LEARNING OBJECTIVES
After participating in this activity, the learner will be better able to:
Discuss the histologic presentation of Wilson disease on liver biopsy.
Identify indications for copper dry weight, if Wilson disease is suspected.
CASE
A 79-year-old female with no prior history of liver disease presented with multiple weeks of generalized weakness and diarrhea. Several months prior, she had upper respiratory symptoms which she treated with loratadine and fluticasone nasal spray. She denied antibiotic use. She denied the use of alcohol, tobacco, illicit drugs, herbal supplements, or recent travel.
On presentation, her labs were notable for serum sodium 110 mEq/L, creatinine 2.3 mg/dL (baseline 1.5), aspartate transaminase 975 IU/L, alanine transaminase 326 IU/L, alkaline phosphatase 1268 IU/L, bilirubin 8.6 mg/dL, international normalized ratio (INR) 1.6. Her white blood cell count was 7800/µL (89% neutrophils, 5.3% lymphocytes), hemoglobin 11.4 g/dL, and platelets 130,000/µL. Notably, liver function tests were normal 3 months prior. CT abdomen and pelvis without contrast showed small bilateral pleural effusions, small volume ascites, anasarca, and borderline retroperitoneal lymph node enlargement along the left para-aortic and iliac chains. There was no evidence of hepatosplenomegaly or biliary ductal dilatation.
She was transferred to a tertiary referral center on hospital day 2. On physical examination, she was jaundiced but did not have stigmata of chronic liver disease. Her abdomen was nontender to palpation. She was alert, fully oriented, and had no evidence of asterixis. Infection, drug-induced liver injury secondary to over-the-counter cold medication use, and autoimmune hepatitis (AIH) were considered as causes of her acute liver injury. Infectious workup was negative for acute viral hepatitis (A, B, C, and E), herpes simplex, varicella zoster, and Epstein-Barr virus infection. Cytomegalovirus DNA was detected but unmeasurable. She had a ferritin level of 9819 mcg/L and a transferrin saturation of 30%. Antinuclear antibody, anti–smooth muscle antibody, and IgG levels were normal. Ultrasound of her liver with Doppler was negative for structural and parenchymal abnormalities. An echocardiogram demonstrated a normal ejection fraction and moderate pericardial effusion.
Question 1
What would be the next step in management?
Empiric prednisone
Serum ceruloplasmin and 24-hour urine copper
Empiric acyclovir
Liver biopsy
Due to the uncertainty of her diagnosis, she underwent ultrasound-guided liver biopsy on hospital day 4 (Figures 1 and 2). Biopsy showed areas of hepatocyte necrosis admixed with atypical cells with varying amounts of cytoplasm. To characterize these cells combined immunohistochemistry was completed. There was a complete absence of B cells and strong diffuse membranous expression of the pan T-cell antigens CD3 and CD45RO; however, there was loss of other pan T-cell antigens (CD5 and CD7). The cells displayed a CD4 and CD8 “double-negative” phenotype. In addition, CD30 and TdT (terminal deoxynucleotidyl transferase) were negative, making atypical large-cell lymphoma and lymphoblastic leukemia/lymphoma unlikely. With no clear immunophenotypic pattern to support an alternative diagnosis, this case was classified as peripheral T-cell lymphoma not otherwise specified (PTCL-NOS).
FIGURE 1.
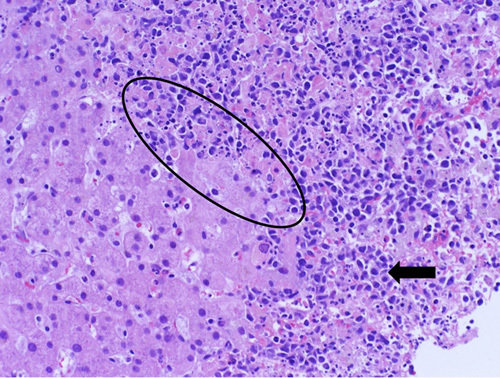
Liver biopsy with hematoxylin and eosin. This shows preserved hepatic parenchyma transitioning into an area of “dirty” necrosis with admixed infiltrating atypical cells (circle). These large plasmacytoid cells demonstrate a variable amount of cytoplasm, and significant nuclear pleomorphism (arrow).
FIGURE 2.
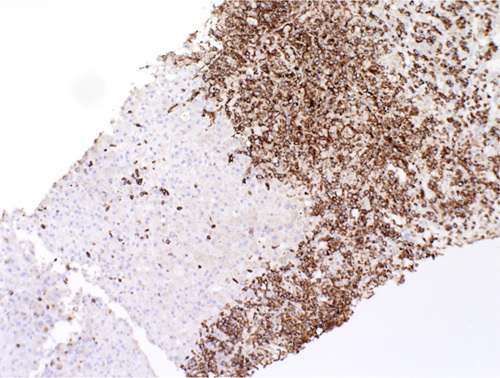
CD3 immunohistochemical staining of the atypical cells within the biopsy. These cells show strong diffuse membranous expression of CD3 consistent with T-cell origin. There is loss of other pan T-cell antigens (CD5 and CD7) and “display a double-negative” phenotype (CD4 and CD8 negative). The lack of clear immunophenotypic pattern classifies this as peripheral T-cell lymphoma not otherwise specified.
Shortly after diagnosis, she had acute worsening of her clinical status leading to renal failure, lactic acidosis, worsening mental status with encephalopathy, coagulopathy (INR 3), and disseminated intravascular coagulation with diffuse mucosal bleeding. After goals of care discussions with family, she was transitioned to comfort care on hospital day 12.
DISCUSSION
Despite having heterogenous etiologies, ALF presents with similar findings of acute liver injury, coagulopathy (INR >1.5), and hepatic encephalopathy within 26 weeks of symptoms onset in patients with no prior liver disease.1–3 As further injury develops, patients develop a systemic inflammatory response due to cytokine release from hepatocytes and surrounding cells leading to cardiovascular collapse, cerebral edema, metabolic derangements, and renal failure.1,4 As such, ALF carries a high mortality rate with a transplant-free recovery rate of ∼45%.5 In the US, over 50% of ALF presentations are due to medications, followed by viral hepatitis, ischemia, AIH, and rarely Wilson disease (Figure 3). No cause is identified in 17% of patients.5,6 Among causes, acetaminophen, shock, and hepatitis A infection have the most favorable outcomes (58-64% spontaneous recovery) compared with drug-induced, AIH, and indeterminate ALF (∼20%–25% spontaneous recovery).5
FIGURE 3.
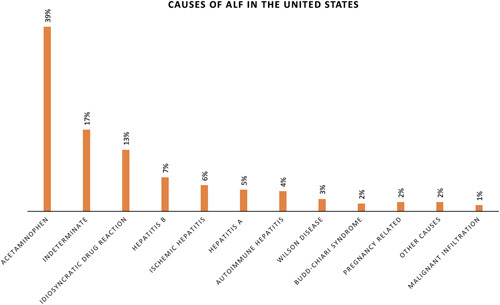
Etiologies of ALF in the US within the US Acute Liver Failure Study Group.6 This prospective study included 308 patients admitted with ALF to 17 tertiary care centers in the US over a 41-month period. The most common etiology for ALF was acetaminophen, idiosyncratic drug reaction, and hepatitis B. The cause was indeterminate in 17% of cases. Malignant infiltration accounted for only 1% of all cases. Abbreviation: ALF indicates acute liver failure.
Specific treatments for ALF are limited, often relying on supportive care and reversal of electrolyte abnormalities.1 Identifying an etiology is crucial for management to reverse the ongoing liver injury, and the differential must extend beyond the common causes. As seen in this case, liver biopsy should be strongly considered if the etiology of ALF is not apparent based upon the history, physical examination, infectious, serologic, and radiographic workup. The goal of biopsy is to identify a potential etiology for the liver injury such as AIH, toxin exposure, and malignancy in which the treatment strategy may change beyond supportive care.7 Biopsy is also important when considering malignant infiltration as a cause for ALF as this would be a contraindication to liver transplant. Preferably, biopsy should be considered early to minimize complications from worsening coagulopathy.
Despite the liver being a common site of malignant metastasis, malignant infiltration represents a very rare presentation of ALF (Table 1). In the King’s College Hospital series of 4020 patients presenting with ALF between 1978 and 1995, only 18 patients (0.44%) were due to malignant infiltration and carried a mortality of 94%.8 In the United States Acute Liver Failure Study Group Registry of 1910 patients between 1998 and 2012, malignant infiltration was identified in 27 (1.4%) of patients.9 Of this group, leukemia/lymphoma was the most common cause (44%) with other causes being breast (30%) and colon (7%). Other cancers include signet ring adenocarcinoma, uterine, prostate, thyroid, pancreatic, and small cell lung cancer (4% each).9
TABLE 1.
Malignant infiltration as cause of acute liver failure within the Acute Liver Failure (ALF) Study Group and King’s College Hospital7,8
| n (%) | ||
|---|---|---|
| Primary tumor | ALF Study Group [n=27 (of 1910 patients)] | King’s College Hospital [n=18 (of 4020 patients)] |
| Breast cancer | 8 (30) | — |
| Leukemia/lymphoma | 11 (41) | 12 (66) |
| Colon cancer | 2 (7) | — |
| Signet ring adenocarcinoma | 1 (4) | — |
| Uterine | 1 (4) | — |
| Prostate | 1 (4) | — |
| Thyroid | 1 (4) | — |
| Pancreatic | 1 (4) | — |
| Small cell lung cancer | 1 (4) | — |
| Metastatic carcinoma | — | 4 (22) |
| Hematophagocytic | — | 2 (11) |
PTCL-NOS represents a heterogenous group of both nodal and extranodal T-cell lymphomas that do not fit the World Health Organization classification of lymphoid neoplasms.10 The median age of presentation is 60 with most presenting at advanced stage III/IV disease (69%). Presence of nodal disease is common with only 13% of patients presenting with extranodal disease alone.11 Extranodal sites include the liver (17%), spleen (24%), skin (16%), subcutaneous tissues (6%), and lungs (8%).11 As a whole, this diagnosis carries a poor prognosis with ∼32% 5-year survival.11 Treatment generally involves multiagent chemotherapy such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone).10
We present a rare case of PTCL-NOS leading to ALF with primary hepatic involvement. Primary hepatic lymphoma (PHL) constitutes only 0.4% of all extranodal non-Hodgkin lymphoma cases. The exact pathogenesis of the disease is not known; however, there have been possible associations with HCV, HBV, Epstein-Barr virus, and immunosuppression from HIV. On imaging, PHL can present as a hypoattenuating solitary lesion (55%–60%), multiple lesions (35%–40%), or with diffuse involvement. More diffuse involvement carries worse prognosis (as in our patient). Most cases of PHL are secondary to diffuse large B-cell lymphoma with non–diffuse large B-cell lymphoma types present in <5%.12
Since malignant infiltration is an uncommon cause of ALF, clinicians must keep a high index of suspicion for this process. Liver biopsy is a key for making the diagnosis and should be strongly considered if the etiology of ALF is not evident after clinical history, infectious, and serologic evaluation are completed.
Question 2
What is the most common infiltrative malignancy associated with acute liver failure?
Colon cancer
Leukemia/lymphoma
Breast Cancer
Melanoma
KEY POINTS
Liver biopsy should be pursued when the etiology of acute liver failure (ALF) is not evident after initial history, laboratory, and radiographic workup. The main role of liver biopsy is to identify reversible causes with specific treatments.
Although rare, malignant infiltration should be considered as a cause for ALF as it would preclude candidacy for transplant.
Leukemia and lymphoma are the most common infiltrative malignancies that lead to ALF.
Acknowledgments
AUTHOR CONTRIBUTIONS
Manuscript Writing: J.L., M.A., M.R.K. and C.W.B.
Manuscript Review: J.L., M.A., M.R.K. and C.W.B.
CONFLICT OF INTEREST
C.W.B. serves as a AASLD Governing Board member. The remaining authors report no conflicts of interest.
Contributor Information
Joshua Lee, Email: jpl49@duke.edu.
Mitchell Arbogast, Email: mitchell.arbogast@duke.edu.
Matthew R. Kappus, Email: matthew.kappus@duke.edu.
Carla W. Brady, Email: carla.brady@duke.edu.
REFERENCES
- 1.Stravitz RT, Lee WM. Acute liver failure. Lancet. 2019;394:869–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013;369:2525–2534. [DOI] [PubMed] [Google Scholar]
- 3.Trey C, Davidson CS. The management of fulminant hepatic failure. Prog Liver Dis. 1970;3:282–298. [PubMed] [Google Scholar]
- 4.Chung RT, Stravitz RT, Fontana RJ, et al. Pathogenesis of liver injury in acute liver failure. Gastroenterology. 2012;143:e1–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee WM, Squires RH, Jr, Nyberg SL, et al. Acute liver failure: summary of a workshop. Hepatology. 2008;47:1401–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostapowicz G, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–954. [DOI] [PubMed] [Google Scholar]
- 7.Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology. 2012;55:965–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rowbotham D, Wendon J, Williams R. Acute liver failure secondary to hepatic infiltration: a single centre experience of 18 cases. Gut. 1998;42:576–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rich NE, Sanders C, Hughes RS, et al. Malignant infiltration of the liver presenting as acute liver failure. Clin Gastroenterol Hepatol. 2015;13:1025–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foss FM, Zinzani PL, Vose JM, et al. Peripheral T-cell lymphoma. Blood. 2011;117:6756–6767. [DOI] [PubMed] [Google Scholar]
- 11.Weisenburger DD, Savage KJ, Harris NL, et al. Peripheral T-cell lymphoma, not otherwise specified: a report of 340 cases from the International Peripheral T-cell Lymphoma Project. Blood. 2011;117:3402–3408. [DOI] [PubMed] [Google Scholar]
- 12.Noronha V, Shafi NQ, Obando JA, et al. Primary non-Hodgkin’s lymphoma of the liver. Crit Rev Oncol Hematol. 2005;53:199–207. [DOI] [PubMed] [Google Scholar]


