Abstract
Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT) are first-line treatments for posttraumatic stress disorder (PTSD) and have been disseminated throughout the U.S. Veterans Health Administration. Treatment non-completion is common and lessens clinical effectiveness; however, prior work has failed to identify factors consistently associated with non-completion. Semi-structured interviews were conducted with a national sample of veterans who recently completed (n = 60) or did not complete (n = 66) PE or CPT. Non-completer interviews focused on factors that contributed to veterans’ decisions to drop out and efforts undertaken to complete PE/CPT. Completer interviews focused on challenges faced in completing treatment and facilitators of completion. Transcripts were coded using a mixed deductive/inductive approach; constant comparison was used to identify differences between completers and non-completers. Completers and non-completers differed in the extent of treatment-specific therapist support received, therapists’ flexibility in treatment delivery, the type of encouragement offered by the care team and social supports, their interpretation of symptom worsening, the perceived impact of treatment on functioning, and the impact of stressors on their treatment engagement. Treatment-specific therapist support, more patient-centered and flexible treatment delivery, leveraging the full care team, and addressing functional concerns are potential targets for PE and CPT engagement interventions.
Keywords: PTSD, Psychotherapy, Engagement, Retention, Qualitative, Veterans
Prolonged exposure (PE) therapy and cognitive processing therapy (CPT), two first-line treatments for posttraumatic stress disorder (PTSD), have been disseminated and implemented within numerous health care systems over the past fifteen years. The U.S. Department of Veterans Affairs (VA) has been in the forefront of this implementation initiative (Karlin & Cross, 2014); over 6500 VA providers have participated in competency based training to deliver PE and CPT and tens of thousands of veterans initiate these treatments annually. A majority of veterans who initiate PE or CPT experience clinically-meaningful symptom reduction; however, a significant proportion of those who start treatment do not complete (Steenkamp et al., 2020). A review of randomized clinical trials (RCTs) examining PE and CPT in active duty and military veterans reported dropout rates ranging from 13 to 39% (Steenkamp et al., 2020). Rates of treatment non-completion in regular VA clinical practice are even higher; over 60% of veterans who initiated PE or CPT at the VA during a fifteen year period did not complete treatment (Maguen et al., 2019). While there is evidence that a minority of patients experience clinically significant change despite early termination (Szafranski et al., 2017), for most patients, sustained PE and CPT attendance yields superior symptom improvement (Berke et al., 2019; Holmes et al., 2019). Further, clinician concerns about high rates of treatment non-completion can limit the implementation of PE and CPT, and behaviors associated with treatment dropout (e.g., session no shows) negatively impact clinic operations and treatment access (Rosen et al., 2016). While PE and CPT do not appear to have uniquely high rates of treatment dropout (Fernandez et al., 2015), their widespread implementation and the potential benefits to be gained from treatment completion make the identification of modifiable factors that contribute to termination essential.
Most studies aimed at understanding dropout from PE and CPT have quantitively examined baseline variables hypothesized to predict subsequent treatment dropout. Patient age has been the only predictor that has consistently emerged across studies, with younger patients more likely to be treatment non-completers (Goetter et al., 2015; Imel et al., 2013; Kehle-Forbes et al., 2016; Maguen et al., 2019). Other demographic variables and characteristics of patients’ baseline clinical picture, including PTSD symptom severity, severity of symptom clusters (e.g., avoidance), and mental health comorbidities have been frequently examined without consistent findings (Berke et al., 2019; Garcia et al., 2011; Goetter et al., 2015; Gros et al., 2011; Grubbs et al., 2015; Hale et al., 2019; Kehle-Forbes et al., 2016; Lewis et al., 2020; Maguen et al., 2019).
In line with recommendations by Cooper et al. (2018), researchers have examined potentially modifiable contributors of non-completion and mechanistic variables that may underlie PE and CPT dropout. For example, a prospective study of veterans initiating PE or CPT across four VA clinics found that veterans whose loved ones encouraged them to face their distress (i.e., exhibited social control) were twice as likely to finish treatment, even after accounting for demographic predictors and baseline illness severity (Meis et al., 2019). Within treatment increases in distress have been hypothesized to lead to dropout; as such, variation in PTSD symptoms during therapy has been examined as a potential predictor of dropout. Eftekhari et al. (2020) examined whether self-reported symptom worsening predicted PE dropout among a national sample of veterans. They found that while PE therapists reported symptom worsening as the most common cause of treatment discontinuation in the sample, neither veteran-reported symptom course nor worsening between sessions emerged as significant predictors of non-completion. Similarly, Larsen et al. (2020) did not find that within treatment symptom increase predicted CPT dropout (Larsen et al., 2020). In examining treatment process variables, Youn et al. (2019) found that repeating treatment content during CPT to meet patient needs predicted treatment completion. While these quantitative studies examining potentially modifiable processes have furthered the literature on PE/CPT engagement, one-off findings without replication across studies continue to be the norm, and thus far, effective interventions for improving PE/CPT completion have remained elusive (Kehle-Forbes & Kimerling, 2017).
The lack of successful engagement interventions suggest that researchers have not yet identified – or properly refined – the most potent mechanisms of treatment discontinuation. Qualitative methods are particularly useful for theory refinement and hypothesis generation that can guide successful intervention development (Sofaer, 1999). Further, they can clarify complex patterns, like those that exist in the bidirectional therapeutic relationship in the context of fluctuating thoughts and behaviors related to treatment discontinuation (Shulman et al., 2019; Sofaer, 1999). Qualitative work examining PTSD treatment initiation more broadly has found that treatment initiators and non-initiators experienced similar barriers to treatment, but completers had additional facilitators to help overcome those difficulties (Sayer et al., 2009). Hundt et al. (2018), in the only known published qualitative examination of PE/CPT non-completion, interviewed 23 veterans at one VA clinic who failed to complete at least eight sessions of PE or CPT to elicit reasons for early termination, and through content analysis quantified the frequency of responses and themes. The most commonly reported theme was issues related to the therapist or therapy content, with lack of treatment buy-in (e.g., disagreement with treatment principles and components, misunderstanding of therapy rationale, preferring a present-focus) as the most common code within the theme. Logistical barriers, such as work demands that made participation more difficult, were the second most-often reported theme, followed by emotional barriers (e.g., treatment too stressful) and VA system-related issues. In a separate study conducted by the same team, most veterans who completed at least eight sessions of PE/CPT at the same VA clinic reported having thoughts of treatment dropout. Among those with thoughts of dropping out, desperation for symptom relief, support from family and therapist/group, and a strong working alliance facilitated completion (Hundt et al., 2017).
These findings point towards the complexity and interrelation of factors that contribute to non-completion, but additional work is needed to develop engagement interventions. To gain a more comprehensive understanding of PE/CPT non-completion with the long-term objective of developing an effective engagement intervention, we fielded theory-based semi-structured qualitative interviews with a national sample of veterans who completed or prematurely discontinued PE/CPT. We expanded Hundt et al.’s (2017, 2018) findings by querying a broad range of factors theorized to be relevant to psychotherapy engagement, in addition to veterans’ self-perceived reasons for completion or dropout; the conceptual model guiding the interviews and analysis was grounded in Social Cognitive Theory and the Theory of Planned Behavior (Ajzen, 1985; Bandura, 2004). This approach enabled the exploration of factors that may not have been identified as central to veterans’ completion, but which nonetheless may have contributed and could be leveraged in an intervention. Further, we asked completers and non-completers about the same set of contextual and treatment experience factors and directly compared their experiences to identify treatment aspects unique to non-completion.
1. Method
The Institutional Review Board of the Minneapolis VA approved all study procedures. All participants provided informed consent prior to study participation; the requirement for written documentation of informed consent was waived.
1.1. Participants
Participants were veterans who discontinued (n = 66) or completed (n = 60) PE or CPT in routine clinical care at VA clinics nationwide. To be eligible, non-completers must have (1) completed at least one but no more than six PE/CPT sessions, (2) been categorized as a treatment dropout by their therapist in the electronic medical record (EMR) or had a six-week lapse since their last PE/CPT session, and (3) not completed a PE/CPT “final session” as outlined in the respective treatment manuals. The non-completer sample focused on those with six or fewer sessions because rates of treatment discontinuation decline sharply after session six (Gutner et al., 2016). Non-completers were excluded if their therapist was engaged in active outreach at the time of recruitment, more than three months had elapsed since their last PE/CPT session, it was clear from the EMR that it would not have been possible for them to complete (e.g., a move), or their PE/CPT therapist initiated the early termination. To be eligible, treatment completers must have completed at least 10 PE or 12 CPT sessions and had a “final session” note. Veterans need not have been considered treatment responders to be included.
We used stratified purposive sampling, which captures the major variations within the population while also identifying common cores within subgroups of interest (Patton, 2002). The completer and non-completer samples were stratified by service era, type of therapy (i. e., PE, individual CPT, and group CPT), and gender. Prior research has found that a homogeneous sample of 12 participants results in the identification of 90% of themes (Guest et al., 2006); thus, we proposed 10–12 interviews per cell (see Fig. 1). If new themes had continued to emerge, additional interviews would have been conducted; however, thematic saturation was reached using the a priori defined sample size. Across strata, we purposively sampled for time of dropout for the non-completer sample, such that at least 25% of the sample discontinued following session one or two, and to enrich the samples in terms of racial and ethnic diversity.
Fig. 1.
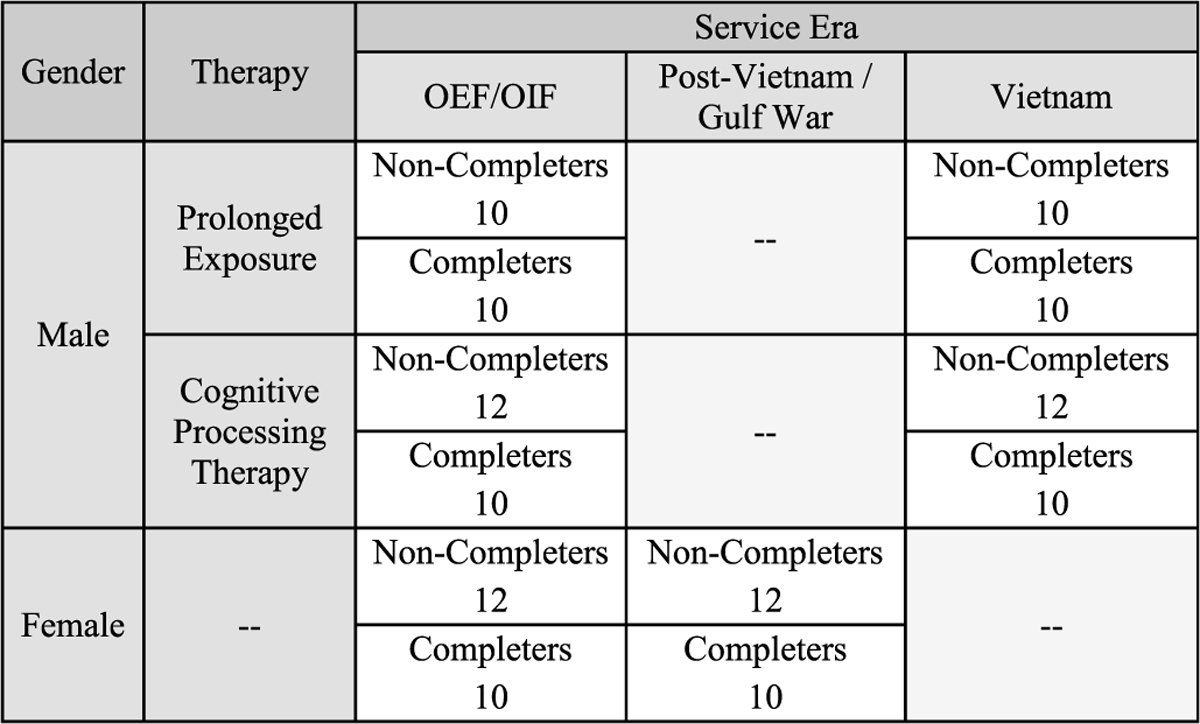
Interview Sampling Strategy Across Prespecified Strata
Note. In the Cognitive Processing Therapy strata, sample sizes were evenly divided across veterans participating in individual and group modalities. Due to the relatively small number of women Vietnam veterans and male Post-Vietnam/Gulf War veterans treated in VA PTSD clinics, veterans from those categories were excluded. OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom.
1.2. Procedures
VA administrative data generated from VA providers’ use of templated progress notes was used to identify veterans who discontinued or completed PE or CPT in routine clinical care. Within the stratum outlined above, a random subsample of veterans was selected for manual chart review to evaluate the inclusion/exclusion criteria. Veterans confirmed as eligible via chart review were first sent a letter informing them of the study, and then were called and invited to participate in a 90-min telephone interview to discuss their PE/CPT experience. Veterans were informed that we wanted to understand veterans’ experience with trauma-focused therapies for PTSD, such as PE and CPT. Veterans were paid $75 for participating in the interview.
Non-completer interviews sought to understand factors and processes that contributed to veterans’ decisions to drop out and efforts undertaken to complete PE/CPT. Interviews with treatment completers focused on challenges faced in completing treatment, the impact of those challenges on the treatment decision-making process, and the processes that facilitated treatment persistence and/or the strategies that veterans used to overcome those obstacles. Initial development of the interview guides was based on our conceptual framework rooted in Social Cognitive Theory (Bandura, 2004), which posits that behavior maintenance results from of a dynamic interaction between personal factors (beliefs and affect), the environment, and behavior. We drew from Theory of Planned Behavior (Ajzen, 1985) to develop questions regarding the specific types of beliefs that may impact PE/CPT treatment completion. Behavioral (beliefs about outcomes and their desirability likely to result from treatment engagement), normative (perceived social pressure to engagement), and control (perceptions about one’s own ability to engage and manage specific demands of engagement) beliefs were queried. In this context, affect refers to PTSD symptoms. The environment consists of both physical (logistical barriers) and social influences (learning that takes place by observing others in the environment including the therapist, care team, and other social supports). As such, the interviews assessed treatment experiences (including therapeutic alliance), social influences, beliefs about treatment and PTSD, symptoms, logistical barriers, and engagement behaviors. Interview guide refinement was an iterative process; during the first six participant interviews, study investigators read the interview transcripts and met after every two interviews to discuss modifications to the interview guides. All domains initially queried were retained during the guide revisions. Examples of modifications included instructions to identify and retain focus on the treatment episode of interest, manage time, and provide the interviewer with the overall goals of question segments to guide follow-up. Further, prompts eliciting detailed information about past care episodes were removed in the interest of time and prompts were edited to more fully elicit the specific content of interest (e.g., querying specific therapy elements, such as imaginal exposure or challenging beliefs worksheets, when asking about treatment experience). Thereafter, the study team met biweekly to make minor modifications to the guide as needed, review emerging problems (e.g., problem solving how to approach interviews with veterans who intended to return to PE/CPT; managing multiple prior episodes of PE/CPT), discuss preliminary themes, and further refine the guide as needed. All interview guide iterations were kept as part of the audit trail, a collection of documents meant to increase the transparency of the research process (Patton, 2002); see Supplemental Materials for the final version of the interview guide. The guide was applied flexibly to ensure a conversational style, while ensuring that all participants were asked the same set of questions. Four doctoral-level (SMKF, PA, LM, RO) and one master-level interviewers with degrees in clinical or counseling psychology conducted the interviews. The doctoral level interviewers were involved in the study either from grant or interview guide development to publication; the masters-level interviewer left the project shortly after data collection began.
1.3. Coding and analysis
Interviews were audio recorded, professionally transcribed, and reviewed for accuracy. NVivo 10 was used for data management and to facilitate the coding process. Top level codes were initially derived from our conceptual model. During the first phase of coding, all members of the coding team (which included all doctoral-level interviewers, two additional doctoral-level clinical psychologists [MS, HVM], and the project coordinator [AL]) applied the top-level codes to six transcripts. After coding each transcript, the team met to refine codes and their definition, identify exemplar quotes, and identify examples of text segments that each code was not intended to capture. Once the top-level codes were fully developed and coding consistency was achieved across coders, they were applied to all completer and non-completer transcripts. Top-level codes were (1) treatment-related expectancies and beliefs about PE/CPT and PTSD, (2) commitment (including dropout thoughts and behaviors) and treatment motivation, (3) engagement strategies used to counter ambivalence/thoughts of dropping out, (4) logistical and social factors, (5) reaction to the treatment components, (6) symptoms and functioning, and (7) therapeutic skill and alliance.
In the second coding phase, pairs of coders deductively identified narrower (more specific) lower-order codes within each top-level code from the content of the transcripts. Coding pairs jointly read a segment of transcripts (typically four to six) to establish the full codebook (names, definitions, examples of what was not included in the code, and exemplary quotes), which was then applied to all text segments that had received a top-level code in the first phase of coding; emerging themes from the interview meeting were also incorporated at this phase as warranted. Throughout, 20% of transcripts were coded by two independent coders to ensure trustworthiness and prevent drift. Discrepancies were resolved by consensus; if the pair could not resolve the discrepancy, it was brought to the full team. The coding team met biweekly to resolve discrepancies, suggest modifications to the codebook, and discuss emerging themes.
Once coding was complete, the coding pairs extracted themes resulting from all codes within their top-level codes. Specifically, each individual team member created a memo summarizing themes present for completers, present for non-completers, and present for both completers and non-completers. Pairs then compared their impressions and prepared a memo summarizing findings that was shared with the full study team. The study team reviewed and discussed the findings within each top-level code and identified themes that cut across top-level coding categories. Content from these discussions was captured in study memos. All summary analytic memos were used in consolidating and finalizing study findings.
2. Results
Across the completer and non-completer samples, 172 veterans were recruited for study participation, 80.8% (n = 139) provided informed consent, and 73% (n = 133) completed interviews. Seven interviews were excluded from the analyses due to poor audio recording quality (n = 3), receipt of PE as part of a different research study (n = 1), confusion regarding target treatment episode (n = 2), and participant opting not to complete the full interview (n = 1). The demographic and treatment characteristics of the 126 veterans whose data were included in the analysis are summarized in Table 1; veterans from 40 unique VA facilities were included in the sample. Among the non-completers, 30.3% (n = 20) were early discontinuers (e.g., dropped out following session 1–2); the remainder (n = 46; 69.7%) discontinued following sessions 3–6. Prominent differences did not emerge between completers and dropouts in several queried domains; both groups reported similar buy-in to the rationale, expectancies of treatment helpfulness at initiation, emotional experiences in approaching trauma content, and reactions to the treatment elements. Identified domains and factors differentiating the experiences of completers and non-completers are displayed in Table 2; the most prominent themes distinguishing veterans who completed from those who did not complete are presented below.
Table 1.
Demographic and treatment characteristics of completers and non-completers.
| Characteristic | Non Completers |
Completers |
Full sample |
|||
|---|---|---|---|---|---|---|
| N | % | n | % | N | % | |
|
| ||||||
| Gender a | ||||||
| Female | 24 | 36.4 | 20 | 33.3 | 44 | 34.9 |
| Male | 42 | 63.6 | 40 | 66.7 | 82 | 65.1 |
| Service era a | ||||||
| Iraq/Afghanistan | 34 | 51.5 | 30 | 50.0 | 64 | 50.8 |
| Post-Vietnam | 12 | 18.2 | 10 | 16.7 | 22 | 17.5 |
| Vietnam | 20 | 30.3 | 20 | 33.3 | 40 | 31.7 |
| Treatment type a | ||||||
| Prolonged Exposure | 29 | 43.9 | 30 | 50.0 | 59 | 46.8 |
| Individual Cognitive Processing Therapy | 23 | 34.8 | 16 | 26.7 | 39 | 31.0 |
| Group Cognitive Processing Therapy | 14 | 21.2 | 14 | 23.3 | 28 | 22.2 |
| Race | ||||||
| White | 33 | 50.0 | 40 | 66.7 | 73 | 57.9 |
| Black/African American | 20 | 30.3 | 14 | 23.3 | 34 | 27.0 |
| Other | 12 | 18.2 | 4 | 6.7 | 16 | 12.7 |
| 1 | 1.5 | 2 | 3.3 | 3 | 2.4 | |
| Ethnicity | ||||||
| Hispanic | 10 | 15.2 | 8 | 13.3 | 18 | 14.3 |
| Not Hispanic | 55 | 83.3 | 51 | 85.0 | 106 | 84.1 |
| Unknown | 1 | 1.5 | 1 | 1.7 | 2 | 1.6 |
| PTSD severity b | ||||||
| Screened positive for PTSD | 47 | 71.2 | 32 | 53.3 | 79 | 62.7 |
| Screened negative for PTSD | 5 | 7.6 | 19 | 31.7 | 24 | 19.0 |
| Unknown | 14 | 21.2 | 9 | 15.0 | 23 | 18.3 |
Note. N = 126 (n = 60 completers, n = 66 non-completers).
Extracted from electronic medical record.
Positive screen was a score of 31 or above on the PTSD Checklist-5.
Table 2.
Summary of veteran differences & similarities in experiences of veteran PE and CPT completers and non-completers.
| Theme | Completers’ Experience | Non-Completers’ Experience | Similarities in Completers’ & Non-Completers’ Experience |
|---|---|---|---|
|
| |||
| Therapists “In the Trenches” with Patients | Therapists provided support specific to engaging in/completing treatment (treatment-specific rapport) Mutual responsibility for treatment completion; patients felt obliged to do their part to complete Therapists perceived as nonjudgmental in response to adherence problems/ambivalence | Fewer conversations about engagement; treatment-specific rapport rare Non-completers less likely to disclose challenges Engagement discussions less collaborative; therapists less likely to assist with challenges when reported | Veterans liked their providers, had positive regard (nonspecific rapport) Veterans thought their providers had their best interest at heart & wanted them to get better |
| Patient-Centered Rather than Protocol-Centered Delivery | Treatment delivery flexible & responsive to patient needs Therapists tailored treatment to meet veteran need, particularly around trauma-specific content Veterans perceived autonomy & shared control in moving through treatment components | Treatment delivery more often rigidly followed protocol; examples of extreme protocol adherence (e.g., reading directly from manual in session) Therapist reiterated protocol/rationale in response to adherence challenges Treatment felt impersonal; veterans didn’t feel understood | None identified |
| Community Support around the Shared Goal of Completion | Non-PE/CPT mental health providers gave support specific to treatment completion Adjunctive treatments used to facilitate completion Friends & family knew more about treatment & gave instrumental social support to aid completion | Few discussed interacting with non-PE/CPT providers during treatments Family & friends did not know details of PE/CPT | Patients reported feeling supported by other care providers & social supports; perceived strong emotional support |
| Meaning Attributed to Increased Distress and Symptom Worsening | Viewed worsening as part of the treatment process Worsening viewed as having only transient impact | Distress/exacerbation more central to experience Worsening taken as evidence the treatment wouldn’t be helpful Worry that worsening would lead to severe and/or long-lasting negative impacts | Nearly all veterans perceived worsening in at least one PTSD symptom, emotional response, or functional domain Overall, descriptions of worsening similar |
| Anticipated Impact of Treatment on Social and Role Functioning | Expected positive impact of treatment on functioning | Anticipated negative consequences of participation on work & family; veterans barely making it, felt treatment risked functioning | Described impact of treatment on functioning during treatment course did not differ |
| Hassles and Stressors Differentially Impact Treatment Engagement | Focused on expected long-term benefit to continue with treatment when facing other stressors | Felt overwhelmed by competing demands & reported need to prioritize between stressors/hassles and treatment participation Used stressors as excuse to discontinue when ambivalent | Reported similar frequency and types of stressors during treatment |
2.1. Therapists “In the trenches” with patients
Most patients had an overall positive regard for their providers, which we termed non-specific rapport. Differences between completers and non-completers were marked in what we labelled treatment-specific rapport, which reflects support specific to engaging in treatment components and treatment completion; completers reported therapists joined them in the shared goal of successful completion. Treatment completers said their providers repeatedly encouraged staying in treatment, engaged them in conversations about their motivations for treatment, reminded them of why they started treatment, elicited their reactions to the materials presented, engaged in collaborative analysis and problem-solving regarding their concerns, and served as “cheerleaders” by pointing out their progress. As one patient reported, his therapist was “someone in my corner rooting for me, [saying] ‘You’re going to get better, this is going to help and I’m here to help you.’” Further, in the face of concerns, ambivalence, or non-adherence, completers’ therapists were not perceived as engaging in negative behaviors (e.g., did not get angry, pressure, or badger), but rather, they were viewed as non-judgmentally joining the patient in finding solutions to facilitate completion. One veteran reported,
“I didn’t do the homework one time because it was so rough. I apologized to him. I told him that I was anxious about going that day … But he made me feel comfortable and he said, ‘I don’t want you to ever be anxious about coming here. We’re doing this for you.’”
Completers reported this stance led them to feel less ashamed or concerned about inadvertently insulting their therapist by bringing up concerns, which encouraged conversations about adherence. The result was a perception that the therapist and veteran were “in the trenches” together, and completers often noted that their relationship with their therapist helped them push through tough times and complete therapy. The mutual commitment led veterans to not want to disappoint their therapist and to feel as though they were responsible for at least meeting the therapists’ investment in making treatment successful.
Conversely, non-completers reported fewer conversations about their reactions to the treatment and less collaborative interactions; as such, this aspect of treatment-specific rapport rarely developed. While a few non-completers reported appreciating therapists encouraging them to stick it out or cheering them on after a hard session, many said therapists did not address their concerns or help navigate problems as they came up. This resulted in a pattern in which patients reported being less likely to disclose concerns or ambivalence to their provider, thereby limiting opportunities for problem solving. As one veteran reported, “I didn’t realize the appointment had been set, and so I missed the appointment. [The therapist] called me and reprimanded me for not showing up. Then I was afraid to actually see her, but I couldn’t change therapists.”
2.2. Patient-centered rather than protocol-centered delivery
One facet of treatment delivery that both contributed to and resulted from the treatment-specific rapport described above was flexibility that prioritized the needs of the patient. Completers frequently reported their therapists were responsive to their needs and flexible in the treatment delivery, whereas non-completers were more likely to describe rigid protocol adherence. This was particularly evident regarding approaching trauma-specific content. For example, when veterans were unable or unwilling to engage with trauma accounts at the session indicated in the protocol, completers indicated their therapists would collaboratively tailor treatment by deciding what trauma content the veteran could engage with at that session and developing a plan for moving towards protocol-consistent activity. One completer stated that when he expressed concerns, his provider would respond with, “Why don’t you think you could do this? How can we get this done?” Completers may have started with only a segment of their trauma narrative, with a less distressing trauma, or modified the exercise to make it less intense (e.g., writing rather than speaking during imaginal exposure).
Further, completers reported feeling reassured that they would not be made to do anything they did not want to do, being encouraged to take breaks as needed in session and during homework, and being encouraged to try treatment components with the promise of shared problem-solving if they were unable to continue. This patient-centered treatment approach encouraged patient autonomy, lent itself to a sense of control over the treatment, made patients feel heard, and contributed to treatment-specific rapport. One completer said of his therapist,
“[He] left a lot of decisions up to me. I felt like he was taking my experience into consideration and not just his diagnosis [of me] … I felt like he allowed me to take part in what I felt was going to work for me.”
In contrast, non-completers reported that their therapists would refer the patient back to the treatment protocol without tailoring the treatment to veterans’ concerns. For example, PE non-completers frequently were skeptical regarding the focus on one trauma, given their complex trauma histories. Non-completers reported their therapists often responded by reiterating the rationale, rather than allowing for the possibility of conducting imaginal exposure with an additional trauma or bringing in discussion of other important traumas during processing. Overly strict applications of the protocol were also reported in more mundane treatment aspects by non-completers; examples included discouraging the use of verbal recordings in lieu of worksheets and a low-literacy veteran being chided for having his wife record his homework.
This restrictive interpretation of how to deliver the treatment protocol contributed to the treatment feeling impersonal and veterans feeling as though their therapists did not know or understand them. One non-completer stated, “Like I said, there was no personal questions about my symptoms and how I live. She actually still doesn’t know me.” This decreased their belief that treatment would be effective as they questioned how a therapist who does not know them could be helpful. It also prevented the development of treatment-specific rapport as veterans became less willing to share concerns or ambivalence, thus giving providers fewer opportunities to tailor the treatment and join with the veteran in the shared goal of completion. Finally, the overly strict protocol application caused non-completers to question their providers’ motivation, skill, and expertise. One veteran said, “The entire time she read from a sheet. It was extremely impersonal and forced. Like she was there for a paycheck instead of what she was there to do.”
2.3. Community support around the shared goal of completion
The principles of treatment-specific rapport were mirrored in other relationships for treatment completers; specifically, other members of the care team and family and friends provided support specific to PE/CPT treatment completion, rather than general or non-specific support. There was a marked difference in the role that non-PE/CPT therapists and psychiatrists played for treatment completers as compared to non-completers. Completers were more likely to report contact with a non-PE/CPT therapist during treatment and were more likely to describe instances in which these providers were supportive of their PE/CPT attendance, provided positive reinforcement and encouragement, held veterans accountable, and reiterated the importance of treatment attendance. One completer noted of their non-PE therapist, “She would still make sure that I was in therapy doing the Prolonged Exposure … She was always making sure that it was going okay and that if I needed anything that she’d be there.” Completers also described communication among their providers to ensure consistency in messaging and treatment goals. One completer reported, “They communicated with each other … them having that open communication and having a set goal not to mess up the other [helped me continue].”
Both non-PE/CPT therapists and psychiatrists also assisted veterans in managing other life stressors or increased distress that arose during PE/CPT, facilitating continued participation. For example, multiple completers noted that psychiatrists prescribed sleep medications to use in the short-term in response to increased difficulty sleeping early in PE/CPT; this allowed veterans to continue in treatment without concerns about a negative impact on functioning. One veteran reported that in response to symptom worsening early in treatment, “[PE therapist] ended up referring me to an additional psychiatrist to discuss possible medication options, as well as some alternative methods like herbal supplements and things like that to help me to deal with the extra symptoms.” Relatively few non-completers reported engaging with other mental health providers during treatment; those that did described providers who were agnostic about PE/CPT and provided non-specific support to veterans in making their own choices about continuation.
The type of support offered by social supports outside of the treatment context also differed for completers and non-completers. Completers indicated their social contacts tended to know more about treatment and offered more treatment-specific support. Examples of such support included driving veterans to appointments and staying in the waiting room as a show of support, watching veterans’ children while veterans worked on homework assignments, helping with homework and participating in in vivo exercises, and talking with the provider to better understand assignments and what to expect. A completer noted, “After every session I would talk to [my wife]. I would discuss with her what happened and tell her my homework assignments so she could hold me accountable.” Non-completers reported that a majority of social contacts did not know the content or potential impacts of PE/CPT. They also reported more general emotional support rather than specific support of treatment completion, as exemplified by the following quote from a non-completer: “Everyone just wants the best for me, and so whatever decision I made they back me up. Everyone told me, ‘It’s your decision. We’ll support you.’”
2.4. Meaning attributed to increased distress and symptom worsening
Most completers and non-completers reported perceived worsening in at least one PTSD symptom, other emotional response, or domain of functioning. Descriptions of worsening included acute, transient symptom exacerbation immediately surrounding sessions and homework assignments, and more sustained worsening lasting days or weeks. A small number of non-completers reported severe worsening (e.g., increased suicidal ideation, difficulty functioning), but such reports were rare. Differences between completers and non-completers emerged in the meaning attached to perceived worsening and the perceived severity of potential consequences of sustained symptom worsening. Treatment completers viewed worsening as part of the treatment process. One PE completer reported, “Once I started repeating [the trauma] constantly I would wake up two, three, sometimes four times a week with nightmares … I assume that was supposed to happen.” As such, exacerbation did not signal to them that the treatment was ineffective, allowing them to focus on the anticipated long-term benefit when facing trauma content. One completer stated he was able to keep the “better times in mind” when distressed. This enabled completers to continue to engage with trauma content long enough to see improvement, which in turn strengthened resolve.
Non-completers spoke more extensively about worsening than completers, and distress/exacerbation was more central to their experience. It was viewed as an indicator that treatment was not working, and was not going to work, rather than part of the treatment process. This was in part due to a violation of assumptions about how one would feel during and immediately after sessions; many non-completers reported the expectation that therapy sessions would improve their mood and symptoms acutely, and that they would leave feeling better than they came. Faced with increased distress during and after sessions or lack of improvement, they concluded therapy was not effective. One non-completer stated, “By the third session I just kind of figured I’m not changed a lot and I don’t want the paperwork so I’m just not going to go.”
Non-completers also worried more about the impact of continuing treatment in the face of symptom worsening and their feared negative impacts were more severe. Concerns regarding onset of deep depression, harming oneself or others, being unsafe or retraumatized, losing control, or relapsing on alcohol or other drugs were considerably more common for non-completers. A non-completer illustrated these fears saying, “[I was worried it would] make a wreck of me; I was already depressed and really scared of myself. Scared of my own damn demons.” Completers also frequently discussed potential negative consequences, but their worries had less severe and shorter lasting consequences (e.g., temporary irritability with loved ones, difficulty concentrating). Finally, as described below, non-completers more often discussed fears of impairment in functioning related to treatment.
2.5. Anticipated impact of treatment on social and role functioning
In addition to the anticipated impact of symptom exacerbation, non-completers were generally more likely than completers to anticipate negative consequences of treatment participation on functioning in important life domains. Worries about having to go back to work and family with increased distress were common. Many non-completers reported the sentiment that they were “barely making it” and decided continued participation was not worth the risk of considerable and permanent damage. A non-completer said,
“I don’t know if there’s a way to get a person mentally back from all of that reliving. I couldn’t—I knew I wasn’t what I wanted to be as far as school and in my family life after the sessions. It left me out there and I didn’t know how to come back.”
As another veteran noted, post-session he “carried it with him” back to his family, which he viewed as unacceptable. The perceived costs of the amount of time required to engage in treatment on family and work also contributed to the cost/benefit analysis described by non-completers. Completers did not express the same concerns regarding impact of participation; they more often discussed potential benefits of treatment on family and work functioning.
2.6. Hassles and stressors differentially impact treatment engagement
Completers and non-completers reported similar frequency and types of stressors during treatment; however, their impact on treatment differed in that life events disrupted treatment more often for non-completers. This was particularly notable for minor stressors and daily hassles; non-completers found it necessary to prioritize between competing demands and often chose not to prioritize treatment completion. They felt overwhelmed by the competing demands, illustrated in the following quote from a non-completer: “Just put it on hold … so that I wouldn’t have to be dealing with two or three different things at a time.” On occasion, non-completers reported using life stressors (real and exaggerated) as reasons for ending treatment early in the face of ongoing ambivalence. One non-completer reported, “I had surgery and it was just convenient not to go. It was like okay, I’ll just use that as my excuse.” Completers did not report having difficulty managing competing demands; in instances where they needed to prioritize, they chose to focus on treatment, often due to the belief in a longer-term benefit.
2.7. Limited differences emerged by treatment type
Finally, we examined differences in the treatment experiences of completers and non-completers who received PE, individual CPT, and group CPT. The themes reported above were present in all treatment types, although modest differences emerged in the relative prominence of themes by treatment type. Reports of acute (within or immediately post-session) distress were somewhat more common among those who participated in PE and was cited more often by PE than CPT non-completers. Those who discontinued CPT more often reported that the treatment structure was too rigid as compared to those who discontinued PE. Finally, logistical barriers were more common among group CPT non-completers than individual PE or CPT non-completers. Given the structure of group, it is not possible to re-arrange appointments to accommodate life stressors or daily hassles. A sizable minority of CPT group non-completers reported that they were considered dropouts once they missed two sessions, which typically happened as the result of scheduling challenges or other daily hassles (e.g., lack of transportation). Treatment-specific therapeutic rapport did not differentiate CPT group completers and non-completers as starkly as for those in individual PE or CPT; similarly, the importance of treatment tailoring and patient-centeredness was not as often discussed by group CPT completers.
3. Discussion
This qualitative study of a national sample of veterans who did and did not complete PE and CPT found that completion was facilitated by social environmental influences including therapeutic rapport specific to the components of treatment and a care team and social system supporting completion, control beliefs regarding one’s ability to weather increased distress/symptom exacerbation (i.e., affect) without fear of serious impact, and behavioral beliefs including fewer concerns about the impact of participation on long-term functioning and prioritization of treatment in the context of life stressors. Treatment-specific factors such as flexible patient-centered protocol delivery also facilitated completion. Directly comparing the experiences of completers and non-completers revealed that factors thought to be unique to non-completers were shared by both groups. For example, logistical barriers (physical environment influences) and a lack of buy-in were previously identified as being associated with dropout by (Hundt et al., 2018), while our findings suggest they are a shared experience for both completers and non-completers. The comparison also revealed that nuances between the two groups within the same theme – rather than differences at the broad thematic level – differentiated outcomes. Hundt et al. (2018) found that alliance issues contributed to dropout; the current study expanded on that conclusion in finding that non-specific rapport was similar for non-completers and completers, while treatment-specific rapport was associated with completion. The importance of such nuances in understanding dropout may partially explain why quantitative approaches have largely failed to identify predictors and why engagement interventions have had limited success.
There were limitations to the study methodology, including a reliance on retrospective accounts of veterans’ treatment experiences. While interviews were conducted as soon as was practicable following treatment, veterans’ ultimate treatment outcomes may have influenced their recollections. Further, the themes presented reflect only the patient perspective. While that is arguably the most important data source for what is ultimately a patient decision, it is possible that two veterans may interpret the same action by a provider differently, leading to divergent outcomes. Provider and objective data (e.g., session coding) would likely clarify and expand findings. Given that a sizable minority of CPT group non-completers reported that they were considered dropouts once they missed two sessions rather than due to their own decision to discontinue with treatment. caution must be used in applying the findings to group CPT. This distinct aspect of group treatment may necessitate unique interventions. Finally, it is unclear how these findings generalize to non-veteran samples and non-VA settings. Nevertheless, our study interviewing a national sample of veterans and directly comparing the experiences of completers and non-completers provides a nuanced, in depth understanding of factors that lead to treatment dropout and point toward multiple promising intervention targets.
Treatment-specific therapeutic rapport was one of the most prominent facilitators of completion. Across diagnosis and treatment types, the therapeutic relationship or working alliance has repeatedly been found to predict treatment engagement, including session attendance, and has been demonstrated to be a stronger predictor than client or treatment-specific factors (Holdsworth et al., 2014). Research on specific aspects of working alliance have been limited, although consistent with our findings, prior work has pointed to therapist flexibility as a facilitator and therapist rigidity as an impediment to strong working alliance across treatment approaches (Ackerman & Hilsenroth, 2001, 2003). Further, among therapists treating children with anxiety, flexible application of cognitive-behavioral therapy has been associated with greater patient engagement (Chu & Kendall, 2009; Hudson et al., 2014). We recommend that future research on the specific elements of therapeutic rapport that facilitate PE/CPT completion incorporate objective data (e.g., session ratings) and examine both direct and moderating effects. Our data demonstrated that not only did treatment-specific rapport directly encourage completion, but also buffered the negative impacts of impediments to completion. Other factors such as symptom exacerbation or functional concerns may be more difficult to modify; thus, strengthening this type of rapport may be a particularly potent engagement intervention target.
Balancing flexibility and patient-centeredness with fidelity to core treatment elements has long been encouraged as best-practice in the delivery of protocolized psychotherapies (e.g. Kendall & Frank, 2018). The current findings reinforce the importance of this dialectic. Prior work has demonstrated that the addition of non-protocol stressor sessions to address psychosocial emergencies does not negatively impact CPT outcomes (Galovski et al., 2012) and that fidelity-consistent adaptations (i.e., modifications that do not change core treatment elements) can enhance CPT outcomes (Marques et al., 2019) However, research identifying necessary treatment elements and adaptations that optimize outcomes for PE and CPT has been limited; given the threat of adaptations serving to collude with avoidance in trauma-focused treatments for PTSD, careful documentation of adaptations and outcome monitoring will be essential for engagement interventions encouraging flexible delivery.
Considerably more veterans in the current sample reported distress/symptom worsening than has been found in past quantitative studies (Eftekhari et al., 2020; Keller et al., 2014), although one recent study among veterans receiving CPT reported worsening in about two-thirds of patients (Larsen et al., 2020). Veterans in our study conceptualized increased distress during and immediately following treatment activities as worsening, although such changes in mood or symptoms likely would not be reflected in the pre-session weekly self-report symptom measures typically used when examining exacerbations. Further, prior studies have not found symptom worsening to be predictive of dropout (Eftekhari et al., 2020; Larsen et al., 2020). Given that nearly all completers and non-completers reported worsening, this is not surprising; however, it could lead to inaccurate conclusions that symptom worsening does not play a role in dropout. Rather, the data point toward the need to conduct a thorough assessment of perceived worsening, its feared impact on functioning, and strategies for minimizing its potential impact. One such strategy may be delivering PE/CPT in an intensive, or massed, format. Recent studies examining the effectiveness of PE and CPT with multiple weekly sessions have found considerably lower dropout rates than occur with weekly sessions (Bryan et al., 2018; Foa et al., 2018; Held et al., 2020). This may be because the risk of shorter-term worsening in exchange for nearer-term relief changes the cost/benefit analysis enough to facilitate completion. In addition, patients sometimes take leave from work and/or complete massed treatment in a residential setting, which may lessen fears about the impact of worsening on valued functional domains. Examining mechanisms of increased engagement in future studies of massed treatment may help refine the delivery model and facilitate development of other engagement interventions.
The presence of life stressors and logistical barriers did not differentiate completers and non-completers, although they were discussed by many participants in both groups. This counters prior studies in which therapists attributed their patients’ treatment non-completion to life stressors or competing demands (e.g., Eftekhari et al., 2020). This may be in part because as participants noted, those are the “easy” reasons for non-completion to give a provider, whether or not they played a central role. It may also be because while apparent frequency and severity of such barriers did not differ across groups, they did interfere with treatment for some. The current study cannot answer why daily hassles and life stressors contributed to dropout for a subset of veterans but not others. Potential reasons include a deficit in coping or organizational skills to manage competing demands, a lower tolerance for distress caused by multiple stressors, or more tenuous functioning that is perceived as taking priority over therapy. These factors may reflect the concept of treatment “readiness.” Clinicians’ assessments of readiness take into account perceptions of patients’ stability, availability of skills to manage PE/CPT, and motivation to change; lack of readiness is often cited by therapists as a cause of treatment dropout (Cook et al., 2017; Hamblen et al., 2015). It is important to note, however, that these factors were not the most prominent in differentiating level of engagement; thus, despite their prevalence in the literature, they may not be the most effective treatment targets.
With the exception of massed delivery, few interventions have succeeded in boosting rates of PE or CPT completion (Kehle-Forbes & Kimerling, 2017). Training and incentivizing PE/CPT therapists to develop strong treatment-specific rapport and increase the patient-centeredness with which treatment is delivered may be an effective target for engagement interventions. In an uncontrolled study, assessing patients’ intent to attend the following trauma-focused session, with a low score triggering a problem-solving discussion with the patient’s therapist, reduced treatment dropout (Shulman et al., 2019); the study’s authors hypothesized the intervention’s effect was due to increased adaptation. Our results also suggest that engaging the full mental health treatment team (e.g., psychiatrists, case managers) in the goal of PE/CPT completion, perhaps through planned outreach or brief contacts after early treatment sessions, could reduce dropout rates. In addition to directly increasing veterans’ motivation to complete treatment, such intervention may buffer against negative effects of other barriers to completion. Given long-standing concerns about potential negative effects of sedatives on PTSD treatment mechanisms, future studies evaluating medication management as a strategy for increasing engagement must closely monitor for unintended consequences, including reduced treatment effectiveness. Reducing the feared negative impact of PE/CPT participation on functioning may also be a worthwhile treatment target. Using a case-formulation approach to assess, monitor, and address functional concerns during the course of trauma-focused therapy may meet this goal; such a case-formulation approach for CPT has been recently detailed by Galovski and colleagues (2020) and is currently under study for its impact on functioning, PTSD, and retention. The current study’s findings also suggest that engagement interventions applied through the full length of PE/CPT may be needed, in contrast to the majority of previously tested engagement interventions that have focused on adding material (e.g., motivational interviewing, readiness groups) prior to the start of PE/CPT (Kehle-Forbes & Kimerling, 2017). Barriers to completion were frequently not evident to veterans at treatment outset, but rather emerged as veterans engaged with the treatment content. Future studies should also examine the degree to which the current study’s findings apply to engagement in episodic treatments for other mental health diagnoses; while identified themes were PTSD-specific, many may be generalizable across cognitive-behavioral protocols. Finally, in evaluating engagement interventions, it will be imperative to study symptom improvement and other patient-centered outcomes, not only treatment completion. In the current study, treatment completers had a wide range of post-treatment PTSD severity scores and a majority continued to screen positive following treatment.
4. Conclusion
We conducted the first national qualitative study comparing the experiences of veterans who did and did not complete outpatient PE and CPT. Differences between the two groups emerged in the specific type of support provided by therapists and other members of the care team, flexibility with which the protocol was delivered, and veteran attributions and worries throughout treatment. Our findings point toward several promising, potentially modifiable targets that may improve the effectiveness of PE and CPT engagement interventions.
Supplementary Material
Acknowledgments
Dr. Valenstein-Mah is now at Lyra Health, Burlingame, CA; Ms. Lyon is now at University of Missouri – Kansas City. This material is based upon work supported by a grant from the United States Department of Veterans Affairs, Health Services Research & Development (IIR14-030). We thank Sean Nugent & Ann Bangerter for their assistance with this project. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. Correspondence concerning this article should be addressed to Shannon M. Kehle-Forbes, Minneapolis VA Medical Center, One Veterans Drive, Minneapolis, MN 55417. Shannon.Kehle-Forbes@va.gov.
Footnotes
Declaration of competing interest
Dr. Foa receives royalties from the sale of Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences Therapist Guide and Reclaiming your Life from a Traumatic Experience Workbook by Oxford University Press. Dr. Chard receives royalties from the sale of Cognitive Processing Therapy for PTSD: A Comprehensive Manual by Guilford Press. No other authors report conflicts of interest.
CRediT authorship contribution statement
Shannon M. Kehle-Forbes: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Funding acquisition. Princess E. Ackland: Formal analysis, Investigation, Writing – review & editing. Michele R. Spoont: Conceptualization, Formal analysis, Writing – review & editing. Laura A. Meis: Formal analysis, Investigation, Writing – review & editing. Robert J. Orazem: Formal analysis, Investigation, Writing – review & editing. Alexandra Lyon: Formal analysis, Project administration. Helen R. Valenstein-Mah: Formal analysis, Writing – review & editing. Paula P. Schnurr: Conceptualization, Writing – review & editing. Susan L. Zickmund: Methodology, Writing – review & editing. Edna B. Foa: Conceptualization, Writing – review & editing. Kathleen M. Chard: Conceptualization, Writing – review & editing. Elizabeth Alpert: Writing – original draft, Visualization. Melissa A. Polusny: Conceptualization, Writing – review & editing.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.brat.2022.104123.
References
- Ackerman SJ, & Hilsenroth MJ (2001). A review of therapist characteristics and techniques negatively impacting the therapeutic alliance. Psychotherapy: Theory, Research, Practice, Training, 38(2), 171–185. 10.1037/0033-3204.38.2.171 [DOI] [Google Scholar]
- Ackerman SJ, & Hilsenroth MJ (2003). A review of therapist characteristics and techniques positively impacting the therapeutic alliance. Clinical Psychology Review, 23(1), 1–33. 10.1016/S0272-7358(02)00146-0 [DOI] [PubMed] [Google Scholar]
- Ajzen I (1985). From intentions to actions: A theory of planned behavior. In Kuhl J, & Beckmann J (Eds.), Action-control: From cognition to behavior (pp. 11–39). Springer. [Google Scholar]
- Bandura A (2004). Health promotion by social cognitive means. Health Education & Behavior, 31(2), 143–164. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Berke D, Kline N, Wachen J, McLean C, Yarvis J, Mintz J, Young-McCaughan S, Peterson A, Foa E, Resick P, & Litz B (2019). Predictors of attendance and dropout in three randomized controlled trials of PTSD treatment for active duty service members. Behaviour Research and Therapy, 118, 7–17. 10.1016/j.brat.2019.03.003 [DOI] [PubMed] [Google Scholar]
- Bryan C, Leifker F, Rozek D, Bryan A, Reynolds M, Oakey D, & Roberge E (2018). Examining the effectiveness of an intensive, 2-week treatment program for military personnel and veterans with PTSD: Results of a pilot, open-label, prospective cohort trial. Journal of Clinical Psychology, 74(12), 2070–2081. 10.1002/jclp.22651 [DOI] [PubMed] [Google Scholar]
- Chu BC, & Kendall PC (2009). Therapist responsiveness to child engagement: Flexibility within manual-based CBT for anxious youth. Journal of Clinical Psychology, 65(7), 736–754. 10.1002/jclp.20582 [DOI] [PubMed] [Google Scholar]
- Cook JM, Simiola V, Hamblen JL, Bernardy N, & Schnurr PP (2017). The influence of patient readiness on implementation of evidence-based PTSD treatments in Veterans Affairs residential programs. Psychological Trauma: Theory, Research, Practice, and Policy, 9(Suppl 1), 51–58. 10.1037/tra0000162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper AA, Kline AC, Baier AL, & Feeny NC (2018). Rethinking research on prediction and prevention of psychotherapy dropout: A mechanism-oriented approach. Behavior modification. 10.1177/0145445518792251. [DOI] [PubMed] [Google Scholar]
- Eftekhari A, Crowley J, Mackintosh M, & Rosen C (2020). Predicting treatment dropout among veterans receiving prolonged exposure therapy. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 405–412. 10.1037/tra0000484 [DOI] [PubMed] [Google Scholar]
- Fernandez E, Salem D, Swift JK, & Ramtahal N (2015). Meta-analysis of dropout from cognitive behavioral therapy: Magnitude, timing, and moderators. Journal of Consulting and Clinical Psychology, 83(6), 1108–1122. 10.1037/ccp0000044 [DOI] [PubMed] [Google Scholar]
- Foa E, McLean C, Zang Y, Rosenfield D, Yadin E, Yarvis J, Mintz J, Young-McCaughan S, Borah E, Dondanville K, Fina B, Hall-Clark B, Lichner T, Litz BT, Roache J, Wright E, & Peterson A (2018). Effect of prolonged exposure therapy delivered over 2 Weeks vs 8 Weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. for the STRONG STAR Consortium JAMA, 319(4), 354. 10.1001/jama.2017.21242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Blain LM, Mott JM, Elwood L, & Houle T (2012). Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology, 80(6), 968–981. 10.1037/a0030600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia HA, Kelley LP, Rentz TO, & Lee S (2011). Pretreatment predictors of dropout from cognitive behavioral therapy for PTSD in Iraq and Afghanistan war veterans. Psychological Services, 8(1), 1–11. 10.1037/a0022705 [DOI] [Google Scholar]
- Goetter E, Bui E, Ojserkis R, Zakarian R, Brendel R, & Simon N (2015). A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans: Dropout from PTSD treatment in OEF/OIF veterans. Journal of Traumatic Stress, 28(5), 401–409. 10.1002/jts.22038 [DOI] [PubMed] [Google Scholar]
- Gros DF, Yoder M, Tuerk PW, Lozano BE, & Acierno R (2011). Exposure therapy for PTSD delivered to veterans via telehealth. Behavior Therapy, 42(2), 276–283. 10.1016/j.beth.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Grubbs K, Fortney J, Pyne J, Hudson T, Moore W, Custer P, Schneider R, & Schnurr PP (2015). Predictors of initiation and engagement of cognitive processing therapy among veterans with PTSD enrolled in collaborative care: Predictors of CPT use in TOP. Journal of Traumatic Stress, 28(6), 580–584. 10.1002/jts.22049 [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, & Johnson L (2006). How many interviews are enough?: An experiment with data saturation and variability. Field Methods, 18(1), 59–82. 10.1177/1525822X05279903 [DOI] [Google Scholar]
- Gutner CA, Gallagher MW, Baker AS, Sloan DM, & Resick PA (2016). Time course of treatment dropout in cognitive–behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 115–121. 10.1037/tra0000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale AC, Bohnert KM, Ganoczy D, & Sripada RK (2019). Predictors of treatment adequacy during evidence-based psychotherapy for PTSD. Psychiatric Services, 70(5), 367–373. 10.1176/appi.ps.201800361 [DOI] [PubMed] [Google Scholar]
- Hamblen JL, Bernardy NC, Sherrieb K, Norris FH, Cook JM, Louis CA, & Schnurr PP (2015). VA PTSD clinic director perspectives: How perceptions of readiness influence delivery of evidence-based PTSD treatment. Professional Psychology: Research and Practice, 46(2), 90–96. 10.1037/a0038535 [DOI] [Google Scholar]
- Held P, Klassen B, Boley R, Wiltsey Stirman S, Smith D, Brennan M, Van Horn R, Pollack M, Karnik N, & Zalta A (2020). Feasibility of a 3-week intensive treatment program for service members and veterans with PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 422–430. 10.1037/tra0000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holdsworth E, Bowen E, Brown S, & Howat D (2014). Client engagement in psychotherapeutic treatment and associations with client characteristics, therapist characteristics, and treatment factors. Clinical Psychology Review, 34(5), 428–450. 10.1016/j.cpr.2014.06.004 [DOI] [PubMed] [Google Scholar]
- Holmes S, Johnson C, Suvak M, Sijercic I, Monson C, & Wiltsey Stirman S (2019). Examining patterns of dose response for clients who do and do not complete cognitive processing therapy. Journal of Anxiety Disorders, 68, Article 102120. 10.1016/j.janxdis.2019.102120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, Kendall PC, Chu BC, Gosch E, Martin E, Taylor A, & Knight A (2014). Child involvement, alliance, and therapist flexibility: Process variables in cognitive-behavioural therapy for anxiety disorders in childhood. Behaviour Research and Therapy, 52, 1–8. 10.1016/j.brat.2013.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hundt N, Barrera T, Arney J, & Stanley M (2017). It’s worth it in the end”: Veterans’ experiences in prolonged exposure and cognitive processing therapy. Cognitive and Behavioral Practice, 24(1), 50–57. 10.1016/j.cbpra.2016.02.003 [DOI] [Google Scholar]
- Hundt N, Ecker A, Thompson K, Helm A, Smith T, Stanley M, & Cully J (2018). It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychological Services. 10.1037/ser0000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlin BE, & Cross G (2014). From the laboratory to the therapy room: National dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. American Psychologist, 69(1), 19–33. 10.1037/a0033888 [DOI] [PubMed] [Google Scholar]
- Kehle-Forbes SM, & Kimerling R (2017). Patient engagement in PTSD treatment. PTSD Research Quarterly, 28(3). https://www.ptsd.va.gov/publications/rq_docs/V28N3.pdf. [Google Scholar]
- Kehle-Forbes SM, Meis LA, Spoont MR, & Polusny MA (2016). Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 8 (1), 107–114. 10.1037/tra0000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller SM, Feeny NC, & Zoellner LA (2014). Depression sudden gains and transient depression spikes during treatment for PTSD. Journal of Consulting and Clinical Psychology, 82(1), 102–111. 10.1037/a0035286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, & Frank HE (2018). Implementing evidence-based treatment protocols: Flexibility within fidelity. Clinical Psychology: Science and Practice, 25(4), Article e12271. 10.1111/cpsp.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen S, Mackintosh M, La Bash H, Evans W, Suvak M, Shields N, Lane J, Sijercic I, Monson C, & Wiltsey Stirman S (2020). Temporary PTSD symptom increases among individuals receiving CPT in a hybrid effectiveness-implementation trial: Potential predictors and association with overall symptom change trajectory. Psychological Trauma: Theory, Research, Practice, and Policy.. 10.1037/tra0000545 [DOI] [PubMed] [Google Scholar]
- Lewis C, Roberts N, Gibson S, & Bisson J (2020). Dropout from psychological therapies for PTSD in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), Article 1709709. 10.1080/20008198.2019.1709709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Li Y, Madden E, Seal KH, Neylan TC, Patterson OV, DuVall SL, Lujan C, & Shiner B (2019). Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Research, 274, 112–128. 10.1016/j.psychres.2019.02.027 [DOI] [PubMed] [Google Scholar]
- Marques L, Valentine S, Kaysen D, Mackintosh M, Dixon De Silva L, Ahles E, Youn SJ, Shtasel D, Simon N, & Wiltsey-Stirman S (2019). Provider fidelity and modifications to cognitive processing therapy in a diverse community health clinic. Journal of Consulting and Clinical Psychology, 87(4), 357–369. 10.1037/ccp0000384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meis L, Noorbaloochi S, Hagel Campbell E, Erbes C, Polusny M, Velasquez T, Bangerter A, Cutting A, Eftekhari A, Rosen C, Tuerk P, Burmeister L, & Spoont M (2019). Sticking it out in trauma-focused treatment for PTSD: It takes a village. Journal of Consulting and Clinical Psychology, 87(3), 246–256. 10.1037/ccp0000386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton M (2002). Qualitative research & evaluation methods (3rd ed.). Sage Publications. [Google Scholar]
- Rosen C, Matthieu M, Wiltsey Stirman S, Cook J, Landes S, Bernardy N, Chard K, Crowley J, Eftekhari A, Finley E, Hamblen J, Harik J, Kehle-Forbes S, Meis L, Osei-Bonsu P, Rodriguez A, Ruggiero K, Ruzek J, Smith B, & Watts BV (2016). A review of studies on the system-wide implementation of evidence-based psychotherapies for posttraumatic stress disorder in the veterans health administration. Administration and Policy in Mental Health and Mental Health Services Research, 43(6), 957–977. 10.1007/s10488-016-0755-0 [DOI] [PubMed] [Google Scholar]
- Sayer NA, Friedemann-Sanchez G, Spoont M, Murdoch M, Parker LE, Chiros C, & Rosenheck R (2009). A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry: Interpersonal and Biological Processes, 72(3), 238–255. 10.1521/psyc.2009.72.3.238 [DOI] [PubMed] [Google Scholar]
- Shulman GP, Buck BE, Gahm GA, Reger GM, & Norr AM (2019). Effectiveness of the intent to complete and intent to attend intervention to predict and prevent posttraumatic stress disorder treatment drop out among soldiers. Journal of Traumatic Stress, 32(5), 784–790. 10.1002/jts.22427 [DOI] [PubMed] [Google Scholar]
- Sofaer S (1999). Qualitative methods: What are they and why use them? Health Services Research, 34(5 Pt 2), 1101–1118. [PMC free article] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, & Marmar CR (2020). First-line psychotherapies for military-related PTSD. JAMA, 323(7), 656. 10.1001/jama.2019.20825 [DOI] [PubMed] [Google Scholar]
- Szafranski D, Smith B, Gros D, & Resick P (2017). High rates of PTSD treatment dropout: A possible red herring? Journal of Anxiety Disorders, 47, 91–98. 10.1016/j.janxdis.2017.01.002. [DOI] [PubMed] [Google Scholar]
- Youn S, Mackintosh M-A, Wiltsey Stirman S, Patrick KA, Aguilar Silvan Y, Bartuska AD, Shtasel DL, & Marques L (2019). Client-level predictors of treatment engagement, outcome and dropout: Moving beyond demographics. General Psychiatry, 32(6), Article e100153. 10.1136/gpsych-2019-100153 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


