr.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Shiner B, D’Avolio LW, Nguyen TM, Zayed MH, Young-Xu Y, Desai RA, … Watts BV (2013). Measuring use of evidence based psychotherapy for posttraumatic stress disorder. Administration and Policy in Mental Health and Mental Health Services Research, 40, 311–318. 10.1007/s10488-012-0421-0 [DOI] [PubMed] [Google Scholar]
- Surís A, Link-Malcolm J, Chard K, Ahn C, & North C (2013). A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress, 26, 28–37. 10.1002/jts.21765 [DOI] [PubMed] [Google Scholar]
- Taylor S (2003). Outcome predictors for three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Cognitive Psychotherapy, 17, 149–162. 10.1891/jcop.17.2.149.57432 [DOI] [Google Scholar]
- Thorp SR, Stein MB, Jeste DV, Patterson TL, & Wetherell JL (2012). Prolonged exposure therapy for older veterans with posttraumatic stress disorder: A pilot study. The American Journal of Geriatric Psychiatry, 20, 276–280. 10.1097/JGP.0b013e3182435ee9 [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Wangelin B, Rauch SA, Dismuke CE, Yoder M, Myrick H, … Acierno R (2013). Health service utilization before and after evidence-based treatment for PTSD. Psychological Services, 10, 401–409. 10.1037/a0030549 [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Grubaugh A, Myrick H, Hamner M, & Acierno R (2011). Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders, 25, 397–403. 10.1016/j.janxdis.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, & Acierno R (2010). A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress, 23, 116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. (2008). VHA handbook 1160.01: Uniform mental health services in VA medical centers and clinics. Washington, DC: Author. [Google Scholar]
- van Minnen A, Arntz A, & Keijsers GPJ (2002). Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy, 40, 439–457. 10.1016/S0005-7967(01)00024-9 [DOI] [PubMed] [Google Scholar]
- van Minnen A, & Hagenaars M (2002). Fear activation and habituation patterns as early process predictors of response to prolonged exposure treatment in PTSD. Journal of Traumatic Stress, 15, 359–367. 10.1023/A:1020177023209 [DOI] [PubMed] [Google Scholar]
- Veterans Health Administration & Department of Defense. (2010). VA/DoD clinical practice guideline for the management of post-traumatic stress. Washington, DC: Author. Retrieved from http://www.healthquality.va.gov/ptsd/cpg_PTSD-FULL-201011612.pdf [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Zayfert C, Deviva JC, Becker CB, Pike JL, Gillock KL, & Hayes SA (2005). Exposure utilization and completion of cognitive behavioral therapy for PTSD in a “real world” clinical practice. Journal of Traumatic Stress, 18, 637–645. 10.1002/jts.20072 [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Fitzgibbons LA, & Foa EB (1999). Response of African American and Caucasian women to cognitive behavioral therapy for PTSD. Behavior Therapy, 30, 581–595. 10.1016/S0005-7894(99)80026-4 [DOI] [Google Scholar]


