Abstract
Objective
To investigate women's perspectives on the quality of maternal and newborn care (QMNC) around the time of childbirth during the COVID‐19 pandemic in Latvia, comparing the years 2020 and 2021, among women who went into labor or had a prelabor cesarean.
Methods
Women giving birth in healthcare facilities in Latvia from March 1, 2020, to October 28, 2021, answered an online questionnaire including 40 WHO standards‐based quality measures. Descriptive and multivariate quantile regression analyses were performed to compare QMNC in 2020 and 2021.
Results
2079 women were included in the analysis: 1860 women who went into labor (group 1) and 219 with prelabor cesarean (group 2). Among group 1, 66.4% (n = 99/149) of women received fundal pressure in an instrumental vaginal birth, 43.5% (n = 810) lacked involvement in choices, 17.4% (n = 317) reported suffering abuse, 32.7% (n = 609) reported inadequate breastfeeding support while 5.2% (n = 96) lack of early breastfeeding. A significant reduction in QMNC due to the COVID‐19 pandemic was reported by 29.5% (n = 219) and 25.0% (n = 270) of respondents in 2020 and 2021, respectively (P = 0.045). Multivariate analyses highlighted a significantly lower QMNC index for 2020 compared with 2021 (P < 0.001).
Conclusion
This first study investigating QMNC in Latvia showed significant gaps in QMNC perceived by respondents, with slightly better results in 2021. Appropriate healthcare strategies to improve health care for women and newborns in Latvia are required.
ClinicalTrials.gov Identifier:NCT04847336.
Keywords: childbirth, COVID‐19, Eastern Europe, IMAgiNE EURO, Latvia, maternity care, newborn care, quality of care
Synopsis
This first study investigating the quality of maternal and newborn care in Latvia showed significant gaps in quality perceived by survey respondents, with slightly better results in 2021.
1. INTRODUCTION
In 2016, after a consultation period with an expert board, the World Health Organization (WHO) established a set of standards for improving maternal and newborn quality of care in health facilities. 1 The goal of adopting these criteria is to decrease maternal and perinatal mortality and morbidity and increase the frequency of positive experiences of respectful and evidence‐based health care. WHO emphasizes the importance of a woman‐centered childbirth environment in which mothers feel free, secure, and respected, with a low risk of traumatic experiences that can cause subsequent fear and mistrust in the healthcare system. 2 , 3
The first step in implementing the WHO standards is assessing the existing quality of care. However, like the majority of Central Eastern European (CEE) countries, Latvia lacks research that examines the quality of maternal and newborn care (QMNC) during childbirth in a comprehensive way (i.e. examining the different domains of quality of care) 4 and no studies have been conducted using the WHO standards as a framework for the analysis. 1
Latvia has a much higher maternal mortality rate than the rest of the European Union, with 19 maternal deaths per 100 000 live births in 2017 compared with the European average of 6 deaths per 100 000 births, 5 and low access to effective maternity care. 4 However, in terms of early neonatal and infant mortality, Latvia's indicators are closer in line with European data, with a reported early neonatal death rate of 1.8 per 1000 live births in 2019 compared with 2.8 per 1000 live births in the WHO European region, and an infant mortality rate of 3.4 per 1000 live births, which is the same as the average in the EU. 6 , 7 , 8 The cesarean rate in 2020 in Latvia was 22.2% 6 and it is one of the few European countries where the rate tends to decrease. 9 Although the average number of cesareans in the country is not high, the high proportion of operative births in small low‐risk maternity wards, as well as in primiparous women in Robson Group 1 (15.0%) and Robson Group 2 (33.2%) in 2020 in Latvia, 10 , 11 is a cause for concern.
For the last two decades, Latvia's health system has been reforming with ongoing continuous adjustments to overcome budget constraints and seek to improve maternity and newborn health care. 12 Latvia presently has a nationwide single‐payer health system that offers universal health care financed by general tax revenues 13 ; however, the country has one of the lowest health expenditure ratios in Europe, with a gross domestic product of 6.3% in 2017 12 compared with an average of 9.6% in Europe. 14 The current coverage plan provides access to a relatively broad range of healthcare services. Women in pregnancy and up to 70 days after childbirth and children aged under 18 years are legally exempt from paying fees for any of the healthcare services on the statutory list. However, due to lengthy waiting lists for medical procedures and consultations in the public system, patients—including pregnant women—frequently choose to pay out of pocket. 12 , 15
Since the WHO declared COVID‐19 a pandemic in March 2020, numerous changes have occurred in healthcare systems throughout Europe, adding a layer of complexity to maternal and newborn care. 16 Changes in the organization of care due to the COVID‐19 pandemic (e.g. use of personal protective equipment [PPE] during labor, reduced numbers of healthcare personnel, requirement for COVID‐19 testing, and increased risk of spread of intrahospital infections) were all factors that may have affected perceived quality of care during the pandemic. 17 , 18 , 19 Inappropriate practices, such as unnecessary separation of the baby from the mother and violations of women's rights, have also been documented during the pandemic. 20 , 21 , 22
IMAgiNE EURO is a multicountry study 23 aimed at understanding women's perspectives on the quality of care around childbirth during the COVID‐19 pandemic in different countries, using an online validated questionnaire exploring 40 WHO standards‐based quality measures. The aim of the present study was to investigate women's perspectives on QMNC around the time of childbirth during the COVID‐19 pandemic in healthcare facilities in Latvia, with emphasis on changes over time by comparing the year 2020, when strict COVID‐19‐related restrictions were in place, with 2021, when limitations were eased. Results were analyzed in two subgroups: women who went into labor and women who had a prelabor cesarean.
2. MATERIALS AND METHODS
2.1. Study design and participants
This cross‐sectional study used the Strengthening the Reporting of Observational Studies (STROBE) in Epidemiology guidelines. 24 The study protocol was registered in ClinicalTrials.gov (NCT04847336).
Women aged 18 years or older who gave birth in Latvia from March 1, 2020, until October 28, 2021, were invited to participate in an online survey. Women who did not give birth in a hospital were excluded from the study. The online survey was available in Latvian, Russian, and more than 20 other languages. The survey was promoted through a dissemination plan that focused primarily on social media (Facebook, Instagram influencer accounts, parenting groups and forums). Furthermore, nongovernmental organizations, universities, hospitals, and other institutions were asked to promote the survey through their social media accounts, websites, and newsletters.
2.2. Data collection
Data were collected from June 13, 2021, until October 28, 2021, using a structured validated online questionnaire, 25 based on the WHO standards of care, 1 and recorded using REDCap 8.5.21 (Vanderbilt University) via a centralized platform.
The questionnaire included sociodemographic questions and 40 questions—each on one WHO standards‐based quality measure—equally distributed across four domains: provision of care (10 questions), experience of care (10 questions), availability of human and physical resources (10 questions), and essential organizational changes related to the COVID‐19 pandemic (10 questions). The 40 measures of the questionnaire contributed to a composite QMNC index (scoring from 0–100), developed as a complementary synthetic measure of QMNC, with higher scores indicating higher adherence to WHO standards.
The process of questionnaire development, validation, and previous use has been reported elsewhere. 25 , 26 , 27 , 28 , 29 The questionnaire was developed in English, translated into Latvian, and back‐translated according to The Professional Society for Health Economics and Outcomes Research (ISPOR) Task Force for Translation and Cultural Adaptation Principles of Good Practice. 30
2.3. Data analysis
Duplicates and cases missing 20% or more answers on 45 key variables (including the 40 key quality measures) and five key sociodemographic variables (i.e. date of birth, age, education, parity, and whether the woman gave birth in the same country where she was born) were excluded.
Descriptive statistics of sociodemographic characteristics and quality measures were reported as absolute frequency and percentage, year of childbirth was compared (i.e. 2020 vs. 2021), and the results were grouped by experience of labor (i.e. women who went into labor vs. those who had a prelabor cesarean). These two groups differed in a few quality measures and were grouped as follows: women with a vaginal birth were considered to have experienced labor; women who had an emergency cesarean were categorized based on their report of having undergone labor (experience of regular uterine contractions) or not, which was informed by the NICE definition of labor provided to them in the questionnaire. 31
Differences in sociodemographic characteristics between the groups were tested with the χ2 or Fisher exact test. Differences in quality measures by year in both subgroups were tested with adjusted odds ratios (ORs) (i.e. adjusting for all sociodemographic variables, type of professionals directly assisting the birth, newborn admission in neonatal intensive or special care baby units, and multiple births).
Quality of maternal and newborn care indexes were calculated based on the predefined criteria previously described 23 for all women providing an answer to all 40 key quality measures. As they were not normally distributed, the QMNC indexes were presented as median and interquartile ranges (IQRs) and plotted by year of childbirth (kernel density). Differences by year of childbirth were firstly tested with a Wilcoxon–Mann–Whitney test and, secondly, to account for potential confounders, multivariate quantile regression models with robust standard errors for the 0.25th, 0.50th, and 0.75th centile were performed with the QMNC index as the dependent variable and all sociodemographic variables, mode of birth, and type of professionals assisting the woman during birth, newborn admission in neonatal intensive or special care baby units, and multiple birth as independent variables, collapsing age and educational level categories with low frequencies. The categories with the highest frequency were used as reference.
Two‐tailed P < 0.05 was considered statistically significant. Statistical analyses were performed using Stata/SE version 14.0 (Stata Corporation) and R version 4.1.1. 32
3. RESULTS
3.1. Participants' characteristics
From all countries involved in the full study, 39 542 women accessed the online questionnaire and, of these 35 556 (89.9%) agreed to participate. By October 28, 2021, the Latvian questionnaire had been accessed by 2914 women, of whom 2750 gave informed consent (94.2%). After excluding women who gave birth outside Latvia, suspected duplicates, and cases missing ≥20% of key variables, a total of 2079 reports of women giving birth in Latvia were analyzed (Figure 1). Of these, 833 gave birth in 2020, accounting for 4.8% of the total 17 344 births in Latvia in 2020, while 1205 women gave birth in 2021, accounting for 7.0% of the total 17 206 births in 2021. 11
FIGURE 1.
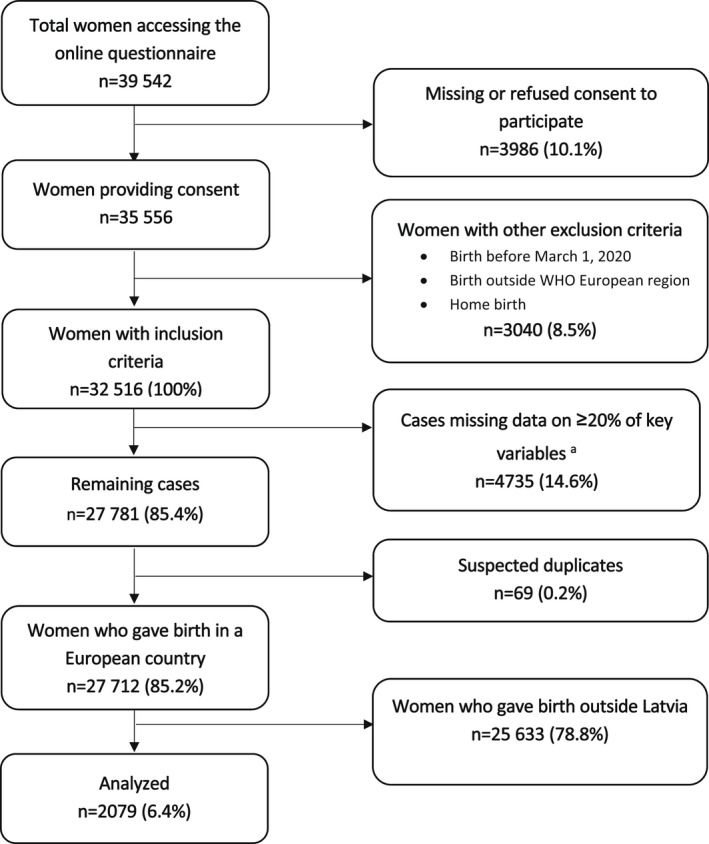
Study flow diagram. aWe used 45 key variables (40 key quality measures and five key sociodemographic questions).
The characteristics of respondents are shown in Table 1. Most of the women were aged 25–35 years (75.9%, n = 1577), with a university degree or higher education (73.8%, n = 1535), and originally born in Latvia (97%, n = 2017). About half were experiencing being in labor for the first time (53.5%, n = 1113). No major differences in women's characteristics were observed by year of childbirth.
TABLE 1.
Characteristics of respondents
| Overall a | Year of childbirth | P value | ||
|---|---|---|---|---|
| 2020 | 2021 | |||
| n = 2079 | n = 833 | n = 1205 | ||
| No. (%) | No. (%) | No. (%) | ||
| Age range, year | ||||
| 18–24 | 218 (10.5) | 75 (9.0) | 140 (11.6) | 0.059 |
| 25–30 | 908 (43.7) | 373 (44.8) | 530 (44.0) | 0.723 |
| 31–35 | 669 (32.2) | 274 (32.9) | 394 (32.7) | 0.926 |
| 36–39 | 209 (10.1) | 93 (11.2) | 115 (9.5) | 0.235 |
| ≥40 | 44 (2.1) | 18 (2.2) | 26 (2.2) | 0.996 |
| Missing | 41 (1.5) | 0 (0.0) | 0 (0.0) | NA |
| Educational level b | ||||
| None | 1 (0.0) | 1 (0.1) | 0 (0.0) | 0.409 |
| Elementary school | 22 (1.1) | 7 (0.8) | 15 (1.2) | 0.385 |
| Junior high school | 199 (9.6) | 80 (9.6) | 115 (9.5) | 0.964 |
| High school | 291 (14.0) | 111 (13.3) | 178 (14.8) | 0.357 |
| University degree | 913 (43.9) | 391 (46.9) | 520 (43.2) | 0.091 |
| Postgraduate degree/Master/Doctorate or higher | 622 (29.9) | 243 (29.2) | 377 (31.3) | 0.308 |
| Missing | 41 (1.5) | 0 (0.0) | 0 (0.0) | NA |
| Born in Latvia | ||||
| Yes | 2017 (97.0) | 821 (98.6) | 1187 (98.5) | 0.922 |
| No | 31 (1.5) | 12 (1.4) | 18 (1.5) | 0.922 |
| Missing | 41 (1.5) | 0 (0.0) | 0 (0.0) | NA |
| Parity | ||||
| 1 | 1113 (53.5) | 474 (56.9) | 634 (52.6) | 0.056 |
| >1 | 935 (45.0) | 359 (43.1) | 571 (47.4) | 0.056 |
| Missing | 41 (1.5) | 0 (0.0) | 0 (0.0) | NA |
| Mode of birth | ||||
| Vaginal spontaneous | 1512 (72.7) | 593 (71.2) | 886 (73.5) | 0.245 |
| Instrumental vaginal birth | 149 (7.2) | 55 (6.6) | 93 (7.7) | 0.340 |
| Cesarean | 418 (20.1) | 185 (22.2) | 226 (18.8) | 0.056 |
| Other characteristics | ||||
| Newborn admission to NICU or SCBU | 148 (7.1) | 58 (7.0) | 87 (7.2) | 0.893 |
| Maternal admission to ICU | 10 (0.5) | 5 (0.6) | 5 (0.4) | 0.790 |
| Multiple birth | 26 (1.3) | 14 (1.7) | 12 (1.0) | 0.249 |
| Stillbirths | 2 (0.1) | 1 (0.1) | 0 (0.0) | 0.853 |
| Presence of an obstetrics/gynecology doctor in the team who assisted the birth | 1247 (60.0) | 511 (61.3) | 731 (60.7) | 0.792 |
Abbreviations: ICU, intensive care unit; NICU, neonatal intensive care unit; SCBU, special care baby unit.
Overall results include 41 women with missing year of childbirth.
Wording on education levels agreed among partners during the Delphi. Questionnaire translated and back‐translated according to ISPOR Task Force for Translation and Cultural Adaptation Principles of Good Practice.
3.2. QMNC indexes and multivariate analysis
The QMNC indexes (Figure 2) differed by subdomains (P < 0.001), with a median index of 85.0 (IQR 75.0–90.0) for provision of care; 85.0 (IQR 70.0–95.0) for experience of care; 70.0 (IQR 55.0–80.0) for availability of physical and human resources; and 90.0 (IQR 80.0–100.0) for reorganizational changes due to COVID‐19. The total QMNC index and the QMNC index in each of the four subdomains were significantly higher in 2021 compared with 2020 (P < 0.001).
FIGURE 2.
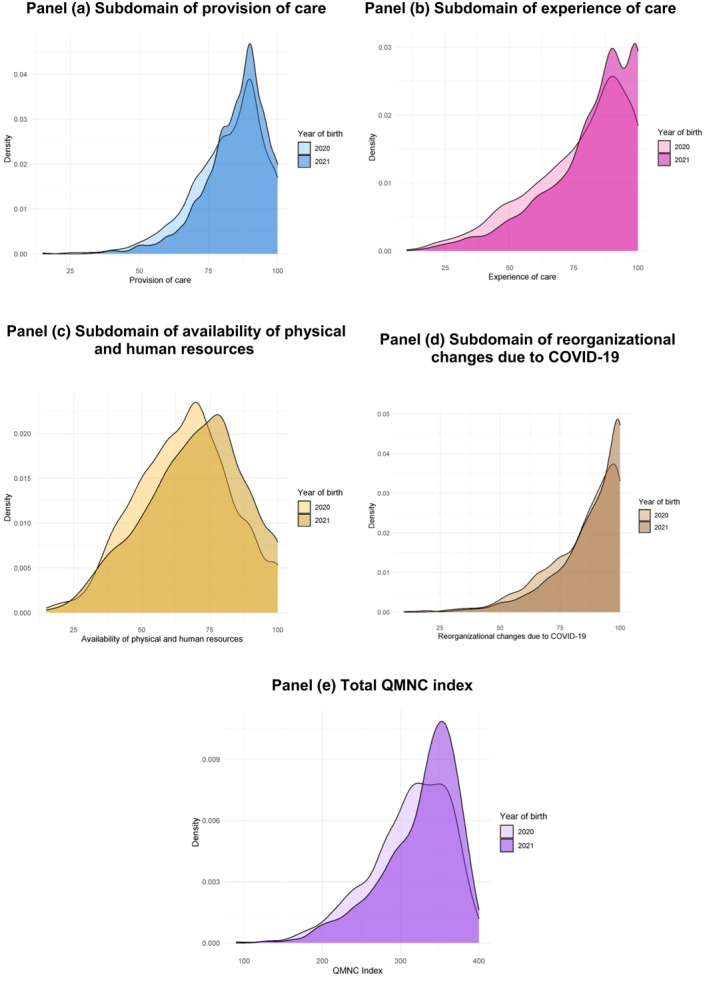
Quality of maternal and newborn care (QMNC) index by year of labor. (a) Subdomain of provision of care. (b) Subdomain of experience of care. (c) Subdomain of availability of physical and human resources. (d) Subdomain of reorganizational changes due to COVID‐19. (e) Total QMNC index
When adjusting for sociodemographic and obstetric variables, quantile regression showed a significantly higher QMNC index in 2021 compared with 2020 (coefficient variation at the 0.25th, 0.50th, and 0.75th quantile respectively of +15, +20, +10) (Table 2). Multiparous women, women assisted by an obstetrician/gynecologist, and women born outside Latvia also had statistically significant a higher QMNC index at more centiles (+22.5, +10, +5 for multiparous women; +15, +10, +5 for women assisted by an obstetrician/gynecologist; +30, +10, 0 for women born outside Latvia). Conversely, instrumental vaginal birth, cesarean, and young women were associated with a statistically significant lower QMNC index at more centiles (−5, −15, −15 for instrumental vaginal birth; −30, −20, −15 for cesarean, and −12.5, −15, −10 for women aged 18–24 years compared with women aged 31–35 years). In addition, women with a lower educational level, newborn admitted to the NICU, and multiple birth reported a significantly lower QMNC score in a single centile.
TABLE 2.
Multiple quantile regression (n = 1659)
| 0.25th centile | 0.50th centile (median) | 0.75th centile | ||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | |
| Year of childbirth | ||||||
| 2020 | Ref | Ref | Ref | |||
| 2021 | 15.00 (7.63–22.37) | <0.001 | 20.00 (14.63–25.37) | <0.001 | 10.00 (4.66–15.34) | <0.001 |
| Parity | ||||||
| 1 | Ref | Ref | Ref | |||
| >1 | 22.50 (14.02–30.98) | <0.001 | 10.00 (3.97–16.03) | 0.001 | 0.020 | |
| Women born in Latvia | ||||||
| Yes | Ref | Ref | Ref | |||
| No | <0.001 | 10.00 (1.24–18.76) | 0.025 | 0.00 (−16.22 to 16.22) | >0.99 | |
| Age range, year | ||||||
| 18–24 | −12.50 (−28.53 to 3.53) | 0.126 | −15.00 (−26.93 to −3.07) | 0.014 | −10.00 (−16.80 to −3.20) | 0.004 |
| 25–30 | Ref | Ref | Ref | |||
| 31–35 | 0.00 (−8.84 to 8.84) | >0.99 | 0.00 (−6.08 to 6.08) | >0.99 | −5.00 (−9.03 to 0.97) | 0.015 |
| >35 | 2.50 (−7.93 to 12.93) | 0.638 | 0.00 (−9.77 to 9.77) | >0.99 | 5.00 (−0.22 to 10.22) | 0.061 |
| Educational level | ||||||
| High school or lower | −7.50 (−17.36 to 2.36) | 0.136 | −5.00 (−12.31 to 2.31) | 0.180 | −5.00 (−9.28 to −0.72) | 0.022 |
| University degree | Ref | Ref | Ref | |||
| Postgraduate degree/Master/Doctorate or higher | 5.00 (−3.18 to 13.18) | 0.231 | 0.00 (−6.31 to 6.31) | >0.99 | 0.00 (−4.14 to 4.14) | >0.99 |
| Mode of birth | ||||||
| Spontaneous VB | Ref | Ref | Ref | |||
| Instrumental VB | −5.00 (−13.89 to 3.89) | 0.270 | −15.00 (−27.14 to −2.86) | 0.015 | −15.00 (−27.74 to −2.26) | 0.021 |
| Cesarean | −30.00 (−41.87 to −18.13) | <0.001 | −20.00 (−27.99 to −12.01) | <0.001 | −15.00 (−19.99 to −10.01) | <0.001 |
| Obstetrics/gynecology doctor in the team who assisted the birth | ||||||
| No | Ref | Ref | Ref | |||
| Yes | 15.00 (6.82–23.18) | <0.001 | 10.00 (4.33–15.67) | 0.001 | 5.00 (1.48–8.52) | 0.005 |
| Newborn admission to NICU or SCBU | ||||||
| No | Ref | Ref | Ref | |||
| Yes | −25.00 (−45.63 to −4.37) | 0.018 | −30.00 (−70.44 to 10.44) | 0.146 | −5.00 (−29.60 to 19.60) | 0.690 |
| Multiple birth | ||||||
| No | Ref | Ref | Ref | |||
| Yes | −32.50 (−119.90 to 54.90) | 0.466 | −45.00 (−82.68 to −7.32) | 0.019 | −25.00 (−141.97 to 91.97) | 0.675 |
| Intercept | 270.00 (259.01–280.99) | <0.001 | 315.00 (307.71–322.29) | <0.001 | 350.00 (343.44–356.56) | <0.001 |
Abbreviations: NICU, neonatal intensive care unit; SCBU, special care baby unit; VB, vaginal birth.
3.3. WHO standards‐based quality measures
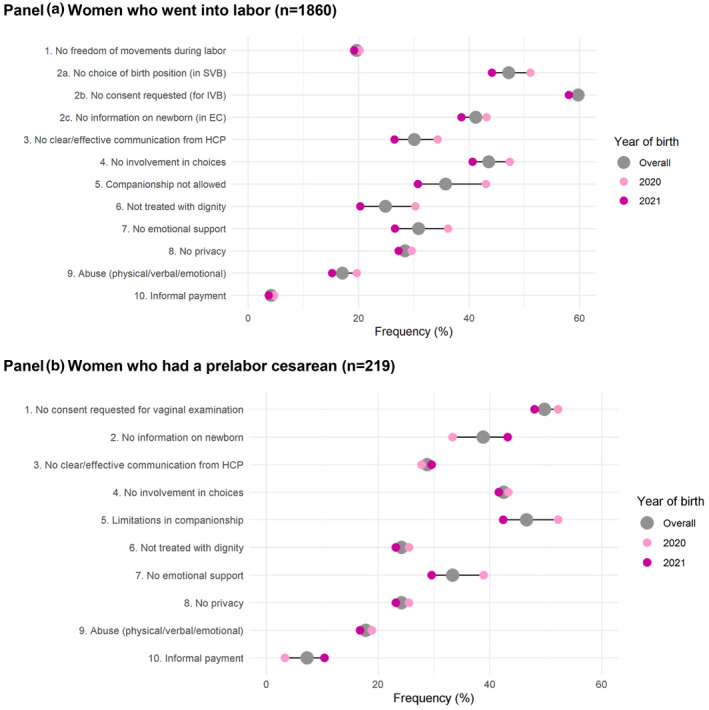
Figures 3, 4, 5, 6 compare the years 2020 and 2021 for each of 40 key quality measures in women who went into labor (Panel a) and those who had a prelabor cesarean (Panel b) in the four QMNC domains explored. Data are provided as the frequency on the overall sample (gray dot) and the frequency on the sample of women giving birth each year (colored dots). Table 3 includes more thorough information with multiple logistic regression analysis comparing quality measures between women who went into labor (n = 1860) and women who had a prelabor cesarean (n = 219) when adjusted for year of childbirth and other sociodemographic variables.
FIGURE 3.
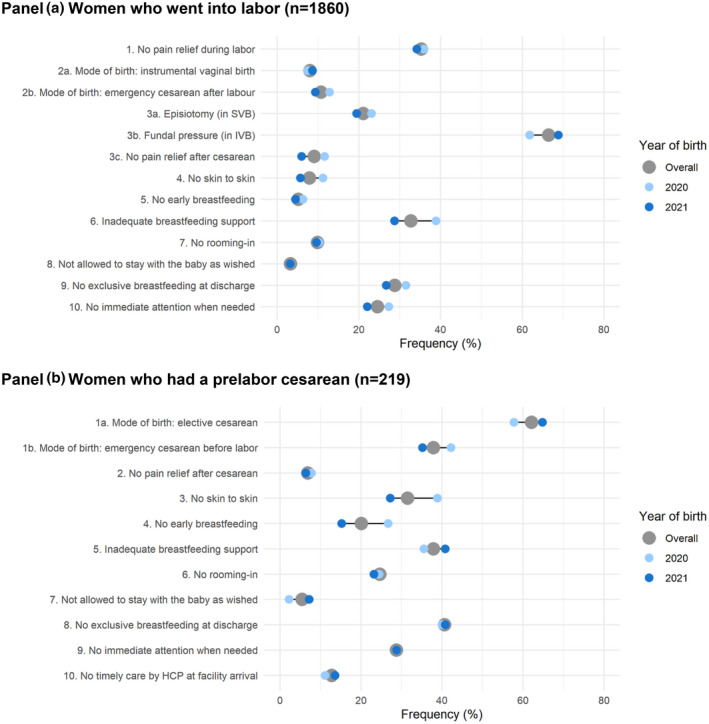
Provision of care. (a) Women who went into labor (n = 1860). (b) Women who had a prelabor cesarean (n = 219). HCP, healthcare provider; IVB, instrumental vaginal birth; SVB, spontaneous vaginal birth. Note: Data are reported as frequency on the total sample (gray dot) and as frequency on the sample of women giving birth in 2020 and 2021 (colored dots). The horizontal gray line represents the range of the frequencies. All the indicators in the domain of provision of care are directly based on WHO standards. Indicators identified with letters (e.g. 3a, 3b) were tailored to take into account different mode of birth (i.e. spontaneous vaginal, instrumental vaginal, and cesarean). These were calculated on subsamples (e.g. 3a was calculated on spontaneous vaginal births; 3b was calculated on instrumental vaginal births).
FIGURE 4.
Experience of care. (a) Women who went into labor (n = 1860). (b) Women who had a prelabor cesarean (n = 219). EC, emergency cesarean; HCP, healthcare provider; IVB, instrumental vaginal birth; SVB, spontaneous vaginal birth. Note: Data are reported as frequency on the total sample (gray dot) and as frequency on the sample of women giving birth in 2020 and 2021 (colored dots). The horizontal gray line represents the range of the frequencies. All the indicators in the domain of experience of care are directly based on WHO standards. Indicators identified with letters (e.g. 2a, 2b) were tailored to take into account different modes of birth (i.e. spontaneous vaginal, instrumental vaginal, and cesarean). These were calculated on subsamples (e.g. 2a was calculated on spontaneous vaginal births; 2b was calculated on instrumental vaginal births).
FIGURE 5.
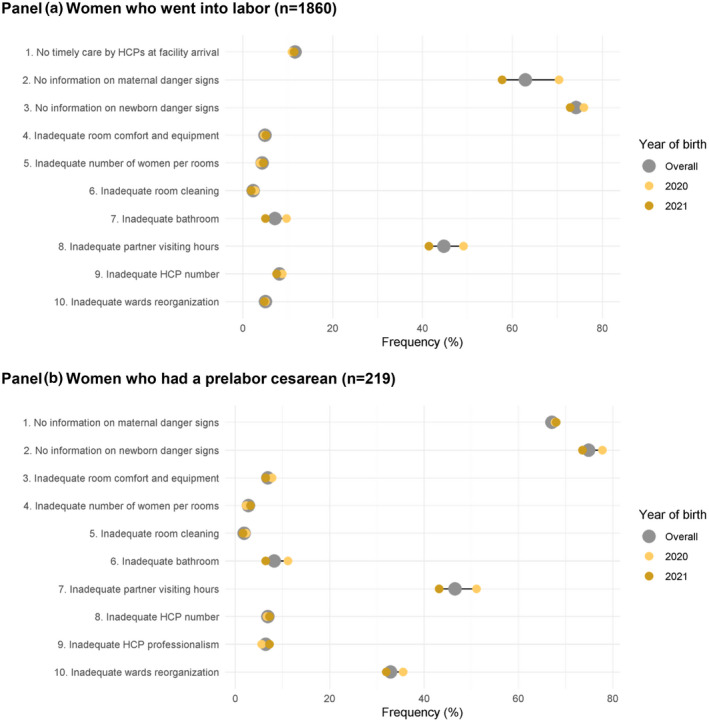
Availability of physical and human resources. (a) Women who went into labor (n = 1860). (b)Women who had a prelabor cesarean (n = 219). HCP, healthcare provider. Note: Data are reported as frequency on the total sample (gray dot) and as frequency on the sample of women giving birth in 2020 and 2021 (colored dots). The horizontal gray line represents the range of the frequencies. All the indicators in the domain of resources are directly based on WHO standards.
FIGURE 6.
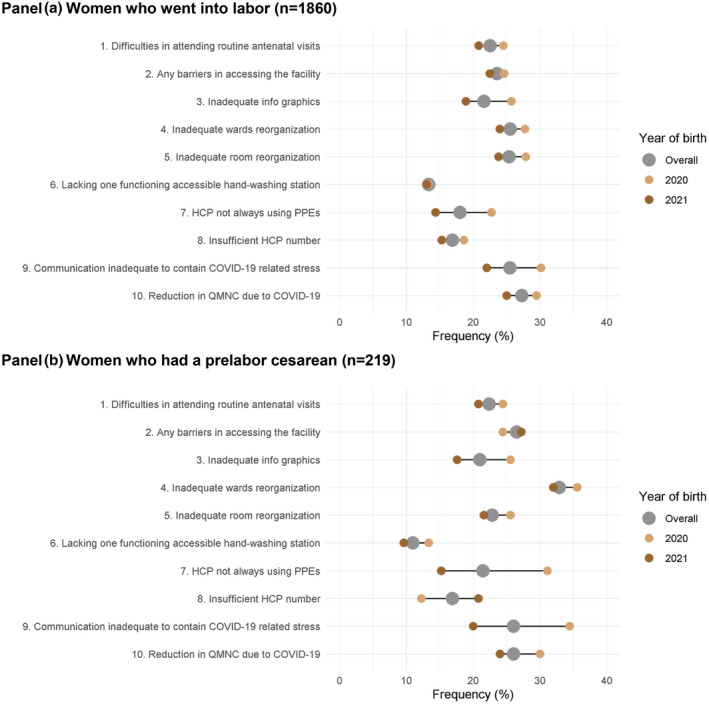
Reorganizational changes due to COVID‐19. (a) Women who went into labor (n = 1860). (b) Women who had a prelabor cesarean (n = 219). HCP, healthcare provider; PPE, personal protective equipment; QMNC, quality of maternal and newborn care. Note: Data are reported as frequency on the total sample (gray dot) and as frequency on the sample of women giving birth in 2020 and 2021 (colored dots). The horizontal gray line represents the range of the frequencies. Indicator 6 in both panels was defined as: at least one functioning and accessible hand‐washing station (near or inside the room where the mother was hospitalized) supplied with water and soap or with disinfectant alcohol solution.
TABLE 3.
Multiple logistic regression comparing quality measures between women who went into labor (n = 1860) and women who had a prelabor cesarean (n = 219) when adjusted for year of labor and other sociodemographic variables a , b , c , d
| Provision of care | Adjusted OR (95% CI) | P value | Experience of care | Adjusted OR (95% CI) | P value | Availability of physical and human resources | Adjusted OR (95% CI) | P value | Reorganizational changes due to COVID‐19 | Adjusted OR (95% CI) | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. No pain relief during birth | NA | NA | 1. No freedom of movements during birth | NA | NA | 1. No timely care by HCPs at facility arrival | 1.26 (0.80–1.97) | 0.312 | 1. Difficulties in attending routine antenatal visits | 1.08 (0.76–1.52) | 0.679 |
| 2. Mode of birth | NA | NA | 2a. No choice of birth position (in SVB) | NA | NA | 2. No information on maternal danger signs | 1.37 (1.00–1.87) | 0.045 | 2. Any barriers in accessing the facility | 1.16 (0.84; –1.62) | 0.365 |
| 2a. IVB | |||||||||||
| NA | NA | ||||||||||
| 2b. EC during birth | |||||||||||
| 3a. Episiotomy (in SVB) | NA | NA | 2b. No consent requested (for IVB) | NA | NA | 3. No information on newborn danger signs | 1.25 (0.89–1.75) | 0.193 | 3. Inadequate info graphics | 1.02 (0.72–1.46) | 0.907 |
| 3b. Fundal pressure (in IVB) | NA | NA | 2c. No information on newborn (at cesarean) | 1.02 (0.65–1.58) | 0.946 | 4. Inadequate room comfort and equipment | 1.59 (0.89–2.83) | 0.120 | 4. Inadequate ward reorganization | 1.49 (1.09–2.03) | 0.012 |
| 3c. No pain relief after cesarean | 0.77 (0.34–1.76) | 0.543 | 3. No clear/effective communication from HCP | 1.14 (0.83–1.58) | 0.426 | 5. Inadequate number of women per rooms | 0.66 (0.28–1.57) | 0.350 | 5. Inadequate room reorganization | 0.91 (0.64–1.28) | 0.574 |
| 4. No skin‐to‐skin contact | 6.69 (4.65–6.62) | <0.001 | 4. No involvement in choices | 1.06 (0.79–1.42) | 0.700 | 6. Inadequate room cleaning | 0.97 (0.34–2.80) | 0.959 | 6. Lack of one functioning accessible hand; washing station | 0.91 (0.58–1.44) | 0.701 |
| 5. No early breastfeeding | 5.35 (3.52–8.14) | <0.001 | 5. Companionship not allowed | 1.40 (1.04–1.88) | 0.027 | 7. Inadequate bathroom | 1.12 (0.66–1.91) | 0.665 | 7. HCP not always using PPE | 1.41 (0.99–2.01) | 0.058 |
| 6. Inadequate breastfeeding support | 1.58 (1.16–2.15) | 0.004 | 6. Not treated with dignity | 1.18 (0.83–1.66) | 0.352 | 8. Inadequate partner visiting hours | 1.00 (0.74–1.34) | 0.982 | 8. Insufficient HCP number | 1.29 (0.88–1.91) | 0.193 |
| 7. No rooming‐in | 3.14 (2.00–4.94) | <0.001 | 7. No emotional support | 1.29 (0.95–1.77) | 0.106 | 9. Inadequate HCP number | 1.05 (0.59–1.84) | 0.878 | 9. Communication inadequate to contain COVID‐19‐related stress | 1.14 (0.82–1.59) | 0.438 |
| 8. Not allowed to stay with the baby as wished | 1.35 (0.61–3.01) | 0.458 | 8. No privacy | 0.85 (0.61–1.19) | 0.354 | 10. Inadequate HCP professionalism | 1.62 (0.88–2.97) | 0.120 | 10. Reduction in QMNC due to COVID‐19 | 1.09 (0.79–1.52) | 0.601 |
| 9. No exclusive breastfeeding at discharge | 1.76 (1.30–2.38) | <0.001 | 9. Abuse (physical/verbal /emotional) | 1.17 (0.80–1.73) | 0.420 | ||||||
| 10. No immediate attention when needed | 1.55 (1.11–2.15) | 0.009 | 10. Informal payment | 1.83 (1.03–3.26) | 0.039 |
Abbreviations: EC, emergency cesarean; HCP, healthcare provider; IVB, instrumental vaginal birth; PPE, personal protective equipment; QMNC, quality of maternal and newborn care; SVB, spontaneous vaginal birth.
ORs were calculated taking women who underwent birth as the reference and adjusting for sociodemographic variables (i.e. year of childbirth, maternal age, maternal education, born in Latvia), parity, type of professional assisting the birth, newborn admission to neonatal intensive or semi‐intensive care unit, and multiple birth.
All the indicators in the domains of provision of care, experience of care, and resources are directly based on WHO standards. Indicators identified with letters (e.g. 3a, 3b) were tailored to take into account different mode of birth (i.e. spontaneous vaginal, instrumental vaginal, and cesarean). These were calculated on subsamples (e.g. 3a was calculated on spontaneous vaginal births; 3b was calculated on instrumental vaginal births).
Indicator 6 in the domain of reorganizational changes due to COVID‐19 was defined as: at least one functioning and accessible hand‐washing station (near or inside the room where the woman was hospitalized) supplied with water and soap or with disinfectant alcohol solution.
Bold values are statistically significant.
In the provision of care domain (Figure 3) in some measures the situation improved or showed no statistically significant difference when compared by year. Key findings for women who went into labor (n = 1860) were: 35.3% (n = 656) were not given pain relief during labor (without significant difference by year); 66.4% (n = 99/149) received fundal pressure during instrumental vaginal birth (without significant difference by year); 32.7% (n = 609) reported inadequate breastfeeding support (with a significant difference between 2020 and 2021: 38.9% vs. 28.7%, P < 0.001); 28.8% (n = 535) reported lack of exclusive breastfeeding at discharge (31.5% vs. 26.7%, without significant difference by year); and 24.5% (n = 456) reported lack of immediate attention when needed (significant difference between 2020 and 2021: 27.3% vs. 22.0%).
Regarding the data on experience of care (Figure 4; Table 3), several indicators improved in 2021 compared with 2020, with the quality measure of limited companionship showing the most significant improvement (falling from 43.1% to 30.7%, P < 0.001). Other key findings included: 59.7% (n = 89/149) of women who had an instrumental vaginal birth were not asked to provide consent for this mode of birth; 47.2% (n = 713/1512) of women who had a spontaneous vaginal birth had no choice of birth position; out of the total sample, 43.5% (n = 810) did not feel involved in choices about their care. Notably, almost one‐fifth (17.0% to 17.8%) of all women reported suffering from physical, verbal, or emotional abuse.
Women who had a prelabor cesarean had an increased odds of not being allowed a birth companion (aOR 1.40; 95% CI, 1.04–1.88, P = 0.027) compared with women who went into labor (Table 3), with a slight but not significant improvement in 2021 (52.2% vs. 42.4%, P = 0.073).
Regarding the domain of availability of physical and human resources (Figure 5; Table 3) both subgroups highlighted inadequate partner visiting hours (44.7% and 46.6%, respectively). In 2021, the situation improved by 7.7% in the labor group (P < 0.001), and by 7.9% in the prelabor cesarean group (P = 0.055). A small percentage of women who went into labor reported inadequate room cleaning (2.3%, n = 42), inadequate number of women per room (4.2%, n = 79), and inadequate room comfort and equipment (4.9%, n = 91). Furthermore, a high percentage of women who went into labor or had a prelabor cesarean reported that they did not receive information on maternal danger signs (62.9% vs. 67.1%, respectively; aOR 1.37; 95% CI, 1.00–1.87, P = 0.045) and no information on newborn danger signs (74.2% vs. 74.9%, respectively; aOR 1.25, 95% CI, 0.89–1.75, P = 0.193).
In the domain of reorganizational changes due to the COVID‐19 pandemic (Figure 6; Table 3), several indicators showed improved practices in 2021 compared with 2020 among women who went into labor: communication inadequate to contain COVID‐19‐related stress (30.1% vs. 22.0%, P < 0.001); healthcare provider not always using PPE (22.7% vs. 14.4%, P < 0.001); reduction in QMNC due to COVID‐19 (29.5% vs. 25.0%, P = 0.045). Women who had a prelabor cesarean had similar results, with the most notable reductions over time found in percentage of healthcare providers not always using PPE (31.1% vs. 15.2%, P = 0.004) and in communication inadequate to contain COVID‐19‐related stress (34.4% vs. 20.0%, P = 0.006).
Multiple logistic regression (Table 3) highlighted that women who had a prelabor cesarean had an increased odds of inadequate ward reorganization (aOR 1.49; 95% CI, 1.09–2.03; P = 0.012) compared with women who went into labor.
4. DISCUSSION
This is the first research in Latvia to adopt a comprehensive approach to explore women's perceptions of quality of care around childbirth at health facilities. Several results are similar to the few existing reports. 4 , 5 , 16 Previous research conducted in Latvia 4 suggested inadequate QMNC, even before the COVID‐19 pandemic, and proposed recommendations to reduce Latvia's maternal mortality ratio—one of the highest in the EU. 5
Similarly, other quality of care indicators reported in our study are aligned with prepandemic data. For example, the observed lack of breastfeeding support (32.7% in our study) aligns with previous data on challenges toward achieving acceptable breastfeeding rates in the country. 33 , 34
The COVID‐19 pandemic has posed additional challenges for Latvian healthcare systems. For example, existing literature has documented that in Latvia, antenatal checkups have been postponed or canceled due to women's concerns about infection or viral spread, resulting in an increase in untreated illnesses throughout pregnancy, leading to emergencies, complications, and death during pregnancy, childbirth, or the postnatal period. 18 In our study, 22.5% of women reported difficulties in attending routine antenatal visits, with an improvement of only approximately 4% in 2021 when compared with 2020.
Furthermore, our data on lack of partnership during childbirth (35.8% of women who went into labor and 46.6% of women who had a prelabor cesarean) are in line with a previous report, which showed that in Latvia, partners did not participate in the birth in 32.5% of cases. 35 During the early phase of the pandemic, most obstetrics departments in Latvia did not allow partners or other family members to be a birth companion. Encouragingly, our data show an improvement in this quality measure in 2021 compared with 2020 of 12.4%. However, several other indicators showed a trend for improvement in 2021 versus 2020, suggesting that further monitoring will be helpful.
Regarding women's experience of care, very little previous evidence is available for Latvia. 17 , 35 A number of studies from different settings worldwide, including high‐income countries, 19 , 35 , 36 , 37 , 38 , 39 show that women are frequently subjected to improper care, such as receiving poor emotional support, enquiries are ignored or rejected, or experience of lack of privacy or other types of mistreatment and abuse, such as rude, insulting, and judgmental attitudes from all levels of healthcare staff. WHO recommends that every healthcare facility should provide respectful maternity care and effective communication, including sensitive, caring, and friendly attitudes from all healthcare personnel 40 and in general. A birth position of choice should be permitted, 40 and as much as possible, women should be actively involved in the decision‐making process, with appropriate communication from healthcare providers, which increases trust in doctors. 37 , 38
Regarding reorganizational changes due to COVID‐19, in 2021 14.4% of women reported that healthcare personnel were still not always using PPE; it is essential to note that this is the first study that outlines such a problem in Latvia. In Latvia, by the end of 2021 more than 4300 people had died from COVID‐19. 41 In this complex historical moment, when the COVID‐19 pandemic had increased levels of stress for most pregnant women, 17 and when vaccine hesitancy and resistance to COVID‐19 prevention measures have been a global problem, healthcare providers should be an example of good practices for all patients, particularly for prevention procedures that aim to protect both patients and colleagues.
Notably, the availability of physical and human resources domain showed the lowest QMNC index across the four domains. Women were relatively satisfied regarding room comfort, number of women per room, room cleaning, and bathroom availability. However, it is alarming that in a very high percentage of cases (57.7%–77.8%), women did not receive information about maternal or newborn danger signs, with a higher frequency in the prelabor cesarean group and no significant changes between 2020 and 2021. Notably, quality measures were substandard in many other countries surveyed for the IMAgiNE EURO study. 23 , 28 , 29 , 42 , 43 , 44 , 45
Overall results from this survey in Latvia show that there is room for substantial improvement. Multiple actions are urgently needed at different levels, such as ensuring an adequate number of skilled healthcare personnel, training on respectful woman‐centered maternal care, development of informative materials for mothers, and other measures to improve the quality of care for mothers and newborns in Latvia. Monitoring of the key quality measures will be critical to evaluate the success of context‐specific actions to improve quality of care in Latvia.
The main strengths of this study are the relatively high number of respondents, approximately 4%–7% out of all births in each year and the validated tools used for data collection, allowing comprehensive assessment of the QMNC. 25 Limitations of the IMAgiNE EURO survey have been acknowledged elsewhere. 23 , 28 , 29 Specific to Latvia, the data collection period (survey launched in June 2021) may have implied a recall bias: women who gave birth in 2020 may have lost detailed memories, especially in cases of traumatic experiences 46 ; surveying at regular intervals (every 4–6 months) would reduce this bias. Future studies could also consider collecting more detailed data on maternal and hospital characteristics. However, this should not limit taking action based on currently available data.
AUTHOR CONTRIBUTIONS
EP initiated this multicountry study in Latvia. DR, DJ, AV, GJS, and KPV were responsible for questionnaire translations, and promoted and supported the process of data collection. EP wrote the first draft of the manuscript with major inputs from all authors. IM analyzed the data. All authors approved the final version of the manuscript for submission.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
IMAgiNE EURO Study Group
Bosnia and Herzegovina: Amira Ćerimagić, NGO Baby Steps, Sarajevo; Croatia: Daniela Drandić, Roda—Parents in Action, Zagreb; Magdalena Kurbanović, Faculty of Health Studies, University of Rijeka, Rijeka; France: Rozée Virginie, Elise de La Rochebrochard, Sexual and Reproductive Health and Rights Research Unit, Institut National d'Études Démographiques (INED), Paris; Kristina Löfgren, Baby‐friendly Hospital Initiative (IHAB); Germany: Céline Miani, Stephanie Batram‐Zantvoort, Lisa Wandschneider, Department of Epidemiology and International Public Health, School of Public Health, Bielefeld University, Bielefeld; Italy: Marzia Lazzerini, Emanuelle Pessa Valente, Benedetta Covi, Ilaria Mariani, Institute for Maternal and Child Health IRCCS “Burlo Garofolo”, Trieste; Sandra Morano, Medical School and Midwifery School, Genoa University, Genoa; Israel: Ilana Chertok, Ohio University, School of Nursing, Athens, Ohio, USA and Ruppin Academic Center, Department of Nursing, Emek Hefer; Rada Artzi‐Medvedik, Department of Nursing, The Recanati School for Community Health Professions, Faculty of Health Sciences at Ben‐Gurion University (BGU) of the Negev; Latvia: Elizabete Pumpure, Dace Rezeberga, Gita Jansone‐Šantare, Department of Obstetrics and Gynecology, Riga Stradins University and Riga Maternity Hospital, Riga; Dārta Jakovicka, Faculty of Medicine, Riga Stradins University, Rīga; Agnija Vaska, Riga Maternity Hospital, Riga; Anna Regīna Knoka, Faculty of Medicine, Riga Stradins University, Rīga; Katrīna Paula Vilcāne, Faculty of Public Health and Social Welfare, Riga Stradins University, Riga; Lithuania: Alina Liepinaitienė, Andželika Kondrakova, Kaunas University of Applied Sciences, Kaunas; Marija Mizgaitienė, Simona Juciūtė, Kaunas Hospital of the Lithuanian University of Health Sciences, Kaunas; Luxembourg: Maryse Arendt, Professional Association of Lactation Consultants in Luxembourg; Barbara Tasch, Professional Association of Lactation Consultants in Luxembourg and Neonatal Intensive Care Unit, KannerKlinik, Centre Hospitalier de Luxembourg, Luxembourg; Norway: Ingvild Hersoug Nedberg, Sigrun Kongslien, Department of Community Medicine, UiT The Arctic University of Norway, Tromsø; Eline Skirnisdottir Vik, Department of Health and Caring Sciences, Western Norway University of Applied Sciences, Bergen; Poland: Barbara Baranowska, Urszula Tataj‐Puzyna, Maria Węgrzynowska, Department of Midwifery, Centre of Postgraduate Medical Education, Warsaw; Portugal: Raquel Costa, EPIUnit—Instituto de Saúde Pública, Universidade do Porto, Porto; Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional, Porto; Lusófona University/HEI‐Lab: Digital Human‐environment Interaction Labs, Lisbon; Catarina Barata, Instituto de Ciências Sociais, Universidade de Lisboa; Teresa Santos, Universidade Europeia, Lisboa and Plataforma CatólicaMed/Centro de Investigação Interdisciplinar em Saúde (CIIS) da Universidade Católica Portuguesa, Lisbon; Carina Rodrigues, EPIUnit—Instituto de Saúde Pública, Universidade do Porto, Porto and Laboratório para a Investigação Integrativa e Translacional em Saúde Populacional, Porto; Heloísa Dias, Regional Health Administration of the Algarve; Romania: Marina Ruxandra Otelea, University of Medicine and Pharmacy Carol Davila, Bucharest and SAMAS Association, Bucharest; Serbia: Jelena Radetić, Jovana Ružičić, Centar za mame, Belgrade; Slovenia: Zalka Drglin, Barbara Mihevc Ponikvar, Anja Bohinec, National Institute of Public Health, Ljubljana; Spain: Serena Brigidi, Department of Anthropology, Philosophy and Social Work, Medical Anthropology Research Center (MARC), Rovira i Virgili University (URV), Tarragona; Lara Martín Castañeda, Institut Català de la Salut, Generalitat de Catalunya; Sweden: Helen Elden, Verena Sengpiel, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg and Department of Obstetrics and Gynecology, Region Västra Götaland, Sahlgrenska University Hospital, Gothenburg; Karolina Linden, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg; Mehreen Zaigham, Department of Obstetrics and Gynecology, Institution of Clinical Sciences Lund, Lund University, Lund and Skåne University Hospital, Malmö; Switzerland: Claire de Labrusse, Alessia Abderhalden, Anouck Pfund, Harriet Thorn, School of Health Sciences (HESAV), HES‐SO University of Applied Sciences and Arts Western Switzerland, Lausanne; Susanne Grylka, Michael Gemperle, Antonia Mueller, Research Institute of Midwifery, School of Health Sciences, ZHAW Zurich University of Applied Sciences, Winterthur.
5. Ethical aspects
The study was approved by Riga Stradins University Research Ethics Committee in Latvia (22–2/140/2021 16.03.2021) and by the Institutional Review Board of the coordinating center: IRCCS Burlo Garofolo Trieste (IRB‐BURLO 05/2020 15.07.2020), as well as by ethical committees of other participating countries. Participation in the survey was entirely voluntary and anonymous. The right to reject participation in the survey, the study methodology, and the research objectives were described for participants and informed consent to participate in the study was requested to progress into the survey. All data were kept and analyzed in Italy (coordination center). Encryption was used to safeguard data transit and storage.
DISCLAIMER
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
ACKNOWLEDGMENTS
This research was supported by the Ministry of Health, Rome—Italy, in collaboration with the Institute for Maternal and Child Health IRCCS “Burlo Garofolo”, Trieste, Italy. We are grateful to the women who dedicated their time to complete this survey. We would like to thank Riga Stradins University and all professional organizations who helped with promotional activities. Special thanks to the IMAgiNE EURO study group for their contribution to the development of this project and support for this manuscript.
Pumpure E, Jakovicka D, Mariani I, et al. Womenʼs perspectives on the quality of maternal and newborn care in childbirth during the COVID‐19 pandemic in Latvia: Results from the IMAgiNE EURO study on 40 WHO standards‐based quality measures. Int J Gynecol Obstet. 2022;159(Suppl. 1):97‐112. doi: 10.1002/ijgo.14461
Contributor Information
Elizabete Pumpure, Email: elizabete.pumpure@rsu.lv.
the IMAgiNE EURO study group:
Amira Ćerimagić, Daniela Drandić Roda, Magdalena Kurbanović, Rozée Virginie, Elise de La Rochebrochard, Kristina Löfgren, Céline Miani, Stephanie Batram‐Zantvoort, Lisa Wandschneider, Sandra Morano, Ilana Chertok, Rada Artzi‐Medvedik, Alina Liepinaitienė, Andželika Kondrakova, Marija Mizgaitienė, Simona Juciūtė, Maryse Arendt, Barbara Tasch, Ingvild Hersoug Nedberg, Sigrun Kongslien, Eline Skirnisdottir Vik, Barbara Baranowska, Urszula Tataj‐Puzyna, Maria Węgrzynowska, Raquel Costa, Catarina Barata, Teresa Santos, Carina Rodrigues, Heloísa Dias, Marina Ruxandra Otelea, Jelena Radetić, Jovana Ružičić, Zalka Drglin, Barbara Mihevc Ponikvar, Anja Bohinec, Serena Brigidi, Lara Martín Castañeda, Helen Elden, Verena Sengpiel, Karolina Linden, Mehreen Zaigham, Claire De Labrusse, Alessia Abderhalden, Anouck Pfund, Harriet Thorn, Susanne Grylka, Michael Gemperle, and Antonia Mueller
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request to the corresponding author.
REFERENCES
- 1. World Health Organization . Standards for improving quality of maternal and newborn care in health facilities. WHO; 2016. Accessed October 15, 2021. https://cdn.who.int/media/docs/default‐source/mca‐documents/advisory‐groups/quality‐of‐care/standards‐for‐improving‐quality‐of‐maternal‐and‐newborn‐care‐in‐health‐facilities.pdf?sfvrsn=3b364d8_2 [Google Scholar]
- 2. Dencker A, Nilsson C, Begley C, et al. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. 2019;32:99‐111. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization . WHO recommendations: intrapartum care for a positive childbirth experience. WHO; 2018. Accessed January 21, 2022. http://apps.who.int/iris/bitstream/handle/10665/260178/9789241550215‐eng.pdf;jsessionid=B7CE10E530E0330FD7B47EB719AB6A08?sequence=1 [PubMed] [Google Scholar]
- 4. Miteniece E, Pavlova M, Rechel B, Rezeberga D, Murauskienė L, Groot W. Barriers to accessing adequate maternal care in Latvia: a mixed‐method study among women, providers and decision‐makers. Health Policy. 2019;123:87‐95. [DOI] [PubMed] [Google Scholar]
- 5. The World Bank . Maternal mortality ratio—European Union. Accessed January 23, 2022. https://data.worldbank.org/indicator/SH.STA.MMRT?locations=EU&name_desc=false [Google Scholar]
- 6. Health Statistics Database . Surgical work by type of operation in all hospitals. 2021. Accessed December 26, 2021. https://statistika.spkc.gov.lv/pxweb/en/Health/Health__Veselibas%20aprupe__StacionaraMediciniskaPalidziba/STAC030_Stacionara_kirurgija_operacijas.px/table/tableViewLayout2/
- 7. Eurostat . Infant mortality sharply declined over the past decades. 2021. Accessed January 20, 2022. https://ec.europa.eu/eurostat/web/products‐eurostat‐news/‐/ddn‐20210604‐1
- 8. World Health Organization European Region . European Health Information Gateway. Early neonatal deaths per 1000 live births. 2021. Accessed January 9, 2022. https://gateway.euro.who.int/en/indicators/hfa_78‐1130‐early‐neonatal‐deaths‐per‐1000‐live‐births/visualizations/#id=18883
- 9. Euro‐Peristat . The European Perinatal Health report 2015: mode of delivery. Accessed March 1, 2022. https://www.europeristat.com/images/EPHR2015_Mode_of_delivery.pdf
- 10. Robson MS. Classification of caesarean sections. Fetal Matern Med Rev. 2001;12:23‐39. [Google Scholar]
- 11. Health Statistics Database . Maternal and child health care. 2021. Accessed January 23, 2022. https://statistika.spkc.gov.lv/pxweb/en/Health/Health__Mates_berna_veseliba/?tablelist=true
- 12. Behmane D, Dudele A, Villerusa A, et al. Latvia: health system review 2019. Health Syst Transit. 2019;21(4):i‐165. Accessed January 23, 2022. https://apps.who.int/iris/bitstream/handle/10665/331419/HiT‐21‐4‐2019‐eng.pdf [PubMed] [Google Scholar]
- 13. Health Inequalities Portal . State of inequality: reproductive, maternal, neonatal and child health. Health Inequalities. 2015. Accessed February 27, 2022. https://health‐inequalities.eu/lv/jwddb/state‐of‐inequality‐reproductive‐maternal‐newborn‐and‐child‐health/ [Google Scholar]
- 14. OECDiLibrary . Health at a Glance: Europe 2018. Accessed February 26, 2022. https://www.oecd‐ilibrary.org/docserver/health_glance_eur‐2018‐en.pdf?expires=1646091769&id=id&accname=guest&checksum=9A96A2FFE7C3BF10F08C1EF301791FBB
- 15. OECD . OECD reviews of public health: Latvia. A Healthier Tomorrow. 2020. Accessed February 28, 2022. https://www.oecd.org/latvia/oecd‐reviews‐of‐public‐health‐latvia‐e9f33098‐en.htm [Google Scholar]
- 16. Partnership for Maternal Newborn and Child Health . Pregnancy and childbirth during COVID‐19. 2021. Accessed February 9, 2022. https://pmnch.who.int/resources/tools‐and‐toolkits/pmnch‐covid‐19‐and‐wcah‐toolkits/maternal‐and‐newborn‐health/pregnancy‐and‐childbirth
- 17. Pumpure E, Rezeberga D, Lazdane G, et al. Relationship between pregnant women and their partners during COVID‐19 and the role of accompanying persons during childbirth. J Hosp Admin. 2021;10:1. [Google Scholar]
- 18. Kovale S, Teraudkalna M, Vasioleka B, Rasnaca K. Childbirth experience during the Covid‐19 pandemic in maternity care institutions in Latvia. Proc Int Sci Conf. 2021;4:368‐378. [Google Scholar]
- 19. Vasilevski V, Sweet L, Bradfield Z, et al. Receiving maternity care during the COVID‐19 pandemic: experiences of women's partners and support persons. Women Birth. 2022;35:298‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Perrotte V, Chaudhary A, Goodman A, Perrotte V, Chaudhary A, Goodman A. “At least your baby is healthy” obstetric violence or disrespect and abuse in childbirth occurrence worldwide: a literature review. Open J Obstet Gynaecol. 2020;10:1544‐1562. [Google Scholar]
- 21. International Confederation of Midwives . Women's rights in childbirth must be upheld during the coronavirus pandemic. 2020. Accessed February 28, 2022. https://www.internationalmidwives.org/assets/files/news‐files/2020/03/icm‐statement_upholding‐womens‐rights‐during‐covid19‐5e83ae2ebfe59.pdf
- 22. Human Rights in Childbirth . Human rights violations in pregnancy, birth and postpartum during the COVID‐19 pandemic. 2020. Accessed February 27, 2022. http://humanrightsinchildbirth.org/wp‐content/uploads/2020/05/Human‐Rights‐in‐Childbirth‐Pregnancy‐Birth‐and‐Postpartum‐During‐COVID19‐Report‐May‐2020.pdf
- 23. Lazzerini M, Covi B, Mariani I, et al. Quality of facility‐based maternal and newborn care around the time of childbirth during the COVID‐19 pandemic: online survey investigating maternal perspectives in 12 countries of the WHO European region. Lancet Reg Health Eur. 2022;13:100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453‐1457. [DOI] [PubMed] [Google Scholar]
- 25. Lazzerini M, Argentini G, Mariani I, et al. WHO standards‐based tool to measure women's views on the quality of care around the time of childbirth at facility level in the WHO European region: development and validation in Italy. BMJ Open. 2022;12:e048195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lazzerini M, Mariani I, Semenzato C, Valente EP. Association between maternal satisfaction and other indicators of quality of care at childbirth: a cross‐sectional study based on the WHO standards. BMJ Open. 2020;10:e037063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lazzerini M, Semenzato C, Kaur J, Covi B, Argentini G. Women's suggestions on how to improve the quality of maternal and newborn hospital care: a qualitative study in Italy using the WHO standards as framework for the analysis. BMC Pregnancy Childbirth. 2020;20:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zaigham M, Linden K, Sengpiel V, et al. Large gaps in the quality of healthcare experienced by Swedish mothers during the COVID‐19 pandemic: a cross‐sectional study based on WHO standards. Women Birth. 2022;35:619‐627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lazzerini M, Covi B, Mariani I, Giusti A, Pessa VE. Quality of care at childbirth: findings of IMAgiNE EURO in Italy during the first year of the COVID‐19 pandemic. Int J Gynecol Obstet. 2022;157:405‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient‐reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94‐104. [DOI] [PubMed] [Google Scholar]
- 31. National Institute for Health and Care Excellence . Intrapartum care for healthy women and babies. Clinical guideline [CG190]. 2017. Accessed February 9, 2022. www.nice.org.uk/guidance/cg190 [PubMed]
- 32. R Core Team . R: a language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R‐project.org/ [Google Scholar]
- 33. Sirina I, Strele I, Siksna I, Gardovska D. Eating patterns and food choices of Latvian infants during their first year of life. Medicina. 2018;54:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gianni ML, Bettinelli ME, Manfra P, et al. Breastfeeding difficulties and risk for early breastfeeding cessation. Nutrients. 2019;11:2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Briedite I, Ancane G, Jansone G. Opinions of postpartum women about the impact of pregnancy and childbirth on sexual life. JSM Sexual Med. 2017;2:1‐5. [Google Scholar]
- 36. Calis . Covid‐19: Riga Maternity Hospital and Pauls Stradins Clinical University Hospital restrict family births. Accessed February 28, 2022. https://www.delfi.lv/calis/jaunumi/covid‐19‐dzemdibu‐nams‐un‐stradinu‐slimnica‐ierobezo‐gimenes‐dzemdibas.d?id=51961649
- 37. Ravaldi C, Skoko E, Battisti A, Cericco M, Vannacci A. Abuse and disrespect in childbirth assistance in Italy: a community‐based survey. Eur J Obstet Gynecol Reprod Bio. 2018;224:208‐209. [DOI] [PubMed] [Google Scholar]
- 38. Castro R, Frías SM. Obstetric violence in Mexico: results from a 2016 National Household Survey. Violence Against Women. 2020;26:555‐572. [DOI] [PubMed] [Google Scholar]
- 39. Ghanbari‐Homayi S, Fardiazar Z, Meedya S, et al. Predictors of traumatic birth experience among a group of Iranian primipara women: a cross sectional study. BMC Pregnancy Childbirth. 2019;19:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Oladapo OT, Tunçalp BM, Lawrie TA, Portela A, Downe S, et al. WHO model of intrapartum care for a positive childbirth experience: transforming care of women and babies for improved health and wellbeing. BJOG. 2018;125:918‐922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Disease Prevention and Control Center (SPKC) . Covid‐19 statistics. 2022. Accessed January 23, 2022. https://www.spkc.gov.lv/lv/covid‐19‐statistika
- 42. Drandić D, Drglin Z, Mihevc B, et al. Women’s perspectives on the quality of hospital maternal and newborn care around the time of childbirth during the COVID‐19 pandemic: results from the IMAgiNE EURO study in Slovenia, Croatia, Serbia, and Bosnia‐Herzegovina. Int J Gynecol Obstet. 2022;. 159(Suppl 1):54‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arendt M, Tasch B, Conway F, et al. Quality of maternal and newborn care around the time of childbirth in Luxembourg during the COVID‐19 pandemic: Results of the IMAgiNE EURO study. Int J Gynecol Obstet. 2022. 159(Suppl 1):113‐125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Costa R, Barata C, Dias H, et al. Regional differences in the quality of maternal and neonatal care during the COVID‐19 pandemic in Portugal: results from the IMAgiNE EURO study. Int J Gynecol Obstet. 2022;. 159(Suppl 1):137‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hersoug Nedberg I, Skirnisdottir Vik E, Kongslien S, et al. Quality of health care around the time of childbirth during the COVID‐19 pandemic: Results from the IMAgiNE EURO study in Norway and trends over time. Int J Gynecol Obstet. 2022;159(Suppl 1):85‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Takehara K, Noguchi M, Shimane T, Misago C. A longitudinal study of women's memories of their childbirth experiences at five years postpartum. BMC Pregnancy Childbirth. 2014;14:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.


