Abstract
The COVID‐19 pandemic led to significant adaptations to healthcare. Provision of mental healthcare in a changing environment presented healthcare workers with unique challenges and demands, including changes in workload and expectations. To inform current and future healthcare service responses, and adaptations, the current review aimed to collate and examine the impact of the pandemic on mental healthcare workers (MHWs). We conducted a rapid systematic review to examine the overall impact of the COVID‐19 pandemic on MHWs. Searches were conducted in Ovid Medline and PsycInfo and restricted to articles published from 2020. Inclusion criteria specified articles written in English, published in peer‐reviewed journals, and that examined any outcome of the impact of COVID‐19 on MHWs; 55 articles fulfilled these criteria. Outcomes were categorized into ‘work‐related outcomes’ and ‘personal outcomes’. Mental healthcare workers worldwide experienced a range of work‐related and personal adversities during the pandemic. Key work‐related outcomes included increased workload, changed roles, burnout, decreased job satisfaction, telehealth challenges, difficulties with work‐life balance, altered job performance, vicarious trauma and increased workplace violence. Personal outcomes included decreased well‐being, increased psychological distress and psychosocial difficulties. These outcomes differed between inpatient, outpatient and remote settings. The COVID‐19 pandemic significantly altered the delivery of mental healthcare and MHWs experienced both work‐related and personal adversities during the COVID‐19 pandemic. With the continuation of changes introduced to healthcare in the initial stages of the pandemic, it will be important to maintain efforts to monitor negative outcomes and ensure supports for MHWs, going forward.
Keywords: COVID‐19, mental health, mental health personnel, mental health services
The rapid spread of the COVID‐19 pandemic allowed little time to prepare or plan, leaving healthcare systems worldwide facing unprecedented demand. In response, healthcare workers reported working longer shifts, with the additional burden of wearing personal protective equipment (PPE) to minimize the risk of exposure and infection (WHO 2020). Although it is reported across nations that the peak of the pandemic is now over, challenges persist as anecdotal evidence suggests demand on healthcare services remains high (Sammons 2022). Governments in many countries implemented mandates designed to limit the spread of COVID‐19, creating an ever‐changing healthcare environment. For mental healthcare workers (MHWs), delivering services online or by telephone, or providing face‐to‐face services to patients under the COVID‐19 protocols, led to increased difficulty in service provision. Assessing mental state and capturing non‐verbal cues, which are used to monitor and manage clinical symptoms, are particularly challenging when connecting remotely (Isautier et al. 2020). Additionally, technological challenges such as appropriate access to hardware, proficiency in using telehealth platforms and unreliable or unstable network connections created additional challenges for both those delivering services, as well as those receiving them, especially in rural areas (Summers‐Gabr 2020). Each of these service provision changes potentially increased the burden of occupational stress experienced by MHWs across the health system, especially during periods of high demand.
Many public mental health systems – already beyond capacity prior to the COVID‐19 pandemic (Olfson 2016) – were required to respond and adapt to governmental requirements and consumer needs amidst a reportedly significant increase in demand. Specifically, in the first year of the COVID‐19 pandemic, the WHO reported a 25% increase in the global prevalence of depression and anxiety (WHO 2022), with increased acute psychiatric hospitalisations in Europe during lockdown (Fasshauer et al. 2021; Gomez‐Ramiro et al. 2021) and increased demand and wait times for outpatient mental health services in Australia (Australian Psychological Society 2021). Ultimately, the challenges the mental health system faced throughout the COVID‐19 pandemic increased the burden on already overloaded MHWs who were expected to quickly adapt and cope with increases in demand, changes in service delivery and staff shortages, whilst also navigating the pandemic themselves.
The impact of COVID‐19 specifically on the psychosocial well‐being of MHWs is currently not clear. Research has indicated a broad spectrum of individual and collective responses, including increased economic strain, uncertainty and isolation (Rahman et al. 2020). For healthcare workers broadly, the psychological impacts of COVID‐19 include insomnia, anxiety, somatisation, depression, obsessive–compulsive symptoms and psychological distress (Mulatu et al. 2021; Zhang et al. 2020). Furthermore, a rapid review early in the pandemic reported healthcare workers' concern for their own health, a fear of infecting their families, friends and colleagues, as well as psychosocial impacts including social isolation, uncertainty, fear of being ostracized by their family and community due to working in a hospital environment, unwillingness to go to work and considering leaving their job (Barello et al. 2020). Even prior to the COVID‐19 pandemic, MHWs had been identified as particularly vulnerable to occupational burnout, which can lead to job dissatisfaction and high staff turnover (Acker 2012; Piko 2006; Scanlan & Still 2019). Caring for patients experiencing mental illness during the COVID‐19 pandemic, whilst facing ongoing changes to service provision, staff shortages and a reported increase in demand, placed significant additional burden on the mental health workforce. An understanding of the nature and extent of the impact of COVID‐19 specifically on MHWs is integral to informing current and future strategies to support their well‐being, motivation and competency, as well as to enhance retention in the workplace. In this context, this review sought to outline the reported impact of the COVID‐19 pandemic on workers in mental health settings.
METHOD
Search strategy
This rapid systematic review was carried out in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analyses (PRISMA; Page et al. 2021) and was registered with the International Prospective Register of Systematic Reviews (PROSPERO identifier CRD42021297008). A systematic search was conducted to examine the impact of COVID‐19 on the health and well‐being of MHWs across the globe. Search terms included both MeSH headings and free terms contained in the title or abstract related to MHWs, mental healthcare settings and the COVID‐19 pandemic (see Supporting Information for the full search algorithms).
A systematic search using the databases Ovid Medline and PsycINFO was conducted. The initial search was conducted on the 20th of December 2021, and the final search was conducted on the 17th of June 2022. Searches were restricted to 2020 or later, to ensure the inclusion of studies related to COVID‐19, as well as exclusion of similar past pandemics such as severe acute respiratory illness (SARS), the Middle East respiratory Syndrome (MERS) and the swine flu (H1N1). Inclusion criteria specified articles published in peer‐reviewed English language journals that examined any outcome of the impact of COVID‐19 on MHWs. Studies were excluded if they reported heterogeneous samples from which outcomes related to MHWs were not specified or able to be extracted independently, were conference proceedings, abstracts, dissertations/theses, articles uploaded to preprint servers or letters to the editor. Additionally, the reference lists of the included studies were searched for extra articles during the database searching; however, no additional articles that fulfilled inclusion criteria were found.
Study selection and data extraction
Search results were exported to Endnote bibliographic management software, duplicates removed and the remainder uploaded to Covidence systematic review software (Covidence Systematic Review Software 2022). Two authors (K.C. and I.G.) independently screened records on title and abstract and then full text against the inclusion criteria. Any disagreements were resolved through discussion. A data extraction template was developed and piloted by K.C., I.G., and Z.J. One reviewer (K.C.) independently extracted relevant data, including information on study characteristics and outcomes; these extractions were confirmed by a second author (I.G.). Following data extraction, themes were coded inductively into two themes, work outcomes or personal outcomes, by Z.J. and discussed in collaboration with K.C. and I.G. throughout the process of extraction and interpretation. Given the rapid review methodology, no risk of bias or quality assessment was conducted in the current review. Risk of bias and quality assessments are commonly omitted in rapid reviews (e.g. Crawshaw et al. 2022; Dittborn et al. 2022; Hussein 2022; Magill et al. 2020; Tabari et al. 2020) in order to facilitate the speed of process for timely dissemination of findings that have potentially important implications for current settings (Hamel et al. 2021; Khangura et al. 2012).
RESULTS
The literature search yielded 1678 unique citations. The full text of 414 citations were examined and, of these, 55 articles met our inclusion criteria (see Fig. 1).
Fig. 1.
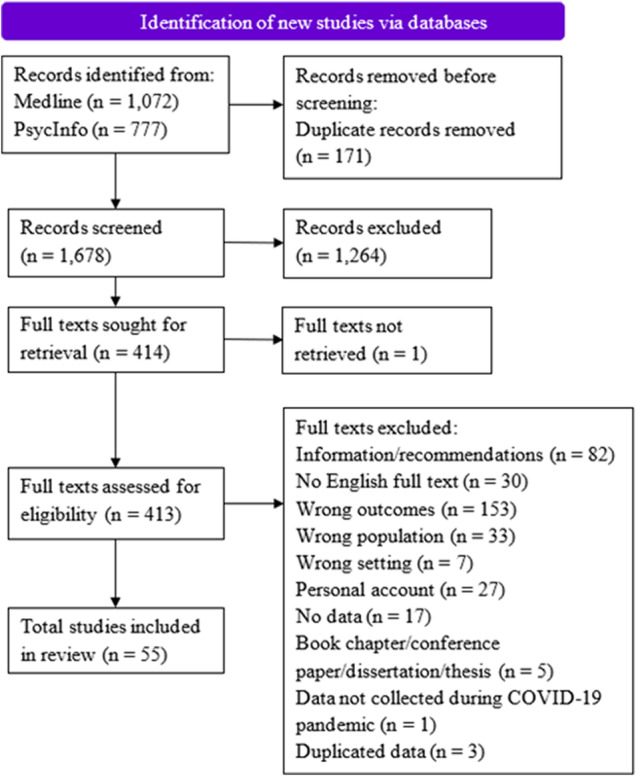
PRISMA flow chart.
The study results were grouped into two themes: ‘work outcomes’ and ‘personal outcomes’. Many of the included studies were of cross‐sectional, qualitative, or mixed‐methods design; some retrospective studies were also included. The characteristics of included studies are displayed in Table 1.
Table 1.
Characteristics of included studies
| Author (Year)/Origin | MH workforce breakdown (N) | Sample size; sex | Age (years) M ± SD or N (%) | MH setting |
|---|---|---|---|---|
| Aafjes‐van Doorn et al. (2020)/United States |
Clinical Psychologist (162) Social Worker (60) Medical Doctor (57) Counselling Psychologist (28) Other (33) |
N = 339; 249F | 55 ± 16.36 | NS |
| Abdelfattah (2020)/Egypt | Psychiatric Resident (20) | N = 25; 8F, 12M | 25–28 | Inpatient |
| Adams et al. (2021)/United States | Peer Support Specialist (1280) | N = 1280; 362M, 851F, 23NS |
18–29: 84 (7.0%) 30–49: 473 (38.0%) 50–64: 555 (45.0%) ≥65: 119 (10.0%) |
Peer‐run organization, non‐peer‐run MH or social service agency, governmental agency or organization |
| Anzola et al. (2022)/Canada |
Nurse (141) Physician (12) Allied Health (60) Other (26) |
N = 240; NS |
<30: 63 (20.2%) 31–50: 129 (53.8%) 51–65: 45 (18.8%) >65: 3 (1.3%) |
Inpatient |
| Ashcroft et al. (2021)/Canada |
Social Worker (20) MH Therapist (10) Program Manager/Coordinator (9) Executive Director (4) Nurse (3) Physician (2) |
N = 48 | NS | Family Health Teams |
| Bae et al. (2022)/Korea |
Psychiatrist (1) Nurse (5) Nurse's aide (2) Administrative staff (2) Caretaker (1) |
N = 11; 5M, 6F | 40.91 ± 9.75 | Inpatient |
| Bekes et al. (2020)/United States |
Psychologist (83) Medical Doctor (45) Social Worker (32) Counsellor (10) Marriage Family Therapist (2) Other (e.g. psychoanalyst/psychotherapist; 18) |
N = 190; 127F, 63M | 60.5 ± 15 | Inpatient, outpatient, private practice |
| Bentham et al. (2021)/United Kingdom |
Nurse (16) Medical (5) Therapists (24) Social Worker (1) NR (5) |
N = 51; 37F, 9M, 5NR | NS | CAMHS |
| Bhome et al. (2021)/United Kingdom |
Nurse (65) Occupational Therapist (21) Psychologist (19) Psychiatrist (18) Peer Support Worker (8) Social Worker (1) Other (26) |
N = 158; 128F | NS | Inpatient, outpatient |
| Billings et al. (2021)/United Kingdom |
Clinical Psychologist (13) Trainee Clinical Psychologist (3) Psychological Well‐being Practitioner (3) High‐intensity CBT Therapist (2) Psychiatrist (2) MH Occupational Therapist (22) Counselling Psychologist (1) Mental Health Practitioner (1) General Practitioner (special interest in mental health; 1) |
N = 28; 23F, 5M | NS | Inpatient, outpatient, specialized clinic |
| Bommersbach et al. (2021)/United States |
Licensed Independent Practitioner (APRN, MD; 6) Social Worker (6) Chaplain (1) Administrator (2) Clinical manager (1) Physical Therapist/Occupational Therapist (1) |
Focus groups: N = 17; 16F |
30–39: 3 (17.6%) 40–49: 5 (29.4%) 50–59: 5 (29.4%) 60–69: 3 (17.6%) NS: 1 (5.9%) |
Inpatient, outpatient |
| Brillon et al. (2021)/Canada |
Psychologist (204) Psychosocial Counsellor (137) Social Worker (74) Clinical Counsellor (55) Other types of mental health providers (e.g. psychiatrists, art therapists, criminologists; 146) |
N = 1274; 1136F | 42.06 ± 12.58 | NS |
| Cabeza et al. (2022)/Colombia |
Psychiatrist (31) Medical Doctor (50) Registered Nurse (52) Health‐care Assistant (125) Psychologist (40) Occupational Therapist (7) Social worker (14) Other (110) |
N = 429; 282F | 33.4 ± 2.68 | Inpatient |
| Carpiniello et al. (2020)/Italy |
Mental Health Departments (71) General Hospital Psychiatric Wards (107) |
NS | NS | Inpatient, outpatient |
| Chemerynska et al. (2021)/United Kingdom | Clinical Psychologist (11) | N = 11; 10F | Median = 41 | Outpatient |
| Csigo & Ritzl (2021)/Hungary |
Psychiatrists/Psychologists (78) Nurses/Other Professionals (41) |
N = 119; 97F, 22M | 41.66 ± 11.20 | Inpatient |
| Dores et al. (2020)/Portugal | Psychologists (108) | N = 108; 89F, 19M | 37.20 ± 10.05 | NS |
| Eddy (2021)/United Kingdom | NS | N = 464 |
18–25: 19 (4.0%) 26–35: 88 (19.0%) 36–45: 97 (21.0%) 45–55: 167 (36.0%) 56–65: 88 (19.0%) >65: 5 (1.0%) |
Inpatient, outpatient |
| Fish & Mittal (2021)/ United States | NS | N = 137 | NS | NS |
| Gao & Tan (2021)/Singapore | Nurse (18) | N = 18 | NS | Inpatient |
| Garcia et al. (2022)/United States |
Clinical Psychology (9) Counselling Psychology (10) School Psychology (4) |
N = 23 | NS | Private practice |
| Guinart et al. (2021)/United States |
Social Worker (247) Licensed Patient Counsellor/Mental Health Counsellor (106) Psychologist/Therapist (88) Care Coordinator/Case Manager (84) Psychiatrist (77) Recovery Coach/Peer Counsellor (73) Nurse/NP (49) Physician (26) Administrative Personnel (20) Resident/Fellow (17) Research Coordinator (6) Other (10) |
N = 819 |
<25: 22 (3.0%) 25–34: 254 (31.0%) 35–44: 216 (27.0%) 45–54: 137 (17.0%) 55–64: 129 (16.0%) 65–74: 48 (6.0%) >74: 4 (1.0%) |
Inpatient, outpatient, residential, specialized clinics |
| Johnson et al. (2020)/United Kingdom |
Nurse (664) Psychologist (347) Psychiatrist (254) Social Worker (97) Peer Support Worker (80) Occupational Therapist (171) Other Qualified Therapist (189) Manager, no professional qualification (63) Other (307) |
N = 2180; 1378F, 341M, 4NS |
<25: 64 (3.7%) 25–34: 385 (22.5%) 35–44: 411 (24.0%) 45–54: 535 (31.2%) 55–64: 298 (17.4%) ≥65: 21 (1.2%) |
Inpatient, residential, outpatient |
| Jokić‐Begić et al. (2020)/Croatia | Psychiatrists (165) | N = 725; 521F | 48.3 ± 11.26 | NS |
| Kagan et al. (2021)/Israel | Nurse Manager (25) | N = 25 | NS | Inpatient |
| Kameg et al. (2021)/China |
APRN (54) RN (74) Other MH Worker (10) |
N = 151; 116F, 23M, 1NB | NS | Inpatient, outpatient |
| Kuki et al. (2021)/Japan |
Doctor Nurse Occupational Therapist Psychologist Laboratory Technician Psychiatric Social Worker Pharmacist Dietitian Other (e.g. officer) |
N = 426; 173M, 253F |
20–29: 53 (12.4%) 30–39: 63 (14.8%) 40–49: 131 (30.8%) 50–59: 108 (25.4%) >59: 71 (16.7%) |
NS |
| Langdon et al. (2021)/United Kingdom | Registered Psychologist (97) | N = 97; 19M, 78F |
21–30: 8 (8.2%) 31–40: 40 (41.2%) 41–50: 28 (28.9%) 51–60: 19 (19.6%) 61–70: 2 (2.1%) |
NS |
| Liberati et al. (2021)/United Kingdom |
Psychiatrist (17) MH Nurse (10) Psychotherapist (5) Clinical Psychologist (3) |
N = 35; 19F, 11M, 5NR | NS | Inpatient, outpatient |
| Limoges et al. (2021)/Canada |
Nursing (43) Allied Health (13) |
N = 56 |
<30: 15 (26.8%) 31–50: 21 (37.5%) 51–65: 20 (35.7%) |
Inpatient |
| Lin et al. (2021)/ United States |
Psychologist (253) Counsellor (45) Social Worker (9) Student Trainee (109) Other MH Professionals (e.g. psychiatrists; 24) |
N = 440; 318F, 117M, 5NB | 48.44 | Inpatient, outpatient, private practice |
| McBeath et al. (2020)/United Kingdom | Psychotherapist (335) | N = 335; 79%F, 18%M, 3%NS | NS | NS |
| Miller & Grise‐Owens (2022)/United States | Social Worker (3920) | N = 3920; 424M, 3436F, 20NS | 42.77 ± 12.01 | NS |
| Minelli et al. (2022)/Italy |
Nurse (86) Psychiatrist/Training psychiatrist (60) PRT/Educator (59) Psychologist/Psychotherapist (44) Other mental health professions (22) |
N = 271; 198F, 73M | 45.37 ± 10.94 | Inpatient, outpatient, residential |
| Morse & Dell (2021)/United States | NS | N = 168 | NS | Outpatient |
| Murphy et al. (2021)/United States |
President/CEO (51) Associate CEOs, Vice Presidents, Senior or Division Directors and other executives (108) Program or Unit Directors (89) Staff members below the director level (47) |
N = 295 | NS | Inpatient, residential, outpatient, emergency services |
| Nair et al. (2021)/India |
Manager of Clinical Services Administrative Staff Psychiatrist Social Worker Psychologist Researcher Staff employed in community research projects |
N = 10 | NS | Inpatient, residential, outpatient, research and training |
| Oderinde et al. (2021)/Nigeria |
Doctor (15) Nurse (97) Pharmacist (9) Laboratory scientist (9) Health attendant (20) Social worker (15) Other (e.g. clinical psychologist, occupational therapist, medical record officer; 23) |
N = 200; 71M, 129F | Median = 40 | Inpatient, outpatient, emergency services |
| Ogutlu et al. (2021)/Turkey |
Adult psychiatrists (109) Child psychiatrists (108) |
N = 217; 150F, 67M | Median = 33 | Inpatient, outpatient |
| Olwill et al. (2021)/Ireland |
NCHD (14) Consultants (12) |
N = 26 |
25–34: 10 (38%) 35–44: 9 (35%) 45–54: 2 (8%) 55–64: 4 (15%) ≥65: 1 (4%) |
Outpatient |
| Pappa et al. (2021)/United Kingdom |
Doctors (45) Nurses (46) Psychologists (52) Health Care Assistant (21) Administrative/ Management (41) Other (76) |
N = 387; 78M, 201F, 4NR |
16–20: 1 (0.4%) 21–30: 64 (22.6%) 31–40: 57 (20.1%) 41–50: 71 (25.1%) 51–65: 83 (29.3%) ≥66: 7 (2.5%) |
Inpatient, outpatient |
| Phillips et al. (2021)/United States |
Psychologist (71) Licensed Counsellor (17) Licensed Marriage and Family Therapist (5) Clinical SW (94) Other Licence (12) |
N = 207; 165F, 39M, 1NB, 2NR | 52.90 ± 12.22 | Private practice |
| Rapisarda et al. (2020)/Italy |
Psychologist (73) Counsellor (68) Medical doctor (28) Social Worker (15) Nurse (27) Peer Supporter (9) Support Worker (7) Manager/coordination (7) Other (7) |
N = 241; 185F | 46.5 ± 12.0 | Inpatient, outpatient |
| Romanchych et al. (2022)/Canada |
Therapist (75) Medical Practitioner (15) Other (27) |
N = 117; NS | NS | Hospital, community mental health centre |
| Rosenheck et al. (2021)/United States | VA staff (112) | N = 217 | NS | Inpatient, outpatient |
| Schneider et al. (2021)/United States |
Psychology Intern (259) Psychology Postdoctoral Fellow/Resident (143) |
N = 400; 347F, 46M, 7NS | 30.87 ± 5.23 | Inpatient, outpatient, private practice, school |
| Shklarski et al. (2021)/United States |
Social Worker (74) Psychologist (16) Counselling (2) |
N = 92; 83F, 9M | 46.2 ± 18.02 |
Institutional practice, private practice |
| Sklar et al. (2021)/United States |
Drug/Alcohol Counselling (13) Social Work (44) Child Development (2) Marriage and Family Therapy (2) Psychology (16) Other (15) NR (1) |
N = 93; 77F, 14M, 1NS, 1NR | 42 ± 14.2 | CMHC |
| Slone et al. (2021)/United States |
Psychiatrist (100) MH Counsellor (100) Social Worker (100) Psychologist (100) Marriage and Family Therapist (100) |
N = 500; 241F, 259M | 40.6 ± 6.6 | Inpatient, outpatient |
| Smith & Gillon (2021)/United Kingdom | Psychotherapist (5) | N = 5; 4F, 1M | NS | Private practice, third sector organization |
| Steidtmann et al. (2021)/United States |
Clinician (14) Psychiatrist (6) Psychiatric Nurse Practitioner (3) Psychologists (4) Social Worker (1) |
N = 25 | NS | Outpatient |
| Sun et al. (2021)/China |
General Physician (389) General Nurse (147) |
N = 536; 370F, 166M | 39 ± 9.63 | Outpatient |
| Trabucco et al. (2021)/Italy |
Psychiatrist (66) Psychologist (104) Psychotherapists (49) |
N = 219; 125F | 47.5 ± 9.5 | Public healthcare sector, private healthcare sector |
| Xie et al. (2021)/ China | NS | N = 10 516; 1630M | 33.2 ± 8.4 | Inpatient |
| Zhu et al. (2022)/China |
Nurse (173) Doctor (83) Technician (14) |
N = 270 | 35.33 ± 8.21 | Inpatient, outpatient |
APRN, Advanced Practice Registered Nurse; CAMHS, Child and Adolescent Mental Health Service; CEO, Chief Executive Officer; CMHC, Community Mental Health Centre; F, female; M, male; MD, Medical Doctor; MH, mental health; NB, non‐binary; NP, Nurse Practitioner; NR, not reported; NS, not specified; PRT, Psychiatric Rehabilitation Therapist; RN, Registered Nurse; VA, Veterans Affair.
Work outcomes
Of the 55 studies, 43 reported work outcomes of MHWs during the COVID‐19 pandemic (see Table 2). Work outcomes included changes in working conditions (N = 25), factors related to occupational well‐being (N = 30), job attitudes (N = 10) and job performance (N = 3).
Table 2.
Work outcomes of MHWs during the COVID‐19 pandemic
| Author (Year) | Measures | Key findings |
|---|---|---|
| Aafjes‐van Doorn et al. (2020) | VTS, non‐validated measure of in‐session experiences | Increased fatigue during therapy sessions (74.9%), decreased competency (34.7%), decreased connection with clients (43.0%), moderate to high vicarious trauma (77.6%) |
| Adams et al. (2021) | Non‐validated questionnaire | Loss of job (9.0%), engagement in new tasks (73.0%), decrease in support tasks (such as individual support provision and group facilitation) |
| Ashcroft et al. (2021) | Semi‐structured interviews | Increase in workload, exhaustion, and isolation |
| Bae et al. (2022) | Semi‐structured interviews | Staff shortages, fear of COVID‐19 infection, guilt related to newly confirmed cases, exhaustion, and distress related to separation from family |
| Bekes et al. (2020) | Non‐validated questionnaire | Lower levels of competence (31.6%), lower confidence in their skills in online therapy (25.3%), increased fatigue conducting online therapy than in F2F sessions (75.3%) |
| Bhome et al. (2021) | Non‐validated online survey |
MHWs in inpatient settings reported concerns included the risk of COVID‐19 spreading between patients (80.6%), the risk they or their colleagues could be infected with COVID‐19 (74.6%), rapid adaption to new work methods (66.7%) MHWs in CMHT reported concerns of patients receiving inadequate services due to service reconfiguration (43.1%), rapid adaption to new work methods (43.1%) and new technologies without adequate training and support (37.9%) |
| Billings et al. (2021) | Semi‐structured interviews | MHWs were motivated and driven to support general healthcare workers. MHWs reported increased workload and working hours, isolation, and reduced confidence in their skills, confidentiality, competence, and poorer therapeutic relationships through telehealth |
| Bommersbach et al. (2021) | Qualitative online survey, focus groups | Increased fatigue |
| Carpiniello et al. (2020) | Non‐validated questionnaire | CMHCs (91.5%) and GHPWs (84.1%) reported concerns about safety and concerns that PPE supply was only partly adequate or inadequate. 52.1% of CMHCs and 28.0% of GHPWs reported COVID‐19 positive cases amongst staff. 21.4% of MHDs reported increased aggression and violence amongst patients |
| Chemerynska et al. (2021) | Semi‐structured interviews | Experiences of guilt and inadequacy related to telehealth, feeling disconnected from their colleagues and clients, inadequate support from management, isolation, difficulty with work‐life balance while WFH, burnout, increased referral rates and increased complexity of presenting patients |
| Dores et al. (2020) | Three‐section non‐validated questionnaire | Difficulties with telehealth practice included establishing and/or maintaining the therapeutic relationship (62.0%) and a lack of non‐verbal communication (61.1%) |
| Eddy (2021) | Five‐section questionnaire | Concern over infection control measures (67.0%) and difficulties communicating with patients (77.0%) |
| Fish & Mittal (2021) | Qualitative online survey | Decreased ability to support patients (82.0%), telehealth fatigue, empathic distress, job dissatisfaction, and feeling physically exhausted |
| Gao & Tan (2021) | Qualitative feedback forms | Feeling physically exhausted |
| Garcia et al. (2022) | 27‐question online survey (mostly qualitative) | Negative impact on work, increased distraction, decreased motivation, Some MHWs (60.9%) reported increased connection with patients, difficulties with work‐life balance while WFH (17.4%) |
| Guinart et al. (2021) | Mixed‐methods online survey | Concerns about missing relevant information (36.0%) and decreased connection with patients (46.0%). Some MHWs reported increased patient engagement through telehealth (41.0%) |
| Johnson et al. (2020) | Mixed‐methods online survey | Concern over rapid adaptation to telehealth (37.4%), working longer hours (21.1%), greater workload (28.5%), safety concerns (25%), inadequate supply of PPE (24.8%), risk of COVID‐19 infection (40.2%), concern of infecting family and friends (35.6%), staff shortages (22.4%) |
| Kagan et al. (2021) | Validated online questionnaire, focus groups |
Increased burnout and fatigue, shortage of PPE, longer hours, and increased workload NUMs reported burnout and feeling overwhelmed, new job demands, changed work functions, but job satisfaction remained high |
| Kameg et al. (2021) | PFI, CAS, PHQ‐8, GAD‐7, items related to burnout, WEMWBS | Decreased professional fulfilment, increased job interference with family life (64%), moderate job satisfaction |
| Langdon et al. (2021) | Mixed‐methods online survey, HSE Management Standards Indicator Tool, WEMWBS | Changes to job requirements including redeployment (23.7%), increased focus upon telephone sessions (84.5%) and video sessions (72.2%), satisfaction and feeling effective at work (50.0%) |
| Liberati et al. (2021) | Semi‐structured interviews | Increased tension and agitation amongst patients in inpatient units, increased workplace violence and stress for MHWs, increased job responsibility, increased hours, concern over threat of redeployment to alternate health service, increased moral injury, challenges with work‐life balance while WFH, decreased support while WFH, isolation, reduced confidence in decision‐making, concern over rapport via telehealth |
| Limoges et al. (2021) | Semi‐structured interviews, open‐ended online survey | Concern of contracting COVID‐19, increased working hours, job variation due to redeployment, stress related to increased patient agitation related to mandated restrictions |
| Lin et al. (2021) | Three‐section online survey | Decreased confidence in skills using telehealth compared to in‐person therapy |
| McBeath et al. (2020) | Mixed‐methods online survey | Telehealth fatigue, reduction in confidence in skills and isolation while WFH |
| Minelli et al. (2022) | Questions about COVID‐19 exposure | Increased workload (42.8%) |
| Morse & Dell (2021) | Mixed‐methods online survey; non‐validated measures of burnout, work satisfaction, supervision, employee engagement | Increased burnout (21.4%), difficulty maintaining work‐life balance while WFH, high job satisfaction (85.7%), satisfaction with training (73.8%), provision of appropriate equipment and resources (53.0%) |
| Murphy et al. (2021) | Qualitative online survey | Burnout and stress related to increased workload (40.0%), concern over contracting COVID‐19 (19.0%), concern over inadequate PPE supply (62.0%) |
| Nair et al. (2021) | In‐depth interviews, focus group | Difficulty maintaining work‐life balance while WFH, increased working hours, decreased interactions with colleagues |
| Ogutlu et al. (2021) | Online study‐specific questionnaire, CBI | At least moderate levels of work‐related burnout 60.8%, at least moderate levels of patient‐related burnout (49.8%), at least moderate levels of personal burnout (31.8%), moderate or high stress (58.1%) |
| Olwill et al. (2021) | Study‐specific mixed‐methods questionnaire | Reduced confidence in making a diagnosis amongst Consultant Psychiatrists (100.0%) and NCHDs (86.0%), decreased confidence in prescribing medication via telehealth amongst Consultant Psychiatrists (33.0%) and NCHDs (43.0%), difficulties with therapeutic alliance (specifically with new clients and establishing rapport without visual cues), increased flexibility and shorter consultation times using telehealth |
| Pappa et al. (2021) | MBI | Moderate to high level of emotional exhaustion (52.3%), moderate to high level of depersonalisation (19.5%), moderate to high level of personal accomplishment (71.7%) |
| Rapisarda et al. (2020) | MBI, ad hoc questions related to work conditions | Severe burnout (31.7%), increased workload (21.2%) |
| Romanchych et al. (2022) | Non‐validated questionnaire | Increased fatigue (70.0%), increased difficulty looking at a computer for extended periods (78.0%), and increased need for extra breaks (59.0%) due to telehealth |
| Rosenheck et al. (2021) | Study‐specific measures of therapeutic alliance and mental health status | Decreased therapeutic relationship due to telehealth |
| Schneider et al. (2021) | Mixed‐methods survey, non‐validated measure of perceived safety and support | MHWs reported feeling unsafe due to inadequate PPE supply and cleaning supplies (49.4%) |
| Shklarski et al. (2021) | Non‐validated questionnaire, qualitative interviews | Difficulty supporting patients with trauma while dealing with own trauma (60.8%), lack of support during transition to telehealth, zoom fatigue |
| Sklar et al. (2021) | Non‐validated measure of COVID‐related work changes, CWBI | Moderate to high burnout, increased role changes, increased turnover intention |
| Slone et al. (2021) | Study‐specific work‐related changes (employment, caseload) and perceptions of quality of care and therapeutic relationships | Role changes (92.0%), increased in caseload (37.0%), decrease in caseload (38.1%) |
| Smith & Gillon (2021) | Semi‐structured interviews | Improvement in counselling skills due to telehealth transition |
| Steidtmann et al. (2021) | Study‐specific mixed‐methods online survey | Increased burnout, compassion fatigue and/or vicarious trauma amongst MHWs (38.5%), fatigue due to telehealth (21.4%), isolation (16.0%), difficulties with work‐life balance (12.0%) |
| Trabucco et al. (2021) | Non‐validated questionnaire | Fear related to inadequate clinical monitoring (particularly for inpatient care), difficulty in concentration while WFH |
| Xie et al. (2021) | WPVS (Chinese version), 2 items from WHOQoL‐BREF | Experience of workplace violence (18.5%) was associated with lower overall QoL and greater anxiety |
| Zhu et al. (2022) | MBI (Chinese version) | MHWs reported at least a mild degree of burnout (50.3%) |
Only measures that are associated with the reported results are listed in the table.
CBI, Copenhagen Burnout Inventory; CMHCs, community mental health centre; CMHT, community mental health teams; CWBI, Copenhagen Work Burnout Inventory; F2F, face‐to‐face; GHPWs, general hospital psychiatric wards; HSCWs, health and social care workers; MH, mental health; MBI, Maslach Burnout Inventory; MHW, mental health worker; NCHD, Non‐consultant hospital doctor; NUM, Nurse Unit Manager; PPE, personal protective equipment; QoL, quality of life; VTS, Vicarious Trauma Scale; WFH, working from home; WHOQOL‐BREF, World Health Organization Quality of Life Questionnaire ‐ Brief Version; WPV, workplace violence; WPVS, Workplace Violence Scale.
Changes in working conditions
Increased workload was consistently reported across included studies (Ashcroft et al. 2021; Billings et al. 2021; Johnson 2020; Kagan et al. 2021; Minelli et al. 2022; Murphy et al. 2021). Many studies also reported staff working longer hours than usual (Johnson 2020), whether to cover staff absences (Liberati et al. 2021) or due to remote working, perturbing boundaries between work and home life (Nair et al. 2021). Increased staff shortages due to the COVID‐19 pandemic were also reported (Bae et al. 2022; Johnson 2020). Two additional studies reported increases in demand for services, including increased referral rates (Chemerynska et al. 2021), or number of new patient requests, and a greater frequency of appointments for existing patients (Slone et al. 2021).
Mental healthcare workers experienced changes to work tasks during the COVID‐19 pandemic. These included nurse unit managers functioning as nurses on the wards (Kagan et al. 2021), an increased focus on referral resources by peer support specialists (Adams et al. 2021) and redeployment to other roles, including outside of qualified discipline (Langdon et al. 2021; Limoges et al. 2021). Such changes often occurred with little notice and without discussion, causing significant stress (Liberati et al. 2021).
Two studies reported decreased job security for MHWs during the pandemic. A small proportion of peer support specialists in the United States (US) were reported to have lost their job due to COVID‐19, while others experienced a reduction in working hours (Adams et al. 2021). A separate study conducted in the US reported almost two‐thirds of MHWs were no longer practising after the onset of the pandemic, with reduced hours for those who continued working (Slone et al. 2021).
Many MHWs who worked remotely throughout the pandemic reported reductions in confidence in their skills, confidentiality, competence and some also reported an impact on their therapeutic relationships with patients (Bekes et al. 2020; Billings et al. 2021; Chemerynska et al. 2021; Dores et al. 2020; Garcia et al. 2022; Guinart et al. 2021; Liberati et al. 2021; Lin et al. 2021; McBeath et al. 2020; Olwill et al. 2021; Rosenheck et al. 2021; Smith & Gillon 2021; Trabucco et al. 2021), with one study raising concerns about patient safety (McBeath et al. 2020). However, two studies reported no change in confidence, competence or therapeutic relationships since before the pandemic and the introduction of online therapy (Aafjes‐van Doorn et al. 2020; Trabucco et al. 2021) and four studies reported positive impacts of telehealth practice including improvement of skills (Smith & Gillon 2021), increased comfort and engagement of patients during telehealth sessions (Guinart et al. 2021; Trabucco et al. 2021) and increased relatability to patients through shared experience of the COVID‐19 pandemic (Garcia et al. 2022).
Occupational well‐being
Outcomes related to occupational well‐being of MHWs were reported across 30 studies. There were numerous reports of moderate‐to‐high levels of burnout, exhaustion, and fatigue amongst MHWs during the COVID‐19 pandemic (Ashcroft et al. 2021; Bae et al. 2022; Bommersbach et al. 2021; Chemerynska et al. 2021; Eddy 2021; Fish & Mittal 2021; Gao & Tan 2021; Kagan et al. 2021; Kameg et al. 2021; Liberati et al. 2021; Morse & Dell 2021; Murphy et al. 2021; Ogutlu et al. 2021; Pappa et al. 2021; Rapisarda et al. 2020; Sklar et al. 2021). These outcomes were attributed to increased workload, stress, feelings of uncertainty and changes in workplace practices (Chemerynska et al. 2021; Kameg et al. 2021; Liberati et al. 2021; Murphy et al. 2021; Sklar et al. 2021). One study found that burnout was highest when work changes were most profound (Sklar et al. 2021), another reported no demonstrable change in burnout levels in majority of MHWs (Steidtmann et al. 2021) or only experienced mild burnout (Zhu et al. 2022). An additional five studies found that MHWs who worked remotely and conducted online therapy experienced increased fatigue during online therapy, also referred to as ‘zoom fatigue’ (Aafjes‐van Doorn et al. 2020; Bekes et al. 2020; Fish & Mittal 2021; McBeath et al. 2020; Romanchych et al. 2022; Shklarski et al. 2021; Steidtmann et al. 2021).
Several studies reported difficulty in management of work‐life balance by MHWs (Chemerynska et al. 2021; Garcia et al. 2022; Johnson 2020; Kameg et al. 2021; Liberati et al. 2021; Morse & Dell 2021; Nair et al. 2021; Steidtmann et al. 2021; Trabucco et al. 2021). This was attributed to blurred boundaries between work and home life while working from home (Chemerynska et al. 2021; Johnson 2020; Morse & Dell 2021; Nair et al. 2021) which was compounded by increased distractions and difficulty concentrating (Garcia et al. 2022; Trabucco et al. 2021), as well as some MHWs feeling as though they were always at work (Liberati et al. 2021). One study, however, found only a small minority of participants experienced difficulties separating work and nonwork responsibilities (Steidtmann et al. 2021). Moreover, job demands for MHWs working in inpatient or outpatient mental health settings were also reported to interfere with family life (Kameg et al. 2021).
A smaller number of studies examined the level of support felt by MHWs during the pandemic, which differed according to workplace setting. Five studies reported reduced access to formal and informal supports for MHWs working remotely (Chemerynska et al. 2021; Johnson 2020; Liberati et al. 2021; Murphy et al. 2021; Nair et al. 2021), yet two studies reported adequate support by colleagues, supervisors and management by MHWs in inpatient or outpatient settings (Billings et al. 2021; Gao & Tan 2021).
Elevated levels of compassion fatigue, empathic distress and vicarious trauma were reported amongst MHWs in five studies (Aafjes‐van Doorn et al. 2020; Billings et al. 2021; Fish & Mittal 2021; Shklarski et al. 2021; Steidtmann et al. 2021). Vicarious trauma was reported following redeployment of MHWs to other healthcare settings, where they witnessed traumatic events, such as patients dying (Billings et al. 2021). Another two reported sources of vicarious trauma through experiences of shared trauma (Billings et al. 2021; Shklarski et al. 2021) and one study observed that vicarious trauma was most frequently reported amongst those of younger age and less clinical experience (Aafjes‐van Doorn et al. 2020). Another two studies revealed evidence of moral injury, which was associated with feeling as though patients had been let down through online service provision (Liberati et al. 2021), leading to MHWs feeling guilty and inadequate (Chemerynska et al. 2021). A further study reported distress amongst MHWs related to patients being separated from family while under isolation in a psychiatric hospital (Bae et al. 2022).
Rates of workplace violence during the pandemic were also reported; two studies found that mandated restrictions, particularly within inpatient units, caused increased agitation and anger amongst patients (Limoges et al. 2021), and in some cases led to more incidents of verbal or physical abuse (Liberati et al. 2021). A third study found that the 2‐month prevalence of workplace violence amongst MHWs was substantially lower during the COVID‐19 pandemic than previously reported rates; however, it is important to note that previous studies had been conducted over longer timeframes (Xie et al. 2021). Those who experienced workplace violence demonstrated significantly lower overall quality of life, as well as significantly higher levels of anxiety than those who had not (Xie et al. 2021).
Job attitudes
High levels of job satisfaction amongst MH nurse managers and behavioural healthcare workers were reported (Kagan et al. 2021; Morse & Dell 2021), while another study reported lower levels of job satisfaction amongst US‐based MHWs (e.g. licensed social workers, marriage and family therapists, counselling psychologists; Fish & Mittal 2021). A further two studies reported moderate levels of job satisfaction or no change in job satisfaction during the COVID‐19 pandemic amongst MHWs (Kameg et al. 2021; Langdon et al. 2021).
Outcomes related to work engagement during the pandemic were again mixed; two reported increased work engagement (Billings et al. 2021; Csigo & Ritzl 2021) while three reported decreased work engagement (Fish & Mittal 2021; Garcia et al. 2022; Trabucco et al. 2021). Turnover intention was greater in those who had experienced high levels of burnout (Sklar et al. 2021).
Job performance
Three studies reported perceived decreased job performance by MHWs during the COVID‐19 pandemic due to factors ranging across difficultly communicating with patients in PPE (Gao & Tan 2021), insufficient appropriate resources (Morse & Dell 2021) and decreased well‐being (Johnson et al. 2020). One of these studies also reported reduced confidence in skills amongst MHWs within an inpatient unit, due to the novel situation the COVID‐19 pandemic presented, with many having no previous experience caring for patients during a pandemic (Gao & Tan 2021).
Personal outcomes
In total, 33 of the included studies reported personal outcomes of MHWs during the COVID‐19 pandemic (see Table 3.). These outcomes included well‐being (N = 8), psychological distress (N = 31), resilience (N = 3) and psychosocial impacts (N = 18).
Table 3.
Personal outcomes of MHWs during the COVID‐19 pandemic
| Author (Year) | Measures | Key findings |
|---|---|---|
| Abdelfattah (2020) | Semi‐structured interviews | Anxiety related to passing COVID‐19 onto family members |
| Anzola et al. (2022) | CAS, DASS‐21 | Mild to extremely severe depressive symptoms (>50%), COVID‐19 anxiety within clinical range (26.4%) |
| Bae et al. (2022) | Semi‐structured interviews | Distress related to separation from family |
| Bentham et al. (2021) | WEMWBS, subjective rating of worry | Well‐being of MHWs was below normative population levels. MHWs reported a high degree of worry, which was greater in those WFH. Concerns included risk of family or friends being infected (80.0%), risk of contracting the infection (63.0%), social isolation due to lockdown (47.0%) |
| Bhome et al. (2021) | Non‐validated online survey | MHWs reported concern over risk of passing COVID‐19 onto family and friends (36.3%) |
| Billings et al. (2021) | Semi‐structured interviews | Redeployed MHWs reported direct and indirect exposure to traumatic and morally injurious events, experiences of shared trauma, and poorer well‐being |
| Bommersbach et al. (2021) | Qualitative online survey, focus groups | Increased anxiety |
| Brillon et al. (2021) | English and French versions of PHQ‐9, GAD‐7, UCLA Loneliness Scale, CD‐RISC | MHWs reported lower symptoms of depression and anxiety, and higher experiences of loneliness and vi than workers from the general population. In regions with a high incidence of COVID‐19, MHWs reported higher symptoms of anxiety and depression, greater experiences of loneliness and lower resilience, than those in regions with a low incidence of COVID‐19 |
| Cabeza et al. (2022) | PSQI (Colombian version), qualitative online survey questions | Poor sleep quality (48.7%), sleep was negatively impacted by COVID‐19 (33.0%), dreams related to COVID‐19 (10.4%), nightmares related to COVID‐19, particularly fear of infection or infecting others (7.2%) |
| Chemerynska et al. (2021) | Semi‐structured interviews | MHWs reported poorer well‐being |
| Csigo & Ritzl (2021) | Non‐validated questionnaire | Psychiatrists/psychologists reported higher anxiety than other MHWs (e.g. nurses, social workers) and 97.5% were concerned about their family members |
| Eddy (2021) | Five‐section questionnaire | Negative impact on relationships (44.0%), less desire to interact with others (55.0%) and social isolation (66.0%), concern of COVID‐19 infection (61.0%), concern of infecting family and friends (78.0%), negative impact on mental health (80.0%) |
| Fish & Mittal (2021) | Qualitative online survey | MHWs reported feeling distressed, depressed, anxious, isolated, fearful, not sleeping well, and having migraines |
| Gao & Tan (2021) | Qualitative feedback forms |
MHWs reported feeling shocked, worried, isolated, reduction in confidence, but felt supported by leaders and management MHWs reported difficulties in effectively communicating with patients in full PPE and observations of increased tensions with patients |
| Garcia et al. (2022) | 27‐question online survey (mostly qualitative) | Increased stress/anxiety (30.4%), improved coping skills, self‐care, and mindfulness (30.4%) |
| Johnson et al. (2020) | Mixed‐methods online survey | MHWs reported decreased job capability due to own safety (19.5%) and difficulties managing work‐life balance while WFH (25.4%) |
| Jokić‐Begić et al. (2020) | CAS, COVID‐19 Pandemic Concerns, CORE‐YP, BRS | Compared with general health physicians, psychiatrists reported decreased anxiety but did not differ in resilience, psychological distress, or COVID‐19 pandemic concerns |
| Kameg et al. (2021) | CAS, PHQ‐8, GAD‐7, WEMWBS | Mild anxiety and depressive symptoms, average levels of mental well‐being |
| Kuki et al. (2021) | GAD‐7 (Japanese version), PHQ‐9 (Japanese version) | Increased anxiety and depression in MHWs in close contact with COVID‐19 patients |
| Langdon et al. (2021) | Mixed‐methods online survey, HSE Management Standards Indicator Tool, WEMWBS | Worry about health (87.3%), worry about health of patients (80.9%), lower well‐being scores than the general population |
| Liberati et al. (2021) | Semi‐structured interviews | MHWs had decreased mental well‐being, increased anxiety, and increased personal leave |
| Miller & Grise‐Owens (2022) | CPDI | Mild or severe COVID‐related distress (46.4%) |
| Minelli et al. (2022) | IES‐R, DASS‐21 | MHWs reported increased post‐traumatic stress symptoms, and increased depressive, anxiety, and stress symptoms |
| Morse & Dell (2021) | Mixed‐methods online survey | MHWs reported stress related to changes to routines, concern for health of family and friends and fear of uncertainty |
| Murphy et al. (2021) | Qualitative online survey | Isolation and decreased support while WFH (25.0%), anxiety and fear (19.0%), decreased mental well‐being (16.0%) |
| Nair et al. (2021) | In‐depth interviews, focus group | Concern over passing COVID‐19 onto family members, difficulties with work‐life balance and reduced time spent with family |
| Oderinde et al. (2021) | Sleep problems (single item) | Sleep problems (23.9%) |
| Pappa et al. (2021) | PHQ‐9, GAD‐7, AIS, RS‐14 | Degree of insomnia (51.6%), mild anxiety symptoms (25.8%), moderate to severe levels of anxiety symptoms (15.9%), mild depressive symptoms (25.8%), moderate to severe levels of depressive symptoms (21.9%), moderate to high level of resilience (94.7%) |
| Phillips et al. (2021) | PSS, non‐validated measure of work changes | Moderate stress levels, commonly related to concerns about COVID‐19, childcare issues due to shutdowns, needing to care for a nonchild loved one. Financial stress was reported by MHWs to be related to decreased practice, insurance concerns and office space rental while working remotely |
| Rapisarda et al. (2020) | GAD‐7, PHQ‐9, ad hoc questions related to work conditions | Somewhat or very worried about COVID‐19 infection (37.8%), moderate/severe anxiety in inpatient settings (16.1%) and outpatient settings (9.1%), moderate/severe depression in inpatient settings (8.0%) and outpatient settings (5.8%) alongside sleep problems, tiredness, and decreased energy |
| Schneider et al. (2021) | Mixed‐methods survey, GAD‐2, PHQ‐2, non‐validated measure of perceived safety and support | Clinically significant anxiety symptoms (40.8%), depressive symptoms (21.7%), concern about passing the virus onto others including family/patients (16.9%) |
| Smith & Gillon (2021) | Semi‐structured interviews | Increased anxiety |
| Sun et al. (2021) | PHQ‐9 | Depressive symptoms (18.8%), anxiety symptoms (9.7%) |
Only measures that are associated with the reported results are listed in the table.
AIS, Athens Insomnia Scale; BRS, Brief Resilience Scale; CAS, COVID‐19 Anxiety Scale; CD‐RISC, Connor Davidson Resilience Scale; CMHCs, community mental health centre; CMHT, community mental health teams; CPDI, COVID‐19 peritraumatic distress index; DASS‐21, Depression, Anxiety Stress Scale; GAD, General Anxiety Disorder; GHPWs, general hospital psychiatric wards; HSCWs, health and social care workers; IES‐R, Impact of Event Scale‐Revised; MH, mental health; MHD, mental health department; MHW, mental health worker; NFRS, Numerical Fear Rating Scale; NUM, Nurse Unit Manager; PHQ, Patient Health Questionnaire; PPE, personal protective equipment; PSS, Perceived Stress Scale; RS, Resilience Scale; WEMWBS, Warwick‐Edinburgh Mental Well‐being Scale; WFH, working from home; WPV, workplace violence.
Well‐being
Decreased well‐being was frequently reported amongst MHWs throughout the COVID‐19 pandemic, often due to working extra hours and sacrificing work‐life balance, or the stress of being potentially exposed to COVID‐19 (Billings et al. 2021; Chemerynska et al. 2021; Liberati et al. 2021; Murphy et al. 2021), which reportedly impacted job performance (Johnson et al. 2020). Notably, two studies compared mental well‐being scores of staff during the pandemic with normative population levels and found that MHWs had significantly lower well‐being scores relative to general population well‐being scores before the beginning of the pandemic (Bentham et al. 2021; Langdon et al. 2021). However, when compared to other population groups (i.e. university students, general population and teachers) during the pandemic, no significant differences were found (Langdon et al. 2021). One study reported that those working in outpatient settings typically reported better mental well‐being than MHWs in inpatient settings (Kameg et al. 2021).
Psychological distress
Depression
Ten studies reported subjective increased symptoms of depression amongst MHWs, which mostly remained subclinical, during the pandemic (Anzola et al. 2022; Fish & Mittal 2021; Kameg et al. 2021; Kuki et al. 2021; Minelli et al. 2022; Pappa et al. 2021; Sun et al. 2021), with one study reporting clinically significant levels of symptoms of depression in a quarter of MHWs (Schneider et al. 2021). Levels of depression were reportedly higher in those working in inpatient settings, than outpatient settings (Rapisarda et al. 2020) and those providing face‐to‐face services, particularly those providing services to people who were quarantined (Sun et al. 2021). Another study reported increased depressive symptoms in staff who had been in close contact with COVID‐19 patients (Kuki et al. 2021). On the contrary, one study reported significantly lower depressive symptoms in MHWs than workers of other professions yet, when compared to MHWs in a region with a low incidence of COVID‐19, those in a region with a high incidence of COVID‐19 reported significantly elevated depressive symptoms (Brillon et al. 2021).
Anxiety and fear
Many studies examined symptoms of anxiety amongst MHWs throughout the COVID‐19 pandemic (n = 18), with reports ranging from mild to severe (Abdelfattah 2020; Anzola et al. 2022; Bommersbach et al. 2021; Brillon et al. 2021; Csigo & Ritzl 2021; Fish & Mittal 2021; Garcia et al. 2022; Jokić‐Begić et al. 2020; Kameg et al. 2021; Kuki et al. 2021; Liberati et al. 2021; Limoges et al. 2021; Minelli et al. 2022; Murphy et al. 2021; Pappa et al. 2021; Smith & Gillon 2021; Sun et al. 2021). One study also reported clinically significant anxiety symptoms in 40.8% of their sample (Schneider et al. 2021). Increased levels of anxiety were attributed to changed work demands (Bommersbach et al. 2021), witnessing the patient experience (Limoges et al. 2021), decision‐making and lack of control through telehealth (Liberati et al. 2021; Smith & Gillon 2021), fear of passing the virus onto others (Abdelfattah 2020) and being in close contact with COVID‐19 patients (Kuki et al. 2021). People working in inpatient settings and those working in regions with a high incidence of COVID‐19 exhibited greater levels of anxiety than those working in areas with a low incidence of COVID‐19 (Brillon et al. 2021; Rapisarda et al. 2020). One study also found psychiatrists and psychologists exhibited higher levels of anxiety than nurses and other health professionals (Csigo & Ritzl 2021). However, it was also reported psychiatrists exhibited lower COVID‐19 anxiety than physicians of other specialties (Jokić‐Begić et al. 2020).
Increased worry amongst MHWs was reported by three studies (Bentham et al. 2021; Gao & Tan 2021; Langdon et al. 2021). Worries were related to the risk of COVID‐19 infection (Gao & Tan 2021), impact on level of functioning if infected, and financial impacts of the COVID‐19 pandemic (Bentham et al. 2021), as well as worries about patients (Langdon et al. 2021). One study also reported a sense of panic in MHWs during the rapid transition to telehealth due to the lack of regulations, such as which platforms to use and billing issues (Shklarski et al. 2021).
There were several reports of services lacking adequate supplies of PPE, including high protection masks, safety glasses and disposable gloves (Carpiniello et al. 2020; Johnson et al. 2020; Langdon et al. 2021; Murphy et al. 2021), which often led MHWs being concerned or fearful of COVID‐19 infection, and further passing it onto loved ones (Eddy 2021; Johnson et al. 2020), or patients (Limoges et al. 2021).
Stress
Elevated stress was reported by eight studies (Ashcroft et al. 2021; Bommersbach et al. 2021; Liberati et al. 2021; Limoges et al. 2021; Minelli et al. 2022; Morse & Dell 2021; Ogutlu et al. 2021; Phillips et al. 2021). Reasons for increased stress included uncertainty about the future, fear of COVID‐19 infection (Morse & Dell 2021), lack of communication from management (Bommersbach et al. 2021), greater responsibilities and longer shifts to cover absences, looming threat of redeployment, agitation amongst patients within inpatient units due to increased restrictions (Liberati et al. 2021), witnessing patient experiences (Limoges et al. 2021), childcare issues during lockdowns, caring for loved ones and concerns related to income (Phillips et al. 2021). A further study reported symptoms of peri‐traumatic distress above normal ranges (Miller & Grise‐Owens 2022).
Resilience
Resilience was explored in three of the included studies (Brillon et al. 2021; Jokić‐Begić et al. 2020; Pappa et al. 2021); one reported moderate‐to‐high levels of resilience in MHWs (Pappa et al. 2021), one found no differences in resilience between psychiatrists and general health physicians (Jokić‐Begić et al. 2020) and another reported MHWs were significantly more resilient than workers of other occupations (e.g. managers, clerical workers and sales; Brillon et al. 2021). However, MHWs who worked in a region with high rates of COVID‐19 reported lower levels of resilience and it was suggested that prolonged or extreme stress may inhibit an individual's ability to employ appropriate coping mechanisms (Brillon et al. 2021).
Psychosocial impact
Five studies reported poorer sleep quality in MHWs throughout the COVID‐19 pandemic (Cabeza et al. 2022; Fish & Mittal 2021; Oderinde et al. 2021; Pappa et al. 2021; Rapisarda et al. 2020). One study found symptoms of depression significantly predicted insomnia (Pappa et al. 2021), while another reported experiences of dreams or nightmares related to COVID‐19, particularly regarding fear of infection or infecting others (Cabeza et al. 2022).
Isolation was commonly reported amongst MHWs as a result of the pandemic, most notably due to telehealth and working from home (Ashcroft et al. 2021; Billings et al. 2021; Brillon et al. 2021; Fish & Mittal 2021; Langdon et al. 2021; McBeath et al. 2020; Steidtmann et al. 2021), which resulted in disconnection from colleagues and loss of informal support (Chemerynska et al. 2021; Liberati et al. 2021; Murphy et al. 2021; Nair et al. 2021). Isolation outside of work was also experienced with less ability to engage with social support, or participate in previously enjoyed activities (Billings et al. 2021). Some MHWs reported less desire to interact with others (Eddy 2021). Movement and space restrictions within hospitals also reportedly caused feelings of isolation as staff interactions were restricted to those on their ward, and in some cases, only one nurse being allowed in the break room at a time (Gao & Tan 2021). Increased frequency of migraines in MHWs was also reported (Fish & Mittal 2021).
DISCUSSION
This review investigated the reported impact the COVID‐19 pandemic had on work‐related and personal outcomes in MHWs to date. Findings underscore that MHWs worldwide report being significantly impacted by the pandemic in a variety of work‐related and personal outcomes, as summarized below.
The current review identified substantial evidence of negative work‐related outcomes in MHWs during the pandemic. The pandemic increased the workload for MHWs as the general population experienced more mental health difficulties and patients with existing mental health conditions presented with increased complexity (Chemerynska et al. 2021), which was further exacerbated by frequent staff shortages (Liberati et al. 2021). Most studies suggested the increase in workload, coupled with additional stress and feelings of uncertainty about the future, as well as the continuous changes to infection control measures, were associated with high levels of burnout and exhaustion in MHWs (Kagan et al. 2021; Ogutlu et al. 2021; Pappa et al. 2021). Although MHWs already experienced high levels of burnout prior to the pandemic (Piko 2006; Scanlan & Still 2019), it is thought that the pandemic may have exacerbated these symptoms, similarly to results found in a longitudinal study of ICU health professionals (Kok et al. 2021). However, given the use of various burnout measures and differing contexts in pre‐COVID research, it is difficult to accurately draw conclusions amongst MHWs in the absence of comparative data. Alongside increased workload, many studies reported the disruptive impact of changed roles during the pandemic. MHWs were required to undertake responsibilities that were beyond, or differed from, their standard duties (Adams et al. 2021; Kagan et al. 2021). The constant fluctuation in roles and redeployments was associated with increased burnout (Sklar et al. 2021), which contributed to increased turnover intention, further exacerbating the cycle of increased workload for MHWs (Sklar et al. 2021).
Of concern, it was reported that some MHWs experienced increased workplace violence during the pandemic. Specifically, mandated restrictions (particularly within inpatient units) caused increased agitation and anger amongst some patients, which led to more incidents of verbal or physical abuse towards MHWs (Liberati et al. 2021; Limoges et al. 2021). Generally, workplace violence is associated with reduced job performance and job satisfaction, as well as increased turnover intention (Abo‐Ali et al. 2020; Zhao et al. 2018); during the pandemic exposure to such incidents was associated with a significantly lower overall quality of life, and much higher levels of anxiety (Xie et al. 2021) in MHWs.
The downstream effects of increased demand, altered roles and reports of increased workplace violence during the pandemic included a reported reduction in self‐efficacy, with MHWs reporting reduced confidence in their skills and feeling that they were unable to perform their job as well as usual (Gao & Tan 2021; Johnson et al. 2020). The prevalence of compassion fatigue, empathic distress and vicarious trauma was also high amongst MHWs during the COVID‐19 pandemic (Fish & Mittal 2021; Steidtmann et al. 2021). It was evident throughout the current review that a unique struggle for MHWs included the twofold nature of trauma experience – while attempting to cope with the trauma of the pandemic in their own lives, MHWs reported struggling to help their patients cope with the trauma of COVID‐19 (Billings et al. 2021; Shklarski et al. 2021). Increased stress from the pandemic was suggested to contribute to an inhibition in adaptive coping mechanisms and consequently an increased susceptibility to vicarious trauma (Brillon et al. 2021). This was exacerbated in younger and less experienced MHWs, who experienced higher levels of vicarious trauma (Aafjes‐van Doorn et al. 2020), suggesting that the ability to cope with secondary traumatisation increases with experience.
A pertinent narrative that emerged across multiple studies was the reported supervisory support provided to MHWs throughout the pandemic. The level of support provided by colleagues and managers varied greatly depending on the setting and available resources. MHWs who provided face‐to‐face services and worked on‐site generally reported feeling adequately supported (Billings et al. 2021; Gao & Tan 2021), whereas incidental support that typically occurs within face‐to‐face settings was abruptly removed for those who rapidly transitioned to remote working (Chemerynska et al. 2021; Liberati et al. 2021). The relationship between work changes, burnout and turnover intention reportedly differed depending on the level of support received, an association which has been reported prior to the COVID‐19 pandemic (Scanlan & Still 2019). Given the evidence of enhanced support provision for staff is associated with decreased burnout and turnover intention in MHWs is not limited to times of crisis, strategies should aim to ensure support is available to MHWs in all service delivery settings.
Interestingly, the transition to telehealth service provision was reported to be accompanied with both challenges and benefits amongst MHWs. Telehealth presented MHWs with a range of challenges that were unique to mental health service provision, including difficulties with the interpretation of non‐verbal cues, maintenance of confidentiality (e.g. when patients have family members in the area or MHWs working from home with other family members present) and challenges developing and maintaining therapeutic rapport (Dores et al. 2020; Smith & Gillon 2021). The increased effort required to process and interpret non‐verbal cues such as facial expressions and body language led to increased fatigue amongst MHWs (Bailenson 2021) and difficulties in assessment of patient mental state by MHWs led to reported reductions in confidence in skills (McBeath et al. 2020). Furthermore, MHWs reported increased moral injury evidenced by feelings of guilt and incompetence when delivering therapy remotely, largely due to the widespread perception that online service provision is inferior to face‐to‐face therapy (Chemerynska et al. 2021; Liberati et al. 2021). However, there were some benefits of telehealth that were reported by MHWs. Ensuring patients remained engaged required acquisition of new therapeutic skills, perceived as a positive challenge by some MHWs, and some therapists felt patients were more comfortable, talkative, or engaged through online therapy (Garcia et al. 2022; Guinart et al. 2021; Trabucco et al. 2021). However, these experiences were more evident in MHWs with higher levels of experience, compared to those starting out in their career, emphasizing that additional support may be required for those early in their career.
A pertinent finding of the current review is that the mental well‐being of MHWs differed according to their workplace environment, in that those working in outpatient settings typically reported better well‐being than those working in an inpatient setting (Kameg et al. 2021). There is limited research comparing the general mental well‐being of inpatient and outpatient MHWs pre‐COVID pandemic, and therefore we are unable to conclude that this difference is a result of changes related to the pandemic. However, this difference was suggested to reflect increased use of telehealth by MHWs in outpatient settings and the associated reduction of exposure to patients with COVID‐19 and associated anxiety, as well as outpatient MHWs being more likely to have completed a postgraduate qualification and have more clinical experience and highly developed coping strategies (Kameg et al. 2021).
Although many staff experienced adversities, some studies found that MHWs experienced enhanced levels of job satisfaction due to their ability to continue to provide support to patients and their colleagues, and the sense that the work they were doing made a difference to the lives of others (Billings et al. 2021; Morse & Dell 2021). This is likely a reflection of MHWs' motivation in selecting a career in mental health (Penman et al. 2018) and also that people who consider their work to be a calling (i.e. having a purpose) tend to exhibit greater job satisfaction than those who consider their work ‘just a job’ (Wrzesniewski et al. 1997).
In addition to challenges specifically related to occupation, MHWs also endured many of the same personal stressors as the general population, with many reporting impaired well‐being (Ashcroft et al. 2021; Billings et al. 2021; Chemerynska et al. 2021; Eddy 2021) and increased stress levels as a direct result of the pandemic (Ogutlu et al. 2021; Phillips et al. 2021). The general population was also similarly impacted, however, a meta‐analysis revealed that psychological distress was still greater in healthcare workers (Salari et al. 2020), likely due to the addition of work‐related pressures above and beyond the general stressors of the pandemic. Moreover, MHWs experienced elevated symptoms of depression and anxiety during the COVID‐19 pandemic (Schneider et al. 2021). Similarly to work‐related outcomes, there were differences in anxiety levels between MHWs in inpatient and outpatient settings, whereby inpatient staff exhibited significantly higher levels of anxiety than MHWs in outpatient settings (Rapisarda et al. 2020), which was likely due to the increased risk of exposure to patients with COVID‐19. Further, MHWs were at heightened risk of depressive and anxiety symptoms if they were providing face‐to‐face services, particularly when providing services to people in quarantine who were suspected to have COVID‐19 (Sun et al. 2021), or those who had been in close contact with COVID‐19 patients (Kuki et al. 2021). For those working remotely throughout the pandemic, anxiety was linked to a sense of lack of control, in terms of managing risk‐related situations (Smith & Gillon 2021), with substantial concern surrounding making the wrong decision about an individual's care (Liberati et al. 2021). Similarly to findings amongst healthcare workers, MHWs reported widespread fear associated with contracting COVID‐19, compounded by concern of passing the virus onto family and close friends (Eddy 2021; Johnson et al. 2020), or patients (Limoges et al. 2021; Ness et al. 2021). Concerns of inadequate availability of PPE were reported (Carpiniello et al. 2020; Johnson et al. 2020; Langdon et al. 2021), with some MHWs being afraid to go into their workplace (Murphy et al. 2021; Ness et al. 2021), which likely exacerbated staff shortages.
While fears and psychological distress were exacerbated in MHWs working in an environment with a high incidence of COVID‐19, there was some evidence to suggest these levels were significantly lower overall than those in the general population (Brillon et al. 2021). A potential explanation for this is that MHWs were found to be comparatively more resilient than workers in alternate occupations (Brillon et al. 2021). Past research has indicated that MHWs typically exhibit significantly greater optimism and hope, higher psychological well‐being and are significantly more able to use emotional coping effectively compared to general non‐health industry workers (Koller & Hicks 2016), all of which contribute to higher levels of resilience. However, the resilience of MHWs was found to be lower amongst MHWs working in regions with a high incidence of COVID‐19. This indicates that prolonged or extreme stress may inhibit an individual's ability to remain resilient (Brillon et al. 2021). These findings warrant further exploration of factors that may enhance resilience in MHWs such as workplace support, team cohesion, purpose, and self‐efficacy by being at work and contributing to society through the care they provide.
Much of the general population experienced psychosocial impacts as a result of the pandemic, with MHWs reporting isolation both inside and outside of work. Akin to many, the government mandated social restrictions meant many MHWs felt isolated outside of work due to being less able to engage with social supports, or participate in previously enjoyed hobbies (Billings et al. 2021); some also reported reduced desire to interact with others (Eddy 2021). This is particularly concerning since social support is an important coping mechanism utilized by MHWs to protect their mental well‐being (Dorociak et al. 2017; Muller et al. 2020). Moreover, MHWs working remotely reported feeling disconnected from their colleagues, having lost a source of informal support (Chemerynska et al. 2021; Liberati et al. 2021; Murphy et al. 2021; Nair et al. 2021). Those working on‐site reported feeling isolated as movement throughout the hospital was often restricted, meaning staff interactions were confined to those on their ward or even a single room (Gao & Tan 2021), and even then, with the strict infection control requirements such as social distancing, casual interactions with colleagues were largely reduced. The role of social support within the workplace, particularly in healthcare settings, in minimizing the stress response is well established (Ma et al. 2020), and the restrictions relating to COVID‐19 greatly impacted the availability of this support. Further psychosocial impacts related to fear of contracting COVID‐19 included migraines (Fish & Mittal 2021) and insomnia (Pappa et al. 2021), with reports of COVID‐19 related dreams and nightmares specifically related to fear of infection or infecting others (Cabeza et al. 2022). Sleep quality was also reportedly poorer in MHWs who had been in close contact with COVID‐19 patients (Cabeza et al. 2022), likely due to the associated anxiety and stress of exposure.
Implications for clinical practice and directions for future research
Overall, the findings of this review have important practical implications for how MHWs can be supported in times of crisis. It is recommended that managers seek to minimize changes at work (i.e. redeployment and altering job tasks) to reduce the impact of the downstream effects on burnout. Where changes are unavoidable, clear and timely communication, and support from management is vital to ensure MHWs can continue to thrive. This is particularly relevant to those providing online therapy, who often identified lack of support and training. Past research has found telehealth education to be an effective tool to assist healthcare students in expanding and building their therapeutic skills to suit the online environment (Chike‐Harris et al. 2021), and the implementation of such education within hospital settings should be considered. In addition, given the importance of social support within the workplace in minimizing the stress response (Ma et al. 2020), it is recommended that efforts are put forward to ensure social interactions in the workplace are maintained. This review also identified higher rates of vicarious trauma amongst therapists of younger age and less experience. Therefore, additional supports and practices, such as peer support groups, regular supervision, and self‐care education (Manning‐Jones et al. 2016) may be required for this group. It is also important to consider how MHWs can be supported to maintain resilience, notably in settings with high rates of COVID‐19. A consistent finding throughout the current review was the exacerbated impact on both work and personal outcomes for MHWs in inpatient settings who provided face‐to‐face care for patients. The aforementioned supports and implications are especially relevant for this group of MHWs.
Future research should aim to replicate assessments of the outcomes included in the current review to allow comparison to levels during the peak of the COVID‐19 pandemic. This will allow observation of the long‐term impact of COVID‐19 on work and personal outcomes in MHWs. It is also recommended that future research aim to determine whether the pandemic resulted in significant increases in the outcomes observed in the current review, as well as any differences in outcomes between countries. Further research should also examine the efficacy of telehealth education on reducing adversities such as burnout, stress, and anxiety amongst MHWs, especially for those who have less experience with providing services online. It will be important to observe the long‐lasting impact of the COVID‐19 pandemic on the psychosocial health of MHWs, given the isolation experienced by many MHWs in remote work, and the impact that this had on their overall social functioning. It would also be valuable to investigate specific aspects that could lend support and maintain resilience in MHWs, and in turn examine how this level of resilience can be maintained in times of extreme stress. Research should inform development of preparedness for future pandemics given that the risk of new outbreaks is greatly increased (Medicine 2022).
Limitations
A limitation of the current review is the lack of comparative data for many of the identified outcomes collected prior to the pandemic. Therefore, the review can only interpret the outcomes as static observations during the COVID‐19 pandemic and cannot examine any change to outcomes in detail. A further limitation is the absence of an assessment of risk of bias or quality of included studies; a methodological constraint of rapid reviews (Hamel et al. 2021; Khangura et al. 2012). Moreover, recent review studies examining the quality of research during the COVID‐19 pandemic revealed that the methodological quality of these studies was lower across all study designs than pre‐COVID‐19 research and with shorter publication times (Jung et al. 2021; Nieto et al. 2020; Raynaud et al. 2021); therefore, results of this review should be taken with caution. Restriction to English language might have limited reports from some particular jurisdictions.
CONCLUSION
This review has synthesized the current evidence of the impact of COVID‐19 on work and personal outcomes in MHWs to date. We found overall, that many MHWs of varying professions and in a range of settings were significantly impacted by the pandemic by increased workload, constant changes in roles and reported increased vicarious trauma and workplace violence. Further impacts included elevated symptoms of burnout, psychological distress and psychosocial challenges. The review also identified challenges for both those working in inpatient settings, and those working remotely, with younger and less experienced MHWs being particularly vulnerable. The social impact of the pandemic was a key theme throughout the review, resulting in MHWs feeling isolated at work and sometimes having less desire to interact with others outside of work. It is unknown whether this will continue postpandemic but is a pertinent finding due to the importance of social interactions for mental well‐being. With the COVID‐19 pandemic still ongoing and associated challenges continuing to evolve and shape mental healthcare provision, it is important to maintain efforts to support a strong and resilient mental health workforce.
Supporting information
Appendix S1 Search strategies.
ACKNOWLEDGEMENTS
The author(s) disclose receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Victorian Department of Health, Australia.
Zoe M.Jenkins, David J. Castle joint senior authors.
Authorship statement: Authors K.C, I.G. and Z.J. designed the study and wrote the protocol. K.C. and I.G. conducted the literature search and screened all papers. K.C. conducted data extraction and analysis. K.C. wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Declaration of conflict of interest: The author(s) report no conflicts of interest in relation to this work.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Aafjes‐van Doorn, K. , Bekes, V. , Prout, T. A. & Hoffman, L. (2020). Psychotherapists' vicarious traumatization during the COVID‐19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12 (S1), S148–S150. 10.1037/tra0000868 [DOI] [PubMed] [Google Scholar]
- Abdelfattah, D. (2020). Stressors occurring in psychiatry residents working in psychiatric hospitals during the COVID‐19 pandemic. The Primary Care Companion for CNS Disorders, 22 (6), 20br02735. 10.4088/PCC.20br02735 [DOI] [PubMed] [Google Scholar]
- Abo‐Ali, E. A. , Zayed, H. A. & Atlam, S. A. (2020). Workplace violence: Effects on job performance and coping strategies among physicians. Journal of High Institute of Public Health, 50 (3), 126–131. 10.21608/JHIPH.2020.120605 [DOI] [Google Scholar]
- Acker, G. M. (2012). Burnout among mental health care providers. Journal of Social Work, 12 (5), 475–490. 10.1177/1468017310392418 [DOI] [Google Scholar]
- Adams, W. E. , Rogers, E. S. , Edwards, J. P. , Lord, E. M. , McKnight, L. & Barbone, M. (2021). Impact of COVID‐19 on peer support specialists in the United States: Findings from a cross‐sectional online survey. Psychiatric Services, 73 (1), 9–17. 10.1176/appi.ps.202000915 [DOI] [PubMed] [Google Scholar]
- Anzola, D. , Limoges, J. , McLean, J. & Kolla, N. J. (2022). Effects of the COVID‐19 pandemic on the mental health of healthcare providers: A comparison of a psychiatric hospital and a general hospital. Frontiers in Psychiatry, 12:720693. 10.3389/fpsyt.2021.720693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashcroft, R. , Donnelly, C. , Dancey, M. et al. (2021). Primary care teams' experiences of delivering mental health care during the COVID‐19 pandemic: A qualitative study. BMC Family Practice, 22 (1), 143. 10.1186/s12875-021-01496-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Psychological Society . (2021). Balancing caseloads and surging demand: Your experience and what we are doing. InPsych, 43 (4). [Cited 22 June 2022]. Available from: URL: https://psychology.org.au/for‐members/publications/inpsych/2021/november‐issue‐4/balancing‐caseloads‐and‐surging‐demand [Google Scholar]
- Bae, H. , Kim, J. , Lee, S. H. et al. (2022). Difficulties of healthcare workers encountered under cohort isolation in a psychiatric hospital during the COVID‐19 pandemic: A qualitative study. Psychiatry Research, 313, 114615. 10.1016/j.psychres.2022.114615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailenson, J. N. (2021). Nonverbal overload: A theoretical argument for the causes of Zoom fatigue. Technology, Mind, and Behavior, 2 (1), 1‐6. 10.1037/tmb0000030 [DOI] [Google Scholar]
- Barello, S. , Falcó‐Pegueroles, A. , Rosa, D. , Tolotti, A. , Graffigna, G. & Bonetti, L. (2020). The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID‐19 emergency: A rapid review. International Journal of Public Health, 65 (7), 1205–1216. 10.1007/s00038-020-01463-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekes, V. , Aafjes‐van Doorn, K. , Prout, T. A. & Hoffman, L. (2020). Stretching the analytic frame: Analytic therapists' experiences with remote therapy during COVID‐19. Journal of the American Psychoanalytic Association, 68 (3), 437–446. 10.1177/0003065120939298 [DOI] [PubMed] [Google Scholar]
- Bentham, C. , Driver, K. & Stark, D. (2021). Well‐being of CAMHS staff and changes in working practices during the COVID‐19 pandemic. Journal of Child and Adolescent Psychiatric Nursing, 34 (3), 225–235. 10.1111/jcap.12311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhome, R. , Huntley, J. , Dalton‐Locke, C. , San Juan, N. V. , Oram, S. , Foye, U. , & Livingston, G. (2021). Impact of the COVID-19 pandemic on older adults mental health services: A mixed methods study. International Journal of Geriatric Psychiatry, 36(11), 1748–1758. Portico. 10.1002/gps.5596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings, J. , Biggs, C. , Ching, B. C. F. et al. (2021). Experiences of mental health professionals supporting front‐line health and social care workers during COVID‐19: Qualitative study. BJPsych Open, 7 (2), e70. 10.1192/bjo.2021.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bommersbach, T. , Dube, L. & Li, L. (2021). Mental health staff perceptions of improvement opportunities around COVID‐19: A mixed‐methods analysis. The Psychiatric Quarterly, 92 (3), 1079–1092. 10.1007/s11126-021-09890-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brillon, P. , Philippe, F. L. , Paradis, A. , Geoffroy, M. C. , Orri, M. & Ouellet‐Morin, I. (2021). Psychological distress of mental health workers during the COVID‐19 pandemic: A comparison with the general population in high‐ and low‐incidence regions. Journal of Clinical Psychology, 78 (4), 602–621. 10.1002/jclp.23238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabeza, G. , Caballero, H. , Castiblanco, F. , Cabrera, D. , Martinez, F. & Lara, G. (2022). Impact of the COVID‐19 pandemic on the quality of sleep of mental health workers in Colombia. Dreaming, 32 (2), 124–134. 10.1037/drm0000210 [DOI] [Google Scholar]
- Carpiniello, B. , Tusconi, M. , Zanalda, E. , Di Sciascio, G. & Di Giannantonio, M. (2020). Psychiatry during the Covid‐19 pandemic: A survey on mental health departments in Italy. BMC Psychiatry, 20 (1), 1–12. 10.1186/s12888-020-02997-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemerynska, N. , Marczak, M. & Kucharska, J. (2021). What are the experiences of clinical psychologists working with people with intellectual disabilities during the COVID‐19 pandemic? Journal of Applied Research in Intellectual Disabilities, 35 (2), 587–595. 10.1111/jar.12971 [DOI] [PubMed] [Google Scholar]
- Chike‐Harris, K. E. , Durham, C. , Logan, A. , Smith, G. & DuBose‐Morris, R. (2021). Integration of telehealth education into the health care provider curriculum: A review. Telemedicine and e‐Health, 27 (2), 137–149. 10.1089/tmj.2019.0261 [DOI] [PubMed] [Google Scholar]
- Covidence Systematic Review Software . (2022). Veritas Health Innovation. Melbourne, Australia: Covidence Systematic Review Software. Available from: URL:. www.covidence.org [Google Scholar]
- Crawshaw, J. , Konnyu, K. , Castillo, G. , van Allen, Z. , Grimshaw, J. & Presseau, J. (2022). Behavioural determinants of COVID‐19 vaccination acceptance among healthcare workers: A rapid review. Public Health, 210, 123–133. 10.1016/j.puhe.2022.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csigo, K. & Ritzl, A. (2021). First reactions and attitudes of psychiatric workers in Budapest psychiatric care units regarding the COVID‐19 pandemic. The Primary Care Companion for CNS Disorders, 23 (3), 32716. 10.4088/PCC.20m02850 [DOI] [PubMed] [Google Scholar]
- Dittborn, M. , Micolich, C. , Rojas, D. & Salas, S. P. (2022). Ethical challenges experienced by healthcare workers delivering clinical care during health emergencies and disasters: A rapid review of qualitative studies and thematic synthesis. AJOB Empirical Bioethics, 1‐17, 123–133. 10.1016/j.puhe.2022.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dores, A. R. , Geraldo, A. , Carvalho, I. P. & Barbosa, F. (2020). The use of new digital information and communication technologies in psychological counseling during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 17 (20), 7663. 10.3390/ijerph17207663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorociak, K. E. , Rupert, P. A. & Zahniser, E. (2017). Work life, well‐being, and self‐care across the professional lifespan of psychologists. Professional Psychology: Research and Practice, 48 (6), 429–437. 10.1037/pro0000160 [DOI] [Google Scholar]
- Eddy, C. M. (2021). The social impact of COVID‐19 as perceived by the employees of a UK mental health service. International Journal of Mental Health Nursing, 30, 1366–1375. 10.1111/inm.12883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasshauer, J. M. , Bollmann, A. , Hohenstein, S. et al. (2021). Impact of COVID‐19 pandemic on involuntary and urgent inpatient admissions for psychiatric disorders in a German‐wide hospital network. Journal of Psychiatric Research, 142, 140–143. 10.1016/j.jpsychires.2021.07.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish, J. N. & Mittal, M. (2021). Mental health providers during COVID‐19: Essential to the US public health workforce and in need of support. Public Health Reports, 136 (1), 14–17. 10.1177/0033354920965266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, Z. & Tan, F. P. L. (2021). Nurses' experiences in response to COVID‐19 in a psychiatric ward in Singapore. International Nursing Review, 68 (2), 196–201. 10.1111/inr.12680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, K. M. , Nanavaty, N. , Nouzovsky, A. , Primm, K. M. , McCord, C. E. & Garney, W. R. (2022). Rapid transition to telepsychology: Health service psychology trainee responses amidst a global Covid‐19 crisis from an ecological perspective. Training and Education in Professional Psychology, 16 (1), 87–94. 10.1037/tep0000369 [DOI] [Google Scholar]
- Gomez‐Ramiro, M. , Fico, G. , Anmella, G. et al. (2021). Changing trends in psychiatric emergency service admissions during the COVID‐19 outbreak: Report from a worldwide epicentre. Journal of Affective Disorders, 282, 26–32. 10.1016/j.jad.2020.12.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guinart, D. , Marcy, P. , Hauser, M. , Dwyer, M. & Kane, J. M. (2021). Mental health care providers' attitudes toward telepsychiatry: A systemwide, multisite survey during the COVID‐19 pandemic. Psychiatric Services, 72 (6), 704–707. 10.1176/appi.ps.202000441 [DOI] [PubMed] [Google Scholar]
- Hamel, C. , Michaud, A. , Thuku, M. et al. (2021). Defining rapid reviews: A systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. Journal of Clinical Epidemiology, 129, 74–85. 10.1016/j.jclinepi.2020.09.041 [DOI] [PubMed] [Google Scholar]
- Hussein, S. (2022). Employment inequalities among British minority ethnic workers in health and social care at the time of COVID‐19: A rapid review of the literature. Social Policy and Society, 21 (2), 316–330. 10.1017/S1474746421000841 [DOI] [Google Scholar]
- Isautier, J. M. J. , Copp, T. , Ayre, J. et al. (2020). People's experiences and satisfaction with telehealth during the COVID‐19 pandemic in Australia: Cross‐sectional survey study. Journal of Medical Internet Research, 22 (12), e24531. 10.2196/24531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, D. (2020). Adolescent patient engagement through telepsychiatry: A case report application. Journal of Psychosocial Nursing and Mental Health Services, 58 (11), 9–12. 10.3928/02793695-20201013-02 [DOI] [PubMed] [Google Scholar]
- Johnson, S. , Dalton‐Locke, C. , Vera San Juan, N. et al. (2020). Impact on mental health care and on mental health service users of the COVID‐19 pandemic: A mixed methods survey of UK mental health care staff. Social Psychiatry and Psychiatric Epidemiology, 56 (1), 25–37. 10.1007/s00127-020-01927-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokić‐Begić, N. , Lauri Korajlija, A. & Begić, D. (2020). Mental health of psychiatrists and physicians of other specialties in early COVID‐19 pandemic: Risk and protective factors. Psychiatria Danubina, 32 (3–4), 536–548. 10.24869/psyd.2020.536 [DOI] [PubMed] [Google Scholar]
- Jung, R. G. , Di Santo, P. , Clifford, C. et al. (2021). Methodological quality of COVID‐19 clinical research. Nature Communications, 12 (1), 1–10. 10.1038/s41467-021-21220-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagan, I. , Shor, R. , Ben Aharon, I. et al. (2021). A mixed‐methods study of nurse managers' managerial and clinical challenges in mental health centers during the COVID‐19 pandemic. Journal of Nursing Scholarship, 53 (6), 663–670. 10.1111/jnu.12685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kameg, B. N. , Fradkin, D. , Lee, H. & Mitchell, A. (2021). Mental wellness among psychiatric‐mental health nurses during the COVID‐19 pandemic. Archives of Psychiatric Nursing, 35 (4), 401–406. 10.1016/j.apnu.2021.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khangura, S. , Konnyu, K. , Cushman, R. , Grimshaw, J. & Moher, D. (2012). Evidence summaries: The evolution of a rapid review approach. Systematic Reviews, 1 (1), 1–9. 10.1186/2046-4053-1-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok, N. , van Gurp, J. , Teerenstra, S. et al. (2021). Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: A longitudinal cohort study. Critical Care Medicine, 49 (3), 419–427. 10.1097/CCM.0000000000004865 [DOI] [PubMed] [Google Scholar]
- Koller, S. L. & Hicks, R. E. (2016). Psychological capital qualities and psychological well‐being in Australian mental health professionals. International Journal of Psychological Studies, 8 (2), 41–53. 10.5539/ijps.v8n2p41 [DOI] [Google Scholar]
- Kuki, K. , Yamaguchi, Y. , Makinodan, M. et al. (2021). Effects of contact with COVID‐19 patients on the mental health of workers in a psychiatric hospital. Psychiatry and Clinical Neurosciences, 75 (2), 67–69. 10.1111/pcn.13179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langdon, P. E. , Marczak, M. , Clifford, C. & Willner, P. (2021). Occupational stress, coping and well‐being among registered psychologists working with people with intellectual disabilities during the covid‐19 pandemic in the United Kingdom. Journal of Intellectual and Developmental Disability, 1‐11, 195–205. 10.3109/13668250.2021.1967588 [DOI] [Google Scholar]
- Liberati, E. , Richards, N. , Willars, J. et al. (2021). A qualitative study of experiences of NHS mental healthcare workers during the Covid‐19 pandemic. BMC Psychiatry, 21 (1), 1–12. 10.1186/s12888-021-03261-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limoges, J. , Anzola, J. D. & Kolla, N. J. (2021). Effects of COVID‐19 on healthcare providers: Opportunities for education and support (ECHOES). Nursing Leadership, 34 (2), 62–74. 10.12927/cjnl.2021.26528 [DOI] [PubMed] [Google Scholar]
- Lin, T. , Stone, S. J. , Heckman, T. G. & Anderson, T. (2021). Zoom‐in to zone‐out: Therapists report less therapeutic skill in telepsychology versus face‐to‐face therapy during the COVID‐19 pandemic. Psychotherapy, 58 (4), 449–459. 10.1037/pst0000398 [DOI] [PubMed] [Google Scholar]
- Ma, H. , Qiao, H. , Qu, H. et al. (2020). Role stress, social support and occupational burnout among physicians in China: A path analysis approach. International Health, 12 (3), 157–163. 10.1093/inthealth/ihz054 [DOI] [PubMed] [Google Scholar]
- Magill, E. , Siegel, Z. & Pike, K. M. (2020). The mental health of frontline health care providers during pandemics: A rapid review of the literature. Psychiatric Services, 71 (12), 1260–1269. 10.1176/appi.ps.202000274 [DOI] [PubMed] [Google Scholar]
- Manning‐Jones, S. , de Terte, I. & Stephens, C. (2016). Secondary traumatic stress, vicarious posttraumatic growth, and coping among health professionals; A comparison study. New Zealand Journal of Psychology, 45 (1), 20. [Google Scholar]
- McBeath, A. G. , du Plock, S. & Bager‐Charleson, S. (2020). The challenges and experiences of psychotherapists working remotely during the coronavirus pandemic. Counselling and Psychotherapy Research, 20 (3), 394–405. 10.1002/capr.12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicine, T. L. R. (2022). Future pandemics: Failing to prepare means preparing to fail. The Lancet. Respiratory Medicine, 10 (3), 221–222. 10.1016/S2213-2600(22)00056-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, J. J. , & Grise‐Owens, E. (2022). The impact of COVID‐19 on social workers: An assessment of peritraumatic distress. Journal of Social Work, 22(3), 674–691. 10.1177/14680173211013243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minelli, A. , Silva, R. C. , Barlati, S. et al. (2022). The elephant in the room: A cross‐sectional study on the stressful psychological effects of the COVID‐19 pandemic in mental healthcare workers. Brain Sciences, 12 (3), 408. 10.3390/brainsci12030408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse, G. A. & Dell, N. A. (2021). The well‐being and perspectives of community‐based behavioral health staff during the COVID‐19 pandemic. Social Work in Health Care, 60 (2), 117–130. 10.1080/00981389.2021.1904315 [DOI] [PubMed] [Google Scholar]
- Mulatu, H. A. , Tesfaye, M. , Woldeyes, E. , Bayisa, T. , Fisseha, H. & Kassu, R. A. (2021). The prevalence of common mental disorders among healthcare professionals during the COVID‐19 pandemic at a tertiary hospital in Addis Ababa, Ethiopia. Journal of Affective Disorders Reports, 6, 100246. 10.1016/j.jadr.2021.100246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller, A. E. , Hafstad, E. V. , Himmels, J. P. W. et al. (2020). The mental health impact of the covid‐19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research, 293, 113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, A. A. , Karyczak, S. , Dolce, J. N. et al. (2021). Challenges experienced by behavioral health organizations in New York resulting from COVID‐19: A qualitative analysis. Community Mental Health Journal, 57 (1), 111–120. 10.1007/s10597-020-00731-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, S. , Kannan, P. , Mehta, K. , Raju, A. , Mathew, J. & Ramachandran, P. (2021). The COVID‐19 pandemic and its impact on mental health services: The provider perspective. Journal of Public Health, 43 (Supplement_2), ii51–ii56. 10.1093/pubmed/fdab163 [DOI] [PubMed] [Google Scholar]
- Ness, M. M. , Saylor, J. , Di Fusco, L. A. & Evans, K. (2021). Healthcare providers' challenges during the coronavirus disease (COVID‐19) pandemic: A qualitative approach. Nursing & Health Sciences, 23 (2), 389–397. 10.1111/nhs.12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieto, I. , Navas, J. F. & Vázquez, C. (2020). The quality of research on mental health related to the COVID‐19 pandemic: A note of caution after a systematic review. Brain, Behavior, & Immunity‐Health, 7, 100123. 10.1016/j.bbih.2020.100123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oderinde, K. O. , Akanni, O. O. & Olashore, A. (2021). Knowledge of the coronavirus disease 2019 (COVID‐19) and sleep problems among a selected sample of psychiatric hospital staff in Nigeria: A cross‐sectional study. The Pan African Medical Journal, 40 (101517926), 39. 10.11604/pamj.2021.40.39.25357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogutlu, H. , McNicholas, F. & Turkcapar, H. (2021). Stress and burnout in psychiatrists in Turkey during COVID‐19 pandemic. Psychiatria Danubina, 33 (2), 225–230. 10.24869/psyd.2021.225 [DOI] [PubMed] [Google Scholar]
- Olfson, M. (2016). Building the mental health workforce capacity needed to treat adults with serious mental illnesses. Health Affairs, 35 (6), 983–990. 10.1377/hlthaff.2015.1619 [DOI] [PubMed] [Google Scholar]
- Olwill, C. , Mc Nally, D. & Douglas, L. (2021). Psychiatrist experience of remote consultations by telephone in an outpatient psychiatric department during the COVID‐19 pandemic. Irish Journal of Psychological Medicine, 38 (2), 132–139. 10.1017/ipm.2020.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10 (1), 1–11. 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa, S. , Barnett, J. , Berges, I. & Sakkas, N. (2021). Tired, worried and burned out, but still resilient: A cross‐sectional study of mental health workers in the UK during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 18 (9), 4457. 10.3390/ijerph18094457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penman, J. , Martinez, L. , Papoulis, D. & Cronin, K. (2018). Voices from the field: Regional nurses speak about motivations, careers and how to entice others to pursue mental health nursing. International Journal of Nursing Education Scholarship, 15 (1), 20170056. 10.1515/ijnes-2017-0056 [DOI] [PubMed] [Google Scholar]
- Phillips, L. A. , Thompson, T. J. , Edelman, S. A. & Ruiz, T. U. (2021). Independent mental health providers' experience in initial months of the COVID‐19 pandemic. Practice Innovations, 6 (4), 209–220. 10.1037/pri0000153 [DOI] [Google Scholar]
- Piko, B. F. (2006). Burnout, role conflict, job satisfaction and psychosocial health among Hungarian health care staff: A questionnaire survey. International Journal of Nursing Studies, 43 (3), 311–318. 10.1016/j.ijnurstu.2005.05.003 [DOI] [PubMed] [Google Scholar]
- Rahman, M. A. , Hoque, N. , Alif, S. M. et al. (2020). Factors associated with psychological distress, fear and coping strategies during the COVID‐19 pandemic in Australia. Globalization and Health, 16 (1), 95. 10.1186/s12992-020-00624-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapisarda, F. , Vallarino, M. , Cavallini, E. et al. (2020). The early impact of the Covid‐19 emergency on mental health workers: A survey in Lombardy, Italy. International Journal of Environmental Research and Public Health, 17 (22), 8615. 10.3390/ijerph17228615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raynaud, M. , Zhang, H. , Louis, K. et al. (2021). COVID‐19‐related medical research: A meta‐research and critical appraisal. BMC Medical Research Methodology, 21 (1), 1–11. 10.1186/s12874-020-01190-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanchych, E. , Desai, R. , Bartha, C. , Carson, N. , Korenblum, M. & Monga, S. (2022). Healthcare providers' perceptions of virtual‐care with children's mental health in a pandemic: A hospital and community perspective. Early Intervention in Psychiatry, 16 (4), 433–443. 10.1111/eip.13196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck, R. , Johnson, B. , Deegan, D. & Stefanovics, E. (2021). Impact of COVID‐19‐related social distancing on delivery of intensive case management. The Journal of Nervous and Mental Disease, 209 (8), 543–546. 10.1097/NMD.0000000000001358 [DOI] [PubMed] [Google Scholar]
- Salari, N. , Hosseinian‐Far, A. , Jalali, R. et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: A systematic review and meta‐analysis. Globalization and Health, 16 (1), 1–11. 10.1016/j.psychres.2020.113382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sammons, M. T. (2022). Unmet mental health needs associated with Covid must be addressed. Journal of Health Service Psychology, 48 (1), 1–2. 10.1007/s42843-022-00057-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlan, J. N. & Still, M. (2019). Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Services Research, 19 (1), 62. 10.1186/s12913-018-3841-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, M. B. , Greif, T. R. , Galsky, A. P. et al. (2021). Giving psychology trainees a voice during the COVID‐19 pandemic: Trainee mental health, perceived safety, and support. Training and Education in Professional Psychology, 15 (1), 76–85. 10.1037/tep0000343 [DOI] [Google Scholar]
- Shklarski, L. , Abrams, A. & Bakst, E. (2021). Navigating changes in the physical and psychological spaces of psychotherapists during Covid‐19: When home becomes the office. Practice Innovations, 6 (1), 55–66. 10.1037/pri0000138 [DOI] [Google Scholar]
- Sklar, M. , Ehrhart, M. G. & Aarons, G. A. (2021). COVID‐related work changes, burnout, and turnover intentions in mental health providers: A moderated mediation analysis. Psychiatric Rehabilitation Journal, 44 (3), 219–228. 10.1037/prj0000480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slone, H. , Gutierrez, A. , Lutzky, C. et al. (2021). Assessing the impact of COVID‐19 on mental health providers in the southeastern United States. Psychiatry Research, 302, 114055. 10.1016/j.psychres.2021.114055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, J. & Gillon, E. (2021). Therapists' experiences of providing online counselling: A qualitative study. Counselling & Psychotherapy Research, 21 (3), 545–554. 10.1002/capr.12408 [DOI] [Google Scholar]
- Steidtmann, D. , McBride, S. & Mishkind, M. C. (2021). Experiences of mental health clinicians and staff in rapidly converting to full‐time telemental health and work from home during the COVID‐19 pandemic. Telemedicine and e‐Health, 27 (7), 785–791. 10.1089/tmj.2020.0305 [DOI] [PubMed] [Google Scholar]
- Summers‐Gabr, N. M. (2020). Rural–urban mental health disparities in the United States during COVID‐19. Psychological Trauma: Theory, Research, Practice, and Policy, 12 (S1), S222–S224. 10.1037/tra0000871 [DOI] [PubMed] [Google Scholar]
- Sun, Y. , Song, H. , Liu, H. , Mao, F. , Sun, X. & Cao, F. (2021). Occupational stress, mental health, and self‐efficacy among community mental health workers: A cross‐sectional study during COVID‐19 pandemic. International Journal of Social Psychiatry, 67 (6), 737–746. 10.1177/0020764020972131 [DOI] [PubMed] [Google Scholar]
- Tabari, P. , Amini, M. , Moghadami, M. & Moosavi, M. (2020). International public health responses to COVID‐19 outbreak: A rapid review. Iranian Journal of Medical Sciences, 45 (3), 157–169. 10.30476/ijms.2020.85810.1537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trabucco, A. , Aguglia, A. , Amerio, A. et al. (2021). COVID‐19 pandemic impact on the therapeutic setting in mental health services. Acta Bio Medica, 92 (Suppl 6), e2021448. 10.23750/abm.v92iS6.12227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Substantial investment needed to avert mental heatlh crisis. The World Health Organization. [Cited 25 October 2021]. Available from: URL: https://www.who.int/news/item/14‐05‐2020‐substantial‐investment‐needed‐to‐avert‐mental‐health‐crisis
- World Health Organization . (2022). COVID‐19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide . [Cited 6 June 2022]. Available from: URL: https://www.who.int/news/item/02‐03‐2022‐covid‐19‐pandemic‐triggers‐25‐increase‐in‐prevalence‐of‐anxiety‐and‐depression‐worldwide
- Wrzesniewski, A. , McCauley, C. , Rozin, P. & Schwartz, B. (1997). Jobs, careers, and callings: People's relations to their work. Journal of Research in Personality, 31 (1), 21–33. 10.1006/jrpe.1997.2162 [DOI] [Google Scholar]
- Xie, X.‐M. , Zhao, Y.‐J. , An, F.‐R. et al. (2021). Workplace violence and its association with quality of life among mental health professionals in China during the COVID‐19 pandemic. Journal of Psychiatric Research, 135, 289–293. 10.1016/j.jpsychires.2021.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W. , Wang, K. , Yin, L. et al. (2020). Mental health and psychosocial problems of medical health workers during the COVID‐19 epidemic in China. Psychotherapy and Psychosomatics, 89 (4), 242–250. 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, S. H. , Shi, Y. , Sun, Z. N. et al. (2018). Impact of workplace violence against nurses' thriving at work, job satisfaction and turnover intention: A cross‐sectional study. Journal of Clinical Nursing, 27 (13–14), 2620–2632. 10.1111/jocn.14311 [DOI] [PubMed] [Google Scholar]
- Zhu, H. , Xie, S. , Liu, X. , Yang, X. & Zhou, J. (2022). Influencing factors of burnout and its dimensions among mental health workers during the COVID‐19 pandemic. Nursing Open, 9 (4), 2013–2023. 10.1002/nop2.1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search strategies.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


