Abstract
Objectives
Determine whether Pre-Game Safety Huddles, a novel and low-resource approach to concussion education, increase the expected likelihood of concussion reporting for youth athletes.
Methods
A cluster-randomised trial compared Safety Huddles to usual care. Safety Huddles bring together athletes and coaches from both teams before the start of each game for coaches to briefly affirm the importance of speaking up if a concussion is suspected. Participants were athletes from 22 competitive community-based American football and girls and boys soccer teams (ages 9–14), and randomisation into intervention or control occurred at the level of the bracket (group of teams that compete against each other during the regular season). The primary outcome was expected likelihood of reporting concussion symptoms to the coach, measured via validated athlete survey at the beginning and end of the season.
Results
Of 343 eligible participants, 339 (99%) completed baseline surveys and 303 (88%) completed surveys at season end. The mean (SD) age was 11.4 (1.1) years, 26% were female soccer athletes, 27% were male soccer athletes and 47% were football athletes. In adjusted analyses accounting for baseline values and clustering by sport and team via random effects, expected likelihood of concussion reporting at the end of the season was significantly higher in the intervention group compared to controls (mean difference=0.49, 95% CI 0.11 to 0.88; Cohen’s d=0.35).
Conclusions and relevance
Pre-Game Safety Huddles increased the expected likelihood of athletes reporting concussion symptoms. While further study is warranted, sport organisations should consider this approach a promising low-resource option for improving concussion safety in their setting.
INTRODUCTION
More than 44 million American youth 6–17 years old participate in organised sports,1 and every year more than 1 million of these youth sustain a concussion.2 Immediate removal from play following injury limits the potential for additional brain trauma during a window of cerebral vulnerability,3 diminishing risk of undiagnosed catastrophic injury and allowing for earlier evaluation and care, both of which are associated with earlier return to full activity.4 5 Problematically, estimates suggest more than half of athletes who experience concussion symptoms continue playing, and either never receive medical attention or receive delayed care.6 Consequently, nearly all organisations that administer contact and collision sport in the USA, at levels ranging from youth to college, require some form of concussion education for athletes aimed at encouraging symptom self-report. 7
Building on a growing body of research about the central role interpersonal interactions and team norms play in concussion-reporting behaviour,8–11 recent consensus guidance from the National Collegiate Athletic Association and US Department of Defense Mind Matters initiative reinforces the importance of implementing educational approaches that foster within-team communication about concussion safety.12 This consensus guidance also states that such messaging should be repeated at multiple points during the season,12 given issues with retention of concussion education messaging,13 and the importance of message salience to behaviour.14 Pre-Game Safety Huddles (hereafter abbreviated as ‘Safety Huddles’) are a novel approach to concussion education consistent with this guidance.12 The theoretical and historical underpinnings of using Safety Huddles as a strategy for concussion education15 and the stakeholder-engaged development process have been described elsewhere.16 Core components of Safety Huddles as a strategy to increase concussion reporting include: (1) bringing athletes and coaches from both teams together before the start of each game, and (2) having one or more team leaders (typically coaches) affirm safety-related messaging. Example messaging is provided in figure 1. Encouraging coach adaptation to make the messaging authentic, Safety Huddles provide a formalised opportunity for establishing norms supportive of concussion-reporting and other valued behaviours such as fair play, and provide a mechanism for reinforcing this messaging throughout the season in the setting most salient to reporting behaviour.
Figure 1.
Pre-Game Safety Huddle information card. Intervention core components are gathering before every game, and addressing the importance of concussion safety. Using this card is optional. It is designed to provide coaches with content to selectively emphasise or adapt when they lead huddles. CTRL, control; INT, intervention.
Safety Huddles are theoretically well positioned to increase secondary prevention of concussion, ensuring that athletes are removed from play following concussive injury and thus preventing concerning sequelae. In addition, bringing athletes from both teams together in a collaborative rather than adversarial context could serve to humanise opponents, particularly if coaches include messaging regarding sportsmanship/fair play. Thus, it is also possible that Safety Huddles could lead to primary prevention of concussion if they decreased the likelihood of athletes engaging in injurious play. This study tested the hypothesis that youth soccer and football athletes on teams assigned to complete Safety Huddles across their competitive season would have higher end- of- season scores on a measure of expected likelihood of reporting concussion symptoms to their coach compared with athletes on teams in the control condition. Whether exposure to Safety Huddles was associated with decreased likelihood of engaging in potentially injurious play was included as a secondary, and exploratory, outcome.
METHODS
Sample and procedure
Intervention
In a sample of male and female youth soccer and football athletes (aged 9–14), we conducted a cluster-randomised trial of Safety Huddles compared with usual care (league-administered standard concussion education). As described above and in detail elsewhere,16 Safety Huddles are a season-long intervention in which opposing teams gather together before each game for brief (<2 min) coach- led messaging encouraging care seeking for a suspected concussion. Standard concussion education was a league-administered informational sheet for parents and youth to review17; all study participants received standard education prior to the start of their competitive season, and athletes on teams randomised to the intervention condition also received Safety Huddles across their competitive season. Research activities were approved by Seattle Children’s Hospital Institutional Review Board. The study was listed in ClinicalTrials.gov (NCT04099329). Data were collected between August and November 2019.
Patient and public involvement
The Safety Huddle concept was developed collaboratively with two Seattle-area football league administrators, and was refined with input from soccer and football athletes, coaches, officials and administrators in the greater Seattle and rural south Georgia regions. Detail on this collaborative process has been described separately.16 A subset of these stakeholders provided input on study procedures (recruitment, data collection), including how study-related information was communicated to their respective communities.
Sample and randomisation
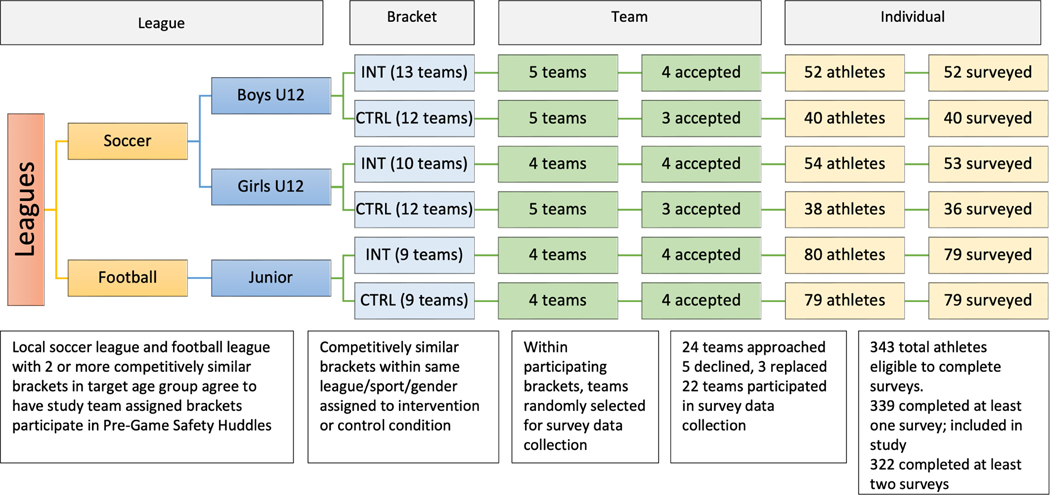
Given that Safety Huddles engage opposing teams across multiple games, randomisation occurred at the level of the ‘bracket’, defined as a group of teams competing against each other in a given league during the regular season. The sampling frame for this study was a youth American football league and a youth soccer league located in the Pacific Northwest region of the USA. Leagues create their own brackets to organise regular season play, and working with the league administrators we identified two competitively similar brackets of 10–13 years old in each sport (football, girls soccer and boys soccer). Competitive similarity was determined by the division or level of competition assigned to the bracket, and within each pair one bracket was randomly assigned to complete Safety Huddles across the regular season and the other to serve as a control. The study team implemented the randomisation process, which was conducted with a 1:1 allocation using a random number generator. Girls and boys soccer each had four eligible brackets, with the number of teams per bracket ranging from 8 to 13, and football had two eligible and competitively matched brackets, with nine teams per bracket (figure 2). All teams in the brackets randomly assigned to the intervention were asked to complete Safety Huddles as a league- endorsed activity. The study team was not blinded to each team’s condition given the nature of the intervention and study team involvement in supporting implementation and data collection.
Figure 2.
Overview of recruitment and participation.
Data collection procedure
Within each bracket (intervention and control) four teams were randomly selected (using a random number generator) to participate in survey data collection. The time-intensive nature of data collection (in-person in order to achieve strong response rates) necessitated limiting the number of teams surveyed in each bracket. Two teams opted out-of-survey data collection at a point in the season that did not allow for replacement, resulting in 22 teams completing surveys. A total of 343 athletes were eligible to complete surveys, exceeding our minimal target sample size of 300 that would allow >80% power to detect a small change in our primary outcome. Parents of athletes on teams eligible for survey data collection received an information sheet about the study, and athletes provided verbal assent prior to participating in survey data collection. Baseline survey data collection occurred before the start of the competitive season, prior to Safety Huddles being initiated but after brackets had been randomised to intervention or control conditions. Soccer teams completed three surveys: baseline, 5 weeks and 10 weeks (the end of their regular competitive season). Because the football season was substantially shorter, football players only completed two surveys: baseline and at 6 weeks (the end of their regular competitive season). At each time point, surveys were administered to athletes in person (ie, after a practice). If an athlete was not present, an online survey hosted on the REDCap platform was subsequently emailed or texted to them. Participation was voluntary and uncompensated; however, snacks and beverages were provided for athletes and coaches.
Implementation procedure
Coach training
Coaches on teams randomised to the intervention condition completed training about leading Safety Huddles. This included all coaches on teams randomised to the intervention condition (ie, irrespective of whether they were subsequently also randomly selected to participate in survey data collection). Training occurred with a study team member present in person or remotely to ensure completion. Additional detail on the development and content of huddle training is described elsewhere.16 The training included content about concussion and how to lead a huddle. with brief videos of coaches modelling different versions of huddles that address core huddle components. Training was completed by more than 90% of coaches (boys soccer 12/13 teams; girls soccer 8/10 teams; football 9/9 teams). Coaches also received a laminated Safety Huddle card with key points they could emphasise during huddles (figure 2).
Reminders
Two hours before games in which Safety Huddles were scheduled to occur, coaches received a text reminder and a link to a mobile-accessible huddle card summarising core huddle components.
Measures
Expected concussion-reporting behaviour
Our primary outcome was the athlete’s expected likelihood of reporting potential concussion symptoms to a coach, measured using the four-item expected concussion-reporting behaviour (CR-E) scale. Measure development occurred in youth athletes (aged 9–16), with evidence of high internal consistency reliability and validity in this age group.18 An example item was ‘If I felt dizzy after a bump of hit to the head, I would tell my coach right away, even if the team was counting on me to play’. Responses to each item were on a 5- point scale (0=never, 1=rarely, 2=sometimes, 3=often, 4=always), and the scale score is reported as an item-level average with a possible range of 0–4, with higher scores representing greater expected likelihood of reporting. Scores were set to missing if the participant was missing more than half of responses. In the present sample, internal consistency reliability was high (Cronbach’s alpha=0.95).
Concussion-reporting behaviour
At baseline and the end of the season, athletes were provided with an age- appropriate definition of concussion and a list of possible concussion symptoms (Flesch-Kincaid Grade Level=4.1, indicating a fourth grade reading level for the text). They were then asked to think about their most recent sports season and indicate whether they had experienced a blow to the head followed by any of these symptoms.19 If they answered yes, they were subsequently asked whether they told anyone about how they were feeling. Response options were yes, no, and I didn’t tell anyone because they already knew (I passed out or it was clear I wasn’t feeling well). Responses were dichotomised as yes or they already knew (1), and no (0).
Expected injurious play
As an exploratory outcome, we assessed whether exposure to Safety Huddles was associated with decreased expected likelihood of engaging in potentially injurious play. Participants were provided with the following prompt: ‘Imagine you are playing a game and you are in the heat of the moment. Sometimes in these situations we act before thinking. In the heat of the moment, how likely would you be to …’ and asked to respond to the following two items: make a play to stop an opponent that has a high chance of causing the opponent a head injury; and make a play to stop an opponent that has a small chance of causing the opponent a head injury. Response options were on a 5-point scale, ranging from not at all likely to very likely, and subsequently dichotomised into categories of ‘likely’ (responses of very likely or somewhat likely) and ‘not likely’ (responses of not at all likely, not very likely or a little bit likely). Items were developed through a process that included formative and cognitive interviews with youth athletes, with the goal of wording questions in way that minimised social desirability bias in responses and maximised response variability.
Previously diagnosed concussions
At baseline, athletes were asked how many times a doctor had ever diagnosed them with a concussion.
Demographic characteristics
At baseline, athletes reported their age, whether they spoke a language other than English at home (yes, no) and race and ethnicity using US Census categories. Coaches reported their gender, age, years coaching, race and ethnicity and highest level of formal education obtained.
Fidelity of implementation
One hour after each game, coaches received a brief text survey asking whether or not they completed a Safety Huddle. Coaches who did not respond were sent follow-up texts the following day and 3–4 days later. If a coach did not complete a scheduled Safety Huddle, a research team member helped troubleshoot via text messaging. Coaches completed a brief postgame phone- based survey about the content of their most recently completed Safety Huddle at two points in the season for football (weeks 3 and 6) and three points for soccer (weeks 3, 6 and 10). Questions addressed whether the recently completed Safety Huddle included core components (both teams together and messaging about concussion reporting).
Analysis
Athlete and coach descriptive characteristics were summarised overall and by study arm, using frequencies and percentages for categorical variables. We quantified missingness in the data and compared baseline characteristics across athletes with and without missing survey data. Differences by study arm were assessed using Pearson’s χ2 tests. Mixed-effects linear regression models were used to estimate the difference in CR-E score between intervention and control groups at the season-end time point. Exploratory analyses by sport, gender and age were also conducted using a separate model for each subgroup. All analyses were based on intent to treat and were adjusted for factors identified a priori or which appeared to vary between groups at baseline, including coach gender and age, athlete gender, athlete age and baseline score. Nested clustering by sport and team is accounted for via random effects (except when analyses were instead stratified by the corresponding variable).
Generalised linear models with a log link and robust variance estimator were used to estimate RRs and 95% CIs of the expected likelihood of engaging in a risky behaviour in the intervention group relative to the control group at each follow-up comparison point. Clustering by team was accounted for using a modified sandwich robust variance estimator for cluster-correlated data. All models were adjusted for baseline response, coach gender and age, athlete gender and athlete age (except in cases where analyses were stratified by the corresponding variable). Exploratory models were stratified by sport and gender group.
Intervention effect on behaviour was explored among the subset of athletes who reported a blow to the head (n=60) using a similar analytical approach as described above for likelihood of engaging in risky behaviour. Analyses were adjusted for only age and gender due to the smaller sample size. We note that the study was not powered to assess change in concussion reporting behavior, and these were post hoc exploratory analyses.
As the soccer season was significantly longer than the football season and involved an additional data collection point, we completed additional analysis of the soccer data to assess potential differential change from baseline to 5 and 10 weeks. All analyses were conducted using Stata V.14.2 (StataCorp, College Station, Texas). All hypothesis tests were two sided with an a priori significance level of α=0.05.
RESULTS
Randomisation and sample characteristics
Demographic characteristics and concussion history for athletes and coaches are reported in tables 1 and 2, separately by intervention and control condition. Of the 343 eligible athletes, 339 (99%) completed baseline surveys and 303 (88%) completed surveys at season end (Figure 2). There were no statistically significant differences in baseline characteristics between athletes who missed a survey and those who did not. Across all time points and teams, 3% of responses were completed remotely.
Table 1.
Baseline characteristics of youth athletes participating in competitive youth leagues in western Washington state during the fall 2019 season
| All n=339 | Intervention group n=184 | Control group n=155 | |
|---|---|---|---|
| Player age (%) | |||
| 9–10 years | 55 (16.2) | 26 (14.1) | 29 (18.7) |
| 11–12 years | 167 (49.3) | 98 (53.3) | 69 (44.5) |
| 13–14 years | 53 (15.6) | 22 (12.0) | 31 (20.0) |
| Missing | 64 (18.9) | 38 (20.7) | 26 (16.8) |
| Child race (%) | |||
| White | 158 (46.6) | 90 (48.9) | 68 (43.9) |
| Black | 16 (4.7) | 8 (4.3) | 8 (5.2) |
| Asian | 24 (7.1) | 10 (5.4) | 14 (9.0) |
| American Indian or Alaska Native | 1 (0.3) | 1 (0.5) | 0 (0.0) |
| Native Hawaiian/Pacific Islander | 3 (0.9) | 2 (1.1) | 1 (0.6) |
| Other | 23 (6.8) | 12 (6.5) | 11 (7.1) |
| Multiple races specified | 33 (9.7) | 18 (9.8) | 15 (9.7) |
| Missing | 81 (23.9) | 43 (23.4) | 38 (24.5) |
| Hispanic ethnicity (%) | |||
| No | 172 (50.7) | 91 (49.5) | 81 (52.3) |
| Yes | 33 (9.7) | 19 (10.3) | 14 (9.0) |
| Missing | 134 (39.5) | 74 (40.2) | 60 (38.7) |
| Do you speak a language other than English at home? (%) | |||
| No | 196 (57.8) | 101 (54.9) | 95 (61.3) |
| Yes | 52 (15.3) | 29 (15.8) | 23 (14.8) |
| Missing | 91 (26.8) | 54 (29.3) | 37 (23.9) |
| Sport/gender (%) | |||
| Soccer/boys | 92 (27.1) | 52 (28.3) | 40 (25.8) |
| Soccer/girls | 89 (26.3) | 53 (28.8) | 36 (23.2) |
| Football/boys | 158 (46.6) | 79 (42.9) | 79 (51.0) |
| Gender (%) | |||
| Female | 89 (26.3) | 53 (28.8) | 36 (23.2) |
| Male | 250 (73.7) | 131 (71.2) | 119 (76.8) |
| Sport (%) | |||
| Football | 158 (46.6) | 79 (42.9) | 79 (51.0) |
| Soccer | 181 (53.4) | 105 (57.1) | 76 (49.0) |
| Number of times diagnosed with concussion by a doctor prior to current season (%) | |||
| 0 | 208 (61.4) | 114 (62.0) | 94 (60.6) |
| 1 | 45 (13.3) | 20 (10.9) | 25 (16.1) |
| 2 | 7 (2.1) | 4 (2.2) | 3 (1.9) |
| 3 | 1 (0.3) | 1 (0.5) | 0 (0.0) |
| 5 | 1 (0.3) | 1 (0.5) | 0 (0.0) |
| Missing | 77 (22.7) | 44 (23.9) | 33 (21.3) |
Table 2.
Characteristics of coaches overseeing youth athletes participating in competitive youth leagues in western Washington state during the fall 2019 season
| Overall n=22 | Intervention group n=12 | Control group n=10 | |
|---|---|---|---|
| Gender (%) | |||
| Male | 17 (77.3) | 10 (83.3) | 7 (70.0) |
| Female | 4 (18.2) | 2 (16.7) | 2 (20.0) |
| Missing | 1 (4.5) | 0 (0.0) | 1 (10.0) |
| Age (years), mean (SD) | 40.5 (9.5) | 37.3 (9.2) | 44.4 (8.9) |
| Years coaching (%) | |||
| 2–5 | 9(40.9) | 6 (50.0) | 3 (30.0) |
| 6–10 | 6 (27.3) | 3 (25.0) | 3 (30.0) |
| >10 | 6 (27.3) | 3 (25.0) | 3 (30.0) |
| Missing | 1 (4.5) | 0 (0.0) | 1 (10.0) |
| Race (%) | |||
| White | 18 (81.8) | 9 (75.0) | 9 (90.0) |
| Black | 3 (13.6) | 3 (25.0) | 0 (0.0) |
| Missing | 1 (4.5) | 0 (0.0) | 1 (10.0) |
| Hispanic ethnicity (%) | |||
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| No | 21 (95.5) | 12 (100.0) | 9 (90.0) |
| Missing | 1 (4.5) | 0 (0.0) | 1 (10.0) |
| Education (%) | |||
| Some college but no degree | 1 (4.5) | 0 (0.0) | 1 (10.0) |
| Associate degree | 2 (9.1) | 1 (8.3) | 1 (10.0) |
| Bachelor’s degree | 14 (63.6) | 9 (75.0) | 5 (50.0) |
| Master’s degree | 2 (9.1) | 1 (8.3) | 1 (10.0) |
| Professional degree (JD, MD) | 2 (9.1) | 1 (8.3) | 1 (10.0) |
| Missing | 1 (4.5) | 0 (0.0) | 1 (10.0) |
Implementation fidelity
From the 120 scheduled Safety Huddles in soccer, 99 (83%) occurred as planned, and from the 72 scheduled Safety Huddles in football, 54 (75%) occurred as planned, for an overall average of 80% across the study. Safety Huddles included opposing teams together 72% of the time, and messaging about concussion reporting and sportsmanship occurred 100% and 93% of the time, respectively.
Expected concussion-reporting behaviour
Adjusted CR- E scores at end of season are reported for intervention and control conditions, as well as the difference between the two groups (table 3). After adjusting for possible confounders (coach gender and age, athlete gender and age), baseline score and accounting for nested clustering by sport and team via random effects, CR- E score at the end of the season was significantly higher (by 0.49 points) in the intervention group compared with the control group (95% CI 0.11 to 0.88; table 3). Among athletes in the intervention condition, at the end of the season 33% responded they would ‘always’ tell a coach about concussion symptoms (CR- E score of 4), compared with 24% of athletes in the control condition. We also conducted exploratory subgroup analyses by sport. The adjusted difference in CR-E score between intervention and control groups at the end of the season was significant for soccer players (0.56 points, 95% CI 0.05 to 1.07), but did not reach significance for football players (0.38 points, 95% CI −0.43 to 1.19; table 3). Secondary analyses of results at the mid-season time point, limited to soccer athletes due to the longer season, were similar to those seen among soccer players at the end of the season (adjusted difference between arms=0.48 mid-season, 95% CI 0.07 to 0.88 vs 0.49 at end, 95% CI 0.11 to 0.88; not shown). Item-level responses by group are provided as online supplemental table 1.
Table 3.
Adjusted CR-E scores and differences between study arms at end of season, overall and for key subgroups of interest
| Mean CR-E score (95% CI) | |||
|---|---|---|---|
|
|
|||
| Intervention | Control | Difference (95% CI) | |
|
| |||
| Overall study population | 3.00 (2.77 to 3.24) | 2.51 (2.26 to 2.76) | 0.49 (0.11 to 0.88) |
| By sport | |||
| Soccer | 3.13 (2.85 to 3.40) | 2.57 (2.19 to 2.95) | 0.56 (0.05 to 1.07) |
| Football (which is male only) | 2.83 (2.31 to 3.35) | 2.45 (2.05 to 2.85) | 0.38 (−0.43 to 1.19) |
| By gender | |||
| Female (which is soccer only) | 3.00 (2.62 to 3.37) | 2.55 (2.08 to 3.01) | 0.45 (−0.21 to 1.11) |
| Male | 3.08 (2.74 to 3.41) | 2.43 (2.1 to 2.76) | 0.64 (0.08 to 1.21) |
| By age | |||
| 9–10 years (which is soccer only) | 3.26 (2.77 to 3.75) | 2.14 (1.62 to 2.66) | 1.12 (0.32 to 1.92) |
| 11–12 years | 2.99 (2.72 to 3.27) | 2.60 (2.27 to 2.93) | 0.39 (−0.08 to 0.87) |
| 13–14 years (which is football only) | 2.67 (1.95 to 3.39) | 2.63 (2.07 to 3.18) | 0.04 (−0.87 to 0.95) |
Adjusted for youth age, team gender, baseline response and coach gender. Bolded differences are statistically significant (p<0.05).
CR-E, expected concussion-reporting behaviour.
Concussion-reporting behaviour
A relatively small number of athletes reported experiencing a blow to the head during the season in which the study occurred (n=32 intervention, n=28 control), and our analysis of actual concussion reporting behavior was thus limited to this smaller sample. Differences in concussion reporting behavior between the two groups were not significant but were in the hypothesised direction (online supplemental table 2).
Expected injurious play
Expected likelihood of engaging in behaviours associated with either low or high risk of injury was not significantly different between study arms at season end; RR=0.9 (95% CI 0.6 to 1.4) for high-risk behaviour and RR=1.2 (95% CI 0.8 to 1.7) for low-risk behaviour. This was also true for sport as well as gender subgroups (online supplemental table 3).
DISCUSSION
Compared with athletes in the control condition, athletes who participated in Safety Huddles had a statistically significant and moderate-sized improvement in our primary outcome of expected likelihood of reporting concussion symptoms. Contextualising these findings relative to other concussion education programmes is challenging because of the low quality of extant evaluations; few educational interventions have been evaluated in terms of their impact on reporting behaviour or intended or expected behaviour, or have included a meaningful follow-up duration. 20 21 Two studies in collegiate athletes observed a smaller effect size for change in reporting intentions at 1-month22 and 1-year follow-up.23 However, we note that both of these comparator studies used measures of concussion-reporting intentions that have limited data regarding validity and reliability. As recommended in recent consensus guidance about concussion education, programmes should be evaluated using common data elements, or at the very least measures with evidence of reliability and validity.12 Such efforts are necessary if the comparative effectiveness of different approaches to concussion education is to be appraised.
Notable strengths of the Safety Huddle intervention are its flexibility/adaptablity and low resource nature. These are particularly important considerations given emergent findings that concussion education and other interventions aimed at supporting concussion reporting are less likely to be adopted and implemented in low- resource communities.24 25 While several steps away from broad diffusion, we designed Safety Huddles with the goal that they might someday become a normative and seamless element of youth sports competitions, similar to a postgame cheer and handshake. In many sport settings Safety Huddles already occur, but are focused on other issues such as the use of shin guards or other protective gear. The present study focused only on concussion reporting, but if Safety Huddles were to become a normative element of youth sport, they would provide an opportunity for communication about other setting- relevant sport safety messaging. Benefits notwithstanding, further research is needed to explore whether there are unintended consequences of repeated safety messaging over the course of a competitive season in terms of affective participant experiences (eg, fear) and related behaviour.
Limitations
Safety Huddles were developed in partnership with competitive youth soccer and football coaches and athletes. Further work is needed to determine whether they are feasible and acceptable in other sports, or at other ages or levels of competition. Our primary outcome was expected likelihood of reporting a concussion, and we were not powered to detect statistically significant differences in concussion reporting behavior. While expected concussion reporting is a theoretically indicated measure for evaluating concussion education interventions,18 there is nonetheless a need for a follow- up trial in a sample that is large enough to detect change in reporting behaviour. Larger sample sizes would also allow for adequately powered assessments of subgroup differences at both the individual level and the bracket level, such as the bracket’s level of competitiveness. Measures were assessed via self-report, which may be subject to social desirability bias, potentially limiting variability in outcome measures and bias findings towards the null. Teams that declined participation may have been different from those that participated in ways that limit the generalisability of the results; such differences would likely be at the coach level, since coaches functioned as the gatekeeper for team participation.
CONCLUSION
Safety Huddles are a flexible and low-resource approach to concussion education that appear to increase the likelihood of youth athletes reporting concussive symptoms. Study results substantiate the appropriateness of a large-scale effectiveness trial to determine whether Safety Huddles lead to meaningful changes in clinical outcomes, such as proportion of athletes appropriately removed from play for medical evaluation.
Supplementary Material
WHAT IS ALREADY KNOWN ON THIS TOPIC
⇒ Immediate removal from play for medical evaluation is a key way to limit harm after a concussion has occurred. Because many symptoms of concussion are not externally visible, removal from play often requires athletes to self-report their injury.
WHAT THIS STUDY ADDS
⇒ Pre-Game Safety Huddles are brief in-person messages about the importance of reporting symptoms of a suspected concussion, shared by coaches prior to the start of every game.
⇒ Youth soccer and American football athletes on teams that held Pre- Game Safety Huddles had expected likelihood of concussion reporting at the end of their competitive season that was higher than athletes on control teams.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
⇒ Pre-Game Safety Huddles are a low-resource and feasibly implemented approach to concussion education. Further research is needed to assess effectiveness in different sports, settings, ages and levels of competition.
Acknowledgements
We thank the football and soccer athletes, coaches and administrators who participated in this study for their time and engagement.
Funding
This study was supported by the CDC of the US Department of Health and Human Services (HHS) through cooperative funding agreement (U01CE002880).
Footnotes
Disclaimer The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, CDC/HHS or the US Government.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication Not applicable.
Ethics approval This study involves human participants and was approved by Seattle Children’s Hospital (ID: STUDY00000972). Participants gave informed consent to participate in the study before taking part.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer- reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Additional supplemental material is published online only. To view, please visit the journal online (http://dx.doi.org/10.1136/ip-2022-044665)
Trial registration number NCT04099329.
Data availability statement
Data are available upon reasonable request. Deidentified data are available upon reasonable request.
REFERENCES
- 1.Langhorst P. Youth sports participation statistics and trends, 2016. Available: http://www.engagesports.com/blog/post/1488/youth-sports-participation-statistics-and-trends [Accessed 4 August 2017].
- 2.Bryan MA, Rowhani-Rahbar A, Comstock RD, et al. Seattle sports concussion research collaborative. Sports- and Recreation-Related concussions in US youth. Pediatrics 2016;138. [DOI] [PubMed] [Google Scholar]
- 3.Greco T, Ferguson L, Giza C, et al. Mechanisms underlying vulnerabilities after repeat mild traumatic brain injuries. Exp Neurol 2019;317:206–13. [DOI] [PubMed] [Google Scholar]
- 4.Asken BM, Bauer RM, Guskiewicz KM, et al. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate Student-Athletes. Am J Sports Med 2018;46:1465–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elbin RJ, Sufrinko A, Schatz P, et al. Removal from play after concussion and recovery time. Pediatrics 2016;138:e20160910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Craig DI, Lininger MR, Vomacka MM, et al. Concussion reporting behaviors of athletes: a systematic review. Athletic Training & Sports Health Care 2020;12:81–8. [Google Scholar]
- 7.Perlin A, Kroshus E. Content analysis of concussion education for coaches of youth and high school sport. Brain Inj 2020;34:905–13. [DOI] [PubMed] [Google Scholar]
- 8.Kroshus E, Kubzansky LD, Goldman RE, et al. Norms, athletic identity, and concussion symptom under-reporting among male collegiate ice hockey players: a prospective cohort study. ann. behav. med 2015;49:95–103. [DOI] [PubMed] [Google Scholar]
- 9.Kroshus E, Garnett BR, Baugh CM, et al. Social norms theory and concussion education. Health Educ Res 2015;30:cyv047–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kroshus E, Baugh CM, Stein CJ, et al. Concussion reporting, sex, and conformity to traditional gender norms in young adults. J Adolesc 2017;54:110–9. [DOI] [PubMed] [Google Scholar]
- 11.Register-Mihalik JK, Linnan LA, Marshall SW, et al. Using theory to understand high school aged athletes’ intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj 2013;27:878–86. [DOI] [PubMed] [Google Scholar]
- 12.Kroshus E, Cameron KL, Coatsworth JD. Improving concussion education: consensus from the NCAA-Department of Defense Mind Matters Research & Education Grand Challenge. Br J Sports Med 2020:bjsports-2020–102185. [DOI] [PubMed] [Google Scholar]
- 13.Kroshus E, Daneshvar DH, Baugh CM, et al. NCAA concussion education in ice hockey: an ineffective mandate. Br J Sports Med 2014;48:135–40. [DOI] [PubMed] [Google Scholar]
- 14.Glanz K, Rimer BK, Viswanath K. Health Behavior: Theory, Research, and Practice. John Wiley & Sons, 2015. [Google Scholar]
- 15.Kroshus E, Chrisman SPD. A new game plan for concussion education. Health Educ Behav 2019;46:916–21. [DOI] [PubMed] [Google Scholar]
- 16.Kroshus E, Chrisman SPD, Hunt T, et al. Stakeholder-engaged development of a theory-driven, feasible, and acceptable approach to concussion education. Health Education & Behavior:109019812210998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Washington Youth Soccer. Concussion & Sudden Cardiac Arrest Awareness. Available: https://washingtonyouthsoccer.org/resources/concussion-sudden-cardiac-arrest-awareness/ [Accessed 13 May 2022].
- 18.Kroshus E, Lowry SJ, Garrett K, et al. Development of a scale to measure expected concussion reporting behavior. Injury Epidemiology 2021;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robbins CA, Daneshvar DH, Picano JD, et al. Self- Reported concussion history: impact of providing a definition of concussion. Open Access J Sports Med 2014;5:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caron JG, Bloom GA, Falcão WR, et al. An examination of concussion education programmes: a scoping review methodology. Inj Prev 2015;21:301–8. [DOI] [PubMed] [Google Scholar]
- 21.Feiss R, Lutz M, Reiche E, et al. A systematic review of the effectiveness of concussion education programs for coaches and parents of youth athletes. Int J Environ Res Public Health 2020;17:2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kneavel ME, Ernst W, McCarthy KS. Randomized controlled trial of a novel peer Concussion-Education program for collegiate athletes. J Athl Train 2020;55:456–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt JD, Weber ML, Suggs DW, et al. Improving concussion reporting across national College athletic association divisions using a Theory-Based, data-driven, multimedia concussion education intervention. J Neurotrauma 2020;37:593–9. [DOI] [PubMed] [Google Scholar]
- 24.Kroshus E, Rivara FP, Whitlock KB, et al. Disparities in athletic trainer staffing in secondary school sport: implications for concussion identification. Clin J Sport Med 2017;27:542–7. [DOI] [PubMed] [Google Scholar]
- 25.Kroshus E, Kerr ZY, Lee JGL Community-Level inequalities in concussion education of youth football coaches. Am J Prev Med 2017;52:476–82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. Deidentified data are available upon reasonable request.