Abstract
Introduction
COVID-19 vaccines are safe, effective, and widely available, but many adults in the U.S. have not been vaccinated for COVID-19. This study examined the associations between behavioral and social drivers of vaccination with COVID-19 vaccine uptake in the U.S. adults and their prevalence by region.
Methods
A nationally representative sample of U.S. adults participated in a cross-sectional telephone survey in August–November 2021; the analysis was conducted in January 2022. Survey questions assessed self-reported COVID-19 vaccine initiation, demographics, and behavioral and social drivers of vaccination.
Results
Among the 255,763 respondents, 76% received their first dose of COVID-19 vaccine. Vaccine uptake was higher among respondents aged ≥75 years (94%), females (78%), and Asian non-Hispanic people (94%). The drivers of vaccination most strongly associated with uptake included higher anticipated regret from nonvaccination, risk perception, and confidence in vaccine safety and importance, followed by work- or school-related vaccination requirements, social norms, and provider recommendation (all p<0.05). The direction of association with uptake varied by reported level of difficulty in accessing vaccines. The prevalence of all of these behavioral and social drivers of vaccination was highest in the Northeast region and lowest in the Midwest and South.
Conclusions
This nationally representative survey found that COVID-19 vaccine uptake was most strongly associated with greater anticipated regret, risk perception, and confidence in vaccine safety and importance, followed by vaccination requirements and social norms. Interventions that leverage these social and behavioral drivers of vaccination have the potential to increase COVID-19 vaccine uptake and could be considered for other vaccine introductions.
INTRODUCTION
Vaccines are a crucial tool to mitigate both individual and community impacts of the COVID-19 pandemic. The Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices first recommended the use of COVID-19 vaccines for priority groups in December 2020. Vaccine eligibility in the U.S. expanded to all persons aged ≥5 years by October 2021.1 Although overall COVID-19 vaccine initiation exceeds 80% in adults, uptake differs by age, race, insurance status, income, region, and rurality.2 , 3 Vaccine hesitancy, defined as a motivational state of being conflicted about or opposed to getting vaccinated, has been identified as a barrier to vaccine uptake.4, 5, 6, 7, 8 To address hesitancy and increase COVID-19 vaccine uptake, it is important to identify the behavioral and social drivers of vaccination and implement interventions that address these drivers in diverse populations and regions in the U.S.
The Behavioral and Social Drivers of vaccination framework,9 , 10 built on the Increasing Vaccination Model, identifies thinking and feeling, social processes, and practical issues as the key domains associated with vaccine uptake (Appendix 1, available online).10 The social processes domain includes constructs such as a recommendation from a healthcare provider, which is consistently associated with higher vaccine uptake across age, racial, and ethnic groups for both COVID-19 vaccine and other vaccines.11 , 12 Within the practical issues domain, difficulty of access has been identified as a barrier to COVID-19 vaccine uptake, whereas vaccination requirements have been suggested to increase uptake.13, 14, 15
The National Immunization Survey Adult COVID Module (NIS-ACM) complements other COVID-19 vaccination surveys,16, 17, 18 providing nationally and regionally representative weekly estimates of the behavioral and social drivers of COVID-19 vaccination.19 , 20 Data from the NIS-ACM were analyzed to assess (1) the proportion of respondents who initiated COVID-19 vaccination overall, by population subgroups and by behavioral and social drivers; (2) the demographic characteristics of access barriers by vaccination status; (3) the prevalence of behavioral and social drivers in 4 regions of the U.S.; and (4) the associations between each level increase in behavioral and social drivers of vaccination and COVID-19 vaccine uptake.
METHODS
Study Sample
The NIS-ACM generated a nationally representative sample of U.S. adults using random-digit dialing of cell phone numbers.20 Participants were from the 50 U.S. states, the District of Columbia, and U.S. territories.20 The overall survey response rate ranged from 20.9% in September to 23.4% in November 2021.
The NIS-ACM conducted a telephone survey in English and Spanish during August 1–November 27, 2021.21 Respondents indicated their consent verbally; they could withdraw their consent by hanging up the phone. Respondents did not receive incentives for participation. The data set for this cross-sectional study was deidentified; access to this data set can be obtained through the NCHS Research Data Centers.22 This activity was reviewed by CDC and conducted consistent with applicable federal law and CDC policy.1 This study followed the STROBE reporting guidelines.23
Measures
The survey assessed self-reported COVID-19 vaccine uptake or initiation with the question, Have you received at least one dose of a COVID-19 vaccine? with binary responses categorized as Yes and No. Self-reported demographic factors included age (categorized as 18–29, 30–39, 40–49, 50–64, 65–74, and ≥75 years), gender (male or female), race and ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic, Asian non-Hispanic, American Indian/Alaska Native non-Hispanic, Native Hawaiian/Pacific Islander non-Hispanic, or other/multiple races), annual household income (below the federal poverty level for 202124; above the federal poverty level but under $75,000; $75,000 and above; or unknown), health insurance (not insured or insured), essential/frontline worker status (essential healthcare, school and child care, other frontline worker, other essential worker, or not a frontline or essential worker), metropolitan statistical area (MSA) (MSA principal city, MSA nonprincipal city, and non-MSA), and U.S. Census region (Northeast, South, Midwest, and West). These demographic factors were selected owing to disparities in vaccine uptake between these subgroups.
In the thinking and feeling domain, 4 questions assessed risk perception, anticipated regret, confidence in vaccine importance, and confidence in vaccine safety. Risk perception was assessed with the question How concerned are you about getting COVID-19? with ordinal responses categorized as Very concerned, Moderately concerned, A little concerned, and Not at all concerned. Anticipated regret if not vaccinated was assessed with the statement “If I [do not get/had not gotten] a COVID-19 vaccine, I [will/would] regret it,” with response options of Very strongly agree, Strongly agree, Somewhat agree, and Do not agree. Confidence in vaccine importance was assessed with the question, How important do you think getting a COVID-19 vaccine is to protect yourself against COVID-19? with response options of Very important, Somewhat important, A little important, and Not at all important. Similarly, confidence in vaccine safety was assessed with the question, How safe do you think a COVID-19 vaccine is for you? with response options of Completely safe, Very safe, Somewhat safe, and Not at all safe.
In the domain of social processes, 1 question assessed provider recommendation, Has a doctor, nurse, or other health professional ever recommended that you get a COVID-19 vaccine? with responses of Yes or No, and another question assessed social norms: If you had to guess, about how many of your family and friends have received a COVID-19 vaccine? with response options of Almost all, Many, Some, or None.
In the domain of practical issues, 2 questions assessed the difficulty of access and vaccine requirements. Difficulty of access was assessed with the question How difficult [would it be for you/was it for you] to get a COVID-19 vaccine? with ordinal response options of Not at all difficult, A little difficult, Somewhat difficult, and Very difficult. Vaccine requirement was assessed with the question Does your work or school require you to get a COVID-19 vaccine? with responses categorized as Yes, No, or Unemployed/not applicable.
Statistical Analysis
Vaccine uptake was weighted to represent the non-institutionalized U.S. population aged ≥18 years using population control totals for age group, gender, MSA, and race/ethnicity, with further calibration to cumulative COVID-19 vaccine administration in September 2021 by gender and age group for each jurisdiction. The unweighted number and weighted proportion of respondents who self-reported COVID-19 vaccine uptake were assessed by demographic characteristics and by responses to the behavioral and social questions. The weighted proportion of respondents who reported that it was very or somewhat difficult to get a COVID-19 vaccine was calculated and stratified by vaccination status. To examine geographic variability, the number and weighted proportion of respondents was calculated in each of the 4 Census regions (Northeast, Midwest, South, and West). For each region, the weighted proportion of respondents who were very or moderately concerned about getting COVID-19, were strongly or very strongly agreed that they would regret not getting a COVID-19 vaccine, were confident that COVID-19 vaccines are completely or very safe, were confident that COVID-19 vaccines are very or somewhat important, had all or almost all friends and family members who were vaccinated against COVID-19, had received a provider recommendation to get a COVID-19 vaccine, believed that it was very or somewhat difficult to get a COVID-19 vaccine, and were subject to a work or school COVID-19 vaccination requirement was reported.
Finally, the associations of COVID-19 vaccine initiation with each behavioral and social driver of COVID-19 were evaluated using separate ordinal logistic regressions and predictive marginals for each driver, controlling for demographic characteristics, including age, gender, race, ethnicity, household income, health insurance status, rurality, frontline/essential worker status, and census region. The unadjusted prevalence differences were reported in the results section because these models assume no interactions. The analyses used staircase coding for the predictors that compared each level with the next higher level (i.e., for a 4-level predictor: 1 vs 2, 2 vs 3, and 3 vs 4). Analyses used t-tests to determine the differences between groups with statistical significance at p<0.05. Analyses were performed using SAS (Version 9.4)25 and SUDAAN (Version 11.0.3).26
RESULTS
Among the 255,763 survey respondents, 20.9% were aged 18–29 years, 21.4% were aged ≥65 years, 51.6% were female, 62.2% were White non-Hispanic, 11.9% were Black non-Hispanic, and 17.2% were Hispanic (Table 1 ). Self-reported vaccine uptake (≥1 dose of COVID-19 vaccine) was 76.1%. Over 75% of respondents in the following categories reported receiving at least 1 dose of a COVID-19 vaccine: respondents aged ≥50 years (82.2%–94.1% by age band), females (78.2%), White non-Hispanic persons (76.6%), Asian non-Hispanic persons (93.7%), Hispanic persons (76.9%), persons with insurance (78.5%), college graduates (85.2%), persons with advanced degrees (92.5%), school and childcare workers (87.2%), healthcare workers (84.0%), and nonessential workers (77.8%). The proportion of unvaccinated respondents who reported difficulty in accessing COVID-19 vaccines was greater among the younger age groups (49.1%), Black non-Hispanic persons (34.6%), American Indian or Alaska Native non-Hispanic persons (51.3%), those with incomes below the federal poverty level (46.3%), and rural residents (37.6%) (Table 2 ).
Table 1.
Demographics and COVID-19 Vaccination (≥1 Dose) Overall and Among Those Vaccinated, National Immunization Survey Adult COVID Module, August–November 27, 2021
| Demographics | Overall |
Received ≥1 dose of COVID-19 vaccine |
||
|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | |
| Overall | 255,763 | 100.0 | 218,521 | 76.1 (75.7, 76.5) |
| Age (years) | ||||
| 18–29 | 43,176 | 20.9 (20.5, 21.2) | 33,661 | 61.6 (60.7, 62.5) |
| 30–39 | 41,312 | 17.4 (17.1, 17.7) | 33,609 | 67.5 (66.6, 68.5) |
| 40–49 | 38,817 | 16.0 (15.7, 16.3) | 32,335 | 73.2 (72.2, –74.1) |
| 50–64 | 70,529 | 24.4 (24.0, 24.7) | 61,908 | 82.2 (81.5, 82.8) |
| 65–74 | 39,541 | 12.6 (12.3, 12.8) | 36,931 | 91.9 (91.3, 92.5) |
| 75+ | 17,993 | 8.8 (8.5, 9.0) | 16,845 | 94.1 (93.4, 94.8) |
| Gender | ||||
| Male | 123,512 | 48.4 (48.0, 48.8) | 103,501 | 74.1 (73.6, 74.7) |
| Female | 130,142 | 51.6 (51.2, 52.0) | 113,636 | 78.2 (77.7, 78.7) |
| Race/ethnicity | ||||
| White, non-Hispanic | 161,506 | 62.2 (61.8, 62.6) | 139,038 | 76.6 (76.1, 77.0) |
| Black, non-Hispanic | 29,123 | 11.9 (11.7, 12.2) | 24,498 | 73.0 (71.9, 74.1) |
| Hispanic | 32,062 | 17.2 (16.8, 17.5) | 27,606 | 76.9 (75.9, 77.8) |
| Asian, non-Hispanic | 11,630 | 4.2 (4.1, 4.4) | 11,211 | 93.7 (92.5, 94.7) |
| American Indian/Alaska Native, non-Hispanic | 3,233 | 1.0 (0.9, 1.0) | 2,400 | 58.9 (54.5, 63.1) |
| Native Hawaiian/Pacific Islander, non-Hispanic | 1,376 | 0.4 (0.3, 0.4) | 1,088 | 73.6 (67.9, 78.6) |
| Other/multiracial | 9,229 | 3.1 (3.0, 3.3) | 7,004 | 64.3 (62.0, 66.5) |
| Household income | ||||
| Below federal poverty level | 23,087 | 10.7 (10.5, 11.0) | 17,748 | 65.6 (64.3, 66.8) |
| Above FPL, <$75k annual income | 79,885 | 32.1 (31.7, 32.4) | 67,339 | 74.4 (73.7, 75.1) |
| Above FPL, ≥$75k annual income | 96,807 | 33.0 (32.6, 33.3) | 87,258 | 82.7 (82.1, 83.2) |
| Unknown income | 55,984 | 24.3 (23.9, 24.6) | 46,176 | 74.0 (73.2, 74.8) |
| Health insurance | ||||
| No | 19,439 | 10.0 (9.7, 10.2) | 13,568 | 57.4 (56.0, 58.7) |
| Yes | 228,709 | 90.0 (89.8, 90.3) | 199,189 | 78.5 (78.1, 78.9) |
| Education | ||||
| High school or less | 62,378 | 39.0 (38.6, 39.4) | 47,414 | 69.0 (68.3, 69.7) |
| Some college | 71,183 | 30.5 (30.2, 30.9) | 58,537 | 74.1 (73.5, 74.8) |
| College graduate | 63,980 | 19.2 (18.9, 19.5) | 58,389 | 85.2 (84.5, 85.9) |
| Advanced degree | 50,571 | 11.2 (11.0, 11.4) | 48,274 | 92.5 (91.9, 93.1) |
| Frontline and essential worker status | ||||
| Essential healthcare | 27,183 | 9.3 (9.1, 9.5) | 24,755 | 84.0 (83.0, 85.0) |
| School and child care | 9,526 | 2.9 (2.8, 3.0) | 8,865 | 87.2 (85.6, 88.7) |
| Other frontline worker | 16,550 | 7.4 (7.1, 7.6) | 12,974 | 66.3 (64.8, 67.8) |
| Other essential worker | 29,336 | 12.5 (12.2, 12.7) | 22,909 | 66.2 (65.0, 67.3) |
| Not a frontline or essential worker | 171,446 | 68.0 (67.6, 68.3) | 148,110 | 77.8 (77.4, 78.2) |
| Rurality | ||||
| MSA, principal city | 89,931 | 33.0 (32.6, 33.3) | 78,932 | 78.2 (77.5, 78.8) |
| MSA, nonprincipal city | 117,845 | 53.2 (52.8,53.6) | 102,002 | 77.3 (76.8, 77.8) |
| Non-MSA | 47,987 | 13.8 (13.6, 14.1) | 37,587 | 66.6 (65.5, 67.6) |
| Census region | ||||
| Northeast | 51,698 | 17.4 (17.2, 17.6) | 46,457 | 84.5 (83.8, 85.1) |
| Midwest | 45,899 | 20.8 (20.5, 21.0) | 38,535 | 70.4 (69.5, 71.3) |
| South | 91,715 | 38.0 (37.7, 38.3) | 77,005 | 72.1 (71.5, 72.7) |
| West | 55,277 | 23.8 (23.5, 24.0) | 46,489 | 80.8 (80.1, 81.5) |
Note: Table reports weighted percentages.
Census regions: West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Washington, and Wyoming. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Maryland, Mississippi, North Carolina, Louisiana, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Indiana, Illinois, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin.
MSA, Metropolitan Statistical Area; NIS-ACM, National Immunization Survey Adult COVID Module; FPL, federal poverty level.
Table 2.
Self-Reported Difficulty in Getting a COVID-19 Vaccine Overall and Among Those Unvaccinated, National Immunization Survey Adult COVID Module, August 1–November 27, 2021
| It was very or somewhat difficult to get a COVID-19 vaccine |
|||
|---|---|---|---|
| Overall |
Not vaccinated | ||
| Demographics | n | % (95% CI) | % (95% CI) |
| Age (years) | |||
| 18–29 | 4,627 | 11.5 (10.9, 12.1) | 49.1 (46.5, 51.8) |
| 30–39 | 5,353 | 12.1 (11.5, 12.7) | 31.6 (28.9, 34.3) |
| 40–49 | 5,076 | 13.9 (13.2, 14.6) | 22.7 (20.5, 25.2) |
| 50–64 | 9,867 | 14.8 (14.2, 15.3) | 14.3 (12.8, 15.9) |
| 65–74 | 7,359 | 20.6 (19.7, 21.4) | 5.5 (4.3, 6.9) |
| 75+ | 3,035 | 20.3 (19.1, 21.5) | 4.9 (3.7, 6.4) |
| Gender | |||
| Male | 15,687 | 13.3 (13.0, 13.7) | 24.2 (22.8, 25.7) |
| Female | 20,021 | 16.0 (15.6, 16.4) | 18.2 (17.0, 19.4) |
| Race/ethnicity | |||
| White, non-Hispanic | 3,903 | 15.8 (15.4, 16.1) | 17.0 (16.0, 18.1) |
| Black, non-Hispanic | 24,008 | 12.4 (11.6, 13.1) | 34.6 (31.3, 38.1) |
| Hispanic | 3,486 | 12.3 (11.6. 13.0) | 27.6 (24.8, 30.7) |
| Asian, non-Hispanic | 1,692 | 15.3 (14.0, 16.7) | 6.0 (3.8, 9.4) |
| American Indian/Alaska Native, non-Hispanic | 410 | 12.3 (10.1, 14.9) | 51.3 (41.4, 61.1) |
| Native Hawaiian/Pacific Islander non-Hispanic | 162 | 13.2 (9.7, 17.8) | 28.3 (17.3, 42.9) |
| Other/multiracial | 1,237 | 16.1 (14.4, 17.8) | 37.0 (31.2, 43.1) |
| Income | |||
| Below FPL | 2,913 | 13.8 (13.0, 14.7) | 46.3 (42.9, 49.8) |
| Above FPL, <$75K annual income | 9,901 | 13.2 (12.7, 13.7) | 23.7 (22.0, 25.6) |
| Above FPL, ≥$75K annual income | 15,069 | 15.9 (15.5, 16.4) | 9.3 (8.3, 10.4) |
| Unknown income | 8,147 | 15.7 (15.1, 16.3) | 24.2 (22.3, 26.2) |
| Health insurance | |||
| No | 2,200 | 12.2 (11.3, 13.1) | 17.9 (17.0, 18.8) |
| Yes | 32,847 | 15.0 (14.7, 15.3) | 51.1 (47.2, 55.0) |
| Education | |||
| High school or less | 7,106 | 12.7 (12.2, 13.2) | 27.1 (25.2, 29.1) |
| Some college | 8,779 | 13.7 (13.2, 14.3) | 18.2 (17.2, 19.3) |
| College graduate | 9,456 | 16.9 (16.3, 17.5) | 36.4 (34.5, 38.4) |
| Advanced degree | 9,629 | 20.5 (19.8, 21.3) | 21.8 (20.2, 23.6) |
| Essential/frontline worker | |||
| No | 26,269 | 15.7 (15.4, 16.1) | 6.9 (5.9, 8.1) |
| Yes | 9,234 | 12.6 (12.1, 13.1) | 4.0 (3.0, 5.3) |
| Rurality | |||
| MSA, principal city | 13,101 | 14.5 (14.0, 14.9) | 21.5 (20.0, 23.2) |
| MSA, nonprincipal city | 18,128 | 15.8 (15.4, 16.2) | 17.6 (16.4, 18.8) |
| Non-MSA | 4,801 | 11.3 (10.6, 11.9) | 37.6 (34.7, 40.6) |
| Census region | |||
| Northeast | 8,498 | 18.7 (18.1, 19.4) | 10.7 (9.4, 12.2) |
| Midwest | 5,954 | 13.8 (13.2, 14.4) | 26.3 (24.1, 28.6) |
| South | 13,553 | 13.8 (13.4, 14.3) | 26.1 (24.5, 27.8) |
| West | 7,126 | 14.4 (13.8, 15.1) | 18.3 (16.4, 20.4) |
FPL, federal poverty level.
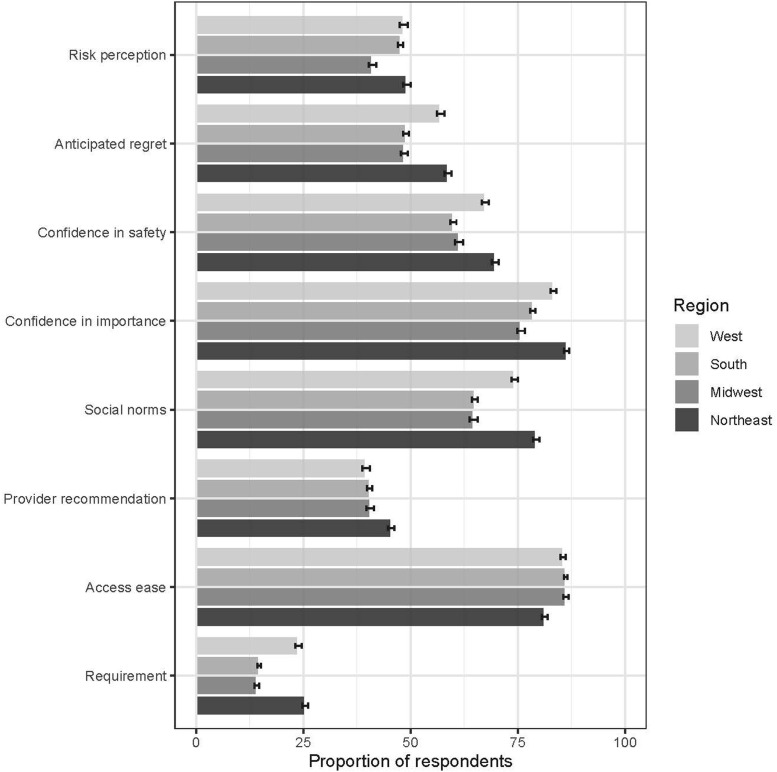
Risk perception varied by region, with 41.1% of respondents in the Midwest and 49.1% of respondents in the Northeast reporting being very or moderately concerned about getting COVID-19 (Figure 1 ). In the Midwest, 75.7% reported confidence that COVID-19 vaccines are very or somewhat important, in contrast to reports in the Northeast, where 86.4% reported confidence that COVID-19 vaccines are very or somewhat important. The proportion of respondents reporting confidence that COVID-19 vaccines are completely or very safe ranged from 60.0% in the South to 69.7% in the Northeast. Only 39.6% of respondents in the West reported receiving a provider recommendation compared with 45.5% in the Northeast. The proportions of respondents who reported having almost all or many vaccinated family and friends ranged from 64.7% in the Midwest to 79.3% in the Northeast. In the Midwest, 14.2% reported COVID-19 vaccine requirements for work or school, whereas 25.5% of respondents in the Northeast reported these requirements. In the Northeast, 81.3% reported that it was a little or not at all difficult to get a COVID-19 vaccine compared with 86.2% of respondents in the South and Midwest.
Figure 1.
Prevalence (and 95% CI) of BeSDs of vaccination among adults by Census region, August 1–November 27, 2021.
BeSD, behavioral and social driver.
Each higher level of the Behavioral and Social Drivers of vaccination constructs was associated with a higher likelihood of vaccine uptake, reported in marginal prevalence differences, where each level was compared with the level preceding (Table 3 ). In the thinking and feeling domain, anticipated regret of not receiving a vaccine and then getting infected with COVID-19, confidence in vaccine safety, and confidence in vaccine importance were most strongly associated with receiving a COVID-19 vaccine. Confidence that COVID-19 vaccines are somewhat safe was associated with an unadjusted 57.0 percentage point (95% CI=55.9, 58.1) higher uptake than a lack of such confidence (Table 3). For each level of confidence in vaccine importance, the likelihood of vaccine uptake was 25.2 (95% CI=23.2, 27.1) to 29.8 (95% CI=28.0, 31.6) percentage points higher. For the social norms construct, reporting some family and friends vaccinated was associated with a 28.1 (95% CI=26.2, 30.0) percentage point higher likelihood of uptake than reporting having no family or friends who were vaccinated. Provider recommendation and vaccination requirements were associated with 11.6 (95% CI=10.9, 12.3) percentage points and 21.8 (95% CI=21.1, 22.6) percentage points higher vaccination likelihood, respectively. Those who reported that it was a little difficult to get a vaccine were 12.9 (95% CI=12.0, 13.9) percentage points more likely to be vaccinated than those who reported that it was not at all difficult. Adjusted rates were similar to the likelihood of vaccine uptake in the unadjusted model.
Table 3.
Association Between Behavioral and Social Drivers and COVID-19 Vaccination (≥1 Dose), National Immunization Survey Adult COVID Module, August 1–November 27, 2021
| Unadjusted |
Adjusted for demographics |
||||
|---|---|---|---|---|---|
| Behavioral and social drivers of vaccination | Vaccinated %a (95% CI) | Marginal prevalence differenceb | (95% CI) | Marginal prevalence differenceb | (95% CI) |
| Thinking and feeling | |||||
| Concerned about getting COVID-19 | |||||
| Not at all concerned | 53.5 (52.7, 54.4) | — | — | ||
| A little concerned | 78.9 (78.2, 79.6) | 25.2** | (24.1, 26.3) | 21.6** | (20.5, 22.6) |
| Moderately concerned | 85.5 (84.9, 86.1) | 6.6** | (5.7, 7.5) | 5.5** | (4.6, 6.4) |
| Very concerned | 89.5 (88.9, 90.1) | 4.0** | (3.1, 4.9) | 3.1** | (2.2, 4.0) |
| Anticipated regret if not vaccinated | |||||
| Do not agree | 32.0 (31.2, 32.7) | — | — | ||
| Somewhat agree | 79.2 (78.3, 80.0) | 47.2** | (46.0, 48.3) | 42.3** | (41.1, 43.5) |
| Strongly agree | 95.2 (94.8, 95.6) | 16.0** | (15.1, 16.9) | 14.0** | (13.0, 14.9) |
| Very strongly agree | 97.3 (97.0, 97.6) | 2.0** | (1.6, 2.5) | 2.1** | (1.7, 2.7) |
| Thinks that a COVID-19 vaccine is important | |||||
| Not at all important | 11.1 (10.4, 11.8) | — | — | ||
| A little important | 40.8 (39.2, 42.5) | 29.8** | (28.0, 31.6) | 31.8** | (30.0, 33.7) |
| Somewhat important | 65.9 (64.8, 67.0) | 25.2** | (23.2, 27.1) | 23.5** | (21.6, 25.5) |
| Very important | 95.3 (95.1, 95.6) | 29.3** | (28.2, 30.4) | 24.5** | (23.5, 25.6) |
| Thinks that a COVID-19 vaccine is safe | |||||
| Not at all safe | 10.2 (9.5, 10.9) | — | — | ||
| Somewhat safe | 67.1 (66.3, 68.0) | 57.0** | (55.9, 58.1) | 55.1** | (53.8–56.4) |
| Very safe | 94.9 (94.5, 95.2) | 27.7** | (26.7, 28.6) | 24.6** | (23.7–25.5) |
| Completely safe | 96.8 (96.5, 97.1) | 1.9** | (1.5, 2.3) | 2.2** | (1.7, 2.7) |
| Social processes | |||||
| Healthcare provider recommended vaccine | |||||
| No | 71.1 (70.6, 71.6) | — | — | ||
| Yes | 82.9 (82.4, 83.4) | 11.6** | (10.9, 12.3) | 8.6** | (7.9, 9.3) |
| Friends and family vaccinated | |||||
| None | 18.5 (16.8, 20.3) | — | — | ||
| Some | 46.5 (45.7, 47.3) | 28.1** | (26.2, 30.0) | 26.5** | (24.2, 28.8) |
| Many | 82.0 (81.3, 82.7) | 35.5** | (34.4, 36.6) | 30.5** | (29.4, 31.6) |
| Almost all | 94.1 (93.8, 94.4) | 12.0** | (11.2, 12.8) | 10.2** | (9.4, 11.0) |
| Practical issues | |||||
| Difficulty in getting a COVID-19 vaccine | |||||
| Not at all difficult | 74.3 (73.8, 74.7) | — | — | ||
| A little difficult | 87.3 (86.4, 88.1) | 12.9** | (12.0, 13.9) | 10.7** | (9.7, 11.6) |
| Somewhat difficult | 84.9 (83.9, 85.9) | −2.3** | (−1.0, 3.6) | −3.8** | (−2.4, 5.2) |
| Very difficult | 66.8 (64.9, 68.5) | −18.3** | (−16.2, 20.4) | −17.8** | (−15.7, 19.9) |
| Work or school requires you to get a COVID-19 vaccine | |||||
| No | 69.6 (69.1, 70.1) | Ref | Ref | ||
| Yes | 91.4 (90.8, 92.0) | 21.8** | (21.1, 22.6) | 19.7** | (19.0, 20.4) |
| Unemployed/not applicable | 85.2 (84.4, 86.0) | 15.5** | (14.6, 16.5) | 1.5* | (0.1, 2.9) |
Note: Boldface indicates statistical significance (** p<0.001 and * p<0.05).
Overall N=218,521. Data were adjusted for age, gender, race/ethnicity, income, insurance status, essential/frontline worker status, rurality, and Census region.
Unadjusted frequencies and weighted percentages and marginal prevalence differences.
The marginal preference difference consecutively adds the difference in uptake between each ordinal level of the Behavioral and Social Drivers of Vaccination constructs (e.g., those who are a little concerned about getting COVID-19 are 21.6 [95% CI=20.5, 22.6] percentage points more likely to have at least 1 dose of COVID-19 vaccine than those who are not at all concerned about getting COVID-19).
DISCUSSION
This nationally representative survey of over 200,000 U.S. adults identified the behavioral and social drivers associated with COVID-19 vaccination nationally and regionally. Vaccine uptake was most strongly associated with anticipated regret if not vaccinated, risk perception, confidence in vaccine safety, and confidence in vaccine importance, followed by a smaller magnitude of association with social norms, vaccination requirements, ease of access, and provider recommendation. In contrast to reports from earlier studies in the COVID-19 vaccination roll out,27 , 28 the analysis did not find self-reported difficulty uniformly associated with lower receipt of vaccine. This unexpected finding might be attributable to extensive efforts to reduce access barriers, including mobile vaccination sites, removing an insurance or identification requirement, and substantial community-led outreach.29, 30, 31 Alternatively, the impact of access barriers on uptake could be modified by other contextual or community-level environmental factors.32, 33, 34 In addition, this finding might be ascribed to a limitation in the survey question, given the heterogeneity between overall rates of difficulty in accessing the vaccine and those rates among the unvaccinated between demographic strata.
Respondents in the Northeast reported the highest prevalence of confidence in vaccine safety and importance, risk perception, social norms, and provider recommendations, whereas respondents in the Midwest and South consistently reported the lowest prevalence of these drivers. The lower prevalence of these behavioral and social drivers in the Midwest and South might contribute to the lower COVID-19 vaccine uptake in these regions than in the Northeast and West.
Although the thinking and feeling constructs were associated with uptake, few effective, evidence-based interventions that act upon these constructs to increase vaccination rates have been identified.10 That is, although anticipated regret in not being vaccinated, confidence in vaccine safety, and confidence in vaccine importance are associated with vaccine uptake, it is not clear how to use persuasive or educational techniques to reliably change these perceptions. More innovative approaches are needed to improve vaccine confidence in a manner that achieves improvements in vaccine uptake.
In the social processes domain, strong associations were identified between the proportion of family and friends vaccinated (social norms) and vaccination uptake. These findings underscore the critical role of social processes in increasing vaccination, particularly because individuals tend to underestimate the proportion of their social networks that are vaccinated.27 , 35 , 36 However, it is also important to note that simply communicating descriptive norms has not been effective in increasing vaccine uptake.37 Tailored and community-led interventions, including ZIP code−level vaccination access planning and community engagement, have been shown to reduce inequities in COVID-19 vaccination by race and ethnicity.38, 39, 40 One particularly promising intervention could be encouraging vaccinated people to be peer ambassadors and disclose their vaccination status to family and friends. After 1 vaccine ambassador training in Los Angeles County, CA, 83% of community vaccine ambassadors reported motivating at least 1 person, and 19% reported motivating at least 6 unvaccinated people to get a COVID-19 vaccine.41 Given the disparities in vaccination rates by race and ethnicity as well as the disproportionate burden of COVID-19 in these communities,42 , 43 it is important to strengthen community-led interventions from trusted individuals among these groups.44 , 45
Provider recommendation remains a key component to increasing vaccine uptake, even for those who describe themselves as vaccine hesitant.46 Providers, pharmacists, and nurses are consistently listed as one of the most trusted sources of health information28 , 47 and are frequently cited as the reason their patients opt to receive a vaccine.48 , 49 The impact of provider recommendations extends to health professionals in other contexts, including mental health.50 The association of provider recommendation and vaccine uptake might be somewhat attenuated in these findings owing to the underuse of primary care services during the COVID-19 pandemic and the high proportion of adults in the U.S. without a primary care provider,51 limiting opportunities for providers to convey recommendations. Actions should be taken to encourage providers to actively reach out to patients and encourage vaccination and to ensure the quality of providers’ recommendations.52, 53, 54, 55
Interventions in the practical issues domain have consistently been associated with increased uptake, even without trying to change risk perception or vaccine confidence.14 , 56 , 57 Although practical issues encompass an array of challenges, including patient experiences, transport costs, and overall difficulty in accessing vaccination,4 this survey explores only 2 facets: self-reported access difficulties and vaccination requirements. These findings illustrate a strong and positive association between vaccination requirements and vaccine uptake. Vaccination requirements have been associated with reductions in ethnic and racial disparities in vaccination coverage41 and higher levels of vaccine confidence among healthcare workers.58 That said, the implementation of vaccination requirements requires care. Because the effectiveness of vaccination requirements depends on the context in which requirements are implemented, best practices include provisions for stable access to vaccines, multiple interventions in addition to requirements that encourage uptake, and fair and equitable administration of vaccination requirements.59 Other promising interventions in the practical issues domain include vaccination incentives (when incentives are delivered immediately, with certainty, and valued by recipients), onsite vaccination, and reminders.60
Limitations
This study has 4 main limitations. First, as a random-digit-dial survey, institutionalized individuals or those without a phone or only a landline telephone would not be eligible for inclusion in this survey. Second, the response rate ranged from 20.9% in September to 23.4% in November, although it is consistent with other nationally representative surveys.20 To address potential bias from incomplete sample frame and nonresponse, the National Immunization Surveys weigh responses to the non-institutionalized U.S. adult population.61 Third, vaccine status was self-reported rather than verified. Although a limitation, assessments have found self-report to be 98% accurate when compared with vaccination attestation.62 In addition, the NIS-ACM survey weights included calibration to regional COVID-19 vaccine administration data, mitigating systematic errors in vaccine uptake from incomplete sample frame, nonresponse, and errors in self-reported vaccination status. Fourth, it was assumed that the relationships between behavioral and social drivers and COVID-19 vaccine uptake remained constant over the 4-month data collection period, as reported elsewhere.63
CONCLUSIONS
This study identifies risk perception, confidence in vaccine safety and importance, and anticipated regret as the leading behavioral and social drivers associated with COVID-19 vaccine uptake, followed by smaller associations between social norms, vaccination requirements, and provider recommendations on vaccine uptake. The findings from this study provide data that can be used to design interventions to increase COVID-19 vaccine uptake: leveraging social norms to equip individuals to be vaccine ambassadors to family and friends, supporting healthcare workers to make effective vaccine recommendations, researching ways to change risk perceptions and confidence in vaccine safety and importance, and implementing vaccination requirements in an equitable manner.
Acknowledgments
ACKNOWLEDGMENTS
No other funding source was involved in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit this manuscript for publication. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention (CDC).
All authors declare no conflicts of interest pertinent to this manuscript; all have provided their conflict of interest disclosures. The coauthors are CDC government employees who did not receive funding specifically for this work. The academic coauthors received funding from the CDC to support the engagement in the COVID-19 vaccination response.
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Kimberly E. Bonner: Conceptualization, Investigation, Methodology, Writing - original draft. Kushagra Vashist: Data curation, Formal analysis, Investigation, Methodology, Writing - review and editing. Neetu S. Abad: Conceptualization, Investigation, Methodology, Resources, Writing - review and editing, Supervision. Jennifer L. Kriss: Data curation, Formal analysis, Investigation, Methodology, Resources, Writing - review and editing. Lu Meng: Conceptualization, Data curation, Formal analysis, Validation, Methodology. James T. Lee: Data curation, Investigation, Methodology, Resources, Writing - review and editing. Elisabeth Wilhelm: Conceptualization, Writing - review and editing. Peng-Jun Lu: Data curation, Formal analysis, Investigation, Methodology, Writing - review and editing. Rosalind J. Carter: Writing - review and editing. Kwanza Boone: Methodology, Writing - review & editing. Brittney Baack: Conceptualization, Writing - review and editing. Nina B. Masters: Writing - review and editing. Debora Weiss: Writing - review and editing. Carla Black: Writing - review and editing. Qian Huang: Writing - review and editing. Sitaram Vangala: Writing - review and editing. Christina Albertin: Writing - review and editing. Peter G. Szilagyi: Conceptualization, Methodology, Writing - review and editing, Supervision. Noel T. Brewer: Conceptualization, Investigation, Methodology, Resources, Writing - review and editing, Supervision. James A. Singleton: Data curation, Investigation, Methodology, Resources, Writing - review and editing, Supervision.
Footnotes
§ See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3,501 et seq.
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2023.01.014.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Fact sheet. President Biden to announce all Americans to be eligible for vaccinations by may 1, puts the nation on a path to get closer to normal by July 4th. The White House.https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/11/fact-sheet-president-biden-to-announce-all-americans-to-be-eligible-for-vaccinations-by-may-1-puts-the-nation-on-a-path-to-get-closer-to-normal-by-july-4th/. Published March 2021. Accessed September 12, 2022.
- 2.Centers for Disease Control and Prevention. COVID Data Tracker. Trends in COVID-19 vaccine confidence and coverage estimates.https://covid.cdc.gov/covid-data-tracker/#vaccine-confidence. Accessed January 21, 2022.
- 3.Barry V, Dasgupta S, Weller DL, et al. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity - United States, December 14, 2020–May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(22):818–824. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022. Wkly Epidemiol Rec. 2022;20(97):209–224. [Google Scholar]
- 5.Yasmin F, Najeeb H, Moeed A, et al. COVID-19 vaccine hesitancy in the United States: A systematic review. Front Public Health. 2021;9:770985. 10.3389/fpubh.2021.770985. [DOI] [PMC free article] [PubMed]
- 6.Centers for Disease Control and Prevention. What is vaccine confidence. https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/building-trust.html. Accessed January 21, 2022.
- 7.MacDonald NE, SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 8.Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLOS Curr. 2015;7:7. doi: 10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Data for action: achieving high uptake for COVID-19 vaccines. https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccination-demand-planning-2021.1. Published April 2021. Accessed April 16, 2022.
- 10.Brewer NT. What works to increase vaccination uptake. Acad Pediatr. 2021;21(4S):S9–S16. doi: 10.1016/j.acap.2021.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen KH, Yankey D, Lu PJ, et al. Report of health care provider recommendation for COVID-19 vaccination among adults, by recipient COVID-19 vaccination status and attitudes - United States, April–September 2021. MMWR Morb Mortal Wkly Rep. 2021;70(50):1723–1730. doi: 10.15585/mmwr.mm7050a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: A meta-analysis and systematic review. Prev Med. 2021;148 doi: 10.1016/j.ypmed.2021.106554. [DOI] [PubMed] [Google Scholar]
- 13.Eshun-Wilson I, Mody A, Tram KH, et al. Preferences for COVID-19 vaccine distribution strategies in the US: a discrete choice survey. PLOS ONE. 2021;16(8) doi: 10.1371/journal.pone.0256394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Omer SB, Benjamin RM, Brewer NT, et al. Promoting COVID-19 vaccine acceptance: recommendations from the Lancet Commission on Vaccine Refusal, Acceptance, and Demand in the USA. Lancet. 2021;398(10317):2186–2192. doi: 10.1016/S0140-6736(21)02507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen KH, Nguyen K, Corlin L, Allen JD, Chung M. Changes in COVID-19 vaccination receipt and intention to vaccinate by socioeconomic characteristics and geographic area, United States, January 6–March 29, 2021. Ann Med. 2021;53(1):1419–1428. doi: 10.1080/07853890.2021.1957998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baack BN, Abad N, Yankey D, et al. COVID-19 vaccination coverage and intent among adults aged 18–39 years - United States, March–May 2021. MMWR Morb Mortal Wkly Rep. 2021;70(25):928–933. doi: 10.15585/mmwr.mm7025e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szilagyi PG, Thomas K, Shah MD, et al. National trends in the US Public's likelihood of getting a COVID-19 vaccine-April 1 to December 8, 2020. JAMA. 2020;325(4):396–398. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021;21(4):1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ryerson AB, Rice CE, Hung MC, et al. Disparities in COVID-19 vaccination status, intent, and perceived access for noninstitutionalized adults, by disability status - national immunization survey adult COVID module, United States, May 30–June 26, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(39):1365–1371. doi: 10.15585/mmwr.mm7039a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. About the National Immunization Surveys. cdc.gov/vaccines/imz-managers/nis/about.html. Accessed January 21, 2022.
- 21.Centers for Disease Control and Prevention National immunization survey adult COVID module questionnaire Quarter 4. NORC. 2021 https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-ACM-Questionnaire-Q4-2021.pdf Accessed Oct 31, 2022. [Google Scholar]
- 22.Centers for Disease Control and Prevention . Research Data Center (RDC); 2022. National Center for Health Statistics.https://www.cdc.gov/rdc/index.htm Accessed April 18. [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85(11):867–872. doi: 10.2471/blt.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Federal poverty level (FPL). HealthCare.gov. https://www.healthcare.gov/glossary/federal-poverty-level-FPL/. Accessed April 16, 2022.
- 25.SAS Institute Inc . SAS/ACCESS® 9.4 Interface to ADABAS: Reference. SAS Institute Inc; Cary, NC: 2013. [Google Scholar]
- 26.SUDAAN (Release 11.0.3). 2018.
- 27.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLOS ONE. 2017;12(1) doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marquez C, Kerkhoff AD, Naso J, et al. A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx populations: from theory to practice. PLOS ONE. 2021;16(9) doi: 10.1371/journal.pone.0257111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.HHS. Awards $125 million in workforce grants for community-based efforts to bolster COVID-19 vaccinations in underserved. https://www.hhs.gov/about/news/2021/06/14/hhs-awards-125-million-in-workforce-grants-to-bolster-covid-19-vaccinations-in-underserved-communities.html. Published June 14, 2021. Accessed October 28, 2022.
- 30.Health Resources and Services Administration. What providers need to know about COVID-19 vaccine fees and reimbursements. https://www.hrsa.gov/sites/default/files/hrsa/coronavirus/provider-covid-vaccine-factsheet.pdf. Accessed April 16, 2022.
- 31.Velasquez DG, Suhas L, Richard, Pissaris A, Martin A. GOTVax: a novel mobile COVID-19 vaccine program. NEJM Catalyst Innovations in Care Delivery. 2021;2(3). 10.1056/CAT.21.0174. [DOI]
- 32.Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention's social vulnerability index. J Environ Health. 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 33.CDC. Behavioral risk factors surveillance system BRFSS. https://www.cdc.gov/brfss/annual_data/annual_2017.html. Accessed March 28, 2019.
- 34.Thompson ZM, Jain V, Chen YH, et al. State-Level Social Vulnerability Index and Healthcare Access in Patients with atherosclerotic cardiovascular Disease (from the BRFSS Survey) Am J Cardiol. 2022;178:149–153. doi: 10.1016/j.amjcard.2022.05.025. [DOI] [PubMed] [Google Scholar]
- 35.Agranov M, Elliott M, Ortoleva P. The importance of Social Norms against Strategic Effects: the case of Covid-19 vaccine uptake. Econ Lett. 2021;206 doi: 10.1016/j.econlet.2021.109979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graupensperger S, Abdallah DA, Lee CM. Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine. 2021;39(15):2060–2067. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinclair S, Agerstrom J. Do social norms influence young People's willingness to take the COVID-19 vaccine? Health Commun. 2023;38(1):152–159. doi: 10.1080/10410236.2021.1937832. [DOI] [PubMed] [Google Scholar]
- 38.Carson SL, Casillas A, Castellon-Lopez Y, et al. COVID-19 vaccine decision-making factors in racial and ethnic minority communities in los Angeles, California. JAMA Netw Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.27582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmidt H, Weintraub R, Williams MA, et al. Equitable allocation of COVID-19 vaccines in the United States. Nat Med. 2021;27(7):1298–1307. doi: 10.1038/s41591-021-01379-6. [DOI] [PubMed] [Google Scholar]
- 40.Long A, Mathew S, Alvarez KS, et al. Co-created messaging for influenza vaccination in a high-risk Hispanic community provides groundwork for COVID-19 vaccine. Health Equity. 2021;5(1):345–352. 10.1089/heq.2020.0132. [DOI] [PMC free article] [PubMed]
- 41.COVID-19 vaccination field guide: 12 strategies for your community. https://www.cdc.gov/vaccines/covid-19/downloads/vaccination-strategies.pdf. Accessed February 14, 2022.
- 42.Ohlsen EC, Yankey D, Pezzi C, et al. Coronavirus disease 2019 (COVID-19) vaccination coverage, intentions, attitudes, and barriers by race/ethnicity, language of interview, and nativity-national immunization survey adult COVID module, 22 April 2021–29 January 2022. Clin Infect Dis. 2022;75(Suppl 2):S182–S192. doi: 10.1093/cid/ciac508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kriss JL, Hung MC, Srivastav A, et al. COVID-19 vaccination coverage, by race and ethnicity - national immunization survey adult COVID module, United States, December 2020–November 2021. MMWR Morb Mortal Wkly Rep. 2022;71(23):757–763. doi: 10.15585/mmwr.mm7123a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reitsma MB, Goldhaber-Fiebert JD, Salomon JA. Quantifying and benchmarking disparities in COVID-19 vaccination rates by race and ethnicity. JAMA Netw Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.30343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Szilagyi PG, Thomas K, Shah MD, et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: results from a national survey. Prev Med. 2021;153 doi: 10.1016/j.ypmed.2021.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Purvis RS, Hallgren E, Moore RA, et al. Trusted sources of COVID-19 vaccine information among hesitant adopters in the United States. Vaccines (Basel). 2021;9(12):1418. 10.3390/vaccines9121418. [DOI] [PMC free article] [PubMed]
- 47.Thompson HS, Manning M, Mitchell J, et al. Factors associated with racial/ethnic group-based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Blendon RJ, Benson JM, Hero JO. Public trust in physicians–U.S. medicine in international perspective. N Engl J Med. 2014;371(17):1570–1572. doi: 10.1056/NEJMp1407373. [DOI] [PubMed] [Google Scholar]
- 49.Zimmerman RK, Santibanez TA, Janosky JE, et al. What affects influenza vaccination rates among older patients? An analysis from inner-city, suburban, rural, and Veterans Affairs practices. Am J Med. 2003;114(1):31–38. doi: 10.1016/s0002-9343(02)01421-3. [DOI] [PubMed] [Google Scholar]
- 50.Brewer NT, Abad N. Ways that mental health professionals can encourage COVID-19 vaccination. JAMA Psychiatry. 2021;78(12):1301–1302. doi: 10.1001/jamapsychiatry.2021.2951. [DOI] [PubMed] [Google Scholar]
- 51.Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dempsey AF, Pyrzanowski J, Campagna EJ, Lockhart S, ST O'Leary. Parent report of provider HPV vaccine communication strategies used during a randomized, controlled trial of a provider communication intervention. Vaccine. 2019;37(10):1307–1312. doi: 10.1016/j.vaccine.2019.01.051. [DOI] [PubMed] [Google Scholar]
- 53.Reno JE, O'Leary S, Garrett K, et al. Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun. 2018;23(4):313–320. doi: 10.1080/10810730.2018.1442530. [DOI] [PubMed] [Google Scholar]
- 54.Kelly MK, Grundmeier RW, Stephens-Shields AJ, et al. Missed opportunities for human papillomavirus vaccination at office visits during which influenza vaccine was administered: an AAP pediatric research in office settings (PROS) national primary care research network study. Vaccine. 2020;38(33):5105–5108. doi: 10.1016/j.vaccine.2020.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics. 2017;139(1) doi: 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- 57.Schoch-Spana M, Brunson EK, Long R, et al. The public's role in COVID-19 vaccination: human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 2021;39(40):6004–6012. doi: 10.1016/j.vaccine.2020.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee JT, Sean Hu S, Zhou T, et al. Employer requirements and COVID-19 vaccination and attitudes among healthcare personnel in the U.S.: findings from National Immunization Survey Adult COVID Module, August–September 2021. Vaccine. 2022;40(51):7476–7482. doi: 10.1016/j.vaccine.2022.06.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Omer SB, Betsch C, Leask J. Mandate vaccination with care. Nature. 2019;571(7766):469–472. doi: 10.1038/d41586-019-02232-0. [DOI] [PubMed] [Google Scholar]
- 60.Brewer NT, Buttenheim AM, Clinton CV, et al. Incentives for COVID-19 vaccination. Lancet Reg Health Am. 2022;8 doi: 10.1016/j.lana.2022.100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wolter KK, Smith PJ, Khare M, et al. Statistical methodology of the national immunization survey, 2005–2014. Vital Health Stat 1. 2017;61(61):1–107. [PubMed] [Google Scholar]
- 62.Siegler AJ, Luisi N, Hall EW, et al. Trajectory of COVID-19 vaccine hesitancy over time and association of initial vaccine hesitancy with subsequent vaccination. JAMA Netw Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.26882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Masters NB, Zhou T, Meng L, et al. Geographic heterogeneity in behavioral and social drivers of COVID-19 vaccination. Am J Prev Med. 2022;63(6):883–893. doi: 10.1016/j.amepre.2022.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.