Abstract
Objective:
Examine associations between perceived neighborhood walkability, physical activity (PA), and obesity among U.S. adults.
Methods:
Data from the 2020 National Health Interview Survey were analyzed. Walkability was assessed using a summative scale and categorized as low, medium, or high. PA was categorized as insufficient (0–149 minutes/week) or sufficient (150+ minutes/week). Multivariable regressions estimated association between obesity/BMI and PA and walkability. Mediation analysis was used to partition contribution of PA as mediator. Effect modification by race/ethnicity in the association between walkability and BMI was explored.
Results:
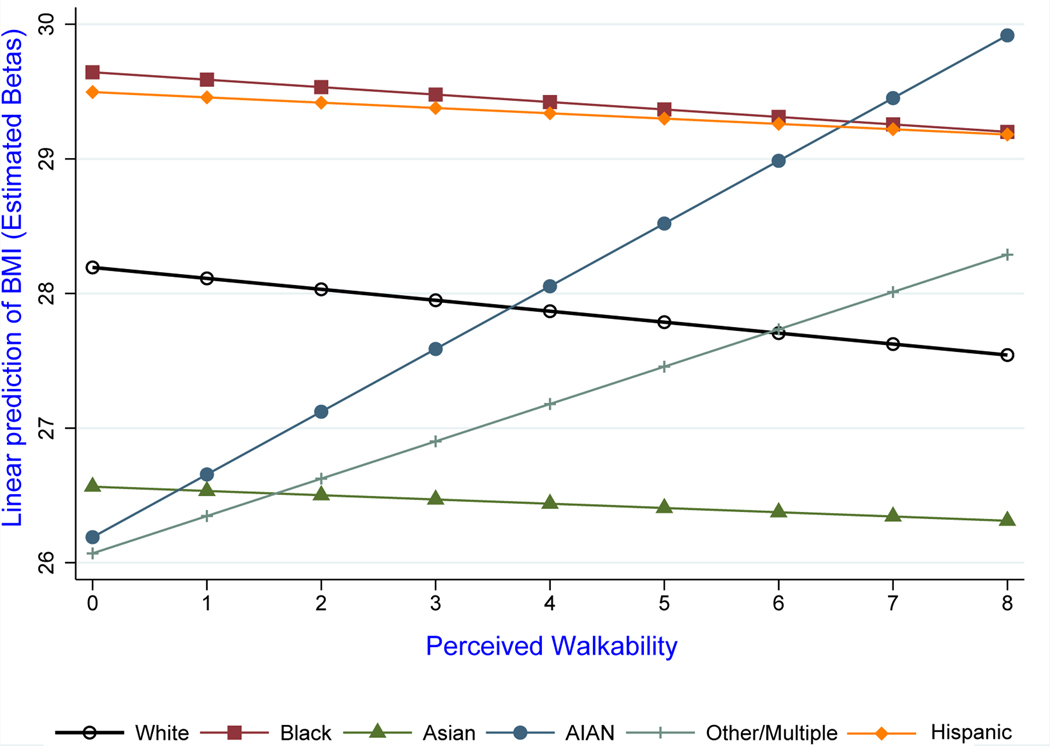
The sample included N=31,568 adults. Compared to those in low walkability neighborhoods, participants in high walkability neighborhoods had increased odds of sufficient PA (odds ratio [OR]=1.48; 95% CI:1.30–1.69) and decreased obesity odds (OR=0.76; 95% CI:0.66–0.87). PA partially mediated the association between walkability and BMI (23.4%; 95% CI:14.6%−62.7%). The association between walkability and BMI was modified by race/ethnicity (F(5,567) =2.75; p=0.018). Among White, Black, Hispanic, and Asian adults, BMI decreased with increasing walkability; among American Indian/Alaska Native and multiracial/other adults, BMI increased with increasing walkability.
Conclusions:
Findings highlight the importance of investing in the built environment to improve perceptions of walkability and promote PA and healthy weight and developing interventions to target racial/ethnic disparities in these outcomes.
Keywords: walkability, built environment, physical activity, obesity
INTRODUCTION
Obesity rates continue to rise among United States (U.S.) adults, with 73.6% of adults ages 20 and up currently falling in the overweight or obese category (1, 2). Three out of four adults do not meet recommended levels of physical activity (PA), defined as at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity a week (3). Given that PA is an established health behavior associated with body mass index (BMI) and obesity (4), identifying barriers and facilitators to engaging in PA is critical to shift population behavioral changes on this obesity risk factor.
Walkability, defined as the extent to which the built environment is conducive to walking (5), is a community-level factor shown to be associated with obesity (6). Studies have demonstrated that higher levels of perceived walkability are associated with improved health outcomes, such as decreased BMI (7), reduced obesity rates (8), improved mental health (9), reduced risk of diabetes, cardiometabolic disease, and hypertension,(10–12) and improved health behaviors, such as increased PA (13). However, studies of walkability and obesity that include nationally representative samples of U.S. adults or have adequate representation of communities of color are limited.
A growing number of studies have explored PA as a mediator in the association between perceived walkability and obesity. Some studies indicate that PA partially mediates the association between walkability and BMI or obesity (14–17), whereas other studies reported no mediating effect of PA on this association (18–20). Individuals who perceive high levels of walkability in their community may feel safer to spend active time outdoors, perceive fewer barriers to walking outdoors, and, thus, engage in overall higher levels of PA. Given that PA may be an important behavioral mechanism between walkability and obesity, examining the association(s) between perceived neighborhood walkability, PA, and obesity among a nationally representative sample of U.S. adults may elucidate important areas for intervention among a nation that is experiencing increasingly higher rates of obesity and decreased PA levels.
Study Objectives and Hypotheses
Using cross-sectional 2020 data from U.S. adults ages 18 and older, this study aimed to: (1) determine if living in an area with higher perceived walkability is associated with levels of PA and frequency of walking near home; (2) examine if living in an area with higher perceived walkability is associated with BMI; and (3) assess PA as a mediator in the association between perceived walkability and BMI. We hypothesized that higher perceived walkability would be associated with increased odds of engaging in adequate PA, increased frequency of walking near one’s home, and decreased odds of obesity and that PA would partially mediate the association between walkability and BMI.
METHODS
Data Source
This study used cross-sectional data from the 2020 National Health Interview Survey (NHIS). The NHIS is a household annual survey on illness, disability, chronic impairments, health insurance, health care access, and health services use. As part of the U.S. Center for Disease Control and Prevention, the National Center for Health Statistics (NCHS) selects one adult aged ≥ 18 years from random households to gather demographic and health-related information from face-to-face interviews. The NCHS also randomly selects one child aged ≤ years - and a parent or guardian answers questions about the child’s health.
The NHIS is a complex, multistage probability sample that incorporates stratification and clustering designed to represent the civilian, noninstitutionalized population living in the 50 states and the District of Columbia at the time of the survey. Since the NHIS adult sample was used in this study, the sample nationally represents the civilian, noninstitutionalized U.S. adult population (21). Due to the COVID-19 pandemic, NCHS shifted to all-telephone interviews in late March 2020 and continued through June of 2020. From July through December 2020 (quarters 3 and 4) of data collection, in-person visit interviewing resumed in areas with a low incidence of COVID-19; however, data collection remained mostly by telephone during this period (21).
Study Population
In 2020, 31,568 adults aged ≥ 18 years completed the interviews. The analytical sample excluded 3,116 participants with disabilities as categorized by the NCHS based on the Washington Group Short Set Composite Disability Indicator (22), as studies demonstrate that adults with disabilities have differing levels of PA and obesity from the general adult population (23, 24).
Measures
The definition and operationalization of the variables included in this analysis are shown in Table 1.
Table 1.
Operational Definition of Measured Variables
| DEPENDENT VARIABLES | Operational Definition of Variables † |
|---|---|
| 1. Physical activity: This variable indicates whether respondents met the 2018 physical activity guidelines for aerobic activity. Inactive: no activity; Insufficiently active: <150 min/week; Sufficiently active: 150+ min/week | ○ Inactive/Insufficiently active [0] ○ Sufficiently active [1] § |
| 2. Frequency of walking near home: How often does the walking you reported earlier take place near home? | ○ Never/Some of the time [0] ○ Most of the time/Almost always [1] § |
| 3. Body mass index: Continuous variables | ○ BMI was created from height and weight values. BMI was calculated using the formula: BMI = kilograms/meters2 where 1 kilogram = 2.20462 pounds and 1 meter = 39.37008 inches. |
| EXPOSURE | |
| Perceived walkability is a sum of eight dichotomous variables (Continuous) | ○ 0–8 |
| 1. Where you live, are there roads, sidewalks, paths, or trails where you can walk? | ○ No [0] ○ Yes [1] |
| 2. Are there shops, stores, or markets that you can walk to? | ○ No [0] ○ Yes [1] |
| 3. Are there bus or transit stops that you can walk to? | ○ No [0] ○ Yes [1] |
| 4. Are there places like movies, libraries, or places of worship that you can walk to? | ○ No [0] ○ Yes [1] |
| 5. Are there places that you can walk to that help you relax, clear your mind, and reduce stress? | ○ No [0] ○ Yes [1] |
| 6. Where you live, do most streets have sidewalks? | ○ No [0] ○ Yes [1] |
| 7. Does traffic make it unsafe for you to walk? Reverse coded | ○ No [0] ○ Yes [1] |
| 8. Does crime make it unsafe for you to walk? Reverse coded | ○ No [0] ○ Yes [1] |
| Perceived walkability (Categorical) | |
| Low | ○ Scores of 0–2 |
| Medium | ○ Scores of 3–5 |
| High | ○ Scores of 6–8 |
| INDEPENDENT VARIABLES | |
| Age in years | Continuous (50–85+) |
| Biological sex | ○ Male [0] §Female [1] |
| Race/Ethnicity | ○ Non-Hispanic White [0] § Racial/Ethnic minorities (Non-Hispanic Black, Non-Hispanic Asian, Non-Hispanic American Indian/Alaska Native, Non-Hispanic other race, Hispanic) |
| Marital status | ○ Single/Widowed/Separated [0] ○ Married/Partnered [1] § |
| Education level | ○ < Bachelor’s degree [0] § ○ ≥ Bachelor’s degree [1] |
| Urban-rural classification | ○ Large central metro [1] § ○ Large fringe metro [2] ○ Medium and small metro [3] ○ Non-metropolitan [4] |
| Region | ○ Northeast [1] § ○ Midwest [2] ○ South [3] ○ West [4] |
| Employment status | ○ Not employed last week or the past year/never [0] § ○ Employed last week or the past year [1] |
| Federal poverty level †† | ○ <=138 % [1] § ○ >138–250 % [2] ○ >250–400 % [3] ○ >400 % [4] |
| Total chronic diseases: Respondents answered “Yes” to having any of these diseases | Obesity, hypertension, type 2 diabetes, asthma, arthritis, COPD, hepatitis, coronary heart diseases, stroke, heart attack, angina, dementia, cirrhosis, kidney failure |
| Self-reported health status | ○ Excellent [1] § Very good [2] ○ Good [3] ○ Fair/Poor [4] |
Source: National Health Interview Survey (NHIS, 2020). National Center for Health Statistics (NCHS) – Centers for Disease Control and Prevention.
Note: Responses “Refused,” “Not ascertained,” “Don’t know” to all the factors questions were recoded as missing.
The Federal poverty level was derived from the ratio of family income to the poverty threshold.
Chosen as reference category in regression analysis.
Outcomes.
Three outcomes were examined and obtained from self-reported participant responses: (1) PA dichotomized as insufficiently active (<150 minutes/week or inactive) or sufficiently active (≥150 minutes/week); (2) frequency of walks near one’s home dichotomized as never/some of the time vs. most of the time/almost always; and (3) BMI assessed continuously and obesity status dichotomized as BMI ≥ 30.0 kg/m2 or BMI < 30.0 kg/m2.
Exposure.
Perceived walkability was the primary exposure of interest and derived from eight dichotomous questions on ease of walking related to neighborhood characteristics, such as traffic, crimes, roads, shops, transit, fun places, relaxing places, and sidewalks (see Table 1 for item questions). A summative continuous variable was created based on participants’ responses to these eight survey items; the range of this variable was 0 to 8, with higher scores indicating higher perceived walkability. Categorical measures of perceived walkability were generated with scores of 0–2 considered low walkability; 3–5 considered medium walkability; and 6–8 considered high walkability.
Potential mediators, moderators, and covariates.
PA was examined as a potential mediator in the association between perceived walkability and continuous BMI based on prior research demonstrating that PA may partially mediate this association (15). Race/ethnicity was examined as a potential effect modifier in the association between perceived walkability (continuous measure) and continuous BMI (25, 26). Sociodemographic variables and covariates assessed included: age in years (capped at 85), biological sex (male or female), race and ethnicity, marital status, education level, urban-rural classification, region, employment status, imputed family income as a percentage of the federal poverty level (FPL), total chronic diseases, and self-reported health status.
See Table 1 for additional details on covariate measurement.
Statistical Analyses
To describe the study population, we computed percentages for categorical variables and means for continuous variables. To gauge uncertainty of the point estimates, 95% confidence intervals (CI) were also computed. We examined bivariate associations between categorical outcomes and each potential sociodemographic variable and mediator using Rao-Scott (1987) Chi-square test (27), which accommodates the NHIS complex survey design (21, 28). For the continuous outcome (BMI), we conducted unpaired two-tailed t-tests.
Multicollinearity was gauged based on the sample variance inflation (VIF). The test indicated no high correlation between independent variables (mean VIF 1.29; range: 1.02–1.90); thus, we performed multivariable logistic regression for the dichotomous outcomes of PA and obesity status to test our hypotheses. To examine associations between perceived walkability and body mass index as a continuous outcome, we estimated a multiple linear regression model, then generated post-regression diagnostic plots to test the assumptions underlying the linear model (e.g., distance below the median, histogram of residuals, QNorm of residuals). For logistic regression models, Somers’ Delta (29) was used to indicate model fit (coefficient closer to 1 suggests better fit) adjusting for survey sampling weights.
To examine whether PA partially mediated the association between perceived walkability and BMI, Hicks and Tingley’s potential outcomes approach (30) was used to partition the effects of perceived walkability directly associated with BMI from its indirect effects mediated by PA. The mediation analysis reports the proportion of total effects mediated as the sum of changes in the probability of the outcome.
An indirect effect is the proportion of the total effect mediated by PA; a proportion between 0% and 50% would mean most of the effect of perceived walkability is direct, and a proportion above 50% would mean most of this total effect is mediated by PA. Statistical significance was set at α=0.05. All descriptive and regression analyses accounted for the complex NHIS survey design (i.e., final survey weights were used to enable computation of unbiased estimates of descriptive parameters and regression parameters as well as design-based standard errors reflecting variance in the weights) (31). Since NHIS imputed income data were used, missing data accounted for less than five percent. Thus, complete case analyses were conducted, and we expected results from multivariate analyses would not significantly change due to this low proportion of missingness (32). Effect modification in the association between walkability and BMI by race/ethnicity was examined using interaction (product term between walkability and race/ethnicity was included in the linear regression model). All analyses were conducted with STATA/SE 17 (33).
RESULTS
Descriptive Analysis
Table 2 describes the characteristics of the overall study population and across categories of the exposure of interest (high, medium, and low walkability). Among participants who were sufficiently active, 60.1% reported living in high walkability areas compared to 33.7% and 6.2% of those in medium and low walkability areas, respectively. Non-Hispanic (NH) Asian participants had the highest proportion of those reporting living in an area with high walkability (68.8%), followed by Hispanic (66.1%), NH other race (62.1%), NH Black (61.0%), NH White (48.7%), and NH American Indian/Alaska Native (AIAN) participants (37.4%). With respect to urbanicity, participants living in large central metro areas had the highest proportion of those reporting high walkability (73.7%), followed by large fringe metro (53.6%), medium and small metro (46.6%), and non-metropolitan (29.3%).
Table 2.
Study Population Characteristics across Levels of Perceived Walkability
| PERCEIVED WALKABILITY | ||||
|---|---|---|---|---|
|
| ||||
| VARIABLES | Unweighted | LOW (Scores 0–2) | MEDIUM (Scores 3–5) | HIGH (Scores 6–8) |
| N | Weighted Row % and (95% confidence intervals)† | |||
|
| ||||
| OUTCOMES | ||||
| Levels of Physical Activity | ||||
| Inactive/Insufficiently active (<150 minutes/week) | 13,580 | 10.5 (9.5,11.5) | 38.0 (36.6,39.5) | 51.5 (49.7,53.3) |
| Sufficiently active (≥150 minutes/week) | 13,942 | 6.2 (5.6,6.9) | 33.7 (32.4,35.0) | 60.1 (58.5,61.6) |
| Frequently Walks Near Home | ||||
| Never/Some of the time | 3,141 | 10.5 (9.1,12.1) | 33.1 (30.7,35.5) | 56.4 (53.7,59.1) |
| Most of the time/Almost always | 16,125 | 4.9 (4.3,5.4) | 35.0 (33.6,36.4) | 60.1 (58.5,61.7) |
| Body Mass Index (BMI) | 26,203 | 28.5 (28.2,28.8) | 28.1 (27.9,28.2) | 27.6 (27.4,27.7) |
|
| ||||
| Age in Years (18–85+) †† | 28,383 | 49.8 (48.9,50.6) | 49.8 (49.2,50.3) | 44.3 (43.9,44.7) |
| Biological Sex | ||||
| Male | 13,251 | 9.4 (8.6,10.2) | 33.7 (32.3,35.1) | 57.0 (55.3,58.6) |
| Female | 15,200 | 11.4 (10.5,12.4) | 36.4 (35.1,37.7) | 52.2 (50.6,53.8) |
| Marital Status | ||||
| Single/Widowed/Separated | 12,242 | 8.0 (7.1,9.0) | 31.6 (30.1,33.1) | 60.5 (58.7,62.2) |
| Married/Partnered | 15,345 | 8.5 (7.7,9.2) | 38.7 (37.4,40.0) | 52.9 (51.3,54.5) |
| Federal Poverty Level | ||||
| <=138% | 6,518 | 13.4 (11.9,14.9) | 32.0 (30.4,33.7) | 54.6 (52.4,56.8) |
| >138–250% | 4,353 | 12.4 (11.0,13.9) | 35.1 (33.1,37.1) | 52.5 (50.3,54.8) |
| >250–400% | 4,003 | 10.0 (8.8,11.3) | 36.8 (34.7,38.9) | 53.3 (51.0,55.5) |
| >400% | 13,578 | 8.0 (7.3,8.8) | 36.4 (34.9,37.9) | 55.6 (53.9,57.3) |
| Education Level | ||||
| < Bachelor’s degree | 13,964 | 11.9 (11.0,12.9) | 35.9 (34.6,37.3) | 52.2 (50.5,53.8) |
| ≥ Bachelor’s degree | 14,364 | 8.1 (7.4,8.9) | 33.8 (32.4,35.2) | 58.1 (56.5,59.7) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 19,802 | 10.8 (10.0,11.6) | 40.5 (39.2,41.8) | 48.7 (47.1,50.3) |
| Non-Hispanic Black | 2,865 | 11.8 (10.0,13.9) | 27.2 (24.7,29.9) | 61.0 (57.8,64.1) |
| Non-Hispanic Asian | 1,611 | 5.2 (47.1,53.5) | 26.0 (23.1,29.0) | 68.8 (65.5,72.0) |
| Non-Hispanic American Indian/Alaska Native | 157 | 27.3 (18.8,37.7) | 35.3 (27.8,43.7) | 37.4 (27.7,48.3) |
| Non-Hispanic other race | 506 | 10.4 (7.6,14.1) | 27.5 (23.0,32.5) | 62.1 (56.5,67.3) |
| Hispanic | 3,511 | 9.2 (7.2,11.6) | 24.7 (22.6,26.9) | 66.1 (62.8,69.3) |
| Employment Status | ||||
| Not employed last year or the past year/never | 8,679 | 10.8 (9.8,12.0) | 43.3 (41.5,45.0) | 45.9 (43.9,47.0) |
| Employed last week or the past year | 19,773 | 10.3 (9.5,11.0) | 32.3 (31.2,33.5) | 57.4 (56.0,58.9) |
| Region | ||||
| Northeast | 5,120 | 9.1 (7.4,11.1) | 31.2 (28.2,34.3) | 59.7 (55.9,63.5) |
| Midwest | 6,439 | 7.8 (6.7,9.0) | 36.6 (34.4,38.8) | 55.6 (52.8,58.4) |
| South | 9,703 | 16.0 (14.6,17.5) | 43.1 (41.3,45.0) | 40.9 (38.6,43.2) |
| West | 7,190 | 4.9 (4.1,5.9) | 24.1 (22.1,26.2) | 71.0 (68.4,73.4) |
| Urban-Rural Classification | ||||
| Large central metro | 8,595 | 5.4 (4.8,6.2) | 20.9 (19.2,22.6) | 73.7 (19.2,22.6) |
| Large fringe metro | 6,822 | 9.1 (8.0,10.3) | 37.3 (35.1,39.5) | 53.6 (50.9,56.2) |
| Medium and small metro | 8,969 | 12.4 (10.8,14.2) | 41.1 (39.1,43.1) | 46.6 (43.7,49.4) |
| Non-metropolitan | 4,066 | 20.0 (17.4,22.9) | 50.7 (47.7,53.7) | 29.3 (26.2,32.6) |
| Self-Reported Health Status | ||||
| Excellent | 7,118 | 8.9 (8.2,10.0) | 31.6 (34.4,37.5) | 59.4 (53.2,56.8) |
| Very good | 10,601 | 9.1 (45.7,48.4) | 35.9 (51.6,54.3) | 55.0 (53.2,56.8) |
| Good | 7,930 | 11.7 (60.0,62.9) | 35.8 (34.1,37.4) | 52.5 (50.6,54.4) |
| Fair/Poor | 2,787 | 15.6 (13.8,17.6) | 39.3 (6.8,41.9) | 45.1 (42.4,47.8) |
| Total chronic diseases (0–11) | 28,452 | 1.5 (1.4,1.6) | 1.4 (1.4,1.4) | 1.0 (1.0,1.1) |
Source: National Health Interview Survey (NHIS, 2020). National Center for Health Statistics (NCHS) - Centers for Diseases Control and Prevention.
Note: Row percentages are presented and should equal 100% after rounding.
In the NHIS, age is top-coded at 85 to protect the confidentiality of the few participants aged >85 years
Regression Analysis
AIM 1: Determine if living in an area with higher perceived walkability was associated with higher odds of engaging in sufficient PA and higher frequency of walking near home.
Table 3 reports adjusted odd-ratios (OR) and 95% CIs for aim 1. Compared to those in low walkability neighborhoods, participants in high walkability neighborhoods had increased odds of engaging in sufficient PA (OR=1.48; CI:1.30, 1.69; p<0.001). The Somers D statistic was 0.70 (CI:0.69, 0.71; p<0.001), indicating a good predictive model. We also found a positive association between perceived walkability and frequency of walks near home; for each one-unit increase in perceived walkability, the odds of reporting walking near home almost always/most of the time vs. never/some of the time increased by 1.15. For this model, the Somers D statistics was 0.52 (CI:0.51, 0.52; p<0.001), indicating a fair predictive model. Compared to NH White participants, NH Black, NH Asian, and Hispanic participants had lower odds of engaging in sufficient PA and walking near one’s home almost always/most of the time (p’s <0.05).
Table 3.
Multivariable Logistic Regression Results: Associations between Perceived Walkability and the Outcomes Physical Activity and Frequency of Walking
| Associations between Perceived Walkability and Physical Activity (95% Confidence Intervals) | Associations between Perceived Walkability and Frequency of Walking near Home Odd-Ratios (95% Confidence Intervals) | |
|---|---|---|
| OUTCOME | OUTCOME | |
|
| ||
| VARIABLES | PHYSICAL ACTIVITY (Inactive/Insufficiently active vs. Sufficiently active) | FREQUENCY OF WALKING NEAR HOME (Never/Some of the time vs. Almost always/Most of the time) |
|
| ||
| Perceived Walkability | ||
| Low | - | - |
| Medium | 1.30*** (1.15,1.47) | 2.47*** (2.02,3.02) |
| High | 1.48*** (1.30,1.69) | 2.79*** (2.27,3.41) |
| Age in Years | 0.99*** (0.99,1.00) | 1.01*** (1.00 – 1.01) |
| Biological Sex | ||
| Male | - | - |
| Female | 0.71*** (0.66,0.76) | 1.17** (1.05,1.31) |
| Marital Status | ||
| Single/Widowed/Separated | - | - |
| Married/Partnered | 0.94 (0.87,1.01) | 1.29*** (1.16,1.43) |
| Federal Poverty Level | ||
| <=138 % | - | - |
| >138–250 % | 0.73 (0.52,1.03) | 1.23 (0.70,2.16) |
| >250–400 % | 0.87 (0.66,1.14) | 0.93 (0.59,1.45) |
| >400 % | 1.14 (0.90,1.46) | 0.85 (0.57,1.27) |
| Education Level | ||
| < Bachelor’s degree | - | - |
| ≥ Bachelor’s degree | 1.61*** (1.50,1.72) | 1.20*** (1.08,1.34) |
| Race/Ethnicity | ||
| Non-Hispanic White | - | - |
| Non-Hispanic Black | 0.79*** (0.70,0.89) | 0.72*** (0.60,0.86) |
| Non-Hispanic Asian | 0.65*** (0.56,0.75) | 0.71*** (0.59,0.87) |
| Non-Hispanic American Indian/Alaska Native | 0.64 (0.38,1.08) | 0.91 (0.47,1.80) |
| Non-Hispanic other race | 0.76* (0.58,0.99) | 0.96 (0.63,1.45) |
| Hispanic | 0.71*** (0.63,0.80) | 0.71*** (0.61,0.83) |
| Employment Status | ||
| Not employed last week or the past year/never | - | - |
| Employed last week or the past year | 0.93 (0.85,1.02) | 0.74*** (0.63,0.85) |
| Region | ||
| Northeast | - | - |
| Midwest | 1.02 (0.90,1.15) | 0.87 (0.73,1.04) |
| South | 0.99 (0.89,1.11) | 1.00 (0.85,1.19) |
| West | 1.28*** (1.13,1.44) | 0.88 (0.75,1.03) |
| Urban-Rural Classification | ||
| Large central metro | - | - |
| Large fringe metro | 1.05 (0.96,1.16) | 0.88 (0.75,1.03) |
| Medium and small metro | 0.91 (0.83,1.00) | 0.79** (0.69,0.92) |
| Non-metropolitan | 0.82** (0.73,0.92) | 0.98 (0.80,1.20) |
| Self-Reported Health Status | ||
| Excellent | - | - |
| Very good | 0.67*** (0.62,0.73) | 0.94 (0.82, 1.07) |
| Good | 0.45*** (0.41,0.49) | 0.85* (0.73,0.99) |
| Fair/Poor | 0.32*** (0.28,0.37) | 0.74** (0.59,0.91) |
| Total Chronic Diseases | 0.91*** (0.88,0.93) | 1.03 (0.98,1.07) |
Source: National Health Interview Survey (NHIS, 2020). National Center for Health Statistics (NCHS) – Centers for Disease Control and Prevention.
Note: Statistical significance:
p<0.001
p<0.01
p<0.05
AIM 2: Determine if living in an area with higher perceived walkability is associated with lower BMI and decreased odds of obesity.
Table 4 reports adjusted ORs and 95% CIs for aim 2. We found a negative association between perceived walkability and obesity; living in an area with higher perceived walkability was associated with lower BMI (= −0.06, CI:−0.10, - 0.02; p=0.006). The diagnostic plots (not shown) suggested that the assumptions of normality and constant variance of the residuals were not violated, giving us confidence in the inferences made. Compared to participants in low walkability neighborhoods, participants in high walkability neighborhoods had decreased odds of obesity (OR=0.76; CI:0.66, 0.87; p<0.001).
Table 4.
Regression Analysis Results: Associations between Perceived Walkability and Body Mass Index/Obesity
| Associations between Perceived Walkability and Body Mass Index (95% Confidence Intervals) | Associations between Perceived Walkability and Obesity (95% Confidence Intervals) | |
|---|---|---|
| VARIABLES | Estimates from Linear Regression | Estimates from Logistic Regression |
|
| ||
| Perceived Walkability | ||
| Low | - | - |
| Medium | 0.78*** (0.68,0.90) | |
| High | 0.76*** (0.66,0.87) | |
| Perceived Walkability (0–8) | −0.06** (−0.10,−0.02) | |
| Age in Years | −0.05*** (−0.05,−0.04) | 0.96*** (0.95,0.96) |
| Biological Sex | ||
| Male | - | - |
| Female | −0.21** (−0.36,−0.06) | 1.07 (0.99,1.16) |
| Marital Status | ||
| Single/Widowed/Separated | - | - |
| Married/Partnered | 0.97*** (0.08,1.14) | 1.49*** (1.37,1.62) |
| Federal Poverty Level | ||
| <=138 % | - | - |
| >138–250 % | 0.12 (−0.77,1.01) | 1.16 (0.76,1.77) |
| >250–400 % | 0.35 (−0.32,1.02) | 1.10 (0.79,1.54) |
| >400 % | 0.30 (−0.29,0.90) | 1.25 (0.93,1.68) |
| Education Level | ||
| < Bachelor’s degree | - | - |
| ≥ Bachelor’s degree | −0.37*** (−0.53,−0.21) | 0.85*** (0.79,0.93) |
| Race/Ethnicity | ||
| Non-Hispanic White | - | - |
| Non-Hispanic Black | 1.59*** (1.30,1.89) | 1.84*** (1.62,2.10) |
| Non-Hispanic Asian | −1.34*** (−1.59,−1.09) | 0.40*** (0.32,0.50) |
| Non-Hispanic American Indian/Alaska Native | 0.53 (−0.66,1.71) | 1.02 (0.53,1.95) |
| Non-Hispanic other race | −0.03 (−0.58,0.51) | 0.95 (0.70,1.29) |
| Hispanic | 1.54*** (1.26,1.82) | 1.84*** (1.62,2.07) |
| Employment Status | ||
| Not employed last week or the past year/never | - | - |
| Employed last week or the past year | 1.44*** (1.21,1.66) | 2.27*** (2.01,2.57) |
| Region | ||
| Northeast | - | - |
| Midwest | 0.28* (0.04,0.52) | 1.08 (0.95,1.22) |
| South | 0.09 (−0.13,0.31) | 1.05 (0.93,1.19) |
| West | −0.27* (−0.50,−0.03) | 0.88 (0.77,1.01) |
| Urban-Rural Classification | ||
| Large central metro | - | - |
| Large fringe metro | 0.14 (−0.07,0.35) | 1.04 (0.92,1.16) |
| Medium and small metro | 0.32** (0.12,0.52) | 1.13* (1.02,1.26) |
| Non-metropolitan | 0.71*** (0.40,1.02) | 1.37*** (1.19,1.58) |
| Self-Reported Health Status | ||
| Excellent | - | - |
| Very good | 0.96*** (0.77,1.15) | 1.54*** (1.37,1.72) |
| Good | 1.49*** (1.26,1.71) | 1.85*** (1.65,2.07) |
| Fair/Poor | 0.80*** (0.43,1.17) | 0.94 (0.78,1.13) |
| Total Chronic Diseases | 2.04*** (1.97,2.11) | 3.85*** (3.63,4.07) |
Source: National Health Interview Survey (NHIS, 2020). National Center for Health Statistics (NCHS) – Centers for Disease Control and Prevention.
Note: Statistical significance:
p<0.001
p<0.01
p<0.05
AIM 3: Determine if PA mediates the association between perceived walkability and BMI
The mediation analysis showed the proportion of the total effect of perceived walkability on BMI was partially mediated by PA (23.4%; 95% CI:14.6%, 62.7%), adjusting for covariates. Additional exploration of potential effect modification showed that the association between perceived walkability and BMI was significantly modified by race/ethnicity (F (5,567) =2.75; p=0.018).
Interactions are graphically depicted in Figure 1 and showed that, on average, for NH White, NH Black, Hispanic, and NH Asian adults, predicted BMI decreased with increased perceived walkability. In contrast, predicted BMI increased with increased perceived walkability among NH AIAN and NH multiracial/other race adults, after controlling for the influence of other covariates.
Figure 1. Race/Ethnicity as an Effect Modifier in the Association between Perceived Walkability and Body Mass Index Note:
The estimated means (adjusted for all the other covariates) of body mass index along the perceived walkability scale is depicted by race/ethnicity. All estimates were statistically significant (p<0.05). While the estimates appear to have a strong magnitude for American Indian/Alaska Native and Non-Hispanic other race persons, those samples are considerably smaller. The 95% confidence intervals are not shown as they would obscure the interaction lines.
DISCUSSION
This study is the first to our knowledge investigate perceived neighborhood walkability and its associations with PA and obesity among a large, nationally representative sample of U.S. adults using 2020 data from the NHIS. Findings demonstrated that adults in our study who reported living in neighborhoods with high walkability were 1.5 times more likely to engage in adequate levels of PA and are 0.76 times less likely to have obesity compared with those who reported living in neighborhoods with low walkability, adjusting for covariates. Additionally, tests of mediation indicated that PA partially mediated the association between perceived walkability and BMI.
The associations between perceived walkability, PA, and obesity observed in this current study are in line with findings from prior research examining these associations among other adult populations, with measures of neighborhood walkability shown to be protective against obesity and positively associated with PA (7, 8, 34). Living in a neighborhood that is more conducive to walking based on a variety of factors may facilitate and encourage residents in that neighborhood to spend more active time outdoors, resulting in overall higher activity levels and subsequently reduced BMI and obesity risk. Our measure of perceived walkability also included assessing perceptions of crime and safety, which have been cited as major barriers that prevent individuals from engaging in outdoor activity (35).
The literature on PA as a mediator between walkability, BMI, and obesity has been mixed. While some studies report that PA partially mediates the association between walkability and BMI or obesity (14–17), other studies have found no mediating effect of PA on this association (18–20). Results from our mediation analysis indicate that in our nationally representative sample of U.S. adults, PA partially mediated the effect of perceived walkability on BMI.
The inconsistent literature on PA as a mediator between walkability and obesity may be attributed to several factors. Walkability and PA have been defined and measured differently across studies (36), with no one standardized assessment or instrument for perceptions of walkability in particular (37). Thus, variations in findings of PA as a mediator between walkability and BMI may be partially explained by variations in instrument measurement. Second, perceived walkability may not necessarily equate higher levels of walking or PA, with preference for walking or PA serving as a potential confounder. Studies demonstrate that preference for walking or PA significantly predicts PA levels (38), even after accounting for objective measures of walkability. Third, walkability may be associated with obesity by capturing other aspects of the built environment (e.g., access to healthy produce) that may influence obesity-related behaviors other than PA, such as diet (39). This body of literature suggests that walkability is one of many important characteristics of the built environment that may shape a variety of weight-related behaviors.
Notably, our study findings also highlighted racial and ethnic inequities in the associations of interest. While higher proportions of NH Black, Hispanic, NH Asian, NH AIAN, and NH other race participants reported living in high walkability areas compared to NH White participants, NH Black, Hispanic, and NH Asian participants had lower odds of engaging in sufficient PA and reporting walking near one’s home almost always or most of the time. One possible explanation for this finding is that while participants may perceive neighborhoods to be walkable, it may not be safe, desirable, or normative to walk in these communities. Additionally, the association between perceived walkability and BMI differed by race/ethnicity. Among NH White, NH Black, Hispanic, and NH Asian participants, BMI decreased with increasing perceived neighborhood walkability. However, among NH AIAN and NH multiracial/other adults, BMI increased with increasing perceived neighborhood walkability. This finding suggests that targeting perceptions of walkability alone may not be sufficient in improving PA and BMI among NH AIAN and NH multiracial/other populations. The racial and ethnic inequities in PA outcomes and in the main association between walkability and BMI may reflect the inequitable built environment conditions and corresponding barriers to PA and other health behaviors that communities of color were exposed to as a result of systemic racism and policies such as racial residential segregation and forced displacement of indigenous populations (40, 41). These inequities highlight the need to prioritize intervention efforts and resources for communities who experience disproportionately higher obesity risk from a health equity lens, such as expanding access to PA places in marginalized communities (42).
The associations observed between perceived neighborhood walkability and BMI in our study and previous studies suggest that enhancing walkability through multiple strategies (e.g., sidewalk redesign, increasing street connectivity, implementing policies and signs that slow traffic, enhancing park quality, incorporating mixed land use) (43, 44) may be high impact intervention targets for addressing obesity and PA. Developing and evaluating interventions that integrate or address walkability, particularly among marginalized communities of color, may be one approach to mitigate racial disparities in PA and obesity. Finally, considering the overall high rates of obesity and inadequate levels of PA at the national level, this study identifies walkability as a critical environmental and community-level characteristic that can be modified and intervened upon to promote PA and prevent obesity.
Limitations
Study limitations include the cross-sectional design of the 2020 NHIS survey, which limits our ability to determine directionality and establish causal inference. PA was also assessed via self-report and may be over-estimated (45) and subject to variations in cultural interpretation (46) or social desirability bias in reporting (47). Causal mediation relies on the validity of the assumption that the exposure (walkability) temporarily precedes the hypothesized mediator (PA)—an assumption that cannot be ensured with cross-sectional data. Our measure of walkability has not, to our knowledge, been validated across different racial and ethnic groups, and responses were based on participants’ perceptions, which may vary based on comfort level and security (5). Dichotomizing obesity as an outcome as in this study limits our understanding of associations for other weight status groups (e.g., individuals with overweight status). Obesity was determined based on self-reported measures of height and weight, which may be subject to biases in reporting. However, a validation study of a national sample of U.S. adults suggests that BMI-based weight status categories derived from self-reported height and weight data is a valid measure among adults (48).
Strengths
This study is first to our knowledge to examine the associations between perceived walkability, PA, and obesity using data from the 2020 NHIS. The NHIS is among the largest of national health surveys of adults in the country, and participants in our sample comprise a nationally representative, random sample. Our study also tested PA as a mediator in the association between walkability and BMI, whereas other studies have not had the statistical power or study design to include this type of analysis. Importantly, this study demonstrated that walkability is significantly associated with decreased odds of obesity and increased odds of adequate PA, with PA partially mediating the association between walkability and BMI and race/ethnicity modifying this association.
CONCLUSION
Perceived high neighborhood walkability was associated with decreased BMI and decreased odds of obesity among a nationally representative sample of U.S. adults. The association between walkability and BMI was partially mediated by PA levels and modified by race/ethnicity. Our findings highlight the need for investment and investigation of a multitude of intervention strategies targeting walkability to promote PA and prevent obesity, particularly among communities of color who are exposed to disparate built environments and have disproportionately higher risk for obesity.
Study Importance.
What is already known on this subject?
Studies have demonstrated that higher levels of perceived walkability are associated with improved health outcomes, such as decreased BMI, reduced obesity rates, improved mental health, reduced risk of diabetes, cardiometabolic disease, and hypertension, and improved health behaviors, such as increased physical activity.
Studies of walkability and obesity that include nationally representative samples of United States (U.S.) adults or have adequate representation of communities of color are limited.
What are the new findings in your manuscript?
Perceived high neighborhood walkability was associated with decreased BMI and decreased odds of obesity among a nationally representative sample of U.S. adults.
The association between walkability and BMI was partially mediated by physical activity.
The association between walkability and BMI was modified by race/ethnicity.
How might your results change the direction of research or the focus of clinical practice?
Findings highlight the need for investment and investigation of a multitude of intervention strategies targeting walkability to promote physical activity and prevent obesity, particularly among communities of color who are exposed to disparate built environments and have disproportionately higher risk for obesity.
Acknowledgments
The 2020 National Health Interview Survey (NHIS) is openly made available by the Centers for Diseases Control and Prevention (CDC) at https://www.cdc.gov/nchs/nhis/2020nhis.htm. No datasets were generated for this study. Any analysis, interpretation, and/or conclusion based on the NHIS 2020 data is solely that of the authors. Opinions, conclusions, and recommendations expressed herein do not necessarily represent those of the National Center for Health Statistics or CDC, which are responsible for the data.
Funding:
his work was supported in part by the University of Arkansas for Medical Sciences Translational Research Institute funding (UL1 TR003107) awarded through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). Analysis, interpretation, and/or conclusions based on the National Health Interview Survey (NHIS) are solely that of the authors and do not represent those of the National Centers for Health Statistics (NCHS), which are responsible for the data.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.National Center for Health Statistics. FastStats - Overweight Prevalence: Centers for Disease Control and Prevention; 2022. Updated September 6, 2022. Accessed June 22, 2022. Available from: https://www.cdc.gov/nchs/fastats/obesity-overweight.htm..
- 2.Fryar C, Carroll M, Afful J. Products - Health E Stats - Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults Aged 20 and Over: United States, 1960–1962 Through 2017–2018. National Center for Health Statistics, Centers for Disease Control and Prevention; 2021.
- 3.Centers for Disease Control and Prevention. Adults meeting aerobic and muscle strengthening guidelines. Nutrition, Physical Activity, and Obesity: Data, Trends, and Maps (2020). Updated October 4, 2022. Accessed June 23, 2022. Available from: https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html.
- 4.Aqeel M, Guo J, Lin L, Gelfand S, Delp E, Bhadra A, et al. Temporal physical activity patterns are associated with obesity in U.S. adults. Prev Med. 2021;148:106538. Epub 20210330. doi: 10.1016/j.ypmed.2021.106538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao B, van den Berg P, van Wesemael P, Arentze T. How Does Walkability Change Behavior? A Comparison between Different Age Groups in the Netherlands. Int J Environ Res Public Health. 2020;17(2):540. Epub 20200115. doi: 10.3390/ijerph17020540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nichani V, Turley L, Vena J, McCormack G. Associations between the neighbourhood characteristics and body mass index, waist circumference, and waist-to-hip ratio: Findings from Alberta’s Tomorrow Project. Health Place. 2020;64:102357. Epub 20200528. doi: 10.1016/j.healthplace.2020.102357. [DOI] [PubMed] [Google Scholar]
- 7.Tarlov E, Silva A, Wing C, Slater S, Matthews S, Jones K, et al. Neighborhood Walkability and BMI Change: A National Study of Veterans in Large Urban Areas. Obesity (Silver Spring). 2020;28(1):46–54. Epub 20191205. doi: 10.1002/oby.22611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowaleski-Jones L, Zick C, Smith K, Brown B, Hanson H, Fan J. Walkable neighborhoods and obesity: Evaluating effects with a propensity score approach. SSM Popul Health. 2018;6:9–15. Epub 20171208. doi: 10.1016/j.ssmph.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao Y, Chung P. Neighborhood environment walkability and health-related quality of life among older adults in Hong Kong. Arch Gerontol Geriatr. 2017;73:182–6. Epub 20170810. doi: 10.1016/j.archger.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Booth G, Creatore M, Luo J, Fazli G, Johns A, Rosella L, et al. Neighbourhood walkability and the incidence of diabetes: an inverse probability of treatment weighting analysis. J Epidemiol Community Health. 2019;73(4):287–94. Epub 20190129. doi: 10.1136/jech-2018-210510. [DOI] [PubMed] [Google Scholar]
- 11.Coffee N, Howard N, Paquet C, Hugo G, Daniel M. Is walkability associated with a lower cardiometabolic risk? Health Place. 2013;21:163–9. Epub 20130208. doi: 10.1016/j.healthplace.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Jones A, Chaudhary N, Patki A, Howard V, Howard G, Colabianchi N, et al. Neighborhood Walkability as a Predictor of Incident Hypertension in a National Cohort Study. Front Public Health. 2021;9:611895. Epub 20210201. doi: 10.3389/fpubh.2021.611895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bojorquez I, Romo-Aguilar M, Ojeda-Revah L, Tena F, Lara-Valencia F, García H, et al. Public spaces and physical activity in adults: insights from a mixed-methods study. Cad Saude Publica. 2021;37(1):e00028720. Epub 20210122. doi: . [DOI] [PubMed] [Google Scholar]
- 14.Brown BB, Werner CM, Smith KR, Tribby CP, Miller HJ. Physical activity mediates the relationship between perceived crime safety and obesity. Preventive medicine. 2014;66:140–4. doi: 10.1016/j.ypmed.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Dyck D, Cerin E, Akram M, Conway T, Macfarlane D, Davey R, et al. Do physical activity and sedentary time mediate the association of the perceived environment with BMI? The IPEN adult study. Health Place. 2020;64:102366. Epub 20200622. doi: 10.1016/j.healthplace.2020.102366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carlson J, Remigio-Baker R, Anderson C, Adams M, Norman G, Kerr J, et al. Walking mediates associations between neighborhood activity supportiveness and BMI in the Women’s Health Initiative San Diego cohort. Health Place. 2016;38:48–53. Epub 20160201. doi: 10.1016/j.healthplace.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colley R, Christidis T, Michaud I, Tjepkema M, Ross N. An examination of the associations between walkable neighbourhoods and obesity and self-rated health in Canadians. Health Rep. 2019;30(9):14–24. doi: 10.25318/82-003-x201900900002-eng. [DOI] [PubMed] [Google Scholar]
- 18.Frank L, Adhikari B, White K, Dummer T, Sandhu J, Demlow E, et al. Chronic disease and where you live: Built and natural environment relationships with physical activity, obesity, and diabetes. Environ Int. 2022;158:106959. Epub 20211109. doi: 10.1016/j.envint.2021.106959. [DOI] [PubMed] [Google Scholar]
- 19.Chandrabose M, Cerin E, Mavoa S, Dunstan D, Carver A, Turrell G, et al. Neighborhood walkability and 12-year changes in cardio-metabolic risk: the mediating role of physical activity. Int J Behav Nutr Phys Act. 2019;16(1):86. Epub 20191015. doi: 10.1186/s12966-019-0849-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malambo P, Kengne A, Lambert E, De Villiers A, Puoane T. Does Physical Activity Mediate the Association Between Perceived Neighborhood Aesthetics and Overweight/Obesity Among South African Adults Living in Selected Urban and Rural Communities? J Phys Act Health. 2017;14(12):925–32. Epub 20171012. doi: 10.1123/jpah.2016-0147. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics. 2020 Survey Description. Centers for Disease Control and Prevention, 2021. [Google Scholar]
- 22.Washington Group of Disability Statistics. Analysis Overview. Published 2022. Accessed September 9, 2022. Available from: https://www.washingtongroup-disability.com/analysis/analysis-overview/.
- 23.Centers for Disease Control and Prevention. Disability and Obesity. Updated September 9, 2019. Accessed December 9, 2022. Available from: https://www.cdc.gov/ncbddd/disabilityandhealth/obesity.html.
- 24.Fox M, Witten M, Lullo C. Reducing Obesity Among People With Disabilities. J Disabil Policy Stud. 2014;25(3):175–85. doi: 10.1177/1044207313494236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Do D, Moore K, Barber S, Diez Roux A. Neighborhood racial/ethnic segregation and BMI: A longitudinal analysis of the Multi-ethnic Study of Atherosclerosis. Int J Obes (Lond). 2019;43(8):1601–10. Epub 20190122. doi: 10.1038/s41366-019-0322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Min J, Goodale H, Xue H, Brey R, Wang Y. Racial-Ethnic Disparities in Obesity and Biological, Behavioral, and Sociocultural Influences in the United States: A Systematic Review. Adv Nutr. 2021;12(4):1137–48. doi: 10.1093/advances/nmaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao J, Scott A. On Simple Adjustments to Chi-Square Tests with Sample Survey Data. The Annals of Statistics. 1987;15(1):385–97. doi: 10.1214/aos/1176350273. [DOI] [Google Scholar]
- 28.Bramlett M, Dahlhamer J, Bose J. Weighting Procedures and Bias Assessment for the 2020 National Health Interview Survey. National Center for Health Statistics, Centers for Disease Control and Prevention, 2021.
- 29.Somers RH. A new asymmetric measure of association for ordinal variables. American Sociological Review. 1962;27(6):799–811. doi: 10.2307/2090408. [DOI] [Google Scholar]
- 30.Hicks R, Tingley D. Causal Mediation Analysis. The Stata Journal. 2011;11(4):605–19. doi: 10.1177/1536867X1201100407. [DOI] [Google Scholar]
- 31.Heeringa S, West BT, Berglund PA. Applied survey data analysis. 2nd ed. CRC Press, Taylor & Francis Group; 2017. [Google Scholar]
- 32.Little RJA, Rubin DB. Statistical analysis with missing data. 3rd ed. Wiley; 2020. [Google Scholar]
- 33.StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. . [Google Scholar]
- 34.Rundle A, Sheehan D, Quinn J, Bartley K, Eisenhower D, Bader M, et al. Using GPS Data to Study Neighborhood Walkability and Physical Activity. Am J Prev Med. 2016;50(3):e65–e72. Epub 20151107. doi: 10.1016/j.amepre.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 35.Fish JS, Ettner S, Ang A, Brown AF. Association of perceived neighborhood safety with [corrected] body mass index. Am J Public Health. 2010;100(11):2296–303. Epub 2010/09/25. doi: 10.2105/ajph.2009.183293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dowd K, Szeklicki R, Minetto M, Murphy M, Polito A, Ghigo E, et al. A systematic literature review of reviews on techniques for physical activity measurement in adults: a DEDIPAC study. Int J Behav Nutr Phys Act. 2018;15(1):15. Epub 20180208. doi: 10.1186/s12966-017-0636-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iroz-Elardo N, Adkins A, Ingram M. Measuring perceptions of social environments for walking: A scoping review of walkability surveys. Health Place. 2021;67:102468. Epub 20201204. doi: 10.1016/j.healthplace.2020.102468. [DOI] [PubMed] [Google Scholar]
- 38.Norman G, Carlson J, O’Mara S, Sallis J, Patrick K, Frank L, et al. Neighborhood preference, walkability and walking in overweight/obese men. Am J Health Behav. 2013;37(2):277–82. doi: 10.5993/ajhb.37.2.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rummo P, Feldman J, Lopez P, Lee D, Thorpe L, Elbel B. Impact of Changes in the Food, Built, and Socioeconomic Environment on BMI in US Counties, BRFSS 2003–2012. Obesity (Silver Spring). 2020;28(1):31–9. Epub 20191105. doi: 10.1002/oby.22603. [DOI] [PubMed] [Google Scholar]
- 40.Bower K, Thorpe R Jr, Yenokyan G, McGinty E, Dubay L, Gaskin D. Racial Residential Segregation and Disparities in Obesity among Women. J Urban Health. 2015;92(5):843–52. doi: 10.1007/s11524-015-9974-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bell C, Kerr J, Young J. Associations between Obesity, Obesogenic Environments, and Structural Racism Vary by County-Level Racial Composition. Int J Environ Res Public Health. 2019;16(5):861. Epub 20190309. doi: 10.3390/ijerph16050861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webber B, Irani K, Omura J, Whitfield G. Observation of and intention to use new places and changed spaces for physical activity during the COVID-19 pandemic - United States, June 2021. Prev Med. 2022;160:107100. Epub 20220525. doi: 10.1016/j.ypmed.2022.107100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith M, Hosking J, Woodward A, Witten K, MacMillan A, Field A, et al. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14(1):158. Epub 20171116. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cairns J, Warren J, Garthwaite K, Greig G, Bambra C. Go slow: an umbrella review of the effects of 20 mph zones and limits on health and health inequalities. J Public Health (Oxf). 2015;37(3):515–20. Epub 20140928. doi: 10.1093/pubmed/fdu067. [DOI] [PubMed] [Google Scholar]
- 45.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 46.Silsbury Z, Goldsmith R, Rushton A. Systematic review of the measurement properties of self-report physical activity questionnaires in healthy adult populations. BMJ Open. 2015;5(9):e008430. Epub 2015/09/15. doi: 10.1136/bmjopen-2015-008430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adams SA, Matthews CE, Ebbeling CB, Moore CG, Cunningham JE, Fulton J, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161(4):389–98. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hodge JM, Shah R, McCullough ML, Gapstur SM, Patel AP. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS One. 2021;15(4):e0231229. doi: 10.1371/journal.pone.0231229. [DOI] [PMC free article] [PubMed] [Google Scholar]