Abstract
Aim
This paper aimed to investigate the relationship between social support and quality of life for nurses in infectious disease departments in China, as well as the function of psychological resilience in mediating this relationship.
Background
Nurses in infectious disease departments play a critical role in the prevention and control of infectious diseases and in public health care services in general, and their quality of life can affect the quality of clinical nursing work they do. However, there are few studies on the relationship between nurses' social support networks and their quality of life.
Methods
A cross‐sectional study was conducted using a sample of 866 clinical nurses from the infectious disease departments of 10 general hospitals in China. Data were collected using a questionnaire survey from January to May 2021. The mediating influence of psychological resilience on social support and quality of life was investigated using structural equation modelling.
Results
The score of quality of life was (36.36 ± 7.64). Quality of life was positively correlated with social support and psychological resilience (r 1 = 0.521, r 2 = 0.583; p < .01), and psychological resilience was positively correlated with social support (r = 0.426; p < .01) as well. The mediating effect of psychological resilience between social support and quality of life was 0.233, accounting for 37% of the total effect.
Conclusion
The quality of life of nurses working in infectious disease departments is in the middle level. Psychological resilience is a mediating variable between social support and quality of life.
Implications for Nursing Management
Managers can improve the quality of life of nurses by both increasing social support and strengthening psychological resilience. Managers should pay attention to the degree of social support provided to nurses and take proactive measures to build psychological resilience so that nurses can effectively manage stress and negative emotions from work and life in order improve their quality of life.
Keywords: mediating effect, nurses, psychological resilience, quality of life, social support, structural equation model
1. INTRODUCTION
Nurses are gaining increasing attention from society in the wake of the COVID‐19 outbreak though they remain in short supply. The World Health Organization's State of the World's Nursing 2020 study released in 2021 stated that the nurse shortage was intensely problematic, and the Chinese Ministry of Health has said that the hiring of nurses in infectious disease departments must be accelerated (NHC, 2022). Infectious disease departments (IDDs) are where patients with infectious diseases receive their primary treatment, and nurses are the providers who have the most direct interaction with these patients (Zakeri et al., 2021). The particularity of the environment and the characteristics of infectious diseases, such as acute onset, sometimes hidden symptoms, high infectivity and diverse transmission routes, as well as needle‐stick and other injuries from ‘sharps’ pose a great risk to the health of nurses (Liyew et al., 2020) that can cause them to suffer a great deal of stress and even fear.
In addition, to some extent the public's fear and prejudice against infectious diseases can be passed to nurses working in IDDs who not only care for patients with infectious illnesses, perform disease prevention and control and sanitize the environment and equipment but also respond directly to public health emergencies (Wan et al., 2022). For example, nurses form the backbone of increasingly successful HIV care delivery systems in many parts of the world, particularly in the most badly afflicted areas (Guilamo‐Ramos et al., 2021), and they play a vital role in social health care. Nevertheless, some scholars have found that nurses' quality of life is significantly related to job turnover caused by on‐the‐job stress (Hwang, 2022; Pang et al., 2020). Therefore, researchers may want to pay closer attention to the quality of life of nurses working in IDDs in order to find ways to decrease turnover and even expand the talent pool of nurses for IDDs in China and around the world.
1.1. Background
The World Health Organization defines quality of life as an individual's overall contentment with their objectives, expectations, standards and living conditions, as well as their general feelings about personal health, in diverse cultures and value systems (Lucas‐Carrasco, 2012; WHO, 1993). Quality of life is widely seen as a thorough assessment of an individual's or group's ability to adjust to physical, psychological and social factors. Nursing quality in IDDs is intimately linked to successful prevention and control of infectious diseases, and nurses' quality of life can significantly influence clinical nursing quality. Nurses in IDDs have greater direct contact with patients with infectious diseases (Remuzzi & Remuzzi, 2020), perform more invasive procedures and are more likely to be infected by blood or bodily fluids than nurses in other departments. Nurses in IDDs are also under more psychological stress than their general hospital counterparts, and their career prospects may be less optimistic, which can have a direct impact on a nursing team's stability. However, there are currently few studies on the quality of life of nurses working in IDDs, both in China and in other countries.
Social support has been recognized as an external protective force. Individuals with adequate social support can minimize psychological stress, relieve negative emotions, cope with stress more effectively (Goodyke et al., 2021; Shojaei et al., 2019) and adapt to society, all of which are important for their physical and mental health (Gonzalez‐Saenz de Tejada et al., 2017; Zhang, Wang, et al., 2021). Many studies have also shown that social support is positively related to quality of life (Alshahrani, 2020; Rambod & Rafii, 2010; Shojaei et al., 2019). Because of the unique nature of IDDs, some patients and their families have misconceptions about IDD nursing, and some family members of IDD nurses are even unwilling to support them in their careers. According to the study of (Li et al., 2020) that looked at 316 nurses in IDDs in Changsha, China, the level of social support for nurses is low, which can decrease their job satisfaction and negatively impact their career status. However, more analysis is needed to see if social support influences the quality of life of nurses in IDDs.
We propose psychological resilience as a mediator of social support's effects on quality of life based on the concept of positive psychology, which refers to an individual's ability to adapt positively to the environment when coping with negative events such as trauma, and which can mobilize psychological resources to face stress with a positive coping attitude, thus reducing its negative effects (Connor & Davidson, 2003; Smith et al., 2008). Psychological resilience is a positive feature that affects quality of life, and research has shown that people who have a high level of psychological resilience have a greater quality of life (Atay et al., 2021; Bermejo‐Toro et al., 2020; Franjić et al., 2021). Many factors influence psychological resilience, and social support is one of them (Huang et al., 2019).
According to Liu et al.'s research, nurses in IDDs are concerned about being infected with or transmitting the disease to their families, and most individuals suffer from anxiety that prevents them from efficiently dealing with work‐related stress (Li & Liu, 2011). In‐depth interviews with nurses who cared for 2019 patients with COVID‐19 were conducted by Huang et al., who discovered that these nurses had a low degree of psychological resilience in to begin with. Nurses self‐reported that they would have more confidence in their capacity to relieve stress if felt supported by family and friends (Chigwedere et al., 2021; Huang et al., 2021). Almazan et al.'s study of older adults who had survived disasters found that social support could help increase the psychological resilience of older adults in the face of disasters (Almazan et al., 2019). Because social support can improve psychological resilience, and psychological resilience is a positive factor on quality of life, psychological resilience may play a mediating role between social support and quality of life. However, research on this topic is scant for nurses in IDDs.
1.2. Study aims
Currently, in the context of COVID‐19, there is increasing public concern regarding nurses in IDDs, but there are few reports available on their quality of life. The aims of this study were (1) to understand the current situation of social support, psychological resilience and quality of life for nurses in IDDs in China; (2) to explore the correlation between quality of life, social support and psychological resilience; (3) to explore the mechanism of social support on quality of life and to explore the mediating role of psychological resilience (Figure 1).
FIGURE 1.
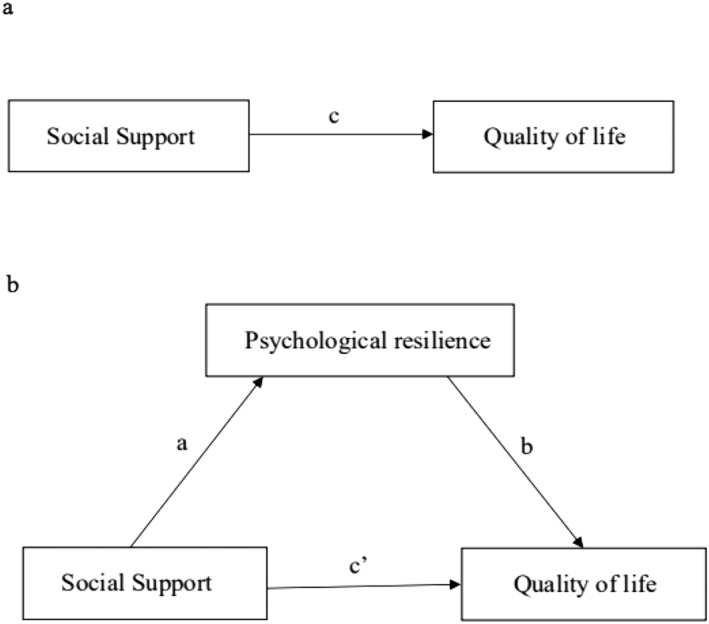
The conceptual mediation model relating psychological resilience, social support and quality of life
2. METHODS
2.1. Study design
This was a cross‐sectional study on Chinese IDD nurses' quality of life. From January to May 2021, using a convenience sampling method, 10 general hospitals with IDDs in the five provinces of Zhejiang, Yunnan, Chongqing, Shaanxi and Shanxi were selected from five regions in eastern, southern, western, northern and central China, respectively. With the assistance of hospital managers and head nurses, IDD nurses were asked to complete a questionnaire regarding social support, psychological resilience and quality of life. Nurses were included in the study if they met the following criteria: (1) They were independently responsible for clinical nursing work in IDDs; (2) they were licensed registered nurses; and (3) they gave their informed consent and participated voluntarily. Exclusion criteria were (1) nurses who performed rotational study programmes and (2) nurses who were not on duty throughout the investigation due to sick leave, maternity leave or other reasons.
2.2. Setting and sample
A sample size of 10 to 15 times the number of questionnaire items was required by our chosen structural equation model (SEM) framework (Thompson, 2000; Xie et al., 2021). There were 67 items in total in this investigation. Therefore, the calculation formula for required sample size was N = (8 + 10 + 25 + 24) × 10 = 670, which meant that at least 670 participants were needed for this study. This target sample size was then expanded by 20% to account for incomplete questionnaires, lost samples and other factors, resulting in a final required sample size of at least 708 participants. Ultimately, a total of 866 nurses in IDDs who met the study inclusion and exclusion criteria participated in our survey.
2.3. Instruments
2.3.1. Demographic data questionnaire
We designed a general demographic data questionnaire that included questions for gender, age, educational background, professional title, employment type, marital status, child status and monthly income.
2.3.2. Social support rating scale
The social support rating scale (SSRS), which was compiled by Shuiyuan Xiao in 1994 (Xiao, 1994), was used to evaluate the level of social support of the nurses in our study. There are 10 items on this scale, with three dimensions: objective support, subjective support and utilization of social support. Questions 1–4 and 8–10 have four response options: A, B, C and D, which are worth 1–4 points, respectively. For example, ‘how many close friends do you have that you can get support and help from?’ Question 5 is ‘Support and care received from family members’ and is answered on a 4‐point scale ranging from 1 (none) to 4 (complete support). Question 6 is ‘What are the sources of help and financial support you have received when you have encountered difficulties?’, and it is assessed based on the number of options, which means number of sources of help. The total score for social support, which ranges from 1 to 66, is the sum of the 10 items on the scale, and the higher the overall score, the higher the level of social support. In this study, the Cronbach's α of the scale was 0.738.
2.3.3. Connor‐Davidson resilience scale
The Connor‐Davidson resilience scale (CD‐RISC) was used to assess psychological resilience (Connor & Davidson, 2003). In this study, the Chinese version of the CD‐RISC was used, which was translated and adapted by Xiaonan Yu and Jianxin Zhang (Yu & Zhang, 2007). There are 25 items on the scale, with three dimensions: strength, tenacity and optimism. Example items are ‘under pressure, I can concentrate and think clearly’, and ‘I believe I'm a powerful person’, which can be answered on a 5‐point scale ranging from 0 (never) to 4 (nearly often). The higher the score, the higher the level of psychological resilience. In this study, the Cronbach's α of the scale was 0.937.
2.3.4. World Health Organization quality of life brief scale
The World Health Organization quality of life brief scale (WHOQOL‐BREF) scale, which was translated into Chinese and revised by Yuantao Hao (Fang et al., 1999; WHO, 1998), was used to assess quality of life in this study. There are 26 items in this scale. The first two items measure the quality of life and self‐health from a subjective point of view. The last 24 items are divided into four dimensions: physical, psychological, social relations and environmental. Example items include ‘Are you satisfied with your interpersonal relationships?’, and ‘Do you think your life is meaningful?’, which are answered on a 5‐point scale from 1 (strongly agree) to 5 (strongly disagree). The total score is the average score of each dimension multiplied by four, and the higher the score, the better the quality of life. In this study, the Cronbach's α of this scale was 0.929.
2.4. Data collection
With the consent of the managers of each of the IDDs, field researchers used the time after staff meetings to explain the purpose of our research, its significance and matters needing attention to the survey subjects. The questionnaire took about 20–30 min to complete, and the researchers collected it on the spot. We disseminated a total of 866 questionnaires and retrieved 845 completed questionnaires with a recovery rate of 97.6%.
2.5. Data analysis
For data analysis and structural equation modelling, we utilized IBM SPSS Statistics 26.0 and Mplus 8.3 and employed the standard approach to check the results' validity. The demographic and medical features of the participants, as well as their levels of social support, psychological resilience and quality of life, were described using descriptive statistics (frequency, percentage, mean and standard deviation). The relationship between social support, psychological resilience and quality of life was investigated using Pearson correlation analysis. We built the SEM using Mplus 8.3, used full information maximum likelihood to estimate the relationship and parameters between variables. Finally, we investigated the mediating effect of psychological resilience on social support and quality of life using a bootstrap to test and validate the mediation effect, with a (two‐tailed) significance threshold of p < .05.
2.6. Ethical considerations
The study was submitted to the ethics committee of the first author's institution Xijing Hospital. Before the questionnaire survey, the field researchers explained the purpose, significance and precautions of the study to the respondents. The researcher distributed the questionnaire only after receiving each nurse's informed written consent. The questionnaire was conducted anonymously, and respondents had the option to withdraw at any time. Respondents' information was protected, and all data collected was limited to sue only in this study.
3. RESULTS
3.1. Participant features
A total of 845 nurses were included in the study, of which 823 (97.4%) were female and 22 (2.6%) were male. The average age of the respondents was 33.04 years old (SD = 6.65; ranging from 21 to 58 years old), and the average years on the job was 11.05 years (SD = 7.44; ranging from 3 months to 40 years). General data are shown in Table 1.
TABLE 1.
General information of surveyed nurses [N = 845, case (percentage, %)]
| Variable | Category | N | % |
|---|---|---|---|
| Gender | |||
| Male | 22 | 2.6 | |
| Female | 823 | 97.4 | |
| Educational background | |||
| Junior college and below | 196 | 23.2 | |
| Undergraduate | 646 | 76.4 | |
| Master's degree and above | 3 | 0.4 | |
| Professional title | |||
| Junior | 142 | 16.8 | |
| Middle | 376 | 44.5 | |
| Senior | 327 | 38.7 | |
| Employment type | |||
| Contract | 629 | 74.4 | |
| Permanent | 170 | 20.2 | |
| Other | 46 | 5.4 | |
| Marital status | |||
| Unmarried | 201 | 23.8 | |
| Married | 627 | 74.2 | |
| Divorced | 15 | 1.8 | |
| Widowed | 2 | 0.2 | |
| Child status | |||
| Have a child | 561 | 66.4 | |
| Not have a child | 284 | 33.6 | |
| Monthly income (RMB) | |||
| ≤3000 | 72 | 8.5 | |
| 3001–5000 | 330 | 39.1 | |
| 5001–8000 | 324 | 38.3 | |
| ≥8001 | 119 | 14.1 |
3.2. Means, standard deviations and correlations among variables
Table 2 shows the means, standard deviations and correlations among the variables. The total scores of social support, psychological resilience and quality of life were 36.36 ± 7.64, 55.88 ± 14.77 and 51.98 ± 8.72, respectively. Quality of life was positively correlated both with social support and psychological resilience (r = 0.521, 0.583, p < .01 for both, respectively), and psychological resilience was positively correlated with social support (r = 0.426, p < .01).
TABLE 2.
Means, standard deviations (SD) and correlations among variables
| Variables | Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Social support | 36.36(7.64) | 1 | ||||||||||||
| 2.Objective support | 9.49(3.31) | 0.814 ** | 1 | |||||||||||
| 3.Subjective support | 19.47(4.48) | 0.894 ** | 0.544 ** | 1 | ||||||||||
| 4.Utilization of social support | 7.39(1.79) | 0.531 ** | 0.268 ** | 0.309 ** | 1 | |||||||||
| 5.Psychological resilience | 55.88(14.77) | 0.426 ** | 0.261 ** | 0.404 ** | 0.326 ** | 1 | ||||||||
| 6.Strength | 19.68(5.05) | 0.372 ** | 0.224 ** | 0.350 ** | 0.299 ** | 0.918 ** | 1 | |||||||
| 7.Tenacity | 28.29(8.41) | 0.407 ** | 0.251 ** | 0.387 ** | 0.308 ** | 0.959 ** | 0.799 ** | 1 | ||||||
| 8.Optimism | 7.91(2.64) | 0.372 ** | 0.232 ** | 0.355 ** | 0.274 ** | 0.781 ** | 0.675 ** | 0.652 ** | 1 | |||||
| 9.Quality of life | 51.98(8.72) | 0.521 ** | 0.363 ** | 0.482 ** | 0.349 ** | 0.583 ** | 0.535 ** | 0.558 ** | 0.459 ** | 1 | ||||
| 10.Physical | 12.63(2.04) | 0.455 ** | 0.306 ** | 0.422 ** | 0.321 ** | 0.552 ** | 0.522 ** | 0.529 ** | 0.406 ** | 0.859 ** | 1 | |||
| 11.Psychological | 13.51(2.75) | 0.485 ** | 0.329 ** | 0.452 ** | 0.333 ** | 0.562 ** | 0.523 ** | 0.533 ** | 0.444 ** | 0.912 ** | 0.750 ** | 1 | ||
| 12.Social relationship | 13.67(2.69) | 0.438 ** | 0.323 ** | 0.411 ** | 0.248 ** | 0.416 ** | 0.370 ** | 0.406 ** | 0.329 ** | 0.839 ** | 0.613 ** | 0.656 ** | 1 | |
| 13.Environment | 12.17(2.49) | 0.443 ** | 0.308 ** | 0.399 ** | 0.325 ** | 0.519 ** | 0.471 ** | 0.494 ** | 0.430 ** | 0.886 ** | 0.699 ** | 0.768 ** | 0.631 ** | 1 |
Note: N = 845.
p < 0.01.
3.3. SEM results
To test if our selected survey had a common method deviation, we applied Harman's one‐factor test. All items for social support, psychological resilience and quality of life were included and nonrotation factor analysis was carried out. As a result, 12 common factors with characteristic roots greater than one were extracted, with the first common factor explaining 25.67% of the variation rate, which is less than the critical value of 40%, indicating that there was no serious common method deviation in this study and that the data can be further analysed reliably.
We used Mplus 8.3 to establish a SEM to investigate the mediating effect of nurses' psychological resilience on the link between social support and quality of life. We used maximum likelihood to estimate the parameters of the following model: The statistical measures used were the chi‐square test (χ 2), the comparative fit index (CFI), the Tucker‐Lewis index (TLI), the root mean square error of approximation (RMSER) and the standardized root mean square residual (SRMR). The fitting index results of this model were as follows: χ 2/df = 2.830 (<5.0), CFI = 0.987 (>0.80), TLI = 0.982 (>0.80), SRMR = 0.037 (≤0.08), RMSEA = 0.046 (<0.05), and the above indices were all within their prescribed ranges, indicating that the model fit the data well (Koo et al., 2021; Martynova et al., 2018).
We used a bootstrap for deviation correction to calculate the confidence intervals of the intermediary effect to further test its significance. We carried out 1000 self‐weighting samples, and the results showed that the path coefficient 95% CI was 0.185 to 0.280 and that the interval did not include 0, suggesting that psychological resilience indeed played a mediating role in the relationship between social support and quality of life.
Table 3 shows that social support had a direct positive effect on quality of life (β = 0.398, p < .001) and that social support played a partly mediating role on quality of life through psychological elasticity (β = 0.233, p < .001). The total effect of social support on quality of life was 0.631 (p < .001), with the psychological elasticity mediating effect accounting for 37% of the total effect. The mediation model between quality of life, social support and psychological resilience is depicted in Figure 2.
TABLE 3.
Direct and indirect effects for the SEM model
| Model pathways | Standardized effect(β) | SE | 95% CI LL | 95% CI UL | p |
|---|---|---|---|---|---|
| Direct effect | |||||
| Social support → quality of life | 0.398 | 0.040 | 0.319 | 0.478 | <.001 |
| Indirect effect | |||||
| Social support → psychological resilience → quality of life | 0.233 | 0.024 | 0.185 | 0.280 | <.001 |
| Total effect | |||||
| Social support → quality of life | 0.631 | 0.033 | 0.566 | 0.696 | <.001 |
Abbreviations: LL, lower limit; SE, standardized error; UL, upper limit.
FIGURE 2.
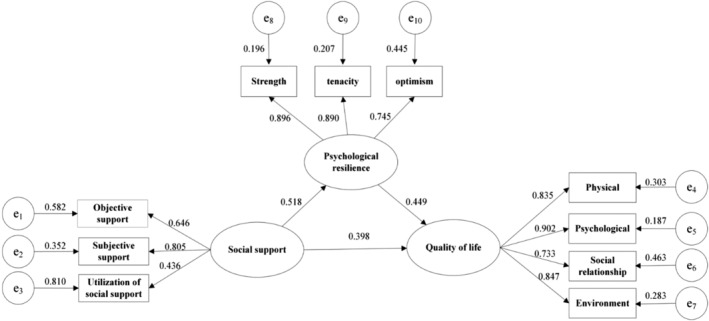
Mediation model. The final SEM model has adequate fit to the data. All the coefficients in this figure are standardized and significant at p < .05. Abbreviation: e1–e3, manifest variables of the three dimensions of social support; e4–e7, manifest variables of the three dimensions of quality of life; e8–e10, manifest variables of the three dimensions of psychological resilience
4. DISCUSSION
4.1. Levels of social support, psychological resilience and quality of life
The above results show that nurses in IDDs had a middle level of social support, which is similar to the findings of Li et al. (Li et al., 2020) but significantly lower than Shen's analysis of neonatal nurses (t = −16.089, p < .001) (Shen et al., 2022). We propose the following possible explanations for our results: (1) The IDD nurses may be overworked. As a group they expressed a strong desire for their departments to meet their needs, indicating that objective support could be improved (Li et al., 2020). The rate of job burnout among Chinese nurses in general is as high as 50% (Zhang, Miao, et al., 2021), and it may be difficult to get more support and understanding from family members when nurses are unable to strike a balance between job and family life. (2) Nurses have a lower amount of social prestige than physicians in the general public's view (Feng et al., 2017; Zhou et al., 2015). Because there is a lack of public understanding about infectious diseases, many people are afraid of being infected. Nurses' families and friends may even distance themselves from the nurses to some extent as a result of the nurses' long‐term contact with patients with infectious diseases, which can put nurses under a lot of stress. However, in the wake of COVID‐19, the public has gradually begun to pay more respect to front‐line medical staff, resulting in nurses receiving more support from society and their families.
The psychological resilience of nurses in IDDs was at the middle level, which was considerably lower than the results of Leng et al.'s study on 2981 nurses from a university‐affiliated hospital in China (t = −10.766, p < .001) (Leng et al., 2020). Our findings showed that most nurses in IDDs lacked strong resolve and an upbeat attitude in the face of challenges and that they were not adept at dealing with situations in a positive light. We speculate that this could be caused by any of the following reasons: (1) The infectious diseases treated in general hospitals are diverse and complex; nurses have long‐term direct contact with infectious disease patients, and their occupational exposure risk is significant, which can be great sources of worry; (2) the use of isolation and protective equipment makes nursing operations more complicated, and this can impact nurses' sense of accomplishment at work; and (3) nurses in IDDs in China must not only care for patients' illnesses but must also disinfect and isolate wards, as well as provide health education to patients' families. In addition, they must respond to epidemics that occur unexpectedly. Nurses' enthusiasm for their jobs may wane as a result of these heavy workloads, negatively impacting their psychological resilience.
The quality of life of nurses in IDDs is in the middle level, which was significantly lower than the quality of life of the Brazilian nurse practitioners studied by Caliari et al. (t = −16.030, p < .001) (Caliari et al., 2021), and for this, we offer the following are possible explanations: (1) The clinical nursing workload in China is currently substantial due to a nurse shortage and the unique nature of IDDs. Nurses often must also pay attention to psychological nursing for patients and their families because patients with infectious diseases are more sensitive to anxiety, depression and other negative feelings (Chen et al., 2021; Freeland et al., 2021). (2) In addition, the nurses' jobs are made more difficult to perform by the need to don a variety of protective equipment. (3) In IDDs, there are numerous isolation wards, and nurses' everyday work environment is relatively independent, reducing communication between them and their coworkers in a manner that can negatively affect interpersonal communication. (4) The decrease in nurses' participation in leisure and recreational activities can also have an impact on the development of interpersonal and social relationships among nurses, as well as their sense of well‐being and quality of life.
4.2. The correlations of quality of life, social support and psychological resilience
Our correlation results show that quality of life of nurses in IDDs was positively correlated with social support and its various dimensions. The higher the social support, the higher the quality of life, which is consistent with the existing relevant research results (Iwanowicz‐Palus et al., 2021; Zhou et al., 2022). Nurses' quality of life may improve if they can obtain sufficient material support in their work and life, as well as good social relationships with others. Furthermore, because of the unique nature of the IDD working environment, if nurses can receive and feel support and respect from family, friends and managers, they may achieve enough subjective support to help them realize a greater sense of self‐worth and may be more motivated and efficient in their work.
Social support can help to reduce job burnout in nurses (Velando‐Soriano et al., 2020) and enhance their job and life satisfaction (Khatatbeh et al., 2021), thus improving quality of life. Moreover, social support is a two‐way street. Nurses should not only accept and appreciate others' assistance and support but also actively provide it. Establishing good social relationships and cultivating an atmosphere of mutual assistance can help to improve quality of life.
The quality of life and psychological resilience of nurses in IDDs had a positive correlation, indicating that the higher the level of psychological resilience, the better the quality of life, and this is consistent with the findings of (Keener et al., 2021). The higher the level of psychological resilience, the stronger the ability to mobilize psychological resources and the greater the capacity for psychological adjustment (Tay & Lim, 2020). Nurses in IDDs play a vital role in epidemic prevention during periods of abrupt and novel infectious illnesses. Compared with nurses in general departments, they have more frequent contact with infected patients and have a higher chance of occupational exposure, which puts them under more psychological stress. According to Juzhe Xi et al. (Xi et al., 2008), psychological resilience serves as a stress buffer, meaning that people with higher psychological resilience have more tenacity and optimism and are better able to face difficulties bravely and to alleviate the negative effects of pressure and adversity (Wermelinger Ávila et al., 2017). Such people may also experience a more profound sense of work accomplishment and life satisfaction. Nurses with greater psychological resilience, as well as with more positive attitudes, may also motivate and influence those around them. They are also more likely to be liked by others in work and life, which helps to build social relationships, and this all helps to enhance their quality of life.
Psychological resilience was also positively correlated to social support; the higher the level of social support, the greater the psychological resilience. Such a finding is also consistent with that of other researchers (Kılınç & Sis Çelik, 2021; Zhang et al., 2017). The level of psychological resilience had the strongest correlation to subjective support of any variable in this study. Our results show that nurses in IDDs had a high demand for the emotional experiences of respect, support and understanding from people from all walks of life, which had a significant impact on their psychological resilience. Nurses feel greater self‐worth and are more driven to work if they receive more social support. When faced with difficulties, such nurses are better able to solve them optimistically, thus reducing the formation of negative emotions (Lee & Kang, 2020).
4.3. The predictive ability of social support on quality of life and the mediating role of psychological resilience
The results of our mediating effect analysis show that nurses' social support had a direct positive predictive influence on their quality of life and that psychological resilience had a partial mediating effect between social support and quality of life. The higher the level of social support, the better the psychological resilience and the higher the quality of life. The reasons for this relationship may be as follows: (1) The higher the level of social support, the more likely a nurse may be to feel understanding and respect from friends, family and colleagues, and the more likely, the nurse may be to utilize the assistance provided by the support to the fullest. All of these factors contribute to nurses' increased confidence and courage in the face of adversity and to their ability to successfully regulate pressure, enhancing their psychological resilience. (2) Nurses who have a higher level of psychological resilience may be more willing to take on more difficult tasks at work, such as participating in anti‐epidemic initiatives.
4.4. Limitations and recommendations
There are some limitations to this study. First, this study used a cross‐sectional survey to analyse the quality of life of nurses, and we made no attempt to discern the causal relationship between variables. We suggest that randomized controlled trials should be used in future studies to test the effectiveness of psychological resilience and social support intervention in improving IDD nurse quality of life. Second, this study explored the effects of psychological resilience and social support on quality of life. The various other factors that may affect quality of life are not considered comprehensively, and more factors should be included in future studies in order to analyse the quality of life more comprehensively.
5. CONCLUSIONS
Nurses in IDDs have a middle level of social support, psychological resilience and quality of life, and we believe efforts should be made to improve this. We also found that social support can directly or indirectly affect nurses' quality of life through psychological resilience so that in general, enhancing the social support and psychological resilience of nurses in IDDs can help to improve their quality of life. Improved quality of life may in turn improve their clinical job performance and thus help with prevention and treatment of sudden epidemics.
6. IMPLICATIONS FOR NURSING MANAGEMENT
IDD nursing managers should pay special attention to the mental health and quality of life of their nurses and provide adequate social support. They should strengthen humanized management, focusing more attention on people‐oriented management and support the material and emotional needs of nurses. Managers should develop reasonable incentives, flexible scheduling and reduced the workloads for nurses. They should also create more opportunities for continuing education and learning in order for nurses to realize their full career potential. Managers should establish a certain level of contact with nurses' family members, encouraging family members to support, understand and respect the work of the nurses.
Managers should also pay attention to the key role of psychological resilience as a mediator in improving nurses' quality of life, by organizing positive psychology knowledge lectures to help nurses cultivate confidence and positive attitudes and improve their ability to self‐regulate their emotional state. By setting up sessions for exchanging experiences, junior nurses will be better able to cope with stress and negative emotions and strike a balance between work and life. These sessions will be led by experienced nurses with high levels of psychological resilience. Good communication channel with nurses is beneficial for the release of their emotions and stress, and for understanding the psychological needs of nurses, both of which can improve their job satisfaction and happiness.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
This study was conducted under ethical guidelines described in the Helsinki Declaration and the standards of the institution and national research committee. This study received ethical approval from the ethics committee of Xijing Hospital of Fourth Military Medical University (KY20192028‐F‐2).
AUTHOR CONTRIBUTIONS
Jiaran Yan and Chao Wu contributed equally to the research design, analysis and interpretation of the data and drafting. Chunyan He, Yawei Lin, Shizhe He and Yanling Du contributed to distribute and withdrew the questionnaires and validation of the data. Baohua Cao contributed to design the research and provide guidance from the perspective of statistics. Hongjuan Lang supervised the project and contributed to conception and design of the study, critical revision and final approval of the manuscript.
ACKNOWLEDGEMENTS
The authors thank managers of infectious disease departments of general hospitals for organization and coordination.
Yan, J. , Wu, C. , He, C. , Lin, Y. , He, S. , Du, Y. , Cao, B. , & Lang, H. (2022). The social support, psychological resilience and quality of life of nurses in infectious disease departments in China: A mediated model. Journal of Nursing Management, 30(8), 4503–4513. 10.1111/jonm.13889
Jiaran Yan and Chao Wu contributed equally to this work.
Contributor Information
Baohua Cao, Email: cbh528@fmmu.edu.cn.
Hongjuan Lang, Email: langhj@fmmu.edu.cn.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Almazan, J. U. , Albougami, A. S. , Alamri, M. S. , Colet, P. C. , Adolfo, C. S. , Allen, K. , Gravoso, R. , & Boyle, C. (2019). Disaster‐related resiliency theory among older adults who survived typhoon Haiyan. International Journal of Disaster Risk Reduction, 35, 101070. 10.1016/j.ijdrr.2019.101070 [DOI] [Google Scholar]
- Alshahrani, A. M. (2020). Quality of life and social support: Perspectives of Saudi Arabian stroke survivors. Science Progress, 103(3), 36850420947603. 10.1177/0036850420947603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atay, N. , Sahin, G. , & Buzlu, S. (2021). The relationship between psychological resilience and professional quality of life in nurses. Journal of Psychosocial Nursing and Mental Health Services, 59(6), 31–36. 10.3928/02793695-20210218-01 [DOI] [PubMed] [Google Scholar]
- Bermejo‐Toro, L. , Sánchez‐Izquierdo, M. , Calvete, E. , & Roldán, M. A. (2020). Quality of life, psychological well‐being, and resilience in caregivers of people with acquired brain injury (ABI). Brain Injury, 34(4), 480–488. 10.1080/02699052.2020.1725127 [DOI] [PubMed] [Google Scholar]
- Caliari, J. S. , Santos, M. A. D. , Andrechuk, C. R. S. , Campos, K. R. C. , Ceolim, M. F. , & Pereira, F. H. (2021). Quality of life of nurse practitioners during the COVID‐19 pandemic. Revista Brasileira de Enfermagem, 75(suppl 1), e20201382. 10.1590/0034-7167-2020-1382 [DOI] [PubMed] [Google Scholar]
- Chen, F. , Pang, X. , & Dai, X. (2021). Effect of comprehensive nursing on the pain, anxiety and malnutrition of hepatitis B patients. American Journal of Translational Research, 13(5), 4656–4665. https://www.ncbi.nlm.nih.gov/pubmed/34150045 [PMC free article] [PubMed] [Google Scholar]
- Chigwedere, O. C. , Sadath, A. , Kabir, Z. , & Arensman, E. (2021). The impact of epidemics and pandemics on the mental health of healthcare workers: A systematic review. International Journal of Environmental Research and Public Health, 18(13). 10.3390/ijerph18136695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor, K. M. , & Davidson, J. R. (2003). Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Fang, J. , Hao, Y. , & Li, C. (1999). Reliability and validity for Chinese version of WHO quality of life scale. Chinese Mental Health Journal, 04, 203–205. [Google Scholar]
- Feng, D. , Su, S. , Yang, Y. , Xia, J. , & Su, Y. (2017). Job satisfaction mediates subjective social status and turnover intention among Chinese nurses. Nursing and Health Sciences, 19(3), 388–392. 10.1111/nhs.12357 [DOI] [PubMed] [Google Scholar]
- Franjić, D. , Babić, D. , Marijanović, I. , & Martinac, M. (2021). Association between resilience and quality of life in patients with colon cancer. Psychiatria Danubina, 33(Suppl 13), 297–303. https://www.ncbi.nlm.nih.gov/pubmed/35150498 [PubMed] [Google Scholar]
- Freeland, C. , Racho, R. , Kamischke, M. , Moraras, K. , Wang, E. , Cohen, C. , & Kendrick, S. (2021). Health‐related quality of life for adults living with hepatitis B in the United States: A qualitative assessment. Journal of Patient‐Reported Outcomes, 5(1), 121. 10.1186/s41687-021-00398-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez‐Saenz de Tejada, M. , Bilbao, A. , Baré, M. , Briones, E. , Sarasqueta, C. , Quintana, J. M. , & Escobar, A. (2017). Association between social support, functional status, and change in health‐related quality of life and changes in anxiety and depression in colorectal cancer patients. Psycho‐Oncology, 26(9), 1263–1269. 10.1002/pon.4303 [DOI] [PubMed] [Google Scholar]
- Goodyke, M. P. , Hershberger, P. E. , Bronas, U. G. , & Dunn, S. L. (2021). Perceived social support and heart rate variability: An integrative review. Western Journal of Nursing Research, 44, 1057–1067. 10.1177/01939459211028908 [DOI] [PubMed] [Google Scholar]
- Guilamo‐Ramos, V. , Thimm‐Kaiser, M. , Benzekri, A. , Hidalgo, A. , Lanier, Y. , Tlou, S. , De Lourdes Rosas López, M. , Soletti, A. B. , & Hagan, H. (2021). Nurses at the frontline of public health emergency preparedness and response: Lessons learned from the HIV/AIDS pandemic and emerging infectious disease outbreaks. The Lancet Infectious Diseases, 21(10), e326–e333. 10.1016/s1473-3099(20)30983-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, F. , Lin, M. , Sun, W. , Zhang, L. , Lu, H. , & Chen, W.‐T. (2021). Resilience of frontline nurses during the COVID pandemic in China: A qualitative study. Nursing and Health Sciences, 23(3), 639–645. 10.1111/nhs.12859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. , Huang, Y. , Bao, M. , Zheng, S. , Du, T. , & Wu, K. (2019). Psychological resilience of women after breast cancer surgery: A cross‐sectional study of associated influencing factors. Psychology, Health & Medicine, 24(7), 866–878. 10.1080/13548506.2019.1574353 [DOI] [PubMed] [Google Scholar]
- Hwang, E. (2022). Factors affecting the quality of work life of nurses at tertiary general hospitals in the context of the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 19(8), 4718. 10.3390/ijerph19084718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwanowicz‐Palus, G. , Mróz, M. , & Bień, A. (2021). Quality of life, social support and self‐efficacy in women after a miscarriage. Health and Quality of Life Outcomes, 19(1), 16. 10.1186/s12955-020-01662-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keener, T. A. , Hall, K. , Wang, K. , Hulsey, T. , & Piamjariyakul, U. (2021). Relationship of quality of life, resilience, and associated factors among nursing faculty during COVID‐19. Nurse Educator, 46(1), 17–22. 10.1097/nne.0000000000000926 [DOI] [PubMed] [Google Scholar]
- Khatatbeh, H. , Al‐Dwaikat, T. , Oláh, A. , Onchonga, D. , Hammoud, S. , Amer, F. , Prémusz, V. , & Pakai, A. (2021). The relationships between paediatric nurses' social support, job satisfaction and patient adverse events. Nursing Open, 8(6), 3575–3582. 10.1002/nop2.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kılınç, T. , & Sis Çelik, A. (2021). Relationship between the social support and psychological resilience levels perceived by nurses during the COVID‐19 pandemic: A study from Turkey. Perspectives in Psychiatric Care, 57(3), 1000–1008. 10.1111/ppc.12648 [DOI] [PubMed] [Google Scholar]
- Koo, B. , Lee, K.‐S. , & Khojasteh, J. (2021). An introduction to multilevel modeling techniques (4th edition). Structural Equation Modeling‐a Multidisciplinary Journal, 28(1), 162–164. 10.1080/10705511.2020.1815539 [DOI] [Google Scholar]
- Lee, J. , & Kang, S. J. (2020). Factors influencing nurses' intention to care for patients with emerging infectious diseases: Application of the theory of planned behavior. Nursing and Health Sciences, 22(1), 82–90. 10.1111/nhs.12652 [DOI] [PubMed] [Google Scholar]
- Leng, M. , Xiu, H. , Yu, P. , Feng, J. , Wei, Y. , Cui, Y. , Zhang, M. , Zhou, Y. , & Wei, H. (2020). Current state and influencing factors of nurse resilience and perceived job‐related stressors. Journal of Continuing Education in Nursing, 51(3), 132–137. 10.3928/00220124-20200216-08 [DOI] [PubMed] [Google Scholar]
- Li, H. , Yuan, S. , Chen, J. , Zeng, L. , Li, Y. , & Li, H. (2020). A path analysis of impacts of psychological capital and social support on career status among nurses in the infection wards of tertiary hospitals. Chinese Journal of Nursing Education, 17(6), 556–560. 1672‐9234(2020)17:6<556:Xlzbhs>2.0.Tx;2‐s. <Go to ISI>://CSCD:6751393 [Google Scholar]
- Li, S. , & Liu, C. (2011). Investigation of the anxiety in nurses in department of infectious diseases. Chinese Journal of Nosocomiology, 21(16), 3418–3419. 1005‐4529(2011)21:16<3418:Grxjbk>2.0.Tx;2‐c. <Go to ISI>://CSCD:4286092 [Google Scholar]
- Liyew, B. , Sultan, M. , Michael, M. , Tilahun, A. D. , & Kassew, T. (2020). Magnitude and determinants of Needlestick and sharp injuries among nurses working in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. BioMed Research International, 2020, 6295841. 10.1155/2020/6295841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas‐Carrasco, R. (2012). The WHO quality of life (WHOQOL) questionnaire: Spanish development and validation studies. Quality of Life Research, 21(1), 161–165. 10.1007/s11136-011-9926-3 [DOI] [PubMed] [Google Scholar]
- Martynova, E. , West, S. G. , & Liu, Y. (2018). Principles and practice of structural equation modeling. Structural Equation Modeling‐a Multidisciplinary Journal, 25(2), 325–329. 10.1080/10705511.2017.1401932 [DOI] [Google Scholar]
- NHC . (2022, 05/10/). China: Policy Interpretation of 'National Nursing Development Plan (2021–2025)'. https://search.ebscohost.com/login.aspx?direct=true&db=edsgit&AN=edsgit.A703153722&lang=zh‐cn&site=eds‐live
- Pang, Y. , Dan, H. , Jung, H. , Bae, N. , & Kim, O. (2020). Depressive symptoms, professional quality of life and turnover intention in Korean nurses. International Nursing Review, 67(3), 387–394. 10.1111/inr.12600 [DOI] [PubMed] [Google Scholar]
- Rambod, M. , & Rafii, F. (2010). Perceived social support and quality of life in Iranian hemodialysis patients. Journal of Nursing Scholarship, 42(3), 242–249. 10.1111/j.1547-5069.2010.01353.x [DOI] [PubMed] [Google Scholar]
- Remuzzi, A. , & Remuzzi, G. (2020). COVID‐19 and Italy: What next? The Lancet, 395(10231), 1225–1228. 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen, Y. J. , Wei, L. , Li, Q. , Li, L. Q. , & Zhang, X. H. (2022). Mental health and social support among nurses during the COVID‐19 pandemic. Psychology, Health & Medicine, 27(2), 444–452. 10.1080/13548506.2021.1944653 [DOI] [PubMed] [Google Scholar]
- Shojaei, F. , Puryaghoob, M. , Babahaji, M. , Rezaei, S. G. , & Jafari, S. (2019). The relationship between quality of life and social support among nurses: A cross‐sectional study. Industrial Psychiatry Journal, 28(2), 242–247. 10.4103/ipj.ipj_29_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, B. W. , Dalen, J. , Wiggins, K. , Tooley, E. , Christopher, P. , & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Tay, P. K. C. , & Lim, K. K. (2020). Psychological resilience as an emergent characteristic for well‐being: A pragmatic view. Gerontology, 66(5), 476–483. 10.1159/000509210 [DOI] [PubMed] [Google Scholar]
- Thompson, B. (2000). Ten commandments of structural equation modeling. In Reading and understanding more multivariate statistics (pp. 261–283). [Google Scholar]
- Velando‐Soriano, A. , Ortega‐Campos, E. , Gómez‐Urquiza, J. L. , Ramírez‐Baena, L. , De La Fuente, E. I. , & Cañadas‐De La Fuente, G. A. (2020). Impact of social support in preventing burnout syndrome in nurses: A systematic review. Japan Journal of Nursing Science, 17(1), e12269. 10.1111/jjns.12269 [DOI] [PubMed] [Google Scholar]
- Wan, Z. , Lian, M. , Ma, H. , Cai, Z. , & Xianyu, Y. (2022). Factors associated with burnout among Chinese nurses during COVID‐19 epidemic: A cross‐sectional study. BMC Nursing, 21(1), 51. 10.1186/s12912-022-00831-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wermelinger Ávila, M. P. , Lucchetti, A. L. , & Lucchetti, G. (2017). Association between depression and resilience in older adults: A systematic review and meta‐analysis. International Journal of Geriatric Psychiatry, 32(3), 237–246. 10.1002/gps.4619 [DOI] [PubMed] [Google Scholar]
- WHO . (1993). Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Quality of Life Research, 2(2), 153–159. https://www.ncbi.nlm.nih.gov/pubmed/8518769. 10.1007/BF00435734 [DOI] [PubMed] [Google Scholar]
- WHO . (1998). Development of the World Health Organization WHOQOL‐BREF quality of life assessment. The WHOQOL group. Psychological Medicine, 28(3), 551–558. 10.1017/s0033291798006667 [DOI] [PubMed] [Google Scholar]
- Xi, J. , Sang, B. , & Zuo, Z. (2008). Review and Prospect of resilience research. Psychological Science, 31(4) 995‐998+977. 10.16719/j.cnki.1671-6981.2008.04.044 [DOI] [Google Scholar]
- Xiao, S. (1994). The theoretical basis and application of social support scale. Journal of Clinical Psychological Medicine, 4(2), 98–100. [Google Scholar]
- Xie, C. , Li, X. , Zeng, Y. , & Hu, X. (2021). Mindfulness, emotional intelligence and occupational burnout in intensive care nurses: A mediating effect model. Journal of Nursing Management, 29(3), 535–542. 10.1111/jonm.13193 [DOI] [PubMed] [Google Scholar]
- Yu, X. , & Zhang, J. (2007). A comparison between the Chinese version of ego‐resiliency scale and Connor‐Davidson resilience scale. Psychological Science, 30(5), 1169–1171. 10.3969/j.issn.1671-6981.2007.05.038 [DOI] [Google Scholar]
- Zakeri, M. A. , Rahiminezhad, E. , Salehi, F. , Ganjeh, H. , & Dehghan, M. (2021). Burnout, anxiety, stress, and depression among Iranian nurses: Before and during the first wave of the COVID‐19 pandemic. Frontiers in Psychology, 12, 789737. 10.3389/fpsyg.2021.789737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, D. , Wang, R. , Zhao, X. , Zhang, J. , Jia, J. , Su, Y. , & Wang, K. (2021). Role of resilience and social support in the relationship between loneliness and suicidal ideation among Chinese nursing home residents. Aging and Mental Health, 25(7), 1262–1272. 10.1080/13607863.2020.1786798 [DOI] [PubMed] [Google Scholar]
- Zhang, H. , Zhao, Q. , Cao, P. , & Ren, G. (2017). Resilience and quality of life: Exploring the mediator role of social support in patients with breast cancer. Medical Science Monitor, 23, 5969–5979. 10.12659/msm.907730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W. , Miao, R. , Tang, J. , Su, Q. , Aung, L. H. H. , Pi, H. , & Sai, X. (2021). Burnout in nurses working in China: A national questionnaire survey. International Journal of Nursing Practice, 27(6), e12908. 10.1111/ijn.12908 [DOI] [PubMed] [Google Scholar]
- Zhou, K. , Ning, F. , Wang, X. , Wang, W. , Han, D. , & Li, X. (2022). Perceived social support and coping style as mediators between resilience and health‐related quality of life in women newly diagnosed with breast cancer: A cross‐sectional study. BMC Women's Health, 22(1), 198. 10.1186/s12905-022-01783-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, W. , He, G. , Wang, H. , He, Y. , Yuan, Q. , & Liu, D. (2015). Job dissatisfaction and burnout of nurses in Hunan, China: A cross‐sectional survey. Nursing and Health Sciences, 17(4), 444–450. 10.1111/nhs.12213 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


