Highlights
-
•
Vicarious racism and perceived discrimination are sources of distress and are associated with increased alcohol use.
-
•
Perceived discrimination plays a role in how a socially unjust negative event—like the murder of George Floyd—relates to problematic alcohol use.
-
•
Veterans who reported perceived discrimination had more severe alcohol-related problems than Veterans who reported no discrimination.
-
•
Racial/ethnic minorities reported experiencing greater subjective impact related to the murder of George Floyd.
-
•
Incorporating screening tools and having systems in place within substance use clinics that require clinicians to inquire about discrimination history in a culturally sensitive manner is recommended.
Keywords: Alcohol use, Perceived discrimination, Veterans, Social justice, Vicarious racism
Abstract
Introduction
On May 25, 2020, George Floyd was murdered by a Minneapolis police officer leading to increased social justice and antiracism movements (SJARM) across the United States. Vicarious exposure to racism and perceived discrimination are salient sources of distress which may lead to increased alcohol use as means of coping. The primary aim of the current study was to examine how perceived discrimination and the subjective impact and personal distress related to the SJARM following the George Floyd murder interact and relate to unhealthy alcohol use among U.S. Veterans.
Methods
286 Veterans were assessed for unhealthy alcohol use (AUDIT-10), perceived discrimination (EDS), and subjective impact and personal distress related to the SJARM. Two moderation analyses were performed to examine whether subjective impact and personal distress moderated relations between perceived discrimination and alcohol use. In-depth follow-up analyses were conducted to examine differences and relationships among variables.
Results
In two different moderation models, perceived discrimination moderated the association between both subjective impact (p <.001) and personal distress (p <.001) felt by the SJARM and unhealthy alcohol use. In planned exploratory analyses, Veterans who reported perceived discrimination reported higher levels of unhealthy alcohol use (M = 14.71, SD = 9.39) than those who did not t(2 8 4) = 5.61, p <.001. In post-hoc analyses, racial/ethnic minorities were significantly more likely to report perceived racial discrimination (p <.001) while non-Hispanic Whites were more likely to report perceived discrimination based on education or income level (p <.01).
Conclusions
In the context of a socially unjust event amidst a global pandemic, perceived discrimination contributes to unhealthy alcohol use and subjective impact and personal distress associated with the SJARM following the murder of George Floyd. Results highlight the importance of addressing discrimination experiences in Veterans who seek alcohol treatment, particularly as rates of unhealthy alcohol use are on the rise.
1. Introduction
Social, political, economic, ecological, and historical disruptions on a global scale, can lead to increases in substance use, tend to disproportionately impact vulnerable populations and can disrupt healthcare services and treatment utilized by those who use substances (Mackey & Strathdee, 2015). COVID-19, a global pandemic is such an event that resulted in increases in alcohol consumption and alcohol sales (Callinan et al., 2021, Grossman et al., 2020, Pollard et al., 2020, Schmidt et al., 2021). As the COVID-19 death toll was close to surpassing 100,000 in the United States, a second event occurred. On May 25, 2020, George Floyd was murdered by a Minneapolis police officer which led to an increase in social justice and antiracism movements (SJARM) in the U.S., and across the globe. Although increases in unhealthy alcohol use due to COVID-19 during this time period have been reported (Alpers et al., 2021, Barbosa et al., 2021, Killgore et al., 2021, Schmidt et al., 2021), there is a dearth of information on how the additional distress and impact from the George Floyd murder may have influenced unhealthy alcohol use among U.S. Veterans.
Unhealthy alcohol use (Saitz, 2005), including risky or hazardous drinking or alcohol use disorder (AUD), is common among U.S. Veterans (Miller et al., 2022, Teeters et al., 2017). Two in five Veterans have a lifetime history of AUD (Fuehrlein et al., 2016) which places this population at greater risk for a higher burden of disease and related mortality (Carvalho et al., 2019). Veterans who belong to socially disadvantaged groups are at greater risk for developing poor health outcomes and engaging in maladaptive health-related behaviors (e.g., unhealthy alcohol use) compared to their colleagues who belong to majority groups (Carlson et al., 2018, Hausmann et al., 2013). In recent years, the U.S. Veteran population has become increasingly more diverse (Kondo et al., 2017, MacDonald et al., 2020) and the number of Veterans who hold minority identities—e.g., racial and ethnic minorities, women, gender and sexual minorities—has increased (Sohn & Harada, 2008). When considering intersecting identities (i.e., Veteran identity, racial/ethnic minority, gender and sexual orientation), several studies suggest that poorer health outcomes exist among Veterans with AUD, particularly among those who have lower socioeconomic status (SES) and who hold minority status (Carr et al., 2021, Chen et al., 2020, Fuehrlein et al., 2016, Jegede et al., 2022, Kondo et al., 2017). Research has demonstrated that Veterans who identify as Black, Indigenous and/or people of color (BIPOC) have a higher prevalence of clinically recognized AUD, receive lower rates of alcohol-related care, and are less likely to receive AUD medications (Chen et al., 2020; E. C. Williams et al., 2016, Williams et al., 2017 ). Furthermore, BIPOC Veterans with lifetime AUD tend to have poorer functional outcomes and higher rates of co-occurring disorders such as major depressive disorder (Carr et al., 2021).
Discrimination, “the prejudicial treatment of individuals or groups of people based on their membership in socially constructed categories” (Dovidio, 1986, Glass et al., 2020) is a strong, consistent predictor of poorer health in Veterans with minority status (Carlson et al., 2018, Glass et al., 2020, Hausmann et al., 2013, MacDonald et al., 2020, Ruben et al., 2019). Veterans who experience discrimination are at an increased risk for alcohol-related problems, such as greater alcohol consumption and greater risk for AUD (Gilbert and Zemore, 2016, Jones et al., 2016, Livingston et al., 2019, Ruben et al., 2019). Although discrimination is linked with unhealthy alcohol use, a recent study found that Veterans who have experienced discrimination more frequently tend to be less willing to seek treatment (Miller et al., 2022). In an effort to understand the social determinants of health, there is an increasing body of research on how discrimination impacts health-related outcomes (Hausmann et al., 2013); however, literature on discrimination and its impact on U.S. Veterans has not been widely studied. As the commitment to health equity becomes increasingly more important (Hausmann et al., 2013, Kondo et al., 2017), an understanding of how the social determinants of health that impact the Veteran population is crucial.
With the rise of social media, there has been an increase in racism experienced online and vicarious racism experienced through various forms of media (Moody et al., 2022, Keum and Ángel Cano, 2022). The video of the murder of George Floyd and subsequent videos of the SJARMs that took place afterward were vastly replayed and shared across media outlets and social media (Eichstaedt et al., 2021, Giorgi et al., 2020). Vicarious experiences of racial, and socially unjust events—like the murder of George Floyd—have negative impacts on mental health and increases psychological distress (Bor et al., 2018, Maxie-Moreman and Tynes, 2022). Results from recent studies conducted during the COVID-19 pandemic suggest that vicarious racism was a source of psychological distress and concern among minority groups (Chae et al., 2021, Maxie-Moreman and Tynes, 2022). Similarly, research has also found that depression and anxiety symptoms related to vicarious racism experienced online may have led to an increased motivation to drink alcohol as a means of coping with distress (Keum & Ángel Cano, 2022). Despite these findings, a recent systematic review emphasized the dearth of studies in vicarious racism and the growing importance of this area of research given the rise of social media and prevalence of smart phones (Kirkinis et al., 2021).
Prior research suggests that individuals who identify with an affected group tend to be the most affected by traumatic group events (Eichstaedt et al., 2021, Goldenberg et al., 2020). For instance, although anger, sadness, anxiety, and depression increased among Americans after the murder of George Floyd, the increase was significantly more pronounced among Black Americans than White Americans (Eichstaedt et al., 2021). Similarly, distress due to perceived systemic racism and racial disparities in COVID-19-related health outcomes has been found to be high among BIPOC Veterans (Jegede et al., 2022). Veterans are disproportionately exposed to trauma and stress (Carlson et al., 2018) and discrimination is an additional chronic stressor that has demonstrated a significant association with unhealthy alcohol use (Albright et al., 2021, Seedat, 2021). It is possible that Veterans who have prior experiences of discrimination experienced higher levels of personal distress and subjective impact related to the SJARMs that took place after the murder of George Floyd which in turn, may have increased alcohol use.
The current study examines how perceived discrimination and the subjective impact and personal distress related to the SJARM after the George Floyd murder interact and relate to unhealthy alcohol use. We hypothesized a priori that greater perceived discrimination, higher personal distress, and more subjective impact related to the SJARM would result in increased reports of unhealthy alcohol use among a cohort of U.S. Veterans. In planned exploratory analyses, we examined how Veterans with different discrimination experiences (discrimination vs no experience of discrimination) differed in reporting of unhealthy alcohol use. We expected that Veterans who had experienced discrimination would report greater amounts of unhealthy alcohol use compared to the no discrimination group. In post-hoc analyses we also examined participants’ perceived reasons for discrimination, whether those reasons predicted unhealthy alcohol use, and whether those reasons differed among participants who identify as non-Hispanic White and participants who identify as racial and ethnic minorities.
2. Methods
2.1. Participants and procedures
The present study is based on secondary analyses of an outcome study that was initially developed to explore the characteristics, mental health symptoms, and substance use behaviors of U.S. Veterans following the emergence of the COVID-19 pandemic. Participants were recruited using the Qualtrics survey platform. Focused online research panels within Qualtrics were used to target our sample of U.S. Veterans, all of whom previously agreed to participate in survey-based research. Study inclusion criteria included being a U.S. Veteran between 18 and 70 years of age and currently residing in the U.S. Participants were excluded if they were not a U.S. Veteran, did not complete the entire survey, failed an embedded survey attention check, and/or their current residence within the U.S. could not be verified. Data were collected between October 23rd and November 3rd of 2020.All procedures were approved by the University of California, San Francisco.
2.2. Measures
2.2.1. Unhealthy alcohol use
Unhealthy alcohol use was measured using the Alcohol Use Disorders Identification Test 10 (AUDIT-10). The AUDIT-10 is a 10-item screening tool developed by the World Health Organization (WHO) to assess alcohol consumption, drinking behaviors, and alcohol-related negative consequences (Babor et al., 2001). Scores of 8 or more are indicative of hazardous or harmful alcohol use, and scores of 13 or more (among women) and 15 or more (among men) suggest possible alcohol use disorder.
2.2.2. Perceived discrimination
Perceived discrimination was measured using the Everyday Discrimination Scale (EDS). The EDS is a 9-item self-report scale that measures aspects of chronic or episodic day-to-day, subjective experiences of perceived discrimination (Williams et al., 1997). Responses are coded on a 6-point Likert scale ranging from ‘never’ to ‘almost everyday.’ Greater scores represent higher levels of perceived discrimination. If participants answered “never” to all 9 items, they were coded into the non-discrimination group. If participants answered any other choice aside from “never” to any of the questions, they were coded into the discrimination group and a follow-up question of, “What do you think is the main reason for these experiences?” was asked. Responses to the follow-up question (of which respondents could choose more than one) included: (1) your ancestry or national origins, (2) your gender, (3) your race, (4) your age, (5) your religion, (6) your height, (7) your weight, (8) some other aspect of your physical appearance, (9) your sexual orientation, (10) your education or income level, (11) a physical disability, (12) your shade of skin color, (13) your tribe, or (14) other.
2.2.3. Social justice anti-racism movement impact and distress items
Given that there were no standardized research questions to assess for subjective impact and personal distress related to the SJARM following the murder of George Floyd, the research team developed two face-valid questions to measure subjective impact and personal distress. To measure subjective impact, participants were asked the following question, “Overall, how much has your life been impacted by the SJARM?” Answer choices were in Likert Scale format and ranged from 0 (not at all) to 4 (extremely). To measure personal distress, participants were asked the following, “Please rate the extent to which social injustices and racism since George Floyd’s death have caused you distress.” Answer choices were in a scale format and ranged from 0 (not at all) to 10 (a lot).
2.3. Statistical analyses
2.3.1. Power estimates
An a priori power analysis was performed for sample size estimation using G*Power (Faul et al., 2009) version 3.1.9.2. This study was designed for adequate power for two moderated regressions that examine the interaction between two continuous predictors (personal distress and subjective impact from SJARM and perceived discrimination). Power calculations were conducted based on a 0.05 alpha level and 80% power (1-β). These calculations suggested that for a moderated regression, total sample size of 36 to 77 is required to detect a medium to large effect size (0.15 ≤ ƒ2 ≥ 0.35). Given these power approximations, we expected our study sample of 286 to be appropriately powered to detect the hypothesized effects.
2.3.2. Descriptive and statistical model analyses
All analyses were performed using IBM SPSS Statistics for Windows, version 27 (IBM Corp., Armonk, N.Y., USA). Prior to analyses, participants who indicated that they drank alcohol within the past six months were selected and included in the analysis. Dependent variable normality was confirmed. Demographic characteristics were compared between the two discrimination groups using one-way ANOVAs for continuous variables and the chi-square test for categorical variables. To examine the interplay between impact and distress felt by the SJARM, perceived discrimination, and AUDIT scores, two moderation analyses were performed using Hayes PROCESS Model 1 (Hayes, 2017). Model one included problematic alcohol use (total AUDIT score) as the criterion, with the SJARM impact score, total perceived discrimination score, and SJARM impact score-by-total perceived discrimination interaction term as fixed effects. Model two included unhealthy alcohol use (total AUDIT score) as the criterion, with the SJARM personal distress score, total perceived discrimination score, and SJARM impact score-by-total perceived discrimination interaction term as fixed effects. All continuous variables were mean-centered. To clarify the direction of a significant interaction we performed follow-up tests that examined associations between SJARM impact and distress and unhealthy alcohol use at low, average, and high perceived levels of discrimination, where low and high represent 1 standard deviation below and above the group mean, respectively. In planned exploratory analyses, an independent samples t-test was conducted on total AUDIT score to analyze differences between participants with and without a self-reported history of perceived discrimination. In post-hoc analyses, (1) a multiple regression analysis was conducted among those with a discrimination history to investigate which perceived reasons for discrimination predicted AUDIT scores, and (2) chi-square tests of independence were conducted on perceived reasons for discrimination experience(s) to analyze differences between participants who identify as non-Hispanic White and participants who identify as racial and ethnic minorities.
3. Results
3.1. Participant characteristics
The total sample consisted of 286 Veterans who endorsed drinking alcohol within the past 6 months. Mean participant age was 45.6 (SD ± 13.05). Most participants identified as cisgender males (n = 222; 77.6 %). About one quarter of the sample identified as cisgender females (n = 63; 22.0 %), with one participant identifying as non-binary. Most participants identified as non-Hispanic (n = 258; 90.2 %) and White (n = 250; 87.4 %). Approximately 10 % of the sample identified as Black or African American (n = 29), with the remainder of participants identifying as Indigenous (n = 7; 2.4 %), Asian (n = 2; 0.7 %), Multiracial (n = 6; 2.1 %) or an unknown or unreported racial identity (n = 3; 1.0 %). Most participants reported that they were married (n = 222; 77.6 %), followed by single (n = 28; 9.8 %) and divorced (n = 26; 9.1 %). Over half of the sample (n = 151; 52.8 %) reported that they served in the U.S. Army, with the remainder identifying past service in the Navy (n = 51; 17.8 %), Air Force, (n = 41; 14.3 %), Marine Corps (n = 25; 8.7 %), National Guard (n = 13; 4.5 %), and/or other branches of the military (n = 5; 1.7 %). Characteristics of the sample are summarized in Table 1.
Table 1.
Characteristics of the sample.
| Total (N = 286) |
No Discrimination (n = 58) |
Discrimination (n = 228) |
|
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age (M ± SD)*** | 45.6 ± 13.05 | 53.9 ± 11.91 | 43.5 ± 12.48 |
| Gender** | |||
| Male | 222 (77.6 %) | 52 (89.7 %) | 170 (74.6 %) |
| Female | 63 (22.0 %) | 6 (10.3 %) | 57 (25 %) |
| Non-binary | 1 (0.3 %) | 0 (0 %) | 1(0.4 %) |
| Race (%) | |||
| White | 250 (87.4 %) | 54 (93.1 %) | 196 (85.9 %) |
| Black or AA | 29 (10.1 %) | 4 (6.9 %) | 26 (11.4 %) |
| Indigenous | 7 (2.4 %) | 2 (3.4 %) | 5 (2.2 %) |
| Asian | 2 (0.7 %) | 0 (0 %) | 2 (0.9 %) |
| Multiracial | 6 (2.1 %) | 2 (3.4 %) | 4 (1.8 %) |
| Prefer not to state / Not Listed | 3 (1.0 %) | 0 (0 %) | 3 (1.3 %) |
| Ethnicity | |||
| NH/LTX | 258 (90.2 %) | 56 (96.6 %) | 202 (88.6 %) |
| H/LTX | 26 (9.1 %) | 2 (3.4 %) | 24 (10.5 %) |
| Not reported | 2 (0.7 %) | (0.0 %) | 2 (0.9 %) |
| Military branch | |||
| Air Force | 41 (14.3 %) | 8 (13.8 %) | 33 (14.5 %) |
| Army | 151 (52.8 %) | 29 (50.0 %) | 122 (53.5 %) |
| Coast Guard | 2 (0.7 %) | 0 (0 %) | 2 (0.9 %) |
| Marine Corps | 25 (8.7 %) | 5 (8.6 %) | 20 (8.8 %) |
| Merchant Marine | 1 (0.3 %) | 0 (0 %) | 1 (0.4 %) |
| National Guard | 13 (4.5 %) | 1 (1.7 %) | 12 (5.3 %) |
| Navy | 51 (17.8 %) | 14 (24.1 %) | 37 (16.2 %) |
| Other | 2 (0.7 %) | 1 (1.7 %) | 1 (0.4 %) |
| U.S. region | |||
| Northeast | 95 (33.2 %) | 12 (20.7 %) | 83 (36.4 %) |
| South | 114 (39.9 %) | 29 (50.0 %) | 85 (37.3 %) |
| West | 26 (9.1 %) | 4 (6.9 %) | 22 (9.6 %) |
| Non-contiguous (Alaska) | 51 (17.8 %) | 13 (22.4 %) | 38 (16.7 %) |
| Marital status | |||
| Single | 28 (9.8 %) | 6 (10.3 %) | 22 (9.6 %) |
| Married | 222 (77.6 %) | 40 (69.0 %) | 182 (79.8 %) |
| Separated | 1 (0.3 %) | 0 (0 %) | 1 (0.4 %) |
| Divorced | 26 (9.1 %) | 10 (17.2 %) | 16 (7 %) |
| Widowed | 7 (2.4 %) | 2 (3.4 %) | 5 (2.2 %) |
| Other | 2 (0.7 %) | 0 (0 %) | 2 (0.9 %) |
**p <.01, ***p <.001. H/LTX = Hispanic/Latinx. NH/LTX = Not Hispanic/Latinx. AA African American.
3.2. A priori analyses
3.2.1. Interaction between personal distress felt by the SJARM and perceived discrimination on AUDIT scores (Model 1)
The overall moderation model was significant (p <.001), and we observed a significant SJARM personal distress-by-perceived discrimination interaction on AUDIT scores (β = 0.04, [95 % CI, 0.01 – 0.06], p <.001). Further interrogation of this interaction revealed that SJARM personal distress predicted AUDIT scores at all levels of perceived discrimination, while the relationship between SJARM personal distress and AUDIT scores became significantly stronger as perceived discrimination increased (Low: β = 0.45, [95 % CI, 0.10 – 0.80]; Average: β = 0.88, [95 % CI, 0.61 – 1.15]; High: β = 1.31, [95 % CI, 0.91– 1.71], all p <.01). Estimated marginal means of linear trends for this model can be found in Table 2.
Table 2.
Estimated Marginal Means of Linear trends Moderation Model 1 and 2.
| 95 % Confidence Interval |
||||
|---|---|---|---|---|
| B (SE) | Lower | Upper | p-value | |
|
SJARM Personal Distress ∼ AUDIT Score −1 SD Perceived Discrimination (-11.88) |
0.45 (0.18) |
0.10 |
0.80 |
0.01 |
| Mean Perceived Discrimination (0.00) | 0.88 (0.14) | 0.61 | 1.15 | 0.001 |
| +1 SD Perceived Discrimination (11.88) | 1.31 (0.20) | 0.91 | 1.71 | 0.001 |
|
SJARM Subjective Impact ∼ AUDIT Score −1 SD Perceived Discrimination (-11.88) |
1.57 (0.43) |
0.74 |
2.41 |
0.001 |
| Mean Perceived Discrimination (0.00) | 2.37 (0.33) | 1.73 | 3.02 | 0.001 |
| +1 SD Perceived Discrimination (11.88) | 3.17 (0.46) | 2.26 | 4.09 | 0.001 |
3.2.2. Interaction between subjective impact felt by the SJARM and perceived discrimination on AUDIT scores (Model 2)
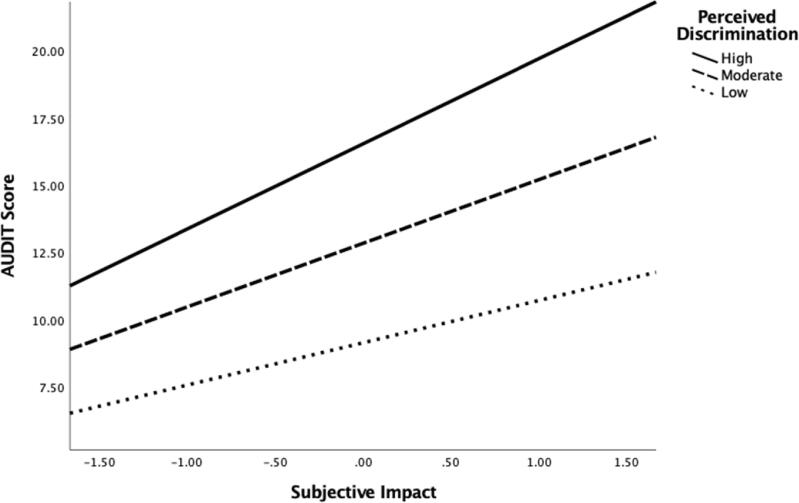
The overall moderation model was significant (p <.001) and we observed a significant SJARM subjective impact-by-perceived discrimination interaction for AUDIT scores (β = 0.07, [95 % CI, 0.02 – 0.12], p <.01). Further interrogation of this interaction revealed that SJARM subjective impact predicted AUDIT scores at all levels of perceived discrimination, while the relationship between SJARM subjective impact and AUDIT scores became significantly stronger as perceived discrimination increased (Low: β = 1.57, [95 % CI, 0.74 – 2.41], p <.001; Average: β = 2.37, [95 % CI, 1.73 – 3.02], p <.001; High: β = 3.17, [95 % CI, 2.26– 4.09], p <.001). Estimated marginal means of linear trends for this model are in Table 2 and a graphical representation is located in Fig. 1.
Fig. 1.
Perceived Discrimination Moderating Effect Between Hazardous Alcohol Use and Subjective Impact.
3.3. Planned exploratory analyses
3.3.1. Group differences in discrimination history
There was a statistically significant difference in AUDIT scores between the discrimination (M = 14.71, SD = 9.39) and non-discrimination group (M = 7.55, SD = 4.99); t(284) = 5.61, p <.001. This difference, 95 % CI [4.65, 9.68], represented an effect size of d = 0.82.
3.4. Post-hoc analyses
3.4.1. Multiple regression analysis predicting hazardous alcohol use
The results of the regression indicated that the model explained 18.2 % of the variance and that the model was a significant predictor of AUDIT scores, F (14, 213) = 3.38, p <.001. Religion (B = 3.24, p <.05), tribe (B = 6.11, p <.05), and other (B = -8.41, p <.05) were significant predictors in the model. Participants were able to provide text responses if they selected the “other” option; some responses that were provided by participants included: Politics, being a Veteran, a stutter and having a mental disorder; 100 % of participants who indicated perceived discrimination based on other factors identified as non-Hispanic White. Of those who indicated perceived discrimination based on religion, 90.4 % identified as non-Hispanic White. Similarly, participants who indicated perceived discrimination based on tribe were predominantly non-Hispanic White (80 %).
3.4.2. Differences between participants who identify as non-Hispanic whites vs racial/ethnic minorities in perceived reasons for discrimination experience(s)
Racial/ethnic minorities were significantly more likely to report perceived racial discrimination [R/E: 57.4 % vs W: 26.4 %; χ2 (1, N = 228) = 17.67, p <.001] and perceived discrimination based on shade of skin color [R/E: 42.6 % vs W: 8.6 %; [χ2 (1, N = 228) = 34.24, p <.001]. Non-Hispanic White participants were significantly more likely to report perceived discrimination based on religion [W: 27 % vs R/E: 9.3 %; [χ2 (1, N = 228) = 7.38, p <.01], and perceived discrimination based on education or income level [W: 31 % vs R/E: 11.1 %; [χ2 (1, N = 228) = 8.44, p <.01].
Based on these findings from post-hoc analyses, we conducted three additional t-tests to examine differences between non-Hispanic White participants and racial/ethnic minority participants in reporting unhealthy alcohol use, subjective impact related to the SJARM, and personal distress related to the SJARM. There was a statistically significant difference in subjective impact between the non-Hispanic White group (M = 1.76, SD = 1.38) and the racial/ethnic minority group (M = 2.15, SD = 1.23); t (284) = -1.98, p <.05. This difference, 95 % CI [-0.576. -0.001], represented an effect size of d = -0.29.
4. Discussion
The complex intersections between individual identities, structural systems of oppression—i.e., racism, health disparities, poverty, inequity— and their deleterious impact on health were magnified during COVID-19 and they became more evident with the murder of George Floyd (Aaron and Stanford, 2022, Eichstaedt et al., 2021, Hagle et al., 2021, Homan et al., 2021, Krieger, 2020, Weine et al., 2020). In the context of a socially unjust event amidst a global pandemic, perceived discrimination contributes to unhealthy alcohol use. Our primary findings indicate that perceived discrimination plays a role in how a socially unjust negative event—like the murder of George Floyd—relates to unhealthy alcohol use. In two different moderation models, we found that perceived discrimination moderated the association between both subjective impact and personal distress felt by the SJARM and unhealthy alcohol use. Specifically, as levels of perceived discrimination increased, the strength of the relationship between SJARM distress/impact and unhealthy alcohol use also increased.
These findings suggest that learning about a socially unjust event may be related to increased unhealthy alcohol use in individuals who have experienced similar socially unjust events such as perceived discrimination. Findings from previous studies indicate that individuals who experience discrimination may be drinking to cope with these stressful and harmful encounters (Desalu et al., 2019, Kalb et al., 2018, Livingston et al., 2019). Similarly, research has found that experiencing discrimination has a cumulative effect on mental health suggesting that discrimination continues to impact individuals after they have experienced it (Wallace et al., 2016). It is possible that in this study, Veterans who had previously experienced discrimination may be drinking to cope and may have already had more alcohol-related problems compared to those who had not previously experienced discrimination.
There is a considerable body of research that suggests that experiencing discrimination—particularly race/ethnic and sexual/gender minority discrimination—is positively associated with increased alcohol use (Gilbert & Zemore, 2016), one of the leading modifiable risk factors for morbidity and mortality in the U.S. (Rehm & Shield, 2019). In this study, Veterans who reported perceived discrimination had more severe alcohol-related problems than Veterans who reported no discrimination. Experiences of discrimination and minority stress are also associated with higher rates of alcohol-related problems among Veterans who hold marginalized identities (e.g., gender and sexual minorities, disability, lower socioeconomic status) that are not specific to race (Bryan et al., 2017, Livingston et al., 2017, MacLean et al., 2018). Social factors compounded with adversity exacerbate alcohol use and the health consequences associated with these factors (Galea and Vlahov, 2002, Melamed et al., 2020).
Research on the various levels of discrimination and alcohol use remains underdeveloped as the majority of the literature focuses on racial and sexual orientation discrimination (Gilbert & Zemore, 2016). According to an extensive systematic review examining the relationship between discrimination and heavy and hazardous drinking, no studies examined the association between religious discrimination and alcohol use (Gilbert & Zemore, 2016). Results from the current study however, found that religious discrimination was a significant predictor of unhealthy alcohol use. Although religion has been found to be a protective factor against alcohol use among Veterans (Sharma et al., 2017), experiencing the stress of being discriminated against due to religion may be a risk factor.
Likewise, perceived discrimination based on one’s tribe was also a significant predictor of unhealthy alcohol use in this sample of Veterans. It is important to note that the EDS does not operationally define the term ‘tribe,’ therefore, individuals from different racial and ethnic compositions may interpret the term ‘tribe’ in different ways. For example, Indigenous participants may have very specific and strong spiritual, judicial, and geographical associations with the use of the word tribe. Interestingly, no participants who identified as Indigenous indicated experiencing perceived discrimination based on tribe however, 80 % of non-Hispanic Whites did. These results may reflect how non-Hispanic White participants characterize their fellow Veteran group given that the military indoctrinates service members to have a collectivistic perspective and the sharing of a unique identity (McGurk et al., 2006), which in their perspective may resemble a colloquial understanding of the word tribe. Accurate definitions of culturally sensitive terminology must be prioritized to: 1) honor the dignity of cultures that might be impacted by its misuse and 2) draw appropriate interpretations in our research.
Finally, perceived discrimination based on various other factors was also found to be a significant predictor of unhealthy alcohol use. Responses that were provided by participants who indicated perceived discrimination based on other factors included being a Veteran, politics, a stutter, and having a mental disorder. Discrimination, regardless of the cause is linked to higher levels of stress (APA, 2016) and the anxiolytic effect of alcohol can influence one’s motivation to drink to alleviate stress (Becker, 2017). Participants who indicated other factors of perceived discrimination may be experiencing a higher level of stress from these specific reasons and thus may also be drinking to cope.
Findings from exploratory analyses also indicated differences in reasons for perceived discrimination between non-Hispanic Whites and racial and ethnic minorities. Non-Hispanic Whites were more likely to report perceived discrimination due to religion and education or income level. It is possible that non-Hispanic White participants who experienced perceived religious discrimination live in areas in which their religious affiliations are the minority. Research has found that Whites tend to report more experiences of discrimination when they perceive themselves as the minority (Craig & Richeson, 2018). Non-Hispanic Whites Veterans who reported discrimination based on education or income level may be of low-income which would subject them and their family members to a considerable amount of stress (Glass et al., 2020) which may lead to alcohol use. Furthermore, our findings that racial and ethnic minorities are more likely report perceived discrimination based on race and shade of skin color is vastly supported by previous research which has found racial discrimination to be a prominent feature in the lives of minority groups (Lee et al., 2019). Finally, there was a statistically significant difference between non-Hispanic White Veterans and racial/ethnic minority Veterans in subjective impact related to the SJARM, with racial/ethnic minorities reporting higher subjective impact. Recent research focused on the emotional and mental health impact following the George Floyd murder has found that collective trauma due to social and racially unjust events such as police killings negatively impacts mental health for Black Americans while White Americans experience a significantly lower impact (Eichstaedt et al., 2021). Similarly, previous research has demonstrated that individuals who have a strong identification to their racial/ethnic group, are sensitive to and concerned about racial discrimination tend to react more strongly to race-based harm that occurs to another member of their racial/ethnic group; these individuals are also more likely to have repetitive, worrisome thoughts about racist events that have happened to others which may increase negative psychological responses to specific incidents of vicarious racism (Mason et al., 2017). Racism-related vigilance and ruminative distress in response to witnessing vicarious racism are psychologically taxing coping responses (Chae et al., 2021), which in turn may have increased the subjective impact felt by the Veterans in this sample who identify as racial/ethnic minorities.
The acknowledgement and understanding of how the social determinants of health impact alcohol use among Veterans who hold marginalized identities is crucial, yet it is merely the first step in addressing these issues in clinical care. Screening tools to assess for single and multiple social risks in clinical settings such as substance use disorder clinics at the VA have been used (Hawkins et al., 2012). However, national recommendations for multidimensional screening of the social determinants of health are not available since there is scant evidence to lend support for such recommendations (Andermann, 2018). Despite this, it is crucial that frontline clinicians and health care workers inquire about potential social risks in an empathetic, patient-centered, and culturally sensitive manner (Andermann, 2016, Hawkins et al., 2012). Furthermore, given that the results from this study are broadly in line with a previous systematic review which has found a positive association between discrimination experiences and alcohol consumption, alcohol related problems, and alcohol use disorder (Gilbert & Zemore, 2016), incorporating screening tools and having systems in place within substance use clinics that require clinicians to inquire about discrimination history in a culturally sensitive manner is recommended. Moreover, considering the significant impact that discrimination can have on BIPOC and other minority identities, it is crucial for clinicians to conceptualize their patients in accordance with their ethnic and cultural heritage on an ongoing basis (Williams et al., 2018). Finally, taking into account that clinicians and researchers have been socialized within systems that perpetuate oppression, it is of the utmost importance that we practice anti-racism through ongoing training, reading, adopting culturally informed treatment approaches, and reexamining what does and does not work with patients who have alcohol related problems (Hagle et al., 2021, Homan et al., 2021, Matsuzaka and Knapp, 2020, Williams et al., 2019).
A commitment to health equity around the globe has become increasingly more important (Hausmann et al., 2013, Kondo et al., 2017). This study contributes to literature that seeks to understand social determinants of health among U.S. Veterans. Taken together, these data underscore the continual reality of the various structures of oppression—i.e., structural racism, health disparities, poverty, inequity—that are present in the United States. Veterans who hold minority identities and those who represent unique intersections of minority status—i.e., Veteran, BIPOC, gender and sexual minorities, (non)religious minorities—have been found to be at greater risk for AUD and poorer health outcomes (Carr et al., 2021, Chen et al., 2020, Fuehrlein et al., 2016, Jegede et al., 2022, Kondo et al., 2017). Additionally, this study investigated multiple discrimination categories and their relationship to unhealthy alcohol use, adding to the understanding of the many facets of discrimination that require further exploration (Gilbert & Zemore, 2016). However, our overall understanding of the many intersecting levels of discrimination on drinking on an individual and systemic level remain woefully underdeveloped and more research is necessary (Gilbert & Zemore, 2016). Finally, while substantial research has been conducted on the correlates and consequences of discrimination among minority groups, this study contributes to the little-known research about how different types of perceived discrimination impact hazardous drinking in non-Hispanic White Veterans.
4.1. Limitations and future directions
This study has several limitations. First, the cross-sectional nature of the research design limits our ability to make causal interpretations of the results. Although we were able to garner meaningful insights on the relationships that perceived discrimination and the murder of George Floyd have with alcohol-related problems, we did not measure changes over time. The acute, detrimental distress and impact felt soon after the murder of George Floyd observed in this study may have attenuated over time. Second, this study relied on self-report and complaints of distress, impact and alcohol symptoms were not objectively measured. Third, the study team developed two face-valid questions to measure the subjective impact and personal distress specifically related to the SJARM after the George Floyd murder. Although no other measures have been developed and tested to gather this specific information, the research team acknowledges the psychometric constraints associated with the questions developed for this study. Fourth, given that this study is based on secondary analyses of a larger outcome study that was initially developed to explore the characteristics, mental health symptoms, and substance use behaviors of U.S. Veterans following the emergence of the COVID-19 pandemic, COVID-19 was not accounted for in the analyses. Perhaps the biggest limitation is that despite the study’s large, nationally represented sample, most participants self-identified as non-Hispanic and White. Although this demographic is common among Veterans, this study had an underrepresentation of racial and ethnic minorities relative to national census data (U.S. Census Bureau, 2021). It is possible that the use of an online survey platform influenced the sample demographics since previous research has found that these methods tend to yield non-Hispanic White samples (Heen et al., 2014). Despite this limitation however, the current study elucidates specific cultural nuances between different racial groups, distinct types of perceived discrimination, and how types of perceived discrimination relate to unhealthy alcohol use and racially unjust events. Likewise, the findings of this study revealed the importance of providing accurate definitions of culturally sensitive terminology within measures that are utilized for research and clinical care. Furthermore, collecting data during the COVID-19 pandemic may have impacted the results of this study. During the start of the COVID-19 pandemic, studies identified drastic increases in alcohol consumption as a means for individuals to cope with its impact (Callinan et al., 2021, Grossman et al., 2020, Pollard et al., 2020). Given that alcohol consumption was already increasing, it is possible that participants in this study may have already been engaging in unhealthy drinking prior to the SJARM. In addition, given the voluntary and online nature of the study, results presented cannot be generalized to individuals who chose not to participate, do not have access to the internet, or are not familiar with online survey platforms. Finally, two variables in the study—personal distress and subjective impact felt by the SJARM—were measured by two separate, single-item questions that were developed by the study team and have not been standardized or validated. Nevertheless, this research is unique in focusing on how perceived discrimination is related to alcohol use after a racial socially unjust event.
Future studies that investigate the combined impact of COVID-19 and racial discrimination on unhealthy alcohol and other substance use among Veterans are warranted. Future research should aim to collect data that is more representative of the U.S. population as convenience samples greatly impacts study quality; this is particularly important for research that is focused on discrimination and other elements of the social determinants of health as hard-to-reach populations may remain hidden due to structural forms of discrimination. It is strongly recommended that future research refrain from non-probability sampling. Also, incorporating different methods of collecting data other than self-report would be beneficial in examining constructs such as perceived discrimination. Longitudinal data on the lasting impacts of racial socially unjust events on alcohol use would be useful for analyzing change in alcohol use over time. Moreover, future studies may consider including standardized discrimination scales which assess for multiple levels of discrimination, such as the EDS (Williams et al., 1997) to further our knowledge and understanding of the complex nuances of different discrimination categories and how they may impact alcohol use. The results of this study highlight the importance of addressing discrimination experiences in Veterans, particularly as rates of unhealthy alcohol use are on the rise.
Author agreement
All authors contributed to and approved the final manuscript.
Funding
This research was supported by the National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA) (T32DA007250 [MTC]). Support was also provided by the Office of Research and Development, Clinical Science Research and Development (CSR&D), Department of VA Clinical Science Research & Development (1IK2CX001510-01 [DLP]), National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA) (DA039903 [DLP]).
CRediT authorship contribution statement
Monique T. Cano: Conceptualization, Methodology, Formal analysis, Writing – original draft. Jill V. Reavis: Investigation, Writing – review & editing. David L. Pennington: Formal analysis, Writing – review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA) (T32DA007250). Office of Research and Development, Clinical Science Research and Development (CSR&D), Department of VA Clinical Science Research & Development (1IK2CX001510-01). National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA) (DA039903).
Data availability
The dataset is not publicly available, because it was created as part of Veteran’s Administration approved research. Requests to access should be directed to David Pennington, david.pennington2@va.gov.
References
- Aaron D.G., Stanford F.C. Medicine, structural racism, and systems. Social Science & Medicine. 2022;298 doi: 10.1016/j.socscimed.2022.114856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albright D.L., McDaniel J., Suntai Z., Wallace J. Alcohol misuse among older military veterans: An intersectionality theory perspective. Journal of Addictive Diseases. 2021;39(4):504–512. doi: 10.1080/10550887.2021.1897201. [DOI] [PubMed] [Google Scholar]
- Alpers S.E., Skogen J.C., Mæland S., Pallesen S., Rabben Å.K., Lunde L.-H., Fadnes L.T. Alcohol consumption during a pandemic lockdown period and change in alcohol consumption related to worries and pandemic measures. International Journal of Environmental Research and Public Health. 2021;18(3):1220. doi: 10.3390/ijerph18031220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association, & American Psychological Association. (2016). Stress in America: The impact of discrimination. Stress in America Survey, 2016.
- Andermann A. Taking action on the social determinants of health in clinical practice: A framework for health professionals. Cmaj. 2016;188(17–18):E474–E483. doi: 10.1503/cmaj.160177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andermann A. Screening for social determinants of health in clinical care: Moving from the margins to the mainstream. Public Health Reviews. 2018;39(1):1–17. doi: 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). Audit. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for Use in Primary Care.
- Barbosa C., Cowell A.J., Dowd W.N. Alcohol consumption in response to the COVID-19 pandemic in the United States. Journal of Addiction Medicine. 2021;15(4):341. doi: 10.1097/ADM.0000000000000767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker H.C. Influence of stress associated with chronic alcohol exposure on drinking. Neuropharmacology. 2017;122:115–126. doi: 10.1016/j.neuropharm.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J., Venkataramani A.S., Williams D.R., Tsai A.C. Police killings and their spillover effects on the mental health of black Americans: A population-based, quasi-experimental study. Lancet (London, England) 2018;392(10144):302–310. doi: 10.1016/S0140-6736(18)31130-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan A.E., Kim H.-J., Fredriksen-Goldsen K.I. Factors associated with high-risk alcohol consumption among LGB older adults: The roles of gender, social support, perceived stress, discrimination, and stigma. The Gerontologist. 2017;57(suppl_1):S95–S104. doi: 10.1093/geront/gnw100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan S., Mojica-Perez Y., Wright C.J.C., Livingston M., Kuntsche S., Laslett A.-M.…Kuntsche E. Purchasing, consumption, demographic and socioeconomic variables associated with shifts in alcohol consumption during the COVID-19 pandemic. Drug and Alcohol Review. 2021;40(2):183–191. doi: 10.1111/dar.13200. [DOI] [PubMed] [Google Scholar]
- Carlson M., Endlsey M., Motley D., Shawahin L.N., Williams M.T. Addressing the impact of racism on veterans of color: A race-based stress and trauma intervention. Psychology of Violence. 2018;8(6):748–762. doi: 10.1037/vio0000221. [DOI] [Google Scholar]
- Carr M.M., Potenza M.N., Serowik K.L., Pietrzak R.H. Race, ethnicity, and clinical features of alcohol use disorder among US military veterans: Results from the national health and resilience in veterans study. The American Journal on Addictions. 2021;30(1):26–33. doi: 10.1111/ajad.13067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho A.F., Heilig M., Perez A., Probst C., Rehm J. Alcohol use disorders. The Lancet. 2019;394(10200):781–792. doi: 10.1016/S0140-6736(19)31775-1. [DOI] [PubMed] [Google Scholar]
- Chae D.H., Yip T., Martz C.D., Chung K., Richeson J.A., Hajat A.…LaVeist T.A. Vicarious racism and vigilance during the COVID-19 pandemic: Mental health implications among Asian and Black Americans. Public Health Reports. 2021;136(4):508–517. doi: 10.1177/00333549211018675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.A., Glass J.E., Bensley K.M., Goldberg S.B., Lehavot K., Williams E.C. Racial/ethnic and gender differences in receipt of brief intervention among patients with unhealthy alcohol use in the US Veterans Health Administration. Journal of Substance Abuse Treatment. 2020;119 doi: 10.1016/j.jsat.2020.108078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig M.A., Richeson J.A. Majority no more? The influence of neighborhood racial diversity and salient national population changes on Whites’ perceptions of racial discrimination. RSF: The Russell Sage Foundation. Journal of the Social Sciences. 2018;4(5):141–157. [Google Scholar]
- Desalu J.M., Goodhines P.A., Park A. Racial discrimination and alcohol use and negative drinking consequences among Black Americans: A meta-analytical review. Addiction. 2019;114(6):957–967. doi: 10.1111/add.14578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio J.D. Academic Press; 1986. Prejudice, Discrimination, and Racism. [Google Scholar]
- Eichstaedt J.C., Sherman G.T., Giorgi S., Roberts S.O., Reynolds M.E., Ungar L.H., Guntuku S.C. The emotional and mental health impact of the murder of George Floyd on the US population. Proceedings of the National Academy of Sciences. 2021;118(39) doi: 10.1073/pnas.2109139118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Fuehrlein B.S., Mota N., Arias A.J., Trevisan L.A., Kachadourian L.K., Krystal J.H.…Pietrzak R.H. The burden of alcohol use disorders in US military veterans: Results from the National Health and Resilience in Veterans Study. Addiction. 2016;111(10):1786–1794. doi: 10.1111/add.13423. [DOI] [PubMed] [Google Scholar]
- Galea S., Vlahov D. Social determinants and the health of drug users: Socioeconomic status, homelessness, and incarceration. Public Health Reports. 2002;117(Suppl 1):S135. [PMC free article] [PubMed] [Google Scholar]
- Gilbert P.A., Zemore S.E. Discrimination and drinking: A systematic review of the evidence. Social Science & Medicine. 2016;161:178–194. doi: 10.1016/j.socscimed.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi, S., Guntuku, S. C., Rahman, M., Himelein-Wachowiak, M., Kwarteng, A., & Curtis, B. (2020). Twitter corpus of the# blacklivesmatter movement and counter protests: 2013 to 2020. ArXiv Preprint ArXiv:2009.00596.
- Glass J.E., Williams E.C., Oh H. Racial/ethnic discrimination and alcohol use disorder severity among United States adults. Drug and Alcohol Dependence. 2020;216 doi: 10.1016/j.drugalcdep.2020.108203. [DOI] [PubMed] [Google Scholar]
- Goldenberg A., Garcia D., Halperin E., Gross J.J. Collective emotions. Current Directions in Psychological Science. 2020;29(2):154–160. [Google Scholar]
- Grossman E.R., Benjamin-Neelon S.E., Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. International Journal of Environmental Research and Public Health. 2020;17(24) doi: 10.3390/ijerph17249189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagle H.N., Martin M., Winograd R., Merlin J., Finnell D.S., Bratberg J.P.…MacLane-Baeder D. Dismantling racism against black, indigenous, and people of color across the substance use continuum: A position statement of the association for multidisciplinary education and research in substance use and addiction. Substance Abuse. 2021;42(1):5–12. doi: 10.1080/08897077.2020.1867288. [DOI] [PubMed] [Google Scholar]
- Hausmann L.R.M., Kwoh C.K., Hannon M.J., Ibrahim S.A. Perceived Racial Discrimination in Health Care and Race Differences in Physician Trust. Race and Social Problems. 2013;5(2):113–120. doi: 10.1007/s12552-013-9092-z. [DOI] [Google Scholar]
- Hawkins E.J., Grossbard J., Benbow J., Nacev V., Kivlahan D.R. Evidence-based screening, diagnosis, and treatment of substance use disorders among veterans and military service personnel. Military Medicine. 2012;177(suppl_8):29–38. doi: 10.7205/milmed-d-12-00125. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford publications; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Heen, M.S.J., Lieberman, J. D., & Terance Miethe. (2014). A Comparison of Different Online Sampling Approaches for Generating National Samples. Doi: 10.13140/RG.2.2.24283.62243.
- Homan P., Brown T.H., King B. Structural intersectionality as a new direction for health disparities research. Journal of Health and Social Behavior. 2021;62(3):350–370. doi: 10.1177/00221465211032947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jegede O., Na P.J., Haeny A.M., Krystal J.H., Pietrzak R.H. Association of Distress Due to Systemic Racism and Racial Disparities With Psychopathology and Suicidal Ideation Among US Veterans During the COVID-19 Pandemic. The Journal of Clinical Psychiatry. 2022;83(5):42085. doi: 10.4088/JCP.22br14410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.L., Mor M.K., Cashy J.P., Gordon A.J., Haas G.L., Schaefer J.H., Hausmann L.R.M. Racial/Ethnic Differences in Primary Care Experiences in Patient-Centered Medical Homes among Veterans with Mental Health and Substance Use Disorders. Journal of General Internal Medicine. 2016;31(12):1435–1443. doi: 10.1007/s11606-016-3776-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalb N., Roy Gillis J., Goldstein A.L. Drinking to cope with sexual minority stressors: Understanding alcohol use and consequences among LGBQ emerging adults. Journal of Gay & Lesbian Mental Health. 2018;22(4):310–326. [Google Scholar]
- Keum B.T., Ángel Cano M. Online Racism, Depressive and Anxiety Symptoms, Coping-related Drinking Motives, and Alcohol Use Severity among Black, Latinx, and Asian Emerging Adults. Addictive Behaviors. 2022;107468 doi: 10.1016/j.addbeh.2022.107468. [DOI] [PubMed] [Google Scholar]
- Killgore W.D., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Alcohol dependence during COVID-19 lockdowns. Psychiatry Research. 2021;296 doi: 10.1016/j.psychres.2020.113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkinis K., Pieterse A.L., Martin C., Agiliga A., Brownell A. Racism, racial discrimination, and trauma: A systematic review of the social science literature. Ethnicity & Health. 2021;26(3):392–412. doi: 10.1080/13557858.2018.1514453. [DOI] [PubMed] [Google Scholar]
- Kondo, K., Low, A., Everson, T., Gordon, C. D., Veazie, S., Lozier, C. C., Freeman, M., Motu’apuaka, M., Mendelson, A., Friesen, M., Paynter, R., Friesen, C., Anderson, J., Boundy, E., Saha, S., Quiñones, A., & Kansagara, D. (2017). Health Disparities in Veterans: A Map of the Evidence. Medical Care, 55, S9. Doi: 10.1097/MLR.0000000000000756. [DOI] [PubMed]
- Krieger, N. (2020). ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change—and time for health justice, democratic governance, and an equitable, sustainable future. In American Journal of Public Health (Vol. 110, Issue 11, pp. 1620–1623). American Public Health Association. [DOI] [PMC free article] [PubMed]
- Lee R.T., Perez A.D., Boykin C.M., Mendoza-Denton R. On the prevalence of racial discrimination in the United States. PLOS ONE. 2019;14(1):e0210698. doi: 10.1371/journal.pone.0210698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston, N. A., Berke, D. S., Ruben, M. A., Link to external site, this link will open in a new window, Matza, A. R., & Shipherd, J. C. (2019). Experiences of trauma, discrimination, microaggressions, and minority stress among trauma-exposed LGBT veterans: Unexpected findings and unresolved service gaps. Psychological Trauma: Theory, Research, Practice, and Policy, 11(7), 695–703. http://dx.doi.org.ucsf.idm.oclc.org/10.1037/tra0000464. [DOI] [PubMed]
- Livingston N.A., Flentje A., Heck N.C., Szalda-Petree A., Cochran B.N. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. Journal of Consulting and Clinical Psychology. 2017;85(12):1131. doi: 10.1037/ccp0000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald S., Judge-Golden C., Borrero S., Zhao X., Mor M.K., Hausmann L.R.M. Experiences of Perceived Gender-based Discrimination Among Women Veterans: Data From the ECUUN Study. Medical Care. 2020;58(5):483–490. doi: 10.1097/MLR.0000000000001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey T.K., Strathdee S.A. Big Events and Risks to Global Substance Using Populations: Unique Threats and Common Challenges. Substance Use & Misuse. 2015;50(7):885–890. doi: 10.3109/10826084.2015.983008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean R.R., Sofuoglu M., Rosenheck R. Tobacco and alcohol use disorders: Evaluating multimorbidity. Addictive Behaviors. 2018;78:59–66. doi: 10.1016/j.addbeh.2017.11.006. [DOI] [PubMed] [Google Scholar]
- Mason T.B., Maduro R.S., Derlega V.J., Hacker D.S., Winstead B.A., Haywood J.E. Individual differences in the impact of vicarious racism: African American students react to the George Zimmerman trial. Cultural Diversity and Ethnic Minority Psychology. 2017;23(2):174. doi: 10.1037/cdp0000099. [DOI] [PubMed] [Google Scholar]
- Matsuzaka S., Knapp M. Anti-racism and substance use treatment: Addiction does not discriminate, but do we? Journal of Ethnicity in Substance Abuse. 2020;19(4):567–593. doi: 10.1080/15332640.2018.1548323. [DOI] [PubMed] [Google Scholar]
- Maxie-Moreman A.D., Tynes B.M. Exposure to online racial discrimination and traumatic events online in Black adolescents and emerging adults. Journal of Research on Adolescence. 2022;32(1):254–269. doi: 10.1111/jora.12732. [DOI] [PubMed] [Google Scholar]
- McGurk, D., Cotting, D. I., Britt, T. W., & Adler, A. B. (2006). Joining the Ranks: The Role of Indoctrination in Transforming Civilians to Service Members. In Military life: The psychology of serving in peace and combat: Operational stress, Vol. 2 (pp. 13–31). Praeger Security International.
- Melamed O.C., Hauck T.S., Buckley L., Selby P., Mulsant B.H. COVID-19 and persons with substance use disorders: Inequities and mitigation strategies. Substance Abuse. 2020;41(3):286–291. doi: 10.1080/08897077.2020.1784363. [DOI] [PubMed] [Google Scholar]
- Miller M.B., Monk J.K., Flores L.Y., Everson A.T., Martinez L.D., Massey K.…McCrae C.S. Impact of discrimination and coping on Veterans’ willingness to seek treatment for physical and mental health problems. Psychology of Addictive Behaviors. 2022 doi: 10.1037/adb0000861. [DOI] [PubMed] [Google Scholar]
- Moody M.D., Thomas Tobin C.S., Erving C.L. Vicarious Experiences of Major Discrimination and Psychological Distress among Black Men and Women. Society and Mental Health. 2022 doi: 10.1177/21568693221116631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Shield K.D. Global burden of alcohol use disorders and alcohol liver disease. Biomedicines. 2019;7(4):99. doi: 10.3390/biomedicines7040099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruben M.A., Livingston N.A., Berke D.S., Matza A.R., Shipherd J.C. Lesbian, Gay, Bisexual, and Transgender Veterans’ Experiences of Discrimination in Health Care and Their Relation to Health Outcomes: A Pilot Study Examining the Moderating Role of Provider Communication. Health Equity. 2019;3(1):480–488. doi: 10.1089/heq.2019.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Unhealthy alcohol use. New England Journal of Medicine. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Schmidt R.A., Genois R., Jin J., Vigo D., Rehm J., Rush B. The early impact of COVID-19 on the incidence, prevalence, and severity of alcohol use and other drugs: A systematic review. Drug and Alcohol Dependence. 2021;228 doi: 10.1016/j.drugalcdep.2021.109065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat S. Commentary on the special issue on disproportionate exposure to trauma: Trauma, stress, and adversities and health disparities among disenfranchised groups globally during the COVID pandemic. Journal of Traumatic Stress. 2021;34(5):1061–1067. doi: 10.1002/jts.22746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma V., Marin D.B., Koenig H.K., Feder A., Iacoviello B.M., Southwick S.M., Pietrzak R.H. Religion, spirituality, and mental health of US military veterans: Results from the National Health and Resilience in Veterans Study. Journal of Affective Disorders. 2017;217:197–204. doi: 10.1016/j.jad.2017.03.071. [DOI] [PubMed] [Google Scholar]
- Sohn L., Harada N.D. Effects of Racial/Ethnic Discrimination on the Health Status of Minority Veterans. Military Medicine. 2008;173(4):331–338. doi: 10.7205/MILMED.173.4.331. [DOI] [PubMed] [Google Scholar]
- Teeters J.B., Lancaster C.L., Brown D.G., Back S.E. Substance use disorders in military veterans: Prevalence and treatment challenges. Substance Abuse and Rehabilitation. 2017;8:69–77. doi: 10.2147/SAR.S116720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace S., Nazroo J., Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. American Journal of Public Health. 2016;106(7):1294–1300. doi: 10.2105/AJPH.2016.303121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weine S., Kohrt B.A., Collins P.Y., Cooper J., Lewis-Fernandez R., Okpaku S., Wainberg M.L. Justice for George Floyd and a reckoning for global mental health. Global Mental. Health. 2020;7 doi: 10.1017/gmh.2020.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Yu Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams E.C., Gupta S., Rubinsky A.D., Glass J.E., Jones-Webb R., Bensley K.M., Harris A.H. Variation in receipt of pharmacotherapy for alcohol use disorders across racial/ethnic groups: A national study in the US Veterans Health Administration. Drug and Alcohol Dependence. 2017;178:527–533. doi: 10.1016/j.drugalcdep.2017.06.011. [DOI] [PubMed] [Google Scholar]
- Williams E.C., Gupta S., Rubinsky A.D., Jones-Webb R., Bensley K.M., Young J.P.…Harris A.H. Racial/ethnic differences in the prevalence of clinically recognized alcohol use disorders among patients from the US Veterans Health Administration. Alcoholism: Clinical and Experimental Research. 2016;40(2):359–366. doi: 10.1111/acer.12950. [DOI] [PubMed] [Google Scholar]
- Williams M.T., Metzger I.W., Leins C., DeLapp C. Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Practice Innovations. 2018;3(4):242. [Google Scholar]
- U.S. Census Bureau. (2021). Race and Ethnicity in the United States: 2010 Census and 2020 Census. Retrieved October 29, 2021, from https://www.census.gov/library/visualizations/interactive/race-and-ethnicity-in-the-united-state-2010-and-2020-census.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset is not publicly available, because it was created as part of Veteran’s Administration approved research. Requests to access should be directed to David Pennington, david.pennington2@va.gov.