Dear Editor,
SARS-CoV-2 infections are expected in ~ 10% of the vaccinated population (breakthrough infection) [1]. Although early data showed that progression to critical illness was less likely among vaccinated than unvaccinated patients [2], recent data show that mortality in patients requiring admission to the intensive care unit (ICU) did not differ [3], or was higher [4, 5] in vaccinated than unvaccinated patients.
This study sets up to test the hypothesis that when age, comorbidities, and pathophysiological conditions are considered, vaccines are effective to prevent deaths in patients requiring ICU admission for breakthrough infection.
This prospective multicenter observational study enrolled patients from 27 ICUs in Italy (June 1st, 2021–June 31st, 2022). Entry criteria were age ≥ 18 and respiratory failure associated to coronavirus disease 2019 (COVID-19) with a P/F < 300. Exclusion criteria were (a) pre-existing limitations on the use of life-sustaining treatments; (b) no/incomplete information on vaccination status.
Study endpoint was hospital mortality. Age, comorbidities, arterial-to-inspiratory O2 ratio (P/F), Simplified Acute Physiology Score (SAPS) II, and Sequential Organ Failure Assessment (SOFA) score were collected. Patients were classified as “vaccinated” (two-dose of mRNA vaccines or single-dose vaccine) and “unvaccinated” (one-dose of mRNA vaccines or no dose). Hospital mortality was adjusted using a multivariate logistic regression model that included age, comorbidities, clinical conditions at ICU admission, vaccination status, period of admission to the ICU (June 1st, 2021–December 31st, 2021, vs. January 1st, 2022–June 31st, 2022) and their interaction (online supplement). A sensitivity analysis was conducted comparing predicted vs. observed mortality in vaccinated and unvaccinated patients [6].
Among the 916 patients admitted, 262 were vaccinated (28.6%) (Fig. 1, online supplement). Vaccinated patients were older (71 vs. 63 years p < 0.001), with more comorbidities (91.2% vs. 65.7%, p < 0.001), had more renal and metabolic failures (40.5% vs. 25.1% and 26.3% vs. 18.5%, respectively; p < 0.001), and had higher SAPS II and SOFA scores (39 vs. 32 and 6 vs. 4, respectively; p < 0.001) (Table 1, online supplement).
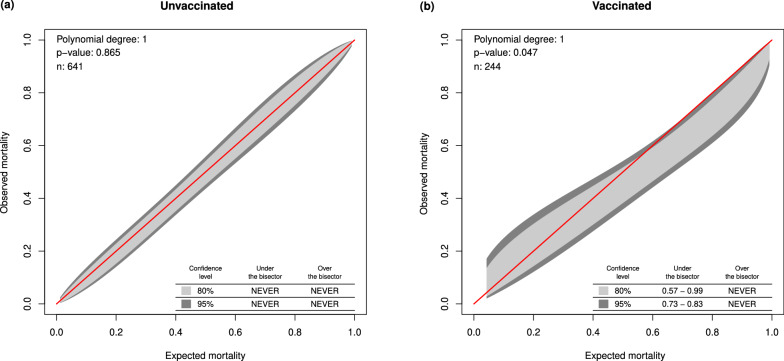
Crude hospital mortality and risk of death in vaccinated were higher than in unvaccinated [54.7% vs. 41.3%, p < 0.001; OR 1.72 (95%CI: 1.28–2.30); p < 0.001, respectively]. After adjusting for covariates, risk of death in vaccinated was lower than in unvaccinated patients [OR 0.66 (95%CI: 0.44–0.98); p = 0.04)]. Neither year of admissions nor its interaction with vaccination status was statistically significant (Figs. 2 and 3, online supplement). In vaccinated patients, observed hospital mortality was lower than expected hospital mortality (Fig. 1, p = 0.047).
Fig. 1.
Calibration belts (light and dark gray: 80% and 95% confidence levels, respectively) comparing observed and expected mortality for unvaccinated (a) and vaccinated patients (b). A calibration belt below the line of identity indicates that observed mortality is lower than mortality expected according to the model
Lack of information regarding (a) time and vaccine brand; (b) whether the patients received a third booster dose; (c) the type of the SARS-CoV-2 variants infecting the patient are the major limitations of the present analysis. Although other techniques are available to deal with confounding factors, the granularity of the identified risk factors and the inclusion of the non-linear behavior of some of these factors allowed our logistic regression model to correct the observed risk of death [6]. The robustness of these methods may explain the difference in vaccination efficacy to reduce the risk of death also in ICU patients with outbreak infection observed in the present study but not reported in previous studies [3–5] in vaccinated than unvaccinated patients.
Our study therefore confirms the effectiveness of vaccination to reduce the risk of death also in ICU patients with breakthrough infection.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The Authors thank Roberto Fumagalli and Caterina Rizzo for their invaluable suggestions in designing this study and their helpful comments on our manuscript. GiViTI: Gruppo Italiano per la Valutazione Interventi in Terapia Intensiva. Writing Committee. Stefano Finazzi, Matilde Perego, Giovanni Tricella (Laboratory of Clinical Data Science, Department of Public Health, Mario Negri Institute for Pharmacological Research IRCCS, Ranica (BG), Italy) Daniele Poole (Anesthesia and Intensive Care, San Martino Hospital, Belluno, Italy) Caterina Rizzo (Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy), Mario Peta (Anesthesia and Intensive Care, Ospedale Cà Foncello - Treviso, Aulss 2 Marca Trevigiana, Italy), and V. Marco Ranieri (Alma Mater Studiorum–Università di Bologna, IRCCS Policlinico di Sant’Orsola, Anesthesia and Intensive Care Medicine, Bologna, Italy). Investigators and Centers. Antonella Jorio: Ospedale Area Vasta 2, Jesi; Nicola Petrucci: Azienda Socio-Sanitaria Territoriale Del Garda, Desenzano; Andrea Della Selva: Ospedale Michele E Pietro Ferrero, Verduno; Rita Tenio: Ospedale S. Croce, Mondovi; Francesco Cocciolo: Ospedale M. Bufalini, Cesena; Manuela Bonizzoli: Azienda Ospedaliero Universitaria Careggi, Firenze; Francesca Covani Frigieri: Ospedale S. M. Annunziata, Bagno A Ripoli; Romano Giuntini: Ospedale San Giuseppe, Empoli; Vieri Parrini: Ospedale Del Mugello, Borgo San Lorenzo; Giampiero Bagalini: Ospedale Augusto Murri, Fermo; Stefano Falini: Ospedale Usl9, Grosseto; Rita Ciceri: Ospedale Asst, Lecco; Monica Giuntoli: Spedali Riuniti, Livorno; Omar Alquati: Ospedale Maggiore, Lodi; Loredana Faraldi: Ospedale Niguarda, Milano-ICU building A; Riccardo Giudici: Ospedale Niguarda, Milano-ICU building B; Alessandra Parnigotto: Ospedale Ulss 6 Euganea, Monselice; Dino A.C. Di Pasquale: Ospedale Felice Lotti, Pontedera; Paolo Malacarne: Azienda Ospedaliera-Universitaria Pisana, Pisa; Manuela Carli: Ospedale Di Pistoia, Pistoia; Andrea Bottazzi: Fondazione Policlinico San Matteo, Pavia; Maria Babini: Ospedale Civile Lugo, Lugo; Gianluca Zani: Ospedale Santa Maria Delle Croci, Ravenna; Michela Zardin: Ospedale S. Chiara, Trento; Alessandro Mastroianni: Ospedale Maggiore, Chieri; Mario Peta: Ospedale Cà Foncello Santa Maria Dei Battuti, Treviso; Alice Pero: Ospedale San Andrea, Vercelli. GiViTI Steering Committee: Francesca Baroncelli, S.C. Anestesia e Rianimazione 2, Ospedale San Giovanni Bosco, Torino, Italy; Pietro Caironi, Department of Anesthesia and Critical Care, Azienda Ospedaliero-Universitaria S. Luigi Gonzaga, Orbassano, Italy; Arturo Chieregato, S.C. Neurorianimazione, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy; Cristiana Alessandra Cipolla, S.C. Neurorianimazione, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy; Stefano Finazzi, Laboratory of Clinical Data Science, Department of Public Helath, Mario Negri Institute for Pharmaoclogical Research IRCCS, Ranica (BG), Italy; Roberto Fumagalli, Dipartimento di Anestesia e Rianimazione, ASST Grande Ospedale Metropolitano Niguarda, School of Medicine and Surgery, University of Milano-Bicocca, Milan, Italy; Elena Garbero, Laboratory of Clinical Data Science, Department of Public Helath, Mario Negri Institute for Pharmaoclogical Research IRCCS, Ranica (BG), Italy; Aimone Giugni, UOC Anestesia, Rianimazione ed Emergenza Territoriale 118 – Bologna Dipartimento di Emergenza Ospedale Maggiore – AUSL di Bologna, Italy; Martin Langer, Emergency ONG-ONLUS, Milan, Italy; Carlo Olivieri, Anesthesia and Intensive Care, ospedale Sant’Andrea, Vercelli, Italy; Daniele Poole, Operative Unit of Anesthesia and Intensive Care, San Martino Hospital, Belluno, Italy; Mario Tavola; Bruno Viaggi, Department of Anesthesiology, Neuro-Intensive Care Unit, Florence Careggi University Hospital, 50139 Florence, Italy; Anna Zamperoni, Ospedale Ca’ Foncello, Treviso, Italy. GiViTI Coordinating Center, Laboratory of Clinical Data Science, Mario Negri Institute for Pharmacological Research IRCCS: Stefano Finazzi, Head of Laboratory; Alice Lavetti, Secretary; Valentina Barbetta, Project Manager; Francesca Dore, Project Manager; Elena Garbero, Project Manager; Francesca Sommariva, Project Manager; Mauro Bellinzona, ICT; Alessandro Esposito, ICT; Mauro Ghilardi, ICT; Michele Giardino, ICT; Michele Zanetti, ICT; Demetrio Magatti, Statistical Analysis; Matilde Pergo, Statistical Analysis; Giovanni Tricella, Statistical Analysis.
Author contributions
All authors have contributed substantially to the conception and design of the study, the acquisition of data, or the analysis and interpretation of the data. All authors drafted or provided critical revision of the article. All authors provided the final approval of the version submitted for publication.
Funding
This work was supported by Regione Piemonte and Toscana (SF, MP, and GT) and PRIN 2017_J4BE7A (VMR).
Data availability
Data are available upon request at stefano.finazzi@marionegri.it.
Declarations
Conflicts of interest
CR declared consultancy fees for ad hoc advisory board meeting and honoraria for Lecture from Seqirus, MSD, Sanofi, outside from the submitted work. All other authors declare no conflicts of interest.
Footnotes
Stefano Finazzi and Matilde Perego equally contributed as first author.
The full list of members, Steering Committee, Investigators and Coordinating center of GiViTi are listed in the Acknowledgement section at the end of the manuscript.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Stefano Finazzi, Email: stefano.finazzi@marionegri.it.
V. Marco Ranieri, Email: m.ranieri@unibo.it.
GiViTI (Italian Group for the Evaluation of Interventions in Intensive Care Medicine):
Caterina Rizzo, Roberto Fumagalli, Jorio Antonella, Petrucci Nicola, Della Selva Andrea, Tenio Rita, Cocciolo Francesco, Bonizzoli Manuela, Covani Frigieri Francesca, Giuntini Romano, Parrini Vieri, Bagalini Giampiero, Falini Stefano, Ciceri Rita, Giuntoli Monica, Alquati Omar, Faraldi Loredana, Giudici Riccardo, Parnigotto Alessandra, Di Pasquale Dino, Aurelio Cleto, Malacarne Paolo, Carli Manuela, Bottazzi Andrea, Babini Maria, Zani Gianluca, Zardin Michela, Mastroianni Alessandro, Peta Mario, and Pero Alic.
References
- 1.Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65. doi: 10.1038/s41577-021-00662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tenforde MW, Self WH, Adams K, Gaglani M, Ginde AA, McNeal T, Ghamande S, Douin DJ, Talbot HK, Casey JD, Mohr NM, Zepeski A, Shapiro NI, Gibbs KW, Files DC, Hager DN, Shehu A, Prekker ME, Erickson HL, Exline MC, Gong MN, Mohamed A, Henning DJ, Steingrub JS, Peltan ID, Brown SM, Martin ET, Monto AS, Khan A, Hough CL, Busse LW, Ten Lohuis CC, Duggal A, Wilson JG, Gordon AJ, Qadir N, Chang SY, Mallow C, Rivas C, Babcock HM, Kwon JH, Halasa N, Chappell JD, Lauring AS, Grijalva CG, Rice TW, Jones ID, Stubblefield WB, Baughman A, Womack KN, Rhoads JP, Lindsell CJ, Hart KW, Zhu Y, Olson SM, Kobayashi M, Verani JR, Patel MM, Influenza, Other Viruses in the Acutely Ill N Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021;326:2043–2054. doi: 10.1001/jama.2021.19499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hilty MP, Keiser S, Wendel Garcia PD, Moser A, Schuepbach RA, Switzerland R-IIf mRNA-based SARS-CoV-2 vaccination is associated with reduced ICU admission rate and disease severity in critically ill COVID-19 patients treated in Switzerland. Intensive Care Med. 2022;48:362–365. doi: 10.1007/s00134-021-06610-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motos A, Lopez-Gavin A, Riera J, Ceccato A, Fernandez-Barat L, Bermejo-Martin JF, Ferrer R, de Gonzalo-Calvo D, Menendez R, Perez-Arnal R, Garcia-Gasulla D, Rodriguez A, Penuelas O, Lorente JA, Almansa R, Gabarrus A, Marin-Corral J, Ricart P, Roche-Campo F, Sancho Chinesta S, Socias L, Barbe F, Torres A, Project C Higher frequency of comorbidities in fully vaccinated patients admitted to the ICU due to severe COVID-19: a prospective, multicentre, observational study. Eur Respir J. 2022;59:2102275. doi: 10.1183/13993003.02275-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G, Zanella A, Carlesso E, Florio G, Canakoglu A, Bellani G, Bottino N, Cabrini L, Castelli GP, Catena E, Cecconi M, Cereda D, Chiumello D, Forastieri A, Foti G, Gemma M, Giudici R, Grazioli L, Lombardo A, Lorini FL, Madotto F, Mantovani A, Mistraletti G, Mojoli F, Mongodi S, Monti G, Muttini S, Piva S, Protti A, Rasulo F, Scandroglio AM, Severgnini P, Storti E, Fumagalli R, Pesenti A, Network C-LI. Association of COVID-19 vaccinations with intensive care unit admissions and outcome of critically ill patients with COVID-19 pneumonia in Lombardy, Italy. JAMA Netw Open. 2022;5:e2238871. doi: 10.1001/jamanetworkopen.2022.38871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finazzi S, Poole D, Luciani D, Cogo PE, Bertolini G. Calibration belt for quality-of-care assessment based on dichotomous outcomes. PLoS ONE. 2011;6:e16110. doi: 10.1371/journal.pone.0016110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request at stefano.finazzi@marionegri.it.