Abstract
Background
Although remote dietary counselling practices have increased in the COVID‐19 pandemic, it is not known which method is more effective. This study aimed to determine the effect of diet counselling by phone or video on weight loss and to compare it with the traditional follow‐up method.
Methods
Forty‐six participants living with obesity were randomised into the phone counselling (n = 15), video counselling (n = 15), and traditional follow‐up groups (n = 16), and were followed for 10 weeks. The anthropometric measurements, quality‐of‐life questionnaire (SF‐36) scores and total calorie/macronutrient intakes were recorded and compared at baseline and at the end of the study.
Results
In the phone counselling, video counselling and traditional follow‐up groups body weight (−4.8 ± 0.9, −5.7 ± 1.8 and −3.3 ± 0.8 kg, respectively) and SF‐36 general health scores (14.2 ± 4.2, 15.9 ± 3.6 and 10.2 ± 3.7, respectively) of the participants changed significantly compared to baseline (group × time interaction, p < 0.05). The change in the body weight and SF‐36 general health score was more in the phone counselling and video counselling groups relative to the traditional follow‐up group (group × time interaction, p < 0.01). The highest decrease in total calorie (−301.4 ± 112.2 kcal) and carbohydrate (−26.6 ± 11.2 g) intake was in the video counselling group compared to the other groups (group × time interaction, p < 0.01).
Conclusion
Video counselling and phone counselling were effective in weight loss in the COVID‐19 pandemic. It is important to maintain remote dietary counselling practices to support weight management when face‐to‐face meetings are not possible.
Keywords: COVID‐19, dietary intervention, phone counselling, remote counselling, video counselling, weight loss
The effect of phone and video counselling given to participants living with obesity in the COVID‐19 pandemic
Key points
Video counselling and phone counselling were effective in supporting weight management in the COVID‐19 pandemic.
The quality‐of‐life sub‐scores increased more in the video and phone counselling groups compared to the traditional follow‐up group.
It is important to maintain remote dietary counselling practices for weight management when face‐to‐face meetings are not possible.
INTRODUCTION
Obesity, which is defined as excessive accumulation of adipose tissue in the body, affects all organs and systems. 1 According to the World Health Organization (WHO) data, over 650 million adults are living with obesity, and the prevalence of obesity is increasing dramatically. 2 In addition to obesity, studies to prevent obesity are also increasing and new cost‐effective, accessible, and sustainable options are being implemented. These new options are important to reach socio‐economically disadvantaged groups and those who need support. 3
The use of phone/video consultancy applications for body weight control and diet monitoring is increasing. 4 One of the main reasons for this is that individuals care more about the social distance rule as a result of the increase in health concerns because of COVID‐19 (Severe Acute Respiratory Syndrome [SARS‐CoV‐2]) pandemic. 5 In addition, due to the uncertainty of how long the pandemic will last, many people are adapting to online applications and programmes quickly. The main purpose of using such applications and programmes in diet monitoring is to improve the nutritional status of individuals and increase their quality of life. 6 Some studies showed that counselling support practices have a significant effect on weight loss and prevention of unhealthy nutrition practices. 7 , 8 , 9 However, results were inconsistent and varied depending on the type of consultation or the web‐based application used. Therefore, it is unclear which method of phone‐/video‐based diet counselling is more successful or preferable to traditional diet follow‐up. Based on the aforementioned information, this study aimed to determine the effect of diet counselling via phone or video on weight loss and to compare it with the traditional follow‐up method in the COVID‐19 pandemic.
METHODS
Study design and subjects
This study was conducted at the Internal Medicine Clinic and Nutrition and Diet Clinic of Sabuncuoğlu Serefeddin Education and Research Hospital of Amasya University. Individuals referred to the Nutrition and Diet Clinic from the Internal Medicine Clinic for obesity treatment were included in the study.
Inclusion criteria
Being between the ages of 20 and 65 years
Having a body mass index (BMI) ≥ 30 kg/m2
Having a smartphone with internet access and being competent to use it
Volunteering to participate in study
Exclusion criteria
Being pregnant/lactating
Having a hearing problem
Being on a followed diet programme
Being infected with COVID‐19 in the past 6 months (due to its effects on appetite)
Individuals who met the study criteria (n = 68) were randomised according to their file numbers (via: randomizer.org) and divided into three groups: phone counselling (n = 23), video counselling (n = 22) and traditional follow‐up group (n = 23) (Figure 1). The diet programme was continued for 10 weeks, and food consumption records, anthropometric measurements and quality‐of‐life scale scores of all individuals were recorded at the beginning and at the end of the study face to face (Figure 2). To prevent interaction between the groups, all diet programmes were prepared individually at different times, and the study was completed with 46 individuals. The study was approved by the Amasya University Ethics Committee (approval no.: 15‐1003‐18) and registered under clinicaltrials.gov (identifier no.: NCT05276544), and all participants provided written consent.
FIGURE 1.
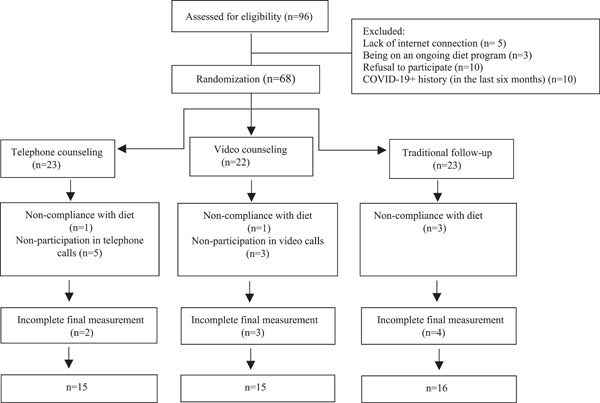
Flowchart of the study
FIGURE 2.
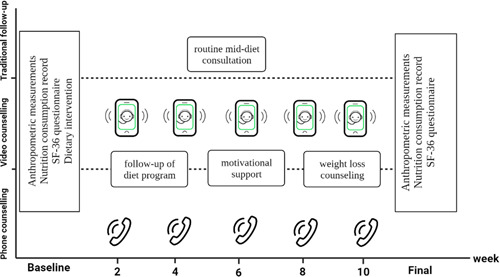
Study design (created with BioRender.com). Individuals in the video counselling group were interviewed every 2 weeks via the Zoom programme, and individuals in the phone counselling group were interviewed every 2 weeks by phone to ensure the continuity of the diet programme and to motivate individuals. No intervention was made to the traditional diet follow‐up group, except for the routine diet programme, with mid‐consultation at the fifth or sixth week. All measurements and records were noted at the beginning and the end of the study
Anthropometric measurements
Body weight, total body fat (%) and muscle mass were measured using a Tanita BC 545 device (Tartı Medical, https://www.tarti.com/) while fasting and without shoes. Waist circumference and hip circumference measurements were taken using a non‐stretchable tape measure. BMI was calculated by dividing body weight by the square of height (kg/m2). 10 All measurements were repeated at the end of the study.
Dietary intervention
The diet programme was prepared specifically for all individuals participating in the study, and all interviews were conducted at different times and one on one to prevent mutual interaction between the groups. The basal metabolic rate (BMR) of individuals was calculated using the Mifflin equation according to their adjusted body weight, age and gender. 11 The total calorie requirement was calculated by multiplying the BMR value with the average physical activity level. The diet programme consisted of about 10%–20% protein, 45%–60% carbohydrates and 20%–35% fat, and was continued for 10 weeks to achieve the goal of clinically significant weight loss (approximately 5%–10%). 12 , 13
Individuals in the video counselling group were interviewed every 2 weeks via Zoom programme (Zoom Video Conferencing Software Inc., San Francisco, CA, USA), whereas those in the phone counselling group were interviewed every 2 weeks by phone. It was aimed to ensure the continuity of the diet programme and to motivate individuals in these interviews, which lasted about 20 min and were conducted by a registered dietitian. No intervention was made to the traditional diet follow‐up group, except for the routine diet programme with mid‐consultation at the fifth or sixth week. The last food consumption records of all individuals for 24 h were noted and analysed at the beginning and the end of the study (via BeBIS software 2022).
Quality‐of‐life scale (SF‐36)
The scale consists of 36 items with 8 subscales, and the total score ranges from 0 to 100 points. Higher scores reflect a better quality of life for each subscale. In the study, the Turkish‐validated form of the scale was used. 14
Statistical analysis
For sample size calculation, the change in body weight of the participants in the study of Johnson et al. were taken as a reference (videoconferencing [8.23 ± 4.5 kg]; control [2.9 ± 3.9 kg]), and a G Power 3.0.10 programme was used for calculations. 15 The study was completed with a 90.0% power (one tail). Data analyses were carried out using the SPSS software package (Statistical Package for Social Science, version 22.0, IBM, Armonk, NY, USA) software package. The normality of data distribution was examined using Shapiro–Wilk test. Descriptive statistics were presented as mean ± standard deviation, whereas nominal variables were presented as the number of cases and percentages (%). Within‐group differences in the dependent groups were analysed using a paired t‐test. A repeated measures analysis of variance (ANOVA) model was used to test the between‐group differences from baseline to 10 weeks (time × treatment interaction), and post hoc results were shown with letters. The confidence interval of 95.0% and p < 0.05 were considered significant in all statistical tests.
RESULTS
During the eligibility process, 28 of the 96 participants were excluded from the study. A total of 68 participants were randomised, and the study was completed with 46 participants at the end of 10 weeks (Figure 1). BMI values were 32.9 ± 2.8 kg/m2 in the phone counselling group (n = 15), 32.3 ± 2.5 kg/m2 in the video counselling group (n = 15) and 33.2 ± 2.9 kg/m2 in the traditional follow‐up group (n = 16) (p > 0.05). Individuals in all groups were mostly (>50.0%) women, graduated from secondary school and were non‐smokers (p > 0.05). Diabetes mellitus was the most common disease in all groups. Less than one‐third of individuals in all groups had a COVID‐19+ history (more than 6 months) (p > 0.05) (Table 1).
TABLE 1.
Demographic characteristics
| Phone counselling (n = 15) | Video counselling (n = 15) | Traditional follow‐up (n = 16) | p | |
|---|---|---|---|---|
| Age (years) | 39.9 ± 10.0 | 45.5 ± 7.0 | 42.6 ± 10.1 | 0.210 |
| BMI (kg/m2) | 32.9 ± 2.8 | 32.3 ± 2.5 | 33.2 ± 2.9 | 0.762 |
| Gender (%) | 0.105 | |||
| Male | 40.0 | 33.3 | 37.5 | |
| Female | 60.0 | 66.7 | 62.5 | |
| Education level (%) | ||||
| Primary school | 20.0 | 26.7 | 25.0 | 0.503 |
| Secondary school | 53.3 | 53.3 | 50.0 | |
| University and above | 26.7 | 20.0 | 25.0 | |
| Comorbid diseases (%) | ||||
| Hypertension | 13.3 | 6.7 | ‐ | 0.415 |
| Diabetes mellitus | 13.3 | 20.0 | 18.8 | |
| Hypercholesterolaemia | – | 6,7 | 6.25 | |
| Active smoking (%) | 16.6 | 16.6 | 12.5 | 0.209 |
| COVID‐19+ history (%)a | 26.6 | 20.0 | 31.2 | 0.338 |
Abbreviation: BMI, body mass index.
More than 6 months.
Body weight decreased in the phone counselling (−4.8 ± 0.9 kg, p < 0.01), video counselling (−5.7 ± 1.8 kg, p < 0.001) and traditional follow‐up groups (−3.3 ± 0.8 kg, p < 0.05) compared to baseline. In addition, BMI (kg/m2), waist to hip ratio, waist circumference (WC, cm) and total body fat (%) decreased compared to baseline in all groups (p < 0.05). Body weight and BMI decreased more in the phone counselling and video counselling groups relative to the traditional follow‐up group (group × time interaction, p < 0.01). WC and total body fat decreased more in the video counselling group relative to the phone counselling and traditional follow‐up groups (group × time interaction, p < 0.05) (Table 2).
TABLE 2.
Changes in anthropometric measurements
| Phone counselling (n = 15) | Video counselling (n = 15) | Traditional follow‐up (n = 16) | p (group × time) | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Change (Δ) | Baseline | Change (Δ) | Baseline | Change (Δ) | ||
| Body weight (kg) | 91.4 ± 11.8 | −4.8 ± 0.9** | 86.4 ± 7.8 | −5.7 ± 1.8*** | 87.4 ± 9.6 | −3.3 ± 0.8* | 0.001a , b |
| BMI (kg/m2) | 32.9 ± 2.8 | −1.8 ± 0.5** | 32.3 ± 2.5 | −2.2 ± 0.7*** | 33.2 ± 2.9 | −1.2 ± 0.6* | 0.001a , b |
| WHR | 0.92 ± 0.09 | −0.06 ± 0.03* | 0.90 ± 0.08 | −0.07 ± 0.03* | 0.95 ± 0.07 | −0.07 ± 0.02* | 0.092 |
| WC (cm) | 106.6 ± 13.4 | −4.2 ± 4.8* | 103.3 ± 11.7 | −6.5 ± 5.5** | 108.1 ± 10.3 | −3.3 ± 3.8* | 0.014a , c |
| Total body fat (%) | 39.2 ± 8.2 | −1.4 ± 1.5* | 37.3 ± 8.1 | −1.9 ± 2.2** | 34.7 ± 5.9 | −1.0 ± 1.2* | 0.016a , c |
| Muscle mass (kg) | 49.8 ± 7.3 | −1.1 ± 1.2 | 49.1 ± 6.0 | −1.0 ± 1.7 | 51.3 ± 9.1 | −0.9 ± 1.3 | 0.459 |
Notes: Data were presented as mean ± standard deviation. Within‐group significance is shown using symbols (*). Between group post hoc results are shown using letters.
Abbreviations: BMI, body mass index; WC, waist circumference; WHR, waist to hip ratio.
Video counselling × traditional follow‐up group.
Phone counselling × traditional follow‐up group.
Video counselling × phone counselling group.
p < 0.05
p < 0.01
***p < 0.001.
General health score increased in the phone counselling (14.2 ± 4.2), video counselling (15.9 ± 3.6) and traditional follow‐up (10.2 ± 3.7) groups compared to baseline (p < 0.05). Physical functioning, mental health, pain and physical role scores also increased in all groups compared to baseline (p < 0.05). General health, physical functioning, physical role and mental health scores increased more in the phone counselling and video counselling groups relative to the traditional follow‐up group (group × time interaction, p < 0.05) (Table 3).
TABLE 3.
Changes in SF‐36 quality‐of‐life scale subscale scores
| Phone counselling (n = 15) | Video counselling (n = 15) | Traditional follow‐up (n = 16) | p (group × time) | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Change (Δ) | Baseline | Change (Δ) | Baseline | Change (Δ) | ||
| General health | 61.6 ± 13.4 | 14.2 ± 4.2** | 53.3 ± 14.2 | 15.9 ± 3.6** | 50.7 ± 11.3 | 10.2 ± 3.7** | 0.015a , b |
| Emotional role | 71.1 ± 21.3 | 5.2 ± 5.9 | 62.2 ± 17.2 | 4.8 ± 11.5 | 64.1 ± 18.7 | 4.4 ± 6.1 | 0.129 |
| Physical functioning | 62.3 ± 14.4 | 13.6 ± 14.8** | 61.3 ± 11.5 | 14.0 ± 15.5** | 64.6 ± 12.4 | 8.2 ± 8.9* | 0.021a , b |
| Vitality | 42.6 ± 18.3 | 3.6 ± 5.11.9 | 44.0 ± 13.5 | 4.6 ± 5.9 | 51.1 ± 12.7 | 2.9 ± 6.6 | 0.240 |
| Mental health | 58.9 ± 8.0 | 9.3 ± 3.5** | 59.7 ± 7.4 | 8.2 ± 2.7** | 66.6 ± 10.3 | 6.2 ± 4.7* | 0.010a , b |
| Social functioning | 75.0 ± 12.5 | 4.2 ± 7.4 | 77.5 ± 15.0 | 4.9 ± 7.6 | 77.8 ± 13.6 | 2.6 ± 5.0 | 0.073 |
| Pain | 83.1 ± 10.8 | 8.8 ± 9.5** | 89 ± 8.11.2 | 11.1 ± 8.2** | 80.1 ± 17.0 | 8.6 ± 10.0** | 0.457 |
| Physical role | 65.0 ± 12.6 | 8.5 ± 5.1* | 68.3 ± 11.4 | 10.0 ± 6.1** | 69.2 ± 10.9 | 6.3 ± 5.4* | 0.032a , b |
Notes: Data were presented as mean ± standard deviation. Within‐group significance is shown using symbols (*). Between‐group post hoc results are shown using letters.
Video counselling × traditional follow‐up group.
Phone counselling × traditional follow‐up group.
p < 0.05
p < 0.01.
Total calorie intake decreased compared to baseline in the phone counselling (−227.6 ± 96.3 kcal), video counselling (−301.4 ± 112.2 kcal) and traditional follow‐up (185.1 ± 108.2 kcal) groups (p < 0.01). Carbohydrate (g), fat (g), saturated fatty acids (g) and poly‐unsaturated fatty acid (g) intake also decreased in all groups (p < 0.05). Compared to other groups, the highest decrease in total calorie and carbohydrate (g) intake was in the video counselling group, and the least decrease was in the traditional follow‐up group (group × time interaction, p < 0.01). Fat intake decreased more in the phone counselling and video counselling groups relative to the traditional follow‐up group (group × time interaction, p < 0.05) (Table 4).
TABLE 4.
Changes in total energy and macronutrient intakes
| Phone counselling (n = 15) | Video counselling (n = 15) | Traditional follow‐up (n = 16) | p (group × time) | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Change (Δ) | Baseline | Change (Δ) | Baseline | Change (Δ) | ||
| Total calories (kcal) | 1850.1 ± 98.5 | −227.6 ± 96.3** | 1790.3 ± 120.6 | −301.4 ± 112.2** | 1907.7 ± 105.8 | −185.1 ± 108.2** | 0.001a , b , c |
| Carbohydrates (g) | 179.9 ± 54.7 | −20.1 ± 14.9** | 165.21 ± 53.8 | −26.6 ± 11.2** | 201.3 ± 62.8 | −17.3 ± 12.0** | 0.005a , b , c |
| Protein (g) | 54.3 ± 15.6 | −4.5 ± 7.5 | 61.1 ± 17.3 | −5.3 ± 9.2 | 60.8 ± 11.8 | −4.0 ± 11.4 | 0.226 |
| Fat (g) | 83.3 ± 21.7 | −12.2 ± 11.3** | 81.9 ± 18.4 | −13.5 ± 16.7** | 90.2 ± 19.9 | −9.7 ± 10.1* | 0.013a , b |
| SFA (g) | 25.5 ± 9.1 | −3.2 ± 5.5* | 19.8 ± 10.2 | –3.9 ± 4.4* | 26.6 ± 9.4 | –3.0 ± 5.2* | 0.546 |
| MUFA (g) | 22.8 ± 13.1 | –2.5 ± 5.1 | 18.2 ± 13.3 | −3.2 ± 4.9 | 23.2 ± 15.4 | −2.1 ± 5.5 | 0.207 |
| PUFA (g) | 36.1 ± 16.7 | −5.8 ± 4.0* | 34.8 ± 15.9 | −5.6 ± 4.1* | 38.2 ± 19.6 | −4.1 ± 3.3* | 0.328 |
Notes: Data were presented as mean ± standard deviation. Within‐group significance is shown using symbols (*). Between‐group post hoc results are shown using letters.
Abbreviations: MUFA, mono‐unsaturated fatty acids; PUFA, poly‐unsaturated fatty acids; SFA, saturated fatty acids.
Video counselling × traditional follow‐up group.
Phone counselling × traditional follow‐up group.
Video counselling × phone counselling group.
p < 0.05
p < 0.01.
DISCUSSION
The devastating consequences of the COVID‐19 pandemic have dramatically changed our lives. In particular, the restrictions and distance rules in the pandemic have forced individuals to spend more time at home by keeping them away from socialising. 16 Many individuals who avoided crowded environments because of fear of contracting the COVID‐19 infection had to delay their health checks, including dietitian meetings. 17 , 18 In this process, remote health services provided online or through phone have made our lives much easier. 19 According to the results of our study, body weight and BMI changes in the phone counselling and video counselling groups were found to be higher than those in the traditional follow‐up group (group × time interaction, p < 0.01). This was an expected result because there were control meetings every 2 weeks in the phone and video counselling groups. The most significant change from baseline was observed in the video counselling group (p < 0.001) (Table 2). This may be because the visual interaction in video calls increased diet compliance and continuity. In the study of Johnson et al., the effectiveness of videoconferencing and in‐person dietary counselling in participants living with obesity was compared. At the end of 12 weeks, it was found that the videoconferencing group had higher participation in the interviews due to the ease of access and lost more weight than the in‐person group. 19 In another study, comparing virtual diet intervention and in‐person diet intervention during the pandemic process, diet compliance and weight loss of the participants in virtual diet classes were found to be higher than those in the in‐person group. 7 However, there are also studies showing similar effects of dietary intervention in weight loss through in‐person or phone/video interviews. 8 , 20
In addition to BMI, waist circumference and body fat degree are used as indicators of adiposity. 21 Studies conducted during the COVID‐19 pandemic have shown that these indicators also increase. 22 , 23 In this study, after 10 weeks of dietary intervention, WC and total body fat decreased in the phone counselling, video counselling and traditional follow‐up groups compared to the baseline, and the most significant change was observed in the video counselling group (group × time interaction, p < 0.05) (Table 2). As mentioned earlier, the probable reason for this may be that the mutual interaction in video calls increases the dietary compliance of individuals. In the study of Hall et al., 9 the total body fat percentage of individuals who applied a low‐calorie diet via videoconferencing decreased at the end of 6 months. In the study of Liñan et al., 20 the WC of participants living with obesity who received nutritional support via phone during the COVID‐19 pandemic decreased at the end of 3 months. In another study evaluating the effect of online dietary support for children living with obesity, muscle mass increased in the videoconferencing group at the end of 3 months, whereas fat mass increased in the control group (p < 0.05). 24
Health‐related problems and social isolation obligations during the pandemic have led to a significant decrease in the quality of life. 25 In particular, the fear of COVID‐19 infection has increased the stress and anxiety levels of individuals. 26 In our study, general health, physical functioning, mental health and physical role scores of all groups increased after diet intervention compared to baseline, and the change in video and phone counselling groups was found to be higher than that in the traditional follow‐up group (group × time interaction, p < 0.05) (Table 3). Because the physical and mental health problems caused by obesity significantly reduce the quality of life, it was an expected result that the quality‐of‐life scores increase after weight loss. In addition, checking the individuals in the video and phone counselling groups every 2 weeks may have contributed to the increase in the quality‐of‐life scores, as it provides mental support during the pandemic. In the study of Ghazanfarpour et al. 27 it was observed that tele‐support given to hospital staff during the COVID‐19 pandemic decreased depression and anxiety scores. In the study of Dalbosco‐Salas et al. after the tele‐rehabilitation programme provided to COVID‐19 survivors, the quality‐of‐life score of individuals increased from 39.6 ± 17.6 to 58.9 ± 20.5. 28 In other studies, evaluating the effects of remote dietary intervention in participants living with obesity, it was also found that quality‐of‐life scores of individuals increased after weight loss. 29 , 30
The basic principle in dietary intervention is to balance the total calorie intake because the main cause of weight gain is the intake of more calories than what is spent. 31 For the sustainability of the diet, it is important to note that the total calories taken should not be below the basal metabolism level. 11 Considering the increasing prevalence of obesity in the COVID‐19 pandemic and the effects of proper nutrition on the immune system, a personalised nutrition plan is very important in weight loss. 32 In this study, the diet of individuals in all groups was prepared and followed by a registered dietitian. At the end of the study, the most significant change in total calorie and carbohydrate intake was in the video counselling group. The change in total fat intake in the phone and video counselling groups was higher than that in the traditional follow‐up group (group × time interaction, p < 0.05) (Table 3). These results show the importance of regular diet follow‐up and remote interaction in diet success. In other studies, in parallel with our study, the total calorie and fat intake of individuals decreased after remote diet counselling. 33
This study has some limitations. Due to pandemic restrictions, individuals could not be included in a regular physical activity programme. Because blood findings are not routinely requested during the diet follow‐up process, the results of the study were not supported by blood findings. The number of women participating in the study was more than that of men. However, this was an expected result because the prevalence of obesity is higher in women than in men. 34 No blinding was performed, due to the nature of the study, which may have caused some bias.
Despite these limitations, the randomised controlled and prospective design has increased the power of the study. Comparison of detailed anthropometric measurements and total calorie/macronutrients (within group and between groups) took this study one step ahead of other studies in the literature. Conducting video and phone counselling in separate groups and comparing them with the control group also helped to determine which method was more effective.
CONCLUSIONS
It was found that video counselling and phone counselling were effective in weight loss during the COVID‐19 pandemic. In particular, the most significant change in total calorie and carbohydrate change was observed in the video counselling group. The quality‐of‐life sub‐scores also increased more in the video and phone counselling groups compared to the traditional follow‐up group. Considering all these results and the ongoing pandemic situation, remote dietary counselling is quite necessary. The development of new and more useful dietary counselling applications or web‐based programmes is important for supporting effective weight management when face‐to‐face meeting is not possible.
AUTHOR CONTRIBUTIONS
Ümüş Özbey Yücel: conceptualisation, literature search, data collection and writing. Murat Yücel: data analysis, writing, critical appraisal and supervision.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The study was approved by the Amasya University Ethics Committee (approval no.: 15‐1003‐18) and registered under clinicaltrials.gov (identifier no.: NCT05276544), and all participants provided written consent.
TRANSPARENCY DECLARATION
The lead author affirms that this manuscript is an honest, accurate and transparent account of the study being reported. The reporting of this work is compliant with CONSORT guidelines. The lead author affirms that no important aspects of the study have been omitted and that no discrepancies from the study as planned.
ACKNOWLEDGEMENTS
The authors thank Furkan Kaçar for clinical support. This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
Biographies
Ümüş Özbey Yücel is a lecturer in the Department of Nutrition and Dietetics. Her research focuses on ways to improve nutrition and lifestyle to prevent and treat chronic diseases.
Murat Yücel is a lecturer and a PhD student in the Department of Biostatistics and Medical Informatics. His research focuses on the development of nutrition scales.
Yücel ÜÖ, Yücel M. The effect of phone and video counselling given to participants living with obesity on weight loss and quality of life during the COVID‐19 pandemic: a randomised controlled trial. J Hum Nutr Diet. 2023;1–8. 10.1111/jhn.13126
DATA AVAILABILITY STATEMENT
Data cannot be shared because it contains private information. This study was conducted at the Nutrition and Diet Clinic of Sabuncuoğlu Serefeddin Education and Research Hospital of Amasya University. Individuals referred to the Nutrition and Diet Clinic from the Internal Medicine Clinic for obesity treatment were included in the study.
REFERENCES
- 1. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. [DOI] [PubMed] [Google Scholar]
- 2. Ahirwar R, Mondal PR. Prevalence of obesity in India: a systematic review. Diabetes Metab Syndr. 2019;13:318–21. [DOI] [PubMed] [Google Scholar]
- 3. Kumanyika SK. A framework for increasing equity impact in obesity prevention. Am J Public Health. 2019;109:1350–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alencar MK, Johnson K, Mullur R, Gray V, Gutierrez E, Korosteleva O. The efficacy of a telemedicine‐based weight loss program with video conference health coaching support. J Telemed Telecare. 2019;25:151–7. [DOI] [PubMed] [Google Scholar]
- 5. Kämpfen F, Kohler IV, Ciancio A, Bruine de Bruin W, Maurer J, Kohler HP. Predictors of mental health during the Covid‐19 pandemic in the US: role of economic concerns, health worries and social distancing. PLoS One. 2020;15:e0241895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shah S, Diwan S, Kohan L, Rosenblum D, Gharibo C, Soin A, et al. The technological impact of COVID‐19 on the future of education and health care delivery. Pain Physician. 2020; 23:S367–80. [PubMed] [Google Scholar]
- 7. Zaman A, Sloggett KJ, Caldwell AE, Catenacci V.A., Cornier MA, Grau L, et al. The effects of the COVID‐19 pandemic on weight loss in participants in a behavioral weight loss intervention. Obesity. 2022;30:1015–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ross KM, Carpenter CA, Arroyo KM, Shankar MN, Yi F, Qiu P, et al. Impact of transition from face‐to‐face to telehealth on behavioral obesity treatment during the COVID‐19 pandemic. Obesity. 2022;30:858–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall M, Spiers L, Knox G, Hinman RS, Sumithran P, Bennell KL. Feasibility of exercise and weight management for people with hip osteoarthritis and overweight or obesity: a pilot study. Osteoarthr Cartil Open. 2021;3:100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Garrouste‐Orgeas M, Troché G, Azoulay E, Caubel A, de Lassence A, Cheval C, et al. Body mass index. Intensive Care Med. 2004;30:437–43. [DOI] [PubMed] [Google Scholar]
- 11. Henry C. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr. 2005;8:1133–52. [DOI] [PubMed] [Google Scholar]
- 12. Ahsan H. Dietary carbohydrates‐requirement and recommendation in the human diet. Curr Nutr Food Sci. 2021;17:904–10. [Google Scholar]
- 13. Valsdottir TD, Øvrebø B, Falck TM, Litleskare S, Johansen EI, Henriksen C, et al. Low‐carbohydrate high‐fat diet and exercise: effect of a 10‐week intervention on body composition and cvd risk factors in overweight and obese women—a randomized controlled trial. Nutrients. 2020;13(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kocyigit H. Reliability and validity of the Turkish version of short form‐36 (SF‐36): a study in a group of patients will rheumatic diseases. Turk J Drugs Ther. 1999;12:102–106. [Google Scholar]
- 15. Johnson KE, Alencar MK, Coakley KE, Swift DL, Cole NH, Mermier CM, et al. Telemedicine‐based health coaching is effective for inducing weight loss and improving metabolic markers. Telemed J E‐Health. 2019;25:85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pandi‐Perumal SR, Vaccarino SR, Chattu VK, Zaki N.F.W., BaHammam AS, Manzar D, et al. Distant socializing, not ‘social distancing’ as a public health strategy for COVID‐19. Pathog Glob Health. 2021;115:357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brunton C, Arensberg MB, Drawert S, Badaracco C, Everett W, McCauley SM. Perspectives of registered dietitian nutritionists on adoption of telehealth for nutrition care during the COVID‐19 pandemic. Healthcare. 2021;9(2):235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hajek A, De Bock F, Kretzler B, König H‐H. Factors associated with postponed health checkups during the COVID‐19 pandemic in Germany. Public Health. 2021;194:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fitts MS, Russell D, Mathew S, Liddle Z, Mulholland E, Comerford C, et al. Remote health service vulnerabilities and responses to the COVID‐19 pandemic. Aust J Rural Health. 2020;28:613–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liñan CC, Mayorga JHA, Lozada‐Urbano M. The effects of telenutrition in overweight and obese adults in a nutritional center in Lima, Peru. F1000Res. 2021;10:545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ho‐Pham LT, Campbell LV, Nguyen TV. More on body fat cutoff points. Mayo Clin Proc. 2011;86:584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chwałczyńska A, Andrzejewski W. Changes in body mass and composition of the body as well as physical activity and time spent in front of the monitor by students of the Wroclaw University of Health and Sport Sciences during the period of COVID‐19 restrictions. Int J Environ Res Public Health. 2021;18:7801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Biamonte E, Pegoraro F, Carrone F, Facchi I, Favacchio G, Lania AG, et al. Weight change and glycemic control in type 2 diabetes patients during COVID‐19 pandemic: the lockdown effect. Endocrine. 2021;72:604–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pecoraro P, Gallè F, Muscariello E, Di Mauro V, Daniele O, Forte S, et al. A telehealth intervention for ensuring continuity of care of pediatric obesity during the CoVid‐19 lockdown in Italy. Nutr Metab Cardiovas Dis. 2021;31:3502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ferreira LN, Pereira LN, da Fé Brás M, Ilchuk K. Quality of life under the COVID‐19 quarantine. Qual Life Res. 2021;30:1389–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sher L. COVID‐19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ghazanfarpour M, Ashrafinia F, Zolala S, Ahmadi A, Jahani Y, Hosseininasab A. Investigating the effectiveness of tele‐counseling for the mental health of staff in hospitals and COVID‐19 clinics: a clinical control trial. Trends Psychiatry Psychother. 2021;44:e20200176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dalbosco‐Salas M, Torres‐Castro R, Rojas Leyton A, Morales Zapata F, Henríquez Salazar E, Espinoza Bastías G., et al. Effectiveness of a primary care telerehabilitation program for post‐COVID‐19 patients: a feasibility study. J Clin Med. 2021;10:4428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Donaldson EL, Fallows S, Morris M. A text message based weight management intervention for overweight adults. J Hum Nutr Diet. 2014;27:90–7. [DOI] [PubMed] [Google Scholar]
- 30. Haggerty AF, Hagemann A, Barnett M, Thornquist M, Neuhouser ML, Horowitz N, et al. A randomized, controlled, multicenter study of technology‐based weight loss interventions among endometrial cancer survivors. Obesity. 2017;25:S102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hafekost K, Lawrence D, Mitrou F, O'Sullivan TA, Zubrick SR. Tackling overweight and obesity: does the public health message match the science? BMC Med. 2013;11:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Calder PC. Nutrition, immunity and COVID‐19. BMJ Nutr Prev Health. 2020;3:74–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Perri MG, Shankar MN, Daniels MJ, Durning PE, Ross KM, Limacher MC, et al. Effect of telehealth extended care for maintenance of weight loss in rural US communities: a randomized clinical trial. JAMA Netw Open. 2020;3:206764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Erem C. Prevalence of overweight and obesity in Turkey. IJC. 2015;8:38–41. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared because it contains private information. This study was conducted at the Nutrition and Diet Clinic of Sabuncuoğlu Serefeddin Education and Research Hospital of Amasya University. Individuals referred to the Nutrition and Diet Clinic from the Internal Medicine Clinic for obesity treatment were included in the study.


