Abstract
Aim
To examine effects of holistic sleep improvement strategies on frontline nurses who served in Wuhan, China, during a public health emergency (COVID‐19).
Design
A pre–post‐test design with single group was conducted with a convenience sample applied the Transparent Reporting of Evaluations with Non‐randomized Designs statement.
Methods
Fifty‐two nurses were recruited from a COVID‐19 designated hospital, receiving holistic sleep improvement intervention, which concentrated on scientific human resource management, comfortable sleep environment establishment, self‐relaxation and self‐adjustment training and humanistic care. Data was collected at baseline and 4‐week follow‐up post intervention using self‐reported questionnaires.
Results
The total score of Pittsburgh Sleep Quality Index scale was 8.69 ± 4.346 at baseline. After 4 weeks of follow‐up, the score statistically significantly decreased to 7.48 ± 3.691. Subjective sleep quality (p = .016), sleep efficiency (p = .015), sleep disturbances (p = .007) were statistically significantly improved after the intervention, while there were no statistically significant differences in sleep latency (p = .205), sleep duration (p = .375), sleep medication (p = .723) or daytime dysfunction (p = .747).
Keywords: COVID‐19 pandemic, nurse, nursing, public health emergency, sleep, sleep quality
1. INTRODUCTION
In the past few months, COVID‐19 spread all over the world, which attracted the attention of national and local governments. On January 20th, 2020, COVID‐19 was included in Class B infectious diseases and managed according to Class A in China (National Health Commission of the People's Republic of China, 2020). And on the evening of January 30th, the World Health Organization (WHO) announced that the novel coronavirus epidemic was listed as a public health emergency of international concern (WHO, 2020a). After the promulgation of “International Health Regulations” in 2007, WHO has announced only six public health emergencies, the first five of which were H1N1 influenza in 2009, the polio in 2014, Ebola outbreak in West Africa in 2014, the “Zika” in 2015–2016, and the Ebola outbreak in Congo (DRC), which began in 2018. The COVID‐19 belongs to the same coronavirus group as the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) viruses that caused two of the more severe epidemics in recent years.
According to WHO's latest real‐time statistics on February 4th of 2021, there were a total of 103,631,793 confirmed cases and 2,251,613 deaths by COVID‐19 worldwide. Apart from China, there are 222 countries, regions or territories reporting COVID‐19 cases in the world (WHO, 2020b). COVID‐19 is such a highly contagious disease and capable of high human transmission. To protect against the COVID‐19 pandemic, the WHO proposed intervening guidance that included movement restrictions, isolation, restriction of national and international travel or movement, and full or partial closure of organizations and institutions (WHO, 2021). National Health Service organizations all over the world had made a series of modifications to prevent the spread of COVID‐19 and to treat the confirmed and suspected cases (Simonetti et al., 2021). In China, at the beginning of the outbreak, the General Office of the State Health Commission issued a plan for the prevention and control of COVID‐19 pandemic, requiring the improvement of epidemic information surveillance reports, timely detection and reporting of COVID‐19 cases, and standardizing the management of close contacts, guiding the public and specific groups to do personal protection, strictly implementing the disinfection of specific places, to achieve the goal of reducing the mortality and reducing the harmful influence to public health (General Office of the State Health Commission, 2020).
Since the outbreak of COVID‐19, several designated hospitals and “Fangcang” shelter hospitals have been set up immediately in China. At the same time, professional medical teams have been organized to treat and nurse patients suspected or confirmed with COVID‐19 (Chen et al., 2020). Healthcare institutions have rearranged human resources and medical resources to ensure the timely treatment of diagnosed patients and the COVID‐19 screening of patients in emergency and outpatient departments. Public hospitals also responded by increasing the number of beds in both intensive and designated infection units and increasing the number of healthcare workers, aimed at effectively responding to the needs of those confirmed and suspected cases who required admission (Liang et al., 2020). A huge number of nurses were recruited to support and join the front line of the fight against COVID‐19 pandemic. The COVID‐19 high risk of infection increased the workload of healthcare workers, especially nurses, as they are the highest proportion of healthcare workforce. These problems can lead to mental problems (Al Maqbali et al., 2021). The health of these nurses has received great attention.
2. BACKGROUND
Based on a systematic review and meta‐analysis, sleep quality was reported to be poor among nurses in different countries and different departments (Kang, Ma, et al., 2020; Kang, Noh, et al., 2020), especially among female hospital staff nurses (Chien et al., 2013). Previous studies have revealed that sleep problems among nurses included poor sleep quality, sleep deprivation, insomnia and insufficient sleep (Furihata et al., 2020). However, each nurse may simultaneously have had one or more sleep problems. Poor sleep quality was associated with night shift work. The sleep quality of shiftwork nurses was reported to be affected by their individual health, perceived health condition, circadian type, experience with shift work and perceived shiftwork condition (Jeong & Gu, 2018). Not only nurses, abut also other healthcare workers or emergency personnel, if they had poor sleep quality or sleep deficiencies, they would be more likely to suffer from mental problems, decreased work performance, poor decision‐making, medical errors, personal health challenges and burnout (Cox et al., 2021).
When the public health emergency broke out, nurses' working environment and work pressure suddenly changed, and their sleep quality also be influenced sensitively and accordingly.
After the outbreak of COVID‐19, the sleep quality of healthcare workers was found to be even worse than general population. A systematic review and meta‐analysis (Jahrami et al., 2021), involving a total of 54,231 participants from 13 countries, concluded that the prevalence of sleep problems during the COVID‐19 pandemic was high and affected approximately 40% of people from the general and healthcare populations, 36.0% for healthcare workers and 32.3% for the general population, respectively. Meanwhile, sleep disturbance were found among healthcare workers in different ages (Grossman et al., 2021; Liu et al., 2021) and in different countries and regions (Beck et al., 2021; Dey et al., 2021; Marelli et al., 2021; Robillard et al., 2021). In addition, insomnia prevalence among healthcare works was estimated at 38.9% across five studies (Pappa et al., 2020).
Particularly for nurses, as they are the highest proportion of healthcare workforce, it was proved that they had poorer sleep quality among all the healthcare worker served during the COVID‐19 pandemic. Eighteen studies assessed nurses' sleep disturbance and the total prevalence was high to 43.0% (Al Maqbali et al., 2021). Similar result (34.8%) occurred in another meta‐analysis based on six cross‐sectional studies involving a total of 3,745 nurses (Salari et al., 2020).
Working against the pandemic, nurses played a pivotal role in public health. In China, there were about 28,600 nurses involved in the nursing of patients diagnosed or suspected with COVID‐19 (National Health Commission, 2020). Compared with doctors, nurses spent more time contacting with patients directly and worked under higher workload pressure. The nursing work during pandemic period was different from usual, which was involved intensive care, emergency care and also supplied management (Tang et al., 2020). Many nurses were relocated from their usual practice areas to specialized pandemic departments to meet the needs of nursing severe cases (Seale et al., 2009). Including them, all frontline nurses were required to adapt to the new work mode in short time and undertake rescue tasks at any time (Tang et al., 2020). In addition, isolation and separation from their families were known to lead to an increased risk of psychological distress (Bansal et al., 2020). Moreover, facing with fears of virus contagion during direct contact with patients brought great risk and stress to frontline nurses and would lead to potentially series of psychological consequences (Fernandez et al., 2020). At last, frontline nurses had to take night shifts. Previous studies have shown that night shifts can lead to sleep disorders, and most night shift nurses will have varying degrees of neurasthenia, gastrointestinal dysfunction, endocrine disorders and low immunity (Fernandez et al., 2020; Tian & Song, 2012).
The workloads and stress of frontline nurses during the pandemic would have a negative impact on their sleep quality and increase the risk of physical and mental health damage (Dong et al., 2017; Han et al., 2016; Wu et al., 2021), thus, causing negative outcomes for the safety of patients (in terms of mortality and morbidity) and health professionals (in lower job satisfaction, burnout and intention to leave) (Wu et al., 2021). In order to improve the sleep quality of frontline nurses during the pandemic period, we conducted a sleep intervention based on holistic sleep improvement strategies to improve sleep quality of the frontline nurses served during the public health emergency (COVID‐19).
3. STUDY AIM
The aim of this study was to investigate the sleep quality of frontline nurses served during a public health emergency (COVID‐19) in Wuhan, China, and to explore the effects of a sleep intervention based on holistic sleep improvement strategies for frontline nurses.
4. METHODS
4.1. Design
A pre‐post‐test design was used to examine the effects of a holistic sleep intervention on sleep quality in anti‐pandemic frontline nurses applied the Transparent Reporting of Evaluations with Non‐randomized Designs statement (Appendix S1).
4.2. Participants
The study was conducted in Wuhan, a city in central China on February, 2020. A convenience sample was recruited from a specialized pandemic hospital that only treated confirmed cases of COVID‐19. Inclusion criteria were: (a) frontline nurses working in a specialized pandemic hospital; (b) had worked at frontline for at least 2 weeks; (c) ability to use telephone applications “WeChat” and “Questionnaire Star”. Exclusion criteria were: (a) unwilling to participate in the survey; (b) lack of internet access; (c) inability to complete an online survey; (d) presence of long‐term medical disorders.
The sample size was calculated using statistical package G * Power (3.1.9.7) Software (Kang, 2021). Power analysis indicated that sample size of 43 participants would provide statistical power ≥0.9, assuming a significance level of 0.05, a moderate effect size. Considering 20% attrition and missing data rate, we finally determined the sample size to be 52.
4.3. Intervention
The intervention was designed to help improve the sleep quality and ensure nursing quality and safety during pandemic period. Facing up to frontline nurses' sleep problems, the sleep improvement strategies were established based on holistic nursing theory to provide support for frontline nurses. The strategies were concentrated on scientific human resource management, comfortable sleep environment establishment, self‐relaxation and self‐adjustment training and humanistic care. The intervention was delivered by a sleep improvement collaboration team, consisting of hospital administrators, nursing managers, psychologists, rehabilitation therapists, logistics support departments and so on. Specific measures of the sleep improvement strategies are shown in Table 1.
TABLE 1.
Specific measures of the sleep improvement strategies
| Strategy | Specific measures |
|---|---|
| 1. Scientific human resource management to balance labour intensity |
|
| 2. Establish independent rest areas and create a good sleep environment |
|
| 3. Encourage self‐relaxation and self‐adjustment training |
|
| 4. Strengthen humanistic care and take care of nurses' mental health |
|
4.4. Measures
4.4.1. Demographic data
A demographic characteristics questionnaire asked for age, gender, education level, marital status, personnel relationship, working years, nurse level, professional title, position, department and past public health emergencies working history.
4.4.2. Pittsburgh Sleep Quality Index (PSQI)
Pittsburgh Sleep Quality Index is a self‐rated questionnaire that assesses sleep quality and sleep disturbances occurred over the past month. Eighteen items generate seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication and daytime dysfunction. Each component is scored according to 0–3 (Buysse et al., 1989). The total score ranges from 0–21, higher scores reflect poorer sleep quality, and those with a total score >7 are categorized as having poor sleep quality (Yin et al., 2017). The Cronbach's α of the seven components has been reported as .83, the sensitivity and specificity of the original version have been reported at 89.6% and 86.5% (Buysse et al., 1989). Liu et al. (1996) translated PSQI into Chinese version. The Chinese version of PSQI has been used in many epidemiological studies with good reliability and validity (Guo et al., 2016; Liu et al., 1996).
4.5. Data collection
The sleep quality was investigated at baseline and after 4‐week follow‐up through online questionnaire software “Questionnaire Star”, instead of face‐to‐face survey. “Questionnaire Star” is an online survey tool and it permits questionnaire design, data collection, custom reporting and analysis of results (Shi et al., 2000).
The purpose, significance and anonymity and confidentiality of the research were delivered by WeChat group by the first author. Then, the above scales were uploaded to the “Questionnaire Star” and the QR code was sent to participants from the first author's account at baseline and after 4‐week follow‐up. The informed consent form was also signed through the “Questionnaire Star”. When the participants completed the survey on the mobile phone, the data would be directly collected through the “Questionnaire Star” software and formed an Excel form.
4.6. Ethics statement
The study protocol was approved by the Ethics Committee of a teaching hospital (protocol approval No. TJ‐IRB20201216). Participants were informed that they could refuse to participate or withdraw from the study at any time, and all information would be held confidential.
4.7. Data analysis
SPSS 20.0 (IBM) software was used for statistical analyses. Categorical variables are presented as counts and percentages. Continuous variables are presented as mean and standard deviation (SD). The differences were compared by paired t‐test in normally distributed continuous variables, or by non‐parametric test in abnormal distribution variables. A p‐value of ≤.05 was considered statistically significant.
5. RESULTS
5.1. Demographic characteristics
Fifty‐two nurses completed the study without data leakage (Figure 1). The included nurses' ages ranged from 22–41 years (M = 30.81, SD = 4.927). A high proportion of nurses (96.2%) were female. Nurses came from a wide variety of educational backgrounds. The vast majority (96.2%) earned a college degree (5.8%) or a bachelor's degree (90.4%), but others had a master's degree (3.8%). In terms of marriage, most (57.5%) were married. The most of nurses (67.3%) have worked for less than 10 years, and only 32.7% had worked for more than 10 years. Fifty‐one of them were clinical nurses, and only one was engaged in nursing management as a head nurse in the usual practice areas. Almost all of them (88.5%) had no experience working in a public health emergency (Table 2).
FIGURE 1.
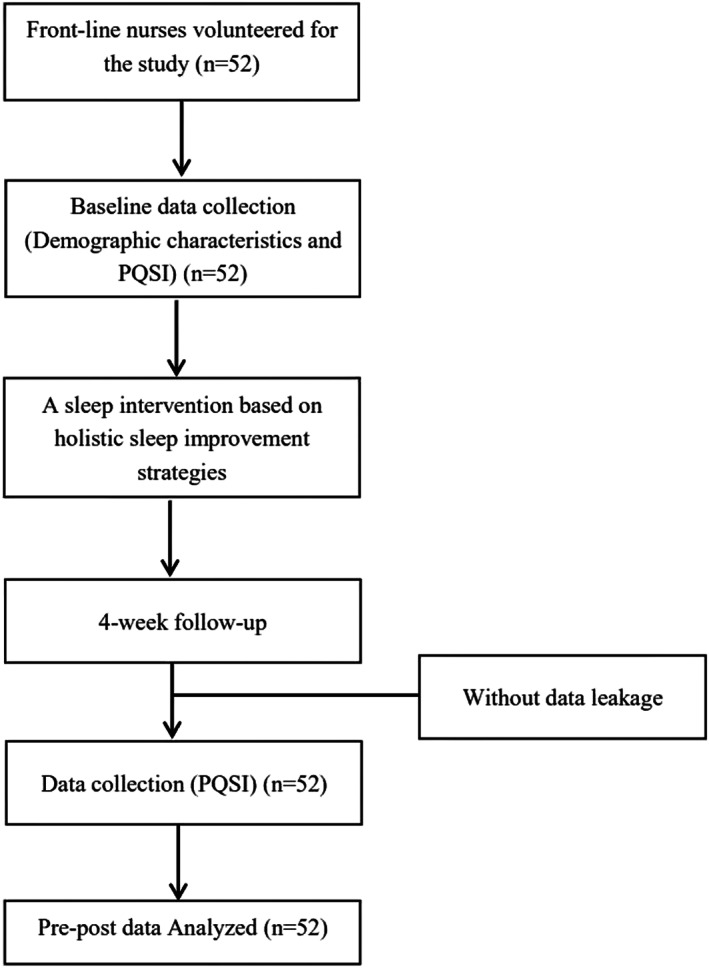
Flow chart of research design and participants
TABLE 2.
Demographic characteristics included nurses (N = 52)
| Variable | Frequency | Ratio (%) |
|---|---|---|
| Gender | ||
| Male | 2 | 3.8 |
| Female | 50 | 96.2 |
| Education level | ||
| College | 3 | 5.8 |
| Bachelor | 47 | 90.4 |
| Master and above | 2 | 3.8 |
| Marital status | ||
| Single | 22 | 42.3 |
| Currently married | 30 | 57.7 |
| Personnel relationship | ||
| Contract nurses | 49 | 94.3 |
| Personnel agency nurse | 2 | 3.8 |
| Formal establishment nurse | 1 | 1.9 |
| Working years | ||
| <3 | 4 | 7.7 |
| 3–5 | 17 | 32.7 |
| 6–10 | 14 | 26.9 |
| >10 | 17 | 32.7 |
| Nurse level | ||
| N0 | 3 | 5.8 |
| N1 | 19 | 36.5 |
| N2 | 13 | 25.0 |
| N3 | 16 | 30.8 |
| N4 | 1 | 1.9 |
| Professional title | ||
| Junior nurse | 7 | 13.5 |
| Senior nurse | 31 | 59.6 |
| Supervisor nurse | 14 | 26.9 |
| Position | ||
| Nurse | 51 | 98.1 |
| Head nurse | 1 | 1.9 |
| Department | ||
| Surgical | 20 | 38.5 |
| Medical | 6 | 11.5 |
| Gynaecology | 3 | 5.8 |
| Paediatrics | 7 | 13.5 |
| Outpatient and emergency | 7 | 13.5 |
| ICU | 9 | 17.2 |
| Past public health emergencies working history | ||
| Yes | 6 | 11.5 |
| No | 46 | 88.5 |
| Variable | M | SD |
|---|---|---|
| Age | 30.81 | 4.927 |
Abbreviations: M, mean; SD, standard deviation.
5.2. Sleep quality of frontline nurses during COVID‐19 pandemic (PSQI scores of included nurses at baseline)
As shown in Table 3, the total score of PQSI of frontline nurses was 8.69 ± 4.346, higher than 7, indicating that the sleep quality of frontline nurses at baseline was poor. Compared with the norm (Buysse et al., 1989), there were statistically significant differences in total scores (p < .01) and components of subjective sleep quality (p < .01), sleep latency (p < .01), sleep efficiency (p < .01), sleep disturbances (p < .01), sleep medication (p < .01) and daytime dysfunction (p < .01), except sleep duration (p = .387).
TABLE 3.
Status of sleep quality of frontline nurses at baseline (M ± SD) (N = 52)
| Variable | Baseline (M ± SD) | Norm (M ± SD) | t | p |
|---|---|---|---|---|
| N = 52 | N = 112 | |||
| Total score of PSQI | 8.69 ± 4.346 | 3.88 ± 2.52 | 8.932 | <.001 |
| Subjective sleep quality | 1.42 ± 0.776 | 0.63 ± 0.67 | 6.677 | <.001 |
| Sleep latency | 2.21 ± 0.915 | 0.70 ± 0.86 | 10.252 | <.001 |
| Sleep duration | 0.83 ± 0.964 | 0.70 ± 0.58 | 1.071 | .387 |
| Sleep efficiency | 1.23 ± 1.246 | 0.15 ± 0.47 | 8.044 | <.001 |
| Sleep disturbances | 1.60 ± 0.823 | 0.90 ± 0.44 | 7.093 | <.001 |
| Sleep medication | 0.31 ± 0.781 | 0.06 ± 0.24 | 3.096 | .002 |
| Daytime dysfunction | 1.27 ± 0.952 | 0.73 ± 0.83 | 3.697 | .003 |
Abbreviations: M, mean; PSQI, Pittsburgh Sleep Quality Index; SD, standard deviation.
5.3. Effects of holistic sleep improvement strategies on sleep quality of frontline nurses (comparison of PSQI scores at baseline and 4‐week follow‐up)
Compared with the PSQI score at baseline, the total score statistically significantly decreased at 4‐week follow‐up after the intervention, but the total score still showed to be higher than 7, representing that the sleep quality improved and still poorer than norm. Beside, statistically significant differences were found in subjective sleep quality (p = .016), sleep efficiency (p = .015), sleep disturbances (p = .007), but not in sleep latency (p = .205), sleep duration (p = .375), sleep medication (p = .723) and daytime dysfunction (p = .747) at 4‐week follow‐up after the intervention (shown in Table 4).
TABLE 4.
Comparison of sleep quality of frontline nurses at baseline and 4‐week follow‐up (N = 52)
| Variables | Baseline (pre‐test) | 4‐Week follow‐up (post‐test) | Parameters | p |
|---|---|---|---|---|
| (M ± SD) | (M ± SD) | t | ||
| PSQI total score | 8.69 ± 4.346 | 7.48 ± 3.691 | 3.042 | .004 |
| M [P25, P75] | M [P25, P75] | Z | ||
|---|---|---|---|---|
| Subjective sleep quality | 1.00 [1.00, 2.00] | 1.00 [1.00, 2.00] | −2.408 | .016 |
| Sleep latency | 2.50 [1.25, 3.00] | 2.00 [1.00, 3.00] | −1.268 | .205 |
| Sleep duration | 1.00 [0, 1.00] | 0 [0, 1.00] | −0.887 | .375 |
| Sleep efficiency | 1.00 [0, 2.75] | 1.00 [0, 1.00] | −2.436 | .015 |
| Sleep disturbances | 1.00 [1.00, 2.00] | 1.00 [1.00, 2.00] | −2.675 | .007 |
| Sleep medication | 0 [0, 0] | 0 [0, 0.75] | −0.354 | .723 |
| Daytime dysfunction | 1.00 [1.00, 2.00] | 1.00 [1.00, 2.00] | −0.323 | .747 |
Abbreviations: M, mean; P25, 25th percentile; P75, 75th percentile; PSQI, Pittsburgh Sleep Quality Index; SD, standard deviation.
6. DISCUSSION
6.1. The sleep quality of frontline nurses served during COVID‐19 was worse than norm
The results of this study showed that the total score and each component score of PSQI, except sleep duration, in frontline nurses at baseline were statistically significantly higher than those of the norm (p < .01). Twenty‐eight frontline nurses had sleep quality problems by self‐reported, accounting for 53.85% of the total participants. It was higher than the norm rate (13.18%) reported by Liu et al. (1996) in Chinese population and also higher than the rate reported in other populations (Beck et al., 2021; Dey et al., 2021; Marelli et al., 2021; Robillard et al., 2021), even higher than anti‐pandemic nurses in other countries and locations (Jahrami et al., 2021; Pappa et al., 2020).
However, similar result was found in a large sample survey at the same time in Wuhan (Tang et al., 2020). This was probably because the baseline survey was conducted in Wuhan in early February 2020, when the epidemic had just broken out. Either healthcare institutions or the healthcare works were shocked and not well‐prepared to face up with such unfamiliar disease and the changing international situation. Most of the nurses were organized and arranged to participate in the nursing of suspected or confirmed patients without enough time to do physical and psychological preparation for the following heavy anti‐epidemic tasks. Therefore, in addition to the pressure, they also felt a sense of uncertainty, which produced negative emotions such as anxiety and fear, and leading to a series of psychological problems, such as depression, insomnia, irritability and so on.
6.2. Holistic sleep improvement strategies were effective in improving the sleep quality of frontline nurses
The total score of PSQI statistically significantly decreased at 4‐week follow‐up after the intervention. Beside, statistically significant differences were found in subjective sleep quality (p = .016), sleep efficiency (p = .015) and sleep disturbances (p = .007) as well. Four different sleep improvement strategies all played an important role in improving the sleep quality of frontline nurses.
6.2.1. Strategy 1: Scientific human resource management helped balance labour intensity
Burnout is an important factor leading to sleep problems of frontline nurses (Payne, 2001; Tang et al., 2020). Nurses' sleep problems not only affect their physical and psychological health, but also reduce their work efficiency and affect nursing quality. Effective support from organization was very important for nurses to cope with work stress. Therefore, health administrators should create a harmonious working atmosphere and strengthen the management of human resources for the frontline nurses (Duan & Shi, 2015). The increased shifts effectively reduced the working hours of each shift, and controlled the workload of each shift in a bearable range, thus ensuring all frontline nurses obtain sufficient rest or sleep after each shift. Moreover, the reserved batches of nurses for rotation (Liu, Wang, et al., 2020; Simonetti et al., 2021) ensured that there were sufficient human resources prepared to work during the pandemic and avoided the condition of continuous rotation or working with fatigue or illness. At last, the systematic pre‐service training increased nurses' self‐confidence and sense of safety, decreased the sense of uncertainty, thus reduced the work stress and improved their sleep quality.
6.2.2. Strategy 2: The independent rest areas created a good sleep environment
The frontline nurses belonged to the self‐isolated groups according to the anti‐epidemic regulations (Liang et al., 2020). Managers should provide quiet and suitable rest areas for frontline nurses to ensure they can have a comfortable sleep environment after each shift. The rest areas should be quiet, clean and hygienic, with suitable light, temperature, humidity and comfortable bedding, without sleep interference. Due to the droplet transmission of COVID‐19, central air conditioners cannot be used in winter. Managers should pay attention to the temperature and provide thermal insulation products, such as electric blankets and hot water bags. In addition, all frontline nurses needed to work day and night shifts, half the time they had to rest in daylight. Some nurses reported that the bright and noisy environment made it difficult to fall asleep on daytime. Hospital managers could provide goggles, earplugs or some other products to reduce daytime interference to help nurses improve the sleep efficiency. The results showed that the sleep efficiency and sleep disturbances were statistically significantly improved, which proved that the sleep improvement strategy focused on sleep environment was effective.
6.2.3. Strategy 3: Self‐relaxation and self‐adjustment training helped release stress
Studies have shown that white noise had an auditory masking effect and could increase the awakening threshold, thus consolidating sleep (Shao et al., 2018). In different studies, patients with sleep problems were arranged in the environment with white noise of 50–60 or 60–75 decibels, and all of them achieved improved sleep quality (Forquer & Johnson, 2007). After years of research, personalized music intervention has been proved to be a good method to improve sleep quality (Wen, 2018). Respiratory relaxation (Xie et al., 2010) and progressive muscle relaxation (Guo et al., 2017; Liu, Chen, et al., 2020) have also been proved to reduce psychological stress and effectively improve sleep quality. Based on these research evidences, hospital managers provided white noise or light music packages and encourage frontline nurses to listen to white noise or light music they preferred to relax before sleep. Some respiratory relaxation or progressive muscle relaxation courses, preferably online, could be further help frontline nurses to train their relaxation skills. Closing eyes and taking deep breathes in the music background, and imagining relaxing the muscles from head to toe in a beautiful natural environment, which was proved to helping relieve tension, shorten sleep latency (Liu, Chen, et al., 2020).
Furthermore, therapy devices have been reported to help alleviate sleep disorders in China and abroad at present, such as insomnia therapy, transcranial magnetic stimulation therapy, transcranial ultrasound electrical stimulation therapy, brain electrical somatosensory music relaxation system and so on (Wang et al., 2015). The above devices are non‐invasive and painless and can effectively regulate mood state and improve sleep quality. Hence, in anti‐epidemic hospitals, managers could set up a sleep department specialized for frontline medical staff, making good use of the above devices and organizing professional therapists, helping to alleviate sleep disorders for the frontline nurses.
6.2.4. Strategy 4: Humanistic care and psychological care helped to maintain mental health
In the front line of public health emergency, just like the previous SARS and the current COVID‐19 epidemic, the heavy work pressure, risk of infection, network consensus and worries about family members, all these factors led to great psychological pressure and caused a variety of bad emotions on frontline nurses (Xu & Zhang, 2020). Studies have explored that emotional state and mental health were closely related to sleep quality (Tang et al., 2020; Xu & Zhang, 2020). Managers should attach great importance to the psychological status, realize the impact of emotional problems on nurses' sleep and health and take measures from multiple angles (Kang, Ma, et al., 2020; Kang, Noh, et al., 2020).
Ni and Sun's research (Ni & Sun, 2008) showed that verbal affirmation and praise can help nurses relieve negative emotions caused by work stress more than material rewards. Hospital administrators were recommended to give timely affirmation and encouragement to frontline nurses' work and sacrifices.
Psychological assessment, counselling and assistance were necessary and required to be organized (Kang, Ma, et al., 2020; Kang, Noh, et al., 2020). Psychiatrists could carry out online counselling and courses to teach frontline nurses how to do self‐adjustment and guide them to face up to the bad emotions and to establish positive attitudes. In this special period, medical staff would also have feelings of fear and sadness. Nurses should be encouraged to release their negative feelings and understand that the current medical methods may not guarantee all patients be cured in such a sudden epidemic. They could not be plagued by the sense of frustration or repeatedly blame themselves when facing with patients' deaths.
Family support was a key power that support frontline nurses to keep the confidence to defeat the epidemic. Hospital administrators should encourage and create channels promote nurses to keep in touch with families and friends. Moreover, taking good care of their families greatly helped frontline nurses solving their worries about families. Administrators could pay attention to taking the initiative to care about nurses' families, for example, uniting social forces to provide free food, masks or disinfectant.
In addition, facing with such a special emergency like COVID‐19, the whole country of China united as one again just like what happened in the history of SARS. All medical sources were united and combined together and entered into the front line one by one without complaining. Their spirit of unity and dedication has forged the greatest strength in the fight against the epidemic. The frontline nurses were working in a harmonious and united team, which to a certain extent appeasing some emotional problems related to the surrounding environment, such as interpersonal sensitivity, hostility and paranoia (Tang et al., 2020; Xu & Zhang, 2020).
7. CLINICAL IMPLICATIONS
Based on holistic nursing theory, we searched evidences and formulated sleep improvement interventions from the four dimensions of human resource management, environmental improvement and psychological care and relaxation training. Starting from external factors, we have taken measures to optimize human resources and improve the sleeping environment. Internally, we carried out relaxation training and humanistic care among frontline nurses.
These holistic sleep improvement strategies have been proved to be effective in reducing sleep disorders and improving sleep quality of frontline nurses, which is worth popularizing. During the epidemic period, hospital administrators should formulate relevant policies to promote the physical and mental health of frontline nurses. The most important is to pay attention to the sleep quality of frontline nurses and then formulate sleep intervention strategies and take action. The holistic sleep improvement strategies approach to both internal and external environments of frontline nurses were recommended. In terms of external environment, optimized human resources reduced work burden and work pressure, and the comfortable sleep environment effectively reduced sleep disturbance. As for internal environment, relaxation training and humanistic care took full account of the psychological problems of frontline nurses and provided them several ways to relax and release. The results of this study strongly demonstrate that holistic sleep improvement strategies can improve the sleep quality of nurses working in public health emergencies, and these strategies can be extended to nurses working in other special circumstances, such as wind disasters, earthquakes and so on. In addition, it is hoped that the intervention methods and results of this study can promote the formation of a standardized mechanism for protecting the rights and interests of nurses in the general practice places and other special working environments.
8. LIMITATIONS AND FUTURE STUDY
There were some limitations to the present study. First, the participants were a convenience sample from one‐single anti‐epidemic city. These nurses are working and living in same circumstances, and their work forms in the frontline are basically similar. The sample of this study may no present all the nurses served during COVID‐19 pandemic in the whole world. The representativeness of the sample needs to be improved. Second, self‐reported sleep quality may have been subject to social desirability bias.
Despite these limitations, the study explored the sleep quality and the effects of the holistic sleep improvement strategies in frontline nurses served during a public health emergency (COVID‐19) in Wuhan, China. The sleep quality of frontline nurses statistically significantly improved after receiving a sleep intervention concentrated on human resource management, comfortable sleep environment establishment, self‐relaxation and self‐adjustment training and humanistic care. Based on this intervention research, further research could study the effect of the reported sleep improvement strategies on frontline nurses in other cities or countries. Meanwhile, other specific intervention could be designed to improve sleep quality of nurses served during public health emergencies.
9. CONCLUSIONS
The sleep quality of frontline nurses is not only closely related to their physical and psychological health, but also related to clinical nursing safety and nursing quality, which are indispensable guarantee factors for the victory of the fight against public health emergency. The firstline nurses served during public health emergency (COVID‐2019) had a middle level of sleep quality. However, the sleep quality of frontline nurses statistically significantly improved after receiving a sleep intervention concentrated on human resource management, comfortable sleep environment establishment, self‐relaxation and self‐adjustment training and humanistic care. Hospital administrators need to face up to the existed sleep disorders and establish reasonable sleep management strategies to help improve the sleep quality and ensure nursing quality and safety during COVID‐2019 pandemic. A sleep improvement intervention including scientific human resource management, comfortable sleep environment establishment, self‐relaxation and self‐adjustment training and humanistic care was suggested.
10. RELEVANCE TO CLINICAL PRACTICE
This study can give some inspiration and suggestions to hospital administrators on the sleep management of frontline nurses in public health emergencies. Healthcare institutions should pay attention to the sleep quality of nurses served during public health emergencies and establish sleep management strategies to help improve the sleep quality and ensure nursing quality and safety. The sleep intervention based on holistic sleep improvement strategies can improve nurses' sleep quality and reduce sleep disorders, which is worth popularizing.
AUTHOR CONTRIBUTIONS
Yanli Zhang involved in conceptualization, data collection, writing, reviewing and editing. Manli Tang involved in conceptualization, data collection, writing the original draft. Yanrong Zhou involved in methodology, reviewing and supervision.
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ETHICAL APPROVAL
This study was approved by the Institutional Review Board of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology (No.TJ‐IRB20201216).
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
The authors would like to thank all the participants and contributions in this study, and we really appreciate those who were not listed as authors, but also provided help.
Zhang, Y. , Tang, M. , & Zhou, Y. (2023). Holistic sleep improvement strategies for frontline nurses served during a public health emergency (COVID‐19) in Wuhan, China: A quasi‐experimental study. Nursing Open, 10, 1471–1481. 10.1002/nop2.1397
Yanli Zhang and Manli Tang contributed equally to this work.
DATA AVAILABILITY STATEMENT
The raw data that support the findings of this study are available by the authors upon reasonable request.
REFERENCES
- Al Maqbali, M. , Al Sinani, M. , & Al‐Lenjawi, B. (2021). Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Psychosomatic Research, 141, 110343. 10.1016/j.jpsychores.2020.110343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bansal, P. , Bingemann, T. A. , Greenhawt, M. , Mosnaim, G. , Nanda, A. , Oppenheimer, J. , Sharma, H. , Stukus, D. , & Shaker, M. (2020). Clinician wellness during the COVID‐19 pandemic: Extraordinary times and unusual challenges for the allergist/immunologist. The Journal of Allergy and Clinical Immunology: In Practice, 8(6), 1781–1790. 10.1016/j.jaip.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, F. , Léger, D. , Fressard, L. , Peretti‐Watel, P. , Verger, P. , & Coconel Group . (2021). Covid‐19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. Journal of Sleep Research, 30(1), e13119. 10.1111/jsr.13119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F., 3rd , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Chen, S. , Zhang, Z. , Yang, J. , Wang, J. , Zhai, X. , Bärnighausen, T. , & Wang, C. (2020). Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet, 395(10232), 1305–1314. 10.1016/S0140-6736(20)30744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien, P. L. , Su, H. F. , Hsieh, P. C. , Siao, R. Y. , Ling, P. Y. , & Jou, H. J. (2013). Sleep quality among female hospital staff nurses. Sleep Disorders, 2013, 283490. 10.1155/2013/283490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox, S. D. , Benoit, J. S. , Brohard, C. L. , & McIntyre, T. M. (2021). Evaluation of sleep quality among nursing faculty: Application of the Pittsburgh Sleep Quality Index‐A descriptive correlational study. Nursing Open, 9, 339–348. 10.1002/nop2.1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey, A. , Majumdar, P. , Saha, A. , & Sahu, S. (2021). COVID‐19 pandemic lockdown‐induced altered sleep/wake circadian rhythm, health complaints and stress among traffic police personnel in India. Chronobiology International, 38(1), 140–148. 10.1080/07420528.2020.1831524 [DOI] [PubMed] [Google Scholar]
- Dong, H. , Zhang, Q. , Sun, Z. , Sang, F. , & Xu, Y. (2017). Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry, 17(1), 241. 10.1186/s12888-017-1402-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, X. , & Shi, Y. (2015). Status quo of occupational stress and sleep quality and its correlations among ICU nurses. The Journal of Nursing, 22(6), 1–5 (in Chinese). 10.16460/j.issn1008-9969.2015.06.001 [DOI] [Google Scholar]
- Fernandez, R. , Lord, H. , Halcomb, E. , Moxham, L. , Middleton, R. , Alananzeh, I. , & Ellwood, L. (2020). Implications for COVID‐19: A systematic review of nurses' experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111, 103637. 10.1016/j.ijnurstu.2020.103637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forquer, L. A. M. , & Johnson, C. M. (2007). Continuous white noise to reduce sleep latency and night wakings in college students. Sleep and Hypnosis, 9(2), 60–66. [Google Scholar]
- Furihata, R. , Saitoh, K. , Suzuki, M. , Jike, M. , Kaneita, Y. , Ohida, T. , Buysse, D. J. , & Uchiyama, M. (2020). A composite measure of sleep health is associated with symptoms of depression among Japanese female hospital nurses. Comprehensive Psychiatry, 97, 152151. 10.1016/j.comppsych.2019.152151 [DOI] [PubMed] [Google Scholar]
- General Office of the State Health Commission . (2020). Circular of the General Office of the State Health Commission on issuing COVID‐19's prevention and control plan (fourth edition) . http://www.gov.cn/zhengce/zhengceku/2020‐02/07/content_5475813.htm
- Grossman, E. S. , Hoffman, Y. , Palgi, Y. , & Shrira, A. (2021). COVID‐19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Personality and Individual Differences, 168, 110371. 10.1016/j.paid.2020.110371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, Q. , Qin, W. , Zhao, D. , & He, B. Y. (2017). Influence of progressive muscle relaxation training on sleep quality and fatigue in patients of maintenance hemodialysis. Chinese Nursing Research, 31(14), 1756–1758 (in Chinese). 10.3969/j.issn.1009-6493.2017.14.026 [DOI] [Google Scholar]
- Guo, S. , Sun, W. , Liu, C. , & Wu, S. W. (2016). Structural validity of the Pittsburgh Sleep Quality Index in Chinese undergraduate students. Frontiers in Psychology, 8(7), 1126. 10.3389/fpsyg.2016.01126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, Y. , Yuan, Y. , Zhang, L. , & Fu, Y. (2016). Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatria Danubina, 28(2), 176–183. [PubMed] [Google Scholar]
- Jahrami, H. , BaHammam, A. S. , Bragazzi, N. L. , Saif, Z. , Faris, M. , & Vitiello, M. V. (2021). Sleep problems during the COVID‐19 pandemic by population: A systematic review and meta‐analysis. Journal of Clinical Sleep Medicine, 17(2), 299–313. 10.5664/jcsm.8930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong, J. Y. , & Gu, M. O. (2018). Structural equation model for sleep quality of female shift work nurses. Journal of Korean Academy of Nursing, 48(5), 622–635. 10.4040/jkan.2018.48.5.622 [DOI] [PubMed] [Google Scholar]
- Kang, H. (2021). Sample size determination and power analysis using the G*Power software. Journal of Educational Evaluation for Health Professions, 18, 17. 10.3352/jeehp.2021.18.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, J. , Noh, W. , & Lee, Y. (2020). Sleep quality among shift‐work nurses: A systematic review and meta‐analysis. Applied Nursing Research, 52, 151227. 10.1016/j.apnr.2019.151227 [DOI] [PubMed] [Google Scholar]
- Kang, L. J. , Ma, S. M. , Chen, M. , Yang, J. , Wang, Y. , Li, R. T. , Yao, L. H. , Bai, H. P. , Cai, Z. X. , Yang, B. X. , Hu, S. H. , Zhang, K. R. , Wang, G. H. , Ma, C. , & Liu, Z. C. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 Novel Coronavirus Disease Outbreak: A cross‐sectional study. Brain, Behavior, and Immunity, 87, 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, L. B. , Zhao, J. , Wang, C. , Tao, S. Y. , & Wu, Q. H. (2020). Thoughts of health emergency management in public hospitals in COVID‐19 epidemic situation. Chinese Hospital Management, 40(3), 4–6, 11 (in Chinese). [Google Scholar]
- Liu, K. , Chen, Y. , Wu, D. , Lin, R. , Wang, Z. , & Pan, L. (2020). Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID‐19. Complementary Therapies in Clinical Practice, 39, 101132. 10.1016/j.ctcp.2020.101132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, X. C. , Tang, M. Q. , Hu, L. , Wang, A. Z. , Wu, H. X. , Zhao, G. F. , Gao, C. N. , & Li, W. S. (1996). Reliability and validity of the Pittsburgh Sleep Quality Index. Chinese Journal of Psychiatry, 29(2), 103–107 (in Chinese). 10.1007/978-94-007-0753-5_2173 [DOI] [Google Scholar]
- Liu, Y. , Wang, H. , Chen, J. H. , Zhang, X. Y. , Le, X. , Ke, J. , Wang, B. H. , & Peng, C. H. (2020). Emergency management of nursing human resources and material resources for novel coronavirus pneumonia. Chinese Journal of Nursing, 55(3), 343–346 (in Chinese). 10.3761/j.issn.0254-1769.2020.03.004 [DOI] [Google Scholar]
- Liu, Z. , Tang, H. , Jin, Q. , Wang, G. , Yang, Z. , Chen, H. , Yan, H. , Rao, W. , & Owens, J. (2021). Sleep of preschoolers during the coronavirus disease 2019 (COVID‐19) outbreak. Journal of Sleep Research, 30(1), e13142. 10.1111/jsr.13142 [DOI] [PubMed] [Google Scholar]
- Marelli, S. , Castelnuovo, A. , Somma, A. , Castronovo, V. , Mombelli, S. , Bottoni, D. , Leitner, C. , Fossati, A. , & Ferini‐Strambi, L. (2021). Impact of COVID‐19 lockdown on sleep quality in university students and administration staff. Journal of Neurology, 268(1), 8–15. 10.1007/s00415-020-10056-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission . (2020). Nurses account for 68% of the front‐line medical staff supporting the fight against COVID‐19 epidemic . Health People. http://health.people.com.cn/n1/2020/0229/c14739‐31610814.html
- National Health Commission of the People's Republic of China . (2020). Announcement of the National Health Commission of the People's Republic of China: No.1 of 2020 . http://www.nhc.gov.cn/jkj/s7916/202001/44a3b8245e8049d2837a4f27529cd386.shtml
- Ni, J. P. , & Sun, H. Y. (2008). Phenomenological study on nurses' job burnout and its influencing factors. Journal of Nursing Administration, 8(12), 1–3 (in Chinese). [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne, N. (2001). Occupational stressors and coping as determinants of burnout in female hospice nurses. Journal of Advanced Nursing, 33(3), 396–405. 10.1046/j.1365-2648.2001.01677.x [DOI] [PubMed] [Google Scholar]
- Robillard, R. , Dion, K. , Pennestri, M. H. , Solomonova, E. , Lee, E. , Saad, M. , Murkar, A. , Godbout, R. , Edwards, J. D. , Quilty, L. , Daros, A. R. , Bhatla, R. , & Kendzerska, T. (2021). Profiles of sleep changes during the COVID‐19 pandemic: Demographic, behavioural and psychological factors. Journal of Sleep Research, 30(1), e13231. 10.1111/jsr.13231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari, N. , Khazaie, H. , Hosseinian‐Far, A. , Ghasemi, H. , Mohammadi, M. , Shohaimi, S. , Daneshkhah, A. , Khaledi‐Paveh, B. , & Hosseinian‐Far, M. (2020). The prevalence of sleep disturbances among physicians and nurses facing the COVID‐19 patients: A systematic review and meta‐analysis. Globalization and Health, 16(1), 92. 10.1186/s12992-020-00620-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale, H. , Leask, J. , Po, K. , & MacIntyre, C. R. (2009). “Will they just pack up and leave?” – Attitudes and intended behaviour of hospital health care workers during an influenza pandemic. BMC Health Services Research, 9, 30. 10.1186/1472-6963-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao, L. W. , Huang, L. H. , Huang, X. W. , Wei, J. H. , Gao, C. H. , Pan, X. Y. , & Chen, X. (2018). Effect of white noise on sleep quality of ICU patients. Chinese Journal of Critical Care Medicine, 11(4), 286–288 (in Chinese). 10.3877/cma.j.issn.1674-6880.2018.04.016 [DOI] [Google Scholar]
- Shi, Y. D. , Wang, J. , Yang, Y. T. , Wang, Z. Q. , Wang, G. Q. , Hashimoto, K. , Zhang, K. , & Liu, H. Z. (2000). Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID‐19. Brain, Behavior, & Immunity ‐ Health, 4, 100064. 10.1016/j.bbih.2020.100064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonetti, V. , Durante, A. , Ambrosca, R. , Arcadi, P. , Graziano, G. , Pucciarelli, G. , Simeone, S. , Vellone, E. , Alvaro, R. , & Cicolini, G. (2021). Anxiety, sleep disorders and self‐efficacy among nurses during COVID‐19 pandemic: A large cross‐sectional study. Journal of Clinical Nursing, 30(9–10), 1360–1371. 10.1111/jocn.15685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, M. L. , Wang, H. , Zhou, Y. R. , Zhang, Y. L. , Xiao, H. , Xia, L. , & Xiao, X. S. (2020). Correlation between sleep quality, psychological condition and work burnout among first clinical first‐line nurses fighting against COVID‐19. Chinese Nursing Research, 34(19), 3545–3549 (in Chinese). 10.12102/j.issn.1009-6493.2020.19.040 [DOI] [Google Scholar]
- Tian, J. J. , & Song, B. B. (2012). Investigation on stressors of night shift work among nurses in cardiology department. Chinese Journal of Modern Nursing, 18(5), 547–549 (in Chinese). 10.3760/cma.j.issn.1674-2907.2012.05.017 [DOI] [Google Scholar]
- Wang, B. Y. , Gao, X. Y. , Wu, J. H. , He, X. W. , Ge, J. R. , Huang, J. S. , Zhang, Y. , Yu, H. Q. , Gu, L. , & Wu, W. Y. (2015). A randomized, single‐blind, blank‐controlled clinical efficacy study of the SML100 multi‐functional insomnia treatment instrument. Chinese Journal of Clinical Neurosciences, 23(1), 77–81 (in Chinese). [Google Scholar]
- Wen, X. Y. (2018). The effect of Liuzijue breathing method combined with music intervention on negative emotion and sleep quality in patients with esophageal varices of liver cirrhosis. International Journal of Nursing, 37(7), 919–922 (in Chinese). 10.3760/cma.j.issn.1673-4351.2018.07.017 [DOI] [Google Scholar]
- World Health Organization . (2020a). Novel coronavirus (2019‐nCoV) situation report‐12 . https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200201‐sitrep‐12‐ncov.pdf?sfvrsn=273c5d35_2
- World Health Organization . (2020b). Coronavirus disease (COVID‐19) pandemic . https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019
- World Health Organization . (2021). Coronavirus disease (COVID‐19) advice for the public . https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/advice‐for‐public
- Wu, T. , Jia, X. , Shi, H. , Niu, J. , Yin, X. , Xie, J. , & Wang, X. (2021). Prevalence of mental health problems during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Affective Disorders, 281, 91–98. 10.1016/j.jad.2020.11.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, L. Q. , Zhang, J. P. , & Tang, H. (2010). Influence of progressive relaxation training on sleep state of fractures patients accepted operation. Chinese Nursing Research, 24(25), 2296–2297 (in Chinese). 10.3969/j.issn.1009-6493.2010.25.016 [DOI] [Google Scholar]
- Xu, M. C. , & Zhang, Y. (2020). Psychological status survey of first clinical first‐line support nurses fighting against pneumonia caused by COVID‐19. Chinese Nursing Research, 34(3), 368–370 (in Chinese). 10.12102/j.issn.1009-6493.2020.03.002 [DOI] [Google Scholar]
- Yin, H. , Phillips, M. R. , Wardenaar, K. J. , Xu, G. , Ormel, J. , Tian, H. , & Schoevers, R. A. (2017). The Tianjin Mental Health Survey (TJMHS): Study rationale, design and methods. International Journal of Methods in Psychiatric Research, 6(3), e1535. 10.1002/mpr.1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
The raw data that support the findings of this study are available by the authors upon reasonable request.


