Abstract
Objective
To describe the impact of the COVID‐19 pandemic on trends in incidence rates (IR) of diagnoses of eating disorders (ED) among adolescents and young adults.
Methods
Population‐based cohort study using primary care records of people aged 10–24 years between January, 2016 and December, 2021 in Catalonia, Spain. IRs were calculated monthly and grouped by the different stages of the COVID‐19 pandemic in Catalonia: (1) the pre‐lockdown (January, 2016–February, 2020), (2) lockdown (March–June, 2020) and, (3) post‐lockdown (July, 2020–December, 2021) periods. Incidence rate ratios (IRR) relative to the corresponding periods in 2018–2019 were calculated.
Results
A total of 1,179,009 individuals were included. The IR was 9.2 per 100,000 person‐months (95% confidence intervals [CI]: 8.9–9.5) during the pre‐lockdown period. It decreased during the lockdown period (6.3 per 100,000 person‐months [5.5–7.3]), but substantially increased during the following period (19.4. per 100,000 person‐months [18.7–20.1]). While large reductions in IRs were observed for both sexes during the lockdown period (IRR 95% CI: 0.65 [0.54–0.78] in females and 0.46 [0.29–0.71] in males), substantial increases during the post‐lockdown period were limited to females, and were particularly pronounced among those aged 10–14 and 15–19 years (2.50 [2.23–2.80] and 2.29 [2.07–2.54], respectively).
Discussion
The COVID‐19 pandemic has resulted in a substantial increase in ED diagnoses, primarily driven by higher rates among adolescent females.
Public Significance
This population‐based cohort study demonstrated a substantial increase in incidence rates of eating disorders in primary care following the end of lockdown in Catalonia, Spain, with adolescent girls seen to be most affected.
Keywords: COVID‐19, eating disorders, epidemiology
1. INTRODUCTION
The COVID‐19 pandemic presented a public health emergency worldwide. Unprecedented restrictions were adopted to reduce the community spread of the virus, causing major disruptions in socialization and daily routines. This holds true especially for adolescents and young adults, whose lives have been dramatically restricted by the pandemic (Kazi & Mushtaq, 2021; Lee, 2020). Prolonged school closures and reduced interactions with peers, along with family stressors and missed or delayed social and educational milestones, are likely to have negatively impacted their physical and mental well‐being. Indeed, the rapidly accumulating evidence on the negative impact of the COVID‐19 on youth mental health suggests that psychological distress increased considerably during the pandemic (Racine et al., 2021; von Soest et al., 2022).
The impact of the pandemic on eating disorders (ED) among adolescents and young adults has not gone unnoticed (Zipfel et al., 2022). An increase in incidence rates of EDs has been reported in different countries, often occurring with more severe symptomatology and increased rates of in‐patient care (Agostino et al., 2021; Asch et al., 2021; Gilsbach et al., 2022; Haripersad et al., 2021; Lin et al., 2021; Spettigue et al., 2021; Taquet et al., 2021). Several factors related to the COVID‐19 pandemic have been identified as potentially detrimental to ED risk and recovery. Some of those are food insecurity (e.g., reduced access to “safe” foods or increased urge to binge), exercise limitations (e.g., increased weight concerns), increased media consumption (e.g., exposure to fatphobic messages or stressful media coverage), and fear of contagion from COVID‐19 (e.g., restrictive diets focused on increased immunity) (Cooper et al., 2022; Rodgers et al., 2020). Furthermore, the COVID‐19 pandemic and its associated control measures have negatively affected protective factors against EDs, such as structured routines, social support and healthy coping mechanisms, and have hampered access to healthcare services (Rodgers et al., 2020).
In Spain, a national lockdown was implemented on March 14, 2020 following the declaration of the State of Alarm (Real Decreto 436/2020, 2020). The freedom of movement was limited to a few exceptions, such as grocery shopping, health emergencies or essential work. Moreover, it forced the suspension of all non‐necessary commercial and recreational activities. Educational activities were provided when possible by on‐line platforms, and educational institutions remained closed until the following academic year, which started in September 2021 (Viguria & Casamitjana, 2021). Population‐wide restrictions, such as mandatory mask use, limitations in social gatherings and in the capacity of commercial establishments and events continued once lockdown measures were lifted on June 21, 2020 (Real Decreto 555/2020, 2020). Strict nationwide measures were implemented from October 25, 2020 to May 9, 2021 due to a resurgence of COVID‐19 cases, including mobility restrictions and curfew hours (Real Decreto 926/2020, 2020). The timeline of the restrictions implemented during this period in Catalonia, Spain, has been described in further detail elsewhere (Perramon et al., 2021). While successive COVID‐19 waves occurred during the following months (Generalitat de Catalunya, 2022a), measures were progressively eased as the pandemic continued. However, some restrictions persisted throughout the end of the year (e.g., mask use, limitations in social gatherings and events, closure of indoor nightlife venues).
To date, few longitudinal studies have studied the potential effect of the COVID‐19 pandemic on ED diagnoses (Asch et al., 2021; Bilu et al., 2022; Haripersad et al., 2021; Lin et al., 2021; Taquet et al., 2021). However, most of these were focused on the short‐ or mid‐term effects of the pandemic, and none included incidence rates stratified by socioeconomic status or in European countries (Asch et al., 2021; Haripersad et al., 2021; Lin et al., 2021; Taquet et al., 2021). Understanding the long‐term consequences of COVID‐19 on EDs among adolescents and young adults and how they differ by sociodemographic characteristics could provide valuable information to plan interventions and prevention strategies to better support those particularly affected by the pandemic. In the present study, we aim to describe the impact of the COVID‐19 pandemic on incidence trends of EDs among adolescents and young adults through the end of 2021 in a large primary care longitudinal dataset representative of the population living in Catalonia, Spain.
2. METHODS
2.1. Study design
We conducted an open cohort study based on electronic health records (EHR) from January 1, 2016 to December 31, 2021 in Catalonia, Spain. We described the first wave of the pandemic in Spain as the lockdown period given that it was the only wave where a stay‐at‐home order was issued. The study periods were defined as: (1) the pre‐lockdown period, from January 1, 2016 to February 29, 2020; (2) the lockdown period, from March 1, 2020 to June 30, 2020; (3) the post‐lockdown period, from July 1, 2020 to December 31, 2021.
2.2. Setting, data source, and study participants
The Catalan healthcare system is publicly financed and provides universal health coverage to people living in Catalonia. Primary care is the main entry point for accessing public nonemergency health‐related services, and provides continuous care throughout the life span. Pediatric services in primary care are provided up until age 15, when adolescents are transferred to adult‐oriented services.
Data were obtained from the Information System for Research in Primary Care (SIDIAP; www.sidiap.org), a primary care database that contains pseudo‐anonymized EHR from approximately 75% of the population in Catalonia, Spain. SIDIAP has been shown to be representative of the Catalan population in terms of age, sex, and geographic distribution (Recalde et al., 2022). SIDIAP has been linked to COVID‐19 RT‐PCR test results, hospital records, and regional mortality data, and it has been mapped to the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) (Burn et al., 2021).
All individuals aged 10–24 years old during the study period with at least 1 year of prior history at the index date (i.e., the day they entered the cohort) and with no diagnosis of ED prior to the index date were included. Individuals were followed from the start of the study (January 1, 2016), the start of the observation period (the day in which they were registered on the database) or the day after they turned 10 years, whichever came last. Participants were followed to the earliest of the following: first incident ED diagnosis, end of data availability (December 31, 2021), the day on which participants turned 25 years, or until they were transferred out of the database or died.
2.3. Variables
We considered the first incident ED diagnosis as the outcome of interest. Diagnosis of EDs was made at primary care facilities based on standard practice, and were registered by general practitioners or pediatricians during their daily practice. EDs were identified on the basis of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Clinical Modification (ICD‐10‐CM) codification system. All descendants of the F50 code were considered, including anorexia nervosa (F50.1), bulimia nervosa (F50.2), other specified EDs including binge‐eating disorder and avoidant restrictive food intake disorder (F50.8), and unspecified EDs (F50.9).
We also extracted information on sex (female, male) and age. The age range included in this study was defined according to the World Health Organization definition of adolescents and young adults (10–19 and 15–24 years, respectively) (World Health Organization, 2022), and was further divided into three age groups (10–14, 15–19, and 20–24 years).
We assessed socioeconomic status using the Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales (MEDEA) deprivation index, which is calculated at the census tract level and it is categorized into quintiles, with the first and fifth quintiles representing the least and most deprived areas (Domínguez‐Berjón et al., 2008). We included a rural category, as the MEDEA deprivation index is only available for individuals living in urban areas of Catalonia.
2.4. Statistical methods
We summarized the characteristics of participants at their index date, with categorical variables presented as number and percentage and numerical variables presented as median and interquartile range (IQR). This analysis was descriptive in nature, with the explicit intention of exploring new‐onset ED trajectories among adolescents and young adults in Catalonia, Spain. Incidence rates (IR) with 95% confidence intervals (CI) were calculated for each month and study period by dividing the number of new cases of EDs by 100,000 person‐months at risk. Incidence rate ratios (IRR) with 95% CI were calculated to estimate differences in the incidence of each strata of the population during the lockdown and post‐lockdown periods compared to the same periods from March, 2018 to December, 2019. We stratified IRs and IRRs by sex (males and females), age groups (10–14, 15–19, and 20–24 years; calculated monthly) and the MEDEA deprivation index. We used 95% CI to interpret differences between study periods. When the 95% CIs did not overlap, we understood the differences between time periods to be significant (p < 0.05).
To test the robustness of our findings, we re‐calculated IRRs using data from March, 2016 to December, 2017 as the comparison period.
Following governance requirements, results with less than 5 individuals were blinded and reported as <5.
All analyses were performed in R v 4.1.
3. RESULTS
We identified 1,367,785 individuals aged 10–24 years during the study period. We excluded 11,017 individuals with an ED diagnosis before the index date, and 177,759 with less than a year of prior history (Figure S1). The final study population included 1,179,009 people, who contributed 58,506,600 person‐months of data. Among all participants, 48.3% were female, and the median age at inclusion was 13.0 (IQR: 10.0–19.0) years (Table 1).
TABLE 1.
Population characteristics of adolescents and young adults included in the study, 2016–2021
| Total (n = 1 179 009) | |
|---|---|
| Age at index date, median (IQR), years | 13.0 (10.0,19.0) |
| Females, n (%) | 569 261 (48.3) |
| Sex: females | |
| Age group at entry (years), n (%) | |
| 10–14 | 314 823 (55.3) |
| 15–19 | 125 953 (22.1) |
| 20–24 | 128 485 (22.6) |
| Sex: males | |
| Age group at entry (years), n (%) | |
| 10–14 | 334 485 (54.9) |
| 15–19 | 137 313 (22.5) |
| 20–24 | 137 950 (22.6) |
| MEDEA deprivation index, n (%) ( a ) | |
| First, least deprived | 168 451 (14.3) |
| Second | 168 044 (14.3) |
| Third | 167 388 (14.2) |
| Fourth | 1 68 473 (14.3) |
| Fifth, most deprived | 177 897 (15.1) |
| Rural | 200 793 (17.0) |
| Missing | 127 963 (10.9) |
| Years of prior history at index date, median (IQR) | 10.0 (10.0,10.0) |
| Years contributed to the cohort, median (IQR) | 4.9 (2.4, 6.0) |
Abbreviations: IQR, Interquartile range; MEDEA, Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales.
Rural was included as a category since the index cannot be calculated for people living in rural areas.
We identified 6994 individuals with a first diagnosis of an ED during the study period. The unspecified form of EDs was the most common recorded diagnosis (66.1%), and was followed by anorexia (21.5%) and bulimia (11.3%) (Table 2). Other specified disorders only represented 2.5% of the recorded diagnoses. More than 85% of the cases diagnosed were females with the exception of other specified EDs, in which they accounted for 74.1% of the diagnoses (Table 2). The median age at diagnosis was 15.0 (IQR: 14.0–18.0), and was similar for all disorder types except for bulimia (17.0 [IQR: 15.0–20.0]). For socioeconomic status, we found a gradient in the number of cases of anorexia, with the highest reported among the second least deprived quintile (17.2%), and the lowest among the most deprived (10.9%). This gradient was reversed when analyzing other specified EDs (10.6% and 19.4% among the least and most deprived, respectively) (Table 2).
TABLE 2.
Population characteristics of adolescents and young adults diagnosed with eating disorders according to disorder type, 2016–2021
| Eating disorders (any) | Anorexia | Bulimia | Other eating disorders | Unspecified eating disorders | |
|---|---|---|---|---|---|
| Cases, n (row %) ( a ) | 6994 (100) | 1494 (21.5) | 783 (11.3) | 170 (2.5) | 4591 (66.1) |
| Age at diagnosis, median (IQR), years | 15.0 (14.0, 18.0) | 15.0 (14.0, 17.0) | 17.0 (15.0, 20.0) | 15.0 (13.0, 18.0) | 15.0 (13.0, 17.0) |
| Females, n (%) | 6085 (87.0) | 1362 (91.2) | 688 (87.9) | 126 (74.1) | 3949 (86.0) |
| Sex: females | |||||
| Age group at diagnosis (years), n (%) | |||||
| 10–14 | 2276 (37.4) | 503 (36.9) | 101 (14.7) | 59 (46.8) | 1627 (41.2) |
| 15–19 | 2838 (46.6) | 685 (50.3) | 374 (54.4) | 48 (38.1) | 1754 (44.4) |
| 20–24 | 971 (16.0) | 174 (12.8) | 213 (31.0) | 19 (15.1) | 568 (14.4) |
| Sex: males | |||||
| Age group at diagnosis (years), n (%) | |||||
| 10–14 | 469 (51.6) | 62 (47.0) | 20 (21.1) | 22 (50) | 367 (57.2) |
| 15–19 | 325 (35.8) | 60 (45.5) | 47 (49.5) | 15 (34.1) | 204 (31.4) |
| 20–24 | 115 (12.7) | 10 (7.6) | 28 (29.5) | 7 (15.9) | 71 (11.1) |
| MEDEA deprivation index, n (%) ( b ) | |||||
| First, least deprived | 990 (14.2) | 250 (16.7) | 110 (14.0) | 18 (10.6) | 616 (13.4) |
| Second | 1116 (16.0) | 257 (17.2) | 133 (17.0) | 19 (11.2) | 713 (15.5) |
| Third | 1074 (15.4) | 199 (13.3) | 105 (13.4) | 29 (17.1) | 748 (16.3) |
| Fourth | 957 (13.7) | 168 (11.2) | 107 (13.7) | 26 (15.3) | 661 (14.4) |
| Fifth, most deprived | 944 (13.5) | 163 (10.9) | 115 (14.7) | 33 (19.4) | 642 (14.0) |
| Rural | 1194 (17.1) | 285 (19.1) | 126 (16.1) | 29 (17.1) | 762 (16.6) |
| Missing | 719 (10.3) | 172 (11.5) | 87 (11.1) | 16 (9.4) | 449 (9.8) |
| Study period, cases, n (row %) ( a ) | |||||
| Pre‐COVID | 3832 (100) | 856 (22.3) | 506 (13.2) | 89 (2.3) | 2405 (63.3) |
| Lockdown | 218 (100) | 49 (22.5) | 15 (6.9) | <5 | 151 (69.3) |
| Post‐lockdown | 2944 (100) | 589 (20.0) | 262 (8.9) | 77 (2.6) | 2035 (69.1) |
Abbreviations: IQR, interquartile range; MEDEA, Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales.
Not mutually exclusive. Counts are limited to diagnoses performed at the first day of a recorded diagnosis of an eating disorder (i.e., more than one diagnosis can be recorded at the same day). ICD‐10‐CM codes were used to identify forms of EDs. The F50.1 and F50.2 codes were used to define anorexia nervosa and bulimia nervosa, respectively. Conditions classified under the F50.8 diagnostic code were considered as other eating disorders, and included binge eating disorder and avoidant restrictive food intake disorder, among others. Conditions classified under the F50.9 diagnostic code were considered as unspecified eating disorders.
Rural was included as a category since theindex cannot be calculated for people living in rural areas.
3.1. Incidence rates
The IR of EDs was 9.2 per 100,000 person‐months (95% CI 8.9–9.5) during the pre‐lockdown period. Monthly IRs exhibited pronounced fluctuations, but remained stable between 2016 and 2019 when using yearly aggregated data (Table S1; Figure S2). The IR decreased during the lockdown period (6.3 per 100,000 person‐months [5.5–7.3]), but was double the figures observed before the pandemic during the post‐lockdown period (19.4 per 100,000 person‐months [18.7–20.1]) (Tables S3 and S4).
The impact of the COVID‐19 pandemic on incidence trends of EDs was particularly pronounced among females (Figure 1). Rates during the pre‐pandemic period were 15.9 per 100,000 person‐months (15.4–16.5) among females and 2.9 per 100,000 person‐months (2.6–3.1) among males (Table S2). Among females, the IR was substantially reduced in March, 2020, and reached its minimum value in April, 2020 (5.2 per 100,000 person‐months [3.2–8.0]). Conversely, the IR steadily increased from May, 2020 to March, 2021 despite a few minor fluctuations. This increase was particularly profound from September, 2020 onwards (54.4 per 100,000 person‐months [47.4–62.1] in March, 2021). The IR decreased during the following months, and substantially dropped in August, 2021 (23.9 [19.4–29.3]). The IR increased during the following months, reaching its second peak in November, 2021 (57.1 [49.8–65.2]). Females up to 19 years old showed higher IR compared to those aged 20–24 years across study periods, and showed abrupt changes in monthly IRs following the lockdown announcement in March, 2020 (Figure 2).
FIGURE 1.
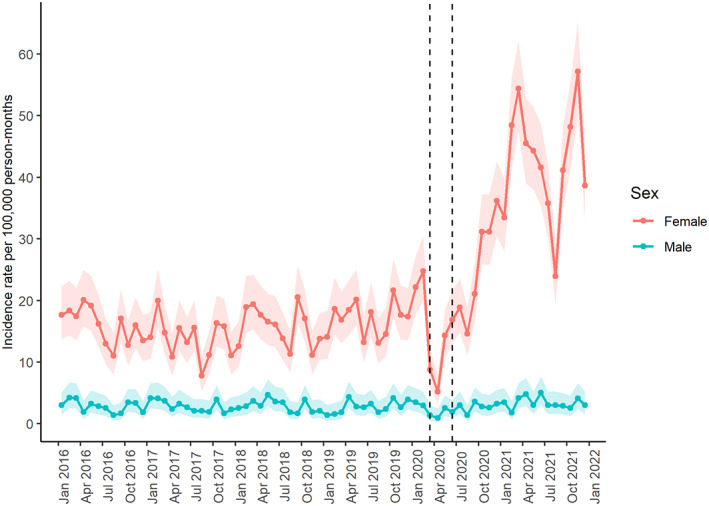
Monthly incidence rates stratified by sex. Points indicate monthly incidence rates of eating disorders from January, 2016 to December, 2021. Shaded areas represent 95% confidence intervals. The lockdown period is delimited by two vertical lines, which indicate March, 2020 and June, 2020.
FIGURE 2.
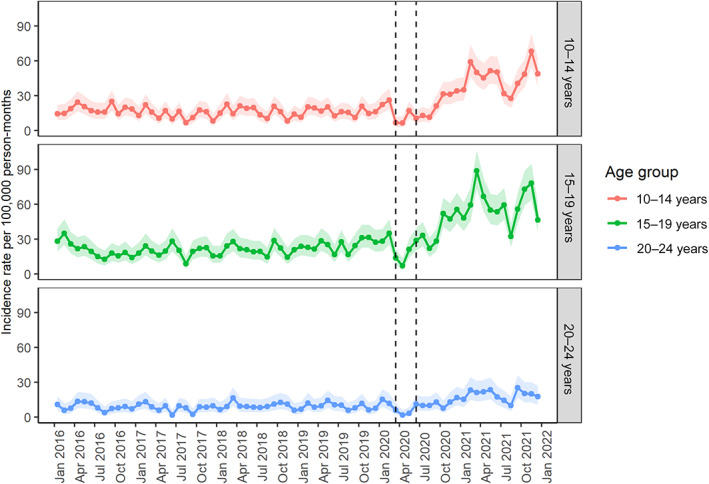
Monthly incidence rates stratified by age groups in females. Points indicate monthly incidence rates of eating disorders from January, 2016 to December, 2021. Shaded areas represent 95% confidence intervals. The lockdown period is delimited by two vertical lines, which indicate March, 2020 and June, 2020.
The IR of EDs among males slightly fluctuated over the study period, ranging from 1.0 per 100,000 person‐months (0.3–2.5) in March, 2020 to 5.1 per 100,000 person‐months (3.1–7.7) in April, 2021 (Figure 1). Although we observed some similarities between trends in both sexes (i.e., IR decreased in March, 2020 but increased in the following months), increases in the IR among males were less pronounced than those observed in females (Figure 1).
A similar trend in IRs was also observed across MEDEA deprivation quintiles although fluctuations over time differed across subgroups (Figure S3). Information on the number of events, person‐time at risk, and incidence rates over study periods by sex, age, and socioeconomic status is described in Appendix S1 (Tables S2–S4).
3.2. Incidence rate ratios
Compared to the corresponding period in 2018–2019, the overall IR of EDs decreased during the lockdown period (IRR: 0.61 [0.51–0.73]), and increased during the following period (2.11 [1.98–2.25]) (Table S5). The initial decrease in IR during lockdown occurred in both sexes, but was particularly pronounced among males (0.46 [0.29–0.71] in males versus 0.65 [0.54–0.78] in females). The IR substantially increased among females during the post‐lockdown period (2.28 [2.12–2.44]), but suggested a lower difference in incidence among males (1.20 [1.00–1.45]) (Figure 3; Table S5).
FIGURE 3.
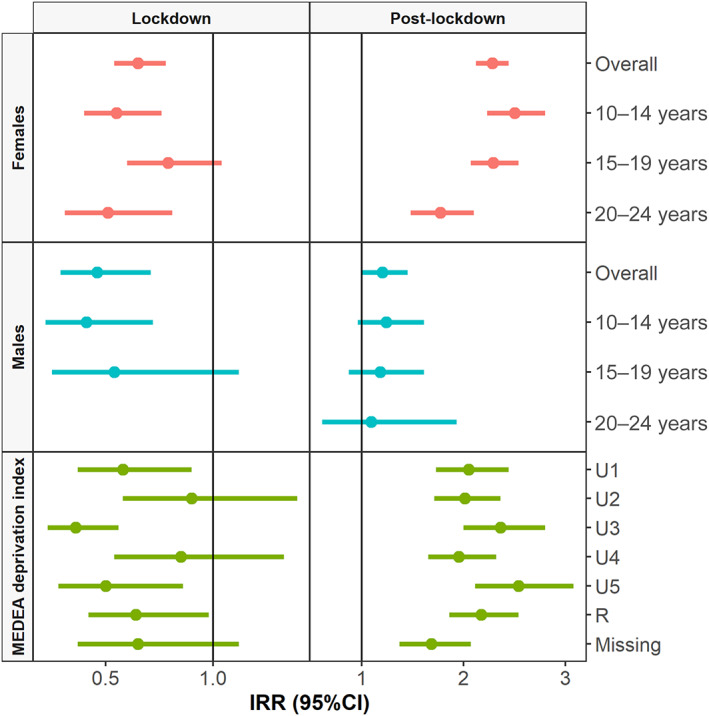
Incidence rate ratios (IRRs) with 95 % confidence intervaks (CI) of first recorded cases of eating disorders overall and stratified by sex, age group and deprivation index. IRRs were calculated by dividing the incidence rate obtained for each strata during the COVID‐19 periods by the incidence rate obtained for the same strata during the same periods in 2018 and 2019. IRR corresponding to events with less than five occurrences have been omitted for privacy reasons. MEDEA: Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales; R, rural; U, urban.
During the lockdown period, reductions were found across age groups, with the biggest drops observed among females aged 10–14 and 20–24 years (0.55 [0.40–0.76] and 0.51[0.31–0.81], respectively), and males aged 10–14 years (0.41 [0.22–0.72]). Males aged 20–24 years obtained less than five occurrences and were blinded following the requirement of information governance (Table S5). Compared to the corresponding period in 2018–2019, IRs substantially increased during the post‐lockdown period and more than doubled among females aged 10–14 and 15–19 years (2.50 [2.23–2.80] and 2.29 [2.07–2.54], respectively). Among males, this increase was much less pronounced for all age groups (Figure 3; Table S5).
For socioeconomic status, we observed a drop in IRs during the lockdown period across deprivation quintiles and rural areas (Figure 3). Compared to the corresponding period in 2018 and 2019, IRs across deprivation quintiles increased during the post‐lockdown period and doubled among most subgroups (Figure 3). The most deprived quintile of the population obtained the highest increase in IR during the post‐lockdown period (2.54 [2.11–3.08]) compared to the corresponding period in 2018–2019. Rural areas exhibited a similar pattern, with a substantial increase in IR during the post‐lockdown period (2.17 [1.86–2.54]) (Table S5).
We found similar results in sensitivity analysis when computing IRRs stratified by age and sex groups using data from 2016 to 2017 as the comparison period (Table S6). However, IRRs differed when stratifying results by deprivation quintiles. For instance, while absolute figures did not account for large differences, the most deprived quintile of the population obtained the highest increase in IRRs during the post‐lockdown period in the main analysis, but the lowest increase when comparing IRs to 2016–2017 data (Table S6). Notwithstanding these variations, the overall pattern was consistent across deprivation quintiles in both analyses (i.e., decreased IR during lockdown and substantial increases afterwards) (Table S6).
4. DISCUSSION
In this population‐based cohort study of more than one million adolescents and young adults living in Catalonia, we observed a sustained and pronounced increase in the incidence of EDs diagnosed in primary care following the end of lockdown, which was preceded by a brief decrease in diagnoses in the early months of the lockdown measures in Catalonia. This increase was unequal across the study population, with females, particularly those aged 10–19 years, more affected than others.
The increase in incidence of EDs observed in this study is consistent with growing literature describing worsening EDs symptoms during the pandemic (Devoe et al., 2022). The temporary reduction in diagnoses of EDs in March–April, 2020 observed in this study is in line with the substantial drop in all‐cause diagnoses observed during the first months of the pandemic in Catalonia (Pifarré I Arolas et al., 2021). We observed a sustained increase in the incidence rates of EDs from May, 2020 to March, 2021. Given that health care systems were heavily disrupted at the onset of the pandemic, we hypothesize that the steep upward trend in incidence rates after September, 2020 is partially to be explained by the late reporting of prevalent cases developed during the first wave of the pandemic. This increase might likely reflect the accumulated effect of the COVID‐19 pandemic on EDs, and the increasing number of people who presented to care once the immediate effects of the pandemic were lessened. The fluctuations in incidence rates observed throughout the second half of 2021 must be interpreted with caution. Incidence rates peaked in March and November, 2021, with substantial drops in August and December of the same year. We hypothesize that these fluctuations could be partially explained by seasonal effects (i.e., low utilization of services during the holidays), as other diagnoses recorded in SIDIAP have exhibited similar patterns (Raventós et al., 2022). While seasonal patterns were also observed during the pre‐pandemic period, these variations seemed to be more pronounced during the post‐lockdown period, which could respond to an accentuated effect of seasonality due to higher incidence rates (Moltchanova et al., 2009). The afterwards increase in incidence rates, such as the one observed from September to November 2021, could be due to the accumulation of cases and late reporting rather than to the detection of new cases. Nevertheless, the overall higher IRs of ED diagnoses in the post‐lockdown period suggest that the COVID‐19 pandemic and its associated control measures are still affecting ED diagnoses in our setting. In this line, the recovery to pre‐pandemic levels is far from complete. Further evidence is required to assess whether trends in the near future will continue to reflect similar patterns to those observed during the pre‐pandemic period.
Our results align with other EHR‐based studies reporting increased IRs of EDs during the COVID‐19 pandemic (Asch et al., 2021; Taquet et al., 2021). A large cohort study including more than 5 million patients mainly from the United States, found that IRs of EDs steadily increased from May, 2020 to January, 2021, after a brief initial decline in diagnoses in the early months of the pandemic. Similar to our study, they found that the increased risk of EDs during the pandemic was limited to females and was greatest for adolescents aged 10–19 years old (Taquet et al., 2021). Another US study including more than 3 million commercially insured individuals examined trends in health care for ED from 2018 to 2020, and found an increase in the number of individuals receiving outpatient care during the pandemic. Furthermore, they found a strong increase in the number and length of inpatient stays related to these conditions (Asch et al., 2021). Increases in the number of ED‐related medical hospitalizations have also been reported in other studies (Agostino et al., 2021; Gilsbach et al., 2022; Haripersad et al., 2021; Lin et al., 2021; Spettigue et al., 2021). None of these studies stratified their results by socioeconomic status. Emerging evidence based on EHR data from Israel also suggests a significant rise in EDs diagnoses among adolescents aged 12–17 years old, with higher increases among those with medium and high socioeconomic status (Bilu et al., 2022). In the present study, the most deprived quintile of the population obtained the highest increase in incidence rates during the post‐lockdown period compared to those obtained in 2018–2019. However, these results must be interpreted with caution, as our study failed to identify consistent socioeconomic differences in risk when using different study years as the comparison period to calculate IRRs.
4.1. Strengths and limitations
The main strength of this study is the large sample size of the SIDIAP database, which is representative of the population living in Catalonia, and the availability of longitudinal data. In addition, our study investigates the COVID‐19‐related effects up to December, 2021, providing detailed data across sociodemographic strata up to 22 months after the onset of the COVID‐19 pandemic in Catalonia. However, we acknowledge some limitations. First, our results might likely represent an underestimation of the true burden of newly diagnosed EDs. Our data is limited to diagnoses recorded in primary care, and therefore it does not capture cases diagnosed in mental health services, emergency care or in‐patient care. Although primary care is the first‐point of care within the healthcare system, some people might have experienced barriers to access outpatient care during the pandemic. Accordingly, delayed care might have eventually led to an increased use of emergency services or in‐patient care. Therefore, we might have missed cases among patients who directly accessed those services. In terms of mental health services, referrals must be indicated by a general practitioner or a pediatrician in primary care. Although referrals from primary care must include a recorded diagnosis, some individuals might have been referred to mental health services through other resources, such as psycho‐pedagogical services in educational settings or social services. Moreover, individuals already using mental health services due to other mental health problems might directly access care without requiring a new referral from their primary care physician. Given that EDs are associated with both prior and later psychiatric disorders (Momen et al., 2022; Plana‐Ripoll et al., 2019), we might have missed cases among patients already receiving care in specialized mental health services. In addition, 28.7% of people in Catalonia in 2021 were estimated to have double health coverage, which translates into access to both public and private healthcare services (Generalitat de Catalunya, 2022b). Thus, we might have missed cases who accessed private healthcare services or other forms of help without interacting with the public healthcare system. Third, our study was underpinned by EHR of routinely collected primary care data, and therefore, there is a potential risk of misclassification of ED diagnoses. However, this risk is minimized in our analysis as the IRs depicted is for all forms of EDs and, more importantly, we do not expect the degree of misclassification to have changed during the study period. Our data do not accurately capture information on symptomatology or severity of illness at presentation, which was beyond the scope of our study. Additional data might allow a more detailed study to determine whether the acuity of EDs and its disorder subtypes have changed during the pandemic in our setting. Lastly, we found inconsistencies in ED risk across deprivation quintiles using different time periods to compare incidence rates over the COVID‐19 periods. Given that the MEDEA deprivation index was only available for individuals living in urban areas, socioeconomic differences in rural areas were not explored. Further evidence is required to disentangle potential socioeconomic or geographic differences in the impact of the COVID‐19 pandemic on EDs.
5. CONCLUSION
We found a substantial increase in incidence rates of EDs in primary care after the initial phase of the COVID‐19 pandemic, which was particularly pronounced in adolescent females. Our results are of importance to better understand the effect of the COVID‐19 pandemic on incidence trends of EDs among adolescents and young adults in Catalonia and to identify groups that are most in need of attention.
AUTHOR CONTRIBUTIONS
Berta Raventós: Conceptualization; data curation; formal analysis; investigation; methodology; visualization; writing – original draft. Alicia Abellan: Writing – review and editing. Andrea Pistillo: Writing – review and editing. Carlen Reyes: Investigation; writing – review and editing. Edward Burn: Conceptualization; formal analysis; investigation; methodology; software; supervision; writing – review and editing. Talita Duarte‐Salles: Conceptualization; funding acquisition; investigation; methodology; project administration; resources; supervision; writing – review and editing.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors. TDS acknowledges receiving financial support from the Instituto de Salud Carlos III (ISCIII; Miguel Servet 2021: CP21/00023).
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ETHICS STATEMENT
This project was approved by the Clinical Research Ethics Committee of the IDIAPJGol (project code: 21/052‐PCV).
Supporting information
Appendix S1: Supporting information
Figure S1. Flow chart
Figure S2. Trends during the pre‐pandemic period
Table S1. Annual incidence rates of eating disorders
Table S2. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the pre‐lockdown period
Table S3. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the lockdown period
Table S4. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the post‐lockdown period
Figure S3: Monthly incidence rates stratified by the MEDEA deprivation index
Table S5. Incidence rate ratios (IRRs) of first recorded cases of eating disorders
Table S6. Sensitivity analysis for incidence rate ratios (IRRs) of first recorded cases of eating disorders.
ACKNOWLEDGMENTS
This study was carried out as part of the Doctoral Program in Biomedical Research Methodology and Public Health at the Autonomous University of Barcelona. The authors would like to acknowledge the efforts of all public healthcare workers in Catalonia who daily register information in the populations' electronic health records.
Raventós, B. , Abellan, A. , Pistillo, A. , Reyes, C. , Burn, E. , & Duarte‐Salles, T. (2023). Impact of the COVID‐19 pandemic on eating disorders diagnoses among adolescents and young adults in Catalonia: A population‐based cohort study. International Journal of Eating Disorders, 56(1), 225–234. 10.1002/eat.23848
Action Editor: Ruth Striegel Weissman
Edward Burn and Talita Duarte‐Salles are Joint senior authorship.
Contributor Information
Berta Raventós, Email: braventos@idiapjgol.info.
Talita Duarte‐Salles, Email: tduarte@idiapjgol.org.
DATA AVAILABILITY STATEMENT
In accordance with current European and national law, the data used in this study is only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online (https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure) or by contacting SIDIAP (sidiap@idiapjgol.org).
REFERENCES
- Agostino, H. , Burstein, B. , Moubayed, D. , Taddeo, D. , Grady, R. , Vyver, E. , Dimitropoulos, G. , Dominic, A. , & Coelho, J. S. (2021). Trends in the incidence of new‐onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID‐19 pandemic in Canada. JAMA Network Open, 4(12), e2137395. 10.1001/jamanetworkopen.2021.37395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asch, D. A. , Buresh, J. , Allison, K. C. , Islam, N. , Sheils, N. E. , Doshi, J. A. , & Werner, R. M. (2021). Trends in US patients receiving care for eating disorders and Other common behavioral health conditions before and during the COVID‐19 pandemic. JAMA Network Open, 4(11), e2134913. 10.1001/jamanetworkopen.2021.34913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilu, Y. , Flaks‐Manov, N. , Bivas‐Benita, M. , Akiva, P., Kalkstein, N., Yehezkelli, Y., Mizrahi‐Reuveni, M., Ekka‐Zohar, A., David, S. Shapiro Ben, Lerner, U., Bodenheimer, G., & Greenfeld, S. (2022) . Data‐driven assessment of adolescents' mental health during the COVID‐19 pandemic. medRxiv. 10.1101/2022.01.06.22268809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burn, E. , Fernández‐Bertolín, S. , Voss, E.A , Blacketer, C., Aragón, M. Recalde, M., Roel, E., Pistillo, A., Raventós, B., Reye,s C., van Sandijk, S., Halvorsen, L., Rijnbeek, P.R., Duarte‐Salles. (2021). Establishing and characterising large COVID‐19 cohorts after mapping the information system for research in primary care in Catalonia to the OMOP common data model. medRxiv. 10.1101/2021.11.23.21266734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, M. , Reilly, E. E. , Siegel, J. A. , Coniglio, K. , Sadeh‐Sharvit, S. , Pisetsky, E. M. , & Anderson, L. M. (2022). Eating disorders during the COVID‐19 pandemic and quarantine: an overview of risks and recommendations for treatment and early intervention. Eating Disorders, 30(1), 54–76. 10.1080/10640266.2020.1790271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devoe, D.J. , Han, A. , Anderson, A. , Katzman, D.K. , Patten, SB , Soumbasis, A. , Flanagan, J., Paslakis, G., Vyver, E., Marcoux, G., & Dimitropoulos, G. (2022). The impact of the COVID‐19 pandemic on eating disorders: A systematic review. The International Journal of Eating Disorders. 10.1002/eat.23704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domínguez‐Berjón, M. F. , Borrell, C. , Cano‐Serral, G. , Esnaola, S., Nolasco, A., Pasarín, M.I., Ramis, R., Saurina, C., & Escolar‐Pujolar, A. (2008). Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto MEDEA) [Constructing a deprivation index based on census data in large Spanish cities (the MEDEA project)]. Gaceta Sanitaria, 22(3), 179–187. 10.1157/13123961 [DOI] [PubMed] [Google Scholar]
- Generalitat de Catalunya . (2022a). Salut/Dades COVID. Accessed September 15, 2022. https://dadescovid.cat/
- Generalitat de Catalunya . (2022b). Health status, health‐related behaviours and health service utilisation in Catalonia: ESCA 2021 main results. Executive Summary. Accessed September 15, 2022. https://salutweb.gencat.cat/web/.content/_departament/estadistiques-sanitaries/enquestes/Enquesta-de-salut-de-Catalunya/Resultats-de-lenquesta-de-salut-de-Catalunya/documents/2021/summary-ESCA-2021.pdf
- Gilsbach, S. , Plana, M. T. , Castro‐Fornieles, J. , Gatta, M. , Karlsson, G. P. , Flamarique, I. , Raynaud, J. P. , Riva, A. , Solberg, A. L. , van Elburg, A. A. , Wentz, E. , Nacinovich, R. , & Herpertz‐Dahlmann, B. (2022). Increase in admission rates and symptom severity of childhood and adolescent anorexia nervosa in Europe during the COVID‐19 pandemic: data from specialized eating disorder units in different European countries. Child and Adolescent Psychiatry and Mental Health, 16(1), 46. 10.1186/s13034-022-00482-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haripersad, Y. V. , Kannegiesser‐Bailey, M. , Morton, K. , Skeldon, S. , Shipton, N. , Edwards, K. , Newton, R. , Newell, A. , Stevenson, P. G. , & Martin, A. C. (2021). Outbreak of anorexia nervosa admissions during the COVID‐19 pandemic. Archives of Disease in Childhood, 106(3), e15. 10.1016/j.jadohealth.2021.05.019 [DOI] [PubMed] [Google Scholar]
- Kazi, F. , & Mushtaq, A. (2021). Adolescents navigating the COVID‐19 pandemic. Lancet Child & Adolescent Health, 5(10), 692–693. 10.1016/S2352-4642(21)00279-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. (2020). Mental health effects of school closures during COVID‐19. Lancet Child & Adolescent Health, 4(6), 421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, J. A. , Hartman‐Munick, S. M. , Kells, M. R. , Milliren, C. E. , Slater, W. A. , Woods, E. R. , Forman, S. F. , & Richmond, T. K. (2021). The impact of the COVID‐19 pandemic on the number of adolescents/young adults seeking eating disorder‐related care. The Journal of Adolescent Health, 69(4), 660–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moltchanova, E. V. , Schreier, N. , Lammi, N. , & Karvonen, M. (2009). Seasonal variation of diagnosis of Type 1 diabetes mellitus in children worldwide. Diabetic Medicine, 26(7), 673–678. 10.1111/j.1464-5491.2009.02743.x [DOI] [PubMed] [Google Scholar]
- Momen, N. C. , Plana‐Ripoll, O. , Yilmaz, Z. , Thornton, L. M. , McGrath, J. J. , Bulik, C. M. , et al. (2022). Comorbidity between eating disorders and psychiatric disorders. The International Journal of Eating Disorders, 55(4), 505–517. 10.1002/eat.23687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perramon, A. , Soriano‐Arandes, A. , Pino, D. , Lazcano, U. , Andrés, C. , Català, M. , Gatell, A. , Carulla, M. , Canadell, D. , Ricós, G. , Riera‐Bosch, M. T. , Burgaya, S. , Salvadó, O. , Cantero, J. , Vilà, M. , Poblet, M. , Sánchez, A. , Ristol, A. M. , Serrano, P. , … Soler‐Palacin, P. (2021). Schools as a Framework for COVID‐19 epidemiological surveillance of children in Catalonia, Spain: A population‐based study. Frontiers in Pediatrics, 9, 754744. 10.3389/fped.2021.754744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pifarré I Arolas, H. , Vidal‐Alaball, J. , Gil, J. , López, F. , Nicodemo, C. , & Saez, M. (2021). Missing diagnoses during the covid‐19 pandemic: A year in review. International Journal of Environmental Research and Public Health, 18(10), 5335. 10.3390/ijerph18105335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plana‐Ripoll, O. , Pedersen, C. B. , Holtz, Y. , Benros, M. E. , Dalsgaard, S. , de Jonge, P. , Fan, C. C. , Degenhardt, L. , Ganna, A. , Greve, A. N. , Gunn, J. , Iburg, K. M. , Kessing, L. V. , Lee, B. K. , Lim, C. C. W. , Mors, O. , Nordentoft, M. , Prior, A. , Roest, A. M. , … McGrath, J. J. (2019). Exploring Comorbidity Within Mental Disorders among a Danish National Population. JAMA Psychiatry, 76(3), 259–270. 10.1001/jamapsychiatry.2018.3658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine, N. , McArthur, B. A. , Cooke, J. E. , Eirich, R. , Zhu, J. , & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID‐19: A meta‐analysis. JAMA Pediatrics, 175(11), 1142–1150. 10.1001/jamapediatrics.2021.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raventós, B. , Pistillo, A. , Reyes, C. , Fernández‐Bertolín, S. , Aragón, M. , Berenguera, A. , Jacques‐Aviñó, C. , Medina‐Perucha, L. , Burn, E. , & Duarte‐Salles, T. (2022). Impact of the COVID‐19 pandemic on diagnoses of common mental health disorders in adults in Catalonia, Spain: a population‐based cohort study. BMJ Open, 12(4), e057866. 10.1136/bmjopen-2021-057866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Real Decreto 463/2020 . (2020). de 14 marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID‐19. [Royal Decree 463/2020, of March 14, declaring a state of emergency to manage the public health crisis triggered by COVID‐19]. Boletín Oficial del Estado, 67, de 14 de marzo de 2020. Accessed September 15, 2022. https://boe.es/buscar/act.php?id=BOE-A-2020-3692.
- Real Decreto 555/2020 . (2020). de 5 de junio, por el que se prorroga el estado de alarma declarado por el Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID‐19. [Royal Decree 555/2020, of June 5, extending the state of emergency declared under Royal Decree 463/2020, of March 14, declaring a state of emergency to manage the public health crisis triggered by COVID‐19]. Boletín Oficial del Estado, 159, de 6 de junio de 2020. Accessed September 15, 2022. https://www.boe.es/diario_boe/txt.php?id=BOE-A-2020-5767.
- Real Decreto 926/2020 . (2020). de 25 de octubre, por el que se declara el estado de alarma para contener la propagación de infecciones causadas por el SARS‐CoV‐2. [Royal Decree 926/2020, of October 25, declaring a state of emergency to contain the spread of infections caused by SARS‐CoV‐2]. Boletín Oficial del Estado, 282, de 25 de octubre de 2020. Accessed September 15, 2022. https://www.boe.es/buscar/doc.php?id=BOE-A-2020-12898.
- Recalde, M. , Rodríguez, C. , Burn, E. , Far, M. , García, D. , Carrere‐Molina, J. , Benítez, M. , Moleras, A. , Pistillo, A. , Bolíbar, B. , Aragón, M. , & Duarte‐Salles, T. (2022). Data resource profile: The Information System for Research in Primary Care (SIDIAP). International Journal of Epidemiology, dyac068. 10.1093/ije/dyac068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , Linardon, J. , Courtet, P. , & Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. The International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spettigue, W. , Obeid, N. , Erbach, M. , Feder, S. , Finner, N. , Harrison, M. E. , Isserlin, L. , Robinson, A. , & Norris, M. L. (2021). The impact of COVID‐19 on adolescents with eating disorders: a cohort study. Journal of Eating Disorders, 9(1), 65. 10.1186/s40337-021-00419-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet, M. , Geddes, J. R. , Luciano, S. , & Harrison, P. J. (2021). Incidence and outcomes of eating disorders during the COVID‐19 pandemic. The British Journal of Psychiatry, 220(5), 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viguria, U. A. , & Casamitjana, N. (2021). Early interventions and impact of covid‐19 in Spain. International Journal of Environmental Research and Public Health, 18(8), 4026. 10.3390/ijerph18084026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Soest, T. , Kozák, M. , Rodríguez‐Cano, R. , Fluit, D. H. , Cortés‐García, L. , Ulset, V. S. , Haghish, E. F. , & Bakken, A. (2022). Adolescents' psychosocial well‐being one year after the outbreak of the COVID‐19 pandemic in Norway. Nature Human Behaviour, 6(2), 217–228. 10.1038/s41562-021-01255-w [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2022) Adolescent and young adult health. Updated August 10, 2022. Accessed September 12, 2022. https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions/. [Google Scholar]
- Zipfel, S. , Schmidt, U. , & Giel, K. E. (2022). The hidden burden of eating disorders during the COVID‐19. The Lancet Psychiatry, 9(1), 9–11. 10.1016/S2215-0366(21)00435-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting information
Figure S1. Flow chart
Figure S2. Trends during the pre‐pandemic period
Table S1. Annual incidence rates of eating disorders
Table S2. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the pre‐lockdown period
Table S3. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the lockdown period
Table S4. Incidence rates overall and stratified by sex, age group and the MEDEA deprivation index during the post‐lockdown period
Figure S3: Monthly incidence rates stratified by the MEDEA deprivation index
Table S5. Incidence rate ratios (IRRs) of first recorded cases of eating disorders
Table S6. Sensitivity analysis for incidence rate ratios (IRRs) of first recorded cases of eating disorders.
Data Availability Statement
In accordance with current European and national law, the data used in this study is only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online (https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure) or by contacting SIDIAP (sidiap@idiapjgol.org).


