Abstract
Aims
Diabetes mellitus is a chronic disease that limits the quality and duration of life. We aimed to estimate the impact of demographic change on the burden of prediabetes and diabetes between 2010 and 2021, and the projections to 2030 and 2045 in Turkiye.
Materials and methods
Prediabetes and diabetes estimates were calculated by direct standardization method using age- and sex-specific prevalence data from the previous ‘Turkish Epidemiology Survey of Diabetes, Hypertension, Obesity and Endocrine Disease’ (TURDEP-II) as reference. The 2010–2021 population demographics were obtained from TurkStat. Comparative age-adjusted diabetes prevalence was estimated using the standard population models of world and Europe.
Results
Estimates depicted that the population (20–84 years) of any degree of glucose intolerance in Turkiye increased by over 5.7 million (diabetes: 2.4 million and prediabetes: 3.3 million) from 2010 to 2021. While the increase in prediabetes and diabetes prevalence was 24.3% and 35.2% in overall population, corresponding increase were 46.5% and 51.3% in the elderly. Estimated prevalence of prediabetes and diabetes in 2021 was significantly higher in women than in men (prediabetes: 32.6% vs. 25.2%; diabetes: 17.1% vs. 14.2%). The comparative age-adjusted diabetes prevalence to the European population model was higher than that of the world population model (19.4% vs. 15.0%). According to the projections the prevalence of diabetes will reach 17.5% in 2030 and 19.2% in 2045.
Conclusion
Assuming age- and sex-specific diabetes prevalence of TURDEP-II survey remained constant, this study revealed that the number of people with diabetes in the general population (particularly in the elderly) in the last 11 years in Turkiye has increased in parallel with the population growth and aging; it will continue to grow over the coming decades. This means the burden of diabetes on the social, economic and health services will remain to increase. The fact suggests that there is an urgent need for re-organization of care as well as to develop and implement a country-specific prevention program to reduce this burden.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10654-022-00960-8.
Keywords: Epidemiology, Population-based field survey, Age- and sex-specific prevalence, Age-adjusted prevalence, Comparative prevalence, Prediabetes, Diabetes, Elderly
Introduction
Diabetes mellitus, particularly type 2, is recognized as a serious public health problem with a significant impact on human life and health expenditures [1]. With the increase in obesity and the adoption of a sedentary lifestyle in recent decades, the incidence and prevalence of diabetes have increased rapidly all over the world in both developed and developing countries [2]. According to recent estimates by the International Diabetes Federation (IDF), the global diabetes age-adjusted prevalence in 2021 was 10.5% (over half a billion people with diabetes); the prevalence raised by 12.9% since the previous estimates in 2019 [1, 2]. Diabetes is projected to 11.3% in 2030 and 12.2% in 2045 [1].
Diabetes is a costly disease due to high complication rates, treatment, and monitoring expenses; It is also well known that diabetes reduces the quality of life and life expectancy as it responsible to an estimated USD 966 billion in global health expenditure in 2021 [1]. Although much progress has been achieved in promoting population health and extending life, diabetes remained the second biggest cause of reduced global health-adjusted life expectancy worldwide [3]. Approximately 6.7 million adults are estimated to have died due to diabetes or its complications in 2021. This accounts for 12.2% of global deaths from all causes [1].
Although many epidemiologic studies have been conducted at different time points and regions in Turkiye, the number of reproducible studies reflecting the general population is limited. In this respect, population-based TURDEP surveys provided important knowledge in terms of the frequency of prediabetes and diabetes, risk factors, and comorbidities such as obesity and hypertension. In the Turkish Diabetes Epidemiology (TURDEP-I) survey conducted in the adult (20 + years, n = 24,788) population in 1998, the age-adjusted diabetes prevalence was reported 7.2% (F: 8.0% and M: 6.2%) [4]. Twelve years after, in the Turkish Epidemiology Survey of Diabetes, Hypertension, Obesity and Endocrine Disease (TURDEP-II; n = 26,499), performed at the same 540 centers and using the same methodology, the age- and sex-specific crude prevalence of diabetes increased to 16.5% (F: 17.2% and 16% for men) [5]. It is noteworthy that diabetes prevalence nearly doubled over 12 years. Other relatively smaller studies conducted in the period close to this study such as Chronic Renal Disease in Turkey (CREDIT) [6], Turkish Adult Risk Factor (TEKHARF) [7], and Metabolic Syndrome (MetSend) studies [8] also confirmed this increase. Although the previous studies have implied a sharp increase in the prevalence of diabetes in the population [6–8], evidence from a later meta-analysis of studies with low risk of bias in Turkiye suggested that the incidence of diabetes would be levelling off as it is seen in several developed countries recently [9, 10]. Nonetheless, due to population growth, diabetes continues to pose a significant public health burden as one of the most important noncommunicable diseases (NCDs) in the country [11].
Unfortunately, no field study conducted to observe diabetes epidemiology across the country since 2010. Although global, regional, and country-based diabetes estimates are periodically published by large research groups [10, 12–14], studies that reference to the country's own population and using the real demographic dynamics may provide more valuable information on the burden of diabetes.
The lack of high-quality data in recent years has been an obstacle to reassessing the burden of diabetes in Turkiye. In fact, a new study was planned for 2020 with the same methodology as previous population-based surveys to understand the changes from 2010, nevertheless, it could not be performed due to the COVID-19 pandemic restrictions.
Therefore, assuming that the age- and sex-specific prevalence of diabetes in Turkiye does not change considerably, we aimed to estimate the impact of demographic change on the burden of diabetes and prediabetes between 2010 and 2021 and its implications for 2030 and 2045.
Material and methods
Terminology
For the purpose of avoiding any confuses, the terms we used to describe the prevalence of prediabetes and diabetes at different settings in this paper are explained as follows: Age- and sex-specific prevalence refers to the raw prevalence obtained from a study conducted in the country (in this case TURDEP-II survey); Age-adjusted prevalence refers to the estimated prevalence in the official annual population or the projected population of the country [15]; and Comparative prevalence refers to the estimated age-adjusted prevalence using the standard population models [16, 17].
American Diabetes Association (ADA) criteria were taken into account in the diagnosis of prediabetes and diabetes. Isolated impaired fasting glucose (i-IFG): Fasting plasma glucose (FPG) 5.6–6.9 mmol/L and OGTT 2-hrPG < 7.8 mmol/L; isolated impaired glucose tolerance (i-IGT): FPG < 5.6 mmol/L and OGTT 2-hrPG 7.8–11.0 mmol/L; combined glucose intolerance (IFG + IGT): FPG 5.6–6.9 mmol/L and OGTT 2-hrPG 7.8–11.0 mmol/L; high risk group (HRG): Glycosylated hemoglobin A1c (HbA1c) 39–48 mmol/mol [18].
Population and demographic data
In this study, we used the crude prevalence data of TURDEP-II survey. It is important to note that this data is standardized to the country’s official population as well as to the standard populations. Annual demographic data of the population of Turkiye at the provincial and regional levels between 2010 and 2021 are obtained from Address-Based Population Registration System (ABPRS) which is publicly available in the official data portal of the National Institute of Statistics (TurkStat) [15]. For international comparisons, the WHO [16] and Europe [17] standard population models are used.
Age groups and age-adjusted prevalence
Age-adjusted prediabetes and diabetes prevalence each time calculated for the general (20–84 years) as well as the elderly (65–84 years) populations. For calculations, the age by 5-year intervals and both sexes considered as determined in the TURDEP-II survey [5]. Thus, we used a 2 × 13 matrix for the general and a 2 × 4 matrix for the elderly populations. The prevalence was estimated at the provincial level first, and then the regional and national averages were calculated via weighted averages considering the population of the provinces. The estimated age-adjusted prevalence between 2010 and 2021 was calculated by applying the observed age- and sex-specific prevalence to the population using the direct standardization method [19].
Future projections
Population projections were obtained from TurkStat first, which is produced this data based on the ABPRS and used the cohort component method. In this method, demographic change components including gender and age specific mortality rates, fertility rates and net migration were taken into account according to the recommendations of the United Nations Population Division (UNPD). To predict the age-adjusted prevalence of diabetes for 2030 and 2045, we applied the raw prevalence results of TURDEP-II survey to the projected populations by TurkStat. We also calculate the prevalence using the UNDP projections (obtained from its data portal) [20]. In addition, we performed a regression analysis of the age-adjusted prevalence between 2010 and 2021, since we obtained a linear trend, we predicted the diabetes prevalence for 2030 and 2045 using the regression line.
Comparative prevalence
To remove the effect of differences in the age structure and permit international comparisons of prediabetes and diabetes prevalence between Turkiye and other countries, two comparative estimates were performed. In this case, the raw prevalence of TURDEP-II (by 5-year age intervals, in both sexes) is standardized to the world and the European population models [16, 17].
Ethical approval
Ethics Committee approval was obtained from Istanbul Faculty of Medicine for TURDEP-II study [5] which forms the basis of the current paper (16.4.2008/699). Although ethics committee approval is not required for the present study, the subject was discussed at the Turkish Institute of Public Health and Chronic Diseases Board and it was found appropriate to conduct the study (November 9th, 2020, no. 9).
Statistical analysis
The results were shown as frequencies (percentages) for categorical variables, and mean values and 95% CIs for continuous variables. Pairwise comparisons analyzed with Student’s t-test or Pearson chi-squared test, as appropriate. A p value < 0.05 was used as the level of statistical significance.
The future estimates were calculated for 20–84 years of age by 5-year intervals and females and males, separately. In this case, the raw prevalence results applied to the projected populations. We also performed a regression analysis of estimated prevalence for 2010–2021 period which showed a linear trend; then, we predicted the future prevalence from the regression line. The accuracy of the model was assessed through the explained variance (R2 > 0.99 and p < 0.05).
Results
Estimates on age-adjusted prediabetes prevalence over 11-year
While the age-adjusted estimated total prediabetes prevalence was 29.6% (F: 32.3%, M: 24.4%) in 2010, it was calculated as 30.2% (F: 32.6% and M: 25.2%) for 2021. The estimated 11-year population growth with prediabetes was 24.3% (2010: 13,687,585 million vs. 2021: 17,015,340 million). In contrast, the estimated prevalence of elderly prediabetes was 33.9% (F: 34.9%, M: 32.5%) and the 11-year population increase was calculated as 46.5%. In 2021, 14.6% of the estimated entire prediabetes population was in the 65–84 age group (Table 1).
Table 1.
Estimated age-adjusted prediabetes and diabetes prevalences between 2010 and 2021 in Turkiye (20–84 years and 65–84 years) [18]
| Category | 2010% Prevalence (n) | 2021% Prevalence (n) | 11-year Difference% Change (n) | ||||
|---|---|---|---|---|---|---|---|
| Men | Women | General | Men | Women | General | General | |
| Prediabetes based on FPG and OGTT 2-hrPG (20–84 years) | |||||||
| Total prediabetes (IFG and/or IGT) | 24.4%(5,860,213) | 32.3%(7,827,372) | 29.6%(13,687,585) | 25.2%(7,369,989) | 32.6%(9,645,351) | 30.2%(17,015,340) | 24.3%(3,327,755) |
| i-IFG | 14.6%(3,503,287) | 14.5%(3,507,173) | 14.6%(7,010,460) | 14.8%(4,316,571) | 14.4%(4,259,032) | 14.6%(8,575,603) | 22.3%(1,565,143) |
| i-IGT | 5.2%(1,245,267) | 9.0%(2,175,310) | 7.7%(3,420,577) | 5.4%(1,587,168) | 9.1%(2,696,776) | 7.9%(4,283,944) | 25.2%(863,367) |
| Combined glucose intolerance (IFG + IGT) | 4.6%(1,111,659) | 8.9%(2,144,889) | 7.3%(3,256,548) | 5.0%(1,466,250) | 9.4%(2,763,423) | 7.8%(4,229,673) | 29.9%(973,125) |
| Elderly prediabetes based on FPG and OGTT 2-hrPG (65–84 years) | |||||||
| Total prediabetes (IFG and/or IGT) | 32.5%(730,438) | 34.9%(969,810) | 34.0%(1,700,248) | 32.5%(1,115,800) | 34.9%(1,375,473) | 33.9%(2,491,273) | 46,5%(791,025) |
| i-IFG | 12.3%(274,485) | 9.8%(271,196) | 10.9%(545,681) | 12.3%(422,134) | 9.9%(411,325) | 10.9%(833,459) | 52.7%(287,778) |
| i-IGT | 10.5%(233,919) | 11.2%(309,977) | 10.9%(543,896) | 10.4%(357,842) | 11.2%(465,038) | 10.9%(822,880) | 51.3%(278,984) |
| Combined glucose intolerance (IFG + IGT) | 10.0%(222,034) | 14.0%(388,637) | 12.2%(610,671) | 9.8%(335,824) | 13.8%(572,990) | 12.1%(908,814) | 48.8%(298,143) |
| Prediabetes based on HbA1c (20–84 years) | |||||||
| HRG | 17.3%(4,145,750) | 23.0%(5,578,396) | 21.0%(9,724,146) | 18.7%(5,458,253) | 24.4%(7,205,341) | 22.3%(12,663,594) | 23.2%(2,939,448) |
| Elderly prediabetes based on HbA1c (65–84 years) | |||||||
| HRG | 35.7%(794,913) | 36.0%(1,001,121) | 35.9%(1,796,034) | 35.3%(1,210,624) | 35.9%(1,493,170) | 35.7%(2,703,794) | 50.5%(907,760) |
| Diabetes mellitus (20–84 years) | |||||||
| Total diabetes | 12.7%(3,060,002) | 15.5%(3,752,871) | 14.3%(6,812,873) | 14.2%(4,151,754) | 17.1%(5,061,058) | 15.5%(9,212,812) | 35.2%(2,399,939) |
| Known diabetes | 6.9%(1,653,653) | 8.2%(1,984,945) | 7.6%(3,638,598) | 7.8%(2,283,363) | 9.2%(2,731,262) | 8.6%(5,014,625) | 37.8%(1,376,027) |
| Undiagnosed diabetes | 5.8%(1,402,672) | 7.3%(1,761,661) | 6.7%(3,164,333) | 6.4%(1,864,876) | 7.9%(2,321,594) | 7.3%(4,186,470) | 32.3%(1,022,137) |
| Elderly diabetes (65–84 years) | |||||||
| Total diabetes | 30.1%(671,001) | 38.7%(1,074,916) | 35.0%(1,745,917) | 30.2%(1,035,594) | 38.6%(1,605,932) | 35.1%(2,641,526) | 51.3%(895,609) |
| Known diabetes | 16.7%(372,155) | 22.6%(627,570) | 20.0%(999,725) | 17.0%(584,326) | 22.9%(949,584) | 20.4%(1,533,910) | 53.4%(534,185) |
| Undiagnosed diabetes | 14.4%(298,846) | 16.1%(446,559) | 14.9%(745,405) | 13.2%(451,268) | 15.8%(655,156) | 14.7%(1,106,424) | 48.4%(361,019) |
FPG, fasting plasma glucose; OGTT, oral glucose tolerance test; 2-hrPG, 2-hour plasma glucose; i-IFG, isolated impaired fasting glucose; i-IGT, isolated impaired glucose tolerance; HbA1c, glycosylated hemoglobin A1c; HRG, high risk group
The prevalence of i-IFG in the general population in 2010 was 14.6% (F: 14.5%, M: 14.6%), i-IGT 7.7% (F: 9% and M: 5.2%), and combined glucose intolerance (IFG + IGT) 7.3% (F: 8.9%, M: 4.6%). The estimated increase in people with i-IFG, i-IGT, and IFG + IGT between 2010 and 2021 was 22.3%, 25.2%, and 29.9%, respectively.
In the elderly group in 2010, the prevalence of i-IFG was 10.9% (F: 9.8%, M: 12.3%), i-IGT 10.9% (F: 11.2% and M: 10.5%), and IFG + IGT 12.2% (F: 14%, M: 10%). The estimated increase in people with i-IFG, i-IGT, and IFG + IGT between 2010 and 2021 was 52.7%, 51.3%, and 48.8%, respectively (Table 1).
Similarly, in 2010, the prevalence of HRG in the general population was 21% (F: 23%, M: 17.3%), while in the elderly it was 35.9% (F: 36%, M: 35.7%). In the 11-year period from 2010 to 2021, the estimated increase in people at HRG category was 23.2% for the general population and 50.5% for the elderly group (Table 1).
Estimates on age-adjusted diabetes prevalence over 11-year
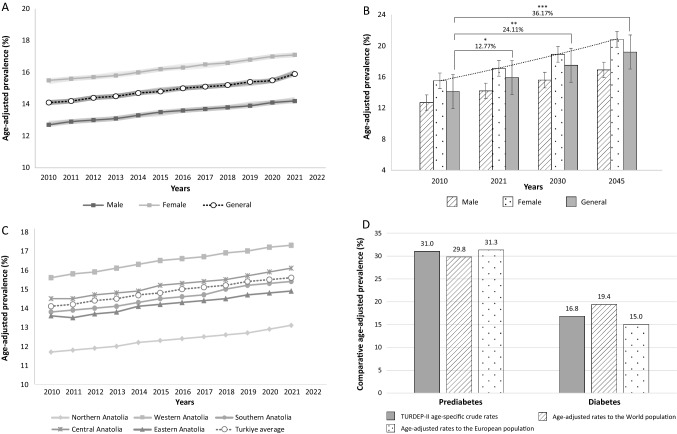
Annual estimates for age-adjusted diabetes prevalence between 2010 and 2021 showed a linear trend, increased from 14.3% (F: 15.5%, M: 12.7%) in 2010 to 15.5% (F: 17.1%, M: 14.2%) in 2021 (Table 2, and Fig. 1A). The estimated rate of increase in this period was 12.8%, p < 0.05 (Fig. 1B).
Table 2.
The distribution according to years and genders of the age-adjusted diabetes prevalence in Turkiye
| Results | 2000a | 2007a | 2010b | 2011b | 2012b | 2013b | 2014b | 2015b | 2016b | 2017b | 2018b | 2019b | 2020b | 2021b | 2030c | 2045c |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | 0.056 | 0.061 | 0.127 | 0.129 | 0.130 | 0.131 | 0.133 | 0.135 | 0.136 | 0.137 | 0.138 | 0.139 | 0.141 | 0.142 | 0.156 | 0.169 |
| LL 95% CI | 0.056 | 0.061 | 0.127 | 0.129 | 0.130 | 0.131 | 0.133 | 0.134 | 0.136 | 0.137 | 0.138 | 0.139 | 0.141 | 0.142 | 0.156 | 0.169 |
| UL 95% CI | 0.056 | 0.061 | 0.128 | 0.129 | 0.130 | 0.131 | 0.133 | 0.135 | 0.136 | 0.137 | 0.138 | 0.140 | 0.141 | 0.143 | 0.157 | 0.170 |
| Women | 0.076 | 0.083 | 0.155 | 0.156 | 0.157 | 0.158 | 0.160 | 0.162 | 0.163 | 0.165 | 0.166 | 0.168 | 0.170 | 0.171 | 0.189 | 0.208 |
| LL 95% CI | 0.076 | 0.082 | 0.154 | 0.156 | 0.157 | 0.158 | 0.160 | 0.162 | 0.163 | 0.164 | 0.166 | 0.168 | 0.170 | 0.171 | 0.189 | 0.208 |
| UL 95% CI | 0.076 | 0.083 | 0.155 | 0.156 | 0.157 | 0.159 | 0.160 | 0.162 | 0.164 | 0.165 | 0.166 | 0.168 | 0.170 | 0.171 | 0.190 | 0.208 |
| General | 0.066 | 0.072 | 0.141 | 0.142 | 0.144 | 0.145 | 0.147 | 0.148 | 0.150 | 0.151 | 0.152 | 0.154 | 0.155 | 0.155 | 0.175 | 0.192 |
| LL 95% CI | 0.066 | 0.072 | 0.141 | 0.142 | 0.144 | 0.145 | 0.147 | 0.148 | 0.150 | 0.151 | 0.152 | 0.153 | 0.155 | 0.155 | 0.175 | 0.192 |
| UL 95% CI | 0.066 | 0.072 | 0.141 | 0.142 | 0.144 | 0.145 | 0.147 | 0.149 | 0.150 | 0.151 | 0.152 | 0.154 | 0.155 | 0.155 | 0.176 | 0.193 |
LL 95% CI, lower limit of 95% confidence interval; UL 95% CI, upper limit of 95% confidence interval. aCalculated based on the national census data and the reference diabetes prevalences are obtained from TURDEP-I survey. bCalculated based on the annual TurkStat data between 2010 and 2021, and the reference diabetes prevalences are obtained from TURDEP-II survey. cPredictions based on the annual TurkStat data between 2010 and 2021, and the reference diabetes prevalence results are obtained from TURDEP-II survey
Fig. 1.
A Change of age-adjusted diabetes prevalence between the years 2010 and 2021 in Turkiye. B Comparison of estimated prevalence for 2030 and 2045 with those of 2010 and 2021. Statistical comparisons made on the general population. *p < 0.05, **p < 0.01, ***p < 0.001. C Age-adjusted diabetes prevalence of the five geographical regions of Turkiye between 2010 and 2021. D Comparative age-adjusted prediabetes and diabetes prevalence according to the world [16] and European [17] standard populations. Bottom note: Prediabetes prevalence based on impaired fasting glucose and/or impaired glucose tolerance
Approximately, 28.7% of people with diabetes was in the elderly age. Estimated age-adjusted diabetes prevalence in 2021 was 35.1% (F: 38.6%, M: 30.2%) in this group. The estimated diabetes increase over the 11-year period was 35.2% in the general population and 51.3% in the elderly group. In other words, the number of adults (20–84 years old) with diabetes increased nearly 2.4 million between 2010 and 2021, exceeding 9.2 million in total (at least 2.6 million of whom in the elderly ages).
Between 2010 and 2021, the age-adjusted estimated prevalence of known diabetes in the general population increased from 7.8 to 8.6%. Undiagnosed diabetes also increased, from 6.7 to 7.3%. Both known and undiagnosed diabetes were higher in women than men. In the elderly group, known diabetes was 20.4% and undiagnosed diabetes was 14.7%. Similar to the general population, both were more common in women than men (Table 1).
Future projections
The calculated prevalence of diabetes for 2030 and 2045 by three methods gave very close estimates, with only small differences in decimals. Based on TurkStat projections the predicted prevalence of diabetes in the general population was 17.5% (F: 18.9%, M: 15.6%) in 2030, and 19.2% (F: 20.8%, M: 16.9%) in 2045. Accordingly, expected rate of increase in diabetes in the general population will be 24.1% (p < 0.01) between 2010 and 2030 and 36.1% (p < 0.001) between 2010 and 2045 (Table 2 and Fig. 1B). The corresponding general diabetes prevalence using the UNPD projections was 17.2% in 2030, and 19.3% in 2045. While based on the linear increasing trend between 2010 and 2021, the age-adjusted diabetes prevalence in general is predicted to reach 17.3% in 2030 and 19.1% in 2045. The results of the linear regression model and those of the UNPD projections are presented as electronic supplementary material (Suppl. Table 1).
Regional status
Geographically, the diabetes trends increased in all regions of the country with the highest estimated frequency in Western Anatolia (from 15.6% in 2010 to 17.3% in 2021), and the lowest in Northern Anatolia (from 11.7% in 2010 to 13.1% in 2021). Whereas diabetes trends in Central, Southern, and Eastern Anatolian regions were similar, and close to each other (Fig. 1C).
Comparative prevalence
In TURDEP-II survey, the age- and sex-specific prevalence of prediabetes (IFG and/or IGT) was 31%, HRG 23.5%, and diabetes 16.8%, (Suppl. Table 2). In this study, the comparative age-adjusted prevalence of prediabetes (IGT and/or IFG) is estimated 29.8% and 31.3% based on the standard world and the European population models, respectively. Whereas, the comparative age-adjusted prevalence of HRG is calculated 18.2% and 22.1%, in the same order. On the other hand, the comparative age-adjusted diabetes prevalence using the standard world and the European population models is estimated 15.0% and 19.4%, respectively (Fig. 1D, Suppl. Table 2).
Discussion
Considering only the population dynamics between 2010 and 2021, this study estimates that the 11-year growth in the country’s population with any degree of glucose intolerance is over 5.7 million (nearly 2.4 million with diabetes and 3.3 million with prediabetes). Diabetes prevalence is projected to increase to 17.5% in 2030 and 19.2% in 2045. In the general population (20–84 years), the estimated increase in the prediabetes population between 2010 and 2021 was 24.3% and diabetes 35.2%. However, the rate of increase in the elderly group (65–84 year) was much higher (prediabetes: 46.5%, diabetes: 51.3%).
Our study is referenced to a large nationwide population-based field survey [5]. TURDEP-II provided important information about changes in the prevalence and risk factors of diabetes, hypertension and obesity in the country over a twelve-year period. When compared to the previous nationwide TURDEP-I survey [4], the results had been suggested that diabetes reached to an epidemic proportion in the country, and the fact was confirmed by others [6–8]. Undoubtedly, one of the most important reasons for it was sociocultural and economic transition of the society experienced in the last quarter of the twentieth century. The effect of this transition on public health which was inevitably led to changing lifestyle, i.e., consuming high-calorie foods, and reduced physical activity. Genetic and epigenetic factors and the longer life expectancy were other accountable factors for the increase in the prevalence of diabetes. On the contrary, a later meta-analysis revealed that the diabetes prevalence reached a stable level [9]. However, even if age- and sex-specific diabetes prevalence remained constant, the results of the current study indicated a considerable increase in the number of people at risk of diabetes and patients with diabetes and it will go on in the coming decades.
Aging of the population
Increased life expectancy due to decreasing birth and mortality rates has led to the aging of the society. Median age, which is one of the best indicators in this regard, increased from 24.8 to 33.1 years in Turkiye between 2000 and 2019, corresponding to an increased average life expectancy at birth from 67 to 75.9 years in men and from 73 to 81.2 years in women [21]. While the population aged 65 years and above was 8.2% of the total population in 2015 and reached 9.7% (over 8.2 million people) in 2021 (55.7% women). The proportion of the elderly population will continue to increase; It is expected to be 11.0% by 2025 and 16.3% by 2040 [22].
Diabetes mellitus is a common chronic disease in the elderly, being either a known disease with a long history (often type 2 diabetes) or may have been ignored for a rather long time. Age and weight are main risk factors for the development of diabetes. Notable in normal aging there is nearly 0.1 mmol per liter per decade rise in FPG, placing older people at increased risk for the development of diabetes [23]. Weight gain and decreased muscle mass are often seen with increasing age, resulting in worsened insulin resistance and impaired beta-cell function. In addition, concomitant diseases, decreased activity, and medications can worsen insulin resistance. According to the 2021 estimates of the current study, the prevalence of age-adjusted diabetes in the general population is 15.5%, while it was 2.3 times higher (35.1%) in the 65 years and older group. Furthermore, the 11-year diabetes increase in the elderly group was nearly 1.5 times higher than in the general population (51.3% vs. 35.2%). With the improvements in the follow-up and treatment of diabetes, diabetes-related deaths in Turkiye have been started to decline. While the death rate due to diabetes was 22.0 per 100,000 in 2010, it decreased to 17.1 per 100,000 in 2019 (the number of annual death due to diabetes have been obtained from publicly available TurkStat portal, and the rates calculated by the authors). The decrease in diabetes-related mortality may contribute to the increase in the population with diabetes (especially the elderly). The situation in elderly diabetes is very similar in developed countries. However, the proportion of elderly at risk of diabetes is not yet as high as in developed countries. One-third of the U.S. population over 65 years old has diabetes, and one half of those has prediabetes [24].
Other national studies on diabetes and prediabetes
Although a limited number of population-based studies have been conducted in the country since the beginning of the 2000s, there was no consistency between the studies, especially in age of the participants and the method of diagnosis. Except that the TURDEP surveys, OGTT was not used. Diagnosis of diabetes was based on self-reported diabetes on antidiabetic therapy and FPG and/or HbA1c.
The Ministry of Health periodically screens for NCDs including diabetes and prediabetes in the population. Accordingly, the prevalence of diabetes in the adult population in ‘Turkey Frequency of Chronic Diseases and Risk Factors Survey, 2011’ was 12.3% [25], in ‘WHO STEPwise approach to NCD risk factor Surveillance (STEPS)-Turkey, 2017’ was 12.2% [26], and in ‘Turkey Nutrition and Health Survey, 2017′ 13.5% [27]; Diabetes was always more prevalent among women than men. The results of the studies cited above have confirmed that the rapid increase in diabetes incidence between 1998 and 2010 is at least slowed-down or stopped.
However, in the case of prediabetes since OGTT was not performed, we do not have information about IGT. Besides, there is an uncertainty for IFG as some studies used ADA [18] and others WHO (FPG 6.1–6.9 mmol/L) criteria [28]. The prevalence of IFG in ‘Turkey Frequency of Chronic Diseases and Risk Factors Survey, 2011’ (ADA criteria, in age 15 + years) was 15.8% [25]; whereas using WHO criteria [28] in ‘STEPS-Turkey, 2017’ (15 + years) 7.9% [26]; and in ‘Turkey Nutrition and Health Survey, 2017’ (20 + years) 17.3% [27]. In the latter, 24.3% of the participants had HRG [27].
Based on the 2021 estimates from the current study, we can assume that three out of ten adults in the country have IFG and/or IGT and one out of five adults has HRG. In the elderly population, one-in-three people may have any degree of prediabetes. IGT is more prevalent among women. In addition, 11-year increase in prevalence of prediabetes and HRG are close to each other; estimates for the general population are 24.3% and 23.2%; while in the elderly, the rate of increase in both categories was 1.9 and 2.2 times higher than in the general population (Table 1).
Geographic distribution
In ‘Turkey Frequency of Chronic Diseases and Risk Factors Survey, 2011’, known diabetes was highest in West Marmara (10.2%) and lowest in Northeast Anatolia (5.9%) [25]. Similarly, in ‘Turkey Nutrition and Health Survey, 2017’, the highest diabetes prevalence was in Western BlackSea Region (14.4%) [27]. The results of the current study are consistent with the above-mentioned studies; accordingly, it is estimated that total diabetes is lowest in North Anatolia (13.1%) and highest in West Anatolia (17.3%) in 2021.
Diabetes in the Middle East and Balkan countries
According to the diabetes trends between the years 1980–2014 reported by WHO, the Eastern Mediterranean Region has experienced the greatest rise in diabetes prevalence [11]. Likewise, IDF’s Middle East and North Africa (MENA) region had the highest comparative prevalence above seven regions [2]. Diabetes affects over 25% of the adults in Saudi Arabia [29], 16.7% in Qatar [30]. Rapid transformation of lifestyle from rural to urban, socioeconomic development, decreased physical activity, and high consumption of fat and sweetened foods are responsible from obesity and diabetes epidemics in these countries [31]. Whereas, based on IDF 2019 estimations, Lebanon (11.2%) and Libya (10.2%) had the closest comparative prevalence to Turkiye (11.1%) [2]. The prevalence of diabetes in STEPS-Iran was 7.7% in 2005 and 10.9% in 2016, higher among females than males; [35]. In Jordanian adults, diabetes increased gradually from 6.4% in 2002 to 23.7% in 2017 [36].
The lifestyle in Balkans shows much similarities with the Turkish population. In Greece, EMENO survey (2013–2016), 11.6% of the adult population had diabetes [32]. In Republic of Macedonia, the prevalence of known diabetes in population 20–79 years was 5.0%, higher in females than in males [33]. A study in Bulgaria reported a 7.9% diabetes prevalence in 2006 and 9.6% in 2012, both more prevalent among men [34].
Global situation of diabetes and prediabetes
NCD Risk Factor Collaboration reported that age-adjusted global diabetes prevalence slightly increased since 1980. However, due to population growth and aging, the number of adults with diabetes nearly four times increased over three decades [13]. Age-adjusted diabetes prevalence in 2014 was lowest in north-western Europe and highest in Polynesia and Micronesia, followed by MENA [13].
Global Burden of Disease collaborators stated that the prevalence of type 2 diabetes in 2017 was 13.2%, higher among males than females, especially in high-income countries. Generally, the burden of diabetes had increased significantly since 1990. In 2017, the global incidence, prevalence, death, and disability-adjusted life-years related with diabetes were 22.9, 476, 1.4, and 67.9 million; with a projection to 26.6, 571, 1.6, and 79.3 million in 2025, respectively [37]. Accordingly, the estimated number of new type 2 diabetes cases in Turkiye was reported 257,336 in 2017, representing a 35.6% increase since 2007. The incidence rate was 290 per 100,000 population in 2017, representing a 7.6% increase throughout the study period [38]. In a WHO report, the comparative age-adjusted diabetes prevalence in Turkiye was 12.2% in 2014 [11], and rose to 13.2% in 2016 [39].
Our estimates from 2010 to 2021 revealed that the burden of diabetes is increasing. This is consistent with the existed studies in the region and it seems to continue over the couple of decades. Recently, IDF declared that Turkiye ranks the top first country in Europe with both diabetes prevalence and population with diabetes [1]. In the present study, the comparative diabetes prevalence was calculated 19.4% using the standard European population. This indicates that if our society aged like the European countries; the burden of diabetes will continue to increase.
Finally, the projected diabetes prevalence is forecasted to increase among the elderly appreciably in this country. IDF projections imply that Turkiye will be the top ninth country with nearly 5 million elderly people with diabetes by 2045 [40]. It is clear that the public health impact and challenge of increasing numbers of older people with diabetes will likely be substantial. It seems that diabetes will continue to stretch the financial budget for public health and social care services due to more years to be lived unhealthy, frail, and disability in our aging society.
The strengths and limitations
This study is the first comprehensive analysis to estimate the age-adjusted diabetes prevalence and forecast the future expectations in Turkiye using reference data from a previous population-based field survey and annual demographic dynamics of the population. In addition, the use of both FPG, OGTT, and HbA1c made it possible to make predictions for various degrees of prediabetes categories. Other strengths of our study are that we calculated the comparative prevalence to the standard world and European populations, as well as the expected diabetes increase to 2030 and 2045. Obviously, results of the current study will help to rearrange the healthcare system particularly for the elderly patients with diabetes. The huge proportion of the population at risk of diabetes emphasizes the need for more specific programs to prevent or postpone diabetes.
Nevertheless, we were not able to model different risk factors such as nutritional and exercise habits, obesity, hypertension, smoking, alcohol consumption, birth weight, socioeconomic status, or public health interventions. Another limitation of our study is that we could not take into account the effects of the diabetes prevention measures carried out throughout the country since 2010. In the 2010–2021 period, two national action plans were prepared for diabetes prevention. In the first (The Turkey Diabetes Prevention and Control Program 2011–2014), legislations for schools, workplaces and other collective living spaces, circulars for environmental regulations by the local governments have been prepared and put into effect; Guidelines, training modules and instructions were prepared for physicians and other healthcare professionals. During ‘The National Diabetes Program 2015–2020’, specific programs have been designed to tackling the obesity. 'Healthy Nutrition and Active Life Program’ was implemented within this framework. As, limited progress could be obtained in practice, to expand the scope and measure the effectiveness, a software program named "Disease Management Platform" was put into practice aiming to screen for NCDs including diabetes and follow-up people (especially the elderly) with NCDs, at the family health centers [41]. In the TURDEP-II field survey, the prevalence of new diabetes in the general population was 6.7%, while it was 14.9% in the elderly group. Of the total diabetics, 45.1% in the general population and 42.6% in the elderly group were unaware of their disease [5]. It is strongly possible that screening and prevention programs increased awareness and reduced the rate of undiagnosed diabetes. For example, in ‘STEPS-Turkey, 2017’, the average prevalence of undiagnosed diabetes was 24.2%; however, the rate in men was still high (men: 40.2% vs. women 13.1%) [26].
The restrictions imposed by the COVID-19 pandemic, which has affected the whole world since the beginning of 2020, have caused people to gain weight due to increased inactivity and changed eating habits [42]. If the increase in obesity cannot be stopped; It will be inevitable that we will face a more intense diabetes pandemic globally in the next decades. In this scenario, our and others' modeling is likely to have underestimated future diabetes trends for 2030 and 2045 [2, 10, 37].
Conclusion
Forecasts based on population dynamics that provide projections for the country's medium-term future will provide critical information for health policy makers. Periodic prevalence estimates and projections for diabetes can offer a rational guidance to facilitate the promotion of prevention programs, particularly for type 2 diabetes, and improve care for all people with diabetes. According to our estimates, more than 9.2 million people (including 2.6 million elderly) are currently suffering from diabetes in Turkiye, and another 17 million with any degree of prediabetes (including 2.5 million elderly). It is projected that the prevalence of diabetes will increase to 17.5% in 2030 and 19.2% by 2045 reflecting a steady increase in diabetes population in all regions of the country in both men and women over the next decades.
This scenario poses that the burden of diabetes on the society that could hinder social and economic development. Further actions are needed to understand the drivers of this problem and develop more rational prevention strategies addressing the growing public health challenge. Unless fundamental steps are taken through a national prevention program to reduce diabetes in Turkiye, the burden of diabetes on health services will become even more overwhelming.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the TURDEP Study Groups who worked in the epidemiological field surveys and the TurkStat for allowing access to demographic data.
Author Contributions
IS designed the study and gathered the data. HI and KYA created the database. SB and FO analyzed data with input from SC, NE and MY. SB, YDM, MY and SC searched the literature and assisted in the interpretation of the results. GG drew the figures. IS and SB drafted the manuscript. KYA and HI critically revised it for important intellectual content. All authors have read and approved the final version of the paper.
Funding
This study did not receive any external grants from government, private or commercial sources. The original TURDEP-II survey was funded by The Turkish Scientific and Technical Research Council–TUBITAK (Project no. 109S166), The Society of Endocrinology and Metabolism of Turkey (SEMT), and Istanbul University Scientific Research Fund (Project no. 6417 and 6418).
Declarations
Conflict of interest
The authors declared no competing interests in this work.
Footnotes
The list of TURDEP-II Study Group members was published in Eur J Epidemiol 2013;28(2):169-80.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
I. Satman, S. Bayirlioglu, K. Y. Arga and H. Issever have contributed equally to this work.
References
- 1.International Diabetes Federation. Diabetes Atlas, 10th Ed, IDF Press, Bruxelles: 2021. Available at https://diabetesatlas.org/atlas/tenth-edition/. Accessed on Dec 15th, 2021. ISBN 978–2–930229–98–0.
- 2.International Diabetes Federation. IDF Diabetes Atlas, 9th edition. Brussels, 2019. Available at https://diabetesatlas.org/idfawp/resource-files/2019/07/IDF_diabetes_atlas_ninth_edition_en.pdf. Accessed on Jan 15th, 2021. ISBN 978-2-930229-87-4.
- 3.Chen H, Chen G, Zheng X, Guo Y. Contribution of specific diseases and injuries to changes in health adjusted life expectancy in 187 countries from 1990 to 2013: retrospective observational study. BMJ. 2019;364:l969. doi: 10.1136/bmj.l969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Satman I, Yilmaz T, Sengül A, Salman S, Salman F, Uygur S, Bastar I, Tütüncü Y, Sargin M, Dinççag N, Karsidag K, Kalaça S, Ozcan C, King H. Population-based study of diabetes and risk characteristics in Turkey: results of the Turkish diabetes epidemiology study (TURDEP) Diabetes Care. 2002;25(9):1551–1556. doi: 10.2337/diacare.25.9.1551. [DOI] [PubMed] [Google Scholar]
- 5.Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, Karsidag K, Genc S, Telci A, Canbaz B, Turker F, Yilmaz T, Cakir B, Tuomilehto J; TURDEP-II Study Group. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28(2):169–80. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed]
- 6.Suleymanlar G, Utas C, Arinsoy T, Ates K, Altun B, Altiparmak MR, Ecder T, Yilmaz ME, Camsari T, Basci A, Odabas AR, Serdengecti K. A population-based survey of Chronic REnal Disease In Turkey–the CREDIT study. Nephrol Dial Transplant. 2011;26(6):1862–1871. doi: 10.1093/ndt/gfq656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Onat A, Cakır H, Karadeniz Y, Donmez I, Karagoz A, Yuksel M, Can G. TEKHARF 2013 taramasi ve diyabet prevalansinda hizli artis [Turkish Adult Risk Factor survey 2013: rapid rise in the prevalence of diabetes] Turk Kardiyol Dern Ars. 2014;42(6):511–6. doi: 10.5543/tkda.2014.27543. [DOI] [PubMed] [Google Scholar]
- 8.Gundogan K, Bayram F, Gedik V, Kaya A, Karaman A, Demir O, Sabuncu T, Kocer D, Coskun R. Metabolic syndrome prevalence according to ATP III and IDF criteria and related factors in Turkish adults. Arch Med Sci. 2013;9(2):243–253. doi: 10.5114/aoms.2013.34560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yilmaz MB, Kilickap M, Abaci A, Barcin C, Bayram F, Karaaslan D, Goksuluk H, Kayikcioglu M, Ozer N, Suleymanlar G, Sahin M, Tokgozoglu L, Satman I. Temporal changes in the epidemiology of diabetes mellitus in Turkey: A systematic review and meta-analysis. Turk Kardiyol Dern Ars. 2018;46(7):546–55. doi: 10.5543/tkda.2018.88225. [DOI] [PubMed] [Google Scholar]
- 10.Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi: 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tokgozoglu L, Kayikcioglu M, Altay S, Aydogdu S, Barcin C, Bostan C, Cakmak HA, Catakoglu AB, Emet S, Ergene O, Kalkan AK, Kaya B, Tulunay Kaya C, Kaymaz C, Koylan N, Kultursay H, Oguz A, Ozpelit E, Unlu S. EUROASPIRE-IV: Avrupa Kardiyoloji Dernegi’nin koroner arter hastalarinda yasam tarzi, risk faktörleri ve tedavi yaklasimi uzerine calismasi: Türkiye verileri [EUROASPIRE-IV: European Society of Cardiology study of lifestyle, risk factors, and treatment approaches in patients with coronary artery disease: Data from Turkey] Turk Kardiyol Dern Ars. 2017;45(2):134–44. doi: 10.5543/tkda.2016.82352. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Global status report on noncommunicable diseases 2014. WHO. Geneva: Switzerland, 2014. ISBN 978-924-156-485-4. Available at https://apps.who.int/iris/handle/10665/148114. Accessed on Jan 15th, 2021.
- 13.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30. doi: 10.1016/S0140-6736(16)00618-8. Erratum in: Lancet. 2017;389(10068):e2. [DOI] [PMC free article] [PubMed]
- 14.Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107–111. doi: 10.2991/jegh.k.191028.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.TurkStat Data Portal. Address Based Population Registration System, 2021. Release date Feb 4th 2022. Available at https://data.tuik.gov.tr/Bulten/Index?p=The-Results-of-Address-Based-Population-Registration-System-2021-45500&dil=2. Accessed on June 21st, 2022.
- 16.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inouue M. A New WHO Standard. GPE Discussion Paper Series: No.31, EIP/GPE/EBD., World Health Organization 2001. Available at https://www.who.int/healthinfo/paper31.pdf. Accessed on Jan 15th, 2021.
- 17.Eurostat European Commission. Revision of the European Standard Population: Report of Eurostat's task force. Eurostat methodologies and Working papers. 2013 edition. Luxembourg; 2013. ISSN 1977–0375.
- 18.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl. 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tripepi G, Jager KJ, Dekker FW, Zoccali C. Stratification for confounding–part 2: direct and indirect standardization. Nephron Clin Pract. 2010;116(4):c322–c325. doi: 10.1159/000319591. [DOI] [PubMed] [Google Scholar]
- 20.Kontsevaya A, Farrington J, Balcilar M, Ergüder T. Annex 3. Population projections: detailed methodology and results. In: Prevention and control of noncommunicable diseases in Turkey: The case for investment. World Health Organization Regional Office for Europe. WHO/EURO:2018-3291-43050-60248. Copenhagen: 2018, pp. 33–34. Available on https://apps.who.int/iris/handle/10665/345584. Accessed on June 21st, 2022.
- 21.TurkStat Data Portal. World Population Day, 2022. Available at https://data.tuik.gov.tr/Bulten/Index?p=World-Population-Day-2022-45552. Accessed on June 21st, 2022.
- 22.TurkStat Data Portal. Elderly Statistics, 2021. Available at https://data.tuik.gov.tr/Bulten/Index?p=Elderly-Statistics-2021-45636. Accessed on June 21st, 2022.
- 23.Chia CW, Egan JM, Ferrucci L. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ Res. 2018;123(7):886–904. doi: 10.1161/CIRCRESAHA.118.312806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–1029. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 25.Unal B, Ergor G, Dinc Horasan G, Kalaca S, Sozmen K. Unal B, Ergor G (Eds). Türkiye Kronik Hastaliklar ve Risk Faktorleri Sikligi Calismasi. Saglik Bakanligi, Yayin No. 909, Ankara: 2013. ISBN 978–975-590-461-0.
- 26.Uner S, Balcilar M, Erguder T, Girayalp A, Yuzuncu U, Dinc S, Sarac C, Menet G, Toker S. Report of the National Household Health Survey in Turkey: Prevalence of Noncommunicable Disease Risk Factors, 2017. World Health Organization, 2018. ISBN 978 92 890 5313 6. Available at ‘euro.who.int/en/countries/turkey/publications/national-household-health-survey-prevalence-of-noncommunicable-disease-risk-factors-in-turkey-2017–2018. Accessed on Jan 12th, 2022.
- 27.Akgun S, Pekcan G, Aksoydan E, Kiziltan G, Karaagaoglu E, Karahan S, Ogul H, Yardim N, Kocadag S, Celikay N, Aykul F, Kelat Z. Türkiye Beslenme ve Saglik Arastirmasi (TBSA). T.C. Saglik Bakanligi Halk Sagligi Genel Mudurlugu, Yayin No. 1132, Ankara: 2019. ISBN: 978–975–590–722–2.
- 28.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20(7):1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed]
- 29.Alwin Robert A, Al Dawish MA. Microvascular complications among patients with diabetes: An emerging health problem in Saudi Arabia. Diab Vasc Dis Res. 2019;16(3):227–235. doi: 10.1177/1479164118820714. [DOI] [PubMed] [Google Scholar]
- 30.Awad SF, Dargham SR, Toumi AA, Dumit EM, El-Nahas KG, Al-Hamaq AO, Critchley JA, Tuomilehto J, Al-Thani MHJ, Abu-Raddad LJ. A diabetes risk score for Qatar utilizing a novel mathematical modelling approach to identify individuals at high risk for diabetes. Sci Rep. 2021;11(1):1811. doi: 10.1038/s41598-021-81385-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haghravan S, Mohammadi-Nasrabadi F, Rafraf M. A critical review of national diabetes prevention and control programs in 12 countries in Middle East. Diabetes Metab Syndr. 2021;15(1):439–445. doi: 10.1016/j.dsx.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Touloumi G, Karakosta A, Kalpourtzi N, Gavana M, Vantarakis A, Kantzanou M, Hajichristodoulou C, Chlouverakis G, Trypsianis G, Voulgari PV, Alamanos Y, Makrilakis K, Liatis S, Chatzipanagiotou S, Stergiou G, EMENO Study Group. High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey. BMC Public Health. 2020;20(1):1665. doi: 10.1186/s12889-020-09757-4. [DOI] [PMC free article] [PubMed]
- 33.Smokovski I, Milenkovic T, Cho NH. First stratified diabetes prevalence data for Republic of Macedonia derived from the National eHealth System. Diabetes Res Clin Pract. 2018;143:179–183. doi: 10.1016/j.diabres.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 34.Borissova AM, Shinkov A, Kovatcheva R, Vlahov J, Dakovska L, Todorov T. Changes in the prevalence of diabetes mellitus in Bulgaria (2006–2012) Clin Med Insights Endocrinol Diabetes. 2015;8:41–45. doi: 10.4137/CMED.S24742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebrahimi H, Pishgar F, Yoosefi M, Moradi S, Rezaei N, Djalalinia S, Modirian M, Peykari N, Naderimagham S, Haghshenas R, Rahimi S, Jamshidi H, Esteghamati A, Larijani B, Farzadfar F. Insulin pen use and diabetes treatment goals: A study from Iran STEPS 2016 survey. PLoS ONE. 2019;14(8):e0221462. doi: 10.1371/journal.pone.0221462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ajlouni K, Batieha A, Jaddou H, Khader Y, Abdo N, El-Khateeb M, Hyassat D, Al-Louzi D. Time trends in diabetes mellitus in Jordan between 1994 and 2017. Diabet Med. 2019;36(9):1176–1182. doi: 10.1111/dme.13894. [DOI] [PubMed] [Google Scholar]
- 37.Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu M, Zhan X, Yang Z, Huang Y. Measuring the global, regional, and national burden of type 2 diabetes and the attributable risk factors in all 194 countries. J Diabetes. 2021;13(8):613–639. doi: 10.1111/1753-0407.13159. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. Diabetes country profiles: Diabetes Turkey 2016 country profile. 31 May 2016, Technical document. Available at ‘https://www.who.int/publications/m/item/diabetes-tur-country-profile-2016’. Accessed on Dec 13th, 2021.
- 40.Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R. Diabetes and global ageing among 65–99-year-old adults: Findings from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2020;162:108078. doi: 10.1016/j.diabres.2020.108078. [DOI] [PubMed]
- 41.Turkey Healthy Nutrition and Active Life Program: Prevention of Adult and Childhood Obesity and Physical Activity Action Plan 2019 – 2023. 4th ed. The Ministry of Health General Directorate of Public Health, Ankara: 2019. ISBN 978–975–590–777–2. Available at https://hsgm.saglik.gov.tr/depo/birimler/saglikli-beslenme-hareketli-hayat-db/beslenme_konsey/Eylem_Plani_.pdf. Accessed on June 18th, 2022.
- 42.Yazıcı D, Fersahoğlu MM, Fersahoğlu T, Bulut NE, Çiğiltepe H, Çeler Ö, Sancak S, Sulu C, Durcan E, Şahin S, Polat Korkmaz Ö, Bozdoğan Polat SH, Taşkın E, İşeri C, Gürsoy E, Küçük Yetgin M, Kaya T, Özdemir F, Mestanoğlu İstanbullu N, Kıyıcı S, Öztürk S, Güngör K, Can B, Sargın M, Tabak Z, Averi S, Nazlı A, Polat Y, Akbas F, Tekin S, Topaloğlu Ö, Boz Uzaldı E, Çatalçam S, Bayraktaroğlu T, Çalıkoğlu BF, Nasifova V, Soyluk Selçukbiricik Ö, Karşıdağ K, Sezer H, Özışık S, Bulut H, Bekdemir B, Deyneli O, Dinçer C, Gogas Yavuz D, İlkova H, Yumuk VD. Status of weight change, lifestyle behaviors, depression, anxiety, and diabetes mellitus in a cohort with obesity during the COVID-19 lockdown: Turk-Com Study Group. Obes Facts. 2022;15(4):528–539. doi: 10.1159/000522658. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.