Abstract
A 43-year-old Japanese woman with rheumatoid arthritis treated by infliximab and methotrexate for 11 years was admitted for proteinuria and purpura. A kidney biopsy revealed endothelial damage-dominant nephritis with IgA deposition. Infliximab and methotrexate were discontinued, and tocilizumab was started; however, proteinuria persisted. Therefore, tocilizumab was discontinued, and oral prednisolone and methylprednisolone pulse therapy were administered. After 6 months, urinary protein was less than 0.1 g/day, and purpura subsided. To our knowledge, this is the first case of endothelial damage-dominant nephritis related to IgA vasculitis involving the skin and kidney after long-term use of infliximab and methotrexate.
Keywords: endocapillary glomerulonephritis, IgA vasculitis, tocilizumab, rheumatoid arthritis
Introduction
Until the early 2000s, treatment of rheumatoid arthritis (RA) was known to cause renal complications, such as membranous nephropathy (1). Thereafter, biologics, e.g. tumor necrosis factor alpha (TNFα) inhibitors and humanized anti-interleukin (IL)-6 receptor antibody, started to be used for RA, and the details of kidney damage in RA patients consequently changed, as vasculitis related to TNFα inhibitors became a new complication (2). Furthermore, AA amyloidosis became treatable (1,3).
We herein report a case of endothelial damage-dominant nephritis related to IgA vasculitis that developed after long-term use of infliximab and methotrexate for RA and improved with steroid therapy.
Case Report
A 43-year-old Japanese woman was admitted for the evaluation of proteinuria and purpura. The patient had been diagnosed with RA when she developed bilateral arthropathy of the hands at 32 years old. Treatment was started with a combination of methotrexate 8 mg/week and infliximab 150 mg/day every 8 weeks, and the disease activity of RA subsequently subsided. Six weeks before admission to our hospital, the patient developed purpura on both lower limbs that gradually worsened. After 2 weeks, she was found to have proteinuria (1.74 g/day).
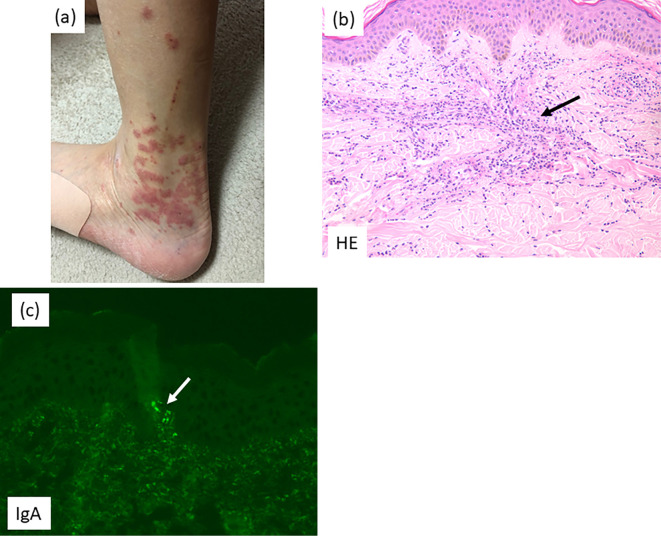
On admission, the patient was 162.0 cm tall and weighed 49.7 kg; her blood pressure was 128/74 mmHg, and her temperature was 37.0°C. A physical examination did not reveal any abnormalities of the heart, lungs or peripheral nerves. Her fingers were deformed at the proximal interphalangeal and metacarpophalangeal joints bilaterally. Non-blanching palpable purpura was noted in scattered patches on the lower limbs and left abdomen (Fig. 1a).
Figure 1.
Skin lesion. a: Purpura on the lower leg. b: Light microscopy: Neutrophils with nuclear debris and eosinophils (arrow) are seen surrounding blood vessels in the subcutaneous tissue (Hematoxylin and Eosin staining). c: Immunofluorescence microscopy: Blood vessels showed positivity for IgA (arrow).
The laboratory findings were as follows: serum creatinine, 0.67 mg/dL; estimated glomerular filtration rate, 75.5 mL/min/1.73 m2; C-reactive protein, 0.02 mg/dL; and serum amyloid A protein, <2.5 mg/dL. In addition, rheumatoid factor was 10 U/mL (normal level, <10), and cyclic citrullinated peptide antibodies were positive with 116.5 U/mL (normal level, <4.5 U/mL). The 24-h urinary protein excretion was 2.84 g, and the urine sediment contained <1 red blood cell per high-power field. The disease activity score with C-reactive protein was 2.4. A lower leg skin biopsy and kidney biopsy were performed.
Skin biopsy details
Neutrophils with nuclear debris and eosinophils were seen surrounding blood vessels in the subcutaneous tissue, and leukocytoplastic vasculitis was diagnosed (Fig. 1b). In addition, immunofluorescence microscopy showed IgA, C3 and fibrinogen depositions in the blood vessels (Fig. 1c).
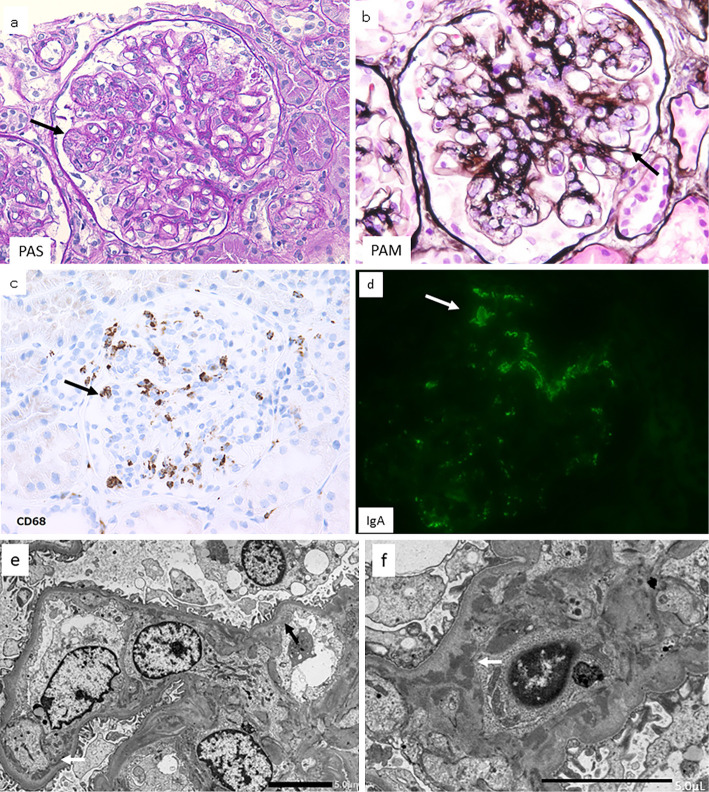
Kidney biopsy details
A light microscopic examination showed global sclerosis in 1 out of 41 glomeruli. Almost all glomeruli displayed endothelial damage-dominant nephritis, which was characterized by endothelial cell swelling with subendothelial edema (resulting in obstruction and/or narrowing of the glomerular cavity) (Fig. 2a) and a double-contour appearance and thickening of the glomerular basement membrane (Fig. 2b); however, neither thrombosis nor spike formation was observed. CD68-positive cells (related to the development of IgA vasculitis) were seen in the glomeruli (Fig. 2c). Tubular atrophy and tubulointerstitial fibrosis were present in <10% of the cortical region. Arterioles and interlobular arteries were not sclerotic, and no crescent formation was seen. Immunofluorescence microscopy showed that the glomeruli were mildly positive for IgA (Fig. 2d), positive for IgA1, and weakly positive for C3; however, they were negative for IgG and IgM. Electron microscopy revealed endothelial cell swelling with expansion of the subendothelial space and loss of mesangial architecture (mesangiolysis). Small amounts of electron-dense deposits were noted in the subendothelial space and paramesangial area, and moderate foot process effacement was seen (Fig. 2e, f).
Figure 2.
Kidney lesion. Microscopy findings of the kidney biopsy specimen. a: Light microscopy: Almost all glomeruli displayed endocapillary glomerulonephritis that was characterized by endothelial cell swelling (arrow), resulting in the obstruction and/or narrowing of the glomerular cavity; periodic acid-Schiff staining. b: Light microscopy: Double-contour appearance and thickening of the glomerular basement membrane (arrow) (periodic acid-methenamine silver staining). c: Light microscopy: CD68-positive cells (arrow) were seen in the glomeruli (CD68 staining). d: Immunofluorescence microscopy: Glomeruli showed mild positivity for IgA (green area, arrow). e: Electron microscopy: Endothelial cells were swollen, and subendothelial edema was seen (black arrow); electron-dense deposits (white arrow) were found in the subendothelial space. f: Electron microscopy: electron-dense deposits (white arrow) were found in the paramesangial area.
The diagnosis
The patient was diagnosed with endocapillary glomerulonephritis with endothelial damage-dominant nephritis complicated by IgA vasculitis involving the kidneys and skin.
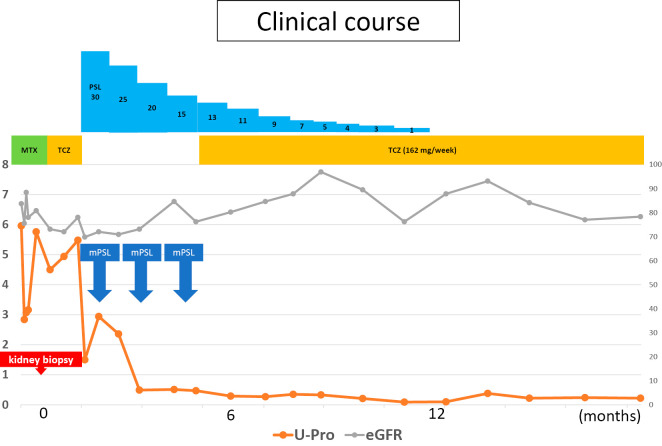
Clinical course
After a kidney biopsy, methotrexate and infliximab were discontinued; however, proteinuria and purpura persisted, and arthralgia recurred. Therefore, subcutaneous tocilizumab was started at a dose of 162 mg once a week. Because proteinuria persisted (4-5 g/day), tocilizumab was discontinued, and oral prednisolone 30 mg/day was started with concomitant thrice-monthly cycles of methylprednisolone pulse therapy (500 mg/day for 3 days). After 6 months, urinary protein decreased to less than 0.1 g/day, and purpura disappeared. Prednisolone was tapered to 13 mg/day, but arthralgia recurred. Therefore, tocilizumab was restarted, and prednisolone was discontinued after 12 months. With continued monotherapy with tocilizumab, the RA disease activity subsided, and proteinuria is negative as of the most recent examination (at 20 months) (Fig. 3).
Figure 3.
Clinical course. MTX: methotrexate, TCZ: tocilizumab, PSL: prednisolone, mPSL: methylprednisolone
Discussion
Although IgA vasculitis has been reported as a disease associated with IgA deposition in the skin and kidneys, we confirmed the importance of this case report by carefully examining how many previous reports of vasculitis after TNFα inhibitor administration had focused on IgA vasculitis. We conducted a PubMed search for cases of vasculitis related to TNFα inhibitors and found several papers that described vasculitis after TNFα inhibitor administration. However, we found no reports of endothelial damage-dominant nephritis related to IgA vasculitis involving the skin and kidneys.
Saint Marcoux et al. investigated 39 cases of vasculitis that occurred during treatment with TNFα inhibitors, including etanercept (21 cases), infliximab (15 cases), adalimumab (2 cases), and another drug (1 case) (2). The mean duration of treatment before development of vasculitis was 14.1±8.7 years. Vasculitis was found in the skin (32 cases) and kidneys (7 cases), and skin biopsies showed non-necrotizing vasculitis (12 cases), necrotizing vasculitis (7 cases), and inflammatory dermatitis (3 cases); however, this publication did not describe the presence of IgA deposits. A kidney biopsy showed extracapillary glomerulonephritis with IgA deposits in two of the patients. Some patients improved with the discontinuation of TNFα inhibitors, but others required treatment with steroids or other drugs (2).
Mohan et al. reported 35 cases of leukocytoplastic vasculitis diagnosed by a skin biopsy that occurred during treatment with TNFα inhibitors. The duration of treatment before development of vasculitis ranged from 28 weeks to more than 10 years. In most patients, the skin lesions improved after discontinuation of the TNFα inhibitor. However, this paper also did not mention the presence of IgA depositions or a diagnosis of IgA vasculitis (4).
Michel et al. reported a 47-year-old woman with RA who developed hematuria and proteinuria soon after starting treatment with abatacept, a cytotoxic T-lymphocyte antigen 4 immunoglobulin and selective T-cell co-stimulation modulator (5). A kidney biopsy showed IgA nephropathy with necrosis and extracapillary crescent formation. Urinary protein levels decreased several months after the administration of a corticosteroid.
Karasawa et al. reported a 48-year-old woman with purpura, microscopic hematuria, and proteinuria that appeared during the use of etanercept for RA (6). Based on the kidney biopsy results, the patient was diagnosed with IgA vasculitis with nephritis with crescent formation and IgA1 deposition. A skin biopsy showed leukocytoplastic vasculitis with C3 deposition. In this paper, we found no description of IgA deposition in skin lesions or renal lesions. Etanercept was discontinued, and steroid pulse treatment and corticosteroid treatment were performed. Proteinuria disappeared six months later (6).
IgA vasculitis and nephritis have been frequently reported in pediatric cases and are diagnosed by the presence of IgA deposits in the skin and kidney. Infections and drugs have been considered as causes of IgA vasculitis and nephritis, but the frequency is low, and the actual cause cannot be identified, although it is considered to be idiopathic. This characteristic is also true for adult cases. However, while there have been many recent reports of vasculitis after the administration of TNFα inhibitors, there have been few cases in which IgA vasculitis and nephritis were definitely identified. In the present case, the onset of vasculitis after the administration of the agents suggested that it may have been secondary. Gd-IgA1-specific antibody KM55 is one indicator, but more information is still needed to differentiate between primary and secondary disease (7).
In the International Study of Kidney Disease in Children (ISKDC) classification of Henoch-Schönlein purpura nephritis (IgA vasculitis and nephritis), crescent formation is considered an indicator of activity, but there is also the membranoproliferative-like glomerulonephritis type, which case may correspond to membranoproliferative-like glomerulonephritis type (8).
Sokumbi et al. reported eight patients with vasculitis associated with anti-TNFα therapy. These drugs are widely used for entities other than RA, and the fact that vasculitis also occurred in patients with ulcerative colitis and Crohn's disease suggests that they are not disease-specific but drug-specific. The mean duration of treatment before development of vasculitis was 34.5 months (9). The relationship between IgA vasculitis and TNFα inhibitors should be given focus in future studies of RA patients (1).
Considering the findings of previous reports, kidney involvement of vasculitis occurring during treatment with TNFα inhibitors seems to be characterized by extracapillary glomerulonephritis, but there have been no reports of endothelial damage-dominant nephritis related to IgA vasculitis (2,5,6).
In conclusion, we describe the first case of endothelial damage-dominant nephritis related to IgA vasculitis involving skin and kidney after long-term use of infliximab and methotrexate. These kidney and skin lesions did not improve even after discontinuation of the drugs suspected of being responsible, and prednisolone therapy with concomitant methylprednisolone pulse therapy was required to achieve remission.
The patient gave her written informed consent for the publication of the details of her case.
The authors state that they have no Conflict of Interest (COI).
Financial Support
This study was funded by the Okinaka Memorial Institute for Medical Research.
References
- 1. Sawamura M, Sawa N, Yamanouchi M, et al. Use of biologic agents and methotrexate improves renal manifestation and outcome in patients with rheumatoid arthritis: a retrospective analysis. Clin Exp Nephrol 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saint Marcoux B, De Bandt M; CRI (Club Rhumatismes et Inflammation). Vasculitides induced by TNFα antagonists: a study in 39 patients in France. Joint Bone Spine 73: 710-713, 2006. [DOI] [PubMed] [Google Scholar]
- 3. Fukuda M, Sawa N, Hoshino J, Ohashi K, Miyazono M, Ubara Y. Tocilizumab preserves renal function in rheumatoid arthritis with AA amyloidosis and end-stage kidney disease: two case reports. Clin Nephrol 95: 54-61, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohan N, Edwards ET, Cupps TR, et al. Leukocytoclastic vasculitis associated with tumor necrosis factor-alpha blocking agents. J Rheumatol 31: 1955-1958, 2004. [PubMed] [Google Scholar]
- 5. Michel M, Henri P, Vincent FB, Leon N, Marcelli C. Mesangial immunoglobulin (Ig)A glomerulonephritis in a patient with rheumatoid arthritis treated with abatacept. Joint Bone Spine 80: 660-663, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Karasawa K, Iwabuchi Y, Kyoda M, et al. Primary IgA vasculitis with nephritis in a patient with rheumatoid arthritis diagnosed by anti-galactose-deficient IgA1 immunostaining. Intern Med 58: 2551-2554, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mizerska-Wasiak M, Turczyn A, Cichoń-Kawa K, et al. IgA vasculitis nephritis clinical course and kidney biopsy - national study in children. Pediatr Rheumatol Online J 19: 150, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jelusic M, Sestan M, Cimaz R, Ozen S. Different histological classifications for Henoch-Schönlein purpura nephritis: which one should be used? Pediatr Rheumatol Online J 17: 10, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sokumbi O, Wetter DA, Makol A, Warrington KJ. Vasculitis associated with tumor necrosis factor-α inhibitors. Mayo Clin Proc 87: 739-745, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]