Abstract
Background
Needlestick and sharps injuries (NSIs) are serious problems for dental health care workers (DHCWs) because they are at risk for occupational blood-borne infections. In this study, risk factors for NSIs in DHCWs at Tohoku University Hospital (TUH) in Japan over 19 years were analysed.
Methods
NSI data of DHCWs at TUH from April 2002 to March 2020 were collected from the Exposure Prevention Information Network (EPINet) and statistically analysed.
Results
A total of 195 NSIs occurred during the 19-year study period. Approximately 58.5% of NSIs occurred in DHCWs with less than 5 years of experience. Injection needles were the most frequent cause of NSIs (19.0%) followed by suture needles (13.3%) and ultrasonic scaler chips (12.8%). Needle injuries occurred mainly on the left hand, whereas ultrasonic scaler chip and bur injuries occurred on the right hand and other body parts whilst DHCWs were placing the instruments back on the dental unit hanging holder without removing the sharps. NSIs from other instruments primarily occurred on both hands and foot insteps during cleanup. No case of occupational blood-borne infection caused by NSIs was observed during the study period at TUH.
Conclusions
NSIs occurred in DHCWs with less experience, and there were associations between the instruments, timing of use, and NSI site. EPINet was considered a valuable tool for monitoring NSIs in order to develop future strategies for minimising NSIs.
Key words: Needlestick and sharps injuries, Dental health care workers, Blood-borne infection, EPINet, Long-term study
Introduction
Needlestick and sharps injuries (NSIs) are a major occupational risk for health care workers. The proportion of infections with hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in health care workers attributable to occupational exposure to percutaneous injuries has been reported as 39%, 37%, and 4.4%, respectively.1 Dental health care workers (DHCWs) are often exposed to the blood or body fluids of patients during dental procedures and are at risk for NSIs.2, 3, 4, 5, 6, 7 Individuals with HBV, HCV, and HIV sometimes visit dental clinics for oral care services and dental treatments without disclosing their infection status.
There are some reports on the underreporting of NSIs.8,9 The Division of Infection Control at Tohoku University Hospital (TUH) monitors NSIs using the Exposure Prevention Information Network (EPINet), which was developed by the International Healthcare Worker Safety Center at the University of Virginia in 1992.10 The objectives of this study were to analyse and investigate the risk factors related to NSIs at TUH during the past 19 academic years from 2002 to 2020.
Methods
Ethics statement
This study was approved by the Institutional Review Board (IRB) of the Tohoku University Graduate School of Dentistry (IRB approval number: 2019-3-024). All procedures in this study were performed in accordance with the ethical principles outlined in the current version of the Declaration of Helsinki.
Data collection
The Division of Infection Control at TUH required all workers to report any sharps injuries and record each case using the EPINet form. We extracted the NSI data on DHCWs from April 2002 to March 2020.
Serologic testing of DHCWs and patients
Testing for anti-HBV surface (HBs) antibody, HBs antigen (HBsAg), HBV envelope antigen, anti-HCV antibody, anti-HIV antibody, syphilis, and human T-cell leukemia virus type 1 (HTLV-1) antibody was carried out on all DHCWs who had reported sharps injuries as well as the patients who were the source of contamination. All DHCWs and patients provided informed consent for these examinations.
Statistical analysis
Fisher exact test was used to analyse differences in frequency between groups owing to the small number of particular cells observed. We compared each pair within the 3 groups and estimated P values. Each P value was then recalculated based on the Bonferroni correction for multiple comparisons. We used Stata/MP version 16.1 (StataCorp) for statistical analysis. A P value < .001 was regarded as significant.
Results
NSIs of DHCWs at TUH over 19 years
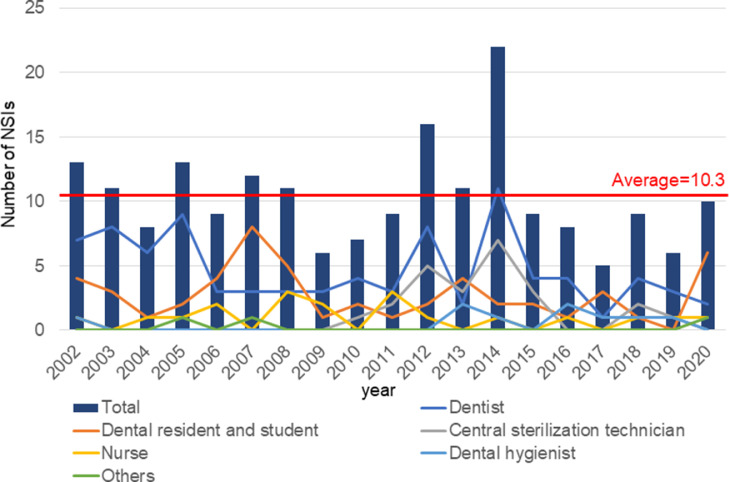
During a 19-year surveillance period at the dental division of TUH, 195 DHCWs experienced NSIs (Figure 1). The number of NSIs in each academic year ranged from 5 to 22 (average ± SD, 10.3 ± 3.9). The average number of NSIs per 100,000 patients per year was 6.77 (range, 3.83–12.18). In 2014, most NSIs at TUH were recorded by dentists and central sterilisation technicians.
Fig. 1.
Needlestick and sharps injuries (NSIs) in dental health care workers at Tohoku University Hospital (TUH) over the course of 19 years. The number of NSIs in each academic year ranged from 5 to 22 (average ± standard deviation, 10.3 ± 3.9). In 2014, most NSIs at TUH were reported by dentists and central sterilisation technicians.
Analysis of NSIs of DHCWs
Of the injured DHCWs, 45.1% were dentists and 27.6% were dental residents and students (Table 1). Dental residents at TUH are defined as those in their first year after receiving a dentist license and mainly treat patients in the Department of Comprehensive Dentistry. Dental students at TUH are engaged in some treatments and are supervised by their instructors. Most NSIs occurred in DHCWs with less than 5 years of clinical experience (n = 114, 58.4%) and at the outpatient clinic (n = 130, 66.7%). The highest number of NSIs (29.6%) occurred in the Department of Oral and Maxillofacial Surgery followed by the Department of Comprehensive Dentistry (12.3%) and the Central Sterile Room (12.3%). The NSIs most commonly involved injection needles (19.0%), followed by suture needles (13.3%) and ultrasonic scaler chips (12.8%). For 75.4% of the NSIs, the injured person was holding the device, and in approximately 20% of injuries, the device was held by someone else.
Table 1.
Analysis of NSIs from April 2002 to March 2020 (N = 195).
| n | % | Mean per year | |
|---|---|---|---|
| Occupations of DHCWs with NSIs | |||
| Dentist | 88 | 45.1 | 4.6 |
| Resident and student | 52 | 26.7 | 2.7 |
| Central supply technician | 24 | 12.3 | 1.3 |
| Nurse | 19 | 9.7 | 1.0 |
| Dental hygienist | 9 | 4.6 | 0.5 |
| Other | 3 | 1.5 | 0.2 |
| Years of experience of DHCWs with NSIs | |||
| 0–0.9 | 35 | 17.9 | 1.8 |
| 1–2.9 | 53 | 27.2 | 2.8 |
| 3–4.9 | 26 | 13.3 | 1.4 |
| 5–9.9 | 34 | 17.4 | 1.8 |
| 10–19.9 | 24 | 12.3 | 1.3 |
| 20+ | 20 | 10.3 | 1.1 |
| Unknown | 3 | 1.5 | 0.2 |
| Places where NSIs occurred | |||
| Outpatient clinic | 130 | 66.7 | 6.8 |
| Central sterile room | 24 | 12.3 | 1.3 |
| Operating room | 19 | 9.7 | 1.0 |
| Inpatient room | 13 | 6.7 | 0.7 |
| Other | 9 | 4.6 | 0.5 |
| Clinical departments where NSIs occurred | |||
| Oral and Maxillofacial Surgery | 48 | 24.6 | 2.5 |
| Comprehensive Dentistry | 24 | 12.3 | 1.3 |
| Central Sterile Room | 24 | 12.3 | 1.3 |
| Prosthodontics | 23 | 11.8 | 1.2 |
| Operative Dentistry | 14 | 7.2 | 0.7 |
| Pediatric Dentistry | 11 | 5.6 | 0.6 |
| Dentistry for the Disabled | 11 | 5.6 | 0.6 |
| Periodontology and Endodontology | 8 | 4.1 | 0.4 |
| Dental Diagnosis | 6 | 3.1 | 0.3 |
| Orthodontics | 6 | 3.1 | 0.3 |
| Preventive Dentistry | 6 | 3.1 | 0.3 |
| Other | 14 | 7.2 | 0.7 |
| Devices causing NSIs | |||
| Injection needle | 37 | 19.0 | 1.9 |
| Suture needle | 26 | 13.3 | 1.4 |
| Ultrasonic scaler chip | 25 | 12.8 | 1.3 |
| Dental tweezer | 22 | 11.3 | 1.2 |
| Bur | 20 | 10.3 | 1.1 |
| Explorer | 14 | 7.2 | 0.7 |
| Scalpel | 11 | 5.6 | 0.6 |
| Endodontic file | 6 | 3.1 | 0.3 |
| Hand scaler | 6 | 3.1 | 0.3 |
| Other needles | 6 | 3.1 | 0.3 |
| Fingernails/teeth | 6 | 3.1 | 0.3 |
| Clasp of removable denture | 2 | 1.0 | 0.1 |
| Orthodontic wire | 2 | 1.0 | 0.1 |
| Others | 8 | 4.1 | 0.4 |
| Unknown | 4 | 2.1 | 0.2 |
| Device holder when NSIs occurred | |||
| Injured person | 147 | 75.4 | 7.7 |
| Other than the injured person | 40 | 20.5 | 2.1 |
| No one | 8 | 4.1 | 0.4 |
DHCWs, dental healthcare workers; NSIs, needlestick and sharps injuries.
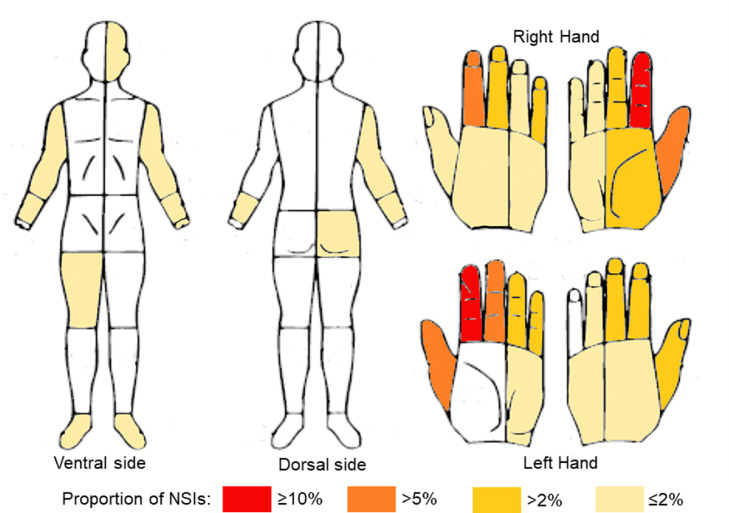
Site of NSIs of DHCWs
The majority of NSIs occurred on both hands, especially on the fingers (Figure 2). The ventral side of the left index finger was the most frequent NSI site (13.8%), followed by the ventral side of the right index finger (10.8%), ventral side of the left middle finger (7.2%), ventral side of the left thumb (6.7%), ventral side of the right thumb (6.2%), and dorsal side of the right index finger (6.2%). NSIs also occurred on other areas such as the arms, right thigh, left buttock, left side of face, and both foot insteps.
Fig. 2.
Sites map of needlestick and sharps injuries (NSIs) in dental health care workers. NSIs occurred predominantly on the hands but also on other body parts.
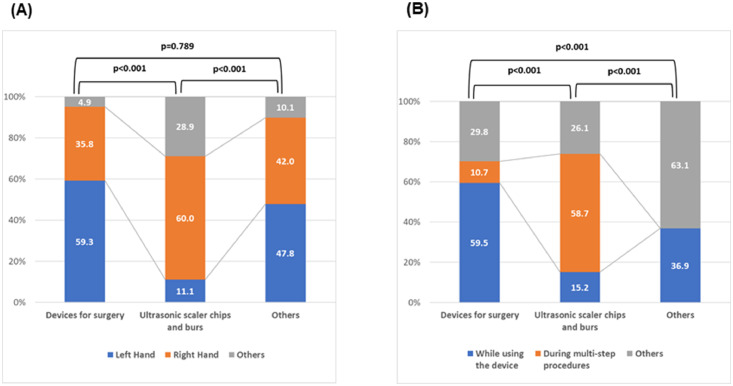
Relationship between devices and site/timing of NSIs
Regarding the relationship between devices involved in NSIs and the site/timing of NSIs, we divided the devices into 3 groups: devices for surgery, ultrasonic scaler chips and burs, and others. Devices for surgery included injection needles, suture needles, other needles, scalpels, and scissors. The site of injury was divided into 3 groups: left hand, right hand, and others. The timing was also divided into 3 groups: whilst using the device, during multistep procedures, and others. During multistep procedures refers to the time between multiple treatment steps, specifically when the device is placed on a tray or when devices such as burs and ultrasonic scaler chips attached to handpieces are placed back on the dental unit hanging holder without the sharps being removed.
Most injuries involving devices for surgery were to the left hand (59.3%), which is not the dominant hand for most Japanese people, followed by the right hand (35.8%) (Figure 3A). Injuries involving ultrasonic scaler chips and burs occurred most frequently to the right hand (60.0%), followed by other sites such as the face, arms, thigh, and buttock (28.9%). Injuries involving other devices occurred on the left (47.8%) and the right (42.0%) hands.
Fig. 3.
Relationship between devices and site/timing of needlestick and sharps injuries (n = 195). Fisher exact test was conducted to analyse the differences between each pair within the groups. Each P value was corrected based on the Bonferroni correction, and each initially estimated P value was multiplied by the number of times the test was conducted. Each P value presented in the result is after multiplying 3-fold. A, Relationship between devices and site of NSIs. B, Relationship between devices and timing of NSIs.
Concerning the timing of NSIs, injuries with surgical devices most frequently occurred whilst the DHCW was using the device (Figure 3B). NSIs involving surgical devices at other times, such as when the device is being handed over to another person or when the device is in the possession of another person, occurred more frequently than during the multistep procedures. In contrast, injuries involving ultrasonic scaler chips and burs mainly occurred during multistep procedures. NSIs involving other devices mainly occurred when the device protruded from a cage or when the instrument was dropped during treatment or cleanup.
Serologic testing
Serologic testing revealed that 22 source patients (11.3%) had positive findings for communicable diseases such as HBV, HCV, HIV, and HTLV-1 (Table 2). Approximately 65.6% of injured DHCWs were positive for anti-HBs antibody.
Table 2.
Blood-borne infection of source patient and anti-HBs antibody of injured DHCWs (N = 195).
| n | % | |
|---|---|---|
| Blood-borne infection of source patient | 22 | 11.3 |
| HBsAg | 8 | 4.1 |
| HBeAg | 0 | 0.0 |
| Anti-HCV | 11 | 5.6 |
| Anti-HIV | 1 | 0.5 |
| HTLV-1 antibody | 2 | 1.0 |
| Syphilis | 0 | 0.0 |
| Anti-HBs antibody of injured DHCWs | ||
| Yes (vaccination) | 128 | 65.6 |
| Yes (except for vaccination) | 8 | 4.1 |
| No | 47 | 24.1 |
| Unknown | 12 | 6.2 |
DHCW, dental health care worker; HBs, hepatitis B virus surface; HBsAg, hepatitis B virus surface antigen; HBeAg, hepatitis B virus envelope antigen; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HTLV-1, human T-cell leukemia virus type 1.
Discussion
NSIs of DHCWs at TUH over 19 years
The average annual number of NSIs in DHCWs in our study was similar to that reported previously at university hospitals in Japan (range, 3.6–15.9)4 but less than that in the United States (range, 7.9–37.2).8 Some studies have found that underreporting of percutaneous injuries is a significant and consistent issue.8,9,11,12 Our hospital has workers’ accident compensation insurance covering NSIs, and workers cannot apply for insurance without reporting their injury. Therefore, underreporting may not be a significant issue in our study.
The Division of Infection Control in TUH creates monthly reports on NSIs and the measures taken each time. In 2014, because most NSIs at TUH were reported by dentists and central sterilisation technicians, dentists were reminded to handle injection needles using the one-hand scoop technique. After that, there were no NSIs when injection needles were recapped. Instead, NSIs involving injection needles still occurred during treatment and disassembly. It was also found that many central sterilisation technicians were injured with dental tweezers because discarded tweezers in cleaning baskets would stick out of the coarse mesh of the cleaning basket. After changing to a finer basket mesh, the number of NSIs decreased in this group. However, despite the various measures taken, NSIs still occur, and it has been necessary to continue taking measures to prevent them.
Analysis of NSIs of DHCWs
Most NSIs occurred in DHCWs with less than 5 years of clinical experience. Education on NSIs is essential in a university hospital, and students must receive clinical training to prevent NSIs.8,9,13,14 In non-hospital settings, most NSIs involve dental assistants, and the importance of education for dental assistants has been similarly pointed out.15,16 Of the 195 DHCWs who experienced NSIs, 73 were men and 122 were women. However, because all central supply technicians, dental nurses, and dental hygienists were women, we thought that specifying the sex of our subjects was not relevant.
Most NSIs occurred in the Department of Oral and Maxillofacial Surgery, most commonly involving injection needles. This result is characteristic of a university hospital, as noted in previous studies.2, 3, 4,8 In contrast, most NSIs involving dental burs occur in non-hospital settings.16 Differences in NSI characteristics between university hospitals and non-hospital clinics should be considered.
The NSIs in 75.4% of our participants occurred when the injured person was holding the device, but in approximately 20% of NSIs, the device was held by someone else. Countermeasures against the latter involve strengthening communication between staff members and setting up a neutral zone.
Site map of NSIs
The site map of NSIs of DHCWs showed that the majority of NSIs occurred on both hands, especially on the fingers (Figure 2). The ventral side of the left index finger was the most frequent NSI site, as was also reported in a previous study in Japan.2 NSIs also occurred on other body parts. The arms, right thigh, left buttock, and left side of the face were mainly injured during multistep procedures, for example, when the device was placed on the tray or when devices such as burs and ultrasonic scaler chips attached to the handpieces were placed back on the dental unit hanging holder without the sharps being removed. Bilateral foot insteps were also injured when instruments were dropped during treatment or cleanup.
Relationship between devices and site/timing of NSIs
To analyse the relationship between devices involved in NSIs and the site/timing of NSIs, each category of devices, site, and timing of NSIs was divided into 3 groups. NSIs involving devices for surgery mainly occurred on the left hand, which is not the dominant hand for most Japanese people (Figure 3A). Injuries to the right hand more frequently involved ultrasonic scaler chips and burs because most Japanese people are right-handed and DHCWs were injured whilst trying to get other instruments over the chips and burs during multistep procedures. Other body parts such as the face, arms, thigh, and buttock were also injured with ultrasonic scaler chips and burs placed on the hanging holder of the dental unit when DHCWs moved near the sharps without realising this.
Concerning the timing of NSIs, injuries with surgical devices most frequently occurred whilst the DHCW was using the device (Figure 3B). NSIs involving surgical devices at other times such as whilst handing over the device or whilst the device was in the possession of another person were more frequent than during the multistep procedures. In contrast, injuries involving ultrasonic scaler chips and burs mainly occurred during multistep procedures. A previous study found that most percutaneous injuries involved dental burs attached to a handpiece that were placed on a dental unit by the operator, sometimes resulting in a puncture injury to the operator or the assistants.16 We recommend the immediate cleanup of used ultrasonic scaler chips and burs. Dukka et al8 introduced additional protective measures to cover burs in handpieces and scaler tips with either a plastic cup or a cotton roll. Multifaceted measures are needed.
NSIs with other devices mainly resulted from the device protruding from the cage during cleanup or instruments being dropped during treatment or cleanup. Bilateral foot insteps were also injured by instruments being dropped during treatment or cleanups. As a countermeasure, we instructed DHCWs to wear footwear that covered the instep, and improvement was observed. We should pay attention to when specific injuries tend to occur with certain instruments during certain procedures.
Serologic testing
Some studies have reported that NSIs and occupational exposure to infections, including HIV, HBV, and HCV, are a constant threat in dental practice.17,18 TUH recommends HBV vaccination for all health care workers. In this study, approximately two-thirds of DHCWs with NSIs had anti-HB antibody positivity. Some individuals did not show an increase in their antibody titers even after vaccination. When a DHCW has an NSI, the Division of Infection Control at TUH provides immediate advice on countermeasures according to their serologic results (Table 2). If a DHCW was anti-HB antibody negative with an NSI from an HBsAg-positive patient, the DHCW is vaccinated against HBs. If an NSI occurs with an HIV-positive patient, the DHCW must decide whether to take prophylactic anti-HIV medication immediately at their discretion. Blood samples of DHCWs who might have been exposed to a blood infection are tested at 1, 3, and 6 months after the initial injury. In the 19-year survey, 22 patients (11.3%) were serologically positive for HBsAg, HCV, HIV, or HTLV-1, but there were no cases of blood-borne infection. These measures by the Division of Infection Control were considered very effective during these periods.
In this study, we analysed 19 years of EPINet data to clarify the relationship between dental devices and site/timing of NSIs in DHCWs. EPINet is a valuable tool for monitoring NSIs in order to develop a strategy for minimising NSIs.19, 20, 21 It is very important to analyse NSIs using EPINet, take immediate measures to prevent NSIs, and continuously remind DHCWs about the need to prevent NSIs.
Acknowledgments
Acknowledgements
The authors wish to thank the staff members of the Division of Infection Control at TUH, who provided special care for DHCWs with NSIs.
Conflict of interest
None disclosed.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.identj.2022.04.009.
Appendix. Supplementary materials
REFERENCES
- 1.Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48(6):482–490. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto H, Sunakawa M, Suda H, Izumi Y. Analysis of factors related to needle-stick and sharps injuries at a dental specialty university hospital and possible prevention methods. J Oral Sci. 2019;61(1):164–170. doi: 10.2334/josnusd.18-0127. [DOI] [PubMed] [Google Scholar]
- 3.Lee JJ, Kok SH, Cheng SJ, Lin LD, Lin CP. Needlestick and sharps injuries among dental healthcare workers at a university hospital. J Formos Med Assoc. 2014;113(4):227–233. doi: 10.1016/j.jfma.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Morinaga K, Hagita K, Yakushiji T, Ohata H, Sueishi K, Inoue T. Analysis of needlestick and similar injuries over 10 years from April 2004 at Tokyo Dental College Chiba Hospital. Bull Tokyo Dent Coll. 2016;57(4):299–305. doi: 10.2209/tdcpublication.2015-0036. [DOI] [PubMed] [Google Scholar]
- 5.Zachar JJ, Reher P. Percutaneous exposure injuries amongst dental staff and students at a university dental clinic in Australia: a 6-year retrospective study. Eur J Dent Educ. 2022;26(2):288–295. doi: 10.1111/eje.12701. [DOI] [PubMed] [Google Scholar]
- 6.Pavithran VK, Murali R, Krishna M, Shamala A, Yalamalli M, Kumar AV. Knowledge, attitude, and practice of needle stick and sharps injuries among dental professionals of Bangalore. India. J Int Soc Prev Community Dent. 2015;5(5):406–412. doi: 10.4103/2231-0762.165932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Ali K, Hashim R. Occupational health problems of dentists in the United Arab Emirates. Int Dent J. 2012;62(1):52–56. doi: 10.1111/j.1875-595X.2011.00091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dukka H, Byrd P, Qian C, Baughman G, Butt S, Rai SN. Occupational percutaneous injuries and exposures in a dental teaching environment: a 10-year report. J Dent Educ. 2021;85(11):1729–1738. doi: 10.1002/jdd.12731. [DOI] [PubMed] [Google Scholar]
- 9.Pervaiz M, Gilbert R, Ali N. The prevalence and underreporting of needlestick injuries among dental healthcare workers in Pakistan: a systematic review. Int J Dent. 2018;2018 doi: 10.1155/2018/9609038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.EPINet: a computerized blood and body fluid exposure reporting system from Dr. Janine Jagger. Healthc Hazard Mater Manage. 1992;5(11):5–8. [PubMed] [Google Scholar]
- 11.Tada A, Watanabe M, Senpuku H. Factors affecting changes in compliance with infection control practices by dentists in Japan. Am J Infect Control. 2015;43(1):95–97. doi: 10.1016/j.ajic.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 12.Westall JO, Dickinson C. Compliance with occupational exposure risk management procedures in a dental school setting. Br Dent J. 2017;222(11):859–863. doi: 10.1038/sj.bdj.2017.498. [DOI] [PubMed] [Google Scholar]
- 13.AlDakhil L, Yenugadhati N, Al-Seraihi O, Al-Zoughool M. Prevalence and associated factors for needlestick and sharp injuries (NSIs) among dental assistants in Jeddah, Saudi Arabia. Environ Health Prev. 2019;24:60. doi: 10.1186/s12199-019-0815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. National Surveillance System for Health Care Workers Group. Preventing percutaneous injuries among dental health care personnel. J Am Dent Assoc. 2007;138:169–178. doi: 10.14219/jada.archive.2007.0133. quiz 247–8. [DOI] [PubMed] [Google Scholar]
- 15.Shah SM, Merchant AT, Dosman JA. Percutaneous injuries among dental professionals in Washington State. BMC Public Health. 2006;6:269. doi: 10.1186/1471-2458-6-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira MC, Mello FW, Ribeiro DM, et al. Prevalence of reported percutaneous injuries on dentists: a meta-analysis. J Dent. 2018;76:9–18. doi: 10.1016/j.jdent.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Samaranayake L, Scully C. Needlestick and occupational exposure to infections: a compendium of current guidelines. Br Dent J. 2013;215(4):163–166. doi: 10.1038/sj.bdj.2013.791. [DOI] [PubMed] [Google Scholar]
- 18.Smith AJ, Cameron SO, Bagg J, Kennedy D. Management of needlestick injuries in general dental practice. Br Dent J. 2001;190(12):645–650. doi: 10.1038/sj.bdj.4801064. [DOI] [PubMed] [Google Scholar]
- 19.Yoshikawa T, Wada K, Lee JJ, et al. Incidence rate of needlestick and sharps injuries in 67 Japanese hospitals: a national surveillance study. PLoS One. 2013;8(10):e77524. doi: 10.1371/journal.pone.0077524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watterson L. Monitoring sharps injuries: EPINet surveillance results. Nurs Stand. 2004;19(3):33–38. doi: 10.7748/ns2004.09.19.3.33.c3701. [DOI] [PubMed] [Google Scholar]
- 21.Nagao Y, Baba H, Torii K, et al. A long-term study of sharps injuries among health care workers in Japan. Am J Infect Control. 2007;35(6):407–411. doi: 10.1016/j.ajic.2006.03.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.