Abstract
Objective
To explore trends in blood pressure (BP) control before and during the COVID-19 pandemic.
Patients and Methods
Health systems participating in the National Patient-Centered Clinical Research Network (PCORnet) Blood Pressure Control Laboratory Surveillance System responded to data queries, producing 9 BP control metrics. Averages of the BP control metrics (weighted by numbers of observations in each health system) were calculated and compared between two 1-year measurement periods (January 1, 2019, through December 31, 2019, and January 1, 2020, through December 31, 2020).
Results
Among 1,770,547 hypertensive persons in 2019, BP control to <140/<90 mm Hg varied across 24 health systems (range, 46%-74%). Reduced BP control occurred in most health systems with onset of the COVID-19 pandemic; the weighted average BP control was 60.5% in 2019 and 53.3% in 2020. Reductions were also evident for BP control to <130/<80 mm Hg (29.9% in 2019 and 25.4% in 2020) and improvement in BP (reduction of 10 mm Hg in systolic BP or achievement of systolic BP <140 mm Hg; 29.7% in 2019 and 23.8% in 2020). Two BP control process metrics exhibited pandemic-associated disruption: repeat visit in 4 weeks after a visit with uncontrolled hypertension (36.7% in 2019 and 31.7% in 2020) and prescription of fixed-dose combination medications among those with 2 or more drug classes (24.6% in 2019 and 21.5% in 2020).
Conclusion
BP control decreased substantially during the COVID-19 pandemic, with a corresponding reduction in follow-up health care visits among persons with uncontrolled hypertension. It is unclear whether the observed decline in BP control during the pandemic will contribute to future cardiovascular events.
The COVID-19 pandemic has resulted in immense disruptions in health care services. Dramatic early declines in in-person visits, and in particular, preventive and elective care visits, were observed in the first months of the COVID-19 pandemic, accompanied by increases in telehealth use.1, 2, 3, 4 Between March and April 2020, a 67% decline in ambulatory care, including emergency department, office, and urgent care visits; behavioral health services; and 3 types of preventive services (colonoscopies, mammograms, and contraception counseling or human immunodeficiency virus screening), was observed using outpatient claims data capturing more than 14.5 million US adults.1 Although ambulatory care rates returned to 97% of expected by the end of 2020, the rate of increase in use of ambulatory care services was lower for persons with Medicaid or Medicare-Medicaid dual eligibility,1 suggesting socioeconomic disparities in access to and/or utilization of care during the COVID-19 pandemic.
In a nationally representative survey of more than 23,000 Medicare beneficiaries in June 2020, nearly one-quarter of patients reported forgone medical care because of COVID-19, with the most common reasons being closure of physicians’ offices or reduced availability of appointments.5 In smaller web-based surveys of US adults, more than 40% of respondents reported having either delayed or forgone medical care,6 , 7 most commonly dental, preventive, diagnostic, and checkup services.5 , 7 In addition, 12% reported having avoided urgent or emergency care, with younger persons, Black persons, Hispanic persons, persons with underlying medical conditions, persons with disabilities, and unpaid caregivers more likely to report avoiding urgent or emergency care.6
These aforementioned disruptions in health care may have affected the management of chronic medical conditions, including hypertension, the leading cause of cardiovascular morbidity and mortality in the United States.8 , 9 Increases in systolic blood pressure (SBP) and diastolic BP have been observed in the United States after the onset of the COVID-19 pandemic compared with prepandemic periods.10 , 11 However, trends in additional measures related to BP management and control, as well as differences across health systems or by patient characteristics, are not well described. In addition, whether the racial/ethnic disparities in BP control12 have persisted or widened as a result of increases in telehealth and barriers to access to care during the COVID-19 pandemic13 is unknown. We aimed to answer these questions, and to test the primary hypotheses that BP control declined and disparities in BP control by race/ethnicity widened during the COVID-19 pandemic, using BP Track, a collaboration of 24 US health systems participating in the National Patient-Centered Clinical Research Network (PCORnet).14 , 15
Methods
Data use agreements with contributing sites prohibit sharing of the data set with external investigators. However, the BP Control Laboratory accepts proposals for collaborative analysis and publications. Proposals are subject to review by the BP Control Laboratory Steering Committee for scientific value, avoidance of overlap with previously approved proposals, compliance with publication policies, and availability of resources for analysis of the data. Interested investigators may contact the corresponding author with inquiries.
BP Track
The BP Control Laboratory Surveillance System (BP Track) uses PCORnet16 for national surveillance of BP control and BP-related quality metrics.14 BP Track includes 27 PCORnet-affiliated health systems across the United States. Each participating health system standardizes their electronic health record data to the PCORnet common data model format, allowing for distributed querying of electronic health record data for research and surveillance.16 Each health system refreshes their data quarterly and submits a data curation query response to the PCORnet Coordinating Center for evaluation of foundational data quality and completeness.17
Participating health systems received repeated queries (quarterly or biannually) for execution against their PCORnet common data model that produced BP control metric results for standardized 1-year measurement periods. The latest query, executed in mid-2021, calculated metrics quarterly for 13 measurement periods from 2017 through 2020 (ie, January 1, 2017, through December 31, 2017; April 1, 2017, through March 31, 2018; January 1, 2020, through December 31, 2020). For each measurement period, patients aged 18 to 85 years with at least 1 clinical encounter and a diagnosis of hypertension (at any time before the measurement period or during the first 6 months of the measurement period) were identified. Patients who received hospice services, were receiving care based on an institutional special needs plan, were residing in a long-term care facility, had end-stage renal disease/dialysis/renal transplantation, or had a pregnancy during the measurement period were excluded, as previously described.15
The queries produced multiple BP control metrics using BP measurements obtained as part of standard clinical care, medication prescribing, and other electronic health record data (Table 1 ).14 , 15 The metrics included 3 quality measures related to BP control and improvement in BP18, 19, 20 and 6 process metrics relevant to clinical management and treatment practices for BP control. Metrics were calculated quarterly to produce a series of thirteen 1-year measurement periods from 2017 to 2020 (Supplemental Figure 1, available online at http://www.mayoclinicproceedings.org). Metrics were estimated overall and by age, sex, and racial/ethnic subgroups for each health system using the following racial/ethnic categories: Hispanic ethnicity (defined as a person of Cuban, Mexican, Puerto Rican, South or Central American, or other Spanish culture or origin; any race), non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and other/multiple/unknown race/ethnicity. Detailed metric definitions have been previously described15 and require assignment of Evaluation and Management Current Procedural Terminology codes for identifying relevant ambulatory encounters such that telehealth and other encounters not using these codes are excluded from consideration. BP Track was approved by the lead site’s institutional review board as a quality improvement research project.
Table 1.
Blood Pressure Control Metric Definitions
| Metric | Definitions | |
|---|---|---|
| BP control (<140/<90 mm Hg) (% of patients) | This overall measure of BP control implements NQF 0018,18 which defines BP control as the percentage of eligible hypertensive patients for whom the BP measurements at their most recent ambulatory care visit were at goal, defined as SBP <140 mm Hg and DBP <90 mm Hg. | |
| BP control to 2017 ACC/AHA Hypertension Clinical Practice Guidelines goal (<130/<80 mm Hg) (% of patients) | This alternative overall measure of BP control is identical to the first metric except that attainment of BP control is defined by SBP <130 mm Hg and DBP <80 mm Hg, as per the goal stated in the 2017 ACC/AHA Hypertension Guidelines.20 Note that while the treatment threshold varies in the Guidelines based on estimated 10-year ASCVD risk, herein the goal of <130/<80 mm Hg is applied to all patients. | |
| Improvement in BP (% of patients) | This overall measure of BP improvement implements CMS065v7,19 which defines BP improvement as either a reduction of 10 mm Hg in SBP or achievement of SBP that is “adequately controlled” (SBP <140 mm Hg) in months 10-12 of the measurement period among hypertensive patients with an SBP not previously controlled. | |
| Confirmatory repeated BP measurement (% of visits) | This process measure is designed to capture the practice of repeating a BP measurement in the same visit when the first measurement in the clinic is high (SBP ≥140 mm Hg or DBP ≥90 mm Hg). | |
| Medication intensification after uncontrolled BP (% of visits) | This process measure captures the proportion of visits where BP is uncontrolled where a BP medication is prescribed that is of a different medication class than had previously been used. Note that this explicitly does not give credit for ordering a simple refill or medication dose increase or for use of a different medication in the same class. | |
| Repeat visit in 4 weeks after uncontrolled BP (% of visits) | This process measure captures the proportion of visits by persons with uncontrolled hypertension that were followed by a subsequent visit within 4 weeks. | |
| Average SBP reduction after medication intensification (mm Hg) | This continuous metric describes the average change in SBP observed between a visit with a medication intensification to the subsequent visit occurring ≥10 days later. | |
| Use of a CCB or thiazide or thiazide-like diuretic among Black patients prescribed ≥1 medication (% of patients) | Use of a CCB or a thiazide or thiazide-like diuretic medication is recommended to treat Black or African American patients as first-line monotherapy due to increased efficacy.20 This metric, which is limited to Black patients with a diagnosis of hypertension prescribed ≥1 medication class, describes the prevalence of those prescribed a CCB or a thiazide or thiazide-like diuretic. | |
| Prescription of fixed-dose combination product among patients prescribed ≥2 classes of medications (% of patients) | Use of fixed-dose combination medications helps with adherence, promotes rational combinations of medications, increases the likelihood of achieving BP control, and is recommended.20 This metric, which is limited to patients taking ≥2 BP medication classes, describes the prevalence of fixed-dose combination medication use. |
ACC/AHA, American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CCB, calcium channel blocker; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Statistical Analysis
BP Track data from each health system were reviewed, compared over time and across repeated queries to identify any potential data quality issues or outliers, and then compiled into an analytic data set. We restricted the present analysis to the 24 health systems that had complete data through the end of 2020 (Supplemental Table 1, available online at http://www.mayoclinicproceedings.org). The academic status (academic, nonacademic, and federally qualified health center) and geographic region (Northeast, Midwest, South, West, and multiple regions) of the 24 health systems were summarized.
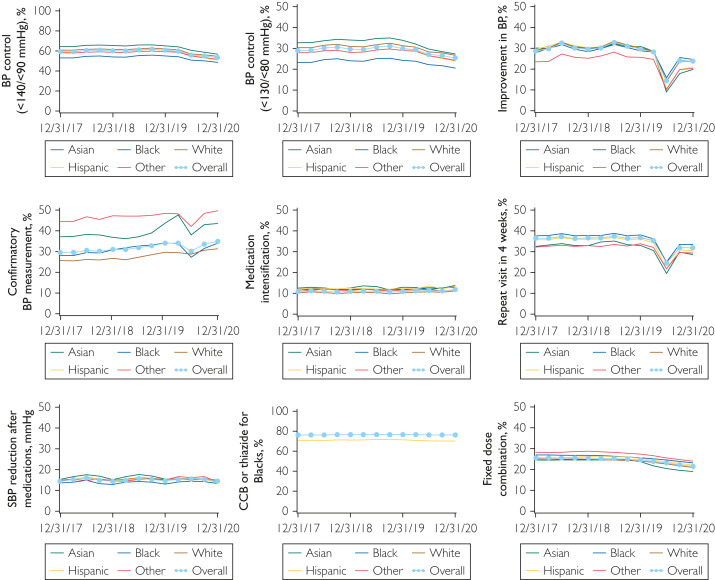
Using data from the entire period (January 1, 2017, through December 31, 2020), trends in each of the 9 BP control metrics were plotted over time. Estimates were plotted for each of the 13 quarterly 1-year measurement periods and labeled on the plot with the end date of the measurement period. For example, measurement period 1 included data from January 1, 2017, through December 31, 2017, and was labeled on the plot as 12/31/17. Lines representing each of the 24 health systems along with a line representing the overall weighted average were plotted. Plots were also constructed summarizing BP control metrics by racial/ethnic group, with lines representing the weighted averages for non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, Hispanic (any race), and other/multiple/unknown racial/ethnic groups. Similarly, plots were constructed summarizing BP control metrics by sex and by age group.
We then conducted a series of statistical analyses using data from 2 comparable 1-year measurement periods (January 1, 2019, through December 31, 2019, and January 1, 2020, through December 31, 2020). For these analyses, we created an expanded data set from the health system– and subgroup-specific summary statistics, creating an observation for each participant-year, each with patient characteristics (age, sex, and race/ethnicity) and binary outcome indicators for patient characteristics and for each BP control metric, summing to the correct totals. We then used a logistic model with robust standard errors, clustered by health system, to generate estimates and conduct a series of hypothesis tests as described later herein.
First, we described characteristics of patients with hypertension, comparing characteristics between the 2 years using χ2 tests from generalized estimating equations logistic (binary factors) or multinomial (multicategory factors) regressions of the factors on year accounting for clustering on health system. For median number of encounters by health system, the P value was obtained using the nonparametric signed rank test to evaluate the difference between totals within health system.
Then, for each of 9 BP control metrics, we estimated the average across the 24 health systems for 2019 and 2020 (weighted by number of observations in each health system), and then calculated a difference between years (2020 – 2019) with corresponding confidence intervals. To obtain P values testing the null hypothesis of no difference between years, we used χ2 tests based on delta method standard errors obtained from the margins procedure to compare the adjusted outcome rates (on the risk difference scale) in 2019 and 2020, accounting for clustering on health system.
Finally, we calculated estimates of differences in each metric between years (2020 – 2019) for subgroups of age, sex, and race/ethnicity and conducted a test of the null hypothesis of no interaction between subgroup and year using a similar procedure as described previously herein. All statistical analyses were conducted using statistical software programs (SAS version 9.4 [SAS Institute Inc] and Stata Statistical Software version 17.0 [StataCorp LP]).
Results
Of the 24 health systems, 10 (42%) were from the Midwest, 6 (25%) from the South, 4 (17%) from the Northeast, and 2 (8%) from the West; the remaining 2 (8%) had locations across multiple regions in the United States. Most were academic health centers (n=18; 75%), with 2 being nonacademic and 4 federally qualified health centers. There were 1,770,547 persons aged 18 to 85 years with hypertension cared for by the 24 health systems in 2019, and 1,726,794 persons with hypertension in 2020 (Table 2 ). The number of ambulatory encounters among these patients decreased approximately 20% from 8.3 million visits in 2019 to 6.6 million visits in 2020 (rate of encounters per person: 4.69 in 2019 and 3.82 in 2020; P<.001). Just more than half of the patients were aged 65 to 85 years, 52% were female, and 68% were non-Hispanic White persons. Nearly two-thirds of patients had stage 1 (BP, 130-139/80-89 mm Hg) or stage 2 (BP, ≥140/90 mm Hg) hypertension based on the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Hypertension Clinical Practice Guidelines classification, although a larger percentage of patients in 2020 were missing BP measurements during the year to categorize stage of hypertension (3% in 2019 and 7% in 2020). Comorbidities were largely similar in the 2019 and 2020 cohorts.
Table 2.
Characteristics of the Patients with Hypertension in 2019 Compared With 2020a
| Characteristic | 2019 | 2020 | P value |
|---|---|---|---|
| Patients with hypertension (No.)b | 1,770,547 | 1,726,794 | -- |
| Encounters (No.)c | 8,295,484 | 6,592,142 | -- |
| Per health system (median [IQR]) | 236,904 (129,212.5-558,980) | 200,575.5 (99,502.5-453,697.5) | <.001 |
| Age (No. [%]) | <.001 | ||
| 18-44 y | 165,782 (9.4) | 159,870 (9.3) | |
| 45-64 y | 707,726 (40.0) | 678,346 (39.3) | |
| 65-85 y | 897,039 (50.7) | 888,578 (51.5) | |
| Sex (No. [%]) | .48 | ||
| Male | 848,107 (47.9) | 828,052 (48.0) | |
| Female | 922,363 (52.1) | 898,655 (52.0) | |
| Other/unknown | 77 (0) | 87 (0) | |
| Race/ethnicity (No. [%]) | .33 | ||
| Non-Hispanic White | 1,206,901 (68.2) | 1,166,537 (67.6) | |
| Non-Hispanic Black | 277,541 (15.7) | 273,065 (15.8) | |
| Non-Hispanic Asian | 44,130 (2.5) | 46,685 (2.7) | |
| Hispanic (any race) | 152,328 (8.6) | 153,163 (8.9) | |
| Other/multiple races/unknown | 89,647 (5.1) | 87,344 (5.1) | |
| Hypertension stage at baseline (No. [%])d | <.001 | ||
| Normal (<120/80 mm Hg) | 287,933 (16.3) | 263,031 (15.2) | |
| Elevated (120-129/80-89 mm Hg) | 260,853 (14.7) | 240,097 (13.9) | |
| Stage 1 (130-139/80-89 mm Hg) | 573,572 (32.4) | 545,310 (31.6) | |
| Stage 2 (≥140/90 mm Hg) | 592,535 (33.5) | 562,603 (32.6) | |
| Missing | 55,654 (3.1) | 115,753 (6.7) | |
| Diabetes (No. [%]) | 499,203 (28.2) | 496,743 (28.8) | .03 |
| Coronary artery disease (No. [%]) | 282,343 (16.0) | 274,626 (15.9) | .78 |
| Heart failure (No. [%]) | 111,656 (6.3) | 112,338 (6.5) | <.001 |
| Depression (No. [%]) | 271,314 (15.3) | 241,173 (14.0) | .32 |
| Chronic obstructive pulmonary disease (No. [%]) | 98,055 (5.5) | 93,463 (5.4) | .01 |
Note: Totals may not sum to 100% due to rounding.
Data are presented as number (%) for categorical variables and median (IQR) for continuous variables. Totals may not add up to 100% exactly due to rounding. IQR, interquartile range.
Includes patients aged 18 to 85 years with at least 1 encounter during the year who had a diagnosis of hypertension at any time before or within the first 6 months of the year. Patients with a pregnancy during the year; who had hospice services; who had diagnoses of end-stage renal disease, dialysis, or renal transplantation; or who were 65 years or older with an Institutional Special Needs Plan or who resided in a long-term care facility were excluded.
Total count of ambulatory visits during the year.
The stage of hypertension was defined using the first blood pressure measurement in the year.
Control of BP (<140/<90 mm Hg) was variable across health systems and ranged between 46% and 74% in 2019 (weighted average, 60.5%) (Table 3 ). BP control was relatively stable within health systems over time before the COVID-19 pandemic (Figure 1 ). Drops in BP control were seen for most but not all health systems in the second quarter of 2020 coinciding with onset of the COVID-19 pandemic. The weighted average BP control in 2020 was 53.3%, and although some health systems saw small increases in BP control in the third and fourth quarters of 2020, BP control did not rebound to prepandemic levels for any of the health systems. Similar observations were seen for BP control to 2017 ACC/AHA Hypertension Clinical Practice Guidelines goal (<130/<80 mm Hg), although the percentage of patients meeting this goal was lower (weighted average, 29.9% in 2019 and 25.4% in 2020; P<.001). The percentage of patients with improvement in BP (reduction of 10 mm Hg in SBP or achievement of SBP <140 mm Hg in patients with previously uncontrolled hypertension) decreased substantially in the second quarter of 2020, with an increase in the third quarter that did not reach prepandemic levels. Improvement in BP control was 29.7% in 2019 and nearly 6% lower in 2020 at 23.8% (P<.001). The proportion of visits with a confirmatory repeated BP measurement did not differ between periods (P=.61).
Table 3.
Weighted Average of Blood Pressure Control Metrics in 2019 Compared With 2020a
| Metric | 2019b | 2020b | Difference (95% CI)c | P value |
|---|---|---|---|---|
| BP control (<140/<90 mm Hg) (% of patients) | 60.5 (45.6-74.3) | 53.3 (32.7-65.7) | –7.2 (–9.0 to –5.4) | <.001 |
| BP control to 2017 Hypertension Clinical Practice Guidelines goal (<130/<80 mm Hg) (% of patients) | 29.9 (21.0-38.2) | 25.4 (14.6-34.9) | –4.6 (–5.4 to –3.7) | <.001 |
| Improvement in BP (reduction of 10 mm Hg in SBP or achievement of SBP <140 mm Hg) (% of patients) | 29.7 (25.1-36.5) | 23.8 (14.3-31.7) | –5.9 (–8.0 to –3.8) | <.001 |
| Confirmatory repeated BP measurement (% of visits) | 34.0 (0-100) | 34.9 (0-100) | 0.8 (–2.5 to 4.1) | .61 |
| Medication intensification after uncontrolled BP (% of visits) | 10.8 (3.4-34.7) | 11.7 (4.2-38.6) | 0.9 (0.5 to 1.4) | <.001 |
| Repeat visit in 4 weeks after uncontrolled BP (% of visits) | 36.7 (15.8-47.0) | 31.7 (10.1-41.5) | –5.1 (–6.0 to –4.1) | <.001 |
| Average SBP reduction after medication intensification (mm Hg) | 14.5 (10.8-16.5) | 14.4 (10.3-17.0) | –0.2 (–0.5 to 0.1) | .61 |
| Use of a CCB or a thiazide or thiazide-like diuretic among Black patients prescribed ≥1 medication (% of patients) | 76.5 (33.2-81.0) | 76.2 (57.9-80.5) | –0.3 (–1.0 to 0.4) | .34 |
| Prescription of fixed-dose combination product among patients prescribed ≥2 classes of medications (% of patients) | 24.6 (14.2-87.0) | 21.5 (12.7-52.6) | –3.0 (–3.5 to –2.5) | <.001 |
BP, blood pressure; CCB, calcium channel blocker; SBP, systolic blood pressure.
Data are presented as weighted averages (range). Weighted averages of health system–specific results were weighted by the total number of observations from each health system meeting eligibility criteria for metric calculation. Range represents the lowest and highest metric result from across the participating health systems.
Adjusted for age, sex, and race/ethnicity.
Figure 1.
Trends in 9 blood pressure (BP) control metrics over time by health system. The 24 light colored lines on each plot correspond to the trend over time in the metric for each participating health system. The bolded line is the weighted average across the 24 health systems. CCB, calcium channel blocker; SBP, systolic blood pressure.
Medication intensification, defined as the percentage of visits by persons with uncontrolled hypertension (BP ≥140/90 mm Hg), where a different class of BP medication was prescribed, increased slightly from 10.8% in 2019 to 11.7% in 2020 (P<.001) (Table 3, Figure 1). However, given fewer encounters in 2020 (Table 2), there were fewer opportunities for medication intensification. Nevertheless, the average SBP reduction obtained after medication intensification was similar in 2019 and 2020 (P=.61). In addition, timely follow-up visits (within 4 weeks) after a visit with uncontrolled hypertension dropped for all health systems at the beginning of the pandemic, and improved but not to prepandemic levels for most health systems in the last 2 quarters of 2020 (36.7% in 2019 and 31.7% in 2020). Prescriptions for fixed-dose combination medications among patients prescribed at least 2 classes of medications decreased (from 24.6% in 2019 to 21.5% in 2020), whereas no difference was observed over time in prescription of calcium channel blockers or thiazide or thiazide-like diuretic medication classes in Black patients (P=.34).
Small differences were observed across age groups for most of the BP control metrics, most notably lower levels of BP control to <130/<80 mm Hg, improvement in BP, and confirmatory BP measurement in the youngest age group (18-44 years) (Supplemental Figure 2, available online at http://www.mayoclinicproceedings.org). However, changes between 2019 and 2020 were similar across age for all BP control metrics except BP control to <140/<90 mm Hg, where a larger drop during the pandemic was observed for patients aged 18 to 44 years (P=.02 for interaction). For all BP control metrics, similar estimates were observed for men and women (Supplemental Figure 3, available online at http://www.mayoclinicproceedings.org). Slightly larger drops in improvement in BP (P=.02 for interaction) and timely follow-up visits (within 4 weeks; P<.001 for interaction) were observed in women.
Differences by racial/ethnic group were observed for most of the BP control metrics (Figure 2 ). BP control to <140/<90 mm Hg and <130/<80 mm Hg was consistently lower in non-Hispanic Black persons, despite a somewhat higher use of follow-up visits within 4 weeks after a visit with uncontrolled hypertension. In addition, non-Hispanic Black persons had the lowest SBP reduction after medication intensification. Persons with other/multiple/unknown race/ethnicity had the lowest percentage improvement in BP, and non-Hispanic Asian persons and those with other/multiple/unknown race/ethnicity had the lowest use of follow-up visits (within 4 weeks) after a visit with uncontrolled hypertension. Differences in the trends over time between 2019 and 2020 were observed for all BP control metrics (P<.05 for interaction for all metrics). Most notably, larger drops in BP control to <140/<90 mm Hg and to <130/<80 mm Hg, and improvement in BP were observed in Hispanic persons and non-Hispanic Asian persons. The difference in BP control to <140/<90 mm Hg between 2019 and 2020 (percentage of patients) was –8.25 in non-Hispanic Asians, –6.11 in non-Hispanic Blacks, –7.11 in non-Hispanic Whites, –9.14 in Hispanics, and –7.67 in persons with other/multiple/unknown race/ethnicity. The difference in improvement in BP between 2019 and 2020 (percentage of patients) was –11.07 in non-Hispanic Asians, –4.90 in non-Hispanic Blacks, –5.69 in non-Hispanic Whites, –8.41 in Hispanics, and –5.45 in persons with other/multiple/unknown race/ethnicity. In addition, larger drops in prescriptions of fixed-dose combination medications were observed in non-Hispanic Asian persons (difference between 2019 and 2020, percentage of patients: –4.61 in non-Hispanic Asians, –2.45 in non-Hispanic Blacks, –3.04 in non-Hispanic Whites, –3.16 in Hispanics, and –3.42 in persons with other/multiple/unknown race/ethnicity).
Figure 2.
Trends in 9 blood pressure (BP) control metrics over time by race/ethnicity. The bolded light blue line is the weighted average across the 24 health systems. CCB, calcium channel blocker; SBP, systolic blood pressure.
Discussion
In this large study including more than 1.7 million patients from 24 US health systems, we observed large variability in BP control across health systems. In 2019, before the COVID-19 pandemic, the weighted average BP control was nonoptimal at 60.5%, but it decreased more than 7 percentage points in 2020. The performance on most BP control process metrics did not decline during the pandemic, except for a large reduction in timely follow-up health care visits among patients with uncontrolled hypertension that declined dramatically at the beginning of the COVID-19 pandemic and improved later in 2020 but not to prepandemic levels. Racial disparities in BP control persisted throughout the pandemic, and Hispanic persons and non-Hispanic Asian persons experienced larger drops in BP control and improvement in BP than persons from the other racial/ethnic groups.
The COVID-19 pandemic resulted in immense disruption in usual health care, including delayed or forgone medical care, which could have affected management of health conditions. In a web-based survey of nearly 5000 persons, by June 30, 2020, 40.9% reported having either delayed or forgone medical care because of concerns about COVID-19, including 31.5% who avoided routine care and 12.0% who avoided urgent or emergency care.6 In a nationally representative survey of more than 23,000 Medicare beneficiaries, 11.5% reported forgone medical care because of COVID-19, with the most common types of forgone services being dental, preventive, and checkup services.5 The rates of forgone medical care declined from 22.4% in June 2020 to 5.2% in April 2021, with the most rapid decline observed in the summer of 2020. Physician-driven factors, such as closed offices, reduced availability of appointments, or other physician priorities or reasons accounted for 70% of foregone medical care, although patient factors, including fear of COVID-19 exposures, also contributed to forgone medical care.
In addition, although increases in telehealth may have offset some of the missed in-person visits, with estimates of approximately two-thirds of the decline in in-person visits offset by telehealth, every state in the United States experienced a drop in total visits during the first months of the pandemic.2 Telehealth was used less frequently in US counties with lower median income, lower population density, and less broadband availability, suggesting that rural and disadvantaged communities may have been disproportionately affected by this shift in care practices.21 Furthermore, in a large academic health system, only 54.4% of patients scheduled for telemedicine visits in primary care and specialty ambulatory clinics completed the visits.22 Patients who were older, Asian race, and non–English speaking were less likely to complete telemedicine visits overall, with lower use of video visits among older patients, females, Black persons, Hispanic persons, and patients with lower household income.
In the present study, the number of ambulatory encounters at the 24 participating health systems decreased approximately 20% in 2020 compared with 2019. In addition, follow-up visits (within 4 weeks) after a visit with uncontrolled hypertension dropped dramatically at the beginning of the pandemic, rebounding in the later half of 2020 but not reaching prepandemic levels. Accompanying the drop in encounters was a substantial decrease in BP control that did not rebound by the end of 2020, with only 53.3% and 25.4% of patients achieving BP control to <140/<90 mm Hg and <130/<80 mm Hg, respectively, in 2020. Although the drop in BP control was substantial, this change may be less than expected given the large 20% decrease in encounters in 2020. Increases in telehealth visits and adherence to BP medications despite canceled in-person clinic visits may have prevented an even larger decline in BP control during the COVID-19 pandemic, although this could not be measured directly from the data. Furthermore, the change in BP control observed during the pandemic was small relative to the large differences observed across individual health systems before the pandemic, as well as the disparity between racial/ethnic groups.
The COVID-19 pandemic may be exacerbating health disparities, including hypertension treatment and control.23 Delayed or forgone urgent or emergency care during the initial months of the COVID-19 pandemic was more common in Black persons and Hispanic persons.6 Furthermore, increases in telehealth may have widened the divide in health care access due to the reliance on high-speed Internet or smartphones for virtual health care. In the Behavioral Risk Factor Surveillance System, Internet use among Black persons and Hispanic persons with hypertension or diabetes mellitus was shown to be substantially lower than among White persons.13 Furthermore, increasing psychosocial and socioeconomic stressors, including financial and job stress, poverty, as well as structural racism and increasing distrust of the health care system may be contributing to increased disparities in BP control.23 , 24
Results from the present study of 24 US health systems indicate that racial disparities in BP control persisted through 2020. BP control was consistently lower in non-Hispanic Black persons, despite a somewhat higher use of follow-up visits within 4 weeks after a visit with uncontrolled hypertension. In addition, increasing racial/ethnic disparities were observed with larger drops in BP control and improvement in BP in Hispanic persons and non-Hispanic Asian persons. However, 75% of the participating health systems were academic, and thus, the results may not be generalizable to all health systems. In addition, continued follow-up beyond 2020 is needed to better understand the long-term effects of the COVID-19 pandemic on disparities in BP control.
BP control was suboptimal before the COVID-19 pandemic, and it dropped considerably in 2020, with only one-quarter of patients meeting the 2017 ACC/AHA Hypertension Clinical Practice Guidelines goal (<130/<80 mm Hg). Hypertension is a major, modifiable risk factor for cardiovascular disease and affects 45% of adults in the United States.25 , 26 Thus, small changes in BP control at a population level could have large long-term consequences on cardiovascular disease incidence and mortality. As such, continued surveillance is needed to understand how these pandemic-related changes in BP control affect rates of future cardiovascular events.
Some limitations to the present study should be acknowledged. First, the results were limited to health systems in the United States participating in PCORnet, most of which are academic medical centers, and thus may not be generalizable to all health systems or to other countries. Second, each health system provided aggregated data, including overall estimates and estimates broken down by age, sex, and racial/ethnic subgroups. As such, the results could be stratified by demographic characteristics, but individual-level data were not available to conduct additional stratified or adjusted analyses. Third, we relied on BP measurements taken in the clinic because home BP monitoring data are not routinely captured in the PCORnet common data model. Fourth, changes in coding practices for telehealth visits and lack of consistency in categorization of telehealth vs in-clinic ambulatory visits across health care systems precluded us from specifically studying changes in telehealth visits between 2019 and 2020, and some of the findings might be attributable to limitations in billing, mapping of variables, or the query code rather than true changes in BP control or related processes. Finally, the last measurement period ended in 2020, and thus we could not present more recent trends in BP control metrics.
Despite these limitations, this study included 24 health systems and more than 1.7 million patients with hypertension. Because all included health systems participate in PCORnet, we could efficiently query data and complete ongoing data queries to observe trends in BP control and process metrics over time. In addition, BP Track was initiated before the COVID-19 pandemic, and this ongoing surveillance allowed us to track BP control metrics during the pandemic.
Conclusion
In this large study including more than 1.7 million patients, we observed large variability in BP control across health systems. BP control was suboptimal before the pandemic and decreased substantially during the COVID-19 pandemic, with a corresponding reduction in follow-up health care visits among persons with uncontrolled hypertension. Although improvements in timely follow-up health care visits were observed in the later half of 2020, the improvement did not reach prepandemic levels. Finally, BP control was consistently lower in non-Hispanic Blacks, but larger declines in BP control were observed in Hispanics and Asians during the pandemic. Continued surveillance is needed to determine whether and when BP control improves to prepandemic levels, whether telehealth visits are sufficient to achieve BP control, and also to monitor trends in future adverse cardiovascular events.
Potential Competing Interests
Mr Maeztu receives consulting fees and support for attending meetings and/or travel from and participates in a data safety monitoring board or advisory board for the University of California at San Francisco and is a Citizen Scientist for the University of Florida. Drs Wozniak and Rakotz are employees of the American Medical Association. Dr Sanchez is an employee of the American Heart Association and has received funding from the Department of Health and Human Services. Dr S Smith has received funding from the National Heart, Lung and Blood Institute, Patient-Centered Outcomes and Research Institute and served on the board of the Consortium for Southeastern Healthcare Quality. Dr Ahmad has received grant support from Amgen and Boehringer Ingelheim and consulting fees from Pfizer. Dr Liu has received grants from the National Institute of Diabetes and Digestive and Kidney Diseases (grant R01DK116986), the National Science Foundation (grant 2014554), and the National Center for Advancing Translational Sciences (grant UL1TR002366) and support for attending meetings and/or travel from the National Institutes of Health and the National Science Foundation. Dr McClay has received grant support from PCORI, the National Institutes of Health, and National Institute of General Medical Sciences and served as co-chair of the HL7 Clinical Interoperability Council. The PCORI funding partially supported salaries (Drs Chamberlain, Cooper-DeHoff, Fontil, Todd, Carton, O’Brien, and Pletcher and Mss Shaw, Smith, and Faulkner Modrow) or consulting income (Mr Maeztu). The other authors report no competing interests.
Acknowledgments
We acknowledge the engagement, input, moral support, and other contributions of our patient advisory board (Carlos Maeztu, Kathi Sigona, Greg Merritt, Debbie Holmes, Patrina Williams, and Patty Poston) and our clinical nurse stakeholder (Judy Sansone). We thank Deborah S. Strain for her assistance in formatting the manuscript.
Footnotes
For editorial comment, see page 644
Grant Support: This study was supported through a collaboration between the Patient-Centered Outcomes Research Institute (PCORI) (contract PaCR-2017C2-8153), the American Medical Association (funding [grant K23HL136899] and in-kind support), and the American Heart Association (in-kind support). The American Medical Association and the American Heart Association are represented on the steering committee. The findings and conclusions are those of the authors and do not necessarily represent the views of the PCORI, the American Medical Association, or the American Heart Association. The funding source had no role in the study design; the collection, analysis, and interpretation of the data; the writing of the report; or the decision to submit the article for publication.
Supplemental material can be found online at http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Mafi J.N., Craff M., Vangala S., et al. Trends in US ambulatory care patterns during the COVID-19 pandemic, 2019-2021. JAMA. 2022;327(2):237–247. doi: 10.1001/jama.2021.24294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel S.Y., Mehrotra A., Huskamp H.A., Uscher-Pines L., Ganguli I., Barnett M.L. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181(3):388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whaley C.M., Pera M.F., Cantor J., et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rose L., Tran L.D., Asch S.M., Vashi A. Assessment of changes in US Veterans Health Administration care delivery methods during the COVID-19 pandemic. JAMA Netw Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.29139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park S., Stimpson J.P. Trends in self-reported forgone medical care among Medicare beneficiaries during the COVID-19 pandemic. JAMA Health Forum. 2021;2(12) doi: 10.1001/jamahealthforum.2021.4299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czeisler M.E., Marynak K., Clarke K.E.N., et al. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Papautsky E.L., Rice D.R., Ghoneima H., et al. Characterizing health care delays and interruptions in the United States during the COVID-19 pandemic: internet-based, cross-sectional survey study. J Med Internet Res. 2021;23(5) doi: 10.2196/25446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Navar A.M., Peterson E.D., Wojdyla D., et al. Temporal changes in the association between modifiable risk factors and coronary heart disease incidence. JAMA. 2016;316(19):2041–2043. doi: 10.1001/jama.2016.13614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Virani S.S., Alonso A., Aparicio H.J., et al. Heart Disease and Stroke Statistics-2021 Update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 10.Laffin L.J., Kaufman H.W., Chen Z., et al. Rise in blood pressure observed among US adults during the COVID-19 pandemic. Circulation. 2022;145(3):235–237. doi: 10.1161/CIRCULATIONAHA.121.057075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah N.P., Clare R.M., Chiswell K., Navar A.M., Shah B.R., Peterson E.D. Trends of blood pressure control in the U.S. during the COVID-19 pandemic. Am Heart J. 2022;247:15–23. doi: 10.1016/j.ahj.2021.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muntner P., Hardy S.T., Fine L.J., et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190–1200. doi: 10.1001/jama.2020.14545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain V., Al Rifai M., Lee M.T., et al. Racial and geographic disparities in internet use in the U.S. among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44(1):e15–e17. doi: 10.2337/dc20-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pletcher M.J., Fontil V., Carton T., et al. The PCORnet Blood Pressure Control Laboratory: a platform for surveillance and efficient trials. Circ Cardiovasc Qual Outcomes. 2020;13(3) doi: 10.1161/CIRCOUTCOMES.119.006115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cooper-DeHoff R.M., Fontil V., Carton T., et al. Tracking blood pressure control performance and process metrics in 25 US health systems: the PCORnet Blood Pressure Control Laboratory. J Am Heart Assoc. 2021;10(21) doi: 10.1161/JAHA.121.022224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forrest C.B., McTigue K.M., Hernandez A.F., et al. PCORnet(R) 2020: current state, accomplishments, and future directions. J Clin Epidemiol. 2021;129:60–67. doi: 10.1016/j.jclinepi.2020.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qualls L.G., Phillips T.A., Hammill B.G., et al. Evaluating foundational data quality in the National Patient-Centered Clinical Research Network (PCORnet(R)) EGEMS (Wash DC) 2018;6(1):3. doi: 10.5334/egems.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quality ID #236 (NQF 0018): Controlling High Blood Pressure - National Quality Strategy Domain: Effective Clinical Care. American Medical Association. 2017. Accessed December 16, 2022. https://www.acr.org/-/media/ACR/NOINDEX/Measures/2018_Measure_236_Registry.pdf.
- 19.Hypertension: Improvement in Blood Pressure. eCQI Resource Center. https://ecqi.healthit.gov/sites/default/files/ecqm/measures/CMS65v7.html
- 20.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17):e484–e594. doi: 10.1161/CIR.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 21.Patel S.Y., Rose S., Barnett M.L., Huskamp H.A., Uscher-Pines L., Mehrotra A. Community factors associated with telemedicine use during the COVID-19 pandemic. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bress A.P., Cohen J.B., Anstey D.E., et al. Inequities in hypertension control in the United States exposed and exacerbated by COVID-19 and the role of home blood pressure and virtual health care during and after the COVID-19 pandemic. J Am Heart Assoc. 2021;10(11) doi: 10.1161/JAHA.121.020997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services . US Department of Health and Human Services, Office of the Surgeon General; 2020. The Surgeon General's Call to Action to Control Hypertension. [Google Scholar]
- 25.Muntner P., Carey R.M., Gidding S., et al. Potential US population impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation. 2018;137(2):109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ostchega Y., Fryar C.D., Nwankwo T., Nguyen D.T. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief. April 2020;(364):1–8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.