Abstract
Complex periprosthetic fractures may occur with existing ipsilateral hip and knee implants. These cases are challenging with few options. We report on a custom coupler used to connect a hinged distal femoral replacement to an existing revision hip stem. This option was preferred to a total replacement of the femur. The custom coupler maintained the anatomic attachments of the proximal femur, preserved abductor strength during ambulation, and mitigated the morbidity which may arise from a total femur replacement. At 15 months postoperatively, the patient reported no pain, did not demonstrate an antalgic gait pattern, and had satisfactory range of motion at the hip and knee. The literature displays clinical and biomechanical efficacy for coupling devices although complications and device failure are quite variable.
Keywords: connector, coupler, distal femur replacement, femoral sleeve, periprosthetic fracture
Introduction
Complex periprosthetic fractures are becoming more common as the number of primary total joint cases is increasing in an aging population. These fractures often occur in elderly patients who have the additional challenges of reduced bone stock, osteopenia, extensive surgical history, and comorbidities. Treatment options include prosthesis revision with potential coaptation of the existing components, femoral replacement with a mega prosthesis, or amputation. Salvage to a total femur is a complex and challenging procedure with substantial morbidity [1]. The difficulty in maintaining ligament attachment to a total femur increases ambulatory dysfunction and gait disturbances in a population that already has limited mobility. Open reduction internal fixation is fraught with failure, has a high complication rate, and may require extended periods of immobility. The goal of surgical management for complex periprosthetic fractures is to provide a stable lower extremity that will allow early mobilization. The invasiveness of a procedure can be predictive for postoperative complications. This consideration is a critical component of the treatment decision due to the physiologic fragility which is common in this patient population.
We report on a custom coupler used to connect a hinged distal femoral replacement (DFR) to an existing revision hip stem. This procedure was indicated following nonunion of a distal periprosthetic supracondylar fracture. The goal of utilizing the custom coupler was to maintain the anatomic attachments of the proximal femur, to preserve abductor strength during ambulation, and to mitigate the morbidity that may arise from a total femur replacement. Following the case report, we review the literature for cases that utilized a coupling device for hip and knee prostheses. Written informed consent was obtained from the patient for the publication of this case report.
Case history
A 68-year-old female with a past medical history of rheumatoid arthritis and existing left-sided total hip and total knee prostheses sustained a fall while on a cruise. Investigation revealed a Vancouver C supracondylar fracture of the left distal femur with intercondylar extension and fractures of the contralateral proximal humerus and olecranon (Fig. 1). The patient had a previous periprosthetic fracture of the proximal femur, treated with cerclage wiring, strut grafting, and retention of the prosthesis. The supracondylar fracture was treated with open reduction internal fixation with a lateral locking plate and intramedullary rod. The locking plate was utilized to provide increased stability and to mitigate the stress concentration created by the proximity of the tip of the nail to the tip of the proximal prosthesis stem. At 3 months postoperatively, the patient was noted to have complete failure of the hardware with breakage of the plate and listing of the screws. This was consistent with nonunion. There was no evidence of loosening of the proximal femoral stem, and all proximal attachments were intact with a good functioning abductor mechanism. Thus, the treatment objective was to “couple” the distal revision implant with the revision femoral stem, creating a total femur equivalent. The proximal portion of the coupler consisted of a hollowed-out cylinder into which the revision stem was cemented. The distal portion maintained the standard connection to a DFR (Zimmer Biomet, Warsaw, IN). Plans were made for revision surgery.
Figure 1.
Anteroposterior radiograph of bilateral femurs with left-sided periprosthetic fracture of the distal femur.
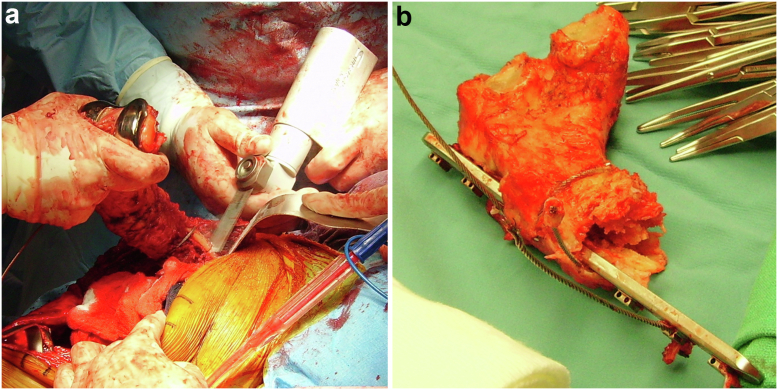
An anterior extensile approach to the knee was performed through a medial parapatellar incision. Broken hardware and screws were removed. The distal femur was resected en bloc (Fig. 2). The distal femoral cortex was removed to expose 80 mm of the distal portion of the revision femoral stem. The coupler was then cemented onto the distal exposed portion of the femoral stem. Distally the coupler was mated to a DFR in the usual fashion (Fig. 3).
Figure 2.
Osteotomy (a) and removal (b) of the distal femur nonunion.
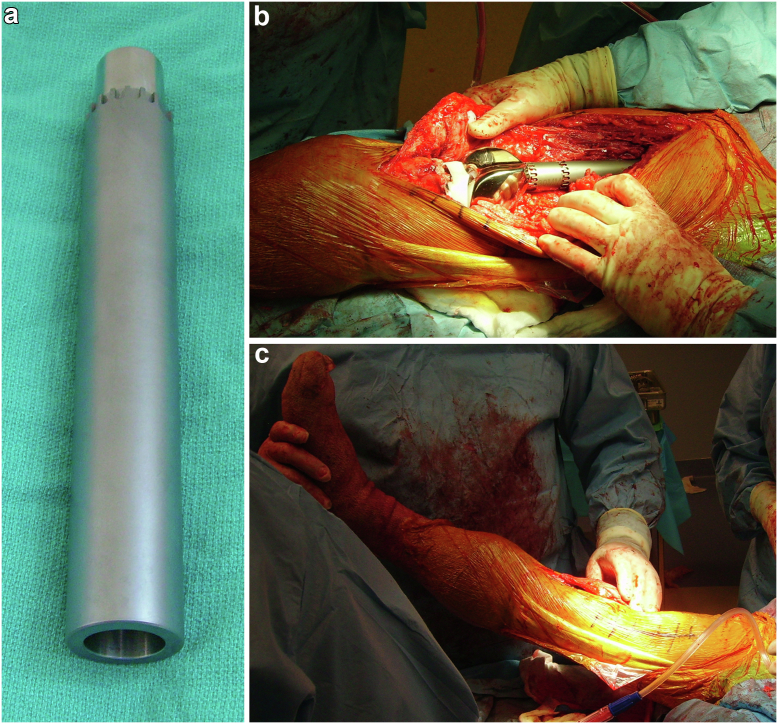
Figure 3.
The custom coupler (a) was cemented into the proximal femur stem and fixed into the distal femur replacement (b and c).
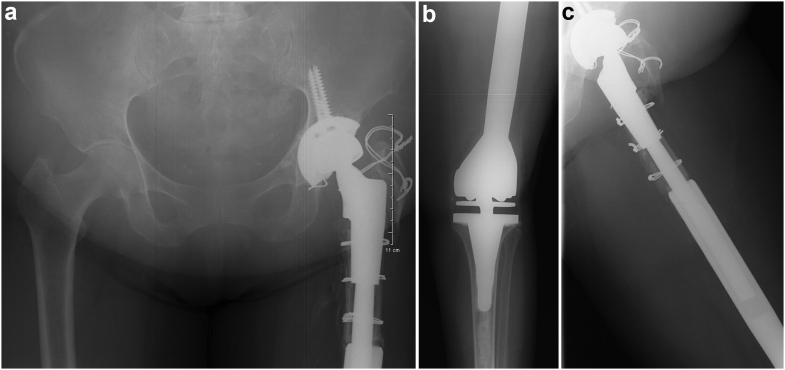
The patient demonstrated satisfactory wound healing with no evidence of infection during early follow-ups, and there was consistent progress in ambulation (Fig. 4). At 15 months postoperatively, the patient reported no pain and was satisfied with the outcome. The patient did not demonstrate an antalgic gait pattern and had satisfactory range of motion at the hip and knee. Computed tomography scan was used to evaluate bilateral limb lengths. The operative (left) leg measured 75.3 cm, and the contralateral (right) leg measured 74.4 cm. At 31 months of follow-up, the patient maintained satisfactory ambulation with a knee arc of motion of 95 degrees and no reported complications.
Figure 4.
Postoperative anteroposterior radiographs of the pelvis (a), left knee (b), and left hip (c) with a custom device coupling the existent proximal femur stem into the distal femur replacement.
Discussion
Complex periprosthetic fractures in the presence of revision implants present unique challenges. The hip and knee components create significant difficulties in achieving union of the fracture. Fixation options are limited due to the reduced bone stock and cortical thinning, which can further compromise fixation and healing. Indeed, these cases are rare, but there is reasonable expectation for increasing frequency due to the projections for increasing rates of primary hip and knee replacement into the 2030s [2,3].
Distal femur replacement has been described as treatment for acute periprosthetic supracondylar fractures and for nonunion of periprosthetic supracondylar fractures [4]. Indications for DFR include the lack of available bone for revision arthroplasty and reduced bone quality, which precludes internal fixation. Furthermore, DFR allows early postoperative mobilization which is critical for mitigating the common sequelae of a surgery. This advantage may be even more pronounced in the elderly comorbid population in which this injury is most common. A recent multicenter study reported on DFR as the treatment for acute fractures, fracture nonunion, and periprosthetic fractures (N = 88) [4]. Nearly all patients in the series were allowed weight-bearing as tolerated immediately following the surgery. Results demonstrated low rates of reoperation (8%), which the authors attribute to early mobilization.
Salvage of the femur with DFR provides advantages compared to total replacement of the femur including retention of the abductor mechanism and proximal ligament attachments that facilitate optimal gait patterns. The surgical approach for total replacement of the femur is more invasive, which increases the risk of blood loss, infection, and postoperative morbidity [1]. Additionally, there is potential for a longer period of postoperative immobilization with total replacement of the femur. DFR with a coupler does require a more time-intensive planning and manufacturing phase; therefore, patient’s condition must be amenable to conservative management during this process.
Grosso et al. reported on 2 cases that utilized a coupling device to connect a DFR to the existing hip prostheses [5] (Table 1). The first case had primary total hip and knee prostheses and sustained a periprosthetic supracondylar fracture that did not unite following internal fixation with a lateral plate. At 2 years postoperatively, the patient ambulated independently. The second case had revision total hip and knee prostheses and sustained a periprosthetic supracondylar fracture that failed to unite following strut grafting and cables. A secondary procedure was required for polyethylene exchange and irrigation and debridement for pretibial abscess. At nearly 1 year postoperatively, the patient was ambulating with support. Both cases utilized a coupling device that was manufactured into the DFR; one of which was designed with a vent hole for cementation. The authors did not detail the rationale for designing 1 component without the vent hole but did surmise that this feature may not be necessary given the short length of the coupler and the ability for cement to release from the top.
Table 1.
Literature review for coupling devices across retrospective series and case reports.
| Study | N | Fixation to prosthesis | Device failure | Revision/reoperation | Infection | Follow-up | Clinical outcomes |
|---|---|---|---|---|---|---|---|
| Case series | |||||||
| Abdelaziz, 2019 | 26 | Cement fixation (2-piece sleeve [+] dual screws) | 21.7% | 30.7% | 13% (PJI) | 48.5 mo | Mean knee flexion 95°, mean Knee Society Score 42.5 (N = 8) |
| Patel, 2014 | 15 | Cement | 6.7% | 6.7% | 6.7% (superficial) | 5.3 y | 93% Ambulatory |
| Citak, 2013 | 4 | Cement and dual screw | 0% | 25% (aseptic loosening) | 0% | 8 y | NR |
| Peters, 2006 | 23 | Press-fit | 0% | 27% | 16.6% (deep sepsis) | 36 mo | Mean knee flexion 95° (N = 16), 91% were ambulatory |
| Tillman, 2006 | 5 | Cement | 0% | 0% | 0% | 47 mo | 80% were ambulatory, 1 case of radiographic loosening and osteolysis |
| Case reports | |||||||
| Sim, 2019 | 1 | Cement proximally, dual screws distally | None | None | None | 14 mo | Bony union |
| Grosso, 2013 | 1 | Cement | None | None | None | 22 mo | Independent supported ambulation |
| 1 | None | Irrigation and debridement with polyethylene exchange | Yes (abscess) | 14 mo | Independent supported ambulation | ||
| Osagie, 2011 | 1 | Cement and screw | None | None | None | 2 y | Knee flexion 120°, hip flexion 95° |
| Walker, 1999 | 1 | Cement | None | None | None | 3 y | Satisfactory function |
| 1 | None | None | None | 15 mo | Satisfactory function | ||
| 1 | None | None | None | 4 y | Ambulation without support, knee flexion 95° | ||
NR, not reported; PJI, periprosthetic joint infection.
Sim et al. reported on a custom coupler to connect a long-stem femoral component to a knee arthrodesis nail following primary total knee arthroplasty failure with osteolysis and gross instability [6]. Proximally, the coupler was cemented to the femoral stem, and distally 2 screws fixated the coupler into the arthrodesis nail. At 14 months postoperatively, there was radiographic evidence of fusion, and the patient was ambulatory without pain.
The biomechanical efficacy of interprosthetic couplers has been previously investigated. Weiser et al. tested a 2-piece coupler that was cemented into the proximal and distal stems and then connected with 2 screws [7]. Their results demonstrated ample stability of the prosthetic coupler, with prosthesis diameter being an important consideration for construct stiffness. Walker et al. reported that compressive stress on the cement mantle was a greater concern than tensile stresses on the interface [8]. The authors provide ideal values for the stem diameter (14 mm), cement mantle (4 mm), and thickness of the implant wall (1 mm).
To our knowledge, the largest literature report on coupling devices is a follow-up on 23 patients across 20 years by Abdelaziz et al. [9]. The mean implant survival was 4.6 years. Mechanical failure due to fracture of the proximal stem occurred in 21.7% of cases. The authors reported that the mean stem overlap inside the coupling sleeve was 3 cm less in the cases with mechanical failure (6.25 cm) than that in cases that did not fail (9.6 cm). Although there are no existing data for the optimal length of stem coverage inside a coupler, this determination highlights the importance of preoperative planning and design to ensure adequate overlap of the existing stem. There were no hip dislocations, which suggests the addition of a coupler may not negatively impact hip stability.
Accurate measurement is a critical step in the custom manufacturing process. The surgeon and design team must determine the size of the existing stem, the required space for cement mantle, and the thickness of the coupler walls. These values will coalesce to determine the diameter of the device. Additionally, measurement of the contralateral limb length is important for the design and implantation process to ensure length equivalency.
Summary
In conclusion, utilization of a custom coupling device is a reasonable treatment option that allows salvage of the femur and retention of a proximal hip prosthesis following nonunion of a periprosthetic supracondylar fracture. The patient’s condition must be amenable to conservative management during the design and manufacturing process. Treatment considerations for these cases include the invasiveness of the surgery, the quality and quantity of the available bone, and the capacity for early postoperative mobilization which can mitigate common sequelae of a surgery. The literature displays clinical and biomechanical efficacy for coupling devices although complications and device failure are quite variable.
Conflicts of interest
A.C. discloses consulting relationship with Exactech and royalties from Arthrex. The other 2 authors declare no potential conflicts of interest.
For full disclosure statements, refer to https://doi.org/10.1016/j.artd.2022.101089.
Informed patient consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Appendix A. Supplementary Data
References
- 1.DeRogatis M.J., Issack P.S. Total femoral replacement as a salvage operation for the treatment of massive femoral bone loss during revision total hip arthroplasty. JBJS Rev. 2018;6:e9. doi: 10.2106/JBJS.RVW.17.00195. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 4.Stancil R., Romm J., Lack W., Bohnenkamp F., Sems S., Cross W., et al. Distal femoral replacement for fractures allows for early mobilization with low complication rates: a multicenter review. J Knee Surg. 2021 doi: 10.1055/s-0041-1731353. 10.1055/s-0041-1731353. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Grosso M.J., Lipman J., Bostrom M.P. Coupling device and distal femoral replacement for periprosthetic supracondylar femur fractures with an ipsilateral total knee and hip replacement. HSS J. 2014;10:68–72. doi: 10.1007/s11420-013-9360-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sim J.A., Lee B.K., Kwak J.H., Moon S.H. Knee arthrodesis in failed total knee arthroplasty with severe osteolysis and ipsilateral long-stem total hip arthroplasty. J Arthroplasty. 2009;24:322.e19–322.e22. doi: 10.1016/j.arth.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Weiser L., Korecki M.A., Sellenschloh K., Fensky F., Püschel K., Morlock M.M., et al. Interposition sleeve as treatment option for interprosthetic fractures of the femur: a biomechanical in vitro assessment. Int Orthop. 2015;39:1743–1747. doi: 10.1007/s00264-015-2788-5. [DOI] [PubMed] [Google Scholar]
- 8.Walker P.S., Yoon W.W., Cannon S.R., Bentley G., Muirhead-Allwood S.K. Design and application of combined hip-knee intramedullary joint replacements. J Arthroplasty. 1999;14:945–951. doi: 10.1016/s0883-5403(99)90008-6. [DOI] [PubMed] [Google Scholar]
- 9.Abdelaziz H., Saleri S., Mau H., Sandiford N.A., Lausmann C., Zahar A., et al. Interprosthetic femoral sleeves in revision arthroplasty: a 20-year experience. J Arthroplasty. 2019;34:1423–1429. doi: 10.1016/j.arth.2019.02.055. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.