Abstract
Compared with the nucleic acid amplification test (NATT), the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) rapid antigen self‐testing (RAST) has advantages in speed and convenience. However, little is known about people's acceptance and influencing factors for SARS‐CoV‐2 RAST. A cross‐sectional study was conducted from April 21 to 30, 2022 in China. The χ 2 test and multivariate logistic regressions were used to identify the influencing factors. The structural equation model was used to test the extended protective motivation theory (PMT) model hypotheses. Among the total of 5107 participants, 62.5% were willing to accept the SARS‐CoV‐2 RAST. There were significant differences in acceptance among different residences (p < 0.001), educational level (p < 0.001), occupation (p < 0.001), monthly income (p < 0.001), travel frequency (p < 0.05), and feelings about NATT (p < 0.001). Response efficacy (β = 0.05; p = 0.025) and self‐efficacy (β = 0.84; p < 0.001) had a positive effect, while response cost showed a negative effect (β = −0.07; p < 0.001). The public's major concerns about SARS‐CoV‐2 RAST are its reliability, testing method, price, and authority. Overall, a moderate intention to use SARS‐CoV‐2 RAST was found among the Chinese population. The extended PMT can be used for the prediction of intention to accept the RAST. We need to take measures to increase people's acceptance of SARS‐CoV‐2 RAST.
Keywords: intention, protective motivation theory, rapid antigen self‐testing, SARS‐CoV‐2, structural equation model
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has continued to wreak havoc on public health worldwide. 1 Early detection and early treatment are key measures to prevent and control infectious diseases. Currently, the nucleic acid amplification test (NAAT) is the gold standard for large‐scale SARS‐CoV‐2 screening, because of its high accuracy and reliability. However, the NAAT approach is usually time‐consuming and laborious and has stringent requirements for equipment and operators. 2 , 3 , 4 By contrast, the rapid antigen test (RAT) and rapid antigen self‐testing (RAST) are easy‐to‐use diagnostic tools to identify new contagious individuals, which have more advantages in speed and convenience, and also have a lower transmission risk by avoiding crowd gathering. 5 , 6 In some European and American countries, RAST has been adopted as a common self‐testing method for detecting SARS‐CoV‐2. According to US Center for Disease Control and Prevention, adults increasingly used self‐tests to evaluate their COVID‐19 status from August 2021 to March 2022. 7 Recently, the China government issued a guideline for the use of RAST on March 10, 2022, 8 and some cities such as Beijing, Shanghai, and Guangzhou are promoting the use of SARS‐CoV‐2 RAST.
To promote the acceptance of SARS‐CoV‐2 RAST, a key issue should be clarified regarding people's attitudes toward SARS‐CoV‐2 RAST. 9 In China, large‐scale NATT has achieved great success and is still the dominant measure with high acceptance for SARS‐CoV‐2 screening in public. However, little is known about the influencing factors for accepting SARS‐CoV‐2 RAST. Therefore, it is necessary to conduct a comprehensive survey to understand Chinese people's willingness to accept SARS‐CoV‐2 RAST.
Protection motivation theory (PMT) is a classical social cognition theory that includes two main constructs: threat appraisal (perceived severity, perceived susceptibility), and coping appraisal (response efficacy, self‐efficacy, and response cost). 10 , 11 It had been widely used to predict the motivation of protecting oneself from dangers such as infectious diseases. In previous studies, PMT has been used successfully to explain people's intention to take vaccines 12 , 13 , 14 or screen for cancer. 15 , 16 However, some recent studies have found that other factors which are not specifically mentioned in traditional PMT, such as the level of knowledge, should be an important factor when explaining the intention of vaccination uptake. 17 , 18 It suggests that the classical PMT should be appropriately extended to increase its predictive performance.
Here, we aimed to assess the acceptance of SARS‐CoV‐2 RAST among the Chinese population, and identify the possible influencing factors associated with the acceptance of SARS‐CoV‐2 RAST. Besides, we attempted to add a new dimension to the classic PMT scale to better anticipate people's intentions. We also investigated the public concerns about SARS‐CoV‐2 RAST. This study will provide evidence to improve the COVID‐19 screening strategies for the government of China and other countries.
2. MATERIALS AND METHODS
2.1. Study design and participants
This study was a nationwide online cross‐sectional study conducted from April 21 to 30, 2022 in China. The online questionnaire was developed using the “Wenjuanxing” platform (https://www.wjx.cn/), and spread by snowball sampling with WeChat (https://web.wechat.com/), a social network application. Participants scanned the quick response (QR) code to fill in the questionnaire and then sent the QR code to their WeChat friends. 19 The inclusion criteria were individuals who (1) were at least 14 years old (according to the Chinese health authorities, SARS‐CoV‐2 RAST cannot be performed under 14 years of old 8 ); (2) were able to read and complete the online questionnaire independently; and (3) voluntarily agreed to participate in the investigation. Participants who failed to answer the questions logically and who incorrectly answered the quality control question (which of the following actions can prevent COVID‐19? A: Smoking, B: drinking, C: wearing a mask, and D: Going to a party) were excluded. The minimum sample size was 1024 based on the following formula from the literature 20 :
For setting the formula parameters, we refer to a similar investigation and assumed that 60% of the participants were willing to use the RAST with a margin of error of 3% and a confidence interval of 95%. 21 Considering invalid questionnaires (~20%) for possible real‐world differences, we increased the minimum sample size to 1280.
2.2. Measures
2.2.1. Questionnaire and data collection
The questionnaire was developed by experienced epidemiologists and contained the following parts: demographic characteristics, recent behavior, intention to use RAST, concerns about RAST, as well as an extended PMT scale. The demographic characteristics included age, gender, education level, residence, occupation, monthly income, travel frequency, health status, and COVID‐19 vaccination status. In addition, the cognitive data toward SARS‐CoV‐2 and RAST were acquired through a special scale based on the PMT.
2.2.2. Extended PMT scale
The extended PMT scale was derived and modified from the classical PMT model, 10 , 11 which is widely used to explain how individuals adopt protective measures to prevent diseases. This extended scale contains six dimensions: perceived severity consisted of three items (A1–A3); perceived susceptibility consisted of two items (B1 and B2); response cost consisted of two items (C1 and C2); response efficiency consisted of three items (D1–D3); self‐efficacy consisted of three items (E1–E3); and in the sixth dimension, we used four items to assess participants' knowledge of RATs for COVID‐19 (K1–K4). The detailed statement of each item is available in the questionnaire used in this survey (refer to Supporting Information Materials). Participants were asked how they agreed with each item's statement, and a 5‐points Likert‐style scale was used to score each item, with a range from strongly disagree (1 point) to strongly agree (5 points). A higher score indicates a higher perception of each dimension. The Cronbach's α for the overall scale was 0.679, which indicated acceptable reliability. 22 The confirmatory factor analysis showed that the extended PMT scale had a good construct validity 23 , 24 (Table 1).
Table 1.
Reliability and validity tests for the extended PMT scale
| Content of tests | Testing indexes | Recommended value | Actual value | Comment |
|---|---|---|---|---|
| Reliability | Cronbach's α | >0.6 | 0.679 | Acceptable |
| Validity | GFI | >0.9 | 0.957 | Acceptable |
| IFI | >0.9 | 0.949 | ||
| RMSEA | ≤0.08 | 0.057 |
Abbreviations: GFI, goodness‐of‐fit index; IFI, incremental‐fit index; PMT, protective motivation theory; RMSEA, root mean square error of approximation.
2.2.3. Overall intention to SARS‐CoV‐2 RAST
The overall intention to use SARS‐CoV‐2 RAST was measured based on participants' responses to the following item: “In general, I prefer to use SARS‐CoV‐two rapid antigen self‐tests.” A 5‐point Likert scale was used, with 1 = “strongly unwilling” to 5 = “strongly willing.” The higher score indicated a higher intention. The responses were further classified into two categories: the willing group (score ≥4) and the unwilling group (score <4).
2.3. Data analysis
Frequency and proportion were used to describe the characteristics of participants. The χ 2 test was performed to compare participants' characteristics between their different intentions to the SARS‐CoV‐2 RAST. Multivariate logistic regression was used to further identify the factors that might influence the intention. The structural equation model (SEM) is a multivariate statistical method, which is often used in the analysis of the relationship between complex variables. 25 Therefore, SEM was used to analyze how each dimension of the extended PMT model influenced people's intention to SARS‐CoV‐2 RAST. The fitness of SEM was assessed using fit indexes including goodness‐of‐fit index (GFI), incremental‐fit index (IFI), comparative‐fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). A series of analyses related to SEM was performed using Amos 24.0. The descriptive statistics, χ 2 test, and multivariate logistic regression were performed by SPSS 26.0 (IBM Corporation). The α level was 0.05, and p < 0.05 was considered statistically significant.
3. RESULTS
3.1. Characteristics of participants
In this survey, we collected a total of 5440 participants to answer the questionnaire. After excluding unqualified participants, 5107 (93.9%) participants were included in the following analysis (Figure 1). Among these qualified participants, 3925 (76.9%) participants were aged between 25 and 39 years old. A total of 2684 (52.6%) participants lived in the city, 2217 (43.2%) participants had a bachelor's degree, and 318 (6.2%) participants were healthcare workers. Besides, 3655 (72.9%) participants had received the COVID‐19 booster vaccination (Table 2).
Figure 1.
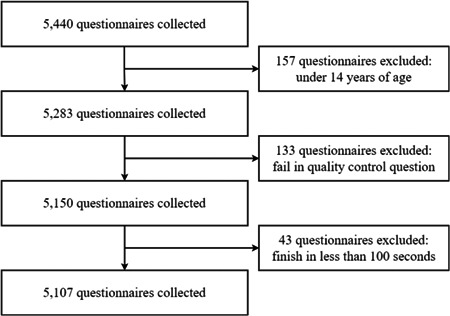
Flowchart of questionnaire collection in this survey. A total of 5440 participants took part in this investigation, and then these unqualified participants, such as inadequate age (157), logical errors in answering the quality control question (133), and too short time to answer the questionnaire (43), were excluded. Finally, 5107 (93.9%) questionnaires were included in the following statistical analysis.
Table 2.
Participants' characteristics and overall intention (N = 5107)
| Characteristics | n | Overall intention | p | |
|---|---|---|---|---|
| Unwilling (%) | Willing (%) | |||
| Gender | 0.121 | |||
| Male | 1027 | 364 (35.4) | 663 (64.6) | |
| Female | 4080 | 1553 (38.1) | 2527 (61.9) | |
| Age | 0.125 | |||
| 14–24 | 258 | 97 (37.6) | 161 (62.4) | |
| 25–39 | 3925 | 1481 (37.7) | 2444 (62.3) | |
| 40–59 | 883 | 331 (37.5) | 552 (62.5) | |
| ≥60 | 41 | 8 (19.5) | 33 (80.5) | |
| Residence | <0.001 | |||
| Urban | 2684 | 931 (34.7) | 1753 (65.3) | |
| Rural | 2423 | 986 (40.7) | 1437 (59.3) | |
| Educational level | <0.001 | |||
| Junior high school or below | 1490 | 629 (42.2) | 861 (57.8) | |
| High school | 1273 | 500 (39.3) | 773 (60.7) | |
| Bachelor | 2217 | 757 (34.1) | 1460 (65.9) | |
| Master or above | 127 | 31 (24.4) | 96 (75.6) | |
| Occupation | <0.001 | |||
| Healthcare workers | 318 | 61 (18.2) | 257 (80.8) | |
| Other | 4789 | 1856 (38.8) | 2933 (61.2) | |
| Chronic conditions | 0.073 | |||
| Yes | 243 | 78 (32.1) | 165 (67.9) | |
| No | 4864 | 1839 (37.8) | 3025 (62.2) | |
| Monthly income | <0.001 | |||
| ≤5000 RMB | 3127 | 1311 (41.9) | 1816 (58.1) | |
| 5001–10 000 RMB | 1458 | 466 (32.0) | 992 (68.0) | |
| >10 000 RMB | 522 | 140 (26.8) | 382 (73.2) | |
| Travel frequency | 0.043 | |||
| Once a week | 26 | 7 (26.9) | 19 (73.1) | |
| Once a month | 70 | 18 (25.7) | 52 (74.3) | |
| Once every 3 months | 103 | 31 (30.1) | 72 (69.9) | |
| Barely | 4908 | 1861 (37.9) | 3047 (62.1) | |
| Went abroad recently | 0.161 | |||
| Yes | 25 | 6 (24.0) | 19 (36.0) | |
| No | 5082 | 1911 (37.6) | 3171 (62.4) | |
| COVID‐19 vaccination | 0.811 | |||
| Never vaccinated | 223 | 78 (35.0) | 145 (65.0) | |
| Received at least one dose | 302 | 111 (36.8) | 191 (63.2) | |
| Fully vaccinated | 917 | 340 (37.1) | 577 (62.9) | |
| Booster vaccinated | 3665 | 1388 (37.9) | 2277 (62.1) | |
| Frequency of NATTs | 0.697 | |||
| ≤3 times a month | 1171 | 431 (36.8) | 740 (63.2) | |
| 4–10 times a month | 3030 | 1157 (38.2) | 1873 (61.8) | |
| 11–20 times a month | 563 | 206 (36.6) | 357 (63.4) | |
| >20 times a month | 343 | 123 (35.9) | 220 (64.1) | |
| Feelings about NATTs | <0.001 | |||
| Unsatisfied or not sure | 431 | 209 (48.5) | 222 (51.5) | |
| Satisfied | 4676 | 1708 (36.5) | 2968 (63.5) | |
Note: The p value was calculated by χ 2 test.
In our survey, we found that the frequency to take NATT in 3030 (59.3%) participants was 4–10 times per month, 563 (11.0%) participants was 11–20 times per month, 343 (6.7%) participants was more than 20 times per month, and the remaining 1171 (22.9%) participants was less 3 times per month. Of note, 4676 (91.6%) participants were satisfied with the experience of their NATTs, while 431 (8.4%) participants were not satisfied.
Totally, 3190 (62.5%) participants were willing to use SARS‐CoV‐2 RAST, whereas 1917 (37.5%) participants were unwilling.
3.2. Factors associated with the intention to use SARS‐CoV‐2 RAST
The results of the univariate analysis revealed that the intention to use SARS‐CoV‐2 RAST was significantly related to the following characteristics: residence (p < 0.001), educational level (p < 0.001), occupation (p < 0.001), monthly income (p < 0.001), travel frequency (p < 0.05), and feelings about NATT (p < 0.001) (Table 2).
Next, we performed the multivariable logistic regression to further identify these characteristics which might affect people's intention to use SARS‐CoV‐2 RAST. The results showed that participants who have a master's degree or above (adjusted odds ratio [AOR]: 1.57, 95% confidence interval [CI]: 1.01–2.42, p = 0.044), whose monthly income between 5001 and 10 000 RMB (AOR: 1.41, 95% CI: 1.23–1.62, p < 0.001) and more than 10 000 RMB (AOR: 1.64, 95% CI: 1.32–2.05, p < 0.001) had higher intention to use SARS‐CoV‐2 RAST. Participants who were satisfied when doing NATT recently (AOR: 1.81, 95% CI: 1.48–2.22, p < 0.001) were more likely to use SARS‐CoV‐2 RAST. In addition, compared with the healthcare workers, participants in other occupations (AOR: 0.45, 95% CI: 0.34–0.60, p < 0.001) were less likely to use SARS‐CoV‐2 RAST (Table 3).
Table 3.
Multivariate logistic regression to analyze the associated factors with the intention to use SARS‐CoV‐2 RAST
| Variable | Classification | AOR | 95% CI | p |
|---|---|---|---|---|
| Residence | Urban | 1.00 | ||
| Rural | 0.93 | 0.83–1.05 | 0.260 | |
| Educational level | Junior high school or below | 1.00 | ||
| High school | 1.04 | 0.89–1.22 | 0.590 | |
| Bachelor | 1.11 | 0.96–1.29 | 0.168 | |
| Master or above | 1.70 | 1.10–2.65 | 0.018 | |
| Occupation | Healthcare workers | 1.00 | ||
| Other | 0.45 | 0.33–0.60 | <0.001 | |
| Monthly income | ≤5000 RMB | 1.00 | ||
| 5001–10 000 RMB | 1.40 | 1.22–1.61 | <0.001 | |
| >10 000 RMB | 1.67 | 1.34–2.08 | <0.001 | |
| Travel frequency | Once a week | 1.00 | ||
| Once a month | 1.18 | 0.42–3.32 | 0.758 | |
| Once every 3 months | 0.98 | 0.37–2.61 | 0.963 | |
| Barely | 0.74 | 0.30–1.79 | 0.499 | |
| Feelings about NATT | Unsatisfied | 1.00 | ||
| Satisfied | 1.81 | 1.48–2.22 | <0.001 |
Note: The p value was calculated by Wald χ 2 test.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; NATT, nucleic acid amplification test; RAST, rapid antigen self‐testing; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2.
3.3. Explaining the intention of SARS‐CoV‐2 RAST using an extended PMT
To clarify whether the extended PMT can explain people's intention to accept SARS‐CoV‐2 RAST, we constructed an SEM as shown in Figure 2. Results showed that the fitness of SEM was acceptable with GFI = 0.950, IFI = 0.945, CFI = 0.935, normed fit index = 0.942, SRMR = 0.055, and RMSEA = 0.061 (Supporting Information: Table S1). To determine whether there were interactions between each dimension of the extended PMT, we analyzed the correlation coefficients between each dimension of the extended PMT. The matrix analysis indicated that the six dimensions of the extended PMT were well correlated with each other (p < 0.05 or p < 0.01), except for perceived susceptibility and response efficacy, perceived susceptibility, and the knowledge of SARS‐CoV‐2 RAST (Table 4). In addition, the path coefficients analysis showed that three dimensions of the extended PMT significantly affected participants' intentions. The response efficacy (β = 0.054; p = 0.025) and self‐efficacy (β = 0.845; p < 0.001) had a positive effect, whereas the response cost showed a negative effect on the participants' intention (β = −0.073; p < 0.001) (Table 5).
Figure 2 .
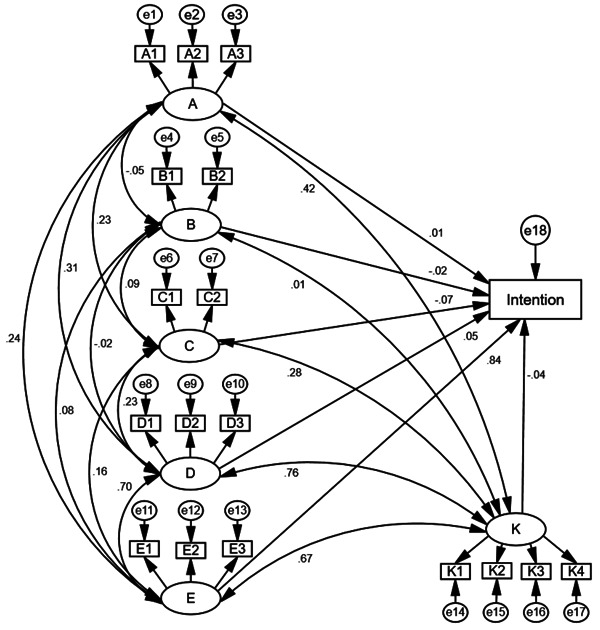
The overview of the structural equation model based on the extended protective motivation theory. Note: A: Perceived severity, A1–A3: Three dimensions of perceived severity; B: Perceived susceptibility, B1 and B2: Two dimensions of perceived susceptibility; C: Response cost, C1 and C2: Two dimensions of response cost; D: Response efficacy, D1–D3: Three dimensions of response efficacy; E: Self‐efficacy, E1–E3: Three dimensions of self‐efficacy; K: Knowledge of RAT, K1–K4: Four dimensions of knowledge; and e1–e18: Measurement error of each observation variable. The path with two‐way arrows represents the correlation between two variables. The path with a single‐way arrow represents regression analyses. The number on the path represents the standardized correlation or regression coefficient.
Table 4.
Correlations between different dimensions of the extended PMT scale
| Variables | A | B | C | D | E | K |
|---|---|---|---|---|---|---|
| A | 1 | |||||
| B | −0.05** | 1 | ||||
| C | 0.23** | 0.09** | 1 | |||
| D | 0.31** | −0.02 | 0.23** | 1 | ||
| E | 0.24** | 0.08** | 0.16** | 0.70** | 1 | |
| K | 0.42** | 0.01 | 0.28** | 0.76** | 0.67** | 1 |
Note: A: perceived severity; B: perceived susceptibility; C: response cost; D: response efficiency; E: self‐efficacy; and K: knowledge of SARS‐CoV‐2 RAST; the correlation coefficients were calculated by the covariance matrix of each variable; and the p value was calculated by t‐test in the SEM analysis.
Abbreviations: PMT, protective motivation theory; RAST, rapid antigen self‐testing; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2; SEM, structural equation model.
p < 0.01.
Table 5.
Path coefficients estimated by structural equation models
| Path | Standardized path coefficients | SE | CR | p |
|---|---|---|---|---|
| A → intention | 0.01 | 0.02 | 0.68 | 0.500 |
| B → intention | −0.02 | 0.10 | −1.92 | 0.055 |
| C → intention | −0.07 | 0.01 | −5.60 | <0.001 |
| D → intention | 0.05 | 0.03 | 2.25 | 0.025 |
| E → intention | 0.84 | 0.03 | 39.73 | <0.001 |
| K → intention | −0.04 | 0.06 | −1.26 | 0.207 |
Note: The p value was calculated by t‐test in the SEM analysis.
Abbreviations: CR, critical ratio; SE, standard error; SEM, structural equation model.
3.4. Public concerns about SARS‐CoV‐2 RAST
In this study, we also investigated what people were concerned about SARS‐CoV‐2 RAST. Most participants (72.0%) were concerned about its reliability. Of note, 59.5% of participants did not accept the current testing method (nasal swabs), 29.8% of participants could accept once a week, and only 1.75% of participants could accept once a day (Supporting Information: Figure S1B). Meanwhile, 65.7% and 40.6% of participants expressed concerns about its convenience and its price, respectively. As for the acceptable price per test, 62.6% of participants chose 0–5 RMB, 25.0% of participants chose 5.1–10 RMB, and only 2.8% of participants could accept more than 20 RMB (Supporting Information: Figure S1A). In addition, 38.3% of participants wonder whether the result of RAST can be approved by the authority (Table 6).
Table 6.
Participants' concerns about SARS‐CoV‐2 RAST (N = 5107)
| Concerns | n (%) |
|---|---|
| Whether the result is reliable | 3679 (72.0%) |
| Whether the operation is convenient | 3356 (65.7%) |
| Whether the price is reasonable | 2075 (40.6%) |
| Whether the result can be approved by the authority | 1957 (38.3%) |
| Whether the result can be got quickly | 1903 (37.3%) |
| Others | 72 (1.4%) |
Abbreviations: RAST, rapid antigen self‐testing; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2.
4. DISCUSSION
Among 5107 participants enrolled in this investigation, there was a moderate intention (62.5%) to use SARS‐CoV‐2 RAST. Compared with our data, recent studies demonstrated that people in European countries had a higher intention (from 72% to 79%) to use SARS‐CoV‐2 RAST. 9 , 26 , 27 This discrepancy may be attributed to several reasons. First, the current SARS‐CoV‐2 RAST kits usually require nasal swabs sampling, while the majority of NAATs conducted in China are sampled from throat swabs. Most Chinese have no experience with nasal swab sampling, and potentially think it is a painful experience. In this survey, we found that 59.5% of participants cannot accept the nasal swabs sampling. In comparison, NAATs in European countries are more frequently sampled from nasal swabs, which is identical to that of the current SARS‐CoV‐2 RAST, and thus the acceptance of nasal swabs sampling is higher in those countries. Of note, some innovative sampling methods are being developed for SARS‐CoV‐2 RAST. For example, a nasal sponge sampling for SARS‐CoV‐2 RAST showed a more comfortable experience in the child and adult populations. 28 Therefore, it is expected to increase the public's acceptance of SARS‐CoV‐2 RAST by using a new sampling approach in the future. Second, the economic level might play a considerable role in the intention to use SARS‐CoV‐2 RAST. In this study, we found that most participants' willingness to pay (WTP) for self‐tests was less than 5 RMB. By contrast, the WTP in Germany was 6.6 euros (≈47 RMB) in the general adult population, 29 which is significantly higher than that in China. It revealed that people in developed countries and developing countries consider prices differently. Consistent with this observation, our study also found that people with a higher monthly income had a higher intention to use SARS‐CoV‐2 RAST. Therefore, to improve the public intention to extensively use RAST, it is necessary to ensure an acceptable price. In addition, the different situations of the COVID‐19 pandemic in different countries might also change attitudes toward the SARS‐CoV‐2 RAST. The low risk of SARS‐Cov‐2 infection in China, because of strong interventions including quarantine, mask mandates, mass vaccination, and extensive NAAT, 30 , 31 , 32 might make people relax their vigilance, so they might think that SARS‐CoV‐2 RAST is unnecessary.
The frequency to take NATT in 59.3% of participants was 4–10 times per month, which reflected that the large‐scale NATT was still the major measure to screen COVID‐19 cases in China. At first, it was worried whether the high frequency of NATT screening would lead to dissatisfaction and even mental stress among the public. However, in this investigation, we found that 91.6% of participants were satisfied with the current NATT experience, even with the high testing frequency. Interestingly, participants who were satisfied with the recent NAAT experience also had a higher intention to use SARS‐CoV‐2 RAST in this study. To our knowledge, the satisfaction with NAAT experience might imply that these participants have a good attitude toward SARS‐CoV‐2 prevention and control, and thus be willing to cooperate with RAST detection. As a result, these participants would be more likely to use SARS‐CoV‐2 RAST. In addition, our study found that healthcare workers' intention to use SARS‐CoV‐2 RAST was higher than that of non‐healthcare workers, which also reflected that the attitude of healthcare workers toward medical interventions is significantly more positive than that of the general public. 33 , 34
A previous study showed a low level of knowledge of SARS‐CoV‐2 detection methods among the public in China. 35 Consequently, we expect that the knowledge of SARS‐CoV‐2 RAST will play a role in people's intentions, and that is why we employed the extended PMT model in this study. The findings of the structural equation model demonstrated an appropriate fit for our extended PMT. Path analysis revealed that response efficacy and self‐efficacy had a direct positive influence on intention, while response cost had a direct negative effect, which was consistent with previous studies on COVID‐19 vaccination willingness. 12 , 36 Although the dimension of knowledge did not show a direct effect on intention in our study, there was a correlation between knowledge and the other five dimensions of PMT. Besides, this study demonstrated that educational level, which is generally considered related to knowledge, is an influential factor in the intention. Furthermore, knowledge has been extensively thought of as a critical component in the fight against COVID‐19, 37 as individuals with high levels of knowledge are more likely to have protective motivation. 38 , 39
This study was the first investigation into the acceptance of RAST among the Chinese population. Compared with previous surveys about SARS‐CoV‐2 RAST, we first time used the extended PMT scale to better explain the people's intentions about SARS‐CoV‐2 RAST. Nevertheless, there are some limitations to our study. First, this investigation was conducted through a convenient sampling, which might not generalize our results. Second, similar to other cross‐sectional studies, we cannot make causal inferences about factors related to public intention. Third, we collected some data about the public's attitudes and behaviors toward NATT, but this questionnaire setting was not detailed enough to analyze the influencing factors of attitudes and behaviors related to NATT. To further understand how well people will accept SARS‐CoV‐2 NATT and RAST, a more in‐depth investigation should be conducted in the future. In addition, as the COVID‐19 pandemic continues to fluctuate, it will be important to monitor the dynamic changes in the public's intention of SARS‐CoV‐2 RAST.
5. CONCLUSION
This study demonstrated that the overall intention to use SARS‐CoV‐2 RAST was moderate in China. Educational level, monthly income, and satisfaction with recent NAAT experience were positively correlated with the intention to use SARS‐CoV‐2 RAST. Major concerns about SARS‐CoV‐2 RAST are its reliability, testing method, price, and authority. Of note, we found for the first time that the extended PMT model is efficient in explaining public intention to use SARS‐CoV‐2 RAST. Thus, interventions based on the extended PMT model should be considered to further improve the acceptance of SARS‐CoV‐2 RAST and the COVID‐19 screening strategies for the government of China and other countries.
AUTHOR CONTRIBUTIONS
Caijun Sun conceived and designed this project. Fan Wu performed this project and analyzed the data. Yanjun Li, Xueying Fan, Chunhuan Zhang, and Xiangyue Zeng contributed to the resources and discussion. Fan Wu, Yue Yuan, Yanjun Li, Bing Lang, Yangguo Zhao, and Di Yin drafted the manuscript. Huachun Zou, Xiangyue Zeng, and Caijun Sun revised and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was approved by the Ethics Committee of the School of Public Health (Shenzhen), Sun Yat‐sen University (Approval number: SYSU‐PHS‐IACUC‐2022 −022).
Supporting information
Supplementary information.
ACKNOWLEDGMENTS
The authors appreciate all members for carefully reading and editing this manuscript. They are also grateful to all the participants in this investigation. This study was funded by the National Key R&D Program of China (2022YFE0203100, 2021YFC2300103), the National Natural Science Foundation of China (82041043, 81971927), and the Science and Technology Planning Project of Shenzhen City (JSGG20200225152008136, 20190804095916056).
Wu F, Yuan Y, Li Y, et al. The acceptance of SARS‐CoV‐2 rapid antigen self‐testing: a cross‐sectional study in China. J Med Virol. 2022;95:e28227. 10.1002/jmv.28227
Contributor Information
Xiangyue Zeng, Email: lwcdczxy@gz.gov.cn.
Caijun Sun, Email: suncaijun@mail.sysu.edu.cn.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.World Health Organisation (WHO) coronavirus (COVID‐19) dashboard 2022. Accessed May 20, 2022. https://covid19.who.int/
- 2. Vogels CBF, Brito AF, Wyllie AL, et al. Analytical sensitivity and efficiency comparisons of SARS‐CoV‐2 RT‐qPCR primer‐probe sets. Nat Microbiol. 2020;5(10):1299‐1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang M, Cao S, Liu Y, et al. Performance verification of five commercial RT‐qPCR diagnostic kits for SARS‐CoV‐2. Clin Chim Acta. 2022;525:46‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yokota I, Shane PY, Teshima T. Logistic advantage of two‐step screening strategy for SARS‐CoV‐2 at airport quarantine. Travel Med Infect Dis. 2021;43:102127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Raïch‐Regué D, Muñoz‐Basagoiti J, Perez‐Zsolt D, et al. Performance of SARS‐CoV‐2 Antigen‐Detecting rapid diagnostic tests for Omicron and other variants of concern. Front Microbiol. 2022;13:810576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Møller IJB, Utke AR, Rysgaard UK, Østergaard LJ, Jespersen S. Diagnostic performance, user acceptability, and safety of unsupervised SARS‐CoV‐2 rapid antigen‐detecting tests performed at home. Int J Infect Dis. 2022;116:358‐364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rader B, Gertz A, Iuliano AD, et al. Use of at‐home COVID‐19 tests—United States, August 23, 2021–March 12, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(13):489‐494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Notice on printing the SARS‐CoV‐2 antigen testing application protocol (Trial) (in Chinese). Accessed March 11, 2022. http://www.gov.cn/xinwen/2022-03/11/content_5678610.htm
- 9. Betsch C, Sprengholz P, Siegers R, et al. Empirical evidence to understand the human factor for effective rapid testing against SARS‐CoV‐2. Proc Natl Acad Sci USA. 2021;118(32):e2107179118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bui L, Mullan B, McCaffery K. Protection motivation theory and physical activity in the general population: a systematic literature review. Psychol Health Med. 2013;18(5):522‐542. [DOI] [PubMed] [Google Scholar]
- 11. Rogers RW. A protection motivation theory of fear appeals and attitude change1. J Psychol. 1983;19(5):469‐479. [DOI] [PubMed] [Google Scholar]
- 12. Xiao Q, Liu X, Wang R, et al. Predictors of willingness to receive the COVID‐19 vaccine after emergency use authorization: the role of coping appraisal. Vaccines. 2021;9(9):967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ling M, Kothe EJ, Mullan BA. Predicting intention to receive a seasonal influenza vaccination using protection motivation theory. Soc Sci Med. 2019;233:87‐92. [DOI] [PubMed] [Google Scholar]
- 14. Wu F, Yuan Y, Deng Z, et al. Acceptance of COVID‐19 booster vaccination based on the protection motivation theory: a cross‐sectional study in China. J Med Virol. 2022;94(9):4115‐4124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wei W, Zhang M, Zuo D, et al. Screening intention prediction of colorectal cancer among urban Chinese based on the protection motivation theory. Int J Environ Res Public Health. 2022;19(7):4203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li Q, Liu Q, Chen X, et al. Protection motivation theory in predicting cervical cancer screening participation: a longitudinal study in rural Chinese women. Psychooncology. 2020;29(3):564‐571. [DOI] [PubMed] [Google Scholar]
- 17. Huang P‐C, Hung C‐H, Kuo Y‐J, et al. Expanding protection motivation theory to explain willingness of COVID‐19 vaccination uptake among Taiwanese university students. Vaccines. 2021;9(9):1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu M, Cui T, Wang Q, et al. Using an extended protection motivation theory to explain vaccine hesitancy: a cross‐sectional study among Chinese adults. Hum Vaccin Immunother. 2022;18(1):2026136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kong Y, Jiang H, Liu Z, Guo Y, Hu D. The uptake and vaccination willingness of COVID‐19 vaccine among Chinese residents: web‐based online cross‐sectional study. Vaccines. 2022;10(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cai H, Bai W, Liu S, et al. Attitudes toward COVID‐19 vaccines in Chinese adolescents. Front Med. 2021;8:691079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thomas C, Shilton S, Thomas C, et al. Values and preferences of the general population in Indonesia in relation to rapid COVID‐19 antigen self‐tests: a cross‐sectional survey. Trop Med Int Health. 2022;27(5):522‐536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peterson Robert A. A meta‐analysis of Cronbach's coefficient alpha. J Consum Res. 1994;21(2):381. [Google Scholar]
- 23. Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238‐246. [DOI] [PubMed] [Google Scholar]
- 24. Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multi Behav Res. 1990;25(2):173‐180. [DOI] [PubMed] [Google Scholar]
- 25. Kang H, Ahn J‐W. Model setting and interpretation of results in research using structural equation modeling: a checklist with guiding questions for reporting. Asian. Nurs Res. 2021;15(3):157‐162. [DOI] [PubMed] [Google Scholar]
- 26. Stillman S, Tonin M. Communities and testing for COVID‐19. Eur J Health Econ. 2022;23(4):617‐625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Goggolidou P, Hodges‐Mameletzis I, Purewal S, Karakoula A, Warr T. Self‐testing as an invaluable tool in fighting the COVID‐19 pandemic. J Prim Care Community Health. 2021;12:21501327211047782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Prazuck T, Gravier A, Pires‐Roteira D, et al. Evaluation of a new “all in one” SARS‐CoV‐2 antigen‐detecting rapid diagnostic test AND self‐test: diagnostic performance and usability in child and adult populations. J Med Virol. 2022;94(9):4097‐4106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hajek A, König H‐H. Willingness to pay for SARS‐CoV‐2 rapid antigen tests during the COVID‐19 pandemic: evidence from the general adult population. Public Health. 2022;207:19‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cai J, Deng X, Yang J, et al. Modeling transmission of SARS‐CoV‐2 Omicron in China. Nat Med. 2022;28(7):1468‐1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chen M, Yuan Y, Zhou Y, et al. Safety of SARS‐CoV‐2 vaccines: a systematic review and meta‐analysis of randomized controlled trials. Infect Dis Poverty. 2021;10(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lin Y, Peng F. Control strategies against COVID‐19 in China: significance of effective testing in the long run. PLoS One. 2021;16(7):e0253901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tsai W‐T, Chen C‐M, Chung M‐C, et al. Important factors influencing willingness to participate in advance care planning among outpatients: a pilot study in central Taiwan. Int J Environ Res Public Health. 2022;19(9):5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Adedeji‐Adenola H, Olugbake OA, Adeosun SA. Factors influencing COVID‐19 vaccine uptake among adults in Nigeria. PLoS One. 2022;17(2):e0264371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lan R, Sujanto R, Lu K, He Z, Zhang C, Ming WK. Perceived effectiveness, safety, and attitudes toward the use of nucleic tests of SARS‐CoV‐2 among clinicians and general public in China. Front Public Health. 2020;8:599862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ansari‐Moghaddam A, Seraji M, Sharafi Z, Mohammadi M, Okati‐Aliabad H. The protection motivation theory for predict intention of COVID‐19 vaccination in Iran: a structural equation modeling approach. BMC Public Health. 2021;21(1):1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Adugna B, Merera O, Negash W, Abdulkadir O, Mohammed Y. Knowledge, attitude and practice (KAP) assessment on LifeStyle, public health measures practiced by society and their impact to contain COVID‐19 transmission among afar community in selected parts of Afar region, Ethiopia. Infect Drug Resist. 2022;15:1277‐1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ding Q, Lin S, Wang S. Determinants and willingness to pay for purchasing mask against COVID‐19: a protection motivation theory perspective. Int J Environ Res Public Health. 2022;19(7):4268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Marks DF. Psychological homeostasis and protective behaviours in the COVID‐19 pandemic. J Health Psychol. 2022;27(6):1275‐1287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


