Abstract
Background:
We examined the relationships of compassion satisfaction and fatigue among shift nurses on nursing engagement activities related to patient safety with the aim of improving shift nurses’ physical and psychological aspects in order to use the findings as a basis to enhance nurses’ engagement in activities related to patient safety.
Methods:
The data collection period for this cross-sectional study was from Nov 21, 2019, to Jan 3, 2020. A convenience sample of 280 shift nurses who were working for more than six months at three tertiary hospitals in Korea was used. Collected data comprised general and job-related characteristics of subjects, compassion satisfaction, compassion fatigue, and patient safety nursing activities. SPSS was used for statistical analysis, and multiple regression analysis was used to examine the relationship between shift nurses’ compassion satisfaction, compassion fatigue, and patient safety nursing activities
Results:
Compassion satisfaction had the greatest impact on engagement in nursing activities related to patient safety (β= .32, P<.001), followed by compassion fatigue. Higher compassion satisfaction and lower compassion fatigue indicates a higher engagement in patient safety-related nursing activities (β= −.15, P<.008).
Conclusion:
In order to maximize compassion satisfaction and reduce compassion fatigue among shift nurses, it is important for health policymakers to improve their welfare system and create a supportive environment where negative emotions can be expressed freely and accepted positively.
Keywords: Compassion fatigue, Compassion satisfaction, Nursing, Patient safety
Introduction
Patient safety accidents refer to damage inflicted on patients during the process of delivering medical services, which may result in high medical costs and endanger patients’ lives (1). Worldwide, approximately 134 million adverse events occur each year, resulting in 2.6 million deaths annually (2). A Korean statistical yearbook on patient safety reported that the number of patient safety accidents increased approximately three-fold in a three-year period, from 3,864 in 2017 to 11,953 in 2019 (3). Approximately 9.2% of these accidents were caused by mistakes or carelessness among medical staff, and 43.5% were preventable (3). Ensuring patient safety is a critical challenge in the healthcare setting (4).
Nurses are healthcare professionals working in close proximity to patients and, therefore, must be aware of their safety. They play a central role in ensuring patient safety by identifying and preventing risks to patients (1). Ensuring patient safety by improving nurses’ engagement in nursing-related activities may directly translate to positive patient outcomes. Thus, the physical and psychological stability of nurses has an important impact on their engagement in nursing activities (5).
Nurses often experience compassion fatigue as they form an empathetic relationship with patients and begin to empathize with their pain. Compassion fatigue is a type of secondary traumatic stress that can be experienced when helping others and does not imply being physically harmed or endangered (6). Nurses with compassion fatigue experience physical and psychological symptoms including headache, indigestion, sleep disorders, fatigue, depression, and apathy and may provide reduced care for their patients (7). Continued compassion fatigue leads to the inability to perform tasks objectively (8) and make professional judgments, incorrect understanding of a patient’s condition, and increased fear of and reduced care for patients (9,10). Compassion fatigue eventually leads nurses to neglect their patients, thus compromising patient safety (11,12). Over 50% of nurses in South Korea experience compassion fatigue (13,14). The early detection and prevention of compassion fatigue is important because it is treatable.
Nursing professionals can also experience compassion satisfaction, a positive emotion. Compassion satisfaction is the sense of pleasure that comes from helping others (15–17). In previous research, a caring nurse–patient relationship emerged as one of the most important predictors of not only patient satisfaction with hospitals, but also patients’ global outcomes and patient safety in healthcare systems (18,19). High compassion satisfaction allows nurses to form close relationships with patients. Moreover, empathy enhances nurses’ nursing abilities and creates a positive work environment that improves organizational commitment, nursing care quality, and nurses’ professionalism (16,17). Thus, it is necessary to reduce compassion fatigue and improve compassion satisfaction among nurses.
Studies have consistently investigated the factors affecting nurses’ engagement in nursing activities related to patient safety (18–20). However, research is lacking on the relationship of compassion fatigue and compassion satisfaction on engagement in nursing activities related to patient safety. Therefore, we aimed to determine the level of compassion fatigue, the level of compassion satisfaction, and patient safety nursing activities and examine their relationships among shift nurses, in addition, provide basic data for establishing a strategy that can promote patient safety nursing activities from a nurse’s perspective.
Methods
Study Design
This was a cross-sectional study to investigate the relationship between compassion satisfaction and fatigue with shift nurses’ patient safety-related activities.
Participants
The participants of this study were shift nurses working in three tertiary hospitals with more than 300 beds in Korea extracted via convenience sampling. The inclusion criteria were: 1) having worked at a hospital for at least six months and 2) being responsible for providing direct nursing care with shift duty at a general hospital. The exclusion criteria were: 1) having been diagnosed with a sleep disorder in the last six months, 2) administrative nurses whose positions were of a head nurse or above, 3) nurses who did not provide direct nursing care, 4) nurses who did not work in shifts, and 5) refusal to participate in the study. The necessary sample size was determined to be 194, with an effect size of 0.15, significance level of 0.05, and test power of 95%. The sample size calculation was performed using the G*power 3.1.9.2 program.
Data Collection
Data were collected from Nov 21, 2019, to Jan 3, 2020. The researchers directly informed the participating nurses of the purpose and methods of this study and provided them with self-report questionnaires after receiving their written consent to participate in the study.
Ethical approval
This study was approved by the Institutional Review Board of D University (IRB No. DGU IRB 20190018–01).
Statistical Analysis
The data collected in this study were analyzed using SPSS/WIN 25.0 (IBM Corp., Armonk, NY, USA). Differences in variables were analyzed according to general and occupational characteristics using the independent t-test and one-way ANOVA, with the Duncan test used for post-hoc analysis. The relationships of compassion fatigue and compassion satisfaction on engagement in nursing activities were analyzed using multiple regression.
Tools
Participants’ Demographic and Job-Related Characteristics
The data collected as general characteristics of the participants were age (in years), gender, religion, marital status, education, living situation, regularity of exercise, disease being treated, drug taking, and subjective health status. Job-related data included clinical experience, working unit, number of monthly night duty shifts, and subjective career stress.
Compassion Fatigue
Compassion fatigue was assessed using the Professional Quality of Life Scale, Compassion Satisfaction/Fatigue subscale ver. 5. Each question was rated on a 5-point Likert scale, with total scores ranging from 10 to 50 points. Scores ≤ 22 points indicated a low level of compassion fatigue, scores ranging from 23–41 indicated an intermediate level of compassion fatigue, and scores ≥ 42 points indicated high levels of compassion fatigue (21). Cronbach’s α for this tool was 0.80 in Stamm (21) and 0.78 in the present study.
Compassion Satisfaction
Compassion satisfaction was assessed using the Professional Quality of Life Scale, Fatigue subscale version 5, adapted in Korean by Kim and Yom (15) and modified by Stamm (21) from the Compassion Satisfaction/Fatigue self-test for helpers, developed by Figley (7). Each question was rated on a 5-point Likert scale, with total scores ranging from 10 to 50 points. Scores ≤ 22 points indicated a low level of compassion satisfaction, scores ranging from 23–42 indicated an intermediate level of compassion satisfaction, and scores ≥ 42 indicated a high level of compassion satisfaction (21). Cronbach’s α for this tool was 0.88 in Stamm (21) and 0.92 in the present study.
Patient Safety Nursing Activities
Levels of nursing activities related to patient safety were assessed using a patient safety management activity tool developed by Lee (22) through a literature review on the standards related to patient safety management, which also included the Joint Commission Accreditation of Healthcare Organization standards. The tool consists of 46 questions rated on a 5-point Likert scale, covering 10 domains: patient examination, communication, verbal and phone call prescription, drug administration, nursing care following surgical procedures, safe environment, infection prevention, fall prevention, bedsore prevention, and risk management/emergency situations. Cronbach’s α for this tool was 0.95 at the time of development and 0.95 in the present study.
Results
Dependent Variable Differences according to General and Occupational Characteristics
The average age of the participants of this study was 28.2 (±5.75) yr, and 265 (94.6%) of the total 280 participants were female nurses.
Table 1 shows Differences among compassion satisfaction, fatigue and patient safety-related activities according to general and job-related characteristics of subjects.
Table 1:
Differences according to general and job-related characteristics of subjects (N=280)
| Characteristics | Categories | n (%) | CF | CS | PSNA | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| M±SD | F or t (p) | M±SD | F or t (p) | M±SD | F or t (p) | |||
| Age (yr) | <25a | 82(29.3) | 2.48±0.62 | 0.57 (.565) | 3.03±0.78 | 1.44 (.238) | 4.25±0.64 | 0.13 (.881) |
| 25–<30b | 116(41.4) | 2.55±0.55 | 2.94±0.66 | 3.98±0.54 | ||||
| ≥30c | 82(29.3) | 2.57±0.50 | 3.05±0.65 | 4.00±0.47 | ||||
| M±SD | 28.20±5.75 | |||||||
| Gender | Male | 15(5.4) | 2.35±0.52 | 0.96 (.184) | 2.90±0.68 | 0.67 (.640) | 4.01±0.57 | 1.88 (.061) |
| Female | 265(94.6) | 2.55±0.56 | 2.91±0.67 | 3.97±0.58 | ||||
| Religion | No | 172(61.4) | 2.53±0.60 | −0.14 (.892) | 2.85±0.65 | −3.20 (.002) * | 3.95±0.55 | −1.51 (.132) |
| Yes | 108(38.6) | 2.54±0.49 | 3.11±0.66 | 4.05±0.53 | ||||
| Marital status | Single | 223(79.6) | 2.52±0.55 | −0.96 (.338) | 2.90±0.66 | −2.61 (.009) * | 3.98±0.56 | −0.39 (.695) |
| Married | 57(20.4) | 2.60±0.57 | 3.15±0.66 | 4.02±0.48 | ||||
| Education | Diplomaa | 117(41.8) | 2.55±0.56 | 0.09 (.914) | 2.87±0.62 | 3.07 (.048)
*
a,b<c |
3.94±0.56 | 0.85 (.429) |
| Bachelor’sb | 159(56.8) | 2.53±0.56 | 2.99±0.69 | 4.02±0.54 | ||||
| ≥Master’sc | 4(1.4) | 2.62±0.33 | 3.60±0.49 | 4.12±0.29 | ||||
| Living with | Alone | 74(26.4) | 2.51±0.53 | 0.16 (.855) | 2.91±0.69 | 0.37 (.694) | 3.97±0.57 | 0.96 (.384) |
| Family | 139(49.7) | 2.55±0.54 | 2.94±0.66 | 3.97±0.51 | ||||
| Friend | 67(23.9) | 2.54±0.63 | 3.01±0.67 | 4.07±0.59 | ||||
| Regular exercise | No | 119(42.5) | 2.55±0.54 | 0.25 (.802) | 2.86±0.66 | −1.96 (.051) | 3.90±0.50 | −2.33 (.020) * |
| Yes | 161(57.5) | 2.53±0.57 | 3.02±0.67 | 4.06±0.57 | ||||
| Disease being treated | Yes | 3(1.1) | 2.86±0.20 | −1.01 (.315) | 2.86±0.47 | 0.23 (.821) | 3.97±0.27 | 0.08 (.937) |
| Medication | Yes | 4(1.4) | 2.60±0.55 | −0.21 (.834) | 2.67±0.54 | 0.84 (.403) | 3.90±0.25 | 0.32 (.747) |
| Subjective’ health status | Gooda | 75(26.8) | 2.53±0.68 | 0.88 (.415) | 3.12±0.72 | 3.59 (.029)
*
b<a |
4.12±0.58 | 2.73 (.067) |
| Moderateb | 177(63.2) | 2.52±0.50 | 2.87±0.61 | 3.95±0.53 | ||||
| Poorc | 28(10.0) | 2.67±0.54 | 2.99±0.76 | 3.91±0.52 | ||||
| Clinical experience (year) | <2 | 108(38.6) | 2.48±0.55 | 0.83 (.437) | 2.85±0.63 | 1.78 (.171) | 4.03±0.56 | 0.57 (.568) |
| 2–<5 | 76(27.1) | 2.56±0.56 | 3.00±0.71 | 3.95±0.58 | ||||
| ≥5 | 96(34.3) | 2.58±0.56 | 3.01±0.67 | 3.98±0.50 | ||||
| Working unit | Ward | 221(78.9) | 2.50±0.53 | 0.93 (.464) | 2.96±0.62 | 1.15 (.334) | 3.96±0.54 | 1.44 (.210) |
| ICU | 30(10.7) | 2.52±0.47 | 2.97±0.56 | 4.23±0.45 | ||||
| ED | 29(10.4) | 2.57±0.52 | 3.14±0.67 | 4.01±0.47 | ||||
| Number of night duties (Monthly) | ≤6 | 95(33.9) | 2.52±0.66 | 0.95 (.421) | 2.96±0.74 | 0.71 (.547) | 3.95±0.59 | 0.54 (.658) |
| 7–8 | 138(49.3) | 2.52±0.48 | 2.91±0.60 | 4.03±0.53 | ||||
| ≥9 | 47(16.8) | 2.65±0.57 | 3.07±0.73 | 3.96±0.52 | ||||
| Subjective career stress | Heavya | 189(67.5) | 2.61±0.59 | 7.36 (.001)
*
c<b,a |
2.86±0.68 | 5.51 (.004) * | 3.94±0.54 | 5.63 (.004) * |
| Moderateb | 83(29.6) | 2.42±0.43 | 3.12±0.61 | 4.07±0.55 | ||||
| Lightc | 8(2.9) | 2.20±0.57 | 3.28±0.40 | a<c | 4,52±0.34 | a,b<c | ||
M=mean; SD=standard deviation; CF=compassion fatigue; CS=compassion satisfaction; PSNA= patient safety nursing activities; ICU=intensive care unit; ED=emergency
Values were analyzed by Sheffe test
A significant difference in the level of compassion fatigue was found between the shift nurses who responded that they experienced intermediate to high levels of occupational stress compared to those who did not (F=7.36, P<.001; Table 1). Religious shift nurses (F= −3.20, P=.002) and those who completed graduate studies or above had significantly higher levels of compassion satisfaction (F=3.07, P=.048). Nurses with low subjective levels of occupational stress had high levels of compassion satisfaction (F=5.51, P=.004) and significantly high levels of nursing activities related to patient safety (F=5.63, P=.004).
Table 2 shows the levels of compassion fatigue, compassion satisfaction, and engagement in nursing activities related to patient safety among the participants.
Table 2:
Compassion fatigue, compassion satisfaction and patient safety nursing activities of participants (N=280)
| Variables | Range | M±SD |
|---|---|---|
|
| ||
| Min-Max | ||
| CF (10 items) | 10∼50 | 25.41±5.63 |
| CS (10 items) | 11∼50 | 29.54±6.72 |
| PSNA (46 items) | 2.35∼5.00 | 3.99±0.55 |
M= Mean; SD=Standard deviation; CF=Compassion Fatigue; CS=Compassion Satisfaction; PSNA= Patient Safety
Nursing Activities
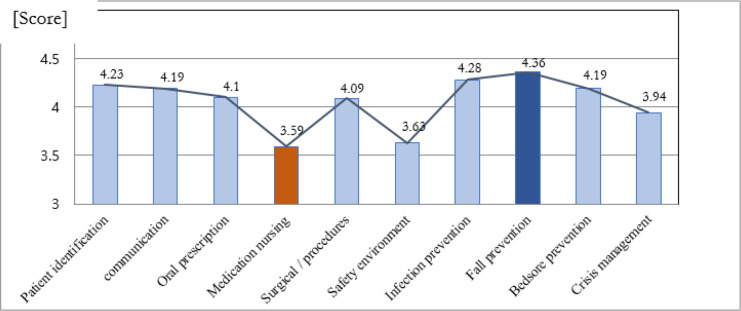
The scores of the 10 subdomains of patient safety nursing activities are shown in Fig. 1.
Fig. 1:
Scores for shift nurses’ patient safety-related nursing activities
Among the sub-domains of 10, the area with the highest score was the fall prevention activity area with 4.36 out of 5 points, and the area with the lowest score was identified as medication nursing with 3.59 points.
Factors Affecting Nursing Activities Related to Patient Safety
A multiple regression analysis was performed to investigate the factors affecting nursing activities related to patient safety, with work experience as a confounder and physical activities, subjective levels of occupational stress, compassion fatigue, and compassion satisfaction as independent factors.
The model was significantly associated with the level of engagement in nursing activities related to patient safety (F=7.93, P<.001). Moreover, compassion satisfaction (β = .32, P<.001) had the highest impact on engagement in nursing activities related to patient safety, followed by compassion fatigue (β= −.15, P<.008) (Table 3).
Table 3:
Factors influencing participants’ patient safety-related nursing activities (N=280)
| Variables | B | SE | β | t | P |
|---|---|---|---|---|---|
| Clinical experience (yr) | −0.01 | 0.01 | −0.01 | −0.14 | .889 |
| Regular exercise | 0.11 | 0.06 | 0.10 | 1.68 | .095 |
| CF | −0.15 | 0.06 | −0.16 | −2.67 | .008 |
| CS | 0.32 | 0.05 | 0.32 | 5.52 | <.001 |
Model fit: R2=.15, Adj. R2=.130, F=7.93, P<.001, Durbin-Watson 1.64 CF=compassion fatigue; CS=compassion satisfaction
Discussion
In the current study, compassion satisfaction and compassion fatigue were found to affect shift nurses’ engagement in nursing activities related to patient safety in general hospitals. Of these, compassion satisfaction had the greatest impact on nursing activities related to patient safety. The mean compassion satisfaction score was 29.54 (±6.72) out of 50 points, corresponding to intermediate levels of compassion satisfaction. This was close to the score reported by Lee et al. (23) but lower than the 37.94 points reported earlier (8, 24), who assessed clinical nurses abroad, indicating that South Korean nurses have lower levels of compassion satisfaction.
Empathy is an important factor that enhances nurses’ sensitivity and responsiveness to patient needs, thereby increasing patient safety. Nurses who are highly sensitive to risks have been shown to experience fewer near misses (25, 26). Furthermore, compassion satisfaction has been shown to increase job satisfaction (27), which affects a patient prognosis by helping nurses positively accept their work environment and reduce harmful accidents (28). Improved job satisfaction increases organizational commitment, which results in better emotional stability and reduced emotional fatigue by effective communication with team members (29). The results in the current study support this conclusion.
In the current study, after compassion satisfaction, compassion fatigue was found to have the greatest impact on shift nurses’ engagement in nursing activities related to patient safety. Their mean score for compassion fatigue was 25.41 (±5.63) out of 50 points, corresponding to intermediate levels of compassion fatigue (intermediate level: 23–41). The score was lower than those reported (28.53 points) (30) and (28.8 points) (31), who measured compassion fatigue among nurses in general hospitals. Considering the compassion fatigue scores of 22.41–22.65 points reported (32), who assessed oncology nurses in the United States and Canada, the nurses in the present study had relatively high levels of compassion fatigue. These results may reflect the current situation in which clinical nurses are forced to suppress their emotions and opinions at work due to growing emphasis on customer service within medical institutions (33), which gradually increases compassion fatigue.
Nurses with higher levels of compassion fatigue have lower levels of engagement. Compassion fatigue causes physical fatigue and sleep disorders and can lead to impaired professional judgment, incorrect understanding of a patient’s conditions, and lack of care for patients, resulting in mistakes, increased turnover rates, and reduced nursing productivity (12, 30, 31). Compassion fatigue compromises a nurse’s ability to perform tasks, increases the risks of mistakes or harm, and causes the inability to psychologically and physically adapt to work environments (11, 12). Therefore, consistent education and management are needed to identify factors associated with compassion fatigue and enhance positive emotions, thereby preventing and reducing compassion fatigue.
Repeated research that considers the various environmental characteristics of multiple institutions is needed to confirm the level of compassion fatigue among nurses, since compassion fatigue is affected by personal situations or characteristics, the environment in which nursing care is provided, variations in occupational situations in the workplace environment, and sociocultural characteristics of individual hospitals. Systematic research is needed to investigate the inducing factors, along with interventions that can reduce compassion fatigue in current nursing situations.
In the present study, nurses with good subjective health obtained higher compassion satisfaction scores than did those with poor subjective health. This result is similar to that of a previous study that examined the relationship between subjective health status and compassion satisfaction in doctors and nurses working in general hospitals (32). These results were obtained because subjective health status has an important impact on the care nurses provide for their patients. Nurses with good subjective health experience higher levels of compassion satisfaction when helping others (34). Thus, hospitals need financial systems that help nurses manage their own mental health. Nurses themselves must make use of their leisure time and engage in physical activities, such as regular stretching, to assist with mental health. Since subjective occupational stress affects compassion satisfaction (35), nurses with high levels of occupational stress experience difficulties providing high-quality nursing care and may have reduced compassion satisfaction (36). These nurses must explore methods to manage and cope with occupational stress to improve their compassion satisfaction.
This study has a few limitations. First, shift nurses from three general hospitals in certain regions of South Korea were included by convenience sampling and therefore cannot represent nurses from all medical institutions across the country; thus, the results of this study should be generalized with caution. Second, this study examined the individual characteristics related to compassion satisfaction, compassion fatigue, and nursing activities related to patient safety among shift nurses and did not consider organizational variables such as managers’ attitudes and workplace culture. Further research on nursing activities related to patient safety considering these variables is needed. Third, since this was a cross-sectional study using self-report questionnaires, causal inferences cannot be drawn. Despite these limitations, this study may provide basic research data that can be used to develop methods to enhance shift nurses’ job satisfaction and engagement in nursing activities related to patient safety.
Implications for Nursing and Health Policy
Nurses’ psychological well-being is related to turnover intention (31) and can affect the performance and development of hospital organizations. Nurses’ compassion fatigue and burnout not only harms their own health but also has a significant relationship with patient safety, by creating a hazardous environment and affecting patient satisfaction. It is necessary for shift nurses to identify negative factors that can lead to burnout early and prepare self-management interventions to resolve them. From an organizational perspective, it is important for hospital policymakers to improve welfare systems and create a supportive environment in which negative emotions can be communicated freely so as to improve empathy, which is a positive reward. This will be an effective human resource management policy for the three-shift nursing system to improve nurses’ physical and psychological well-being and quality of life at work, as it will allow nurses to take care of patients more comfortably and safely, thereby obtaining positive patient outcomes.
Conclusion
Maximizing compassion satisfaction and minimizing compassion fatigue among shift nurses were found to improve nurses’ engagement in nursing activities related to patient safety. Based on these results, this study makes two suggestions. First, further research is required to develop an intervention program that can efficiently increase compassion satisfaction and manage compassion fatigue among shift nurses and verify its effects. Second, a follow-up study identifying various factors associated with shift nurses’ nursing activities related to patient safety is needed.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This paper was supported by Bumsuk Academic Research Fund in 2021
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.World Health Organization (2017). Patient safety: making health care safer. World Health Organization. [Google Scholar]
- 2.Donaldson L, Ricciardi W, Sheridan S, et al. (2021). Textbook of patient safety and clinical risk management. Cham, Switzerland: Springer Nature. [PubMed] [Google Scholar]
- 3.Patient Safety Statistical Yearbook (2019). https://mdon.co.kr/news/article.html?no=27598 (in Korean).
- 4.Lee SI. (2013). The necessity and direction of enactment of the Patient Safety Act. Health Policy Forum, 11(2):37–42. [Google Scholar]
- 5.Garcia CDL, Abreu LCD, Ramos JLS, et al. (2019). Influence of burnout on patient safety: systematic review and meta-analysis. Medicina (Kaunas), 55 (9): 553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gómez-Salgado J, Navarro-Abal Y, López-López MJ, et al. (2019). Engagement, passion and meaning of work as modulating variables in nursing: a theoretical analysis. Int J Environ Res Public Health, 16 (1): 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Figley CR. (1995). Compassion fatigue. coping with secondary traumatic stress disorder in those who treat the traumatized. Brunner/Mazel. New York. [Google Scholar]
- 8.Kelly L, Runge J, Spencer C. (2015). Predictors of compassion fatigue and compassion satisfaction in acute care nurses. J Nurs Scholarsh, 47 (6): 522–8. [DOI] [PubMed] [Google Scholar]
- 9.Jin M, Wang J, Zeng L, et al. (2021). Prevalence and factors of compassion fatigue among nurse in China: a protocol for systematic review and meta-analysis. Medicine (Baltimore), 100 (3): e24289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duarte J, Pinto-Gouveia J. (2017). The role of psychological factors in oncology nurses’ burnout and compassion fatigue symptoms. Eur J Oncol Nurs, 28: 114–21. [DOI] [PubMed] [Google Scholar]
- 11.Nolte AG, Downing C, Temane A, Hastings-Tolsma M. (2017). Compassion fatigue in nurses: a metasynthesis. J Clin Nurs, 26 (23–24): 4364–78. [DOI] [PubMed] [Google Scholar]
- 12.Alharbi J, Jackson D, Usher K. (2020). Personal characteristics, coping strategies, and resilience impact on compassion fatigue in critical care nurses: a cross-sectional study. Nurs Health Sci, 22: 20–7. [DOI] [PubMed] [Google Scholar]
- 13.Peters E. (2018). Compassion fatigue in nursing: a concept analysis. Nurs Forum, 53 (4): 466–80. [DOI] [PubMed] [Google Scholar]
- 14.Han MY, Lee MS, Bae JY, Kim YS. (2015). Effects of nursing practice environment, compassion fatigue and compassion satisfaction on burnout in clinical nurses. J Korean Acad Nurs Adm, 21 (2): 193–202. [Google Scholar]
- 15.Lee JM, Yom YH. (2013). Effects of work stress, compassion fatigue, and compassion satisfaction on burnout in clinical nurses. J Korean Acad Nurs Adm, 19 (5): 689–97. [Google Scholar]
- 16.Hunsaker S, Chen HC, Maughan D, Heaston S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J Nurs Scholarsh, 47 (2): 186–94. [DOI] [PubMed] [Google Scholar]
- 17.Sacco T, Ciurzynksi S, Harvey ME, Ingersoll G. (2015). Compassion satisfaction and compassion fatigue among critical care nurses. Crit Care Nurse, 35(4):32–43. [DOI] [PubMed] [Google Scholar]
- 18.Hooper C, Craig F, Janvrin D, et al. (2010). Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J Emerg Nurs, 36 (5): 420–427. [DOI] [PubMed] [Google Scholar]
- 19.Ausserhofer D, Schubert M, Desmedt M, et al. (2013). The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: A cross-sectional survey. Int J Nurs Stud, 50(2): 240–252. [DOI] [PubMed] [Google Scholar]
- 20.Sacco TL, Copel LC. (2018). Compassion satisfaction: a concept analysis in nursing. Nurs Forum, 53: 76–83. [DOI] [PubMed] [Google Scholar]
- 21.Stamm BH. (2012). Helping the helpers: compassion satisfaction and compassion fatigue in Self-care, management, and policy. In Resources for Community Suicide Prevention. Eds, Kirkwood AD, Stamm BH. Idaho State University, Meridian and Pocatello, ID, pp 1–4. [Google Scholar]
- 22.Yoo HN, Lee HY. (2014). The initial application of the patient safety management activity scale (PSM-A) for nursing students: Brief on reliability and validity. J Korean Data Analysis Society, 16(6):3423–3436. [Google Scholar]
- 23.Lee Y.M., Lee H.H, Jung J.H, Yang JK, et al. (2018). A study about compassion fatigue, compassion satisfaction and burnout in comprehensive nursing care and general ward nurses. J Korean Clin Nurs Res, 24(2):188–196. [Google Scholar]
- 24.Salimi S, Pakpour V, Rahmani A, et al. (2020). Compassion satisfaction, burnout, and secondary traumatic stress among critical care nurses in Iran. J Transcult Nurs, 31: 59–66. [DOI] [PubMed] [Google Scholar]
- 25.Lee SS, Choi HR. (2019). Convergence influences of nurses’ professional autonomy and empathy on patient safety culture. J Digit Converg, 17 (2): 231–41. [Google Scholar]
- 26.Park JH, Lee EN. (2019). Influencing factors and consequences of near miss experience in nurses’ medication error. J Korean Acad Nurs, 49 (5): 631–42. [DOI] [PubMed] [Google Scholar]
- 27.Lee SN, Kim JA. (2016). Analysis of research on compassion satisfaction among nurses. J Korea Academia-Industrial Cooperation Society, 17 (9): 599–609. [Google Scholar]
- 28.Craig CD, Sprang G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety Stress Coping, 23 (3): 319–39. [DOI] [PubMed] [Google Scholar]
- 29.Loan L. (2020). The influence of organizational commitment on employees’ job performance: The mediating role of job satisfaction. Management Science Letters, 10(14):3307–3312. [Google Scholar]
- 30.Jeong E, Jung MR. (2018). Influences of compassion satisfaction, compassion fatigue, and burnout on positive psychological capital of clinical nurses. J Korea Contents Assoc, 18 (3): 246–55. [Google Scholar]
- 31.Stacey W, Singh-Carlson S, Odell A, et al. (2016). Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncol Nurs Forum, 43 (4): E161–9. [DOI] [PubMed] [Google Scholar]
- 32.Sung KW, Jo KH. (2010). Perceived hurts and forgiveness in clinical nurses - the status and influencing variables. J Korean Acad Nurs Adm, 16 (4): 428–36. [Google Scholar]
- 33.Matheson A, O’Brien L, Reid JA. (2014). The impact of shiftwork on health: a literature review. J Clin Nurs, 23(23–24):3309–3320. [DOI] [PubMed] [Google Scholar]
- 34.Jarrad R, Hammad S, Shawashi T, Mahmoud N. (2018). Compassion fatigue and substance use among nurses. Ann Gen Psychiatry, 17:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pang Y, Dan Y, Jung H, et al. (2020). Depressive symptoms, professional quality of life and turnover intention in Korean nurses. Int Nurs Rev, 67 (3): 387–94. [DOI] [PubMed] [Google Scholar]
- 36.Smart D, English A, James J, et al. (2014). Compassion fatigue and satisfaction: cross-sectional survey among US healthcare workers. Nurs Health Sci, 16: 3–10. [DOI] [PubMed] [Google Scholar]