Abstract
Background
Kawasaki disease (KD) is an acute systemic vasculitis (inflammation of the blood vessels) that mainly affects children. Symptoms include fever, chapped lips, strawberry tongue, red eyes (bulbar conjunctival injection), rash, redness, swollen hands and feet or skin peeling; and enlarged cervical lymph nodes. High fevers and systemic inflammation characterise the acute phase. Inflammation of the coronary arteries causes the most serious complication of the disease, coronary artery abnormalities (CAAs). The primary treatment is intravenous immunoglobulin (IVIG) and acetylsalicylic acid (ASA/aspirin), with doses and regimens differing between institutions. It is important to know which regimens are the safest and most effective in preventing complications.
Objectives
To evaluate the efficacy and safety of IVIG in treating and preventing cardiac consequences of Kawasaki disease.
Search methods
The Cochrane Vascular Information Specialist searched the Cochrane Vascular Specialised Register, CENTRAL, MEDLINE, Embase, and CINAHL databases, and the World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov trials registers to 26 April 2022.
Selection criteria
We included randomised controlled trials (RCTs) investigating the use of IVIG for the treatment of KD. We included studies involving treatment for initial or refractory KD, or both.
Data collection and analysis
We used standard Cochrane methods. Our primary outcomes were incidence of CAAs and incidence of any adverse effects after treatment. Our secondary outcomes were acute coronary syndromes, duration of fever, need for additional treatment, length of hospital stay, and mortality. We used GRADE to assess the certainty of the evidence for each outcome.
Main results
We identified 31 RCTs involving a total of 4609 participants with KD. Studies compared IVIG with ASA, another dose or regimen of IVIG, prednisolone, or infliximab. The majority of studies reported on primary treatment, so those results are reported below. A limited number of studies investigated secondary or tertiary treatment in IVIG‐resistant patients. Doses and regimens of IVIG infusion varied between studies, and all studies had some concerns related to risk of bias.
Primary treatment with IVIG compared to ASA for people with KD
Compared to ASA treatment, IVIG probably reduces the incidence of CAAs in people with KD up to 30 days (odds ratio (OR) 0.60, 95% confidence interval (CI) 0.41 to 0.87; 11 studies, 1437 participants; moderate‐certainty evidence). The individual studies reported a range of adverse effects, but there was little to no difference in numbers of adverse effects between treatment groups (OR 0.57, 95% CI 0.17 to 1.89; 10 studies, 1376 participants; very low‐certainty evidence). There was limited evidence for the incidence of acute coronary syndromes, so we are uncertain of any effects. Duration of fever days from treatment onset was probably shorter in the IVIG group (mean difference (MD) −4.00 days, 95% CI −5.06 to −2.93; 3 studies, 307 participants; moderate‐certainty evidence). There was little or no difference between groups in need for additional treatment (OR 0.27, 95% CI 0.05 to 1.57; 3 studies, 272 participants; low‐certainty evidence). No study reported length of hospital stay, and no deaths were reported in either group.
Primary treatment with IVIG compared to different infusion regimens of IVIG for people with KD
Higher‐dose regimens of IVIG probably reduce the incidence of CAAs compared to medium‐ or lower‐dose regimens of IVIG up to 30 days (OR 0.60, 95% CI 0.40 to 0.89; 8 studies, 1824 participants; moderate‐certainty evidence). There was little to no difference in the number of adverse effects between groups (OR 1.11, 95% CI 0.52 to 2.37; 6 studies, 1659 participants; low‐certainty evidence). No study reported on acute coronary syndromes. Higher‐dose IVIG may reduce the duration of fever compared to medium‐ or lower‐dose regimens (MD −0.71 days, 95% CI −1.36 to −0.06; 4 studies, 992 participants; low‐certainty evidence). Higher‐dose regimens may reduce the need for additional treatment (OR 0.29, 95% CI 0.10 to 0.88; 4 studies, 1125 participants; low‐certainty evidence). We did not detect a clear difference in length of hospital stay between infusion regimens (MD −0.24, 95% CI −0.78 to 0.30; 3 studies, 752 participants; low‐certainty evidence). One study reported mortality, and there was little to no difference detected between regimens (moderate‐certainty evidence).
Primary treatment with IVIG compared to prednisolone for people with KD
The evidence comparing IVIG with prednisolone on incidence of CAA is very uncertain (OR 0.60, 95% CI 0.24 to 1.48; 2 studies, 140 participants; very low‐certainty evidence), and there was little to no difference between groups in adverse effects (OR 4.18, 95% CI 0.19 to 89.48; 1 study; 90 participants; low‐certainty evidence). We are very uncertain of the impact on duration of fever, as two studies reported this outcome differently and showed conflicting results. One study reported on acute coronary syndromes and mortality, finding little or no difference between groups (low‐certainty evidence). No study reported the need for additional treatment or length of hospital stay.
Authors' conclusions
The included RCTs investigated a variety of comparisons, and the small number of events observed during the study periods limited detection of effects. The certainty of the evidence ranged from moderate to very low due to concerns related to risk of bias, imprecision, and inconsistency. The available evidence indicated that high‐dose IVIG regimens are probably associated with a reduced risk of CAA formation compared to ASA or medium‐ or low‐dose IVIG regimens. There were no clinically significant differences in incidence of adverse effects, which suggests there is little concern about the safety of IVIG. Compared to ASA, high‐dose IVIG probably reduced the duration of fever, but there was little or no difference detected in the need for additional treatment. Compared to medium‐ or low‐dose IVIG, there may be reduced duration of fever and reduced need for additional treatment. We were unable to draw any conclusions regarding acute coronary syndromes, mortality, or length of hospital stay, or for the comparison IVIG versus prednisolone. Our findings are in keeping with current guideline recommendations and evidence from long‐term epidemiology studies.
Keywords: Child; Humans; Acute Coronary Syndrome; Aspirin; Aspirin/adverse effects; Fever; Fever/drug therapy; Fever/etiology; Immunoglobulins, Intravenous; Immunoglobulins, Intravenous/adverse effects; Inflammation; Mucocutaneous Lymph Node Syndrome; Mucocutaneous Lymph Node Syndrome/drug therapy; Prednisolone; Prednisolone/therapeutic use
Plain language summary
Immunoglobulin treatment for Kawasaki disease
Key message
In children with Kawasaki disease, high‐dose intravenous immunoglobulin (IVIG) regimens: • probably reduce the risk of coronary artery abnormalities formation compared to aspirin or medium‐ or low‐dose IVIG regimens; • show no clear safety concerns; • probably reduce the duration of fever, but there was little or no difference detected in the need for additional treatment compared to aspirin; • may reduce the duration of fever and need for additional treatment compared to medium‐ or low‐dose IVIG.
Why is this question important?
Kawasaki disease is a condition that causes blood vessels to become swollen and inflamed. Symptoms include high temperature (fever) along with chapped lips, strawberry tongue (swollen, bumpy red tongue), red eyes, a rash, redness and swelling of hands and feet or skin peeling; and swollen glands in the neck. It is most often seen in young children. Swelling and inflammation of the vessels which supply blood to the heart (coronary arteries) is the most serious complication of the disease, causing coronary artery abnormalities. These abnormalities can result in acquired heart disease and sometimes death. Fast diagnosis and treatment can prevent these complications. Intravenous immunoglobulin and aspirin are the main medicines used to treat Kawasaki disease. Different combinations, doses, or timings (regimens) of these medicines are used to treat patients. It is important to know which treatments and regimens are the safest and most effective in preventing heart complications.
What did we do?
We searched for randomised controlled trials (a type of study where participants are randomly assigned to one of two or more treatment groups) that compared treatment of Kawasaki disease with IVIG to treatment with another medicine or regimen. We found 31 studies with a total of 4609 participants. The studies compared IVIG with aspirin, another regimen of IVIG, infliximab, or prednisolone. All studies reported on coronary artery abnormalities, but they did not all report on our other outcomes of interest: adverse effects, acute coronary syndromes (such as a heart attack), duration of fever, need for additional treatment, length of hospital stay, and mortality. Where appropriate, we combined data from the included studies.
What did we find?
We looked at studies that compared IVIG with aspirin. Our results showed that children who received IVIG probably developed fewer coronary artery abnormalities than children treated with aspirin alone. Reporting of adverse effects varied between studies, but there was little or no difference in the number of adverse effects between groups. Acute coronary syndromes were poorly reported, so we cannot say if IVIG affected this. IVIG treatment probably reduced the duration of fever compared to aspirin alone. There was little or no difference in the need for additional treatment between IVIG and aspirin groups, and no study reported on the length of hospital stay. No deaths were reported in either group.
We looked at studies that compared high‐dose IVIG regimens with medium‐ or low‐dose regimens. Our results showed that children who received high‐dose regimens probably developed fewer abnormalities. There was no apparent difference in the number of adverse effects between the high and medium‐ or low‐dose groups. Acute coronary syndromes were poorly reported, with little or no difference seen between groups. Higher‐dose regimens may reduce the duration of fever and need for additional treatment compared to medium‐ and lower‐dose regimens. We did not find a clear difference between regimens in length of hospital stay. One death was reported in one study, so we cannot say for sure if one regimen was better than another for this outcome.
We also looked at studies that compared IVIG with prednisolone. The evidence was very uncertain for number of coronary artery abnormalities and duration of fever, and there was little or no difference between groups in adverse effects, acute coronary syndromes, and deaths. Results for all outcomes were limited by the small number of children with Kawasaki disease involved. No study reported on need for additional treatment or length of hospital stay.
What are the limitations of the evidence?
Our confidence in the evidence provided from the included studies differed between outcomes and ranged from very low to moderate, due to concerns about how some of the studies were carried out, differences in the regimens used, and there were often only small numbers of events and participants providing data. Our findings are in keeping with current guideline recommendations and evidence from long‐term studies involving large numbers of people.
How up‐to‐date is this evidence?
The evidence is current to April 2022.
Summary of findings
Summary of findings 1. Primary treatment with intravenous immunoglobulin (IVIG) compared to acetylsalicylic acid (ASA) for people with Kawasaki disease.
| Intravenous immunoglobulin (IVIG) versus acetylsalicylic acid (ASA) for the primary treatment of Kawasaki disease | ||||||
|
Patient or population: people undergoing initial treatment for KD Settings: hospital Intervention: IVIGa Comparison: ASAb | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with ASA | Risk with IVIG | |||||
|
Incidence of CAAs (up to 30 days) |
Study population | OR 0.60 (0.41 to 0.87) | 1437 (11 RCTs) |
⊕⊕⊕⊝ Moderatec | It is likely that the incidence of CAA was reduced in the IVIG group compared to the ASA group. | |
| 295 per 1000 | 201 per 1000 (147 to 267) | |||||
|
Incidence of any adverse effects after treatment initiation (from 30 days to 30 months) |
Study population | OR 0.57 (0.17 to 1.89) | 1376 (10 RCTs) |
⊕⊝⊝⊝ Very lowd | There was little or no difference in the numbers of adverse effects detected. See Table 2 for adverse effects reported by study. | |
| 67 per 1000 | 39 per 1000 (12 to 120) | |||||
|
Acute coronary syndrome (such as MI or coronary thrombus) (to 30 months) |
Study population | ‐ | 202 (2 RCTs) |
⊕⊕⊝⊝ Lowe | Newburger 1986 reported acute coronary syndromes: 30 months 2/17 participants in the ASA group had coronary thrombus compared to 0/7 in the IVIG group. Matsushima 1985 confirmed no acute coronary events occurred. | |
| See comment | ‐ | |||||
|
Duration of fever (days) (acute phase) |
The mean duration of fever from treatment onset across ASA group ranged from 6 to 7.9 days. | The mean duration of fever from treatment onset in the IVIG group was 4 days lower (5.06 lower to 2.93 lower). | ‐ | 307 (3 RCTs) |
⊕⊕⊕⊝ Moderatef | It is likely that duration of fever was reduced in the IVIG group compared to the ASA group. |
|
Need for additional treatment (up to 30 or 60 days) |
Study population | OR 0.27 (0.05 to 1.57) | 272 (3 RCTs) |
⊕⊕⊝⊝ Lowg | There was little or no difference in the need for additional treatment between groups. | |
| 36 per 1000 |
10 per 1000 (2 to 55) |
|||||
| Length of hospital stay (days) | See comment | ‐ | ‐ | ‐ | ‐ | None of the studies comparing IVIG with ASA reported on length of hospital stay. |
| Mortality (all‐cause) | Study population | ‐ | ‐ | ⊕⊕⊝⊝ Lowe | Details on the incidence of mortality were reported by 2 studies, with no deaths occurring in either study. | |
| See comment | ‐ | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ASA: acetylsalicylic acid; CAA: coronary artery abnormality; CI: confidence interval; IVIG: intravenous immunoglobulin; KD: Kawasaki disease; MI: myocardial infarction; OR: odds ratio; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aIVIG total dose ranged from 100 mg/kg to 2 g/kg, via either single infusion or multiple infusions over three to five days. See Characteristics of included studies tables for specific details. All studies administered ASA to both arms, except for Furusho 1991B, where one of two IVIG study arms did not receive ASA. bMost studies administered ASA initially at 30 mg/kg/day, except for Newburger 1986, who used 100 mg/kg/day every 6 hours to day 14 of illness, and Okuni 1987A, Okuni 1987B, and Onouchi 1988, who used 50 mg/kg/day. cWe downgraded by one level due to concerns related to risk of bias. dWe downgraded by one level due to concerns related to risk of bias, one level for inconsistency (I2 = 73%), and one level for imprecision (small number of events, and confidence intervals include appreciable benefit or harm). eWe downgraded by one level due to concerns related to risk of bias and one level for imprecision (small numbers of participants and events). fWe downgraded by a total of one level due to concerns related to risk of bias and imprecision (small number of participants). gWe downgraded by one level due to concerns related to risk of bias and one level for imprecision (small numbers of participants and events, and confidence intervals include appreciable benefit or harm).
1. Adverse events ‐ primary treatment with IVIG versus ASA.
| Study | IVIGa | ASAa | Comments |
| Furusho 1984 | 1/46 chills and fever | 1/47 liver disorder | IVIG discontinued, and ASA changed to IVIG. |
| Furusho 1991B | Reports no SAE, AE not detailed | ||
| Matsushima 1985 | 1/17 pericardial effusion | 5/15 pericardial effusion | |
| Nagashima 1987 | 8/69 chills and fever 1/69 urticaria |
0/67 | In all cases, symptoms were transient and disappeared in a short time. |
| Newburger 1986 | 0 SAE 3/84 mild congestive heart failure 1/84 shaking/itching 1/84 sepsis 1/84 rash, fever, lymphadenopathy and splenomegaly 1/84 neutropenia and splenomegaly |
4/84 mild congestive heart failure 1/84 neutropenia |
|
| Ogawa 1987 | 21/63 liver disorder | 6/54 liver disorder | |
| Ogino 1987 | 0/50 | 6/42 liver disorder | |
| Okuni 1987A | 0/139 | 0/75 | |
| Okuni 1987B | 0/196 | 0/99 | |
| Onouchi 1988 | 1/97 erythema (200 mg/kg arm) | 8/48 liver disorder 1/48 nasal haemorrhage |
|
| Yabiku 1989 | 4/48 liver disorder | 6/36 liver disorder |
AE: adverse event ASA: acetylsalicylic acid IVIG: intravenous immunoglobulin SAE: serious adverse event aSee Characteristics of included studies tables for doses given.
Summary of findings 2. Primary treatment with intravenous immunoglobulin (IVIG) compared to different infusion regimens of IVIG for people with Kawasaki disease.
| High‐dose versus medium‐ or low‐dose intravenous immunoglobulin infusion (IVIG) regimens for the primary treatment of Kawasaki disease | ||||||
|
Patient or population: people undergoing initial treatment for KD Settings: hospital Intervention: IVIG high‐dose regimensa Comparison: IVIG medium‐ or low‐dose regimensb | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with medium‐ or low‐dose IVIG | Risk with high‐dose IVIG | |||||
|
Incidence of CAAs (up to 30 days) |
Study population | OR 0.60 (0.40 to 0.89) | 1824 (8 RCTs) |
⊕⊕⊕⊝ Moderatec | It is likely that the incidence of CAAs is reduced in the high‐dose infusion regimens compared to the medium‐ or low‐dose regimens. | |
| 204 per 1000 | 133 per 1000 (93 to 186) | |||||
|
Incidence of any adverse effects after treatment initiation (follow‐up ranged from 30 days to 5 years) |
Study population | OR 1.11 (0.52 to 2.37) | 1659 (6 RCTs) |
⊕⊕⊝⊝ Lowd | There was little or no difference in the number of adverse effects detected. See Table 4 for adverse effects reported by study. | |
| 19 per 1000 | 21 per 1000 (10 to 44) | |||||
|
Acute coronary syndrome (such as MI or coronary thrombus) (up to 7 weeks) |
Study population | ‐ | ‐ | ‐ | No studies reported this outcome. | |
| See comment | ‐ | |||||
|
Duration of fever (days) (acute phase) |
The mean duration of fever in the medium‐ or low‐dose infusion regimens ranged from 5 days to 10.3 days. | The mean duration of fever was 0.71 days lower (1.36 lower to 0.06 lower) in the high‐dose infusion regimens. | ‐ | 992 (4 RCTs) |
⊕⊕⊝⊝ Lowe |
Duration of fever may be slightly reduced in the high‐dose regimens compared to the medium‐ or low‐dose regimens. |
|
Need for additional treatment (up to 6 months) |
Study population | OR 0.29 (0.10 to 0.88) | 1125 (4 RCTs) |
⊕⊕⊝⊝ Lowf | Need for additional treatment may be slightly reduced in the high‐dose regimens compared to the medium‐ or low‐dose regimens. | |
| 116 per 1000 | 37 per 1000 (13 to 103) | |||||
|
Length of hospital stay (days) (up to 28 days) |
The mean length of hospital stay (days) ranged from 8.3 days to 18.95 days across medium‐ and low‐dose infusion regimens. | The mean length of hospital stay was 0.24 days lower (0.78 lower to 0.3 higher) in the high‐dose infusion regimens. | ‐ | 752 (3 RCTs) |
⊕⊕⊝⊝ Lowg | There was little to no difference detected in the length of hospital stay between regimens. |
|
Mortality (all‐cause) (up to 7 weeks) |
Study population | ‐ | 549 (1 RCT) |
⊕⊕⊕⊝ Moderateh | Newburger 1991 reported 1 death in the subacute phase of the 400 mg/kg/day for 4 days group. The cause of death was a giant aneurysm. The remaining studies did not report mortalities. | |
| See comment | ‐ | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAA: coronary artery abnormality; CI: confidence interval; IVIG: intravenous immunoglobulin; KD: Kawasaki disease; MI: myocardial infarction; OR: odds ratio; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe included studies that compared different doses or infusion regimens of IVIG for the primary treatment of KD. We defined high dose as single‐ or multiple‐infusion regimens of over 1600 mg/kg total IVIG. bWe defined medium dose to be single‐ or multiple‐infusion regimens of 1600 mg/kg to 1000 mg/kg total IVIG, and low dose to be single‐ or multiple‐infusion regimens of less than 1000 mg/kg total IVIG. cWe downgraded by one level due to concerns related to risk of bias. dWe downgraded by one level due to concerns related to risk of bias and one level for imprecision (small numbers of events, and confidence intervals include appreciable benefit or harm). eWe downgraded by one level due to concerns related to risk of bias and one level for inconsistency (I2 = 71%). fWe downgraded by one level due to concerns related to risk of bias and one level for inconsistency (I2 = 69%). gWe downgraded by a total of two levels due to concerns related to risk of bias and imprecision (confidence intervals include appreciable benefit or harm). hWe downgraded by one level for imprecision (small number of events reported).
2. Adverse events ‐ primary treatment with IVIG versus IVIG.
| Study | IVIG | IVIG | IVIG | Comments |
| Barron 1990 | 10/22 1 g/kg single 4 mild flushing, chills, and nausea and vomiting, mild hypotension, morbilliform rash 6/22 pericardial effusion |
6/22 400 mg/kg/day for 4 days 3 shaking chills, chills and noisy breathing, headache, flushing, and abdominal cramping 3/22 pericardial effusion |
‐ | Numbers of participants with pericardial effusion added separately to other AE, as it is not clear from text if these were different participants to those reporting other AE. |
| Furusho 1991A | 0/41 100 mg/kg/day for 5 days |
0/51 200 mg/kg/day for 5 days |
0/53 400 mg/kg/day for 5 days |
No serious AE were detected. Unclear if this means no AE or not reported |
| Harada 1989 | 2/125 100 mg/kg/day for 5 days rash, mild hypotension |
1/117 400 mg/kg/day for 5 days anaphylactic shock |
‐ | |
| He 2021 | 1/129 1 g/kg/day for 2 days chickenpox |
0/132 2 g/kg single |
0/138 1 g/kg single |
1/129 recovered without complications. |
| Morikawa 1994 | 13/310 200 mg/kg/day for 5 days |
7/156 400 mg/kg/day for 5 days |
‐ | All reported AE were mild to moderate and included fever, rash, shivering, peripheral cyanosis, hepatic dysfunction. |
| Newburger 1991 | 9/273 2 g/kg single 6/273 new or worsening congestive heart failure 1/273 infusion was SC not IV – oedema and blistering 1/273 generalised oedema 1/273 nasal congestion, cough, nausea |
6/276 400 mg/kg/day for 4 days 3/276 new or worsening congestive heart failure 2/276 had pruritis 1/276 had generalised oedema |
‐ | |
| Nishihara 1988 | ‐ | ‐ | ‐ | Did not report |
| Onouchi 1988 | 1/49 200 mg/kg/day for 3 days erythema |
0/48 400 mg/kg/day for 3 days |
‐ | |
| Onouchi 1992 | 0/57 100 mg/kg/day for 5 days |
0/52 200 mg/kg/day for 5 days |
1/56 400 mg/kg/day for 5 days nausea |
|
| Qin 2006 | 2/122 2 g/kg single 2 cases of rash, nausea, and abdominal pain |
2/120 1 g/kg single 2 cases of rash, nausea, and abdominal pain |
‐ | Related to an allergic reaction to IVIG |
| Sakata 2007 | ‐ | ‐ | ‐ | Did not report |
| Sato 1995 | 0/72 2 g/kg single |
0/73 400 mg/kg/day for 5 days |
‐ | Reported that there were no AE to IVIG treatment in either group |
AE: adverse effects IV: intravenous IVIG: intravenous immunoglobulin SC: subcutaneous
Summary of findings 3. Primary treatment with intravenous immunoglobulin (IVIG) compared to prednisolone for people with Kawasaki disease.
| Intravenous immunoglobulin (IVIG) versus prednisolone for the primary treatment of Kawasaki disease | ||||||
|
Patient or population: people undergoing initial treatment for KD Settings: hospital Intervention: IVIGa Comparison: prednisoloneb | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with prednisolone | Risk with IVIG | |||||
|
Incidence of CAAs (acute phase) |
Study population | OR 0.60 (0.24 to 1.48) | 140 (2 RCTs) |
⊕⊝⊝⊝ Very lowc | The evidence is very uncertain. | |
| 200 per 1000 | 130 per 1000 (57 to 270) | |||||
|
Incidence of any adverse effects after treatment initiation (up to 3 months) |
Study population | OR 4.18 (0.19 to 89.48) | 90 (1 RCT) |
⊕⊕⊝⊝ Lowd | There is little to no difference in the incidence of adverse effects. | |
| 0/40 in prednisolone group | Not estimable | |||||
|
Acute coronary syndrome (such as MI or coronary thrombus) (up to 3 months) |
Study population | ‐ | 90 (1 RCT) |
⊕⊕⊝⊝ Lowe | Nonaka 1995 reported an MI in the IVIG group (1/50 vs 0/40 in the prednisolone group). | |
| See comment | ‐ | |||||
| Duration of fever (days) | See comment | ‐ | ‐ | 140 (2 RCTs) |
⊕⊝⊝⊝ Very lowf | We did not pool, as considerable heterogeneity was detected. |
| Need for additional treatment | Study population | ‐ | ‐ | ‐ | Neither study comparing IVIG with prednisolone reported on the need for additional treatment. | |
| See comment | ‐ | |||||
| Length of hospital stay (days) | See comment | ‐ | ‐ | ‐ | ‐ | Neither study comparing IVIG with prednisolone reported on length of hospital stay. |
|
Mortality (all‐cause) (up to 30 days) |
Study population | ‐ | 90 (1 RCT) |
⊕⊕⊝⊝ Lowe | Nonaka 1995 reported 1/50 deaths in the IVIG group compared to 0/40 in the prednisolone group. Cause of death was a giant aneurysm, intracranial bleeding, and MI. | |
| See comment | ‐ | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAA: coronary artery abnormality; CI: confidence interval; IVIG: intravenous immunoglobulin; KD: Kawasaki disease; MI: myocardial infarction; OR: odds ratio; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aIVIG dose was 400 mg/kg/day IVIG for 3 days, Nonaka 1995, and 1 g/kg/day IVIG for 2 days, Yuan 2000. See Characteristics of included studies tables for specific details. bPrednisolone dose was 2 mg/kg/day for 5 days, Nonaka 1995, or 2 mg/kg/day intravenous methylprednisolone for 5 days, Yuan 2000, then oral prednisolone until C‐reactive protein‐negative. This group did not receive IVIG. cWe downgraded by two levels due to concerns related to risk of bias and one level for imprecision (small numbers of events and participants). dWe downgraded by one level due to concerns related to risk of bias and one level for imprecision (small numbers of events and participants, very wide confidence interval). eWe downgraded by one level due to concerns related to risk of bias and one level for imprecision (small numbers of events and participants). fWe downgraded by one level due to concerns related to risk of bias, one level for inconsistency (I2 = 82%), and one level for imprecision (small numbers of participants).
Background
Description of the condition
Kawasaki disease (KD) is an acute systemic vasculitis (inflammation of the blood vessels) first described in 1967 by Japanese paediatrician Tomisaku Kawasaki that mainly affects children (Kawasaki 1967; Yamaji 2019). The majority of cases are seen in children between six months and five years old, and more often in males than females (21 per 100,000 compared to 15 per 100,000, respectively) (Makino 2019). There is substantial ethnic variation, with the lowest rates seen amongst white children (13.7 per 100,000 children under five) and the highest rates seen in children of Asian descent (29.8 per 100,000 children under five) (Makino 2019), although a Japan‐wide survey reported that KD had increased between 2008 and 2015 (Makino 2015). Data are lacking for black/Hispanic ethnic groups due to too few cases being reported (Holman 2010; Maddox 2015).
There is no specific diagnostic test for KD, with diagnosis being made using clinical criteria and excluding other possible diagnoses. To be diagnosed with KD, individuals must have five or more days of fever as well as four or more of the five principal clinical features (chapped lips, strawberry tongue; bulbar conjunctival injection; rash, redness, and swelling of hands and feet or skin peeling; and enlarged cervical lymph nodes) (see Table 6) (Rife 2020). Individuals who meet the criteria are said to have complete KD (also known as typical or classic KD). Individuals who do not meet all the criteria may be diagnosed as having incomplete KD (also known as atypical KD) (Kobayashi 2020; McCrindle 2017).
3. Diagnosis of classic Kawasaki disease*.
| Diagnosis of classic Kawasaki disease |
Classic KD is diagnosed in the presence of fever for at least 5 days (the day of fever onset is taken to be the first day of fever) together with at least 4 of the 5 following principal clinical features. In the presence of ≥ 4 principal clinical features, particularly when redness and swelling of the hands and feet are present, the diagnosis of KD can be made with 4 days of fever, although in rare cases experienced clinicians who have treated many patients with KD may establish the diagnosis with 3 days of fever.
|
| A careful history may reveal that ≥ 1 principal clinical features were present during the illness but had resolved by the time of presentation. |
| Patients who lack full clinical features of classic KD are often evaluated for incomplete KD. If coronary artery abnormalities are detected, the diagnosis of KD is considered confirmed in most cases. |
| Laboratory tests typically reveal normal or elevated white blood cell count with neutrophil predominance and elevated acute phase reactants such as C‐reactive protein and erythrocyte sedimentation rate during the acute phase. Low serum sodium and albumin levels, elevated serum liver enzymes, and sterile pyuria can be present. In the second week after fever onset, thrombocytosis is common. |
| Other clinical findings may include the following: |
| Cardiovascular |
| Myocarditis, pericarditis, valvular regurgitation, shock |
| Coronary artery abnormalities |
| Aneurysms of medium‐sized non‐coronary arteries |
| Peripheral gangrene |
| Aortic root enlargement |
| Respiratory |
| Peribronchial and interstitial infiltrates on chest x‐ray |
| Pulmonary nodules |
| Musculoskeletal |
| Arthritis, arthralgia (pleocytosis of synovial fluid) |
| Gastrointestinal |
| Diarrhoea, vomiting, abdominal pain |
| Hepatitis, jaundice |
| Gallbladder hydrops |
| Pancreatitis |
| Nervous system |
| Extreme irritability |
| Aseptic meningitis (pleocytosis of cerebrospinal fluid) |
| Facial nerve palsy |
| Sensorineural hearing loss |
| Genitourinary |
| Urethritis/meatitis, hydrocele |
| Other |
| Desquamating rash in groin |
| Retropharyngeal phlegmon |
| Anterior uveitis by slit lamp examination |
| Erythema and induration at BCG inoculation site |
| The differential diagnosis includes other infectious and non‐infectious conditions, including the following: |
| Measles |
| Other viral infections (e.g. adenovirus, enterovirus) |
| Staphylococcal and streptococcal toxin‐mediated diseases (e.g. scarlet fever and toxic shock syndrome) |
| Drug hypersensitivity reactions, including Stevens‐Johnson syndrome |
| Systemic onset juvenile idiopathic arthritis |
| With epidemiologic risk factors: |
| Rocky Mountain spotted fever or other rickettsial infections |
| Leptospirosis |
*American Heart Association guidelines (McCrindle 2017).
BCG: Bacillus Calmette–Guérin (used in vaccine for prevention of tuberculosis) KD: Kawasaki disease
Kawasaki disease is usually triphasic with an acute, subacute, and convalescent phase. The acute phase is characterised by high fevers (lasting from seven to 14 days if untreated), and systemic inflammation in the medium‐sized arteries, multiple organs, and tissues, resulting in the following common clinical findings: liver (hepatocyte damage), lung (interstitial pneumonitis), gastrointestinal tract (abdominal pain, vomiting, diarrhoea, gallbladder hydrops), meninges (aseptic meningitis, irritability), heart (myocarditis, pericarditis, valvulitis), urinary tract (pyuria), pancreas (pancreatitis), and lymph nodes (lymphadenopathy) (McCrindle 2017). Inflammation of the coronary arteries causes the most serious complication of the disease, that is coronary artery abnormalities (CAAs), which include dilatations and aneurysms. Close monitoring of CAA is important, as ischaemic symptoms or myocardial infarction (MI) due to thrombosis or stenosis can occur. In Japan between 2017 and 2018, coronary artery dilatation, aneurysm, and giant aneurysm (lumen size ≥ 8 mm) within 30 days after KD onset were reported to occur in 7.64%, 0.95%, and 0.11% of patients, respectively (Ae 2020). Kawasaki disease is believed to be a leading cause of acquired heart disease in children from high‐income countries, with male patients or those resistant to initial intravenous immunoglobulin (IVIG) treatment at increased risk of CAAs (Newburger 2004; Uehara 2003).
The subacute phase is often asymptomatic, lasting approximately four weeks. During this time there may be peeling of the skin of the hands and feet, joint pain, and abnormal clinical findings such as thrombocytosis (increase in the number of platelets) or joint pain. This is also when the patient is at greatest risk of developing a coronary artery aneurysm. The convalescent phase is typically asymptomatic, four to eight weeks after onset.
Echocardiography is the standard imaging technique used to evaluate coronary abnormalities, with coronary arteries classified according to size. In children less than five years old, a coronary artery lumen diameter of 3 mm or more is abnormal, whilst in children five years or older, 4 mm or more is considered to be abnormal (JMHW 1984). Coronary artery lesions (CAL) are classified using Z scores (the coronary artery dimensions adjusted for body surface area, as dimensions will change with the size of the child) (Dallaire 2010; JMHW 1984; Kobayashi 2016; Olivieri 2008).
The prognosis for children with KD is highly dependent on the severity of coronary artery involvement. The fatality rate in the USA and Japan is reported as less than 0.2%, with MI from coronary occlusion being the main cause of death (Hayasaka 2003).
Description of the intervention
It is thought that KD may be caused by activation of the immune system after infection with an unknown agent, such as a virus, in a genetically susceptible child. This results in an inflammatory cascade where both the innate and adaptive arms of the immune system are activated (Franco 2010; Gedalia 2007; Rowley 1997). However, no infectious cause has yet been identified. A genetic role is indicated by the ethnic relationships and by increased incidence in children whose parents or siblings have also had KD (Uehara 2003; Yashiro 2004), as well as by polymorphisms identified in different genes and gene regions by family linkage and genome studies (Onouchi 2008; Onouchi 2010; Onouchi 2012).
The primary treatments for KD are IVIG and acetylsalicylic acid (ASA) (Newburger 2004; Rife 2020). Standard regimen of the primary treatment consists of a single infusion of high‐dose IVIG (2 g/kg) together with ASA (Newburger 1991). IVIG is most effective when administered within 10 days of the onset of fever, and has been reported to reduce the risk of coronary artery aneurysm formation from 20% to 25%, to 3% to 5% (Newburger 1986). As many as 20% of children are considered to be IVIG resistant (or refractory), as they develop recurrent or persistent fevers after primary treatment (Ashouri 2008; Mori 2004; Newburger 2004). Adjunctive therapy may benefit those patients who are at higher risk of coronary artery aneurysms. Adjuvant treatments may include the use of corticosteroids and tumour necrosis factor‐alpha (TNF‐alpha) blockers such as etanercept and infliximab. Corticosteroids have been shown to reduce the incidence of CALs in KD and decrease fever, duration of hospitalisation, and time to normalisation of C‐reactive protein (CRP) levels (Green 2022). Recent American Heart Association (AHA) guidelines state that giving high‐risk or IVIG‐resistant patients a longer course of corticosteroids should be considered as primary adjunctive therapy (McCrindle 2017). Compared with no treatment or additional treatment with IVIG, TNF‐alpha blockers may have beneficial effects on treatment resistance and the unwanted 'infusion reaction' after treatment initiation for KD (Yamaji 2019).
Other agents include interleukin‐1 (IL‐1) receptor inhibitors (Kone‐Paut 2018), calcineurin inhibition therapy (ciclosporin) (Hamada 2019), cyclophosphamide, methotrexate (Lee 2008), rituximab (Sauvaget 2012), and plasma exchange (Hokosaki 2012), but their use is not widespread due to a lack of evidence (Rife 2020). Statins are also undergoing investigation due to their effects on inflammation, platelet aggregation, coagulation, and endothelial function (Tremoulet 2019).
How the intervention might work
Exactly how IVIG works as a treatment of KD is unknown, but it has a general anti‐inflammatory effect, probably by modulating cytokine and antibody production and by increasing regulatory T‐cell activity (Burns 2015). Acetylsalicylic acid has anti‐inflammatory activity in high dose or antiplatelet activity in low dose, but it does not appear to prevent the development of coronary abnormalities (Baumer 2006). The remaining adjunctive and additional therapeutic agents also act by suppressing the widespread immune response characterised in KD with the aim of minimising symptoms and preventing cardiac abnormalities (Zhang 2020).
Why it is important to do this review
Kawasaki disease is an important cause of acquired heart disease in children in high‐income countries, with the majority of deaths resulting from damage to the coronary arteries. In addition, unexpected death from MI can happen many years later, with incidences of non‐fatal and fatal MI in young adults sometimes thought to result from 'missed' KD in childhood (Burns 1996; Daniels 2012). The primary aim of an accurate diagnosis is to help prevent these complications with quick and effective treatment, and IVIG is widely used for this purpose. In 2020, with the SARS‐CoV‐2 pandemic, increased numbers of KD symptoms have been reported (Verdoni 2020). This review will replace an earlier Cochrane Review on the same topic (Oates‐Whitehead 2003). A new review is planned due to significant changes in Cochrane methodology since the previous review was published. We also aim to include all currently available evidence for IVIG for the treatment of KD in children to aid decision‐making for healthcare providers internationally.
Objectives
To evaluate the efficacy and safety of intravenous immunoglobulin (IVIG) in treating and preventing cardiac consequences of Kawasaki disease.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (RCTs) investigating the use of IVIG for the treatment of KD. We planned to include studies involving treatment for initial or refractory KD, or both. We excluded studies that did not investigate any of our outcomes of interest.
Types of participants
We included studies involving participants diagnosed with KD using Japanese or AHA guidelines (see Table 6) (Ayusawa 2005; McCrindle 2017).
Types of interventions
We included studies using IVIG to treat participants with KD. We included all doses and types of IVIG. We included studies with the following comparisons.
IVIG versus placebo or no treatment.
IVIG versus ASA.
IVIG versus TNF‐alpha blockers.
IVIG versus corticosteroids.
IVIG versus IVIG (i.e. dose versus dose).
IVIG versus any combination of the above providing IVIG was the only difference between the groups, and any treatment effect was not confounded with another co‐treatment.
We excluded studies comparing infusion speed when the same dose was used. We excluded studies that compared one type of IVIG versus another (i.e. different manufacturer or separated/sulphonated).
Types of outcome measures
We recorded the time points of outcomes reported by the included studies. We were interested in the acute phase (up to two weeks) and convalescent phase (four weeks or later after initial treatment).
Primary outcomes
Incidence of CAAs diagnosed by echocardiography or coronary angiography defined by absolute diameter, JMHW 1984, or Z‐scores.
Incidence of any adverse effects after treatment initiation.
Secondary outcomes
Acute coronary syndromes, such as MI or coronary thrombus.
Duration of fever (days).
Need for additional treatment.
Length of hospital stay (days).
Mortality (all‐cause).
Search methods for identification of studies
Electronic searches
The Cochrane Vascular Information Specialist conducted systematic searches of the following databases for RCTs and controlled clinical trials with no language, publication year, or publication status restrictions:
Cochrane Vascular Specialised Register via the Cochrane Register of Studies (CRS‐Web; searched 26 April 2022);
Cochrane Central Register of Controlled Trials (CENTRAL; Issue 3, 2022) via the Cochrane Register of Studies Online (CRSO);
MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE) 1946 to 26 April 2022;
Embase Ovid (1974 to 26 April 2022);
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) (1982 to 26 April 2022).
We developed search strategies for other databases from the search strategy designed for MEDLINE. Where appropriate, these were combined with adaptations of the Highly Sensitive Search Strategy designed by the Cochrane for identifying RCTs and controlled clinical trials (as described in Chapter 4 of the Cochrane Handbook for Systematic Reviews of Interventions, Lefebvre 2022). Search strategies for the major databases are provided in Appendix 1.
We searched the following trials registries:
World Health Organization International Clinical Trials Registry Platform (who.int/trialsearch);
ClinicalTrials.gov (clinicaltrials.gov).
The most recent searches were carried out on 26 April 2022.
Searching other resources
We checked the reference lists of included studies and relevant review articles to identify other ongoing or published studies. We contacted relevant manufacturers for trial information (Baxter Healthcare, Teijin Ltd, Mitsubishi Pharma Corp, Japan Blood Products Organization, Nihon Pharmaceutical Co Ltd, N‐Bayer Yakuhin Ltd, KM Biologics, and Takeda Pharmaceuticals).
Data collection and analysis
Selection of studies
We used Covidence software to screen all reports identified by the Information Specialist (Covidence). One of two review authors assessed reports by title or abstract (CB, SK), with any articles clearly not meeting the inclusion criteria (e.g. non‐RCTs) considered as 'not relevant'. We obtained the full‐text reports of all studies deemed potentially relevant. Two of three review authors (CB, SK, MS) independently assessed the full‐text reports for inclusion in the review. Any disagreements were resolved by discussion. We collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We illustrated the study selection process in a PRISMA diagram (Liberati 2009). We listed all articles excluded after full‐text assessment in the Characteristics of excluded studies tables and provided the reasons for their exclusion.
Data extraction and management
We used a data collection form based on the form provided by Cochrane Vascular to record study characteristics and outcome data. One of three review authors (CB, SK, MS) extracted the following study characteristics from the included studies.
Methods (study design, number of participants, exclusions postrandomisation, losses to follow‐up, intention‐to‐treat analysis, duration of study).
Participants (country, setting, age, sex, inclusion and exclusion criteria).
Interventions (intervention, comparison, concomitant medications).
Outcomes (primary and secondary outcomes specified and collected, and time points reported).
Funding source and declaration of interest of the study authors.
One of three review authors (CB, SK, MS) independently extracted outcome data from the included studies, which a second review author (CB, SK, or MS) checked. When multiple trial arms were reported in a single trial, we included only the relevant arms. Any disagreements were resolved by consensus or by involving a third review author (TK, SI). One review author (CB) transferred data into Review Manager Web (RevMan Web 2022). We double‐checked that data were entered correctly. In the case of unclear or incomplete information or data, we contacted the study authors to request clarification. Additional information was provided for Matsushima 1985.
Assessment of risk of bias in included studies
Two of three review authors (CB, SK, MS) independently assessed the risk of bias of each included study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreements were resolved by discussion or by involving another review author (TK). We assessed risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Other bias
We graded each domain as low, high, or unclear risk of bias, and provided a statement to justify our judgement in the risk of bias table. We summarised the risk of bias judgements across different studies for each of the domains listed. Where necessary, we considered blinding separately for cardiac outcomes and non‐cardiac outcomes.
Measures of treatment effect
We analysed dichotomous data as odds ratios (OR) with 95% confidence intervals (CI), and continuous data as mean difference (MD) with 95% CI. We planned to use standardised mean difference (SMD) if outcomes were reported using different measurement scales, but this was not necessary.
Unit of analysis issues
The unit of analysis was each individual participant. Some papers reported multiple studies. We entered the separate studies into the Characteristics of included studies tables by author, followed by date, followed by either A, B, or C (where A is the earliest of the trials documented) (i.e. Smith 1990A, Smith 1990B, Smith 1990C). Some studies reported three comparison arms. We were careful there were no unit of analysis issues with double‐counting of participants if included studies used multiple intervention arms. If two comparisons (e.g. drug A versus control and drug B versus control) were combined in the same meta‐analysis, we halved the control group to avoid double‐counting. We used intention‐to‐treat analysis when possible.
Dealing with missing data
We contacted study authors to obtain missing study characteristics or outcome data when necessary. When this was not possible, and the missing data were considered sufficient to introduce bias, we would explore the impact of including these studies by sensitivity analysis. We considered missing data sufficient to introduce bias if the missing data were imbalanced between study arms or were potentially a result of the intervention.
Assessment of heterogeneity
We assessed heterogeneity visually by inspecting forest plots. We also used the Chi2 and I2 statistics and Tau2 in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021). We interpreted the I2 value approximately as follows:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
When assessing the importance of the observed value of I2, we considered (i) the magnitude and direction of effects and (ii) the strength of evidence for heterogeneity (e.g. P value from the Chi2 test, or a CI for I2) in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021). If we detected heterogeneity, we explored the reasons for it through subgroup analysis.
Assessment of reporting biases
We planned that when more than 10 studies were pooled for a given outcome, we would create a funnel plot to explore possible small‐study and publication biases.
Data synthesis
We carried out data synthesis using Review Manager Web (RevMan Web 2022). We planned to use a fixed‐effect model when there were no concerns about heterogeneity. As there were differences between many of the studies (doses, infusion regimen, concomitant medications, etc.), we used a random‐effects model for all analyses, not just in the case of substantial heterogeneity (I2 > 50%). We only undertook meta‐analyses where this was meaningful, that is if the treatments, participants, and the underlying clinical question were similar enough for pooling to make sense. When meta‐analysis was not possible, we reported the results using a narrative synthesis.
Subgroup analysis and investigation of heterogeneity
We had planned to undertake subgroup analyses by initial or refractory (secondary) IVIG treatment and by single‐ or multiple‐dose regimens. Given the range of regimens involved in the included studies, it was clinically more appropriate to present initial versus secondary IVIG treatment, and single versus multiple doses as separate comparisons and subgroup by the total dose administered. We investigated any impact on the geographical distribution of participants by subgrouping by trial country setting when possible. When only limited data were available, we considered whether it was appropriate to conduct subgroup analysis, as in such cases results may reflect a lack of information rather than a true effect (Deeks 2021). We used the formal test for subgroup interactions in Review Manager Web (RevMan Web 2022).
We had planned to undertake subgroup analyses on the day of IVIG treatment, age, and weight/body mass index (BMI), but these analyses were precluded by insufficient information. We investigated any impact of study risk of bias using sensitivity analysis (see below).
Sensitivity analysis
We undertook sensitivity analyses to check if the results were robust by excluding studies at high risk of bias from the analysis. We considered studies to be at high risk of bias when assessed as being at high risk of selection bias (i.e. high risk for either random sequence generation or allocation sequence concealment), or at high risk of detection bias for cardiac outcomes. We also undertook sensitivity analysis when it was not clear what KD diagnostic criteria had been used. We further undertook sensitivity analysis when we identified substantial heterogeneity by removing studies from the analyses to assess the individual impact of studies on the results.
Summary of findings and assessment of the certainty of the evidence
We created a summary of findings table to present the evidence in the review for the following outcomes.
Incidence of CAAs.
Incidence of any adverse effects after treatment initiation.
Acute coronary syndrome such as MI or coronary thrombus.
Duration of fever.
Need for additional treatment.
Length of hospital stay.
Mortality (all‐cause).
We included a table for the most clinically relevant comparisons. These were: primary treatment with IVIG compared to ASA (see Table 1); primary treatment with IVIG compared to different infusion regimens of IVIG (see Table 3); and primary treatment with IVIG compared to prednisolone (see Table 5). We used the five GRADE considerations (risk of bias, inconsistency, imprecision, indirectness, and publication bias) to assess the certainty of the evidence as it relates to the studies which contributed data to the meta‐analyses for each prespecified outcome (Atkins 2004). We used the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021; Schünemann 2021), employing GRADEpro GDT software (GRADEpro GDT). We explained all decisions to downgrade the certainty of evidence using footnotes and added comments to aid the reader's understanding of the review when needed.
Results
Description of studies
Results of the search
The searches identified a total of 2679 articles. An additional 23 records were identified from citation screening. After deduplication, we screened 1957 articles by title and abstract. We assessed 237 full‐text articles for eligibility. We included 31 studies (49 records). Several records reported on more than one study. We excluded 13 studies (16 records) with reasons provided. We identified two ongoing studies (three records) and 23 studies as awaiting classification. See Figure 1.
1.
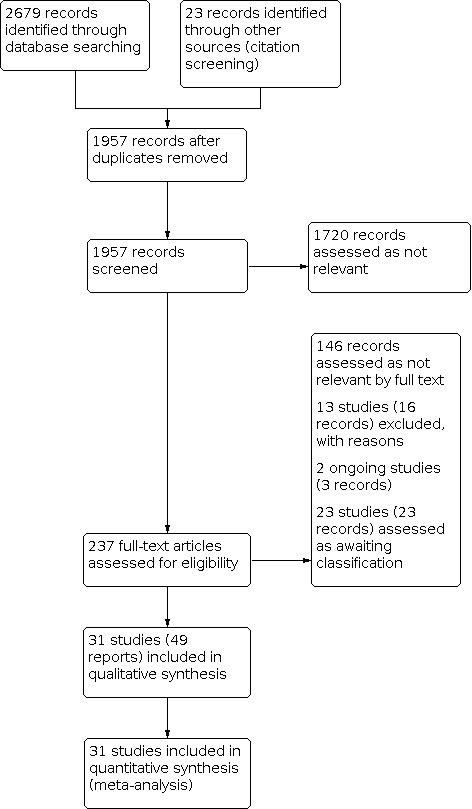
PRISMA flow diagram.
Included studies
See Characteristics of included studies tables.
We included 31 studies with a total of 4609 participants that investigated IVIG treatment for KD (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; Hashino 2001; He 2021; Matsushima 1985; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995; Wang 2020; Yabiku 1989; Youn 2016; Yuan 2000). The majority of studies (21) were carried out in Japan (Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; Hashino 2001; Matsushima 1985; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Sakata 2007; Sato 1995; Yabiku 1989). Five were carried out in the USA or the USA and Canada (Barron 1990; Burns 2008; Burns 2021; Newburger 1986; Newburger 1991), four in China (He 2021; Qin 2006; Wang 2020; Yuan 2000), and one in Korea (Youn 2016).
The size of the included studies varied, with the smallest having 17 participants, Hashino 2001, and the largest 549 participants, Newburger 1991. Nishihara 1988 did not report the numbers of male and female participants. As expected, clinically all studies reported a larger proportion of males overall, with one exception being Yabiku 1989, which reported equal numbers of males and females in the control group.
The age of participants ranged from two months, Hashino 2001, to 14 years, Qin 2006, with the majority of participants aged between 18 and 30 months (Barron 1990; Burns 2008; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; He 2021; Matsushima 1985; Miura 2008; Mori 2017; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Sakata 2007; Sato 1995; Wang 2020; Yabiku 1989). Four studies included some older participants (Burns 2021; Morikawa 1994; Youn 2016; Yuan 2000).
The majority of studies reported on the primary treatment of KD (Barron 1990; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; He 2021; Matsushima 1985; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Qin 2006; Sato 1995; Yabiku 1989; Yuan 2000). One study reported on primary plus additional treatment (Sakata 2007). Six studies reported on secondary or refractory treatment for KD (Burns 2008; Burns 2021; Miura 2008; Mori 2017; Wang 2020; Youn 2016), and one study reported on tertiary treatment (Hashino 2001).
For those studies reporting on primary treatment, treatment was initiated within seven days of onset in 12 studies (Barron 1990; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; Matsushima 1985; Nishihara 1988; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Yabiku 1989), and 10 days in eight studies (He 2021; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nonaka 1995; Sakata 2007; Sato 1995). Initiation of treatment was not clear in Qin 2006 and Yuan 2000.
All studies investigating secondary treatment used IVIG as the initial treatment. Secondary treatment was initiated when fever did not decrease within 36 hours to seven days after initial treatment (Burns 2008; Burns 2021), or 24 to 48 hours after initial treatment (Miura 2008; Mori 2017; Wang 2020; Youn 2016).
Some studies reported three arms (Furusho 1991A; Furusho 1991B; He 2021; Nishihara 1988; Onouchi 1988; Onouchi 1992). When necessary, to be able to report these in analyses using Review Manager Web, we split one of the comparison arms between the other two arms to prevent double‐counting of participants.
We identified and included studies with the following comparisons:
IVIG compared to ASA;
IVIG compared to a different dose of IVIG;
IVIG compared to infliximab;
IVIG compared to methylprednisolone.
We did not identify any randomised studies comparing IVIG to placebo or no treatment.
The total dose and frequency of IVIG treatment varied between studies and ranged from 50 to 100 mg/kg/day to 2 g/kg/day as either a single dose or daily infusions for up to five days. Infusion times ranged from one to 24 hours. The majority of participants received ASA in addition to IVIG. One study also administered dipyridamole (Nonaka 1995). In Burns 2008, participants also received paracetamol and diphenhydramine; heparin was infused with methylprednisolone in Miura 2008; and Sakata 2007 administered flurbiprofen to participants with liver dysfunction.
The majority of studies compared initial IVIG to a different dose or regimen of initial IVIG, Barron 1990; Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Newburger 1991; Nishihara 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995, or to ASA alone, Furusho 1984; Furusho 1991B; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989. Nonaka 1995 and Yuan 2000 compared IVIG to prednisolone. Studies investigating secondary treatment compared IVIG to infliximab, Burns 2008; Burns 2021; Mori 2017; Youn 2016, or methylprednisolone, Miura 2008; Wang 2020. Hashino 2001 investigated tertiary treatment and compared IVIG with methylprednisolone. For specific details on doses and regimens, see the Characteristics of included studies tables.
Coronary artery abnormalities were reported by all included studies, the majority of which described detection and classification of CAA with echocardiography (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Furusho 1991A; Furusho 1991B; Hashino 2001; He 2021; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Nonaka 1995; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Sakata 2007; Sato 1995; Wang 2020; Youn 2016). Seven studies did not describe how they classified CAA (Harada 1989; Matsushima 1985; Ogawa 1987; Ogino 1987; Qin 2006; Yabiku 1989; Yuan 2000).
The remaining outcomes of interest were reported by only some studies:
adverse effects (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Furusho 1991A; Harada 1989; He 2021; Matsushima 1985; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Qin 2006; Sato 1995; Wang 2020; Yabiku 1989; Youn 2016);
acute coronary syndromes (Matsushima 1985; Newburger 1986; Nonaka 1995);
duration of fever (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Harada 1989; Hashino 2001; He 2021; Matsushima 1985; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995; Wang 2020; Yabiku 1989; Youn 2016; Yuan 2000);
need for additional treatment (Burns 2008; Burns 2021; Furusho 1984; He 2021; Matsushima 1985; Mori 2017; Morikawa 1994; Newburger 1991; Onouchi 1988; Onouchi 1992; Sakata 2007; Wang 2020; Youn 2016);
length of hospital stay (Barron 1990; Burns 2021; He 2021; Newburger 1991; Qin 2006; Sakata 2007; Sato 1995; Youn 2016);
mortality (Burns 2021; Furusho 1984; Matsushima 1985; Miura 2008; Newburger 1991; Nonaka 1995).
Eleven studies reported public or government funding sources (Burns 2008; Burns 2021; Harada 1989; Hashino 2001; He 2021; Newburger 1986; Newburger 1991; Okuni 1987A; Okuni 1987B; Qin 2006; Wang 2020). Three studies received funding (or additional funding) from pharmaceutical companies that manufacture blood plasma products or immune‐regulating products (Barron 1990; Burns 2008; Mori 2017). Three studies acknowledged pharmaceutical companies for donating gammaglobulin (Furusho 1984; Ogawa 1987; Ogino 1987). The remaining studies did not report funding sources (Furusho 1991A; Furusho 1991B; Matsushima 1985; Miura 2008; Morikawa 1994; Nagashima 1987; Nishihara 1988; Nonaka 1995; Onouchi 1988; Onouchi 1992; Sakata 2007; Sato 1995; Yabiku 1989; Youn 2016; Yuan 2000). See Characteristics of included studies.
Excluded studies
We excluded a total of 13 studies based on full‐text assessment (ChiCTR2000035163; Hamada 2019; ISRCTN71987471; JPRN‐UMIN000014665; Lee 1996; Lin 2021; Muta 2002; Nanishi 2017; NCT02298062; Portman 2019; RAISE 2012; Sanati 2021; Seki 2021). The reasons for exclusion were as follows:
IVIG was not the differentiating intervention (ChiCTR2000035163; Hamada 2019; Lin 2021; Nanishi 2017; RAISE 2012; Sanati 2021);
study compared injection or infusion speed of IVIG (JPRN‐UMIN000014665; Seki 2021);
study only reported surrogate outcomes (lymphocyte phenotypes), and so did not meet our inclusion criteria (Lee 1996);
study compared different types of IVIG, and dosage was determined by KD severity (Muta 2002);
study randomised to treatment (not IVIG) after initial IVIG treatment (ISRCTN71987471; Portman 2019);
study not completed due to limited participants and COVID‐19 (NCT02298062).
For details of the excluded studies, see Characteristics of excluded studies tables.
Ongoing studies
We identified two ongoing studies (ChiCTR1900027954; EUCTR2020‐003194‐22‐FR). For details, see Characteristics of ongoing studies tables.
Studies awaiting classification
We assessed 23 reports as awaiting classification (Chang 2007; Chang 2008; Chen 2006; Fu 2010; Ho 2003; Ho 2004; Juan 2003; Juan 2005; Juan 2006; Kuo 2009; Li 2008; Li 2009; Liao 2007; Liu 2000; Liu 2004; Liu 2009; Lu 2003; Peng 2001; Teng 2005; Yao 2009; Yen 2007; Yuan 2009; Yueh 2006), which were identified by citation screening from published reviews and not by our database searches. We are currently unable to verify if they meet our inclusion criteria.
Risk of bias in included studies
We assessed the risk of bias of each included study based on the seven domains of the Cochrane risk of bias tool (RoB 1). An overall summary of bias present within each of the included studies is presented in Figure 2 and Figure 3. No studies were at low risk of bias in all domains. Of the 31 included studies, 24 studies had at least one domain at high risk of bias. No study was at high risk of bias in all domains. All studies were at unclear risk of bias in at least one domain.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We selected only RCTs for this review. However, we judged only eight studies to be at low risk of bias for both random sequence generation and allocation concealment domains (Burns 2021; Harada 1989; Mori 2017; Morikawa 1994; Newburger 1986; Newburger 1991; Sakata 2007; Wang 2020). We judged Yuan 2000 to be at high risk for both random sequence generation and allocation concealment domains, as hospital numbers were used to assign treatment. We judged Matsushima 1985 and Nagashima 1987 to be at high risk for both random sequence generation and allocation concealment domains, as odd and even numbers were used to assign treatment. Four studies provided sufficient details to be assessed as at low risk for random sequence generation, but insufficient information to be assessed as low or high risk for allocation concealment, and were therefore judged as unclear (Barron 1990; Burns 2008; He 2021; Sato 1995). Four studies stated that randomisation was arranged centrally, but did not provide details, so were assessed as unclear for random sequence generation and low for allocation concealment (Ogawa 1987; Ogino 1987; Onouchi 1992; Yabiku 1989). Twelve studies did not describe the method of randomisation and allocation at all or did not describe their methods in sufficient detail to permit an assessment, so were assessed as at unclear risk of bias for both domains (Furusho 1984; Furusho 1991A; Furusho 1991B; Hashino 2001; Miura 2008; Nishihara 1988; Nonaka 1995; Okuni 1987A; Okuni 1987B; Onouchi 1988; Qin 2006; Youn 2016).
Blinding
Performance bias
We assessed one study to be at low risk of performance bias, as blinding of clinicians was described (Sakata 2007). We judged nine studies to be at high risk of performance bias, as it was clearly stated that no blinding of participants and personnel had been undertaken (Burns 2008; Burns 2021; Hashino 2001; He 2021; Miura 2008; Mori 2017; Nagashima 1987; Sato 1995; Wang 2020). We assessed the remaining 21 studies as at unclear risk because they did not provide sufficient details to be assessed as at either low or high risk of performance bias. We acknowledge that given the different infusion times between some of the treatments, blinding of participants and personnel would have been difficult.
Detection bias
We assessed each study for detection bias for both cardiac abnormality outcomes and non‐cardiac abnormality outcomes. This was because blinding of cardiac outcome assessment was possible even in situations where blinding of personnel or participants was not.
Fourteen studies provided a clear description of blinding for evaluating cardiac abnormalities and so were judged to be at low risk of detection bias (Barron 1990; Harada 1989; He 2021; Mori 2017; Morikawa 1994; Newburger 1986; Newburger 1991; Nishihara 1988; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Sakata 2007; Sato 1995). This was generally achieved by echocardiogram (ECG) recordings being assessed by clinicians who were not aware of the participant's identity. We judged 12 studies to be at high risk of detection bias for cardiac outcomes because there were no blinding measures, and the outcome could have been influenced by a lack of blinding (Burns 2008; Furusho 1984; Furusho 1991A; Furusho 1991B; Matsushima 1985; Miura 2008; Nagashima 1987; Nonaka 1995; Qin 2006; Wang 2020; Youn 2016; Yuan 2000). When blinding of outcome assessors was insufficiently described, we judged the risk of detection bias as unclear (Burns 2021; Hashino 2001; Ogawa 1987; Ogino 1987; Yabiku 1989).
For non‐cardiac outcomes, Onouchi 1988 and Onouchi 1992 reported that independent assessors were used for non‐cardiac outcomes, therefore we judged these studies to be at low risk of detection bias. We judged 24 studies to be at high risk of bias, as a lack of blinding was likely to influence outcomes (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; Hashino 2001; He 2021; Matsushima 1985; Miura 2008; Mori 2017; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nonaka 1995; Okuni 1987A; Okuni 1987B; Qin 2006; Sato 1995; Wang 2020; Youn 2016; Yuan 2000). We judged four studies to be at unclear risk of detection bias for non‐cardiac outcomes because insufficient details on how these outcomes were assessed were provided, or none of the outcomes measured was likely to be impacted by a lack of blinding (Ogawa 1987; Ogino 1987; Sakata 2007; Yabiku 1989). One study did not report on non‐cardiac outcomes, preventing a judgement of detection bias (Nishihara 1988).
Incomplete outcome data
We assessed no studies as being at high risk of attrition bias. The majority of included studies were at low risk of attrition bias, as data were all reported or accounted for (Barron 1990; Burns 2008; Burns 2021; Furusho 1984; Harada 1989; Hashino 2001; He 2021; Matsushima 1985; Miura 2008; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Nishihara 1988; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1992; Sakata 2007; Sato 1995; Wang 2020; Youn 2016). Nine studies were at unclear risk of attrition bias because missing data were sufficient to potentially impact the results (Mori 2017; Ogawa 1987; Yabiku 1989), or the reasons for missing data were unclear (Furusho 1991A; Furusho 1991B; Nonaka 1995; Onouchi 1988; Qin 2006; Yuan 2000).
Selective reporting
We assessed Furusho 1991A and Furusho 1991B as being at high risk of reporting bias, as no description of outcomes or measurements was provided in a methods section. Seven studies were at low risk of reporting bias, as all expected or planned outcomes per study protocols or trial databases were reported in the results (Burns 2008; Burns 2021; Hashino 2001; He 2021; Mori 2017; Newburger 1991; Wang 2020). We assessed the majority of included studies (22) as at unclear risk of reporting bias, as no protocol was available, or it was not clear what the planned outcomes were (Barron 1990; Furusho 1984; Harada 1989; Matsushima 1985; Miura 2008; Morikawa 1994; Nagashima 1987; Newburger 1986; Nishihara 1988; Nonaka 1995; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995; Yabiku 1989; Youn 2016; Yuan 2000).
Other potential sources of bias
We had no concerns about other potential biases in 21 studies (Burns 2008; Burns 2021; Furusho 1984; Furusho 1991A; Furusho 1991B; Harada 1989; Hashino 2001; He 2021; Matsushima 1985; Morikawa 1994; Nagashima 1987; Newburger 1986; Newburger 1991; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1992; Qin 2006; Sakata 2007; Yuan 2000). No studies were at high risk of other bias. We assessed the remaining studies as at unclear risk of other bias. Reasons for this included an imbalance in gender or ages between groups, and we were not sure if this could have affected the results (Barron 1990; Nonaka 1995; Onouchi 1988; Sato 1995; Yabiku 1989; Youn 2016); study was halted prematurely (Miura 2008); inconsistencies in reporting (Wang 2020); treatments were switched at physician's discretion because of worsening KD in a substantial proportion of participants in both groups (Mori 2017); and results were published as a letter or abstract and likely not peer reviewed (Nishihara 1988).
Effects of interventions
See: Table 1; Table 3; Table 5
We have presented the results of the studies by each comparison and outcome of interest as pre‐planned. For the comparison of IVIG versus IVIG, the studies were heterogeneous in the dose of IVIG used and their infusion regimens. The total dose and frequency of IVIG treatment ranged from 50 to 100 mg/kg/day to 2 g/kg/day as either a single dose or daily infusions for up to five days. In order to present this information as clearly and as usefully as possible, we have indicated the dose and if this was over multiple days (e.g. 200 mg/kg/day for five days), as this is the most clinically familiar way. In the analysis tables, we presented the doses as the total IVIG received and indicated if this was on single or multiple days (e.g. 1000 mg/kg in five days). This was to facilitate a clearer comparison of regimens. We used a random‐effects model for all analyses due to the differences between studies. For specific details on interventions and concomitant medications, please see Characteristics of included studies.
Primary treatment ‐ intravenous immunoglobulin (IVIG) versus acetylsalicylic acid (ASA)
See Table 1.
Eleven studies involving 1396 participants compared IVIG treatment with ASA (Furusho 1984; Furusho 1991B; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989). All studies compared IVIG plus ASA versus ASA. One of two IVIG study arms in Furusho 1991B was not given ASA. Most studies administered ASA initially at 30 mg/kg/day, except for Newburger 1986, who used 100 mg/kg/day every 6 hours to day 14 of illness, and Okuni 1987A, Okuni 1987B, and Onouchi 1988, who used 50 mg/kg/day in both groups. Studies differed in total IVIG dose administered, number of doses, and time points measured.
Incidence of coronary artery abnormalities (CAAs)
All 11 studies reported on the incidence of CAA (Furusho 1984; Furusho 1991B; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989). Where possible, we have presented numbers of CAA excluding any CAA present at enrolment.
Overall, there were fewer CAA detected up to 30 days in the IVIG treatment group compared to the ASA group (odds ratio (OR) 0.60, 95% confidence interval (CI) 0.41 to 0.87; P = 0.008; 11 studies, 1437 participants; moderate‐certainty evidence). See Analysis 1.1.
1.1. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 1: CAA: total dose of IVIG subgrouped by single or multiple infusion (up to 30 days)
Seven studies reported CAA at 60 days or 1 year (Furusho 1984; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Yabiku 1989). There was no clear difference detected at 60 days and over in the IVIG treatment group compared to the ASA group (OR 0.79, 95% CI 0.45 to 1.38; P = 0.41; 7 studies, 679 participants). See Analysis 1.2.
1.2. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 2: CAA: total dose of IVIG subgrouped by single or multiple infusion (≥ 6 months)
Furusho 1984 reported 6/40 (15%) CAA in the IVIG group at 30 days, compared to 19/45 (42%) in the ASA group. No new lesions were detected between day 30 and 60; 14 CAA persisted in the ASA group compared to three CAA in the IVIG group. At day 60, 1/6 CAA were detected in the IVIG group compared to 11/19 CAA in the ASA group.
Furusho 1991B investigated three groups: ASA, ASA + IVIG 200 mg/kg/day, and IVIG 200 mg/kg/day for five days. Before day 30, CAA was reported in 9/49, 10/53, and 19/49 participants respectively. At day 30, CAA was detected in 5/49, 4/51, and 9/47 participants respectively. We halved the ASA group data between subgroup analysis to prevent double‐counting.
Matsushima 1985 compared IVIG 400 mg/kg over 5 days with ASA. This study reported CAA incidence (dilations and aneurysms) at 1, 2, 3, and 4 weeks: 0/17, 3/17, 1/17, and 1/17 versus 0/17, 6/17, 6/17, and 3/17 in the IVIG and ASA groups, respectively.
Nagashima 1987 compared IVIG 400 mg/kg over three days with ASA. This study reported the number of CAA (dilations and aneurysms) at 1, 2, 3, and 4 weeks, and up to day 30, where 11/69 CAA were detected in the IVIG group compared to 25/67 in the ASA group.
Newburger 1986 compared IVIG 400 mg/kg over four days with ASA. They reported the number of CAA at enrolment, 2 and 7 weeks, and 1‐year follow‐up. At enrolment, 2/84 participants in the IVIG group and 4/84 in the ASA group had CAA. At 2 and 7 weeks, excluding those at enrolment, there were 5/74 versus 15/75 and 2/77 versus 11/75 CAA in the IVIG and ASA groups, respectively. At 2 and 7 weeks and 1 year, including those at enrolment, there were 6/75 versus 18/78, 3/79 versus 14/79, and 2/7 versus 9/17 CAA in the IVIG and ASA groups, respectively.
Ogawa 1987 compared IVIG (400 mg/kg/day for 3 consecutive days) with ASA (30 mg/kg/day) versus ASA (30 mg/kg/day). The reported number of CAA at enrolment (1 to 10 days), under 11 to 25 days, 30 days, and 60 days were: 5/63, 11/63, 6/63, and 3/63 in the IVIG with ASA group versus 2/54, 17/54, 9/54, and 7/54 in the ASA group.
Ogino 1987 compared IVIG (200 mg/kg/day for 3 consecutive days) with ASA (30 mg/kg/day) versus ASA (30 mg/kg/day). The reported number of CAA at enrolment (1 to 10 days), under 11 to 25 days, 30 days, 60 days, and 1 year were: 3/50, 15/50, 13/50, 9/50, and 4/50 in the IVIG with ASA group versus 5/42, 13/42, 10/42, 6/42, and 3/42 in the ASA group.
Okuni 1987A compared single 100 mg/kg of IVIG (either pepsin treated or intact) versus ASA. We combined the two types of IVIG used. They reported CAA at enrolment, under 30 days, 30 days, 60 days, 6 months, and 1 year: 13/139, 55/136, 31/139, 24/139, 15/139, and 9/138 in the IVIG group versus 7/75, 29/75, 15/74, 11/74, 8/74, and 3/73 in the ASA group. The study authors reported no difference between groups if CAA numbers at enrolment were excluded, but we do not have those data.
Okuni 1987B compared 100 mg/kg of IVIG for five days (either pepsin treated or intact) versus ASA. We combined the two types of IVIG used. They reported CAA at enrolment, under 30 days, 30 days, 60 days, 6 months, and 1 year: 17/196, 78/192, 36/188, and 21/186 in the IVIG group versus 11/99, 50/97, 30/95, and 20/90 in the ASA group. They also reported the data excluding those present at enrolment for under 30 days, 30 days, 60 days, 6 months, and 1 year: 61/175, 27/171, and 15/169 in the IVIG group versus 39/86, 21/85, and 13/81 in the ASA group.
Onouchi 1988 compared three arms: 200 mg/kg IVIG for 3 days, 400 mg/kg IVIG for 3 days, and ASA. They reported CAA detected before treatment, and at days 15, 30, and 60: IVIG 200 mg/kg: 6/38, 15/38, 10/38, and 7/38 versus IVIG 400 mg/kg: 5/42, 16/42, 10/42, and 6/42 versus ASA: 7/46, 19/46, 14/46, and 6/46. We included the day 15 data in the analysis. We split the ASA group between the analysis to prevent double‐counting.
Yabiku 1989 compared a single dose of IVIG 1 g/kg with ASA versus ASA. They reported the number of CAA at enrolment (1 to 10 days), under 11 to 25 days, 30 days, and 60 days: 4/48, 13/48, 8/48, and 3/48 in the IVIG with ASA group versus 4/36, 12/36, 6/36, and 3/36 in the ASA group, respectively.
Incidence of any adverse effects after treatment initiation
See Analysis 1.3 and Table 2.
1.3. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 3: Adverse effects: total dose of IVIG subgrouped by single or multiple infusion
Ten studies reported a wide range of adverse effects, including: liver disorder, chills and fever, pericardial effusion, urticaria, mild congestive heart failure, shaking/itching, sepsis, lymphadenopathy, splenomegaly, neutropenia, and nasal haemorrhage (Furusho 1984; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989). No serious adverse events were reported. Furusho 1991B did not report adverse effects.
We combined the data in a meta‐analysis and described specific adverse effects by study in Table 2. Overall, there was no clear difference in the number of adverse effects between the IVIG and ASA groups (OR 0.57, 95% CI 0.17 to 1.89; P = 0.35; 10 studies, 1376 participants; very low‐certainty evidence). See Analysis 1.3. We detected substantial heterogeneity (I2 = 73%). This may have been due to the different adverse effects reported by each study. The test for subgroup differences did not detect a difference in adverse effects between the different total IVIG doses used (P = 0.10).
Acute coronary syndromes, such as myocardial infarction (MI) or coronary thrombus
Only Newburger 1986 reported the incidence of acute coronary syndromes. At 30 months, no adverse sequelae were reported in the 7 participants in the IVIG group followed up to this point. Two of 17 participants in the ASA group had a coronary artery thrombus. Matsushima 1985 provided additional information upon request and confirmed that no acute coronary events had occurred. No other studies reported this outcome. We assessed this evidence to be of low certainty.
Duration of fever (days)
Eight studies reported duration of fever (Furusho 1984; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Onouchi 1988; Yabiku 1989). Four studies reported duration from onset of disease (Furusho 1984; Ogawa 1987; Ogino 1987; Yabiku 1989). Three studies reported duration both from disease onset and onset of treatment (Matsushima 1985; Nagashima 1987; Onouchi 1988). Newburger 1986 reported the average fall in temperature and maximum temperature in hospitalised children.
We combined the data from studies reporting duration of fever from treatment onset. Overall, the duration of fever in the IVIG group was shorter than in the ASA group (mean difference (MD) −4.00 days, 95% CI −5.06 to −2.93; P < 0.001; 3 studies, 307 participants; moderate‐certainty evidence). See Analysis 1.4.
1.4. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 4: Duration of fever from treatment onset (days): total dose of IVIG subgrouped by single or multiple infusion
We also combined the data from studies reporting duration from disease onset. Overall, the duration of fever in the IVIG group was shorter than in the ASA group (MD −1.60 days, 95% CI −2.69 to −0.52; P = 0.004; 7 studies, 693 participants). See Analysis 1.5.
1.5. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 5: Duration of fever from KD onset (days): total dose of IVIG subgrouped by single or multiple infusion
Newburger 1986 also reported data from centres where participants were hospitalised for at least two days to prevent bias from home reporting. Between day 1 and 2, the average temperature (± standard error, SE) of the IVIG group fell by 1.3 ± 0.16 ˚C compared to 0.42 ± 0.11 ˚C in the ASA group. At day 2, the number of participants with a maximum temperature ≥ 38 ˚C was 16/35 in IVIG group compared to 30/35 in the ASA group.
Need for additional treatment
Details on the need for additional treatment were limited, with three studies reporting this outcome. Furusho 1984 reported that one IVIG participant was retreated with IVIG and one ASA participant was treated with IVIG because of worsening symptoms. Matsushima 1985 reported that no participants needed retreatment. Onouchi 1988 reported that three ASA participants were retreated, but did not provide details about the medication given. Overall, there was no clear difference in need for additional retreatment between IVIG and ASA groups (OR 0.27, 95% CI 0.05 to 1.57; P = 0.15; 3 studies, 272 participants; low‐certainty evidence). See Analysis 1.6.
1.6. Analysis.

Comparison 1: Primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 6: Need for additional treatment: total dose of IVIG subgrouped by single or multiple infusion
Nagashima 1987 mentions that 1/69 participants in the IVIG group received additional IVIG, but it is unclear if this was the only participant to do so. The need for additional treatment was not clearly reported in the remaining studies in this comparison, and no further information was available upon contacting study authors (Furusho 1991B; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Yabiku 1989).
Length of hospital stay (days)
None of the studies comparing IVIG with ASA reported on length of hospital stay (Furusho 1984; Furusho 1991B; Matsushima 1985; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989).
Mortality (all‐cause)
Two studies reported details on mortality incidence, with no deaths occurring in either study (Furusho 1984; Matsushima 1985). The remaining studies did not mention mortality, and although it is likely this means there were no deaths, we cannot be sure about this (Furusho 1991B; Nagashima 1987; Newburger 1986; Ogawa 1987; Ogino 1987; Okuni 1987A; Okuni 1987B; Onouchi 1988; Yabiku 1989). We assessed this evidence to be of low certainty.
Primary treatment ‐ IVIG versus IVIG
See Table 3.
Twelve studies compared IVIG with a different dose of IVIG or single versus multiple infusions, or multiple versus multiple infusions (Barron 1990; Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Newburger 1991; Nishihara 1988; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995).
Eight studies with a total of 1824 participants compared a high‐dose regimen versus a medium‐ or low‐dose regimen (Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Nishihara 1988; Onouchi 1992; Qin 2006; Sakata 2007). Sakata 2007 administered additional IVIG if needed after the first dose. We included data from the first infusion only in this analysis. We considered a high dose to be more than 1900 mg/kg total IVIG; medium to be 1900 mg/kg to 900 mg/kg total IVIG; and low to be less than 900 mg/kg total IVIG. These dose categories are the same as the nationwide survey in Japan (Ae 2020; Ae 2021). Some studies reported on three groups (Furusho 1991A; He 2021; Nishihara 1988; Onouchi 1992). Where appropriate, we split the data between subgroups to prevent double‐counting.
All eight studies infused a total of 2 g/kg using either a single infusion, He 2021; Qin 2006; Sakata 2007, or multiple infusions over two days, He 2021, or five days, Furusho 1991A; Harada 1989; Morikawa 1994; Nishihara 1988; Onouchi 1992. The medium and low doses ranged from 1000 mg/kg to 500 mg/kg total IVIG by single, He 2021; Qin 2006; Sakata 2007, or multiple infusions over five days, Furusho 1991A; Harada 1989; Morikawa 1994; Nishihara 1988; Onouchi 1992.
Incidence of CAAs
Meta‐analysis showed that fewer CAA were reported in the higher infusion regimens compared to the medium or lower regimens (OR 0.60, 95% CI 0.40 to 0.89; P = 0.01; 8 studies, 1824 participants; moderate‐certainty evidence). See Analysis 2.1. No differences were detected between subgroups (test for subgroup differences P = 0.07).
2.1. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 1: CAA: high‐dose regimens vs medium‐ or low‐dose regimens
Three studies compared higher‐dose single‐infusion regimens with medium‐dose single infusion (He 2021; Qin 2006; Sakata 2007). No clear difference in incidence of CAA was detected between these regimens (OR 0.88, 95% CI 0.59 to 1.32; P = 0.53; 3 studies, 621 participants). See Analysis 2.2.
2.2. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 2: CAA: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens
Six studies investigated higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens (Furusho 1991A; Harada 1989; Morikawa 1994; Nishihara 1988; Onouchi 1988; Onouchi 1992). Higher multiple‐infusion doses were 2 g/kg, Furusho 1991A; Harada 1989; Morikawa 1994; Nishihara 1988; Onouchi 1992, or 1000 mg/kg total, Furusho 1991A; Nishihara 1988; Onouchi 1988; Onouchi 1992, over five days. Overall, fewer CAA were detected in groups receiving the higher‐dose multiple infusions (OR 0.46, 95% CI 0.32 to 0.66; P < 0.001; 6 studies, 1154 participants). See Analysis 2.3. No differences were detected between subgroups (test for subgroup differences P = 0.32).
2.3. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 3: CAA: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens
Four studies investigated single‐infusion regimens versus multiple‐infusion regimens (Barron 1990; He 2021; Newburger 1991; Sato 1995). Sato 1995 only included participants scoring ≥ 4 on Harada score. Single doses ranged from 2 g/kg, He 2021; Newburger 1991; Sato 1995, to 1000 mg/kg, Barron 1990, total dose of IVIG. Multiple doses ranged from 2 g/kg total over two days, He 2021, or five days, Sato 1995, and 1600 mg/kg total over four days (Barron 1990; Newburger 1991). Overall, there was no clear difference in incidence of CAA between the single‐infusion and multiple‐infusion groups (OR 0.61, 95% CI 0.28 to 1.34; P = 0.22; 4 studies, 962 participants). See Analysis 2.4. No differences were detected between subgroups (test for subgroup differences P = 0.31).
2.4. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 4: CAA: single‐infusion regimens vs multiple‐infusion regimens
When splitting participants between subgroup analyses, if groups contained an uneven number of participants so that numbers could not be equally divided, we carried out the analysis in both ways to detect possible differences in the results caused by an unequal division of the numerator and denominator. This did not cause a significant change in size or direction of effect in any of the analyses.
Incidence of any adverse effects after treatment initiation
Ten studies reported adverse effects (or lack of) after treatment initiation (Barron 1990; Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Newburger 1991; Onouchi 1988; Onouchi 1992; Qin 2006; Sato 1995). These included a range of reactions such as mild flushing, chills, nausea and vomiting, mild hypotension, rash, pericardial effusion, chills and noisy breathing, headache, flushing, abdominal cramping, fever, shivering, anaphylactic shock, peripheral cyanosis, hepatic dysfunction, new or worsening congestive heart failure or aortic insufficiency, pruritis, oedema and blistering, nasal congestion, cough, and erythema. No serious adverse events related to treatment were reported.
As above, we have combined data from studies following similar infusion regimens and presented all adverse effects by study in Table 4.
Two studies did not report adverse reactions (Nishihara 1988; Sakata 2007). We cannot be sure if none occurred, or if they were not recorded.
Six studies with a total of 1659 participants compared a high‐dose regimen versus a medium‐ or low‐dose regimen (described above) and reported adverse effects (Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Onouchi 1992; Qin 2006). Overall, no clear difference in the number of adverse effects was detected between regimens (OR 1.11, 95% CI 0.52 to 2.37; P = 0.78; 6 studies, 1659 participants; low‐certainty evidence). See Analysis 2.5. No differences were detected between subgroups (test for subgroup differences P = 0.93).
2.5. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 5: Adverse effects: high‐dose regimens vs medium‐ or low‐dose regimens
Two studies compared higher‐dose single‐infusion with lower‐dose single‐infusion regimens (He 2021; Qin 2006). No clear difference in incidence of adverse effects was detected between regimens (OR 1.02, 95% CI 0.14 to 7.34; P = 0.99; 2 studies, 512 participants). See Analysis 2.6.
2.6. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 6: Adverse effects: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens
Five studies investigated higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens as described above and reported adverse effects (Furusho 1991A; Harada 1989; Morikawa 1994; Onouchi 1988; Onouchi 1992). Overall, there was no clear difference detected between regimens (OR 0.98, 95% CI 0.43 to 2.22; P = 0.96; 5 studies, 1115 participants). See Analysis 2.7. No differences were detected between subgroups (test for subgroup differences P = 0.67).
2.7. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 7: Adverse effects: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens
Four studies investigated single‐infusion regimens versus multiple‐infusion regimens as described above and reported adverse effects (Barron 1990; He 2021; Newburger 1991; Sato 1995). Overall, there was no clear difference detected between regimens (OR 1.61, 95% CI 0.74 to 3.51; P = 0.23; 4 studies, 1005 participants). See Analysis 2.8. No differences were detected between subgroups (test for subgroup differences P = 0.52).
2.8. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 8: Adverse effects: single‐infusion regimens vs multiple‐infusion regimens
Acute coronary syndromes, such as MI or coronary thrombus
No study mentioned acute coronary syndromes, and we cannot be sure if this means none occurred, or if they were not reported (Barron 1990; Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Newburger 1991; Nishihara 1988; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995).
Duration of fever (days)
Four studies comparing a high‐dose regimen versus a medium‐ or low‐dose regimen (as described above) reported on duration of fever such that data could be pooled (Harada 1989; He 2021; Qin 2006; Sakata 2007). All studies reported the mean duration of fever days (± standard deviation (SD)). Harada 1989 reported the duration of fever from treatment onset in days (± SD). The remaining three studies reported mean duration of fever days (± SD) from disease onset (He 2021; Qin 2006; Sakata 2007).
Overall, duration of fever was slightly reduced with higher‐dose regimens (MD −0.71, 95% CI −1.36 to −0.06; P = 0.03; 4 studies, 992 participants; low‐certainty evidence). Heterogeneity was detected (I2 = 71%), which was reduced (I2 = 0%) following sensitivity analysis to exclude Harada 1989 (which measured duration from treatment onset) and Sakata 2007 (study protocol was to administer different additional treatments depending on the group). No differences were detected between subgroups (test for subgroup differences P = 0.10). See Analysis 2.9.
2.9. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 9: Duration of fever (days): high‐dose regimens vs medium‐ or low‐dose regimens
Morikawa 1994 reported that 194/300 (65%) participants were afebrile by 72 hours in the 200 mg/kg/day for 5 days groups compared to 121/152 (80%) in the 400 mg/kg/day for 5 days group. Nishihara 1988 did not provide data, but stated that duration of febrile stages was similar between groups during treatment. Onouchi 1992 reported that more than 50% of participants in the 200 mg/kg/day for 5 days and 400 mg/kg/day for 5 days groups were afebrile by day 2. The 100 mg/kg/day for 5 days group did not reach 50% afebrile until day 4.
Furusho 1991A did not report duration of fever.
Two studies compared higher‐dose single‐infusion with lower‐dose single‐infusion regimens and reported mean duration of fever days (± SD) from disease onset (He 2021; Qin 2006). No clear difference in incidence of adverse effects was detected between regimens (MD −0.12, 95% CI −0.68 to 0.45; P = 0.69; 2 studies, 512 participants). See Analysis 2.10.
2.10. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 10: Duration of fever (days): higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens
Two studies investigated higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens (described above) and reported mean duration of fever days (± SD) from treatment onset (Harada 1989; Onouchi 1988). Overall, no clear difference was detected between regimens (MD −0.64, 95% CI −2.88 to 1.61; P = 0.58; 2 studies, 322 participants). Heterogeneity was detected (I2 = 80%), and a difference was detected between subgroups (test for subgroup differences P = 0.02); this was likely due to the different infusion regimen doses compared in the subgroups. See Analysis 2.11.
2.11. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 11: Duration of fever (days): higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens
Four studies investigated single‐infusion regimens versus multiple‐infusion regimens (described above) and reported on duration of fever. Newburger 1991 and Sato 1995 reported mean duration of fever from enrolment (days ± SD) and treatment onset (days ± SD), respectively. He 2021 reported mean duration of fever from disease onset (days ± SD). Barron 1990 did not report the total duration of fever, instead reporting that the maximum temperature fell an average of 1.41 ˚C in the 1 g/kg single‐infusion group compared to 0.78 ˚C in the 400 mg/kg/day multiple‐infusion group between day 1 and day 2 of treatment. For Newburger 1991, we calculated SD from SE using the RevMan Web calculator. Overall, there was no clear difference between regimens (MD −0.49, 95% CI −1.42 to 0.44; P = 0.30; 3 studies, 961 participants). Heterogeneity was detected (I2 = 87%), which was not reduced by sensitivity analysis to remove each study in turn. See Analysis 2.12.
2.12. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 12: Duration of fever (days): single‐infusion regimens vs multiple‐infusion regimens
Need for additional treatment
Four studies compared a high‐dose regimen versus a medium‐ or low‐dose regimen and reported on the need for additional treatment (He 2021; Morikawa 1994; Onouchi 1992; Sakata 2007). In He 2021, resistant participants (fever persisting for more than 24 hours after completion of IVIG infusion or recrudescent fever associated with at least two symptoms of KD after an afebrile period) received a second dose of IVIG at 2 g/kg. The numbers of participants who received a second IVIG dose were 14/141 in the 2 g/kg group compared to 12/132 in the 1000 mg/kg group. In Morikawa 1994, 17/299 participants in the 200 mg/kg/day for 5 days group compared to 2/151 in the 400 mg/kg/day for 5 days group required additional treatment with further IVIG due to recrudescent or persistent fever. In Onouchi 1992, 6/57 participants in the 500 mg/kg group and 2/52 participants in the 1000 mg/kg group received additional IVIG (based on two‐dimensional echocardiography data). No participants in the 2 g/kg group received additional IVIG. In Sakata 2007, resistant participants in the 2 g/kg group were given an additional 2 g/kg of IVIG (4/54). Participants in the 1 g/kg group were given an additional 1 g/kg (26/55), then a further 2 g/kg if required (6/55). Furusho 1991A, Harada 1989, Nishihara 1988, and Qin 2006 did not report additional treatment. We cannot be sure if this means no participants needed additional treatment, or if this was not recorded.
Pooling of data from the four studies showed a reduced need for additional treatment with the high‐dose regimens compared to the medium‐ or low‐dose regimens (OR 0.29, 95% CI 0.10 to 0.88; P = 0.03; 4 studies, 1125 participants; low‐certainty evidence). No difference was detected between subgroups (test for subgroup differences P = 0.69). Heterogeneity was detected (I2 = 69%), which was no longer detected (I2 = 8%) when sensitivity analysis was undertaken by removing Sakata 2007 from the analysis, suggesting the heterogeneity was caused by including data from this study. See Analysis 2.13.
2.13. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 13: Need for additional treatment: high‐dose regimens vs medium‐ or low‐dose regimens
Two studies compared higher‐dose single‐infusion with lower‐dose single‐infusion regimens (He 2021; Sakata 2007). No clear difference was detected between groups (OR 0.26, 95% CI 0.01 to 4.80; P = 0.36; 2 studies, 382 participants). Heterogeneity was again detected (I2 = 94%), likely for the reason described above. We were unable to undertake sensitivity analysis, as only two studies were included in the analysis. See Analysis 2.14.
2.14. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 14: Need for additional treatment: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens
Two studies comparing higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens reported on the need for additional treatment (Morikawa 1994; Onouchi 1992). Our analysis showed a reduced need for additional treatment in the higher‐dose multiple‐infusion compared to the lower‐dose multiple‐infusion regimens (OR 0.24, 95% CI 0.08 to 0.70; P = 0.009; 2 studies, 615 participants). No differences were detected between subgroups (test for subgroup differences P = 0.88). See Analysis 2.15.
2.15. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 15: Need for additional treatment: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens
Onouchi 1988 compared 200 mg/kg versus 400 mg/kg regimens and reported that no additional treatment was needed in either group.
Two studies comparing single‐infusion regimens versus multiple‐infusion regimens reported on the need for additional treatment (He 2021; Newburger 1991). In Newburger 1991, 5/273 participants in the 2 g/kg single‐infusion group had additional infusion compared to 8/276 in the 400 mg/kg for 4 days group. Our analysis did not detect a clear difference in the need for additional treatment between groups (OR 1.14, 95% CI 0.38 to 3.39; P = 0.81; 2 studies, 818 participants). See Analysis 2.16.
2.16. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 16: Need for additional treatment: single‐infusion regimens vs multiple‐infusion regimens
Barron 1990 and Sato 1995 did not report on additional treatment. We cannot be sure if this means no participants needed additional treatment, or if this was not recorded.
Length of hospital stay (days)
Three studies compared a high‐dose regimen versus a medium‐ or low‐dose regimen and reported on hospital stay in days (± SD) (He 2021; Qin 2006; Sakata 2007). Our analysis did not detect a clear difference in the length of hospital stay between groups (MD −0.24, 95% CI −0.78 to 0.30; P = 0.39; 3 studies, 752 participants; low‐certainty evidence). No differences were detected between subgroups (test for subgroup differences P = 0.40). See Analysis 2.17.
2.17. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 17: Length of hospital stay (days): high‐dose regimens vs medium‐ or low‐dose regimens
Furusho 1991A, Harada 1989, Morikawa 1994, Nishihara 1988, and Onouchi 1992 did not report this outcome.
Three studies compared higher‐dose single‐infusion with lower‐dose single‐infusion regimens (He 2021; Qin 2006; Sakata 2007). Our analysis did not detect a clear difference in the length of hospital stay between groups (MD −0.36, 95% CI −1.09 to 0.37; P = 0.33; 3 studies, 621 participants). See Analysis 2.18.
2.18. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 18: Length of hospital stay (days): higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens
Onouchi 1988 did not report length of hospital stay, so we have no data to compare higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens that are not already reported above.
Four studies investigated single‐infusion regimens versus multiple‐infusion regimens, ranging from 1000 mg/kg to 2 g/kg single IVIG versus 1600 mg/kg to 2 g/kg IVIG over 2 or 4 days, and reported on hospital stay (Barron 1990; He 2021; Newburger 1991; Sato 1995).
Barron 1990 reported that participants were discharged at a median of 4 days after entry into the study in the 1 g/kg group, and at a median of 5 days in the 400 mg/kg group (P = 0.01, study author calculation). This difference at least partially reflects the fact that participants receiving the four doses required a minimum of four days of hospitalisation.
Newburger 1991 recorded that although the study protocol described 4 days of hospitalisation, 6% of participants in the 2 g/kg single‐infusion group compared to 1% of the 400 mg/kg/day for 4 days group were discharged early, the majority at day 3. Again, this must reflect that four doses required a minimum of four days of hospitalisation.
Sato 1995 only included participants scoring ≥ 4 on the Harada score and reported that the mean duration of hospital stay was 13.1 ± 6.0 days in the 2 g/kg single‐infusion group compared to 15.9 ± 7.2 days in the 400 mg/kg/day for 5 days group. It was not clear if the study authors reported SE or SD, but we have assumed these numbers to be SD. He 2021 reported that the mean ± SD of hospital stay in the 2 g/kg single‐infusion group was 8.3 ± 2.7 days compared to 8.4 ± 2.5 days in the 1000 mg/kg/day for 2 days group. We combined the data, and found no clear overall difference between single and multiple IVIG infusions (MD −1.24, 95% CI −3.86 to 1.37; P = 0.35; 2 studies, 414 participants). Heterogeneity was detected (I2 = 82%), which was likely due to the different participant characteristics (≥ 4 on Harada score). We were unable to undertake sensitivity analysis, as only two studies were included in the analysis. See Analysis 2.19.
2.19. Analysis.

Comparison 2: Primary treatment ‐ IVIG versus IVIG, Outcome 19: Length of hospital stay (days): single‐infusion regimens vs multiple‐infusion regimens
Mortality (all‐cause)
Newburger 1991 reported details on incidence of mortality, with one death in the subacute phase of the 400 mg/kg/day for 4 days group. The cause of death was a giant aneurysm. The remaining studies did not mention mortality, and although it is likely this means there were no deaths, we cannot be sure of this (Barron 1990; Furusho 1991A; Harada 1989; He 2021; Morikawa 1994; Nishihara 1988; Onouchi 1988; Onouchi 1992; Qin 2006; Sakata 2007; Sato 1995). We assessed this evidence to be of moderate certainty.
Primary treatment ‐ IVIG versus prednisolone
See Table 5.
Two studies compared IVIG with prednisolone for the treatment of KD (Nonaka 1995; Yuan 2000). Nonaka 1995 randomised participants to 400 mg/kg/day IVIG for 3 days or 2 mg/kg/day of prednisolone for 5 days then 2 mg/kg/day orally until C‐reactive protein (CRP) fell to negative. Yuan 2000 randomised participants to 1 g/kg/day IVIG for 2 days or 2 mg/kg/day intravenous methylprednisolone (IVMP) for 5 days then 2 mg/kg/day orally until CRP negative. Oral dipyridamole was administered if CAA was detected.
Incidence of CAAs
Both studies reported CAAs. Nonaka 1995 reported CAA in the acute period, 30 days, and 3 months: 7/50, 6/50, 3/41 in the IVIG group versus 10/40, 3/31, 3/31 in the prednisolone group.
Yuan 2000 reported CAA at 2 weeks, 3, 6, 9 months, and 1‐year post‐treatment: 3/25, 2/25, 1/25, 0/25 in the IVIG group versus 3/25, 1/25, 0/25, 0/25 in the IVMP group.
Overall, there was no clear difference in the incidence of CAA in the acute phase (OR 0.60, 95% CI 0.24 to 1.48; P = 0.27; 2 studies, 140 participants; very low‐certainty evidence). See Analysis 3.1. No difference was detected by the test for subgroup differences (P = 0.49).
3.1. Analysis.

Comparison 3: Primary treatment ‐ IVIG versus prednisolone, Outcome 1: CAA: total dose of IVIG vs total dose of IV prednisolone
Incidence of any adverse effects after treatment initiation
Nonaka 1995 reported that no adverse effects occurred in the prednisolone group (0/40). There was one report of mild shock and one death (2/50) in the IVIG group (OR 4.18, 95% CI 0.19 to 89.48; P = 0.36; 1 study; 90 participants; low‐certainty evidence). See Analysis 3.2. Yuan 2000 did not report adverse effects. We assessed this evidence to be of low certainty.
3.2. Analysis.

Comparison 3: Primary treatment ‐ IVIG versus prednisolone, Outcome 2: Adverse events: total dose of IVIG vs total dose of IV prednisolone
Acute coronary syndromes, such as MI or coronary thrombus
Nonaka 1995 reported one MI in the IVIG group (1/50) as a cause of death. Yuan 2000 did not report any acute coronary syndromes, but we are not certain whether none occurred or if these were not reported. We assessed this evidence to be of low certainty.
Duration of fever (days)
Nonaka 1995 reported the time to return to normal temperature after treatment started and the overall febrile period from KD onset and found a benefit of prednisolone treatment. Yuan 2000 reported the duration of fever from treatment and found no difference between groups. We pooled the time to return to normal/duration of fever from treatment onset. Overall, there was no clear difference in duration of fever (days) after treatment was started (MD 0.68, 95% CI −0.59 to 1.94; P = 0.29; 2 studies, 140 participants; very low‐certainty evidence). Considerable heterogeneity was detected (I2 = 82%), likely due to differences in study design. A difference was detected by the test for subgroup differences, but given the size of the subgroups, this should be interpreted with caution (P = 0.02). See Analysis 3.3.
3.3. Analysis.

Comparison 3: Primary treatment ‐ IVIG versus prednisolone, Outcome 3: Duration of fever (days) : total dose of IVIG vs total dose of IV prednisolone
Need for additional treatment
Neither Nonaka 1995 nor Yuan 2000 reported this outcome.
Length of hospital stay (days)
Neither Nonaka 1995 nor Yuan 2000 reported this outcome.
Mortality (all‐cause)
Nonaka 1995 reported one death in the IVIG group. Cause of death was a giant aneurysm, intracranial bleeding, and MI. Yuan 2000 did not report any deaths, but we are not certain whether none occurred or if these were not reported. We assessed this evidence to be of low certainty.
Secondary treatment ‐ IVIG versus infliximab
Four studies compared IVIG with infliximab as a secondary treatment for KD (Burns 2008; Burns 2021; Mori 2017; Youn 2016). All participants had received primary treatment of 2 g/kg IVIG but were resistant. Resistance was described as persistent fever 48 hours to 7 days, 36 to 48 hours, 24 to 36 hours, and 36 to 48 hours respectively, after initial treatment. Participants were then randomised to treatment with further IVIG (2 g/kg) or infliximab at 5 mg/kg, Burns 2008; Mori 2017; Youn 2016, or 10 mg/kg, Burns 2021.
Incidence of CAAs
All four studies reported incidence of CAA, but results were difficult to interpret as many participants had CAA at start of secondary treatment.
In Burns 2008, 24 participants were resistant to initial IVIG treatment, and 12 were randomised to 5 mg/kg infliximab and 12 to further IVIG. At baseline (start of second treatment), 3/12 in the infliximab group had CAA compared to 1/12 in the IVIG group. In total, 4/12 CAA were detected in the infliximab group compared to 1/12 in the IVIG group.
In Burns 2021, IVIG‐resistant KD patients were randomised to either further treatment with a second IVIG or 10 mg/kg infliximab. At baseline (start of second treatment), 1/50 participants in the infliximab group had CAA compared to 7/49 in the IVIG group. In total, 4/50 CAA were detected in the infliximab group compared to 1/49 in the IVIG group before receiving cross‐over treatment (or third treatment).
In Mori 2017, the number of CAA detected at the start of the second treatment was unclear. They report that CAAs were found in 1/16 participants receiving 5 mg/kg infliximab (6.3%) and 3/15 participants receiving IVIG (20.0%) through to day 21. No participant had a new CAA after day 21. Mori 2017 reports that no difference in the Z max score (largest of the right coronary artery, left main coronary artery, left anterior descending artery, and left circumflex coronary artery internal diameters) was detected in participants who were evaluated for coronary artery internal diameters (Z‐score) after the start of treatment to day 56 between the infliximab group and the IVIG group.
In Youn 2016, 43 patients who were resistant to initial IVIG treatment were randomised to either a further 2 g/kg IVIG or 5 mg/kg infliximab. No CAA was detected at the start of the second treatment. CAAs developed in 4/32 participants retreated with IVIG and in 1/11 participants treated with infliximab.
Overall, there was no clear difference in the incidence of CAA between the IVIG and infliximab groups (OR 1.31, 95% CI 0.46 to 3.74; P = 0.62; 4 studies, 197 participants). See Analysis 4.1. We have presented data by the total infliximab dose as subgroups. No difference was detected by the test for subgroup differences (P = 0.60).
4.1. Analysis.

Comparison 4: Secondary treatment ‐ IVIG versus infliximab, Outcome 1: CAA: total dose of single IVIG vs single infliximab
Incidence of any adverse effects after treatment initiation
All four studies reported adverse effects (Burns 2008; Burns 2021; Mori 2017; Youn 2016).
Burns 2008 reported that 5 participants (3 infliximab, 2 IVIG) experienced one or more serious adverse events (SAEs). No SAEs were related to the study medication. Eighteen participants (9 infliximab, 4 IVIG, 1 infliximab cross‐over to IVIG, and 4 IVIG cross‐overs to infliximab) experienced one or more adverse events (AEs) attributable to KD (including eczema, CAA, diastolic dysfunction, and pericardial effusion), but it was not clear in which group these occurred. Ten participants experienced 18 AE not attributable to KD: 5 participants were treated with infliximab, 1 with IVIG, 3 with IVIG followed by infliximab, and 1 with infliximab followed by IVIG. Of these AEs, only transient hepatomegaly was deemed possibly related to study drug infusion; 5/12 participants who received infliximab and 1/12 who received IVIG experienced this AE.
Burns 2021 reported 45 adverse events in the infliximab group and 65 adverse events in the second IVIG group: 24/54 participants in the infliximab group and 33/49 participants in the second IVIG group experienced at least one adverse event. There were a total of 51 SAEs: 15/54 in the infliximab group and 36/49 in second IVIG group; 10/54 participants in the infliximab group and 27/49 in the second IVIG group experienced at least one SAE. SAEs that were deemed definitely or likely related to study treatment were experienced by 0/54 participants who received only infliximab and 9/58 participants who received IVIG as either their first or second study treatment; in all nine participants the SAE experienced was haemolytic anaemia.
Mori 2017 reported that AEs occurred in 15/16 participants in the infliximab group and 15/15 participants in the IVIG group. Adverse drug reactions (anti‐double stranded DNA (anti‐dsDNA), rash, and neuralgia) occurred in 11/16 participants in the infliximab group and 10/15 participants in the IVIG group. There were no discontinuations due to AEs. There was one serious AE (relapse of KD) in an IVIG‐treated participant. Infusion reactions were reported in 0/16 infliximab and 2/15 IVIG‐treated participants. In participants with elevated anti‐dsDNA antibodies, this decreased to normal levels by the end of the trial and in participants who were followed after completion of the trial. Lupus‐like syndrome was not observed in any participant.
Youn 2016 reported that no serious AEs such as anaphylactoid reaction, severe infections, or heart failure were observed. In the IVIG group, 5/32 participants experienced infusion reaction defined as fever with or without chill that requires transient interruption of infusion. In the infliximab group, 1/11 participants experienced skin rash developed during infusion.
Overall, there was no clear difference in the incidence of AE between the IVIG and infliximab groups (OR 1.13, 95% CI 0.35 to 3.61; P = 0.84; 4 studies, 201 participants). See Analysis 4.2. We have presented data by the total infliximab dose as subgroups. No difference was detected by the test for subgroup differences (P = 0.09).
4.2. Analysis.

Comparison 4: Secondary treatment ‐ IVIG versus infliximab, Outcome 2: Adverse effects: total dose of single IVIG vs single infliximab
Acute coronary syndromes, such as MI or coronary thrombus
Burns 2008, Burns 2021, and Mori 2017 did not report acute coronary syndromes, and Youn 2016 stated that no SAEs such as heart failure were observed.
Duration of fever (days)
All four studies reported on duration of fever but in different ways (Burns 2008; Burns 2021; Mori 2017; Youn 2016), preventing data pooling. We have reported the results narratively below.
Burns 2008 reported the median area (and range) under temperature curve (AUC) as 1331 (1286 to 1367) in the IVIG group compared to 1333 (1313 to 1354) in the infliximab group. The study authors reported that 1/12 participants had 2 days of fever in the infliximab‐treated group; 2/12 participants had 2 days of fever in the second IVIG‐treated group; and 2/12 participants had > 2 days of fever post‐study drug administration. Participants who did not respond to treatment were crossed over to receive the second treatment. The study authors reported that the participants who crossed over had a higher AUC than those who did not cross over (P = 0.003).
Burns 2021 reported the mean (± SD) days of fever from enrolment as 1.5 (± 1.4) days in the infliximab group versus 2.5 (± 2.5) days in the IVIG group (P = 0.014). They also reported resolution of fever within 24 hours of treatment and no recurrence within 7 days in 40/52 (77%) participants in the infliximab group compared to 25/49 (51%) in the IVIG group.
Mori 2017 reported the median febrile period from start of treatment was 16 hours in the infliximab group compared to 56.1 hours in the IVIG group (no range provided). They also reported that the defervescence rate within 48 hours was greater in the infliximab group (76.7%, 95% CI 56.6 to 96.7%) compared to the IVIG group (37.0%, 95% CI 11.9 to 62.1%; P = 0.02).
Youn 2016 reported the median duration of fever and range was 6 hours (1 to 30 hours) in the infliximab group compared to 17 hours (1 to 154 hours) in the IVIG group (P = 0.044). Defervescence occurred within 24 hours in 9/11 (81.8%) participants treated with infliximab and in 18/32 (56.3%) retreated with IVIG (P = 0.098).
Need for additional treatment
All four studies reported on the need for additional treatment (Burns 2008; Burns 2021; Mori 2017; Youn 2016).
In Burns 2008, fever resolved in 1/12 participants who did not respond to infliximab after crossing over to IVIG. From the IVIG group, 4/12 participants required additional infliximab, and two of these went on to receive further treatment with steroids.
In Burns 2021, 9/52 participants in the infliximab group crossed over to IVIG, and 22/49 in the IVIG group crossed over to the infliximab group. Six participants with persistent fever (4/22 who received infliximab and 2/9 who received second IVIG as their cross‐over treatment) were then further treated with either ciclosporin or steroids at the discretion of the treating physician.
Mori 2017 reported that 5/16 participants in the infliximab group and 9/15 in the IVIG group were switched to another treatment (at physician's discretion) due to worsening KD.
Youn 2016 reported that 11/32 participants in the IVIG group required additional treatment (7 IVMP and 4 crossed to infliximab) compared to 1/11 in the infliximab group who crossed over to IVIG.
We were able to combine these data. Overall, fewer participants receiving infliximab required further (tertiary) treatment (OR 3.99, 95% CI 1.98 to 8.02; P < 0.001; 4 studies, 199 participants). See Analysis 4.3. We have presented data by the total infliximab dose as subgroups. No difference was detected by the test for subgroup differences (P = 0.94).
4.3. Analysis.

Comparison 4: Secondary treatment ‐ IVIG versus infliximab, Outcome 3: Need for additional treatment: total dose of single IVIG vs single infliximab
Length of hospital stay (days)
Presentation of the data for this outcome in the different studies precluded data pooling. We have reported the results narratively below.
Burns 2021 reported the mean ± SD days in hospital from randomisation in the infliximab group as 3.2 ± 2.1 days compared to 4.5 ± 2.5 days in the IVIG group (P < 0.001).
Youn 2016 reported the median number (and range) of days in hospital as 8 days (6 to 12) in the infliximab group compared to 10 days (6 to 14) in the IVIG group (P = 0.046).
Length of hospital stay was not reported by Burns 2008 or Mori 2017.
Mortality (all‐cause)
Burns 2021 reported that no deaths occurred. Burns 2008, Mori 2017, and Youn 2016 did not report incidence of mortality; although this likely means there were no deaths, we cannot be sure of this.
Secondary treatment ‐ IVIG versus prednisolone
Two studies compared IVIG with prednisolone as secondary treatment for KD (Miura 2008; Wang 2020). All participants received primary treatment of 2 g/kg IVIG but were resistant. Resistance was described as recrudescent or persistent fever 36 or 48 hours after initial IVIG infusion, respectively (Miura 2008; Wang 2020). Participants were then randomised to treatment with further IVIG (2 g/kg) or IVMP at 30 mg/kg/day for 3 days, Miura 2008, or intravenous methylprednisolone pulse therapy (MPT) at 15 mg/kg/day for 3 days, Wang 2020.
Incidence of CAAs
Both studies reported incidence of CAA (Miura 2008; Wang 2020). Results for these studies were difficult to interpret as many participants had CAA at start of secondary treatment.
Overall, there was no clear difference in the incidence of CAA between the IVIG and prednisolone groups (OR 0.46, 95% CI 0.02 to 9.18; P = 0.61; 2 studies, 75 participants). See Analysis 5.1. We have presented data by the total prednisolone dose as subgroups. No difference was detected by the test for subgroup differences (P = 0.1).
5.1. Analysis.

Comparison 5: Secondary treatment ‐ IVIG versus prednisolone, Outcome 1: CAA: single IVIG vs multiple prednisolone
In Miura 2008, 22 participants resistant to initial IVIG treatment received secondary treatment with either IVIG or IVMP. Coronary artery dimensions and the prevalence of CAA were similar in the two groups (IVMP 2/11 versus IVIG 3/11). It is not clear at what time point the CAAs were assessed or if they were present at baseline. Miura 2008 was halted prematurely due to adverse events following IVMP infusion.
In Wang 2020, 80 IVIG‐resistant patients were randomised to either IVIG or MPT, and 33/80 had CAA before secondary treatment. They reported CAA at 7 days and 1, 3, 6, 12, and 24 months. No dropouts were CAA‐positive. The numbers of CAA in the IVIG group compared to the MPT group at each time point were as follows: 7 days: 15/40 versus 18/40; 1 month: 8/39 versus 10/40; 3 months: 4/39 versus 3/39; 6 months: 2/35 versus 4/36; 12 months: 0/28 versus 4/25; 24 months: 0/18 versus 4/15). Fewer participants returned for follow‐up ECGs as time progressed.
Incidence of any adverse effects after treatment initiation
Presentation of the data for this outcome in the different studies precluded data pooling. We have reported the results narratively below.
Miura 2008 was halted prematurely due to adverse events following IVMP infusion. The study authors reported increased sinus bradycardia (P = 0.01) and hyperglycaemia (P = 0.01) in the IVMP group. All adverse effects were transient. There were no convulsions, gastrointestinal symptoms, infection, or malignant arrhythmia.
Wang 2020 reported that 5/40 participants in the MPT group developed bradycardia and that there were no adverse reactions in the IVIG group (0/40) (OR 0.08, 95% CI 0.00 to 1.49; P = 0.09; 1 study, 80 participants). See Analysis 5.2.
5.2. Analysis.

Comparison 5: Secondary treatment ‐ IVIG versus prednisolone, Outcome 2: Adverse effects: IVIG vs multiple prednisolone
Acute coronary syndromes, such as MI or coronary thrombus
Miura 2008 reported that there were no embolisms in either group. Wang 2020 did not report any acute coronary syndromes, meaning it is likely that none occurred.
Duration of fever (days)
Presentation of the data for this outcome in the different studies precluded data pooling. We have reported the results narratively below.
Miura 2008 reported that the proportion of febrile participants was lower in the IVMP group compared to the IVIG group until day 3 (1/11 versus 8/11; P < 0.001), but not on or after day 4 (6/11 versus 6/11). Miura 2008 also reported that the mean (SD) minimum body temperature (˚C) at 72 hours after treatment started in IVMP was 35.4˚C (± 0.4) compared to 36.1˚C (± 0.5) in the IVIG group (P = 0.002). Given the data on the proportion of febrile participants, it is likely this difference disappeared after 72 hours.
Wang 2020 reported that the mean (± SD) duration of fever (≥ 38˚C) after additional treatment was 11 ± 6.3 hours in the MPT group compared to 18 ± 4.4 hours in the IVIG group (P < 0.05).
Need for additional treatment
Miura 2008 did not report if any participants required additional treatment. Wang 2020 reported that 4/40 participants in the IVIG group required readmission compared to 11/40 in the MPT group. The same four participants resistant to second IVIG crossed over to MPT or received third‐line IVIG. Those not responsive to MPT received either oral methylprednisolone or IVIG.
Length of hospital stay (days)
Length of hospital stay was not reported by Miura 2008 or Wang 2020.
Mortality (all‐cause)
Miura 2008 reported that there were no sudden deaths in either group. Wang 2020 did not report any deaths, meaning it is likely that none occurred.
Tertiary treatment ‐ IVIG versus prednisolone
One study compared IVIG with prednisolone for the tertiary treatment of KD (Hashino 2001). Hashino 2001 randomised 17 participants who did not respond to initial IVIG 2 g/kg or secondary IVIG 1 g/kg treatment for KD to either a third dose of IVIG 1 g/kg or IVMP at 20 mg/kg/day for 3 days within the acute phase.
Incidence of CAAs
At baseline (before third‐line therapy), 4/17 participants had CAA (2 in each group). During the acute phase, CAA was detected in 5/8 participants in the IVIG group (2 giant aneurysms, 3 small aneurysms, 3 intact coronary arteries) and 7/9 in the IVMP group (2 giant aneurysms, 2 small aneurysms, 3 transient dilations, 2 intact coronary arteries). Given the small numbers in each group, our analysis detected no difference (OR 0.48, 95% CI 0.06 to 3.99; P = 0.49; 1 study, 17 participants). See Analysis 6.1.
6.1. Analysis.

Comparison 6: Tertiary treatment ‐ IVIG versus prednisolone, Outcome 1: CAA: IVIG vs prednisolone
Incidence of any adverse effects after treatment initiation
Hashino 2001 did not report adverse events, so we cannot be certain whether any occurred.
Acute coronary syndromes, such as MI or coronary thrombus
Hashino 2001 did not report acute coronary syndromes, so we cannot be certain whether any occurred.
Duration of fever (days)
Hashino 2001 reported the duration of fever (> 38.5 °C) after retreatment. In the IVIG group, the mean (± SD) duration was 4.8 ± 0.7 days compared to 1.4 ± 0.7 days in the IVMP group. Analysis suggests fever duration is reduced with IVMP treatment compared to a third dose of IVIG (MD 3.40, 95% CI 2.73 to 4.07; P < 0.001; 1 study, 17 participants). See Analysis 6.2.
6.2. Analysis.

Comparison 6: Tertiary treatment ‐ IVIG versus prednisolone, Outcome 2: Duration of fever (days): IVIG vs prednisolone
Need for additional treatment
Hashino 2001 did not report on additional treatment.
Length of hospital stay (days)
Hashino 2001 did not report on the length of hospital stay.
Mortality (all‐cause)
Hashino 2001 did not report on mortality.
Additional subgroup analyses
We performed additional analyses to investigate CAA incidence by geographic distribution unless data for CAA incidence were only provided by studies from one country. Using the test for subgroup differences, we found no differences between countries for CAA incidence for the comparisons IVIG versus ASA (P = 0.17, see Analysis 7.1). For IVIG versus IVIG CAA: high‐dose versus medium‐ or low‐dose regimens (Analysis 2.1) included Chinese and Japanese studies, and subgrouping by geographical distribution did not indicate any differences (P = 0.66, see Analysis 8.1). For high‐dose single‐infusion versus lower‐dose single‐infusion regimens, subgrouping Analysis 2.2 by geographical distribution did not indicate any differences (P = 0.61, see Analysis 8.2). For higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens, only Japanese studies provided data, and no further subgrouping was carried out. For single‐infusion versus multiple‐infusion regimens, subgrouping Analysis 2.4 by geographical distribution did not indicate any difference (P = 0.15, see Analysis 8.3).
7.1. Analysis.

Comparison 7: Additional subgroup analysis: primary treatment ‐ IVIG (and ASA) versus ASA, Outcome 1: Analysis 1.1 subgrouped by geographic distribution
8.1. Analysis.

Comparison 8: Additional subgroup analysis: primary treatment ‐ IVIG versus IVG, Outcome 1: Analysis 2.1.1 subgrouped by geographical distribution
8.2. Analysis.

Comparison 8: Additional subgroup analysis: primary treatment ‐ IVIG versus IVG, Outcome 2: Analysis 2.2 subgrouped by geographical distribution
8.3. Analysis.

Comparison 8: Additional subgroup analysis: primary treatment ‐ IVIG versus IVG, Outcome 3: Analysis 2.4 subgrouped by geographical distribution
When splitting participants between subgroup analyses, if groups contained an uneven number of participants so that numbers could not be equally divided, we carried out the analysis in both ways to detect possible differences in the results caused by an unequal division of the numerator and denominator. This did not cause a significant change in size or direction of effect in any analysis.
Sensitivity analysis
As planned, we undertook sensitivity analyses to exclude studies at high risk of selection bias. This included analyses with data provided by Matsushima 1985, Nagashima 1987, or Yuan 2000.
Analysis 1.1: there was no change in overall direction or size of effect for CAA incidence (up to 30 days) in IVIG versus ASA (OR 0.66, 95% CI 0.44 to 0.98; P = 0.04).
Analysis 1.3: there was no change in overall direction or size of effect for adverse events in IVIG versus ASA (OR 0.48, 95% CI 0.13 to 1.73; P = 0.26).
Analysis 1.4: there was no change in overall direction or size of effect for duration of fever from treatment in IVIG versus ASA (MD −2.60, 95% CI −4.48 to −0.73; P = 0.007).
Analysis 1.5: there was no change in overall direction or size of effect for duration of fever from KD onset in IVIG versus ASA (MD −0.80, 95% CI −1.50 to −0.11; P = 0.02).
Analysis 3.1: there was no change in overall direction or size of effect for CAA incidence in IVIG versus prednisolone (OR 0.49, 95% CI 0.17 to 1.43; P = 0.19).
Analysis 3.3: there was a change in effect to show a possible benefit of prednisolone for duration of fever in IVIG versus prednisolone (MD 1.40, 95% CI 0.42 to −2.38; P = 0.005).
We carried out sensitivity analysis on incidence of CAA where analyses included data from studies that were at high risk of detection bias (cardiac outcomes). This included analyses with data from Burns 2008, Furusho 1984, Furusho 1991A, Furusho 1991B, Matsushima 1985, Miura 2008, Nagashima 1987, Nonaka 1995, Qin 2006, Wang 2020, Youn 2016, or Yuan 2000.
Analysis 1.1: there was no longer a difference in incidence of CAA between groups (up to 30 days) in IVIG versus ASA (OR 0.78, 95% CI 0.51 to 1.19; P = 0.24).
Analysis 1.2: there was no change in overall direction or size of effect for CAA incidence (over 6 months) in IVIG versus ASA (OR 0.88, 95% CI 0.49 to 1.56; P = 0.66).
Analysis 2.1: there was no change in overall direction or size of effect for CAA incidence high‐dose regimens versus medium‐ or low‐dose regimens (OR 0.5, 95% CI 0.30 to 0.82; P = 0.007). A difference was detected between subgroups (test for subgroup differences P = 0.01).
Analysis 2.2: there was no change in overall direction or size of effect for CAA incidence higher‐dose single‐infusion versus lower‐dose single‐infusion regimens (OR 1.01, 95% CI 0.58 to 1.79; P = 0.96).
Analysis 2.3: there was no change in overall direction or size of effect for CAA incidence higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens (OR 0.41, 95% CI 0.28 to 0.61; P < 0.001).
Analysis 3.1: both studies reporting on CAA incidence after treatment with IVIG versus prednisolone were excluded, so no longer estimable.
Analysis 4.1: there was no change in overall direction or size of effect for CAA incidence in IVIG versus infliximab (OR 2.04, 95% CI 0.70 to 5.95; P = 0.19).
Analysis 5.1: both studies reporting on CAA incidence after secondary treatment with IVIG versus prednisolone were excluded, so no longer estimable.
We carried out sensitivity analysis on incidence of CAA where analyses included data from studies lacking a clear description of the criteria used to diagnose KD. This included analyses with data from Miura 2008, Nagashima 1987, Nishihara 1988, Nonaka 1995, Okuni 1987A, Okuni 1987B, or Sakata 2007.
Analysis 1.1: there was no change in overall direction or size of effect for CAA incidence (up to 30 days) in IVIG versus ASA (OR 0.60, 95% CI 0.37 to 0.97; P = 0.04).
Analysis 1.2: there was no change in overall direction or size of effect for CAA incidence (over 6 months) in IVIG versus ASA (OR 0.68, 95% CI 0.37 to 1.26; P = 0.22).
Analysis 2.1: the overall effect for CAA incidence high‐dose regimens versus medium‐ or low‐dose regimens now includes both possible benefit and harm (OR 0.62, 95% CI 0.38 to 1.02; P = 0.06).
Analysis 2.2: there was no change in overall direction or size of effect for CAA incidence higher‐dose single‐infusion versus lower‐dose single‐infusion regimens (OR 0.92, 95% CI 0.59 to 1.45; P = 0.72).
Analysis 2.3: there was no change in overall direction or size of effect for CAA incidence higher‐dose multiple‐infusion versus lower‐dose multiple‐infusion regimens (OR 0.47, 95% CI 0.30 to 0.73; P = 0.001).
Analysis 3.1: there was no change in overall direction or size of effect for CAA incidence in IVIG versus prednisolone (OR 1.00, 95% CI 0.18 to 5.51; P = 1.00).
Analysis 5.1: there was no change in overall direction or size of effect for CAA incidence after secondary treatment with IVIG versus prednisolone (OR 0.08, 95% CI 0.00 to 1.64; P = 0.1).
Discussion
We identified 31 randomised controlled trials (RCTs) involving a total of 4609 participants with Kawasaki disease (KD) that compared intravenous immunoglobulin (IVIG) with either acetylsalicylic acid (ASA), another dose or regimen of IVIG, prednisolone, or infliximab. Most studies had at least one domain at high risk of bias (blinding of participants and personnel, or blinding of outcome assessment (cardiac or non‐cardiac outcomes, or both)), and detailed descriptions of the randomisation process were infrequently provided. See Table 1; Table 3; and Table 5.
Summary of main results
Primary treatment with IVIG compared to ASA for people with KD
Compared to ASA, IVIG probably reduces the incidence of coronary artery abnormalities (CAA) in people with KD. The individual studies reported a range of adverse effects, but there was little to no difference in numbers of these between groups. Evidence for incidence of acute coronary syndromes was limited, so we are uncertain of any effects. Duration of fever was probably shorter in the IVIG group, but there was little or no difference between groups in need for additional treatment. No study reported on length of hospital stay, and there was little to no difference between groups in mortality.
Primary treatment with IVIG compared to different infusion regimens of IVIG for people with KD
We considered a high dose to be more than 1900 mg/kg total IVIG; medium to be 1900 mg/kg to 900 mg/kg total IVIG; and low to be less than 900 mg/kg total IVIG (Ae 2020; Ae 2021). Probably fewer CAA occurred in participants treated with higher‐dose IVIG regimens compared to medium‐ or lower‐dose IVIG regimens. There was little to no difference in CAA incidence between higher‐dose single‐infusion and lower‐/medium‐dose single‐infusion regimens. Likely fewer CAA were detected in higher‐dose multiple‐infusion regimens compared to lower‐dose multiple‐infusion regimens. No clear differences were detected between single‐infusion and multiple‐infusion regimens. There was little to no difference in number of adverse effects between groups irrespective of the regimens compared. No study reported on acute coronary syndromes. Higher‐dose IVIG may reduce the duration of fever compared to medium‐ or lower‐dose regimens. No differences in duration of fever were detected between high‐dose versus medium‐dose single infusions, multiple infusions, or single‐ versus multiple‐infusion regimens. Higher‐dose regimens may reduce the need for additional treatment. We did not detect a difference in length of hospital stay between infusion regimens, and it is likely that there is little to no difference in mortality.
Primary treatment with IVIG compared to prednisolone for people with KD
The evidence for the comparison IVIG versus prednisolone on incidence of CAA is very uncertain, and there was little to no difference between groups in adverse effects, acute coronary syndrome, and mortality. No study reported the need for additional treatment or length of hospital stay. We are very uncertain of the impact on duration of fever, as two studies reported the duration differently and had conflicting results.
Secondary treatment with IVIG compared to infliximab for people with KD
We did not detect a clear difference in CAA incidence between groups treated with IVIG or infliximab following resistance to initial treatment with IVIG. Some participants had CAA at the start of secondary treatment. Similarly, no clear differences in the number of adverse effects were detected. Limited data were available for acute coronary syndromes and duration of fever, which prevented us from drawing any conclusions. Analysis indicated that there may be a reduced need for further (tertiary) treatment in the infliximab group. Given that the participants in this analysis were IVIG resistant, this is not surprising. We are unable to draw any conclusions about length of hospital stay because of differences in outcome reporting between studies. It is likely there were no deaths in either group.
Secondary treatment with IVIG compared to prednisolone for people with KD
We did not detect a clear difference in CAA incidence between groups treated with IVIG or prednisolone following resistance to initial treatment with IVIG. Some participants had CAA at the start of secondary treatment. One study was halted due to adverse effects in the prednisolone group, and the second study reported increased events in the prednisolone group. Data for acute coronary syndromes were limited, and we could not pool data for duration of fever, though both studies reported a shorter fever duration in the prednisolone group. One study reported that fewer participants required additional (tertiary) treatment in the IVIG group. Length of hospital stay was not reported, and no deaths were reported.
Tertiary treatment with IVIG compared to prednisolone for people with KD
One study investigated IVIG compared to prednisolone in participants who were resistant to both initial and secondary IVIG treatment. Evidence was limited, and no clear differences between groups in CAA incidence were detected. The study authors reported that duration of fever was reduced in the prednisolone group; however, this result should be interpreted with caution given the study limitations. No other outcomes of interest were reported.
Overall completeness and applicability of evidence
We have attempted to find all available published and unpublished randomised trials for the use of IVIG in people with KD. We included a total of 31 studies in quantitative synthesis, and we believe that the included trials are comprehensive. However, it should be noted that we were not able to obtain data for all outcomes defined in this systematic review.
As we restricted our inclusion criteria to evidence provided by RCTs, the identified studies provided a low overall number of events, and outcomes tended not to be reported for later time points, as study durations were generally short. We identified a variety of comparisons using a range of doses, recording different time points and reporting different outcomes. Specific details on baseline measurements of outcomes, for example CAA, were not always provided. These factors limit the applicability and completeness of our findings, as we are not accounting for the large amount of non‐randomised evidence gathered by long‐term cohort studies such as the Kawasaki Disease Nationwide Survey (Ae 2021).
Primary treatment
The available evidence indicates that high‐dose IVIG regimens are associated with a low risk of CAA formation, need for additional therapy, and prolonged duration of fever. This suggests that high‐dose IVIG regimens would be beneficial compared to medium‐ or low‐dose IVIG regimens, which are superior to ASA regimens. There were no clinically significant differences in incidence of adverse events between groups, which suggests there is little concern about the safety of IVIG. Regarding acute coronary syndromes and mortality, we could not find signals of effectiveness because the number of events was rarely observed during the observation period of the trials.
Secondary or tertiary treatment
We found no clear evidence to support the effectiveness of IVIG compared to infliximab or prednisolone for the incidence of CAA, adverse effects, duration of fever, length of hospital stay, acute coronary syndrome, or mortality due to lack of sufficient statistical power in the obtained data.
Quality of the evidence
Primary treatment with IVIG compared to ASA for people with KD
See Table 1.
For the outcome CAA, we downgraded the certainty of the evidence by one level to moderate, as four studies included in the analysis were at high risk of bias (selection, performance, detection of cardiac outcomes, or reporting bias), and sensitivity analysis to exclude those studies at high risk of detection bias caused a change in effect size. For adverse effects, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (six studies were at high risk of selection, performance, or detection of non‐cardiac outcomes bias), one level for inconsistency (heterogeneity was high: I2 = 73%), and one level for imprecision (confidence intervals include appreciable benefit or harm) to very low. For acute coronary syndromes, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (one study at high risk of selection/detection bias) and one level for imprecision (small numbers of events and participants, and confidence intervals include appreciable benefit or harm) to low. For duration of fever, we downgraded the certainty of the evidence by a total of one level due to concerns related to risk of bias (three studies were at high risk of selection/performance/detection bias) and imprecision (small number of participants) to moderate. For the outcome need for additional treatment, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (two studies at high risk of selection/detection of non‐cardiac outcomes bias) and one level for imprecision (small numbers of participants and events, and confidence intervals include appreciable benefit or harm) to low. No studies reported length of hospital stay, preventing an assessment of the certainty of the evidence. For mortality, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (two studies at high risk of selection/detection bias) and one level for imprecision (small numbers of participants and events) to low.
Primary treatment with IVIG compared to different infusion regimens of IVIG for people with KD
See Table 3.
For CAA, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (two studies at high risk of detection of cardiac outcomes or performance bias) to moderate. For adverse effects, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (five studies at high risk of detection of non‐cardiac outcomes or performance bias, or both) and one level for imprecision (small numbers of events, and confidence intervals include appreciable benefit or harm) to low. No studies reported acute coronary syndromes, preventing an assessment of the certainty of the evidence. For duration of fever, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (three studies at high risk of detection of non‐cardiac outcomes) and one level for inconsistency (I2 = 71%) to low. Sensitivity analysis indicated that this was explained by study differences (reporting from KD onset or treatment onset). For need for additional treatment, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (two studies at high risk of detection of cardiac outcomes or performance bias) and one level for inconsistency (I2 = 69%) to low. For length of hospital stay, we downgraded the certainty of the evidence by a total of two levels to low due to concerns related to risk of bias and imprecision (confidence intervals include appreciable benefit or harm) to low. For mortality, we downgraded the certainty of the evidence by one level due to imprecision (small number of events reported) to moderate.
Primary treatment with IVIG compared to prednisolone for people with KD
See Table 5.
For CAA, we downgraded the certainty of the evidence by two levels due to concerns related to risk of bias (both studies at high risk of selection/detection bias) and one level for imprecision (small numbers of participants) to very low. For adverse effects, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (study at risk of detection of non‐cardiac outcome bias) and one level for imprecision (small numbers of events and participants, and wide confidence interval) to low. For acute coronary syndrome, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (study at high risk of detection bias) and one level for imprecision (small numbers of events and participants) to low. For duration of fever, we downgraded the certainty of the evidence by one level due to concerns related to risk of bias (both studies at high risk of selection or detection bias), one level for inconsistency (I2 = 82%), and one level for imprecision (small numbers of participants) to very low. Need for additional treatment and length of hospital stay were not reported for this comparison. For mortality, we downgraded the certainty of the evidence by one level for risk of bias and one level for imprecision (small numbers of events and participants) to low.
Potential biases in the review process
We followed standard Cochrane procedures when developing the protocol for this review and in conducting the review. We attempted to contact the study authors where possible to obtain further information. We included studies irrespective of language. We identified additional studies in reference lists of reviews that had not been detected by our searches. These studies have been placed in awaiting classification until we are able to confirm that they meet the inclusion criteria of this Cochrane Review. It is possible that not including data from these studies has impacted the overall review findings. We decided to pool studies that evaluated different doses of treatments using subgroup analysis. We used subgroups for high‐/medium‐/low‐dose IVIG groups, as they represent clinically relevant regimens and allowed important comparisons to be investigated. We decided to include all adverse effects reported by studies in the data analyses, even though studies likely had different definitions of what an adverse effect was. We believe any bias overall would have been minimal, and any differences between treatment groups in individual studies would have been detected. We were limited in only including data from RCTs, and no large‐scale randomised studies have been carried out. This makes detection of rare events unlikely and decreased our confidence in the review findings. As discussed below, further evidence is available from large epidemiological studies.
Agreements and disagreements with other studies or reviews
This review replaces an earlier Cochrane Review (Oates‐Whitehead 2003). Our findings are in agreement with that review. We have included data from more recent studies and widened the scope to include studies also comparing IVIG with tumour necrosis factor‐alpha blockers and corticosteroids, which reflects current clinical options. This review indicates that high‐dose IVIG regimens are probably effective in preventing the formation of CAAs up to 30 days. In Japan, the nationwide survey of Kawasaki disease, which includes more than 90% of new KD patients, has been ongoing since 1970. Based on the latest Kawasaki Disease Nationwide Survey (Ae 2021), chronological changes in the proportion of KD patients treated with IVIG by dose regimens and incidences of CAAs are shown in Figure 4. The chronological trend based on large epidemiological studies shows clearly an inverse relationship between a decrease in CAAs and an increase in the proportion of IVIG administration, especially IVIG 2 g/kg single‐infusion regimen. In the 1980s, most KD patients were treated with ASA alone, and 16% to 18% of KD patients had CAAs. In the early 1990s, more than 80% of KD patients received low‐ to medium‐dose IVIG multiple‐infusion regimens, and the incidence of CAAs decreased to approximately 12%. Since the late 1990s, IVIG had been replaced by 2 g/kg single infusion, and the incidence of CAAs decreased to approximately 4% in the 2000s. Based on these data, the incidence of CAAs decreased by approximately 30% from the ASA era to the low‐ to medium‐dose IVIG era, and then by approximately 60% in the high‐dose IVIG era. The results from this review showed an odds ratio (OR) of 0.60 (95% confidence interval (CI) 0.41 to 0.87) for ASA regimens versus IVIG regimens and an OR of 0.60 (95% CI 0.40 to 0.89) for high‐dose IVIG regimens versus low‐ or medium‐dose IVIG regimens. Based on these findings, the evidence for the preventive effect of IVIG on CAAs is robust and reproducible in large epidemiological studies. Several recent guidelines recommend high‐dose IVIG single infusion as the primary treatment for acute KD (de Graeff 2019; McCrindle 2017; Miura 2021).
4.
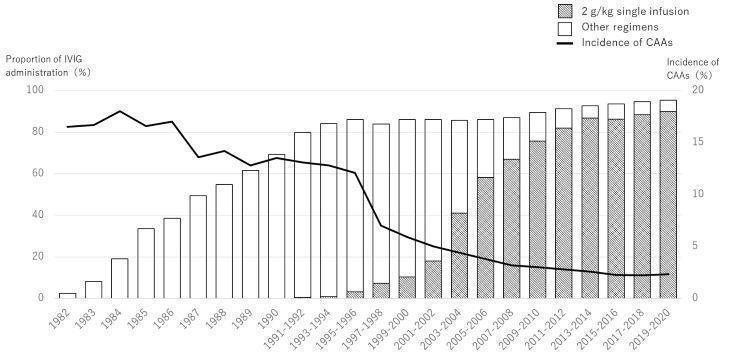
Chronological changes of proportion of intravenous immunoglobulin (IVIG) administration and incidence of coronary artery abnormalities (CAAs) from the Nationwide Survey of Kawasaki Disease in Japan. Created by review author (TK) with data from the Nationwide Survey (with permission from the Director of the Nationwide Survey Kawasaki Disease in Japan).
In this review, we could not show an association between IVIG and mortality because of the short observation period of the clinical trial and the few events that occurred. The National Kawasaki Disease Study has continuously investigated the mortality of people with KD since 1967 and found that mortality was about 2% in the 1960s, 0.8% in the 1970s, 0.2% in the 1980s, 0.1% in the 1990s, 0.04% in the 2000s, and 0.02% in the 2010s (Ae 2021). The rate of death has been declining at a rate of about half a per cent per decade. It is reasonable to assume that the reduction in mortality rates observed in these large observational studies is related to the widespread use of immunoglobulins.
With regard to need for additional treatment, adverse effects, and duration of fever, no large‐scale epidemiological studies have been conducted continuously since the 1980s, therefore it is difficult to compare the association between IVIG and these effects on the basis of large studies.
Authors' conclusions
Implications for practice.
Our findings are in keeping with current guideline recommendations. The strength of our conclusions is limited by restricting to randomised controlled trial (RCT) data. The included RCTs investigated a variety of comparisons, and the small number of events observed during the study periods limited the detection of effects. The available evidence indicated that high‐dose intravenous immunoglobulin (IVIG) regimens are probably associated with a reduced risk of coronary artery abnormalities (CAAs) formation compared to acetylsalicylic acid (ASA) or medium‐ or low‐dose IVIG regimens. Incidence of adverse events did not show clinically significant differences, which suggests there is little concern about the safety of IVIG. Compared to ASA, high‐dose IVIG probably reduced duration of fever, but there was little or no difference detected in the need for additional treatment. Compared to medium‐ or low‐dose IVIG, there may be reduced duration of fever and reduced need for additional treatment. We were unable to draw any conclusions regarding acute coronary syndromes, mortality, and length of hospital stay. We were also unable to determine any effects when comparing IVIG treatment with tumour necrosis factor (TNF)‐blockers or corticosteroids, or in people who were resistant to initial IVIG treatment.
Implications for research.
Although we included 31 RCTs in the review, we found limited short‐ and long‐term RCT evidence for most outcomes, especially acute coronary syndromes, mortality, and length of hospital stay. Further well‐designed RCTs would both provide missing evidence and strengthen our certainty in the effects detected. This is the case for IVIG compared to ASA, other IVIG regimens, and other treatments for Kawasaki disease including TNF‐blockers and corticosteroids. Any such studies should report clinically relevant, clearly defined outcomes in a standardised way and report both short‐ and long‐term follow‐up periods. In order to assess these outcomes appropriately, randomised trials would need to include very large numbers of people. However, as large epidemiological studies are ongoing, it is unlikely that new RCTs investigating different IVIG regimens or comparing IVIG with ASA will begin. Ongoing RCTs identified in our searches compare IVIG with newer treatments (interleukin‐1 receptor antagonists) or are focused on IVIG‐resistant patients. Evidence from RCTs comparing IVIG with other treatments is important for the proportion of patients who fail to respond to initial IVIG treatment, as they are at most risk of serious complications from Kawasaki disease.
History
Protocol first published: Issue 6, 2021
Notes
For the purpose of open access, the author has applied a Creative Commons Attribution (CC‐BY) licence to any Author Accepted Manuscript version arising from this submission.
Parts of the Methods section of this review are based on a standard template established by Cochrane Vascular.
Acknowledgements
The review authors and Cochrane Vascular Editorial base are grateful to the following peer reviewers for their time and comments: Mamoru Ayusawa, MD, PhD, Department of Nutrition and Life Science, Faculty of Health and Medical Sciences, Kanagawa Institute of Technology, Japan; Masaru Miura, MD, PhD, Department of Cardiology, Tokyo Metropolitan Children's Medical Center, Tokyo, Japan; Yuichi Nomura, MD, PhD, Kagoshima City Hospital, Kagoshima, Japan.
The review authors are very grateful to the people who translated studies and extracted information to allow assessment, including Zhe Huang, Jing Xu, and Chew Shu Yui. The review authors are very grateful to the following people for providing additional information about included study data and methods: Mamoru Ayusama, Motofumi Iemura, Taichi Kato, Masaki Matsushima, Masaru Miura, Yoshihiro Onouchi, Zenshiro Onouchi, and Koichi Sakata.
Appendices
Appendix 1. Sources searched and search strategies
| Source | Search strategy | Hits retrieved |
| VASCULAR REGISTER IN CRSW (date of most recent search 26 April 2022) |
#1 Mucocutaneous Lymph Node Syndrome AND INREGISTER #2 kawasaki* AND INREGISTER #3 #1 OR #2 #4 Immunoglobulin* AND INREGISTER #5 Ig* AND INREGISTER #6 IVIG AND INREGISTER #7 civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen AND INREGISTER #8 #7 OR #6 OR #5 OR #4 #9 #3 AND #8 |
July 2021: 110 April 2022: 3 |
| CENTRAL via CRSO (date of most recent search 26 April 2022) |
#1 MESH DESCRIPTOR Mucocutaneous Lymph Node Syndrome EXPLODE ALL TREES 105 #2 (mucocutan* adj syndrome*):TI,AB,KY 195 #3 kawasaki*:TI,AB,KY 320 #4 (Mucocutaneous Lymph Node Syndrome):TI,AB,KY 189 #5 #1 OR #2 OR #3 OR #4 339 #6 MESH DESCRIPTOR Immunoglobulins, Intravenous EXPLODE ALL TREES 831 #7 immunoglobulin*:TI,AB,KY 13976 #8 Ig*:TI,AB,KY 25033 #9 IVIG:TI,AB,KY 1331 #10 (civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen):TI,AB,KY 145 #11 #6 OR #7 OR #8 OR #9 OR #10 32457 #12 #5 AND #11 163 |
July 2021: 163 April 2022: 11 |
| ClinicalTrials.gov (date of most recent search 26 April 2022) |
Mucocutaneous Lymph Node Syndrome OR kawasaki OR Mucocutaneous Syndrome | Immunoglobulins OR Immunoglobulin OR Ig OR IVIG OR civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen | July 2021: 22 April 2022: 1 |
| ICTRP Search Portal (date of most recent search 26 April 2022) |
Mucocutaneous Lymph Node Syndrome OR kawasaki OR Mucocutaneous Syndrome | Immunoglobulins OR Immunoglobulin OR Ig OR IVIG OR civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen | July 2021: 38 April 2022: 9 |
| MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE) 1946 to present (date of most recent search 26 April 2022) |
1 Mucocutaneous Lymph Node Syndrome/ 2 (mucocutan* adj syndrome*).ti,ab. 3 kawasaki*.ti,ab. 4 "Mucocutaneous Lymph Node Syndrome".ti,ab. 5 or/1‐4 6 exp Immunoglobulins, Intravenous/ 7 immunoglobulin*.ti,ab. 8 Ig*.ti,ab. 9 IVIG.ti,ab. 10 (civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen).ti,ab. 11 or/6‐10 12 5 and 11 13 randomized controlled trial.pt. 14 controlled clinical trial.pt. 15 randomized.ab. 16 placebo.ab. 17 drug therapy.fs. 18 randomly.ab. 19 trial.ab. 20 groups.ab. 21 or/13‐20 22 exp animals/ not humans.sh. 23 21 not 22 24 12 and 23 |
July 2021: 1156 April 2022: 196 |
| Embase via Ovid (date of most recent search 26 April 2022) |
1 exp mucocutaneous lymph node syndrome/ 2 (mucocutan* adj syndrome*).ti,ab. 3 kawasaki*.ti,ab. 4 "Mucocutaneous Lymph Node Syndrome".ti,ab. 5 or/1‐4 6 exp immunoglobulin/ 7 immunoglobulin*.ti,ab. 8 Ig*.ti,ab. 9 IVIG.ti,ab. 10 (civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen).ti,ab. 11 or/6‐10 12 5 and 11 13 randomized controlled trial/ 14 controlled clinical trial/ 15 random$.ti,ab. 16 randomization/ 17 intermethod comparison/ 18 placebo.ti,ab. 19 (compare or compared or comparison).ti. 20 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 21 (open adj label).ti,ab. 22 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 23 double blind procedure/ 24 parallel group$1.ti,ab. 25 (crossover or cross over).ti,ab. 26 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 27 (assigned or allocated).ti,ab. 28 (controlled adj7 (study or design or trial)).ti,ab. 29 (volunteer or volunteers).ti,ab. 30 trial.ti. 31 or/13‐30 32 12 and 31 |
July 2021: 698 April 2022: 143 |
| CINAHL via EBSCO (date of most recent search 26 April 2022) |
S28 S12 AND S27 S27 S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 S26 MH "Random Assignment" S25 MH "Triple‐Blind Studies" S24 MH "Double‐Blind Studies" S23 MH "Single‐Blind Studies" S22 MH "Crossover Design" S21 MH "Factorial Design" S20 MH "Placebos" S19 MH "Clinical Trials" S18 TX "multi‐centre study" OR "multi‐center study" OR "multicentre study" OR "multicenter study" OR "multi‐site study" S17 TX crossover OR "cross‐over" S16 AB placebo* S15 TX random* S14 TX trial* S13 TX "latin square" S12 S5 AND S11 S11 S6 OR S7 OR S8 OR S9 OR S10 S10 TX civacir or flebogamma or gamunex or carimune or gammagard or octagam or privigen S9 TX IVIG S8 TX Ig* S7 TX immunoglobulin* S6 (MH "Immunoglobulins, Intravenous") S5 S1 OR S2 OR S3 OR S4 S4 TX Mucocutaneous Lymph Node Syndrome S3 TX kawasaki* S2 TX mucocutan* N2 syndrome* S1 (MH "Mucocutaneous Lymph Node Syndrome") |
July 2021: 113 April 2022: 16 |
| TOTAL before deduplication | July 2021: 2300 April 2022: 379 |
|
| TOTAL after deduplication | July 2021: 1747 April 2022: 320 |
|
| TOTAL 2021 and 2022 after deduplication | April 2022: 1935 | |
Data and analyses
Comparison 1. Primary treatment ‐ IVIG (and ASA) versus ASA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 CAA: total dose of IVIG subgrouped by single or multiple infusion (up to 30 days) | 11 | 1437 | Odds Ratio (M‐H, Random, 95% CI) | 0.60 [0.41, 0.87] |
| 1.1.1 100 mg/kg over single infusion | 1 | 211 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.60, 1.92] |
| 1.1.2 1000 mg/kg over single infusion | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.29, 1.90] |
| 1.1.3 600 mg/kg over 3 days | 2 | 153 | Odds Ratio (M‐H, Random, 95% CI) | 1.77 [0.58, 5.41] |
| 1.1.4 1200 mg/kg over 3 days | 3 | 318 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.27, 0.76] |
| 1.1.5 1600 mg/kg over 4 days | 1 | 149 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.10, 0.84] |
| 1.1.6 500 mg/kg over 5 days | 1 | 256 | Odds Ratio (M‐H, Random, 95% CI) | 0.57 [0.30, 1.09] |
| 1.1.7 1 g/kg over 5 days | 1 | 72 | Odds Ratio (M‐H, Random, 95% CI) | 0.54 [0.13, 2.23] |
| 1.1.8 1 g/kg over 5 days (no ASA) | 1 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.08, 1.34] |
| 1.1.9 2 g/kg over 5 days | 2 | 119 | Odds Ratio (M‐H, Random, 95% CI) | 0.25 [0.10, 0.65] |
| 1.2 CAA: total dose of IVIG subgrouped by single or multiple infusion (≥ 6 months) | 7 | 679 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.45, 1.38] |
| 1.2.1 100 mg/kg over single infusion | 1 | 211 | Odds Ratio (M‐H, Random, 95% CI) | 1.63 [0.43, 6.21] |
| 1.2.2 1000 mg/kg over single infusion | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 0.73 [0.14, 3.87] |
| 1.2.3 600 mg/kg over 3 days | 2 | 153 | Odds Ratio (M‐H, Random, 95% CI) | 1.32 [0.45, 3.82] |
| 1.2.4 1200 mg/kg over 3 days | 2 | 182 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.18, 1.92] |
| 1.2.5 1600 mg/kg over 4 days | 1 | 24 | Odds Ratio (M‐H, Random, 95% CI) | 0.36 [0.05, 2.37] |
| 1.2.6 2 g/kg over 5 days | 1 | 25 | Odds Ratio (M‐H, Random, 95% CI) | 0.15 [0.01, 1.50] |
| 1.3 Adverse effects: total dose of IVIG subgrouped by single or multiple infusion | 10 | 1376 | Odds Ratio (M‐H, Random, 95% CI) | 0.57 [0.17, 1.89] |
| 1.3.1 100 mg/kg over single infusion | 1 | 214 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3.2 1000 mg/kg over single infusion | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.12, 1.75] |
| 1.3.3 600 mg/kg over 3 days | 2 | 165 | Odds Ratio (M‐H, Random, 95% CI) | 0.08 [0.01, 0.49] |
| 1.3.4 1200 mg/kg over 3 days | 3 | 325 | Odds Ratio (M‐H, Random, 95% CI) | 1.63 [0.08, 34.63] |
| 1.3.5 1600 mg/kg over 4 days | 1 | 168 | Odds Ratio (M‐H, Random, 95% CI) | 1.44 [0.44, 4.72] |
| 1.3.6 500 mg/kg over 5 days | 1 | 295 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3.7 2 g/kg over 5 days | 2 | 125 | Odds Ratio (M‐H, Random, 95% CI) | 0.30 [0.04, 2.34] |
| 1.4 Duration of fever from treatment onset (days): total dose of IVIG subgrouped by single or multiple infusion | 3 | 307 | Mean Difference (IV, Random, 95% CI) | ‐4.00 [‐5.06, ‐2.93] |
| 1.4.1 600 mg/kg over 3 days | 1 | 72 | Mean Difference (IV, Random, 95% CI) | ‐2.90 [‐5.54, ‐0.26] |
| 1.4.2 1200 mg/kg over 3 days | 2 | 201 | Mean Difference (IV, Random, 95% CI) | ‐3.84 [‐6.35, ‐1.34] |
| 1.4.3 2 g/kg over 5 days | 1 | 34 | Mean Difference (IV, Random, 95% CI) | ‐4.20 [‐5.77, ‐2.63] |
| 1.5 Duration of fever from KD onset (days): total dose of IVIG subgrouped by single or multiple infusion | 7 | 693 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.69, ‐0.52] |
| 1.5.1 1000 mg/kg over single infusion | 1 | 84 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐1.54, 1.54] |
| 1.5.2 600 mg/kg over 3 days | 2 | 164 | Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐3.56, 1.45] |
| 1.5.3 1200 mg/kg over 3 days | 3 | 318 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐4.62, ‐0.19] |
| 1.5.4 2 g/kg over 5 days | 2 | 127 | Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐2.99, ‐0.60] |
| 1.6 Need for additional treatment: total dose of IVIG subgrouped by single or multiple infusion | 3 | 272 | Odds Ratio (M‐H, Random, 95% CI) | 0.27 [0.05, 1.57] |
| 1.6.1 600 mg/kg over 3 days | 1 | 73 | Odds Ratio (M‐H, Random, 95% CI) | 0.16 [0.01, 4.03] |
| 1.6.2 1200 mg/kg over 3 days | 1 | 72 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 2.01] |
| 1.6.3 2 g/kg over 5 days | 2 | 127 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.06, 16.85] |
Comparison 2. Primary treatment ‐ IVIG versus IVIG.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 CAA: high‐dose regimens vs medium‐ or low‐dose regimens | 8 | 1824 | Odds Ratio (M‐H, Random, 95% CI) | 0.60 [0.40, 0.89] |
| 2.1.1 High‐dose single infusion vs medium‐dose single infusion | 3 | 555 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.55, 1.31] |
| 2.1.2 High‐dose multiple infusion vs medium‐dose single infusion | 1 | 195 | Odds Ratio (M‐H, Random, 95% CI) | 1.09 [0.47, 2.57] |
| 2.1.3 High‐dose multiple infusion vs medium‐dose multiple infusion | 4 | 649 | Odds Ratio (M‐H, Random, 95% CI) | 0.53 [0.20, 1.41] |
| 2.1.4 High‐dose multiple infusion vs low‐dose multiple infusion | 4 | 425 | Odds Ratio (M‐H, Random, 95% CI) | 0.36 [0.20, 0.64] |
| 2.2 CAA: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.2.1 High‐dose single infusion versus medium‐dose single infusion | 3 | 621 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.59, 1.32] |
| 2.3 CAA: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens | 6 | 1154 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.32, 0.66] |
| 2.3.1 High‐dose multiple infusion vs medium‐dose multiple infusion | 4 | 583 | Odds Ratio (M‐H, Random, 95% CI) | 0.49 [0.20, 1.19] |
| 2.3.2 High‐dose multiple infusion vs low‐dose multiple infusion | 4 | 366 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.20, 0.62] |
| 2.3.3 Medium‐dose multiple infusion vs low‐dose multiple infusion | 4 | 205 | Odds Ratio (M‐H, Random, 95% CI) | 0.66 [0.36, 1.23] |
| 2.4 CAA: single‐infusion regimens vs multiple‐infusion regimens | 4 | 962 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.28, 1.34] |
| 2.4.1 High‐dose single infusion vs high‐dose multiple infusion | 3 | 918 | Odds Ratio (M‐H, Random, 95% CI) | 0.54 [0.23, 1.27] |
| 2.4.2 Medium‐dose single infusion vs high‐dose multiple infusion | 1 | 44 | Odds Ratio (M‐H, Random, 95% CI) | 2.10 [0.18, 25.01] |
| 2.5 Adverse effects: high‐dose regimens vs medium‐ or low‐dose regimens | 6 | 1659 | Odds Ratio (M‐H, Random, 95% CI) | 1.11 [0.52, 2.37] |
| 2.5.1 High‐dose single infusion vs medium‐dose single infusion | 2 | 446 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.14, 7.34] |
| 2.5.2 High‐dose multiple infusion vs medium‐dose single infusion | 1 | 195 | Odds Ratio (M‐H, Random, 95% CI) | 1.55 [0.06, 38.63] |
| 2.5.3 High‐dose multiple infusion vs medium‐dose multiple infusion | 3 | 623 | Odds Ratio (M‐H, Random, 95% CI) | 1.22 [0.50, 3.01] |
| 2.5.4 High‐dose multiple infusion vs low‐dose multiple infusion | 3 | 395 | Odds Ratio (M‐H, Random, 95% CI) | 0.53 [0.05, 5.93] |
| 2.6 Adverse effects: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.6.1 High‐dose single infusion vs medium‐dose single infusion | 2 | 512 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.14, 7.34] |
| 2.7 Adverse effects: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens | 5 | 1115 | Odds Ratio (M‐H, Random, 95% CI) | 0.98 [0.43, 2.22] |
| 2.7.1 High‐dose multiple infusion vs medium‐dose multiple infusion | 3 | 572 | Odds Ratio (M‐H, Random, 95% CI) | 1.16 [0.47, 2.86] |
| 2.7.2 High‐dose multiple infusion vs low‐dose multiple infusion | 3 | 345 | Odds Ratio (M‐H, Random, 95% CI) | 0.53 [0.05, 5.93] |
| 2.7.3 Medium‐dose multiple infusion vs low‐dose multiple infusion | 3 | 198 | Odds Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 8.39] |
| 2.8 Adverse effects: single‐infusion regimens vs multiple‐infusion regimens | 4 | 1005 | Odds Ratio (M‐H, Random, 95% CI) | 1.61 [0.74, 3.51] |
| 2.8.1 High‐dose single infusion vs high‐dose multiple infusion | 3 | 961 | Odds Ratio (M‐H, Random, 95% CI) | 1.32 [0.49, 3.56] |
| 2.8.2 Medium‐dose single infusion vs high‐dose multiple infusion | 1 | 44 | Odds Ratio (M‐H, Random, 95% CI) | 2.22 [0.63, 7.82] |
| 2.9 Duration of fever (days): high‐dose regimens vs medium‐ or low‐dose regimens | 4 | 992 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.36, ‐0.06] |
| 2.9.1 High‐dose single infusion vs medium‐dose single infusion | 3 | 555 | Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.56, 0.32] |
| 2.9.2 High‐dose multiple infusion vs medium‐dose single infusion | 1 | 195 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.94, 0.34] |
| 2.9.3 High‐dose multiple infusion vs low‐dose multiple infusion | 1 | 242 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.81, ‐0.59] |
| 2.10 Duration of fever (days): higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.10.1 High‐dose single infusion vs medium‐dose single infusion | 2 | 512 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.68, 0.45] |
| 2.11 Duration of fever (days): higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens | 2 | 322 | Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐2.88, 1.61] |
| 2.11.1 High‐dose multiple infusion vs low‐dose multiple infusion | 1 | 242 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.81, ‐0.59] |
| 2.11.2 Medium‐dose multiple infusion vs low‐dose multiple infusion | 1 | 80 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐1.07, 2.27] |
| 2.12 Duration of fever (days): single‐infusion regimens vs multiple‐infusion regimens | 3 | 961 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.42, 0.44] |
| 2.12.1 High‐dose single infusion vs high‐dose multiple infusion ‐ duration from onset of disease | 1 | 267 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.09, 0.89] |
| 2.12.2 High‐dose single infusion vs high‐dose multiple infusion ‐ duration from onset of treatment | 2 | 694 | Mean Difference (IV, Random, 95% CI) | ‐1.09 [‐2.63, 0.45] |
| 2.13 Need for additional treatment: high‐dose regimens vs medium‐ or low‐dose regimens | 4 | 1125 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.10, 0.88] |
| 2.13.1 High‐dose single infusion vs medium‐dose single infusion | 2 | 316 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.01, 4.67] |
| 2.13.2 High‐dose multiple infusion vs medium‐dose single infusion | 1 | 194 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.19, 1.80] |
| 2.13.3 High‐dose multiple infusion vs medium‐dose multiple infusion | 2 | 530 | Odds Ratio (M‐H, Random, 95% CI) | 0.24 [0.06, 0.92] |
| 2.13.4 High‐dose multiple infusion vs low‐dose multiple infusion | 1 | 85 | Odds Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.56] |
| 2.14 Need for additional treatment: higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.14.1 High‐dose single infusion vs medium‐dose single infusion | 2 | 382 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.01, 4.80] |
| 2.15 Need for additional treatment: higher‐dose multiple‐infusion regimens vs lower‐dose multiple‐infusion regimens | 2 | 615 | Odds Ratio (M‐H, Random, 95% CI) | 0.24 [0.08, 0.70] |
| 2.15.1 High‐dose multiple infusion vs medium‐dose multiple infusion | 2 | 504 | Odds Ratio (M‐H, Random, 95% CI) | 0.23 [0.06, 0.90] |
| 2.15.2 High‐dose multiple infusion vs low‐dose multiple infusion | 1 | 56 | Odds Ratio (M‐H, Random, 95% CI) | 0.13 [0.01, 2.60] |
| 2.15.3 Medium‐dose multiple infusion vs low‐dose multiple infusion | 1 | 55 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.03, 3.56] |
| 2.16 Need for additional treatment: single‐infusion regimens vs multiple‐infusion regimens | 2 | 818 | Odds Ratio (M‐H, Random, 95% CI) | 1.14 [0.38, 3.39] |
| 2.16.1 High‐dose single infusion vs high‐dose multiple infusion | 2 | 818 | Odds Ratio (M‐H, Random, 95% CI) | 1.14 [0.38, 3.39] |
| 2.17 Length of hospital stay (days): high‐dose regimens vs medium‐ or low‐dose regimens | 3 | 752 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.78, 0.30] |
| 2.17.1 High‐dose single infusion vs medium‐dose single infusion | 3 | 558 | Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐1.15, 0.33] |
| 2.17.2 High‐dose multiple infusion vs medium‐dose single infusion | 1 | 194 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.83, 1.03] |
| 2.18 Length of hospital stay (days): higher‐dose single‐infusion regimens vs lower‐dose single‐infusion regimens | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.18.1 High‐dose single infusion vs medium‐dose single infusion | 3 | 621 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.09, 0.37] |
| 2.19 Length of hospital stay (days): single‐infusion regimens vs multiple‐infusion regimens | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.19.1 High‐dose single infusion vs high‐dose multiple infusion | 2 | 414 | Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐3.86, 1.37] |
Comparison 3. Primary treatment ‐ IVIG versus prednisolone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 CAA: total dose of IVIG vs total dose of IV prednisolone | 2 | 140 | Odds Ratio (M‐H, Random, 95% CI) | 0.60 [0.24, 1.48] |
| 3.1.1 1200 mg/kg IVIG over 3 days vs 10 mg/kg prednisolone over 5 days | 1 | 90 | Odds Ratio (M‐H, Random, 95% CI) | 0.49 [0.17, 1.43] |
| 3.1.2 2 g/kg IVIG over 2 days vs 10 mg/kg prednisolone over 5 days | 1 | 50 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.18, 5.51] |
| 3.2 Adverse events: total dose of IVIG vs total dose of IV prednisolone | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.2.1 1200 mg/kg IVIG over 3 days vs 10 mg/kg prednisolone over 5 days | 1 | 90 | Odds Ratio (M‐H, Random, 95% CI) | 4.18 [0.19, 89.48] |
| 3.3 Duration of fever (days) : total dose of IVIG vs total dose of IV prednisolone | 2 | 140 | Mean Difference (IV, Random, 95% CI) | 0.68 [‐0.59, 1.94] |
| 3.3.1 1200 mg/kg IVIG over 3 days vs 10 mg/kg prednisolone over 5 days | 1 | 90 | Mean Difference (IV, Random, 95% CI) | 1.40 [0.42, 2.38] |
| 3.3.2 2 g/kg IVIG over 2 days vs 10 mg/kg prednisolone over 5 days | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.39, 0.59] |
Comparison 4. Secondary treatment ‐ IVIG versus infliximab.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 CAA: total dose of single IVIG vs single infliximab | 4 | 197 | Odds Ratio (M‐H, Random, 95% CI) | 1.31 [0.46, 3.74] |
| 4.1.1 2 g/kg IVIG vs infliximab 5 mg/kg | 3 | 98 | Odds Ratio (M‐H, Random, 95% CI) | 0.99 [0.17, 5.63] |
| 4.1.2 2 g/kg IVIG vs infliximab 10 mg/kg | 1 | 99 | Odds Ratio (M‐H, Random, 95% CI) | 1.76 [0.53, 5.80] |
| 4.2 Adverse effects: total dose of single IVIG vs single infliximab | 4 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 1.13 [0.35, 3.61] |
| 4.2.1 2 g/kg IVIG vs infliximab 5 mg/kg | 3 | 98 | Odds Ratio (M‐H, Random, 95% CI) | 0.66 [0.17, 2.61] |
| 4.2.2 2 g/kg IVIG vs infliximab 10 mg/kg | 1 | 103 | Odds Ratio (M‐H, Random, 95% CI) | 2.58 [1.16, 5.75] |
| 4.3 Need for additional treatment: total dose of single IVIG vs single infliximab | 4 | 199 | Odds Ratio (M‐H, Random, 95% CI) | 3.99 [1.98, 8.02] |
| 4.3.1 2 g/kg IVIG vs infliximab 5 mg/kg | 3 | 98 | Odds Ratio (M‐H, Random, 95% CI) | 4.12 [1.39, 12.23] |
| 4.3.2 2 g/kg IVIG vs infliximab 10 mg/kg | 1 | 101 | Odds Ratio (M‐H, Random, 95% CI) | 3.89 [1.56, 9.70] |
Comparison 5. Secondary treatment ‐ IVIG versus prednisolone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 CAA: single IVIG vs multiple prednisolone | 2 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.46 [0.02, 9.18] |
| 5.1.1 Total dose of IVIG 2 g/kg vs prednisolone 45 mg/kg | 1 | 53 | Odds Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.64] |
| 5.1.2 Total dose of IVIG 2 g/kg vs prednisolone 90 mg/kg | 1 | 22 | Odds Ratio (M‐H, Random, 95% CI) | 1.69 [0.22, 12.81] |
| 5.2 Adverse effects: IVIG vs multiple prednisolone | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.2.1 2 g/kg IVIG vs prednisolone 45 mg/kg | 1 | 80 | Odds Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.49] |
Comparison 6. Tertiary treatment ‐ IVIG versus prednisolone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 CAA: IVIG vs prednisolone | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1.1 Total dose of IVIG 1 g/kg vs 20 mg/kg prednisolone over 3 days | 1 | 17 | Odds Ratio (M‐H, Random, 95% CI) | 0.48 [0.06, 3.99] |
| 6.2 Duration of fever (days): IVIG vs prednisolone | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.2.1 Total dose of 1 g/kg IVIG vs 20 mg/kg prednisolone over 3 days | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 3.40 [2.73, 4.07] |
Comparison 7. Additional subgroup analysis: primary treatment ‐ IVIG (and ASA) versus ASA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Analysis 1.1 subgrouped by geographic distribution | 11 | 1437 | Odds Ratio (M‐H, Random, 95% CI) | 0.60 [0.41, 0.87] |
| 7.1.1 Japan | 10 | 1288 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.43, 0.94] |
| 7.1.2 USA and Canada | 1 | 149 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.10, 0.84] |
Comparison 8. Additional subgroup analysis: primary treatment ‐ IVIG versus IVG.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Analysis 2.1.1 subgrouped by geographical distribution | 3 | 555 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.55, 1.31] |
| 8.1.1 China | 2 | 446 | Odds Ratio (M‐H, Random, 95% CI) | 0.90 [0.55, 1.45] |
| 8.1.2 Japan | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.70 [0.26, 1.89] |
| 8.2 Analysis 2.2 subgrouped by geographical distribution | 3 | 621 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.59, 1.32] |
| 8.2.1 China | 2 | 512 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.59, 1.45] |
| 8.2.2 Japan | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.70 [0.26, 1.89] |
| 8.3 Analysis 2.4 subgrouped by geographical distribution | 4 | 962 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.28, 1.34] |
| 8.3.1 China | 1 | 267 | Odds Ratio (M‐H, Random, 95% CI) | 1.04 [0.53, 2.04] |
| 8.3.2 Japan | 1 | 145 | Odds Ratio (M‐H, Random, 95% CI) | 0.25 [0.07, 0.92] |
| 8.3.3 USA and Canada | 2 | 550 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.16, 2.43] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barron 1990.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 7 (3 no pre‐infusion ECG, 1 pre‐existing CAA, 3 no ECG at 42 to 49 days) Losses to follow‐up: 51 enrolled, 44 completed Intention‐to‐treat analysis: no Duration of study: January 1987 to April 1988 | |
| Participants | Country: USA and Canada Setting: hospitals (7 centres) Number: 47 (intervention n = 25; comparison n = 22) Age (months, mean (SD)): intervention 38.2 (22.2); comparison 30.1 (19.1) Sex (M/F): intervention 17/8; comparison 9/13 Diagnostic criteria described: yes Inclusion criteria: enrolled within 7 days of onset of KD (1st day of fever) Exclusion criteria: clinical or laboratory evidence of disease known to mimic KD; known heart disease; recurrent KD, known immunological defects; prior treatment with any immunomodulating agent | |
| Interventions | Primary or secondary KD treatment: primary Intervention: 1 g/kg (5 to 8 hours) single‐dose IVIG Comparison: 400 mg/kg (4 days), once daily Concomitant medications: both groups ASA 80 to 100 mg/kg/day (every 6 hours); reduced to 3 to 5 mg/kg/day after resolution of fever (for minimum of 2 months) | |
| Outcomes | Incidence of CAA
Differences in laboratory values
Duration of fever
Reduction of clinical symptoms
Changes in vital signs noted Cardiac evaluation: ECG of coronary arteries, left ventricular dimension and shortening fraction, pericardial space, mitral or aortic insufficiency. Cardiac segments graded as normal ‐ enlarged or dilated ‐ aneurysmal Laboratory evaluations: included complete blood cell, differential cell counts, PLT count, total serum bilirubin concentration Time points: entry, days 4 to 6, 14 to 21, 42 to 49 |
|
| Funding | "Supported by a grant from Baxter Healthcare Corporation, Hyland Division, Glendale, Calif., and the American Red Cross." | |
| Declaration of interest | Not reported | |
| Notes | IVIG used was Gammagard (Baxter Healthcare Corp, Hyland Division, Glendale, California); human IgG 3 participants excluded for no ECG at 42 to 49 days, were included in adverse event data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote " ..randomly assigned in blocks of four to receive one of two dosage regimens of IVIG. Each institution was provided with a randomization schedule, and patients were assigned in sequential order to the proper treatment group." |
| Allocation concealment (selection bias) | Unclear risk | Institutions received randomisation schedule, but unclear if this was open or not. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. Unclear if this could impact outcomes |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "Each echocardiogram was recorded on videotape and reviewed by two observers who were unaware of patient identity" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement may be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data, all accounted for |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes reported (no protocol). |
| Other bias | Unclear risk | There is an imbalance of genders between groups: M/F 17/8 group 1 and 9/13 group 2 (P = 0.06). Unclear if this is sufficient to affect the results |
Burns 2008.
| Study characteristics | ||
| Methods | Design: multicentre, prospective RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: September 2004 to September 2006 | |
| Participants | Country: USA Setting: hospitals (6) Number: 24 (intervention n = 12; comparison n = 12) Age (months, median (range)): intervention 22 (3 to 85); comparison 20 (2.4 to 75) Sex (M/F): intervention 9/3; comparison 8/4 Diagnostic criteria described: yes Inclusion criteria: children with acute KD treated with IVIG within 14 days of fever who had persistent or recrudescent fever 48 hours to 7 days after initial IVIG infusion Exclusion criteria: history of TB, histoplasmosis, or coccidiomycosis, recent TB exposure, a chest radiograph suggestive of pulmonary infection obtained within 1 week of study enrolment, immunisation with BCG in the previous 6 months, steroid or other immunomodulatory treatment in previous 1 week | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG 2 g/kg Comparison: infliximab 5 mg/kg Concomitant medications: all participants received an initial IVIG infusion (2 g/kg) prior to study enrolment. Paracetamol (15 mg/ kg orally) and diphenhydramine (1 mg/kg orally or IV) were administered before study drug infusion. ASA was administered orally at 80 to 100 mg/kg/day in 4 doses until the first clinical evaluation at week 1, when the ASA dose was reduced to 3 to 5 mg/kg/day. All other antipyretic or anti‐inflammatory therapies were prohibited. | |
| Outcomes | Primary: pharmacokinetics and safety/tolerability of a single infliximab infusion (5 mg/kg), AE
Secondary: cessation of fever, cytokine and CRP levels, WBC count, serum antibodies to infliximab, complete blood count
Time points: laboratory assessments were performed at baseline and 2 h, 24 h, 1 week, 2 weeks, and 4 weeks in all study participants
CAA reported as AE Cardiac evaluation: ECG at baseline and 2 to 4 weeks after intervention. "The internal lumen diameters of the left anterior descending and right coronary arteries adjusted for body surface and expressed as standard deviation units (Z scores) were recorded. Arteries were classed as normal (Z < 2.5), dilated (Z ≥ 2.5), or aneurysmal (Z ≥ 4.0) with focal dilation of the vessel ≥ 1.5 times the adjacent segment)" |
|
| Funding | Quote "Supported by a grant from Centocor, Inc. and by the National Institute for Child Health and Human Development, Pediatric Pharmacology Research Unit (PPRU) Network (5U10 HD031318). Centocor Inc. performed the determinations of infliximab levels and the assays for anti‐infliximab antibodies. Dr. Gregory F. Keenan and Khalid Mamun participated in editing the manuscript. " GFK and KM employed by Centocor. |
|
| Declaration of interest | Quote "The authors declare no potential conflicts of interest." | |
| Notes | Pilot study No details on IVIG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Subjects were assigned 1:1 to receive intravenous (IV) infliximab 5 mg/kg or IVIG 2 g/ kg using randomly permuted blocks stratified by age" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. "Family members and investigators were aware of the treatment assignment" |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data, all accounted for |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported (NCT00271570). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Burns 2021.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 2 (withdrew consent) Losses to follow‐up: 3 Intention‐to‐treat analysis: yes Duration of study: March 2017 to August 2020 | |
| Participants | Country: USA Setting: 30 hospitals Number: 103 (105 randomised) intervention n = 49; comparison n = 54 Age (years, median (IQR): intervention 2.1 (1.7 to 5.0) ; comparison 3.6 (2.0 to 6.4) Sex (M/F): intervention 30/19; comparison 29/25 Diagnostic criteria described: yes Inclusion criteria: infants and children aged 4 weeks to 17 years who met AHA criteria for complete or incomplete KD and were resistant to initial treatment for KD with IVIG (2 g/kg) within the first 10 days after fever onset were eligible for enrolment Exclusion criteria: initial treatment with IVIG after day 10 of fever and treatment with steroids or other medication for intensification of initial therapy; chronic disease, except asthma, atopic dermatitis, autism, or controlled seizure disorder, known previous infection with TB, coccidioidomycosis, or histoplasmosis, or household contact with active TB; use of TNF α‐blocker within 3 months before enrolment; and patients with a history of hypersensitivity to infliximab | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG 2 g/kg over 8 to 12 hours (according to local practice) Comparison: infliximab 10 mg/kg IV over 2 hours Concomitant medications: ASA 30 to 50 mg/kg/day or 80 to 100 mg/kg/day until discharge and then 3 to 5 mg/kg/day until the participant was off study | |
| Outcomes | Primary outcome: resolution of fever 24 hours after treatment with no recurrence 7 days after discharge
Secondary outcomes:
Cardiac evaluation: participant height, weight, and internal dimension of the right coronary artery, left anterior descending coronary artery, and circumflex artery were recorded at baseline and at study completion. Z scores (internal diameter of the right and left anterior descending normalised for body surface area and expressed as SD units from the mean) were calculated by the Data Coordinating Center in the REDCap database. Z‐worst was defined as the highest Z score for the right coronary artery, left anterior descending coronary artery, or circumflex artery from the echocardiograms at baseline and at study completion. |
|
| Funding | Quote "The study sponsor, Patient‐Centered Outcomes Research Institute, had no role in study design, data collection, data analysis, data interpretation, or writing of the report" | |
| Declaration of interest | Quote "We declare no competing interests" | |
| Notes | Quote "...all infliximab or IVIG products were permitted and the manufacturer’s name was recorded" Not specifically reported in article | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Patients were randomly assigned in a 1:1 ratio to infliximab or second IVIG according to a prespecified randomisation scheme stratified by site, sex (male vs female), and age (>12 months or ≤12 months) by using a randomly permuted block randomisation design with block size of two or four, which was created by the Data Coordinating Center." |
| Allocation concealment (selection bias) | Low risk | Quote "Patient enrolment and randomisation through the REDCap database was done by the study site investigators who could not predict the next treatment assignment." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study, no blinding was undertaken |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Unclear risk | There was no blinding of outcome assessment. Steps were taken to standardise ECG imaging across sites, and Z‐scores were calculated by the Data Coordinating Centre in the REDCap database. Quote "...a single echocardiogram of a non‐study patient with KD was submitted by every site and the technical quality assessed by the Director of Non‐Invasive Imaging (BFP) at Rady Children’s Hospital San Diego (San Diego, CA, USA). A written assessment of the ECG quality with suggestions for improvement as needed was sent to every site. ... Z scores (internal diameter of the right and left anterior descending normalised for body surface area and expressed as SD units from the mean) were calculated by the Data Coordinating Center in the REDCap database" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | There was no blinding of outcome assessment, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data, all accounted for |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported (NCT03065244). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Furusho 1984.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 93 randomised (8 not managed by protocol and excluded from study analysis: 4 participants were given IVGG at doses outside the range of 400 ± 50 mg/kg daily, in 1 case IVGG was discontinued because of a chill, 1 case retreated with IVGG during the study period, 1 participant was removed from the trial because of a hepatic disorder attributed to ASA, and 1 participant in the ASA group was treated with IVGG because of worsening symptoms) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: April 1983 to April 1984 | |
| Participants | Country: Japan Setting: 14 hospitals Number: 85 (intervention n = 40; comparison n = 45) Age (months, mean (SD)): intervention 27 (20); comparison 22 (16) Sex (M/F): intervention 24/16; comparison 25/20 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset Exclusion criteria: recurrent or incomplete KD, if treatment could not begin within 7 days of the onset of KD and those with a CAL on admission | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVGG plus ASA (IVIG 400 mg/kg daily, for 5 days from day 1 of treatment; ASA 30 to 50 mg/kg daily in 3 divided doses, reduced to 10 to 30 mg/kg once a day once fever gone) Comparison: ASA (30 to 50 mg/kg daily in 3 divided doses, reduced to 10 to 30 mg/kg once a day when fever gone) Concomitant medications: none reported | |
| Outcomes | CAL (up to 60 days)
Fever
Laboratory findings (CRP, ESR, PLT count, serum IgG, side effects) Cardiac evaluation: 2‐dimensional ECG 3/week for 60 days after KD onset The development of even a transient dilation of the coronary artery was regarded as indicating a CAL. ECG criteria were those of the KDRC (increase in coronary lumen diameter of 1.5 times or more as compared with adjacent vessel diameter or coronary arteries with diameters of 3 mm or more). A positive report was followed by selective coronary arteriography to confirm the presence of a lesion. Time points: 3 times per week to 60 days for CAA, weeks 1, 2, 3, and 4 for remaining outcomes |
|
| Funding | None reported. Quote "We thank Chemo‐Sero‐Therapeutic Research Institute and TelJin Ltd for donating S‐sulphonated gammaglobulin (Venilon)" | |
| Declaration of interest | Not reported | |
| Notes | IVIG: S‐sulphonated intact gammaglobulin; Venilon, Teijin Ltd, Japan This is study 1 of 3 also reported in Furusho 1991. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible participants were randomly allocated to treatment, but details are insufficient to permit a judgement of low risk or high risk. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding is not described. Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data. Exclusions postrandomisation explained. |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes reported (no protocol). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Furusho 1991A.
| Study characteristics | ||
| Methods | Design: multicentre prospective RCT Exclusions postrandomisation: 20 (not managed according to the trial protocol) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: May 1984 to September 1985 | |
| Participants | Country: Japan Setting: 16 hospitals Number: 145 (IVGG100 n = 41; IVGG200 n = 51; IVGG400 n = 53) Age (months, mean (SD)): IVGG100 23.7 (23.3); IVGG200 25.7 (21.6); IVGG400 29.7 (23.7) Sex (M/F): IVGG100 21/20; IVGG200 30/21; IVGG400 36/17 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset Exclusion criteria: recurrent or incomplete KD, if treatment could not begin within 7 days of the onset of KD, and those with a CAL on admission | |
| Interventions | Primary or secondary KD treatment: primary Interventions: IVGG100: IVIG 100 mg/kg/day for 5 days from day 1 of treatment (5% solution 50 drops/min) IVGG200: IVIG 200 mg/kg/day for 5 days from day 1 of treatment (5% solution 50 drops/min) IVGG400: IVIG 400 mg/kg/day for 5 days from day 1 of treatment (5% solution 50 drops/min) Concomitant medication: ASA 30 to 50 mg/kg in 3 doses whilst fever present. After fever 10 to 30 mg/kg/day | |
| Outcomes | CAL (up to 60 days)
Fever
Laboratory findings (CRP, ESR, PLT count, serum IgG, adverse effects) Cardiac evaluation: 2‐dimensional ECG 3/week for 60 days after KD onset. The development of even a transient dilation of the coronary artery was regarded as indicating a CAL. ECG criteria were those of the JKDRC (increase in coronary lumen diameter of 1.5 times or more as compared with adjacent vessel diameter or coronary arteries with diameters of 3 mm or more). A positive report was followed by selective coronary arteriography to confirm the presence of a lesion. Time points: 3 times per week to 60 days for CAA, weeks 1, 2, 3, and 4 for remaining outcomes |
|
| Funding | None | |
| Declaration of interest | Not reported | |
| Notes | IVIG details: S‐sulphonated intact γ‐globulin (Venilon, Teijin Ltd, Japan) This is study 2 of 3 reported in Furusho 1991. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Eligible patients were allocated at random to three treatment groups." Insufficient information to permit judgement of low risk of high risk |
| Allocation concealment (selection bias) | Unclear risk | Quote "Eligible patients were allocated at random to three treatment groups." Insufficient information to permit judgement of low risk of high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding is not described. Insufficient information to permit judgement of low risk of high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No ITT analysis, 20/145 exclusions after randomisation |
| Selective reporting (reporting bias) | High risk | No description of outcomes or measurements in the methods section. Insufficient information (no protocol) |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Furusho 1991B.
| Study characteristics | ||
| Methods | Design: multicentre, prospective RCT Exclusions postrandomisation: 12 (not managed according to the trial protocol) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: October 1985 to June 1986 | |
| Participants | Country: Japan Setting: 16 hospitals Number: 151 (Group ASA + IVGG n = 49; Group IVGG n = 53; Group ASA n = 49) Age (months, mean (SD)): Group ASA + IVGG 24.3 (21.2); Group IVGG 24.1 (20.0); Group ASA 21.9 (15.1) Sex (M/F): Group ASA + IVGG 28/21; Group IVGG 27/26; Group ASA 26/23 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset Exclusion criteria: recurrent or incomplete KD, if treatment could not begin within 7 days of the onset of KD, and those with a CAL on admission | |
| Interventions | Primary or secondary KD treatment: primary Interventions: Group ASA + IVGG: IVIG 200 mg/kg/day for 5 days from day 1 of treatment (5% solution 50 drops/min) plus ASA 30 to 50 mg/kg in 3 doses whilst fever present. After fever 10 to 30 mg/kg/day Group IVGG: IVIG 200 mg/kg/day for 5 days from day 1 of treatment (5% solution 50 drops/min). Without ASA Group ASA: ASA 30 to 50 mg/kg in 3 doses whilst fever present. After fever 10 to 30 mg/kg/day Concomitant medications: none stated | |
| Outcomes | CAL (up to 60 days)
Adverse effects Cardiac evaluation: 2‐dimensional ECG 3/week for 60 days after KD onset. The development of even a transient dilation of the coronary artery was regarded as indicating a CAL. ECG criteria were those of the JKDRC (increase in coronary lumen diameter of 1.5 times or more as compared with adjacent vessel diameter or coronary arteries with diameters of 3 mm or more). A positive report was followed by selective coronary arteriography to confirm the presence of a lesion. Time points: 3 times per week to 60 days for CAA, then to 24 months if CAA detected. Remaining outcomes unclear |
|
| Funding | None | |
| Declaration of interest | Not reported | |
| Notes | IVIG details: S‐sulphonated intact γ‐globulin (Venilon, Teijin Ltd, Japan) This is study 3 of 3 reported in Furusho 1991. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Eligible patients were allocated at random to three treatment groups." Insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Quote "Eligible patients were allocated at random to three treatment groups." Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding is not described. Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No ITT analysis, 12/151 excluded postrandomisation |
| Selective reporting (reporting bias) | High risk | No description of outcomes or measurements in the methods section. Insufficient information (no protocol) |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Harada 1989.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: 6 (intervention n = 4; comparison n = 2) Intention‐to‐treat analysis: no Duration of study: February 1987 to March 1988 | |
| Participants | Country: Japan Setting: 15 hospitals Number: 242 (intervention n = 125; comparison n = 117) Age (months, mean (SD)): intervention 22.4 (15.0); comparison 19.8 (13.7) Sex (M/F): intervention 76/49; comparison 57/60 Diagnostic criteria described: yes Inclusion criteria: satisfied diagnostic criteria for KD, < 7 days onset, ≤ 4 years old Exclusion criteria: recurrent or incomplete KD, use of steroid or indometacin before treatment | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVGG (100 mg/kg/day for 5 consecutive days) plus ASA (50 mg/kg/day) Comparison: IVGG (400 mg/kg/day for 5 consecutive days) plus ASA (50 mg/kg/day) Concomitant medications: ASA (50 mg/kg/day) | |
| Outcomes | CAL (enrolment, 30 days, 60 days after KD onset, and at 1 year if present at 60 days)
Laboratory test (enrolment ‐ 60 days) Cardiac evaluation: 2‐dimensional ECG at enrolment, 1/week from before IVIG treatment for 60 days after KD onset. Echo results were recorded on video and judged by independent staff. Coronary artery diameter of 3 to 5 mm were considered dilations, and 6 mm or greater were considered aneurysms. |
|
| Funding | Quote "I gratefully acknowledge the support of the Kawasaki Disease Research Committee of Japan for this study" (from Harada 1991) | |
| Declaration of interest | None reported. | |
| Notes | IVIG details: full molecular type immunoglobulin This study is the same as study 3 (of 3) reported in Harada 1991. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | States central randomisation. Groups were assigned under the direction of an independent controller. |
| Allocation concealment (selection bias) | Low risk | States central randomisation. Groups were assigned under the direction of an independent controller. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Harada 1991 reports that ECGs were recorded (stop motion/video) and interpreted by independent observers. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No description of blinding for assessing any other outcome. Unclear if this could have affected other outcome reporting |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Hashino 2001.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: January 1993 to December 1998 | |
| Participants | Country: Japan Setting: hospital Number: 17 (intervention n = 8; comparison n = 9) Age: between 2 months and 10.6 years (no information for groups) Sex (M/F): no information. Quote "no significant difference in gender, age or duration of illness between the patients in these two groups" Diagnostic criteria described: yes Inclusion criteria: diagnosis of KD according to JKDRC criteria, non‐responders to initial and secondary treatment Exclusion criteria: responders to initial or secondary treatment | |
| Interventions | Primary or secondary KD treatment: tertiary (non‐responders to initial and second IVIG treatment) Intervention: IVIG 1 g/kg Comparison: IV methylprednisolone 20 mg/kg/day for 3 days Concomitant medications: initial treatment was IVIG 2 g/kg; second treatment was IVIG 1 g/kg. All participants were given ASA 30 mg/kg per day. | |
| Outcomes | CAA
Duration of fever
Laboratory tests (WBC count, haematocrit, haemoglobin, PLT, CRP, and albumin)
Costs of hospitalisation Cardiac evaluation: 2‐dimensional ECG within 24 hours of hospitalisation, then every 24 hours during retreatment and every 7 days after. Change in coronary artery diameter calculated (% change = (diameter after retreatment − diameter before retreatment)/diameter before retreatment X 100) Time points: 24, 48 hours, 7, 14, 21, 28, 35 days |
|
| Funding | Quote "This study was supported, in part, by Grants‐in‐Aid 10470183 and 09770586 from the Ministry of Education, Science and Culture, Japan." | |
| Declaration of interest | Not reported | |
| Notes | No details on IVIG manufacturer No specific baseline details provided, but states "no significant difference in gender, age or duration of illness between the patients in these two groups". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "We randomly divided these 17 patients into two groups". Insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants or personnel |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Unclear risk | No blinding of outcome assessors, but internal checks on reproducibility on coronary images carried out with little variance. Quote "Two independent observers (KH, MI), with each observer individually selecting the frames to measure and having no knowledge of the results obtained by the other observer, analyzed 20 randomly selected patients at different times." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data, all accounted for |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported (protocol available). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
He 2021.
| Study characteristics | ||
| Methods | Design: open‐label, multicentre, prospective RCT Exclusions postrandomisation: none Losses to follow‐up: 7 (Group A 4; Group B 2; Group C 1) Intention‐to‐treat analysis: no (states primary outcome was ITT) Duration of study: January 2014 to December 2015 | |
| Participants | Country: China Setting: 3 hospitals (Children’s Hospital of Fudan University, Shanghai Children’s Medical Center, and Shanghai Children’s Hospital) Number: 397 (404 randomised) (Group A 138; Group B 127; Group C 132) Age (months, mean ± SD): Group A 26.4 ± 22.7; Group B 28.8 ± 22.3; Group C 26.1 ± 20.0 Sex (M/F): Group A 90/48; Group B 82/45; Group C 77/55 Diagnostic criteria described: yes Inclusion criteria: within 5 to 10 days of KD onset (the first day of illness defined as the first day of fever), age ≤ 1 month at onset to < 12 years of age Exclusion criteria: afebrile before enrolment, previous history of KD; CAL before enrolment; history of administration of steroids (oral, intravenous, intramuscular, or subcutaneous) in the previous 30 days or administration of IVIG in the previous 180 days, severe concomitant medical disorders (chromosomal abnormality, immunodeficiency, complex congenital heart disease, metabolic disorders, nephritis, collagen diseases, etc.), suspected infectious diseases including sepsis, septic meningitis, peritonitis, bacterial pneumonia, varicella, and influenza | |
| Interventions | Primary or secondary KD treatment: primary Intervention Group A: IVIG 2 g/kg once over 12 to 24 hours Intervention Group B: IVIG 1 g/kg twice, over 2 days Intervention Group C: IVIG 1 g/kg once over 12 to 24 hours Concomitant medications: ASA at 30 to 50 mg/kg/day split into 3 doses per day, reduced to 3 to 5 mg/kg per day when fever subsided for 3 days and CRP ≤ 8 mg/L Participants admitted before day 5 of illness were treated with ASA only and began IVIG treatment between day 5 and 10 of illness. | |
| Outcomes | Primary outcomes:
Hours to defervescence
Incidence of CAL Secondary outcomes: IVIG resistance, total fever days, total dose of IVIG, changes in laboratory data 72 hours after completion of initial IVIG infusion, incidence of CAL during the whole study period, length of hospital stay, hospitalisation expenses, and serious adverse events (including death, severe infection, heart failure, allergic reactions) Cardiac evaluation: 2‐dimensional ECG before treatment and approximately 2 weeks, 1, 3, 6 months after onset. Measurement included the diameter of the left main coronary artery, left anterior descending artery, left circumflex coronary artery and proximal, middle and distal segment of right coronary artery. CAL defined as dilation or aneurysm, when luminal diameter was > 3.0 mm in children < 5 years or > 4.0 mm for ≥ 5 years, or when internal diameter of a segment was ≥ 1.5 times adjacent segment, or Z‐score > 2.5. Medium aneurysm defined as an internal luminal diameter from 4 to 8 mm; giant aneurysm defined as an internal luminal diameter > 8.0 mm. CAL severity classified as:
Time points: CAA 2 weeks, 1, 3, and 6 months |
|
| Funding | Quote "This study was funded by Joint Research Projects of Emerging Cutting‐edge Technologies of Shanghai Municipal Hospitals (SHDC12013106), Science and Technology Commission of Shanghai Municipality Projects (15ZR1404300), and Chinese Academy of Medical Sciences Research Unit (2018RU002)" | |
| Declaration of interest | Quote "The authors declare no conflict of interest." | |
| Notes | 2 IVIG products used ‐ both pH4 and manufactured in Shanghai. Participants included 13 incomplete KD patients (9.42%). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Randomization was performed using a simple randomization sequence generated by Microsoft Excel. A set of instructions about correct implementation of the randomized trial was sent to the three participating hospitals." |
| Allocation concealment (selection bias) | Unclear risk | Hospitals had instructions on the correct implementation of randomisation, but insufficient information to permit judgement of low risk or high risk. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote "Patients and physicians were not masked to the group assignments, while echocardiologists assessing CAL were blinded." |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "Patients and physicians were not masked to the group assignments, while echocardiologists assessing CAL were blinded." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding described for other outcomes. Quote "Patients and physicians were not masked to the group assignments, while echocardiologists assessing CAL were blinded." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported (NCT02439996). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Matsushima 1985.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: September 1983 to July 1984 | |
| Participants | Country: Japan Setting: 15 hospitals Number: 34 (intervention n = 17; comparison n = 17) Age (months, mean/SD): intervention 26.1 (16.5); comparison 34.1 (25.1) Sex (M/F): intervention 9/8; comparison 8/9 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 10 days of onset Exclusion criteria: recurrent or incomplete KD | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG (400 mg/kg/day for 5 consecutive days) plus ASA (30 mg/kg/day) Comparison: ASA (30 mg/kg/day) Concomitant medications: none | |
| Outcomes | Fever, laboratory findings (WBC, CRP, ESR, PLT count, serum IgG, albumin score), complement and cellular immunity testing (IgA, IgM, IgE, C3, C4, CH50, T4/T8) Cardiac evaluation: 2‐dimensional ECG 1/week for 30 days after KD onset; coronary artery diameter of 3 to 5 mm were considered dilations, and 6 mm or greater were considered aneurysms Time points: CAA 1, 2, 3, 4 weeks |
|
| Funding | None reported. | |
| Declaration of interest | None reported. | |
| Notes | IVIG details: polyethylene glycol‐treated human normal immunoglobulin (Venoglobulin I) Additional data provided by study authors (unable to provide data on length of hospital stay). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | States central randomisation, but also that interventions were assigned based on even or odd registration numbers ‐ this suggests not true randomisation |
| Allocation concealment (selection bias) | High risk | Assigned based on even or odd registration numbers |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment, and the outcome measurement could have been influenced by lack of blinding |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment, and the outcome measurement could have been influenced by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Miura 2008.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: January 2001 to May 2003 | |
| Participants | Country: Japan Setting: hospital Number: 22 (intervention n = 11; comparison n = 11) Age (months, mean (SD)): intervention 31 (26); comparison 32 (19) Sex (M/F): intervention 5/3; comparison 5/2 Diagnostic criteria described: no (states number of clinical signs in the diagnostic criteria for KD in terms of patients with 5 signs compared to those with 6 signs was 5:2 vs 6:2) Inclusion criteria: patients with acute KD unresponsive to initial IVIG therapy (persistent or recurrent fever ≥ 37.5 ˚C 48 hours after single infusion 2 g/kg IVIG) Exclusion criteria: not described | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG 2 g/kg over 24 hours Comparison: IVMP 30 mg/kg/day for 3 days; heparin continuously infused 15 to 20 units/kg/h Concomitant medications: none stated | |
| Outcomes | Primary outcomes:
Secondary outcomes:
Cardiac evaluation: internal diameters of any coronary arteries, their Z scores (no further details) Time points: enrolment, daily to day 7 |
|
| Funding | Not reported | |
| Declaration of interest | Quote "Competing interests: none declared" | |
| Notes | IVIG: polyethylene glycol‐treated human immunoglobulin (Venoglobulin IH; Mitsubishi Pharma Corp, Osaka, Japan) The study was halted prematurely when 22 participants were recruited because of adverse effects of IVMP. Number of participants differs between the 2 reports (22 vs 15). We contacted the study authors, and they confirmed that the same participants were involved, but cytokines could only be measured in 15. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised, but no details provided Quote "At enrolment, the subjects were randomly assigned to either the IVMP group, 30 mg/kg of methyl‐ prednisolone per day for 3 consecutive days, or the additional IVIG group, 2 g/kg over 24 hours" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote "Treating physicians, echocardiographers, or patients’ families were not blinded, raising the possibility of a bias in interpreting the results." |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | Quote "Treating physicians, echocardiographers, or patients’ families were not blinded, raising the possibility of a bias in interpreting the results." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | Quote "Treating physicians, echocardiographers, or patients’ families were not blinded, raising the possibility of a bias in interpreting the results." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of participants differs between the 2 reports (22 vs 15), but this was explained by study authors (personal communication). |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes reported, but no protocol available. |
| Other bias | Unclear risk | The study was halted prematurely when 22 participants were recruited because of adverse effects of IVMP. |
Mori 2017.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: 14 (worsening KD) Intention‐to‐treat analysis: no Duration of study: May 2012 to September 2014 | |
| Participants | Country: Japan Setting: 10 medical institutions Number: 31 (intervention n = 15; comparison n = 16) Age (years, median (range)): intervention 2.5 (1 to 6); comparison 3.0 (1 to 4) Sex (M/F): intervention 11/4; comparison 10/6 Diagnostic criteria described: yes Inclusion criteria: patients diagnosed with KD aged 1 to 10 years; refractory to initial IVIG therapy (2 g/kg), defined as persistent fever of ≥ 38.0 ˚C (axillary temperature) and ≥ 4 h within 24 to 36 h after completion of the initial IVIG infusion and increases in either WBC count, neutrophil count, or CRP within 24 to 36 h since before initial IVIG administration, fever of ≥ 37.5 ˚C at enrolment, could be administered study drug within 8 days of illness onset (the first day) Exclusion criteria: patients with CAA before enrolment, BCG vaccination within 6 months before enrolment or no BCG vaccination; treatments other than initial IVIG for KD; corticosteroids (prednisolone equivalent of ≥ 1 mg/kg/day) within 4 weeks before enrolment; history of infliximab and other biologics; abnormal laboratory results after consent; complication or a history of infections; history of hypersensitivity to IVIG; immunodeficiency; or serious complications requiring hospitalisation | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG single dose 2 g/kg over 20 hours Comparison: infliximab single dose of 5 mg/kg over 2 hours Concomitant medications: ASA 30 to 50 mg/kg/day at acute stage and 3 to 5 mg/kg/day after defervescence | |
| Outcomes | Primary outcome: defervescence rate within 48 hours after the start of treatment Secondary outcomes:
Cardiac evaluation: CALs were defined as a coronary artery with an internal diameter of ≥ 3 mm in participants aged < 5 years or ≥ 4 mm in participants aged ≥ 5 years. Z‐scores were determined using the lambda‐mu‐sigma method. |
|
| Funding | Quote "Mitsubishi Tanabe Pharma Corporation sponsored this clinical trial and was responsible for the collection and analysis of data. The sponsor was involved with the study design and interpretation of data." | |
| Declaration of interest | Quote "Competing Interests: M.M. received personal fees from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and grants from Chugai Pharmaceutical Co., Ltd.; Ono Pharmaceutical Co., Ltd.; Mitsubishi Tanabe Pharma Corporation; UCB Japan Co., Ltd.; Towa Pharmaceutical Co., Ltd.; AbbVie G.K.; Japan Blood Products Organization; Ayumi Pharmaceutical Co.; CSL Behring; and Nippon Kayaku Co., Ltd.; and personal fees from AbbVie G.K.; MSD K.K.; Daiichi Sankyo Co., Ltd.; and Taisho Pharmaceutical Co., Ltd. outside the submitted work. T.H. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation outside the submitted work. M.K. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. H.S. received grants from Mitsubishi Tanabe Pharma Corporation, during the conduct of the trial and personal fees from Taisho Toyama Pharmaceutical Co., Ltd. outside the submitted work. T.M. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. S.I. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. T.O. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation and TEIJIN PHARMA Limited outside the submitted work. K.H. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation outside the submitted work. N.K. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation outside the submitted work. K.W. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. Y.S. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. Y.O. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial. H.Y. received personal fees from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation outside the submitted work. C.I. received personal fees from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Mitsubishi Tanabe Pharma Corporation outside the submitted work. T.K. received grants from Mitsubishi Tanabe Pharma Corporation during the conduct of the trial and personal fees from Actelion Pharmaceuticals Japan, Ltd.; Astellas Pharma Inc.; and Meiji Seika Pharma Co., Ltd. outside the submitted work. S.F. received personal fees from Mitsubishi Tanabe Pharma Corporation, Teijin Pharma Ltd., Nihon Pharmaceutical Co., Ltd.; and Japan Blood Products Organization outside the submitted work." | |
| Notes | Recruitment target was not reached. 5/16 and 9/15 participants receiving infliximab and IVIG discontinued the trial due to worsening KD (persistent fever or CALs development) and were switched to another treatment at physician’s discretion. IVIG: participants received 1 of 4 approved IVIG formulations in Japan as initial IVIG therapy: VGIH (Venoglobulin IH, Japan Blood Products Organization, Tokyo, Japan), freeze‐dried sulphonated human normal Ig (Kenketsu Venilon‐I, Teijin Co Ltd, Tokyo, Japan), freeze‐dried VGIH (Kenketsu Glovenin‐I, Nihon Pharmaceutical Co Ltd, Tokyo, Japan), or pH4‐treated acidic human normal Ig (Nisseki Polyglobin‐N 5%, 10% I.V., Japan Red Cross Society, Tokyo, Japan) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Randomization was performed centrally using a dynamic allocation method, with sex and age as assignment factors." |
| Allocation concealment (selection bias) | Low risk | Quote "Randomization was performed centrally using a dynamic allocation method, with sex and age as assignment factors." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote "Because of the difference in their infusion periods, infliximab and VGIH [IVIG] were administered open‐label." |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Assessors for CAL were blinded. Quote "CALs were assessed using echocardiography by a Central Review Committee, comprising three KD specialists who were blinded to patient information at all time points except baseline." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 17/31 completed the study (11 in infliximab group, 6 in IVIG group). |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported (NCT01596335). |
| Other bias | Unclear risk | Recruitment target was not reached. 5/16 and 9/15 participants receiving infliximab and IVIG, respectively, discontinued the trial due to worsening KD (persistent fever or CALs development) and were switched to another treatment at physician’s discretion. |
Morikawa 1994.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 15 Losses to follow‐up: 15 Intention‐to‐treat analysis: no Duration of study: September 1991 to January 1993 | |
| Participants | Country: Japan Setting: 95 hospitals Number: 451 (intervention group A n = 147; intervention group B n = 152; intervention group C n = 152) Age, years: 0 to 6 (< 1 year: 50, 52, 51; > 1 < 2 years: 30, 45, 41; > 2 < 3 years: 29, 26, 25; > 3 < 4 years: 19, 19, 18; > 4 < 5 years: 12, 7, 10; > 5 < 6 years: 7, 3, 7; group A, B, C respectively) Sex (M/F): intervention group A 86/61; intervention group B 87/65; intervention group C 87/65 Diagnostic criteria described: yes Inclusion criteria: KD patients enrolled within 9 days of onset, with day 1 defined as the first day of fever, less than 6 years old Exclusion criteria: relapse of KD, CAA before IVIG, IgA deficiency, history of allergic reaction to IVIG, received treatment with IVIG, steroid, or indometacin before referral to the study centre, severe renal failure | |
| Interventions | Primary or secondary KD treatment: primary Intervention group A: IVIG 200 mg/kg per day for 5 days Intervention group B: IVIG 400 mg/kg per day for 5 days Intervention group C: sulphonated IVIG 200 mg/kg per day for 5 days Concomitant medications: ASA 30 mg/kg per day until the fever subsided to < 37.5 ˚C then at 10 mg/kg per day until the 30th day after onset of the illness or the day of hospital discharge | |
| Outcomes | Primary outcome: CAA until 30 days
Secondary outcomes: duration of fever after administration of IVIG, AE Cardiac evaluation: 2‐dimensional ECG, recorded on a videotape and a photograph. Each coronary artery was categorised as non‐visualised, normal (< 3 mm diameter), dilatation (23 mm and < 5 mm diameter), medium aneurysm (35 mm and < 8 mm diameter), and large aneurysm (28 mm diameter) Time points: fever to 120 hours, CAA and AE to 30 days |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG Group A and B: polyethyleneglycol‐treated human immunoglobulin GB‐0998 (The Green Cross Corporation, Osaka, Japan) IVIG Group C: freeze‐dried, sulphonated human immunoglobulin (Teijin Co Ltd, Tokyo, Japan) Quote "Each study center, at which the patient was enrolled, had their own independent interpretation of echocardiograms. The disagreements between the center’s interpretation and that of the study committee were reevaluated and resolved by the individual study center, based on the interpretation of the study committee" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Patients were randomized to the three treatment groups by a central registration system. Randomization was per formed by the minimization method using age (less than one year vs at least one year), sex and study center as prognostic factors for balancing." |
| Allocation concealment (selection bias) | Low risk | Quote "Patients were randomized to the three treatment groups by a central registration system." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of participants and personnel not described. Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "Each patient’s echocardiograms were recorded on a video‐ tape and a photograph. Echocardiograms on photograph were interpreted blindly and independently by two pediatric cardiologists from the Study Committee composed of the authors, under the supervision of the statistician of this study, and videotapes were reviewed repeatedly when necessary." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes reported, but no protocol available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Nagashima 1987.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: July 1984 to April 1986 | |
| Participants | Country: Japan Setting: 16 hospitals Number 136 (intervention n = 69; comparison n = 67) Age (months, mean (SD)): intervention 25.6 (20.1); comparison 22.7 (14.4) Sex (M/F): intervention 46/23; comparison 41/26 Diagnostic criteria described: no Inclusion criteria: children admitted with KD within 10 days of onset Exclusion criteria: CAL before treatment | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 400 mg/kg for 1 to 2 hours for 3 days and ASA 30 mg/kg/day Comparison: ASA 30 mg/kg/day Concomitant medications: none stated | |
| Outcomes | CAL
Laboratory test (WBC, CRP, ESR, total serum protein, protein fractions, IgG, IgM, and IgA)
Febrile period
AE Cardiac evaluation: 2‐dimensional ECG > 3/week. Coronary arteries 3 to 5 mm were considered dilated; > 6 mm or spherical or spindle shape associated with lumen diameter ≥ 1.5 times diameter of adjacent vessel considered as aneurysms Time points: at enrolment, > 3 ECG per week to 30 days, temperature daily |
|
| Funding | None reported. | |
| Declaration of interest | Not reported | |
| Notes | IVIG: polyethylene glycol‐treated intact gammaglobulin (Venoglobulin I, Green Cross Corporation, Japan) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Registered by calling to the controller, with odd registration order being the gammaglobulin group and the even order being the ASA group |
| Allocation concealment (selection bias) | High risk | Registered by calling to the controller, with odd registration order being the gammaglobulin group and the even order being the ASA group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants. The outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessors. The outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessors. The outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Newburger 1986.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: 4 Intention‐to‐treat analysis: no Duration of study: February 1984 to September 1985 | |
| Participants | Country: USA Setting: 6 hospitals Number: 168 (intervention n = 84; comparison n = 84) Age (years, mean (SD)): intervention 2.7 (0.2); comparison 2.3 (0.2) Sex (M/F): intervention 49/35; comparison 50/34 (calculated) Diagnostic criteria described: yes Inclusion criteria: patients met 5 of 6 criteria of KD, enrolled within 10 days of onset, where day 1 was first day of fever Exclusion criteria: clinical or laboratory evidence of any other disease known to mimic KD | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 400 mg/kg/day over 2 hours for 4 days; plus ASA 100 mg/kg/day (80 to 120 mg/kg/day) every 6 hours to day 14 of illness, then reduced to 3 to 5 mg/kg/day single dose Comparison: ASA 100 mg/kg/day (80 to 120 mg/kg/day) every 6 hours until day 14 of illness, then reduced to 3 to 5 mg/kg/day single dose Concomitant medications: none | |
| Outcomes | Primary outcome: CAA
Secondary outcomes:
Cardiac evaluation: 2‐dimensional ECG of the right coronary artery, and left main, anterior descending and circumflex branches of the left coronary artery; at enrolment, 2 and 7 weeks. Defined as abnormal when diameter of the lumen was at least 3 mm or 1.5 times as large as diameter of adjacent vessel Time points: enrolment, 2 and 7 weeks |
|
| Funding | Quote "Supported by grants (HL 34545, RR 2172, RR 69, and RR 827) from the National Institutes of Health" | |
| Declaration of interest | Not reported | |
| Notes | IVIG: intact, unmodified, supplied by Immuno AG (Austria) Not all participants in ASA group hospitalised. Only hospitalised participants used in fever analysis to prevent bias from home reporting. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "The coordinating center developed randomization schemes for each age‐sex group at each clinical center and supplied the centers with four sets of sealed, serially numbered, opaque envelopes containing the subjects' treatment assignments" |
| Allocation concealment (selection bias) | Low risk | Quote "...four sets of sealed, serially numbered, opaque envelopes containing the subjects' treatment assignments" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Echocardiograms recorded and interpreted blindly and independently by 2 paediatric echocardiographers from other centres. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Newburger 1991.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: 6 Intention‐to‐treat analysis: no Duration of study: May 1986 to November 1989 | |
| Participants | Country: USA Setting: 7 centres Number: 549 (intervention n = 273; comparison n = 276) Age (years, mean (SD)): intervention 2.9 (0.1); comparison 2.9 (0.1) Sex (M/F): intervention 164/109; comparison 164/112 Diagnostic criteria described: yes Inclusion criteria: fever plus 4 of 5 diagnostic criteria, enrolled within 10 days of onset, day 1 defined as first day of fever Exclusion criteria: clinical or laboratory evidence of any disease known to mimic KD, treatment with IVIG before referral | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 2 g/kg over 8 to 12 hours (single infusion) Comparison: IVIG 400 mg/kg/day over 2 hours for 4 days Concomitant medications: ASA 80 to 100 mg/kg/day to day 14 then 3 to 5 mg/kg/day | |
| Outcomes | Primary outcomes:
Secondary outcomes:
Cardiac evaluation: 2‐dimensional ECG of the right coronary artery, and left main, anterior descending and circumflex branches of the left coronary artery and posterior descending coronary artery ‐ at enrolment, 2 and 7 weeks. Each coronary artery categorised as non visualised, normal or abnormal (showing ectasia or aneurysm). Defined as abnormal if the lumen diameter (inside to inside) ≥ 3 mm in a child < 5 years of age, or ≥ 4 mm in ≥ 5 years of age; or if the lumen diameter of a segment ≥ 1.5 times that of an adjacent segment; or clearly irregular Time points: enrolment, 2 and 7 weeks |
|
| Funding | Quote "Supported by grants (HL 34545, RR 02172, and RR 69) from the National Institutes of Health" | |
| Declaration of interest | Not reported | |
| Notes | IVIG: Immuno AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "The coordinating center developed randomization schemes for each age‐and‐sex group at each clinical center and supplied the centers with four sets of sealed, serially numbered, opaque envelopments that contained the patient treatment assignments." |
| Allocation concealment (selection bias) | Low risk | Quote "...sealed, serially numbered, opaque envelopments that contained the patient' treatment assignments." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "Each patient's echocardiograms were recorded on a single videotape in chronologic order and were interpreted blindly and independently by two pediatric echocardiographers." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported (NCT00000520). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Nishihara 1988.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 18 (clinical features and dose/duration of IVIG did not meet the criteria) Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: July 1984 to March 1988 | |
| Participants | Country: Japan Setting: 13 paediatric clinics Number: 160 (intervention group A: n = 32; intervention group B: n = 42; intervention group C: n = 36; control* n = 32) Age (months, mean (SD)): intervention group A 17.7 (14.2); intervention group B 19.9 (14.4); intervention group C 19.6 (14.1); control 15.1 (8.6) Sex (M/F): data not provided Diagnostic criteria described: no Inclusion criteria: full clinical expression of KD and under 4 years of age, treatment started within 7 days after the onset Exclusion criteria: treatment given before the study | |
| Interventions | Primary or secondary KD treatment: primary Intervention group A: IVIG 50 to 100 mg/kg/day for 5 days Intervention group B: IVIG 200 mg/kg/day for 5 days Intervention group C: IVIG 400 mg/kg/day for 5 days Control*: ASA 30 mg/kg/day Concomitant medications: ASA 30 mg/kg/day | |
| Outcomes | CAA
Fever
Laboratory data Cardiac evaluation: 2‐dimensional ECG were done once a week for at least 3 weeks, including views of the right coronary artery and of the left main, anterior descending, and circumflex branches of the left coronary artery. The views were categorised into 3 depending on the largest diameter of the coronary artery at the third week of examination: score 0 (normal) for cases of a diameter < 3 mm; and score 2 (severe) for cases > 5.5 mm. The remaining participants scored 1 (mild). Time points: 1, 2, 3 weeks |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | Data reported in a letter. *Patients treated in clinics with ASA were controls ‐ not randomised to treatment, so data from this group were not used in this review. IVIG: sulphonated human gammaglobulin or polyethylene‐glycol‐treated human gammaglobulin | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "The views were interpreted blindly and independently" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Results published as a letter. No other outcomes except for coronary abnormalities reported. |
| Other bias | Unclear risk | Results published as a letter, so likely not peer reviewed. |
Nonaka 1995.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: 9 (accessible administration of another drug) Losses to follow‐up: 1 Intention‐to‐treat analysis: no Duration of study: January 1991 to September 1994 | |
| Participants | Country: Japan Setting: hospital Number: 90 (intervention n = 50; comparison n = 40) Age (months, mean (SD)): intervention 19.9 (16.4); comparison 25.3 (20.3) Sex (M:F): intervention 1.4:1; comparison 1.7:1 Diagnostic criteria described: no Inclusion criteria: children with KD with less than 8 days since onset Exclusion criteria: none described | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 400 mg/kg for 3 days Comparison: prednisolone 2 mg/kg IV for 5 days then 2 mg/kg orally until CRP fell to negative Concomitant medications: ASA 50 mg/kg/day and dipyridamole 5 mg/kg/day (until CRP normalised). Both groups also received ASA 10 mg/kg/day and dipyridamole 5 mg/kg/day during admission, and ASA 5 mg/kg after discharge. | |
| Outcomes | Temperature
Febrile period
Laboratory data (CRP, serum albumin, total protein)
CAL Cardiac evaluation: 2‐dimensional ECG at enrolment and follow‐up. CAA as defined by JKDRC (1 of: dilated lumen diameter of at least 3 mm in children < 5 years and at least 4 mm in children ≥ 5 years; internal diameter at least 1.5 times that of adjacent segment; or lumen clearly irregular) Time points: acute, 30 days, 3 months |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG: no details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 100 children randomised, but results only reported for 90 total, reasons not all clear. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Unclear risk | Possible imbalance in age distributions between groups (13 to 24 months 30%:15% and 37 to 48 months 6%:17.5%, IVIG:prednisolone respectively) |
Ogawa 1987.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 142 were randomised (25 cases were excluded from study analysis: 19 cases did not meet the inclusion criteria; 1 case in IVGG was high dose, 4 cases in IVGG were low dose, and 1 case in IVGG steroid was used) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: July 1985 to June 1986 | |
| Participants | County: Japan Setting: 31 hospitals Number: 117 (intervention n = 63; comparison n = 54) Age (months, mean (SD)): intervention 27.8 (22.2); comparison 26.5 (21.8) Sex (M/F): intervention 35/28; comparison 38/16 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset before treatment, no steroid or indometacin or IVIG use Exclusion criteria: not provided | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG (400 mg/kg/day for 3 consecutive days) plus ASA (30 mg/kg/day) Comparison: ASA (30 mg/kg/day, reduced to 10 mg/kg once a day after CRP‐negative) Concomitant medications: none reported | |
| Outcomes | CAL (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset), frequency of occurrence of the 6 main symptoms (fever, rash, conjunctival hyperaemia, oral‐labial findings, cervical lymph node findings, extremity terminal changes), laboratory findings (CRP, ESR), side effects Cardiac evaluation: 2‐dimensional ECG (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset). A coronary artery inner diameter of 3 mm or more, or 1.5 times the diameter of the surrounding coronary artery was considered abnormal. Aneurysm greater than 4 times the diameter of the surrounding coronary artery was defined as aneurysm large (ANI), greater than 1.5 times and less than 4 times the diameter of the surrounding coronary artery was defined as aneurysm middle (ANm), and less than 1.5 times the diameter of the surrounding coronary artery were defined as aneurysm small (ANs) or Dil. |
|
| Funding | None reported. Quote "We thank Chemo‐Sero‐Therapeutic Research Institute, Fujisawa yakuhin and TelJin Ltd for donating S‐sulphonated gammaglobulin (Venilon)" | |
| Declaration of interest | Not reported | |
| Notes | IVIG: S‐sulphonated intact gammaglobulin; Venilon, Teijin Ltd, Japan This is study 2 of 3 reported by Ogino 1990. We requested additional information regarding randomisation and data. The author can no longer be contacted. The co‐author did not have any additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reports groups were assigned at the direction of an independent controller, but no details provided |
| Allocation concealment (selection bias) | Low risk | States central randomisation by an independent controller |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Unclear risk | States re‐examination by review committee, but no further details |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement of low risk or high risk ‐ states re‐examination by review committee, but no further details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6/123 participants were not included in analysis. These were all in the IVIG group (given a low dose). It was not clear if this could have impacted the results. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Ogino 1987.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 115 were randomised (23 cases were excluded from study analysis: 19 cases did not meet the inclusion criteria; 3 cases in IVGG were low dose, and 1 case in ASA used IVIG) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: May 1984 to April 1985 | |
| Participants | County: Japan Setting: 33 hospitals Number: 92 (intervention n = 50; comparison n = 42) Age (months, mean (SD)): intervention 32.1 (24.5); comparison 27.6 (27.6) Sex (M/F): intervention 29/21; comparison 32/10 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset, no steroid, indometacin, or IVIG used before treatment Exclusion criteria: recurrent or incomplete KD | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG (200 mg/kg/day for 3 consecutive days) plus ASA (30 mg/kg/day) Comparison: ASA (30 mg/kg/day, reduced to 10 mg/kg once a day after CRP‐negative) Concomitant medications: none | |
| Outcomes | CAL (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset), frequency of occurrence of the 6 main symptoms (fever, rash, conjunctival hyperaemia, oral‐labial findings, cervical lymph node findings, extremity terminal changes), laboratory findings (CRP, ESR), side effects Cardiac evaluation: 2‐dimensional ECG (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset). Defined as: a coronary artery inner diameter of 3 mm or more, or 1.5 times the diameter of the surrounding coronary artery was considered abnormal. An aneurysm greater than 4 times the diameter of the surrounding coronary artery was defined as aneurysm large (ANl), greater than 1.5 times and less than 4 times the diameter of the surrounding coronary artery was defined as aneurysm middle (ANm), and less than 1.5 times the diameter of the surrounding coronary artery was defined as aneurysm small (ANs) or Dil. |
|
| Funding | None reported. Quote "We thank Chemo‐Sero‐Therapeutic Research Institute, Fujisawa yakuhin and TelJin Ltd for donating S‐sulphonated gammaglobulin (Venilon)" | |
| Declaration of interest | None reported. | |
| Notes | IVIG details: S‐sulphonated intact gammaglobulin; Venilon, Teijin Ltd, Japan This is study 1 of 3 reported in Ogino 1990. We requested additional information regarding randomisation and data. The author can no longer be contacted. The co‐author did not have any additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reports groups were assigned at the direction of an independent controller, but no details provided. |
| Allocation concealment (selection bias) | Low risk | States central randomisation by an independent controller. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Unclear risk | States evaluation for CAL by independent review committee, but no further details. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Unclear risk | No description. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/96 participants not included in analysis, but reasons provided. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Okuni 1987A.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 3 Losses to follow‐up: 1 Intention‐to‐treat analysis: yes Duration of study: October 1983 to February 1985 | |
| Participants | Country: Japan Setting: hospital Number: 214 (intervention n = 139 (pepsin treated n = 73, intact n = 66); comparison n = 75) Age (months, mean (SD)): intervention (pepsin treated 21.6 (14.7), intact 19.2 (15.4)); comparison 22.1 (15.0) Sex (M/F): intervention (pepsin treated 40/33, intact 36/30); comparison 47/28 Diagnostic criteria described: no Inclusion criteria: satisfied diagnostic criteria for KD, < 7 days KD onset, ≤ 4 years old Exclusion criteria: previously treated with indometacin or corticosteroids | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 100 mg/kg single dose plus ASA 50 mg/kg/day until temperature < 37.5 ˚C, then 30 mg/kg/day Comparison: ASA 50 mg/kg/day until temperature < 37.5 ˚C, then 30 mg/kg/day Concomitant medications: none | |
| Outcomes | CAA (enrolment ‐ 60 days, and at 1 year if present at 60 days)
Laboratory test (enrolment ‐ 60 days) Cardiac evaluation: 2‐dimensional ECG at enrolment and at least once a week in acute phase, then 30 to 60 days from onset. If CAA detected at 60 days, examined at 1 year after onset. Classified as normal, dilation and aneurysm "by the classification standard by Research Committee of Kawasaki Disease" (JMHW 1984) |
|
| Funding | Quote "I gratefully acknowledge the support of the Kawasaki Disease Research Committee of Japan for this study" (from Harada 1991) | |
| Declaration of interest | Not reported | |
| Notes | IVIG: pepsin‐treated and intact gamma globulin used This study is the same as study 1 (of 3) reported in Harada 1991 (now merged). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "These patients randomly assigned to each treatment group, for the three stages of the study". States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. Unclear if this could have impacted outcomes |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | ECGs recorded (stop motion/video) and interpreted by independent observers (from Harada 1991 report). |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No description of blinding for assessment of any other outcome. Unclear if this could have affected other outcome reporting (from Harada 1991 report) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data, all accounted for |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Okuni 1987B.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: 18 Intention‐to‐treat analysis: yes Duration of study: February 1985 to March 1986 | |
| Participants | Country: Japan Setting: hospital Number: 295 (intervention n = 196 (pepsin treated n = 96, intact n = 100); comparison n = 99) Age (months, mean (SD)): intervention (pepsin treated 21.0 (13.4), intact 17.7 (11.3)); comparison 18.5 (12.1) Sex (M/F): intervention (pepsin treated 63/33, intact 59/41); comparison 58/41 Diagnostic criteria described: no Inclusion criteria: satisfied diagnostic criteria for KD, < 7 days onset, ≤ 4 years old Exclusion criteria: previously treated with indometacin or corticosteroids | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 100 mg/kg day for 5 days plus ASA 50 mg/kg/day until temperature < 37.5 ˚C, then 30 mg/kg/day Comparison: ASA 50 mg/kg/day until temperature < 37.5 ˚C, then 30 mg/kg/day Concomitant medications: none stated | |
| Outcomes | CAA (enrolment ‐ 60 days, and at 1 year if present at 60 days)
Laboratory test (enrolment ‐ 60 days) Cardiac evaluation: 2‐dimensional ECG at enrolment and at least once a week in acute phase, then 30 to 60 days from onset. If CAA detected at 60 days, examined at 1 year after onset. Classified as normal, dilation and aneurysm "by the classification standard by Research Committee of Kawasaki Disease" (JMHW 1984) |
|
| Funding | Quote "I gratefully acknowledge the support of the Kawasaki Disease Research Committee of Japan for this study" (from Harada 1991) | |
| Declaration of interest | Not reported | |
| Notes | IVIG: pepsin‐treated and intact gamma globulin used This study is the same as study 2 (of 3) reported in Harada 1991. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote translated "These patients randomly assigned to each treatment group, for the three stages of the study" (from Harada 1991 report). States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. Unclear if this could have impacted outcomes |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | ECGs recorded (stop motion/video) and interpreted by independent observers. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No description of blinding for assessment of any other outcome. Unclear if this could have affected other outcome reporting (from Harada 1991 report) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcome of CAA reported, but no protocol available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Onouchi 1988.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 22 Losses to follow‐up: 3 Intention‐to‐treat analysis: no Duration of study: April 1986 to April 1987 | |
| Participants | Country: Japan Setting: 28 institutions Number: 126 (intervention group A: n = 38, group B: n = 42; comparison: n = 46) Age (months, mean (SD)): group A 22.2 (15.6), group B 23.4 (14.4); comparison 17.0 (12.0) Sex (M/F): group A (18/20), group B (26/16); comparison (32/14) Diagnostic criteria described: yes Inclusion criteria: patients with KD, < 5 years old, treatment initiated within 7 days of KD onset Exclusion criteria: steroid, indometacin, or IVIG prior to study treatment, recurrent disease | |
| Interventions | Primary or secondary KD treatment: primary Intervention group A: IVIG 200 mg/kg/day for 3 days with ASA 50 mg/kg/day until afebrile, then reduced to 30 mg/kg/day Intervention group B: IVIG 400 mg/kg/day for 3 days with ASA 50 mg/kg/day until afebrile, then reduced to 30 mg/kg/day Comparison: ASA 50 mg/kg/day until afebrile, then reduced to 30 mg/kg/day Concomitant medications: none stated | |
| Outcomes | Clinical symptoms (fever, rash, conjunctival congestion, oral cavity and lip findings, cervical lymph node swelling, abnormalities in hands and feet)
CAL
Laboratory tests (RBC, WBC, PLT, total protein, blood biochemistry, urinalysis)
AE Cardiac evaluation: 2‐dimensional ECG of the left coronary artery main trunk, anterior descending branch, circumflex branch and right coronary artery at start of treatment, 15, 30, and 60 days after disease onset. Graded scale was either normal, dilated lesion or aneurysm (medium sized or large) "according to previously published standards (JMHW 1984)". Time points: enrolment, days 15, 30, and 60 |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG: reduced alkylated human IG; Polyglobulin Bayer Yakuhin, Ltd | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised, but sequence appears to have been decided by rule based on hospital visit order using alternate envelope allocation and so not truly random. Quote "The controller assigned one case to each treatment for a total of three cases comprising a single set." Controllers randomly assigned a set of different medication. |
| Allocation concealment (selection bias) | Unclear risk | In the order of receipt of eligible patients, open the envelopes from the lowest number and administer the prescriptions listed inside. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "CAL evaluations were conducted by a committee who based their evaluation on recorded 2DE videotapes. They were blind to treatment involved" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Low risk | Non‐cardiac outcomes assessments were performed by independent members. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | More participant data available for AE (145) than for cardiac evaluation (126), exclusions described. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Unclear risk | Some baseline imbalances between groups reported (more females and lower mean age in the ASA group). |
Onouchi 1992.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 9 Losses to follow‐up: 4 Intention‐to‐treat analysis: no Duration of study: October 1990 to September 1991 | |
| Participants | Country: Japan Setting: 39 institutions Number: 160 (group A (n = 53); group B (n = 51); group C (n = 56)) Age (months, mean (SD)): group A 21.0 (15.8); group B 20.1 (16.3); group C 23.3 (16.8) Sex (M/F): group A 31/22; group B 30/21; group C 30/26 Diagnostic criteria described: yes Inclusion criteria: patients with KD, < 5 years old, treatment initiated within 7 days of KD onset Exclusion criteria: steroid, indometacin, or IVIG prior to study treatment, recurrent disease | |
| Interventions | Primary or secondary KD treatment: primary Intervention group A: IVIG 100 mg/kg/day for 5 days with ASA 30 mg/kg/day Intervention group B: IVIG 200 mg/kg/day for 5 days with ASA 30 mg/kg/day Intervention group C: IVIG 400 mg/kg/day for 5 days with ASA 30 mg/kg/day Concomitant medications: none stated | |
| Outcomes | Clinical symptoms (fever, rash, conjunctival congestion, oral cavity and lip findings, cervical lymph node swelling, abnormalities in hands and feet)
CAL
Laboratory tests (RBC, WBC, PLT, total protein, blood biochemistry, urinalysis)
AE Cardiac evaluation: 2‐dimensional ECG of the left coronary artery main trunk, anterior descending branch, circumflex branch and right coronary artery at start of treatment, 15, 30, and 60 days after disease onset. Graded scale was either normal, dilated lesion or aneurysm (medium‐sized or large) "according to previously published standards (JMHW 1984)". Time points: enrolment, days 15, 30, and 60 |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG: pH4 stabilised acid human IG, Polyglobulin N‐Bayer Yakuhin Ltd | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised centrally, but unclear if sequence was decided by physician. Quote "Controllers randomly assigned a set of three different medication doses" |
| Allocation concealment (selection bias) | Low risk | Controllers randomly assigned a set of 3 different medication doses. The investigators opened the envelope in the order of enrolment of eligible participants, starting with the lowest numbered envelope, and administered the listed prescriptions. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "CAL evaluations were conducted by a committee who based their evaluation on recorded 2DE videotapes. They were blind to treatment involved" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Low risk | Non‐cardiac outcomes assessments were performed by independent members. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9/169 participants not included in analysis, but reasons provided. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Qin 2006.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: none described Losses to follow‐up: 93.4% followed up to 12 months Intention‐to‐treat analysis: unclear Duration of study: July 2000 to October 2005 | |
| Participants | Country: China Setting: hospital Number: 242 (intervention n = 120; comparison n = 122) Age (mean (SD)): mean 4.0 (2.8) years (range 3 months to 14 years; 83.1% < 5 years) Sex (M:F): 1.66:1; intervention 69/51; comparison 82/40 Diagnostic criteria described: yes Inclusion criteria: children with KD. Typical cases meet the KD diagnostic criteria revised by the 3rd International Kawasaki Disease Conference, atypical cases meet at least 3 to 4 main clinical manifestations including fever and CAD formally confirmed by ECG, age < 14 years. Exclusion criteria: irregular ASA or IVIG treatment prior to admission, disease duration > 10 days, KD combined with other congenital heart malformations | |
| Interventions | Primary or secondary KD treatment: primary (within 7 to 10 days of illness) Intervention: IVIG 2 g/kg single IV injection over 8 to 12 hours Comparison: IVIG 1 g/kg single IV injection over 8 to 12 hours Concomitant medications: ASA 80 to 100 mg/kg/d, reduced once fever controlled; if the participant has CAD, ASA continued until diameter normal | |
| Outcomes | CAL, fever, clinical symptoms, WBC, PLT, serum IgG, CRP, ESR, ECG Cardiac evaluation: unclear Time points: enrolment and 2 weeks (follow‐up range 4 months to 5.4 years) |
|
| Funding | National Natural Science Foundation of China | |
| Declaration of interest | None reported. | |
| Notes | Translated Lyophilised low pH human blood IVIG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Translation: randomly divided into 2 groups according to gender, age, stage of the disease, with/without CAL, with/without high‐risk factors States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants and personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Other bias | Low risk | No evidence of other bias |
Sakata 2007.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none described Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: January 2000 to December 2002 | |
| Participants | Country: Japan Setting: hospital Number: 109 (intervention n = 54; comparison n = 55) Age (months, mean (SD)): 28.0 (21.0); intervention 28.89 (19.73); comparison 27.25 (21.95) Sex (M/F): 61/48 Diagnostic criteria described: no Inclusion criteria: KD admitted before day 7 of onset, additional IVIG administered when patient showed 2 or 3 criteria 24 to 36 hours after previous IVIG dose: body temperature > 37.5 ˚C, CRP > 3.0 mg/dL and neutrophils ≥ 7500/mm3 Exclusion criteria: CAL at time of admission, treated with other drugs during the clinical course | |
| Interventions | Primary or secondary KD treatment: primary with additional therapy Intervention: IVIG 2 g/kg single infusion (additional therapy 2 g/kg) Comparison: IVIG 1 g/kg single infusion (1st additional therapy 1 g/kg, and 2nd 2 g/kg) Concomitant medications: ASA 30 mg/kg/day, reduced to 10 mg/kg/day once body temperature ≤ 37.5 ˚C, further reduced to 5 mg/kg/day when CRP ≤ 0.5 mg/dL. ASA was continued for at least 2 months, even if no symptoms of CAL. Flurbiprofen administered in participants with liver dysfunction. | |
| Outcomes | Total dose of IG
CAL
Plasma IG concentration Cardiac evaluation: serial UCG days 5, 7, 10, 14, 21, and 28, of coronary arteries. CAL defined as intact (no morphological change in coronary arteries during clinical course); transient dilation (transient dilated coronary arteries regressed to their normal size with 1 month of illness); aneurysm (diameter of right or left coronary artery > 4 mm or 1.5 times that or coronary orifice at 1 month within onset of illness). If both transient dilation and aneurysm, then regarded as CAL. Abstract reports serial ECG until day 60, no further details. |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG: Venilon (Teijin Pharma, Japan), Venoglobulin‐IH (Venesis, Japan) or Polyglobin‐N (Bayer Yakuhin, Japan), choice institute‐dependent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "a randomization code was generated using a random number table such that the number of patients assigned to each protocol group was almost similar" |
| Allocation concealment (selection bias) | Low risk | Quote "Randomization to either protocol was performed with sequentially numbered, sealed envelopes using the previously determined code." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote "The clinicians treating the patients were blinded to the protocol." |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "The UCG was performed by the same paediatric cardiologists, and the findings recorded on a video were evaluated by more than four paediatric cardiologists." |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Unclear risk | No blinding of outcome assessment described, but total Ig and plasma Ig unlikely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Sato 1995.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: yes Duration of study: January 1991 to December 1995 | |
| Participants | Country: Japan Setting: hospital Number: 145 (intervention n = 72; comparison n = 73) Age (months, mean (SD)): intervention 23.9 (21.7); comparison 22.0 (17.6) Sex (M/F): intervention 46/26; comparison 47/27 Diagnostic criteria described: yes Inclusion criteria: patients with KD, 9 days of onset, scoring ≥ 4 on Harada score Exclusion criteria: ≤ 3 on Harada score | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG 2 g/kg single treatment over 12‐hour infusion Comparison: IVIG 400 mg/kg/day for 5 days over 2‐ to 3‐hour infusions Concomitant medications: ASA 30 mg/kg/day in acute febrile phase and 5 mg/kg/day when afebrile | |
| Outcomes | Primary outcome: CAA
Secondary outcomes:
Cardiac evaluation: 2‐dimensional ECG (at admission, day 4/5, and discharge) of main trunk, anterior descending and circumflex branches of the left coronary artery and the main and distal segments of the right coronary artery. Graded as aneurysmal if the internal lumen diameter was at least 3 mm in children < 5 years or at least 4 mm in children ≥ 5 years; or if the internal diameter was at least 1.5 times that of an adjacent segment. If CAA indicated, coronary angiograms were taken in the convalescent phase. Time points: enrolment, day 4/5 and 7 (approximately discharge) |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | Harada score used, those ≤ 3 on Harada score did not receive IVIG, only ASA (not randomised) IVIG: S‐sulphonated human IG (Kenketsu Venilon‐I, Kaketsuken, Japan) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "We randomly assigned participating patients to treatment groups by means of a stratified randomization according to age (<1 year vs 1 year) and gender (male vs female). Using this random number table..." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants and personnel |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Low risk | Quote "Each patient’s echocardiogram was recorded on a single videotape and reviewed by pediatric cardiologists who were unaware of patient identity" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns about missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Unclear risk | Baseline differences reported in age and blood tests between IVIG and no IVIG group. |
Wang 2020.
| Study characteristics | ||
| Methods | Design: RCT Exclusions postrandomisation: none Losses to follow‐up: 47* Intention‐to‐treat analysis: yes Duration of study: January 2018 to June 2019 | |
| Participants | Country: China Setting: hospital Number: 80 (intervention n = 40; comparison n = 40) Age (months, mean (SD)): intervention 21.0 (14.4); comparison 25.6 (21.1) Sex (M/F): intervention 28/11; comparison 28/13 Diagnostic criteria described: yes Inclusion criteria: diagnosed and hospitalised KD patients initially treated with IVIG then assessed as IVIG resistant (recrudescent or persistent fever at least 36 hours after first IVIG infusion) Exclusion criteria: presence of other diseases that affect temperature in the course of KD (sepsis, influenza, and juvenile idiopathic arthritis), absence of detailed information about initial treatment outside the hospital, prior history of KD, treatment with hormone or immunosuppressant therapy in preceding 30 days, presence of severe immune disease (immunodeficiency or chromosomal abnormality), refusal to sign informed consent, inability to follow up for at least 6 months | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG 2 g/kg single infusion Comparison: MPT 15 mg/kg/day IV for 3 days Concomitant medications: ASA 30 to 50 mg/kg/day; all participants initially treated with IVIG 2 g/kg and ASA 30 to 50 mg/kg/day within the first 10 days of fever onset | |
| Outcomes | Primary outcomes: CAL
Secondary outcomes:
Cardiac evaluation: maximal Z‐scores from ECG assessment of luminal dimensions are categorised as follows:
Time points: enrolment, 48 hours (fever), 1 week (laboratory data, CAL), 1, 3, 6, 12, 24 months (CAL) |
|
| Funding | Quote "This study was supported by the Guangdong Natural Science Fund, China (grant number 2016A030313836), and the Guangdong Science and Technology Project of China (grant number 2017A030223003)" | |
| Declaration of interest | Quote "The authors declare no competing financial interests" | |
| Notes | *As no CAL detected, participants did not return to hospital for further checkups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Non‐participating nurses generated the random tables using a computer. Once eligible subjects had entered the trial, the nurses assigned the groups to trial researchers for clinical trial intervention" |
| Allocation concealment (selection bias) | Low risk | Quote "Once eligible subjects had entered the trial, the nurses assigned the groups to trial researchers for clinical trial intervention" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants and personnel |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment, and the outcome measurement could have been influenced by lack of blinding (strict diagnosis criteria of CAL described, but still high risk as may not prevent bias) |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported as planned in protocol (ChiCTR‐EOC‐17013266). |
| Other bias | Unclear risk | Although randomisation procedure described, protocol states this is a cohort study, without randomisation. |
Yabiku 1989.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: 124 were randomised (40 cases were excluded from study analysis: 32 cases did not meet the inclusion criteria, 8 cases in IVIG group were given low dose) Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: October 1986 to February 1988 | |
| Participants | Country: Japan Setting: 33 hospitals Number: 84 (intervention n = 48; comparison n = 36) Age (months, mean (SD)): intervention 21.4 (18.1); comparison 24.9 (15.0) Sex (M/F): intervention 29/19; comparison 18/18 Diagnostic criteria described: yes Inclusion criteria: treated for KD within 7 days of onset, no steroid, indometacin, or IVIG use before treatment Exclusion criteria: recurrent or incomplete KD | |
| Interventions | Primary or secondary KD treatment: primary Intervention: IVIG (1000 mg/kg/day single dose) plus ASA (30 mg/kg/day) Comparison: ASA (30 mg/kg/day, reduced to 10 mg/kg once a day after CRP‐negative) Concomitant medications: no | |
| Outcomes | CAL (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset), frequency of occurrence of the 6 main symptoms (fever, rash, conjunctival hyperaemia, oral‐labial findings, cervical lymph node findings, extremity terminal changes), laboratory findings (CRP, ESR), side effects Cardiac evaluation: 2‐dimensional ECG (1 to 10 days, 11 to 25 days, 30 days, 60 days after KD onset). Defined as: coronary artery inner diameter of 3 mm or more, or 1.5 times the diameter of the surrounding coronary artery was considered abnormal. Aneurysm greater than 4 times the diameter of the surrounding coronary artery was defined as aneurysm major (ANI), greater than 1.5 times and less than 4 times the diameter of the surrounding coronary artery was defined as aneurysm moderate (ANm), and less than 1.5 times the diameter of the surrounding coronary artery was defined as aneurysm minor (ANs) or Dil. |
|
| Funding | None reported. | |
| Declaration of interest | None reported. | |
| Notes | IVIG: S‐sulphonated intact gammaglobulin; Venilon, Teijin Ltd, Japan This is study 3 of 3 reported in Ogino 1990 Progress in Medicine. We requested additional information regarding randomisation and data. The author can no longer be contacted. The co‐author did not have any additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reports groups were assigned at the direction of an independent controller, but no details provided |
| Allocation concealment (selection bias) | Low risk | States central randomisation by an independent controller |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | Unclear risk | There were insufficient details on blinding provided, but study reports that the final evaluation for CAL was carried out by an independent review committee. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | Unclear risk | No description of blinding provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8/90 participants were not included in analysis. These were all in the IVIG group (given a low dose). It was not clear if this may have impacted the results. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Unclear risk | Imbalance in numbers across intervention (8 participants in IVIG group removed from analysis, no dropouts in ASA group) |
Youn 2016.
| Study characteristics | ||
| Methods | Design: multicentre RCT Exclusions postrandomisation: none Losses to follow‐up: none Intention‐to‐treat analysis: no Duration of study: January 2010 to June 2015 | |
| Participants | Country: Korea Setting: hospital Number: 43 (intervention n = 32; comparison n = 11) Age (range): 3 months to 13 years (data per group not given, but states no baseline differences) Sex (M/F): 28/15 Diagnostic criteria described: initial KD no, retreatment indicated according to institutional KD guidelines Inclusion criteria: persistent or recrudescent fever ≥ 38.0 ˚C beyond 36 to 48 hours after completion of initial IVIG infusion according to institutional guideline Exclusion criteria: none given | |
| Interventions | Primary or secondary KD treatment: secondary Intervention: IVIG 2 g/kg Comparison: infliximab 5 mg/kg, paracetamol (15 mg/kg orally), and chlorpheniramine (2 mg or 4 mg IV) were administered 30 minutes before infliximab infusion Concomitant medications: initial treatment was IVIG 2 g/kg plus ASA 80 to 100 mg/kg/d for 2 to 8 days after the onset of disease | |
| Outcomes | Need for further treatment
Duration of fever elapsed from completion of first retreatment to defervescence (< 37.5 ˚C)
Total days of hospitalisation
CAL
AE
Laboratory data (WBC, PLT counts, aspartate aminotransferase, alanine aminotransferase, protein, albumin, CRP, and N‐terminal pro‐brain natriuretic peptide) Cardiac evaluation: ECG at entry, 1 to 2 weeks, 6 to 8 weeks after retreatment. CAL determined by the criteria of Japanese Ministry of Health and Welfare (JMHW 1984). Changes from baseline were not calculated. Time points: enrolment, day 7, and 1, 3, 6, 12, 24 months |
|
| Funding | Not reported. | |
| Declaration of interest | Quote "The authors have no funding or conflicts of interest to disclose" | |
| Notes | Imbalance in group numbers "...associated with patient selection according to the change in standard practice for patients with IVIG resistant KD in our institution during the study period" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised, but insufficient information to permit judgement of low risk or high risk |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment, and the outcome measurement could have been influenced by lack of blinding. Quote "...echocardiograms were not read blindly" |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No concerns over missing data |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol. |
| Other bias | Unclear risk | Numbers imbalanced between groups, and mention of a change to standard practice for IVIG‐resistant KD during study which caused this. |
Yuan 2000.
| Study characteristics | ||
| Methods | Design: CCT, a parallel study Exclusions postrandomisation: unclear Losses to follow‐up: not reported Intention‐to‐treat analysis: unclear Duration of study: March 1996 to March 1998 | |
| Participants | Country: China Setting: hospital Number: 50 (intervention n = 25; comparison n = 25) Age (months, mean and range): intervention 45 (8 to 90); comparison 53 (9 to 84) Sex (M/F): intervention 13/12; comparison 15/10 Diagnostic criteria described: yes Inclusion criteria: patients were admitted to the paediatric department in hospital between March 1996 and March 1998 and met the clinical diagnostic criteria for KD Exclusion criteria: not specified | |
| Interventions | Primary or secondary KD treatment: primary Intervention: 1 g/kg/d IVIG for 2 days Comparison: IVMP 2 mg/kg/d for 5 days then oral prednisolone until CRP‐negative Concomitant medications: ASA 50 mg/kg/d, oral dipyridamole if CAA detected | |
| Outcomes | Duration of acute symptoms (fever, conjunctival congestion, swelling of hands and feet, swollen lymph nodes in the neck), laboratory indices, CAA Cardiac evaluation: ECG and echocardiography at 2 weeks, 3, 6, and 9 months, 1 year post‐treatment. Assessment of CAA not clear (subjectively described) Time points: 2 weeks, 3, 6, 9, and 12 months |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | IVIG details: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not truly random ‐ used odd/even hospital numbers (quasi‐RCT) |
| Allocation concealment (selection bias) | High risk | Allocation not described, and likely to be insufficient because of alternation used in sequence generation (quasi‐RCT). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding of participants or personnel described. |
| Blinding of outcome assessment ‐ cardiac abnormalities (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Blinding of outcome assessment ‐ non‐cardiac outcomes (detection bias) All outcomes | High risk | No blinding of outcome assessment described, and the outcome measurement could have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear if all data provided |
| Selective reporting (reporting bias) | Unclear risk | Unclear what the outcomes were and how these were defined |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
2DE: 2‐dimensional echocardiography AE: adverse events AHA: American Heart Association ALT: alanine transaminase ASA: acetylsalicylic acid BCG: Bacillus Calmette–Guérin CAA: coronary artery aneurysm CAD: coronary artery dilation CAL: coronary artery lesions CCT: controlled clinical trial CRP: C‐reactive protein ECG: echocardiogram ESR: erythrocyte sedimentation rate Ig: immunoglobulin IgA: immunoglobulin A IgE: immunoglobulin E IgG: immunoglobulin G IgM: immunoglobulin M IQR: interquartile range ITT: intention‐to‐treat IV: intravenous IVGG: intravenous gamma globulin IVIG: intravenous immunoglobulin IVMP: intravenous methylprednisolone JKDRC: Japanese Kawasaki Disease Research Committee JMHW: Japanese Ministry of Health and Welfare KD: Kawasaki disease MPT: methylprednisolone pulse therapy PLT: platelet RBC: red blood cell RCT: randomised controlled trial SD: standard deviation TB: tuberculosis TNF: tumour necrosis factor UCG: ultrasonographic cardiogram VGIH: polyethylene glycol‐treated human immunoglobulin WBC: white blood cell
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ChiCTR2000035163 | Ongoing study to investigate KD treatment in participants either IVIG‐resistant or predicted to be IVIG‐resistant. IVIG not the differentiating intervention |
| Hamada 2019 | Study compared IVIG plus ciclosporin versus IVIG alone in people predicted to be at higher risk for IVIG resistance. IVIG not the differentiating intervention |
| ISRCTN71987471 | Participants randomised to corticosteroid or nothing after initial IVIG plus ASA treatment. |
| JPRN‐UMIN000014665 | Study compared fast versus slow injection of IVIG. |
| Lee 1996 | Study only reported surrogate outcomes (lymphocyte phenotype), so does not meet our inclusion criteria. |
| Lin 2021 | Study plans to evaluate the efficacy of IVIG plus ASA plus prednisolone compared to IVIG plus ASA in Chinese paediatric participants with KD. |
| Muta 2002 | Study compared different types of IVIG, and dosage was determined by KD severity. |
| Nanishi 2017 | Study compared IVIG with IVIG plus clarithromycin. |
| NCT02298062 | Clinical trial report states completed September 2015, but no published report identified. We contacted the study investigators to request data (Fang Liu, Professor, Fudan University, liufang@fudan.edu.cn; January 2022). They replied to say that study was not completed due to limited participants and COVID‐19. |
| Portman 2019 | Study randomised participants to either etanercept or placebo after initial dose of IVIG. |
| RAISE 2012 | Study compared IVIG plus ASA versus IVIG plus prednisolone. |
| Sanati 2021 | Study compared IVIG versus IVIG plus ASA. |
| Seki 2021 | Study compared different speeds of IVIG infusion. |
ASA: acetylsalicylic acid (aspirin) IVIG: intravenous immunoglobulin KD: Kawasaki disease
Characteristics of studies awaiting classification [ordered by study ID]
Chang 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Chang 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Chen 2006.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Fu 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Ho 2003.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Ho 2004.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Juan 2003.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Juan 2005.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Juan 2006.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Kuo 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Li 2008.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Li 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Liao 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Liu 2000.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Liu 2004.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Liu 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text required. Unable to verify if meets our inclusion criteria |
Lu 2003.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Peng 2001.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Teng 2005.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Yao 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text required. Unable to verify if meets our inclusion criteria |
Yen 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Yuan 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Yueh 2006.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Translation required. Unable to verify if meets our inclusion criteria |
Characteristics of ongoing studies [ordered by study ID]
ChiCTR1900027954.
| Study name | Efficacy of infliximab on IVIG‐unresponsive KD |
| Methods | Single‐centre prospective randomised controlled study |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: infliximab Comparison: second dose of IVIG |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | 1 January 2020 |
| Contact information | Yanfei Wang Guangzhou Women and Children's Medical Center, Guangzhou, Guangdong, China Email: wangyanfei@gwcmc.org |
| Notes | Funding: self‐financing |
EUCTR2020‐003194‐22‐FR.
| Study name | A randomized phase III multicentre trial comparing the efficacy and safety of Anakinra versus intravenous immunoglobulin (IVIG) retreatment, in patients with Kawasaki disease who failed to respond to initial standard IVIG treatment (ANACOMP) |
| Methods | Randomised, controlled, parallel, open‐label trial to compare the efficacy of anakinra (IL‐1R1 receptor antagonist) with second‐line IVIG infusion on fever in children with KD who failed to respond to 1 infusion of IVIG (standard treatment) |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: IL‐1R receptor antagonist (Kineret/anakinra 100 mg/0.67 mL) Comparison: human normal immunoglobulin (Privigen 100 mg/mL) |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | December 2021 |
| Contact information | Malika Yahmi
Hopital Saint‐Louis, Paris, France
Email: malika.yahmi@aphp.fr Isabelle Koné‐Paut CHU de Bicêtre, Le Kremlin‐Bicêtre, France Email: isabelle.kone‐paut@aphp.fr |
| Notes | Funding: Ministère de la Santé ANACOMP Study NCT04656184 |
AHA: American Heart Association IL: interleukin IL‐1R: interleukin‐1 receptor IVIG: intravenous immunoglobulin KD: Kawasaki disease NSAIDs: non‐steroidal anti‐inflammatory drugs SmPC: summary of product characteristics TB: tuberculosis TNF‐a: tumour necrosis factor‐alpha
Differences between protocol and review
2022 version
We amended the Types of studies section to clarify that we excluded studies that did not investigate or report any of our outcomes of interest.
We amended the Types of interventions section to clarify that we would not include studies that compared the speed of intravenous immunoglobulin (IVIG) infusion or a particular type of IVIG versus another (i.e. manufacturer or heparinated/sulphonated). We originally planned to undertake subgroup analysis to investigate the efficacy of IVIG produced by different manufacturers. Following discussion, we determined that this was not clinically relevant and it has been removed.
We had planned to use a fixed‐effect model when there were no concerns about heterogeneity. As there were many differences between studies (doses, infusion regimen, concomitant medications, etc.), we used a random‐effects model for all analyses, not only in the case of substantial heterogeneity (I2 > 50%).
We had planned to undertake subgroup analyses by initial or refractory (secondary) IVIG treatment and by single‐ or multiple‐dose regimens. Given the range of regimens involved in the included studies, it was clinically more appropriate to present initial versus secondary IVIG treatment, and single versus multiple doses as separate comparisons and subgrouped by the total dose administered. For the same reason, we presented analyses for all outcomes in this way, not just our primary outcomes as planned at protocol stage. We did not investigate adverse effects by subgroup for geographical distribution as, given the results of the main analysis, this would not have provided any useful information. We carried out additional sensitivity analyses with studies at high risk of detection bias for cardiac outcomes, as coronary artery abnormalities was our most clinically relevant outcome, and for studies where it was not clear what Kawasaki disease diagnostic criteria were used, as this may have impacted the results. We undertook further sensitivity analysis when we identified substantial heterogeneity by removing studies from the analyses to assess the individual impact of studies on the results.
Contributions of authors
CB: study selection and risk of bias assessment, data extraction and analysis, GRADE assessment, writing of review SK: study selection and risk of bias assessment, data extraction and analysis, writing of review MS: study selection and risk of bias assessment, data extraction and GRADE assessment, checking review SI: data analysis and interpretation, checking review TK: data interpretation, writing of review
Sources of support
Internal sources
No sources of support provided
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
CB is supported by a grant from the Chief Scientist Office (CSO CRG/01).
Declarations of interest
CB: none known. As CB is based within Cochrane Vascular, editorial tasks for this review update were carried out by other members of the Cochrane Vascular editorial team. SK: none known MS: none known SI: none known TK: declares that his institution received a scholarship grant from Japan Blood Products Organization (total amount JPY 300,000 in 2021). This does not conflict with his work on this review. TK also reports payments for lectures from Japan Blood Products Organization, Mitsubishi Tanabe Pharma Corporation, Nihon Pharmaceutical, and Teijin Pharma.
New
References
References to studies included in this review
Barron 1990 {published data only}
- Barron KS, Murphy DJ Jr, Silverman ED, Ruttenberg HD, Wright GB, Franklin W, et al. Treatment of Kawaski syndrome: a comparison of two dosage regimens of intravenously administered immune globulin. Journal of Pediatrics 1990;117(4):638-44. [DOI] [PubMed] [Google Scholar]
Burns 2008 {published data only}
- Burns JC, Connor JD, Capparelli EV, Best BM, Mejias A, Mahony L, et al. Infliximab treatment of intravenous immunoglobulin-resistant Kawasaki disease. Journal of Pediatrics 2008;153(6):833-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00271570. Infliximab (Remicade) for patients with acute Kawasaki disease. clinicaltrials.gov/show/NCT00271570 (first received 2 January 2006).
Burns 2021 {published data only}
- Burns JC, Roberts SC, Tremoulet AH, He F, Printz BF, Ashouri N, et al. Infliximab versus second intravenous immunoglobulin for treatment of resistant Kawasaki disease in the USA (KIDCARE): a randomised, multicentre comparative effectiveness trial. Lancet Child and Adolescent Health 2021;5(12):852-61. [DOI] [PubMed] [Google Scholar]
- NCT03065244. KIDCARE (Kawasaki Disease Comparative Effectiveness Trial). clinicaltrials.gov/show/NCT03065244 (first received 27 February 2017).
- Roberts SC, Jain S, Tremoulet AH, Kim KK, Burns JC, KIDCARE Multicenter Study Group. The Kawasaki Disease Comparative Effectiveness (KIDCARE) trial: a phase III, randomized trial of second intravenous immunoglobulin versus infliximab for resistant Kawasaki disease. Contemporary Clinical Trials 2019;79:98-103. [DOI] [PubMed] [Google Scholar]
Furusho 1984 {published data only}
- Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. Intravenous gamma-globulin for Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):799-804. [DOI: 10.1111/j.1442-200x.1991.tb02611.x] [DOI] [PubMed] [Google Scholar]
- Furusho K, Kamiya T, Nakano H. High-dose intravenous gammaglobulin for Kawasaki disease. Lancet 1984;2(8411):1055-8. [DOI] [PubMed] [Google Scholar]
Furusho 1991A {published data only}
- Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. Intravenous gamma-globulin for Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):799-804. [DOI: 10.1111/j.1442-200x.1991.tb02611.x] [DOI] [PubMed] [Google Scholar]
Furusho 1991B {published data only}
- Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. Intravenous gamma-globulin for Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):799-804. [DOI] [PubMed] [Google Scholar]
Harada 1989 {published data only}
- Harada H, Yamaguchi H. Intravenous gamma globulin treatment in Kawasaki disease - comparison between high dose and low dose. Progress in Medicine 1989;9:45-8. [Google Scholar]
- Harada K. Intravenous gamma-globulin treatment in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):805-10. [DOI] [PubMed] [Google Scholar]
Hashino 2001 {published data only}
- Hashino K, Ishii M, Iemura M, Akagi T, Kato H. Re-treatment for immune globulin-resistant Kawasaki disease: a comparative study of additional immune globulin and steroid pulse therapy. Pediatrics International 2001;43(3):211-7. [DOI] [PubMed] [Google Scholar]
He 2021 {published data only}
- He L, Liu F, Huang G. Multi centeral study on IVIG treatment to Kawasaki disease. Cardiology in the Young 2017;27(4):S472. [Google Scholar]
- He L, Liu F, Yan W, Huang M, Huang M, Xie L, et al. Randomized trial of different initial IVIG regimens in Kawasaki disease. Pediatrics International 2021;63(7):757-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He L, Niu CW, Liu F, Huang GY, Wu L, Chu C, et al. A prospective randomised study of intravenous immunoglobulin treatment regimens in acute Kawasaki disease. Journal of the Hong Kong College of Cardiology 2016;24(1):49. [Google Scholar]
- NCT02439996. Different doses of IVIG for Kawasaki disease. clinicaltrials.gov/show/NCT02439996 (first received 12 May 2015).
Matsushima 1985 {published data only}
- Matsushima M, Nagashima M, Matsuoka H. High dose immunoglobulin therapy for Kawasaki disease by a control study. Nihon Shounika Gakkai Zasshi [Journal of the Japanese Pediatric Society] 1986;90:80-7. [Google Scholar]
Miura 2008 {published data only}
- Miura M, Kohno K, Ohki H, Yoshiba S, Sugaya A, Satoh M. Effects of methylprednisolone pulse on cytokine levels in Kawasaki disease patients unresponsive to intravenous immunoglobulin. European Journal of Pediatrics 2008;167(10):1119-23. [DOI] [PubMed] [Google Scholar]
- Miura M, Ohki H, Yoshiba S, Ueda H, Sugaya A, Satoh M, et al. Adverse effects of methylprednisolone pulse therapy in refractory Kawasaki disease. Archives of Disease in Childhood 2005;90(10):1096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mori 2017 {published data only}
- Mori M, Hara T, Kikuchi M, Shimizu H, Miyamoto T, Iwashima S, et al. Infliximab versus intravenous immunoglobulin for refractory Kawasaki disease: a phase 3, randomized, open-label, active-controlled, parallel-group, multicenter trial. Scientific Reports 2018;8(1):1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori M. Clinical trial of the infliximab for Kawasaki disease that an effect is inadequate for by existing treatment in Japan. Rheumatology (United Kingdom) 2017;56(Suppl 3):P1-67.
- NCT01596335. Clinical study of TA-650 in patients with refractory Kawasaki disease. clinicaltrials.gov/ct2/show/NCT01596335 (first received 26 September 2018).
Morikawa 1994 {published data only}
- Morikawa Y, Ohashi Y, Harada K, Asai T, Okawa S, Nagashima M, et al. A multicenter, randomized, controlled trial of intravenous gamma globulin therapy in children with acute Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1994;36(4):347-54. [DOI] [PubMed] [Google Scholar]
- Morikawa Y, Ohashi Y, Harada K, Asai T, Okawa S, Nagashima M, et al. Coronary risks after high-dose gamma-globulin in children with Kawasaki disease. Pediatrics International 2000;42(5):464-9. [DOI] [PubMed] [Google Scholar]
Nagashima 1987 {published data only}
- Nagashima M, Matsushima M, Matsuoka H. High-dose gammaglobulin therapy for Kawasaki disease. Journal of Pediatrics 1987;110(5):710-2. [DOI] [PubMed] [Google Scholar]
Newburger 1986 {published data only}
- Newburger JW, Takahashi M, Burns JC. The treatment of Kawasaki syndrome with intravenous gamma globulin. New England Journal of Medicine 1986;315(6):341-7. [DOI] [PubMed] [Google Scholar]
- Takahashi M, Newburger JW. Long-term follow-up of coronary abnormalities in Kawasaki syndrome treated with and without IV gamma globulin. Circulation 1990;82:717. [Google Scholar]
Newburger 1991 {published data only}
- NCT00000520. Prevention of coronary aneurysms in Kawasaki syndrome. clinicaltrials.gov/show/NCT00000520 (first received 28 October 1999).
- Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. New England Journal of Medicine 1991;324(23):1633-9. [DOI] [PubMed] [Google Scholar]
Nishihara 1988 {published data only}
- Nishihara S, Ishibashi K, Matsuda I. Intravenous gammaglobulin and reduction of coronary artery abnormalities in children with Kawasaki disease. Lancet 1988;2(8617):973. [DOI] [PubMed] [Google Scholar]
Nonaka 1995 {published data only}
- Nonaka Z, Maekawa K, Okabe T, Eto Y, Kubo M. Randomized controlled study of intravenous prednisolone and gammaglobulin treatment in 100 cases with Kawasaki disease. Kawasaki Disease 1995:328-31.
Ogawa 1987 {published data only}
- Ogawa M, Ogino H, Harima Y, Kono S, Ohkuni H, Nishida M. High dose gamma-globulin therapy for Kawasaki disease. Journal of the Japanese Pediatric Society 1987;91(12):3763-71. [Google Scholar]
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nishida M, et al. Clinical evaluation of gammaglobulin preparations for the treatment of Kawasaki disease. Progress in Clinical and Biological Research 1987;250:555-6. [PubMed] [Google Scholar]
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nishida M, et al. High-dose intravenous gammaglobulin treatment of Kawasaki disease. Progress in Medicine 1990;10:29-38. [Google Scholar]
Ogino 1987 {published data only}
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nishida M, et al. Clinical evaluation of gammaglobulin preparations for the treatment of Kawasaki disease. Progress in Clinical and Biological Research 1987;250:555-6. [PubMed] [Google Scholar]
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nishida M, et al. High-dose intravenous gammaglobulin treatment of Kawasaki disease. Progress in Medicine 1990;10:29-38. [Google Scholar]
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nisida M. Clinical evaluation of gamma globulin preparations for the treatment of Kawasaki disease - trial of 200 mg/kg/day. Journal of the Japanese Pediatric Society 1987;91(8):2849-56. [Google Scholar]
Okuni 1987A {published data only}
- Harada K. Intravenous gamma-globulin treatment in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):805-10. [DOI] [PubMed] [Google Scholar]
- Okuni M, Harada K, Yamaguchi H, Yanagawa H, Sonobe T, Kawasaki T. Intravenous gamma globulin therapy in Kawasaki disease - trial of low dose gammaglobulin. Kawasaki Disease 1987:433-9. [PubMed]
Okuni 1987B {published data only}
- Harada K. Intravenous gamma-globulin treatment in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):805-10. [DOI] [PubMed] [Google Scholar]
- Okuni M, Harada K, Yamaguchi H, Yanagawa H, Sonobe T, Kawasaki T. Intravenous gamma globulin therapy in Kawasaki disease - trial of low dose gammaglobulin. Kawasaki Disease 1987:433-9. [PubMed]
Onouchi 1988 {published data only}
- Onouchi Z, Isogai Y, Yanagisawa M, Yamanouchi T, Matsuda H, Morita T, et al. Multicenter randomized controlled study of intravenous immunoglobulin in Kawasaki disease. Journal of the Japanese Pediatric Society 1988;92(11):2367-76. [Google Scholar]
- Onouchi Z, Yanagisawa M, Hirayama T, Kiyosawa N, Matsuda H, Nakashima M. Optimal dosage and differences in therapeutic efficacy of IGIV in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1995;37(1):40-6. [DOI] [PubMed] [Google Scholar]
Onouchi 1992 {published data only}
- Onouchi Z, Yanagisawa M, Hirayama T, Kiyosawa N, Matsuda H, Nakashima M. Optimal dosage and differences in therapeutic efficacy of IGIV in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1995;37(1):40-6. [DOI] [PubMed] [Google Scholar]
- Onouchi Z, Yanagisawa M, Shiraishi H, Hirayama T, Katsube Y, Kiyosawa N, et al. Multi-centre randomized controlled study of intravenous immunoglobulin G (C-425) for Kawasaki disease. Journal of the Japanese Pediatric Society 1992;96(12):2669-79. [Google Scholar]
Qin 2006 {published data only}
- Qin LJ, Wang HW, Hu XF, Liu QJ, Shi H, Wei YX, et al. Therapeutic effectiveness of intravenous immunoglobulin at 1 g/kg and 2 g/kg on Kawasaki disease: a comparative and follow-up study. Zhonghua er ke za zhi 2006;44(12):891-5. [PubMed] [Google Scholar]
Sakata 2007 {published data only}
- Ozawa S, Sakata K, Hamaoka K. Randomized-prospective study of a single infusion of 1g/kg gammaglobulin for reducing a total dose of gammaglobulin in Kawasaki disease treatment. Pediatric Research 2003;53:181. [Google Scholar]
- Sakata K, Hamaoka K, Ozawa SI, Niboshi A, Yoshihara T, Nishiki T, et al. A randomized prospective study on the use of 2 g-IVIG or 1 g-IVIG as therapy for Kawasaki disease. European Journal of Pediatrics 2007;166(6):565-71. [DOI] [PubMed] [Google Scholar]
Sato 1995 {published data only}
- Sato N, Sugimura T, Akagi T, Inoue O, Ono E, Kato H. Selective gammaglobulin treatment in Kawasaki disease: single 2 g/kg or 400 mg/kg/day for 5 days? Kawasaki Disease 1995:332-8.
- Sato N, Sugimura T, Akagi T, Yamakawa R, Hashino K, Eto G, et al. Selective high dose gamma-globulin treatment in Kawasaki disease: assessment of clinical aspects and cost effectiveness. Pediatrics International 1999;41(1):1-7. [DOI] [PubMed] [Google Scholar]
Wang 2020 {published data only}
- ChiCTR-EOC-17013266. The mechanism of coronary artery lesions and effect of treatment in children with Kawasaki disease: a clinical cohort study. chictr.org.cn/showproj.aspx?proj=22637 (first received 11 June 2017).
- Wang Z, Wang Y, Li W, Xie X, Liu P, Zhang X, et al. Methylprednisolone pulse therapy or additional IVIG for patients with IVIG-resistant Kawasaki disease. Journal of Immunology Research 2020;2020:4175821. [DOI: 10.1155/2020/4175821] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yabiku 1989 {published data only}
- Ogino H, Ogawa M, Harima Y, Kono S, Ohkuni H, Nishida M, et al. High-dose intravenous gammaglobulin treatment of Kawasaki disease. Progress in Medicine 1990;10:29-38. [Google Scholar]
- Yabiku M, Kojima S, Ogawa M, Ogino H, Harima Y, Kono S, et al. High dose gammaglobulin therapy for Kawasaki disease. Journal of the Japanese Pediatric Society 1989;93(12):2721-31. [Google Scholar]
Youn 2016 {published data only}
- Youn Y, Kim J, Hong YM, Sohn S. Infliximab as the first retreatment in patients with Kawasaki disease resistant to initial intravenous immunoglobulin. Pediatric Infectious Disease Journal 2016;35(4):457-9. [DOI] [PubMed] [Google Scholar]
Yuan 2000 {published data only}
- Yuan Y. Analysis of recent effects for corticosteroid in treating Kawasaki disease. Chinese Journal of Practical Paediatrics 2000;15:49. [Google Scholar]
References to studies excluded from this review
ChiCTR2000035163 {published data only}
- ChiCTR2000035163. A multicenter clinical trial of a new individualized treatment opinion for Kawasaki disease. chictr.org.cn/showprojen.aspx?proj=57061 (first received 2 August 2020).
Hamada 2019 {published data only}
- Hamada H, Suzuki H, Onouchi Y, Ebata R, Terai M, Fuse S, et al. Efficacy of primary treatment with immunoglobulin plus ciclosporin for prevention of coronary artery abnormalities in patients with Kawasaki disease predicted to be at increased risk of non-response to intravenous immunoglobulin (KAICA): a randomised controlled, open-label, blinded-endpoints, phase 3 trial. Lancet 2019;393(10176):1128-37. [DOI] [PubMed] [Google Scholar]
- Hamada H, Suzuki H, Onouchi Y, Ebata R, Terai M, Fuse S, et al. Efficacy of primary treatment with immunoglobulin plus cyclosporine for prevention of coronary artery abnormalities in Kawasaki disease patients predicted to be at increased risk of IVIG non-response (KAICA study): a controlled, phase 3, randomised, open-label, blinded-endpoints trial. Rheumatology 2019;58(Suppl 2):kez063-031. [DOI: 10.1093/rheumatology/kez063.031] [DOI] [PubMed] [Google Scholar]
ISRCTN71987471 {published data only}
- ISRCTN71987471. Corticosteroids plus standard of care treatment versus standard of care treatment alone to prevent heart complications in Kawasaki disease. isrctn.com/ISRCTN71987471 (first received 31 March 2020).
JPRN‐UMIN000014665 {published data only}
- JPRN-UMIN000014665. The investigation of the therapeutic efficacy of rapid intravenous immunoglobulin injection for acute phase Kawasaki disease. trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000014665 (first received 30 October 2014).
Lee 1996 {published data only}
- Lee HK, Kim DS, Noh GW, Lee KY. Effects of intravenous immune globulin on the peripheral lymphocyte phenotypes in Kawasaki disease. Yonsei Medical Journal 1996;37(5):357-63. [DOI] [PubMed] [Google Scholar]
Lin 2021 {published data only}
- Lin SY, He L, Xie LP, Wang Y, Lin YX, Cao YY, et al. Effects of immunoglobulin plus prednisolone in reducing coronary artery lesions in patients with Kawasaki disease: study protocol for a phase III multicenter, open-label, blinded-endpoints randomized controlled trial. Trials 2021;22(2):898. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muta 2002 {published data only}
- Muta H, Ishii M, Hirose A, Furui J, Sugahara Y, Himeno W, et al. Randomized prospective controlled study of intravenous gamma-globulin products in treatment of Kawasaki disease. Journal of the Japan Pediatric Society 2002;106(6):742-6. [Google Scholar]
- Muta H, Ishii M, Sugahara Y, Akagi T, Kato H. Randomized controlled study of intravenous gamma-globulin products in treatment of Kawasaki disease. Pediatric Research 2003;53(1):181. [Google Scholar]
Nanishi 2017 {published data only}
- Nanishi E, Nishio H, Takada H, Yamamura K, Fukazawa M, Furuno K, et al. Clarithromycin plus intravenous immunoglobulin therapy can reduce the relapse rate of Kawasaki disease: a phase 2, open-label, randomized control study. Journal of the American Heart Association 2017;6(7):e005370. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02298062 {published data only}
- NCT02298062. Infliximab for Kawasaki disease patients resistant to IVIG: a multicentre, prospective, randomised trial. clinicaltrials.gov/ct2/show/NCT02298062 (first received 21 November 2014).
Portman 2019 {published data only}
- Portman MA, Dahdah N, Olson AK, Slee A, Choueiter N, Altman C. Multicenter, randomized, double-blind trial of etanercept in acute Kawasaki disease. Circulation 2017;136:A15447. [Google Scholar]
- Portman MA, Dahdah NS, Slee A, Olson AK, Choueiter NF, Soriano BD, et al. Etanercept with IVIg for acute Kawasaki disease: a randomized controlled trial. Pediatrics 2019;143:6. [DOI: 10.1542/peds.2018-3675] [DOI] [PMC free article] [PubMed] [Google Scholar]
RAISE 2012 {published data only}
- Kobayashi T, Saji T, Otani T, Takeuchi K, Nakamura T, Arakawa H, et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 2012;379(9826):1613-20. [DOI: 10.1016/S0140-6736(11)61930-2] [DOI] [PubMed] [Google Scholar]
Sanati 2021 {published data only}
- Sanati F, Bagheri M, Eslami S, Khalooei A. Evaluation of high-dose aspirin elimination in the treatment of Kawasaki disease in the incidence of coronary artery aneurysm. Annals of Pediatric Cardiology 2021;14(2):146-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seki 2021 {published data only}
- Seki M, Minami T, Oka K, Yokomizo A, Matsubara D, Sato T, et al. Efficacy and safety associated with the infusion speed of intravenous immunoglobulin for the treatment of Kawasaki disease: a randomized controlled trial. Pediatric Rheumatology 2021;19(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Chang 2007 {published data only}
- Chang YC. Two different large dosage of gamma-immunoglobulin for the treatment of Kawasaki disease. Sichuan Medical Journal 2007;28(7):801. [Google Scholar]
Chang 2008 {published data only}
- Chang WH. The different dosage of gamma-immunoglobulin in treating of Kawasaki disease - a clinical study. Journal of Jilin Medical College 2008;29(4):199-201. [Google Scholar]
Chen 2006 {published data only}
- Chen PC, Shi WZ. Medium dose of gamma-immunoglobulin for the treatment of Kawasaki disease - a clinical observation. Zhejiang Clinical Medicine 2006;8(3):308. [Google Scholar]
Fu 2010 {published data only}
- Fu CN, Chen HP. Comparison of the therapeutic effects of different dose intravenous gamma-immunoglobulin in Kawasaki disease. China Modern Drug Application 2010;4(7):121-2. [Google Scholar]
Ho 2003 {published data only}
- Ho HH, Chang Q, Lee JY. Different dosage of intravenous immunoglobulin for the treatment of Kawasaki disease - the observation of therapeutic effect. FJ Medical Journal 2003;25(2):49-50. [Google Scholar]
Ho 2004 {published data only}
- Ho C. Comparison of therapeutic efficacy of two intravenous gamma-immunoglobulin regimen in acute Kawasaki disease. Hebei Medicine 2004;26(4):323. [Google Scholar]
Juan 2003 {published data only}
- Juan HL, Xiang RL, Liang GA, Lu HP. The effect of different IVIG dosage on CD4+ /CD8+ of children with Kawasaki disease. Pediatric Pharmacological Magazine 2003;9(3):18-9. [Google Scholar]
Juan 2005 {published data only}
- Juan C, Yang HB, Juan J, Ho XL. Comparison of therapeutic efficacy of two large dosage intravenous gamma-immunoglobulin regimens in pediatric Kawasaki disease. Practical Clinical Medicine 2005;8(3):48-9. [Google Scholar]
Juan 2006 {published data only}
- Juan C, Cai XJ. Comparison of therapeutic efficacy of two gamma-immunoglobulin regimens in acute Kawasaki disease. Qingdao Medicine and Health 2006;38(3):175-6. [Google Scholar]
Kuo 2009 {published data only}
- Kuo L, Chang HY, Dou JL, Xu FX, Zhai YL. Different dosage of intravenous gamma-immunoglobulin for the treatment of Kawasaki disease. The observation of therapeutic effect and nursing experience. China Practical Clinical Medicine 2009;3(7):116-7. [Google Scholar]
Li 2008 {published data only}
- Li HL, Liao Y. Analysis of the therapeutic efficacy of a single dose gamma-immunoglobulin for the treatment of Kawasaki disease in thirty three children. Journal of Gannan Medical University 2008;28(1):36-8. [Google Scholar]
Li 2009 {published data only}
- Li CK. Two different intravenous gamma-immunoglobulin regimens in the treatment acute Kawasaki disease - an observation of therapeutic efficacy. Practical Clinical Medicine 2009;10(12):60-2. [Google Scholar]
Liao 2007 {published data only}
- Liao J, He KJ. The clinical study of different dosage immune globulin in treating Kawasaki in intravenous injection. China Healthcare Innovation 2007;2(22):8-9. [Google Scholar]
Liu 2000 {published data only}
- Liu HM. The exploration of intravenous immunoglobulin dosage for the treatment of Kawasaki disease. Shantung Medicine 2000;40(8):23-4. [Google Scholar]
Liu 2004 {published data only}
- Liu TC. The observation of therapeutic effect of intravenous gamma-immunoglobulin in Kawasaki disease. Modern Journal of Integrated Traditional Chinese and Western Medicine 2004;13(4):451. [Google Scholar]
Liu 2009 {published data only}
- Liu M, Cheng J, Luo Q. Comparison of therapeutic efficacy of two intravenous gamma-immunoglobulin regimens in children with Kawasaki disease. China Eugenics and Hereditary Magazine 2009;17(2):117-8. [Google Scholar]
Lu 2003 {published data only}
- Lu JX, Zheng ZL. Therapeutic effects of intravenous immune globulin on Kawasaki disease. Oinghai Medical Magazine 2003;33(5):16-8. [Google Scholar]
Peng 2001 {published data only}
- Peng CM, Xiao Q, Chen YL, Su Y. A study on different dose of intravenous immunoglobulins for treating Kawasaki disease. Journal of Nanhua University (Medical Edition) 2001;29(6):581-3. [Google Scholar]
Teng 2005 {published data only}
- Teng MY. Comparison of therapeutic efficacy of two gamma-immunoglobulin regimens in Kawasaki disease. International Medical Health Reports 2005;11(2):33-4. [Google Scholar]
Yao 2009 {published data only}
- Yao SH. The observation of therapeutic efficacy of different intravenous gamma-immunoglobulin for the treatment in sixty-four children with Kawasaki disease. China Community Physician 2009;11(213):68-9. [Google Scholar]
Yen 2007 {published data only}
- Yen P. The observation of therapeutic efficacy of different intravenous gamma-immunoglobulin for the treatment in Kawasaki disease. Community Medical Magazine 2007;5(23):11. [Google Scholar]
Yuan 2009 {published data only}
- Yuan YF, Kuai WX. The application of gamma-immunoglobulin for pediatric Kawasaki disease. Shanxi Medical Magazine 2009;38(4):365-6. [Google Scholar]
Yueh 2006 {published data only}
- Yueh AH, Tian QL, Li H. The observation of therapeutic efficacy of intravenous gamma-immunoglobulin for the treatment in fifty-six children with Kawasaki disease. Clinical Gathering 2006;21(13):962-3. [Google Scholar]
References to ongoing studies
ChiCTR1900027954 {published data only}
- ChiCTR1900027954. Effecacy of infliximab on IVIG-unresponsive Kawasaki disease: a single center prospective randamized controlled study. trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR1900027954 (first received 7 December 2019).
EUCTR2020‐003194‐22‐FR {published data only}
- EUCTR2020-003194-22-FR. A randomized phase III multicentre trial comparing the efficacy and safety of Anakinra versus intravenous immunoglobulin (IVIG) retreatment, in patients with Kawasaki disease who failed to respond to initial standard IVIG treatment (ANACOMP) [Essai multicentrique randomisé de phase III comparant l'efficacité et la sécurité de l'anakinra au retraitement par immunoglobulines intraveineuses (IVIG), chez des patients atteints de la maladie de Kawasaki qui n'ont pas répondu au traitement initial standard par IVIG]. trialsearch.who.int/Trial2.aspx?TrialID=EUCTR2020-003194-22-FR (first received 7 September 2020).
- NCT04656184. A randomized phase III multicenter trial comparing the efficacy and safety of anakinra versus intravenous immunoglobulin (IVIG) retreatment, in patients with Kawasaki disease who failed to respond to initial standard IVIG treatment. clinicaltrials.gov/show/NCT04656184 (first received 7 December 2020).
Additional references
Ae 2020
- Ae R, Makino N, Kosami K, Kuwabara M, Matsubara Y, Nakamura Y. Epidemiology, treatments and cardiac complications in patients with Kawasaki disease: the nationwide survey in Japan, 2017-2018. Journal of Pediatrics 2020;225:23-9.e2. [DOI: 10.1016/j.jpeds.2020.05.034] [DOI] [PubMed] [Google Scholar]
Ae 2021
- Ae R, Yashiro M, Matsubara Y, Osami M, Makino S, Nakamura Y. Results of the 26th nationwide survey of Kawasaki disease in Japan. jichi.ac.jp/dph/wp-dph/wp-content/uploads/2022/04/a19b047d4b9e6fbb84b6b187236779c8.pdf.
Ashouri 2008
- Ashouri N, Takahashi M, Dorey F, Mason W. Risk factors for non response to therapy in Kawasaki disease. Journal of Pediatrics 2008;153(3):3. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayusawa 2005
- Ayusawa M, Sonobe T, Uemura S, Ogawa S, Nakamura Y, Kiyosawa N, Kawasaki Disease Research Committee. Revision of diagnostic guidelines for Kawasaki disease (the 5th revised edition). Pediatrics International 2005;47(2):232-4. [DOI] [PubMed] [Google Scholar]
Baumer 2006
- Baumer JH, Love S, Gupta A, Haines L, Maconochie IK, Dua JS. Salicylate for the treatment of Kawasaki disease in children. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD004175. [DOI: 10.1002/14651858.CD004175.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 1996
- Burns JC, Shike H, Gordon JB, Malhotra A, Schoenwetter M, Kawasaki T. Sequelae of Kawasaki disease in adolescents and young adults. Journal of the American College of Cardiology 1996;28:253–7. [DOI] [PubMed] [Google Scholar]
Burns 2015
- Burns JC, Franco A. The immunomodulatory effects of intravenous immunoglobulin therapy in Kawasaki disease. Expert Reviews of Clinical Immunology 2015;11:819–25. [DOI: 10.1586/1744666X.2015.1044980] [DOI] [PMC free article] [PubMed] [Google Scholar]
ChiCTR‐EOC‐17013266
- ChiCTR-EOC-17013266. The mechanism of coronary artery lesions and effect of treatment in children with Kawasaki disease: a clinical cohort study. chictr.org.cn/showproj.aspx?proj=22637 (first received 11 June 2017).
Covidence [Computer program]
- Covidence. Version accessed 15 June 2021. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Dallaire 2010
- Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. Journal of the American Society of Echocardiography 2011;24(1):60-74. [DOI: 10.1016/j.echo.2010.10.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Daniels 2012
- Daniels LB, Tjajadi MS, Walford HH, Jimenez-Fernandez S, Trofimenko V, Fick DB Jr, et al. Prevalence of Kawasaki disease in young adults with suspected myocardial ischemia. Circulation 2012;125:2447–53. [DOI: 10.1161/CIRCULATIONAHA.111.082107] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG, editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook/archive/v6.2.
de Graeff 2019
- Graeff N, Groot N, Ozen S, Eleftheriou D, Avcin T, Bader-Meunier B, et al. European consensus-based recommendations for the diagnosis and treatment of Kawasaki disease - the SHARE initiative. Rheumatology (OXFORD) 2019;58(4):672-82. [DOI] [PubMed] [Google Scholar]
Franco 2010
- Franco A, Shimizu C, Tremoulet AH, Burns JC. Memory T-cells and characterization of peripheral T-cell clones in acute Kawasaki disease. Autoimmunity 2010;43(4):317–24. [DOI: 10.3109/08916930903405891] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gedalia 2007
- Gedalia A. Kawasaki disease: 40 years after the original report. Current Rheumatology Reports 2007;9(4):336–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 6 November 2020. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Green 2022
- Green J, Wardle AJ, Tulloh RM. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database of Systematic Reviews 2022, Issue 5. Art. No: CD011188. [DOI: 10.1002/14651858.CD011188.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamada 2019
- Hamada H, Suzuki H, Onouchi Y, Ebata R, Terai M, Fuse S, et al. Efficacy of primary treatment with immunoglobulin plus ciclosporin for prevention of coronary artery abnormalities in patients with Kawasaki disease predicted to be at increased risk of non-response to intravenous immunoglobulin (KAICA): a randomised controlled, open-label, blinded-endpoints, phase 3 trial. Lancet 2019;393(10176):1128–37. [DOI] [PubMed] [Google Scholar]
Harada 1991
- Harada K. Intravenous gamma-globulin treatment in Kawasaki disease. Acta Paediatrica Japonica: Overseas edition 1991;33(6):805-10. [DOI] [PubMed] [Google Scholar]
Hayasaka 2003
- Hayasaka S, Nakamura Y, Yashiro M, Uehara R, Oki I, Tajimi M, et al. Analysis of fatal cases of Kawasaki disease in Japan using vital statistical data over 27 years. Journal of Epidemiology 2003;13:246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook/archive/v6.2.
Hokosaki 2012
- Hokosaki T, Mori M, Nishizawa T, Nakamura T, Imagawa T, Iwamoto M, et al. Long-term efficacy of plasma exchange treatment for refractory Kawasaki disease. Pediatrics International 2012;54(1):99-103. [DOI: 10.1111/j.1442-200X.2011.03487.x] [DOI] [PubMed] [Google Scholar]
Holman 2010
- Holman RC, Christensen KY, Belay ED, Steiner CA, Effler PV, Miyamura J, et al. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Medical Journal 2010;69:194–7. [PMC free article] [PubMed] [Google Scholar]
JMHW 1984
- Research Committee on Kawasaki Disease. Report of Subcommittee on Standardization of Diagnostic Criteria and Reporting of Coronary Artery Lesions in Kawasaki Disease. Tokyo: Japanese Ministry of Health and Welfare; 1984.
Kawasaki 1967
- Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi 1967;16(3):178–222. [PubMed] [Google Scholar]
Kobayashi 2016
- Kobayashi T, Fuse S, Sakamoto N, Mikami M, Ogawa S, Hamaoka K, Z Score Project Investigators. A new Z score curve of the coronary arterial internal diameter using the lambda-mu-sigma method in a pediatric population. Journal of the American Society of Echocardiography 2016;29(8):794-801.e29. [DOI: 10.1016/j.echo.2016.03.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kobayashi 2020
- Kobayashi T, Ayusawa M, Suzuki H, Abe J, Ito S, Kato T, et al. Revision of diagnostic guidelines for Kawasaki disease (6th revised edition). Pediatrics International 2020;62(10):1135-8. [DOI: 10.1111/ped.14326] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kone‐Paut 2018
- Kone-Paut I, Cimaz R, Herberg J, Bates O, Carbasse A, Saulnier JP, et al. The use of interleukin 1 receptor antagonist (anakinra) in Kawasaki disease: a retrospective cases series. Autoimmunity Reviews 2018;17(8):768–74. [DOI: 10.1016/j.autrev.2018.01.024] [DOI] [PubMed] [Google Scholar]
Lee 2008
- Lee TJ, Kim KH, Chun JK, Kim DS. Low-dose methotrexate therapy for intravenous immunoglobulin-resistant Kawasaki disease. Yonsei Medical Journal 2008;49(5):714–8. [DOI: 10.3349/ymj.2008.49.5.714] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2022
- Lefebvre C, Glanville J, Briscoe S, Featherstone R, Littlewood A, Marshall C, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Medicine 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maddox 2015
- Maddox RA, Person MK, Lindsay JL, Baherling DL, Steiner CA, Schonberger LB, et al. Monitoring the occurrence of Kawasaki syndrome in the United States. Circulation 2015;131(Suppl 2):Abstract 0.03. [Google Scholar]
Makino 2015
- Makino N, Nakamura Y, Yashiro M, Ae R, Tsuboi S, Aoyama Y, et al. Descriptive epidemiology of Kawasaki disease in Japan, 2011-2012: from the results of the 22nd nationwide survey. Journal of Epidemiology 2015;25(3):239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Makino 2019
- Makino N, Nakamura Y, Yashiro M, Kosami K, Matsubara Y, Ae R, et al. The nationwide epidemiologic survey of Kawasaki disease in Japan, 2015-2016. Pediatrics International 2019;61(4):397–403. [DOI: 10.1111/ped.13809] [DOI] [PubMed] [Google Scholar]
McCrindle 2017
- McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, and Council on Epidemiology and Prevention, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 2017;135(17):e927-99. [DOI: 10.1161/CIR.0000000000000484] [DOI] [PubMed] [Google Scholar]
Miura 2021
- Miura M, Ayusawa M, Fukazawa R, Hamada H, Ikeda S, Ito S, et al. Guidelines for medical treatment of acute Kawasaki disease (2020 revised version). Journal of Pediatric Cardiology and Cardiac Surgery 2021;5(1):41-73. [DOI: 10.24509/jpccs.0501G1] [DOI] [Google Scholar]
Mori 2004
- Mori M, Miyamae T, Imagawa T, Katakura S, Kimura K, Yokota S. Meta-analysis of the results of intravenous gamma globulin treatment of coronary artery lesions in Kawasaki disease. Modern Rheumatology 2004;14(5):361–6. [DOI: 10.1007/s10165-004-0324-3] [DOI] [PubMed] [Google Scholar]
Newburger 1986
- Newburger JW, Takahashi M, Burns JC, Beiser AS, Chung KJ, Duffy CE, et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. New England Journal of Medicine 1986;315(6):341–7. [DOI] [PubMed] [Google Scholar]
Newburger 1991
- Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. New England Journal of Medicine 1991;324:1633–9. [DOI: 10.1056/NEJM199106063242305] [DOI] [PubMed] [Google Scholar]
Newburger 2004
- Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 2004;114(6):1708–33. [DOI: 10.1542/peds.2004-2182] [DOI] [PubMed] [Google Scholar]
Oates‐Whitehead 2003
- Oates-Whitehead RM, Baumer JH, Haines L, Love S, Maconochie IK, Gupta A, et al. Intravenous immunoglobulin for the treatment of Kawasaki disease in children. Cochrane Database of Systematic Reviews 2003, Issue 4. Art. No: CD004000. [DOI: 10.1002/14651858.CD004000] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olivieri 2008
- Olivieri L, Arling B, Friberg M, Sable C. Coronary artery Z score regression equations and calculators derived from a large heterogeneous population of children undergoing echocardiography. Journal of the American Society of Echocardiography 2009;22(2):159-64. [DOI: 10.1016/j.echo.2008.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Onouchi 2008
- Onouchi Y, Gunji T, Burns JC, Shimizu C, Newburger JW, Yashiro M, et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nature Genetics 2008;40(1):35–42. [DOI: 10.1038/ng.2007.59] [DOI] [PMC free article] [PubMed] [Google Scholar]
Onouchi 2010
- Onouchi Y, Ozaki K, Buns JC, Shimizu C, Hamada H, Honda T, et al. Common variants in CASP3 confer susceptibility to Kawasaki disease. Human Molecular Genetics 2010;19(14):2898–906. [DOI: 10.1093/hmg/ddq176] [DOI] [PMC free article] [PubMed] [Google Scholar]
Onouchi 2012
- Onouchi Y, Ozaki K, Burns JC, Shimizu C, Terai T, Hamada H, et al. A genome-wide association study identifies three new risk loci for Kawasaki disease. Nature Genetics 2012;44(5):517–21. [DOI: 10.1038/ng.2220] [DOI] [PubMed] [Google Scholar]
RevMan Web 2022 [Computer program]
- Review Manager Web (RevMan Web). Version 4.12.0. The Cochrane Collaboration, 2022. Available at revman.cochrane.org.
Rife 2020
- Rife E, Gedalia A. Kawasaki disease: an update. Current Rheumatology Reports 2020;22:75. [DOI: 10.1007/s11926-020-00941-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rowley 1997
- Rowley AH, Eckerley CA, Jäck HM, Shulman ST, Baker SC. IgA plasma cells in vascular tissue of patients with Kawasaki syndrome. Journal of Immunology 1997;159(12):5946–55. [PubMed] [Google Scholar]
Sauvaget 2012
- Sauvaget E, Bonello B, David M, Chabrol B, Dubus JC, Bosdure E. Resistant Kawasaki disease treated with anti-CD20. Journal of Pediatrics 2012;160(5):875-6. [DOI: 10.1016/j.jpeds.2012.01.018] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schünemann 2021
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook/archive/v6.2.
Tremoulet 2019
- Tremoulet AH, Jain S, Jone PN, Best BM, Duxbury EH, Franco A, et al. Phase I/IIa trial of atorvastatin in patients with acute Kawasaki disease with coronary artery aneurysm. Journal of Pediatrics 2019;215:107–17.e12. [DOI: 10.1016/j.jpeds.2019.07.064] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uehara 2003
- Uehara R, Yashiro M, Nakamura Y, Yanagawa H. Kawasaki disease in parents and children. Acta Paediatrica 2003;92:694–7. [DOI: 10.1111/j.1651-2227.2003.tb00602.x] [DOI] [PubMed] [Google Scholar]
Verdoni 2020
- Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 2020;395:1771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamaji 2019
- Yamaji N, da Silva Lopes K, Shoda T, Ishitsuka K, Kobayashi T, Ota E, et al. TNF-α blockers for the treatment of Kawasaki disease in children. Cochrane Database of Systematic Reviews 2019, Issue 8. Art. No: CD012448. [DOI: 10.1002/14651858.CD012448.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yashiro 2004
- Yashiro M, Nakamura Y, Yanagawa H. Clinical features of patients with Kawasaki disease whose parents had the same disease. Archives of Pediatrics and Adolescent Medicine 2004;158:1166–9. [DOI] [PubMed] [Google Scholar]
Zhang 2020
- Zhang RL, Lo HH, Lei C, Ip N, Chen J, Law BYK. Current pharmacological intervention and development of targeting IVIG resistance in Kawasaki disease. Current Opinion in Pharmacology 2020;54:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Broderick 2021
- Broderick C, Kobayashi S, Suto M, Ito S, Kobayashi T. Intravenous immunoglobulin for the treatment of Kawasaki disease. Cochrane Database of Systematic Reviews 2021, Issue 6. Art. No: CD014884. [DOI: 10.1002/14651858.CD014884] [DOI] [PMC free article] [PubMed] [Google Scholar]


