Abstract
Background:
There is little information on the clinical presentation, functional impact, and psychiatric characteristics of misophonia in youth, an increasingly recognized syndrome characterized by high emotional reactivity to certain sounds and associated visual stimuli.
Method:
One-hundred-two youth (8–17 years-old) with misophonia and their parents were recruited and compared with 94 youth with anxiety disorders. Participants completed validated assessments of misophonia severity, quality of life, as well as psychiatric symptoms and diagnoses.
Results:
The most common misophonia triggers included eating (96%), breathing (84%), throat sounds (66%), and tapping (54%). Annoyance/irritation, verbal aggression, avoidance behavior, and family impact were nearly universal. Misophonia severity was associated with internalizing symptoms, externalizing behaviors (child-report), and poorer quality of life. High rates of comorbidity with internalizing and neurodevelopmental disorders were found. Quality of life and externalizing behaviors were not significantly different between misophonia and anxiety samples; internalizing symptoms and autism characteristics were significantly higher among youth with anxiety disorders.
Limitations:
This self-selected sample showed limited multicultural diversity.
Conclusions:
This study presents misophonia as a highly impairing psychiatric syndrome. Future interdisciplinary work should clarify the mechanisms of misophonia, establish evidence-based treatments, and extend these findings to randomly sampled and more culturally diverse populations.
Keywords: Sensory sensitivity, Children, Adolescents, Phenomenology, Treatment, Comorbidity, Assessment
Introduction
Misophonia is characterized by strong, unpleasant emotional reactions to certain sounds and associated visual stimuli (Lewin et al., 2021; Potgieter et al., 2019; Rosenthal et al., 2021; Swedo et al., 2022). Although not a formal diagnosis in the DSM-5 or ICD-11, misophonia has been increasingly studied and recognized in clinical practice since it was first described in the early 2000’s by audiologists treating individuals with decreased sound tolerance (Jastreboff and Jastreboff, 2000; Potgieter et al., 2019; Swedo et al., 2022). Misophonia symptoms can arise at any age, though most retrospective studies of adults with misophonia suggest onset during childhood or adolescence.(Claiborn et al., 2020; Jager et al., 2020; Potgieter et al., 2019). Unfortunately, there is an extreme paucity of research on individuals with misophonia across the lifespan, but especially among youth. Without systematic data on the clinical presentation of misophonia in children and adolescents, researchers and clinicians will be unable to develop an understanding of this condition and its treatment.
Adults with misophonia experience disturbing and often intense emotional reactions to sound triggers including annoyance, disgust, anger, hatred, panic, and aggression (Claiborn et al., 2020; Jager et al., 2020; Potgieter et al., 2019; Rouw and Erfanian, 2018). Physical reactions may include muscle tension, heavy breathing, as well as physical or verbal outbursts (Claiborn et al., 2020; Jager et al., 2020; Potgieter et al., 2019; Rouw and Erfanian, 2018). In several studies examining adult samples comprised mostly of females with moderate to severe misophonia symptoms (Claiborn et al., 2020; Jager et al., 2020; Rouw and Erfanian, 2018; Wu et al., 2016), the most common sound triggers were oral or eating sounds in addition to nasal or breathing sounds, and repetitive tapping sounds (e.g., with hands, keyboards, or pens) (Claiborn et al., 2020; Jager et al., 2020; Rouw and Erfanian, 2018; Wu et al., 2016). Almost all affected individuals report severe irritation or anger with triggers and hyper-focus on sounds, with less common emotional responses including disgust and panic (Jager et al., 2020). Many others experience feelings of powerlessness and loss of control (Jager et al., 2020).
Four studies have investigated comorbid psychiatric diagnoses; in one clinic-based study, 28% of 575 adults with misophonia experienced a comorbid psychiatric diagnosis, most commonly mood (10%) and anxiety disorders (9%), as well as higher-than-expected rates of ADHD (5%) (Jager et al., 2020). Erfanian et al. (2019) found that among 52 adults with misophonia, 40% experienced a psychiatric disorder, most commonly posttraumatic stress disorder (15%), OCD (11%), and anorexia (10%). In another study, individuals with misophonia had significantly higher rates of psychiatric comorbidity than adults with general non-misophonic auditory over-responsivity and healthy adults, with 71% of those with misophonia experiencing a comorbid psychiatric disorder, most commonly panic disorder (19%), generalized anxiety disorder (15%), social anxiety disorder (13%), and major depressive disorder (12%) (Siepsiak et al., 2022). Finally, a study with 207 adults with misophonia, the most common comorbidities were anxiety disorders (57%), major depressive disorder (50% lifetime; 7% current), attention-deficit/hyperactivity disorder (15%), and posttraumatic stress disorder (16%) (Rosenthal et al., 2022).The most common psychiatric symptoms in adults with misophonia include mood, anxiety, and obsessive-compulsive disorder (OCD) symptoms or obsessive-compulsive personality disorder traits (Claiborn et al., 2020; Jager et al., 2020).
Case series data among children with misophonia suggest a similar pattern, though these studies are limited by very small samples (Dover and McGuire, 2021; McGuire et al., 2015; Muller et al., 2018; Reid et al., 2016; Sarigedik and Yurteri, 2021). Rinaldi et al (2022a) identified 15 children with elevated misophonia symptoms through population screening rather than self-identification or presentation for treatment. In this sample, 9 participants were female with a mean age of 11.7 years and 6 participants were male with a mean age of 11 years (Rinaldi et al., 2022a). These children showed poorer health-related quality-of-life than peers and higher traits associated with anxiety and OCD (Rinaldi et al., 2022a) as well as autistic traits across several social-cognitive domains, including attention-switching, communication, social skills, attention to detail, and imagination (Rinaldi et al., 2022b).
To address the absence of data describing misophonia in youth, this study evaluated clinical data from a sample of 102 children and adolescents meeting the proposed diagnostic criteria for misophonia (Swedo et al., 2022). First, the study aimed to describe the clinical phenomenology of youth with misophonia, including age, gender distribution, types and frequency of misophonia triggers, misophonia-related emotions, frequency of aggression responses, avoidance behaviors, and areas and degree of impairment. It was expected that anger and irritability would be the most common emotional experiences, eating and breathing sounds the most common trigger sounds, and that the majority of the sample would be female. Second, the study evaluated associations between misophonia severity and psychiatric symptoms as well as quality of life. It was expected that this sample of children and adolescents with misophonia would have high rates of comorbid mood, anxiety, and obsessive-compulsive disorders as well as elevated autism spectrum symptoms based on strong associations between misophonia and psychiatric symptoms in existing reports on misophonia in children and adolescents as well as those in adults (Cusack et al., 2018; Erfanian et al., 2019; Jager et al., 2020; Rinaldi et al., 2022a; Rinaldi et al., 2022b). Exploratory analyses investigated whether youth with misophonia differed significantly in these factors compared to youth with anxiety disorders.
Methods
Procedures
Youth with suspected misophonia were recruited via online advertisements, misophonia/anxiety-focused social media pages, as well as clinical and professional networks. Youth with suspected anxiety disorders were also recruited to serve as a non-misophonia clinical comparison group, as these disorders are also characterized by heightened emotional reactivity to specific stimuli. The majority of participants were recruited via online advertisements.
Participants and their parents assented/consented to participate in the study during an initial video call. Inclusion criteria for both samples were: 1) being 8–17 years, 2) parent willingness to participate, 3) English fluency. For the misophonia group, an additional criterion was: clinically significant misophonia symptoms based on a score of at least 10 on the A-MISO-S, indicating at least moderate misophonia (Schröder et al., 2013). For the anxiety group, additional inclusion criteria were: 1) a Parent-report Multidimensional Anxiety Scale for Children (MASC) T-Score of at least 60, 2) an anxiety disorder diagnosis on the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID), and 3) a score of ≤4 on the A-MISO-S, corresponding with subclinical misophonia symptoms.
After consent and screening, participants were scheduled for a separate assessment video that included online questionnaires and a clinical interview which included the Misophonia Assessment Interview (MAI) (Lewin, 2020; Lewin et al., 2021) and the MINI-KID (Sheehan et al., 2010) Interviewers were research coordinators with a bachelor’s degree in psychology or a related field (e.g., neuroscience) or doctoral students in professional psychology. Training included didactic presentations on the MINI-KID and MAI, observation and co-rating of assessments with a trained rater, and weekly supervision with a licensed psychologist to ensure validity and reliability of assessments.
The Institutional Review Board at Baylor College of Medicine approved the study. All portions of the study were completed virtually.
Participants
One-hundred and twelve youth with suspected misophonia and 140 youth with suspected anxiety disorders were recruited. Of the 112 youth in the misophonia group, 102 were included in analyses; of the 140 in the anxiety group, 94 were included. Reasons for exclusion in the misophonia group included too mild misophonia symptoms (Amsterdam Misophonia Scale [A-MISO-S] score <10), n = 5 (5%), or failed attempts to schedule an assessment visit after the initial informed consent video call, n = 5 (5%). Reasons for exclusion in the anxiety group included: MASC score below the clinical cutoff, n = 26 (19%), A-MISO-S score too high, 9 (6%), no anxiety disorder as assessed on the MINI-KID, n = 9 (6%), and failed attempts to schedule an assessment visit after the initial informed consent video call, n = 2 (1%).
Measures
Misophonia characteristics.
The Misophonia Assessment Interview (Lewin, 2020) is a series of questions evaluating symptoms of sound sensitivity, enhanced emotional and physical reactions to sound triggers, and degrees of avoidance or interference with daily activities. Based on the initially proposed diagnostic criteria for misophonia by Schroeder et al. (2013), it asks about specific sound triggers, emotional responses, and avoidance behaviors. It was developed to follow the format of a commonly used diagnostic interview using the proposed diagnostic criteria of misophonia for an ongoing randomized clinical trial separate from this study (Lewin et al., 2021). This assessment was only administered to the misophonia sample. Responses to items on the MAI are presented descriptively to characterize the presentation of misophonia in youth.
Misophonia severity.
The A-MISO-S, adapted from the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) (Goodman, 1989; Goodman et al., 1989), is a commonly used measure of misophonia severity (Schröder et al., 2013) that has shown strong psychometric properties as a self-report measure in college students, including good internal consistency and a single-factor structure that explained 45% of the variance in item responses (Naylor et al., 2021). It includes six 0–4 Likert scale items assessing time taken by symptoms, functional impairment, emotional distress, resistance against symptoms, control over symptoms, and avoidance. It was administered as a child-report measure in this study, which has showed adequate psychometric properties in youth with misophonia, including a clear single-factor structure as well as adequate convergent validity and internal consistency (Cervin et al., 2022). Because it was developed for adults, to administer the measure in a developmentally-tailored manner, the measure was presented to youth with a trained assessor present to provide additional clarifications on items when youth had questions. Item 4 was not included in the total score because this item does not contribute to overall severity and the measure has been shown to be more internally consistent without it (Cervin et al., 2022); in this sample, internal consistency was α = .68 with all 6 items and α = .76 with 5 items, so the 5-item version was used. The MAQ aids in measuring misophonia severity by evaluating the negative impact of misophonia symptoms on a n individual’s activities, thoughts, and emotions (Dozier, 2015; Johnson and Dozier, 2013). It includes 21 items scored on a 0–3 Likert scale and has also shown strong psychometric properties for both the child-reported (C-MAQ) and parent-reported (P-MAQ) versions, including strong internal consistency and convergent validity (Cervin et al., 2022). The overall MAQ misophonia scale was used in the present study and showed high internal consistency in this sample; C-MAQ: α = .94; P-MAQ: α = .93.
Psychiatric diagnoses.
Psychiatric diagnoses were assessed with the MINI-KID, a commonly used and well-validated psychiatric interview based on DSM-5 and ICD-11 criteria. The MINI-KID has shown strong psychometric properties in general and clinical populations (Boyle et al., 2017; Duncan et al., 2018; Sheehan et al., 2010). It is designed to be a streamlined diagnostic interview that can be administered by raters with a range of training under the supervision of an experienced clinician (Sheehan et al., 2010).
Emotional and behavioral functioning.
The parent-report Child Behavior Checklist (CBCL) and child-report Youth Self Report (YSR) are well-validated, broadband measures of childhood psychopathology that include 112 0–2 Likert scale items (Achenbach and Rescorla, 2001). The CBCL/YSR generates internalizing and externalizing scales that correspond to mood/anxiety symptoms and disruptive behavior symptoms, respectively (Achenbach and Rescorla, 2001). Both subscales across child- and parent-report showed high internal consistency in this sample; CBCL-externalizing: α = .89; CBCL-internalizing: α = .89; YSR-externalizing: α = .83; YSR-internalizing: α = .90.
Autism spectrum features.
The Social Responsiveness Scale, Second Edition (SRS-2) is a measure of deficits in social adaptive functioning and a commonly used, well-validated evaluation of ASD that includes 65 items scored on a 0–3 Likert scale (Bruni, 2014; Constantino and Gruber, 2012). It contains sub-domains scoring social communication and interaction (SRS-SCI) as well as restricted or repetitive behavior (SRS-RRB) corresponding with the symptom domains of autism spectrum disorder described in the Diagnostic and Statistical Manual of Mental Disorders (Constantino and Gruber, 2012). The SRS-2 shows strong psychometric properties and high internal consistency in this sample, SRS-SCI: α = .92; SRS-RRB: α = .82.
Quality of life.
PQLES-Q. The pediatric version of the Short Form of the Quality of Life Enjoyment and Satisfaction Questionnaire is a self-report questionnaire with items scored on a 1–5 Likert scale that assesses quality of life among children and adolescents (Endicott et al., 2006). It has shown strong internal consistency, test-retest reliability, and concurrent validity among both children and adolescents (Endicott et al., 2006). Internal consistency in this sample was α = .89.
Analysis plan
First, data were evaluated for patterns of missingness and conformity to normal distribution assumptions. Missing data were rare (two YSR, one CBCL-Internalizing subscale, one parent-report MAQ, one SRS-RRB), and thus completer-only analyses were conducted. Data were not found to show significant skewness or kurtosis, with all skewness and kurtosis statistics falling within −2 and +2, suggesting they would be appropriate for parametric analyses (George and Mallery, 2010).
To evaluate the clinical characteristics of youth with misophonia, descriptive information from the Misophonia Diagnostic Interview were presented, including frequencies of different trigger sounds, avoidance behaviors, aggression responses, and emotional responses. Demographic information was also presented. To evaluate the psychiatric morbidity of the sample, frequencies of different psychiatric diagnoses were presented as well as norm referenced scale scores on the CBCL, YSR, and SRS-2. One-sample t-tests comparing mean t-scores for each subscale with a population mean of 50 were conducted to estimate significant differences with typical populations. Independent samples t-tests evaluated differences in CBCL, YSR, and SRS-2 scores between the misophonia and anxiety groups. Recruitment targets were based on a power analysis for a cluster analysis (in preparation). For this study, given power = .80, alpha = .01 (for all analyses, p < .01 was interpreted as significant to minimize family-wise error), and sample sizes of 102 and 94, this study was powered to detect a medium between-group effect of d = .48. Within the misophonia sample, partial correlations controlling for age and gender (male vs. non-male) between misophonia symptom severity (using the A-MISO-S and MAQ) and psychiatric symptom scales (CBCL and YSR), quality of life (PQ-LES-Q), and autistic features (SRS-2) were conducted. With 102 participants, given power = .80 and alpha = .01, this study was powered to detect small-to-medium correlations (r = .33).
Results
Sample demographics
The majority of the misophonia sample identified as White (87%) and female (68%). The mean age of the sample was 13.7 years (SD = 2.5) and the mean age of misophonia onset was 8.8 years (SD = 3.0). The majority of the anxiety sample also identified as White (71%) and female (57%), with a mean age of 12.4 years. The misophonia group was significantly older and had a significantly higher proportion of participants who identified as White (see Table 1). A summary of demographic information is presented in Table 1.
Table 1.
Demographics
| Misophonia sample (N = 102) | Anxiety sample (N = 94) | Difference (d or χ2) | |
|---|---|---|---|
|
|
|||
| Age M (SD) | 13.7 (2.5) | 12.4 (2.6) | d = .50** |
| Gender N (%) | χ2 (1) = 2.18 a | ||
| Male | 29 (28%) | 32 (34%) | |
| Female | 69 (68%) | 54 (57%) | |
| Trans male | 1 (1%) | 0 (0%) | |
| Trans female | 1 (1%) | 0 (0%) | |
| Other | 2 (2%) | 8 (9%) | |
| Race N (%) | χ2 (1) = 7.69* b | ||
| White | 89 (87%) | 67 (71%) | |
| Asian | 4 (4%) | 2 (2%) | |
| Black or African American | 3 (3%) | 10 (11%) | |
| Other (self-described) | |||
| Arab | 1 (1%) | ||
| White/African American or Black | 1 (1%) | 1 (1%) | |
| Asian/White | 6 (6%) | ||
| Evite/Latino | 1 (1%) | ||
| Hispanic | 1 (1%) | ||
| Biracial | 1 (1%) | ||
| Did not respond | 4 (4%) | 1 (1%) | |
| Hispanic Ethnicity N (%) | 6 (6%) | 13 (14%) | |
p < .01
p < .001
Comparison was females vs. non-females due to low frequency of non male/female gender identities
Comparison was White vs. non-White due to low frequency of individual non-White racial identities
Clinical characteristics of misophonia in youth
Among youth with misophonia, the most common trigger sounds included: eating sounds (people eating/chewing/swallowing/lip smacking/slurping/teeth tapping), n = 98 (96%), breathing sounds (people breathing/sniffing/exhaling/inhaling/yawning), n = 86 (84%), throat noises (people making throat clearing sounds/coughing), n = 67 (66%), tapping (people tapping with hands, feet, or object), n = 55 (54%), specific language sounds or tones, rustling sounds (rustling/clattering of paper, plastic, or aluminum foil), n = 37 (36%), and environmental sounds (clocks, engines, appliances), n = 29 (28%). See Figure 1 for a summary.
Figure 1.
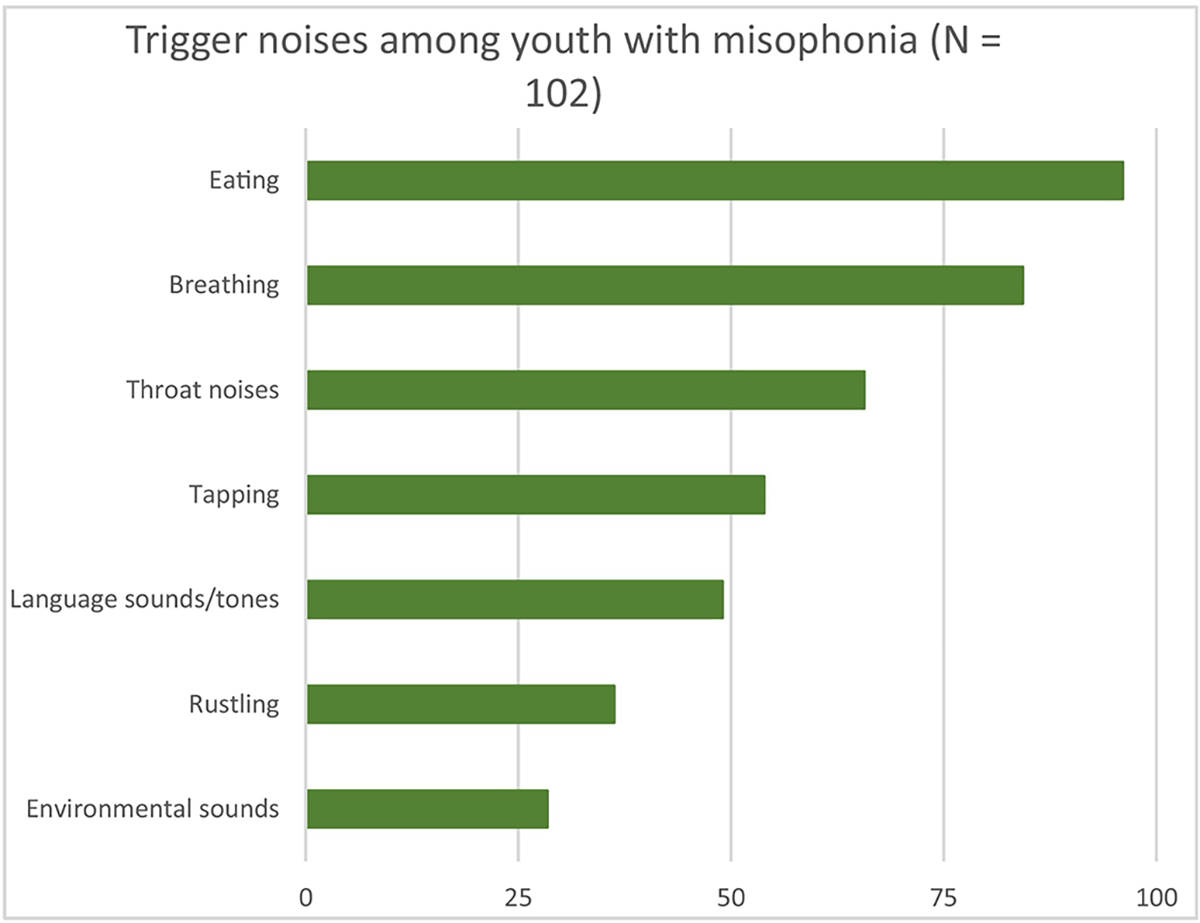
Trigger noises among youth with misophonia (N = 102)
Most youth with misophonia reported experiencing annoyance/irritation, n = 99 (97%) or anger, n = 97 (95%) when hearing (or anticipating hearing) trigger noises. Other emotional responses or anticipatory emotions were also frequently endorsed, including a general feeling of distress, n = 95 (93%), worry/anxiety, n = 81 (79%), disgust, n = 69 (68%), and sadness/depression, n = 44 (43%). Importantly, emotional responses were assessed as in response to or in anticipation of hearing triggers without specifically distinguishing between them. A high portion also endorsed a history of aggressive responses, most frequently verbal aggression, n = 87 (85%), though physical aggression was also common (including aggressive outbursts or damage to objects/property), n = 51 (50%). Avoidance of specific situations was common as well, most frequently family members, n = 82 (80%), and meals, n = 77 (76%). Most of the sample endorsed specific modifications, anticipatory avoidance, or reactive avoidance behaviors, most commonly covering ears with hands, n = 94 (92%), using protective equipment like headphones, n = 93 (91%), or eating privately or with special arrangements (e.g., apart from siblings), n = 86 (84%). A summary of these data is presented in Figure 2.
Figure 2.
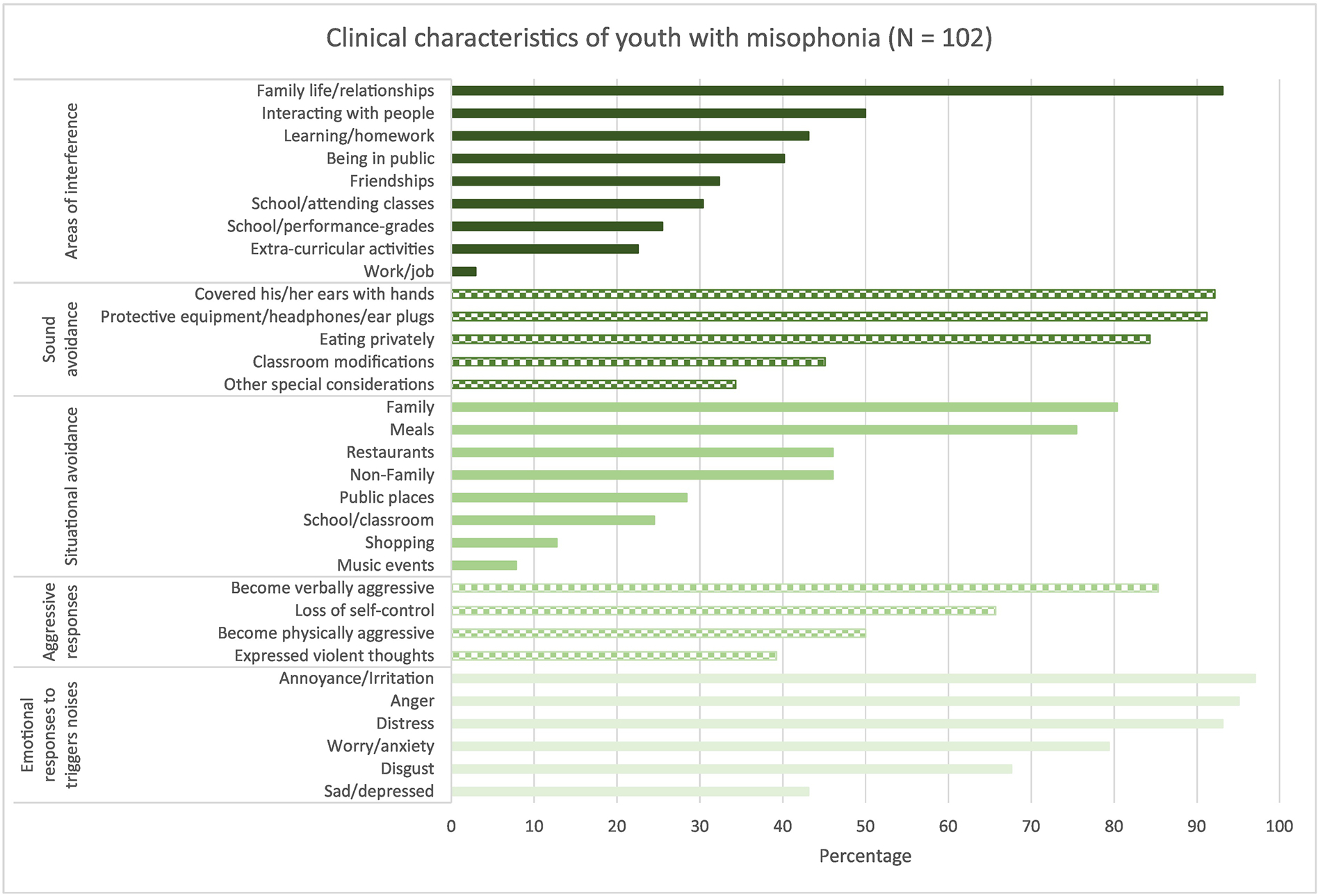
Clinical characteristics of youth with misophonia (N = 102)
Psychiatric morbidity
Psychiatric morbidity in the misophonia sample was high, with 81 participants (79%) meeting criteria for at least one psychiatric diagnosis. Almost half of the sample experienced a major depressive disorder (current or past), n = 48 (47%), with 15 (15%) experiencing a current depressive episode at the time of assessment. Nearly half were experiencing a current anxiety or obsessive-compulsive disorder, n = 46 (45%); the most commonly anxiety disorders were social anxiety disorder, n = 31 (30%) and generalized anxiety disorder n = 27 (27%). Obsessive-compulsive disorder occurred in 8 participants (8%). Other common diagnoses included attention-deficit/hyperactivity disorder, n = 21 (21%) and chronic tic disorders, n = 13 (13%). Please see Figure 3 for a summary of non-misophonia primary and total psychiatric diagnoses in the sample.
Figure 3.
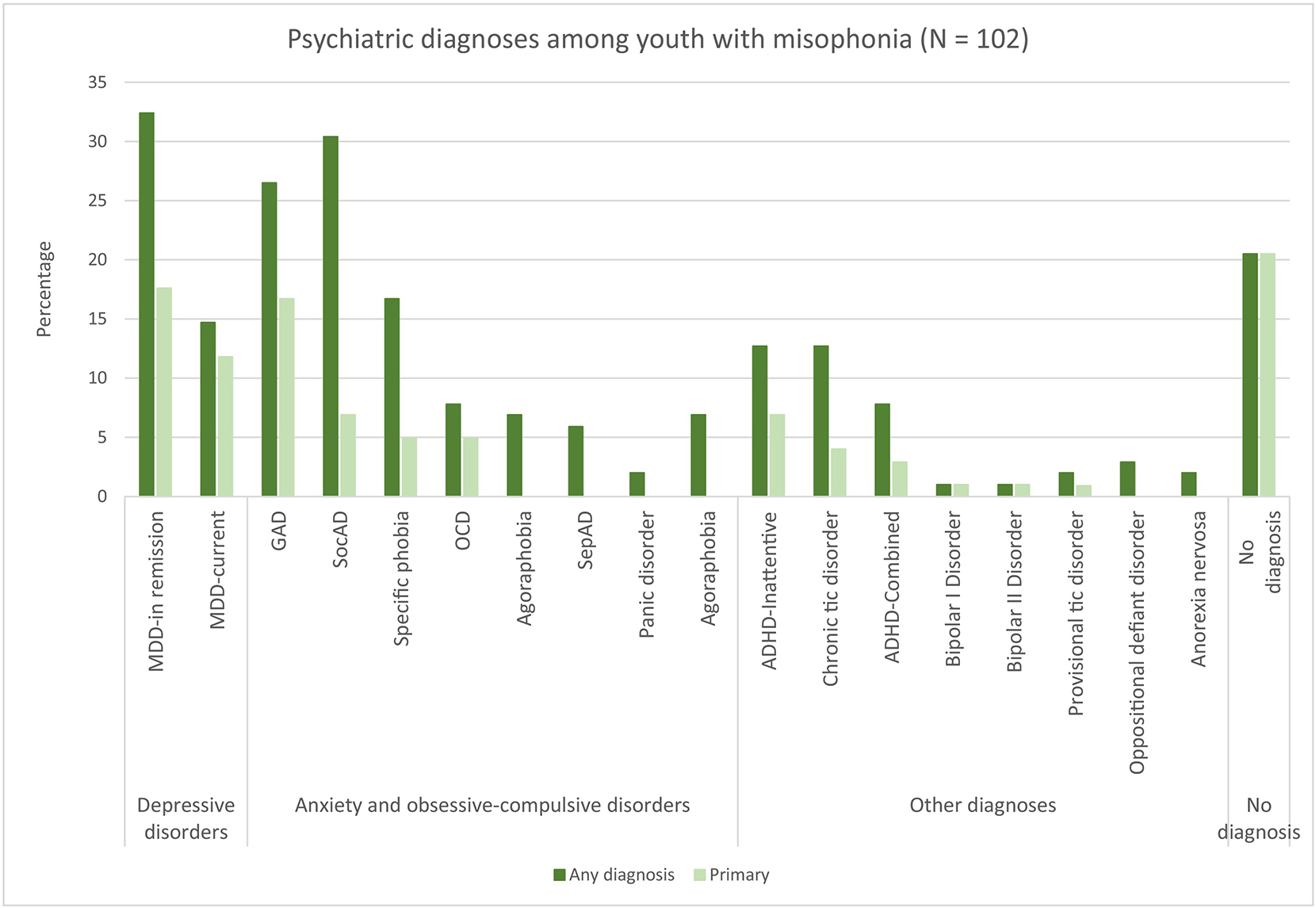
Psychiatric diagnoses among youth with misophonia (N = 102)
Youth were found to have clinically elevated internalizing symptoms per both youth and parent-report, YSR-Internalizing M (SD) = 67.1 (14.2); CBCL-Internalizing M (SD) = 69.8 (16.5). These values were significantly higher than what would be expected in a randomly sampled population, YSR-Internalizing: t (100) = 12.12, d = 1.21, p < .001; CBCL-Internalizing: t (99) = 11.95, d = 1.20, p < .001. Using the CBCL cutoff of a T-score of 70 representing the clinical range, clinically elevated internalizing symptoms were reported in 44 youth with misophonia (43%) based on child-report and 46 youth (45%) based on parent-report. On average, externalizing symptoms were in the non-clinical range per child- or parent-report, YSR-Externalizing M (SD) = 55.4 (8.4); CBCL-Externalizing M (SD) = 52.0 (9.8). The YSR-Externalizing subscale was significantly higher than what might be expected in a typically developing sample, t (100) = 6.51, d = 0.65, p < .001, though the CBCL-Externalizing was not, t (99) = 2.03, d = 0.20, p = .045. Three youth with misophonia (3%) self-reported clinically elevated externalizing symptoms and 6 (6%) parent-reported clinically elevated externalizing symptoms.
On average, youth with misophonia did not show elevated scores on the SRS-SCI, M (SD) = 55.0 (9.3), or the SRS-RRB, M (SD) = 53.9 (10.1), though these values were significantly higher than what would be expected in a randomly sampled population with a mean of 50, SRS-SCI, t(101) = 5.49, d = 0.54, p < .001; t(100) = 3.91, d = .39, p < .001. Using a T-score of 70 as representing the clinical range, 8 (8%) were found to have clinically elevated scores on the SRS-SCI and 11 (11%) on the SRS-RRB.
The most commonly endorsed areas of misophonia-related impairment were family life/relationships, n = 95 (93%), interacting with people, n = 51 (50%), learning/homework, n = 44 (43%), and being in public, n = 41 (40%). A complete summary of these data is presented in Figure 2.
Comparing psychiatric symptoms in anxiety and misophonia samples.
For all comparisons, age-normed T-scores were used. The anxiety group had significantly higher scores on both the YSR-Internalizing, t (191) = 3.49, p < .001, d = .50, and CBCL-Internalizing subscales, t (192) = 3.52, p < .001, d = .51. Externalizing symptoms were not significantly different between the anxiety and misophonia groups, YSR-Externalizing: t (191) = 1.49, p = .14, d = .21; CBCL-Externalizing: t (194) = 1.72, p = .087, d = .25. Youth with anxiety disorders were found to have significantly higher scores on the SRS-SCI, t (194) = 3.82, p < .001, d = .55., and the SRS-RRB, t (192) = 3.07, p = .002, d = .44. There were no significant differences between the samples in PQLES-Q scores, t (192) = 0.39, p = .70, d = .056.
A linear regression was conducted controlling for race (White vs. non-White) and an identical pattern of significance emerged. Specifically, when controlling for race, misophonia sample membership was associated with less severe CBCL-Internalizing, β = −.26, p < .001, ΔR2 = .064, YSR-Internalizing, β = −.24, p < .001, ΔR2 = .056, SRS-SCI, β = −.27, p < .001, ΔR2 = .068, and SRS-RRB scores, β = −.22, p = .002, ΔR2 = .047. There was no significant association with CBCL-Externalizing, β = −.14, p = .051, ΔR2 = .020, YSR-Externalizing, β = −.11, p = .13, ΔR2 = .012, or PQLES-Q scores, β = −.038, p = .61, ΔR2 = .001.
Clinical correlates
Within the misophonia sample, when controlling for age and gender, both the P-MAQ and C-MAQ were associated with a number of other clinical measures, including the YSR-Internalizing subscale, the YSR-Externalizing subscale, the CBCL-Internalizing subscale, the MASC, and the P-QLES-Q. The A-MISO-S was not significantly associated with any of the tested variables, though was modestly associated with the following variables at a trend level: YSR-Internalizing, CBCL-Externalizing, SRS-RRB, and PQLES-Q. See Table 2 for a summary
Table 2.
Correlations between misophonia severity and psychiatric symptoms (controlling for age and gender)
| YSR-Internalizing | YSR-Externalizing | CBCL-Internalizing | CBCL-Externalizing | SRS-2-SCI | SRS-2-RRB | MASC | PQLES-Q | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| A-MISO-S | .22+ | .19 | .15 | .23+ | .16 | .21+ | .12 | −.26+ |
| P-MAQ | .39** | .28* | .26* | .13 | .18 | .20 | .28* | −.32* |
| C-MAQ | .56** | .41** | .30* | .15 | .24+ | .22+ | .38** | −.52** |
p<.05
p<.01
p<.001
A-MISO-S=Amsterdam Misophonia Scale; C-MAQ=Child-report Misophonia Assessment Questionnaire; CBCL=Child Behavior Checklist; MASC=Multidimensional Anxiety Scale for Children; P-MAQ=Parent-report Misophonia Assessment Questionnaire; P-QLES-Q: Quality of Life Enjoyment and Satisfaction Questionnaire; SRS-2-RRB=Social Responsiveness Scale, Second Edition-Repetitive Behaviors and Restricted Interests Subscale; SRS-2-SCI=Social Responsiveness Scale, Second Edition-Social Communication Impairment Index; YSR=Youth Self-Report
Discussion
This study described the clinical presentation of misophonia in a large cohort of children and adolescents. Consistent with studies in adults (Claiborn et al., 2020; Jager et al., 2020; Rouw and Erfanian, 2018; Wu et al., 2016), the most prevalent trigger noises included those related to eating, breathing, or making throat noises, though other triggers were common as well (e.g., tapping, paper rustling). The most common emotional responses were anger and annoyance/irritation, though there was a significant mix of emotional responses, with participants also describing anxiety, disgust, and sadness as well in reaction to or in anticipation of trigger noises. Avoidance behaviors were nearly ubiquitous, with the most frequently endorsed behaviors including covering ears (with hands or noise-blocking devices such as headphones), avoiding places involving eating, and avoiding specific people, most commonly family members. Nearly all youth had become verbally aggressive in response to trigger noises at some point, and over half had engaged in physical aggression. Interference with family life was reported in nearly every participant, though interference with social life outside the family was also present in over half the sample, and interference with various other areas of life were also commonly endorsed (e.g., school, learning/homework). Misophonia severity was associated with poorer quality of life, which was reported at similar levels as youth with anxiety disorders, a population who consistently report quality of life impairments compared with typically developing youth (Bastiaansen et al., 2004; Ramsawh and Chavira, 2016). Also consistent with reports in adults (Claiborn et al., 2020; Jager et al., 2020; Rouw and Erfanian, 2018), most participants were female, although the self-referred nature of the sample warrants caution in interpreting this trend. The age-of-onset was just younger than 9, which aligns with the lower end of the estimates that have been reported in adults (Claiborn et al., 2020; Jager et al., 2020; Rouw and Erfanian, 2018), as would be expected in a study focused on youth.
High rates of psychiatric comorbidity were noted in this sample, with 80% meeting criteria for at least one disorder. The most common psychiatric diagnoses were social anxiety disorder, generalized anxiety disorder, major depressive disorder, and specific phobias. Anecdotally, during interviews, participants frequently described feeling depressed because of the isolation and distress caused by misophonia. It is possible there is a similar causal pathway with social anxiety in severe cases of misophonia, as social avoidance and interference was very commonly reported in this sample. Significant, medium-to-large associations between the parent- and child-report MAQ (assessing misophonia symptoms) and anxiety, internalizing symptoms, quality of life, and externalizing symptoms were found, further supporting a link between misophonia and psychiatric symptoms. It is worth noting more consistent and larger associations between psychiatric symptom measures and the MAQ relative to the A-MISO-S, whose items assess the impact of misophonia (e.g., “My sound issues currently make me unhappy;” “My sound issues currently interfere with my social life”), relative to items more directly assessing misophonia severity on the A-MISO-S (e.g., “How much distress do the misophonic triggers cause you”?). Reliability was also higher on the MAQ, which may have contributed to differential associations. This highlights the need for rigorous psychometric testing and refinement of misophonia assessments in youth, which are only beginning to be conducted (Cervin et al., 2022; Rinaldi et al., 2022a).
These comorbidity findings were consistent with two studies in adults (Rosenthal et al., 2022; Siepsiak et al., 2022), though contrasted two others that recruited patients as part of clinic flow, which found lower rates of comorbidity (Erfanian et al., 2019; Jager et al., 2020, though higher-than-expected depression and ADHD were noted in Jager et al., 2020). It is possible this discrepancy is due to the recruitment methods for these different studies; the current study and the similar adult studies used primarily online and community-based recruitment whereas Erfanian et al. (2019) included both psychiatry and audiology clinic referrals, the latter of which may be less psychiatrically affected. Jager et al. (2020) may have also had referral patterns that resulted in a different clinical presentation.
Results support conceptualizing misophonia as a disorder on the internalizing spectrum, with high rates of negative-valence emotional responses to sound triggers, significant associations with co-occurring internalizing symptoms, and high comorbidity with mood and anxiety disorders. Further, despite frequently reported anger outbursts and family conflict tied to misophonia, externalizing symptoms were not significantly different from youth with anxiety disorders, and similar to what might be expected in a normative sample (Merikangas et al., 2010), suggesting it is likely more an “internalizing” than “externalizing” problem. That said, the anxiety disorder group reported higher internalizing symptoms than the misophonia group. Although this finding may be related to a measurement artifact (i.e., anxiety is more specifically assessed on the CBCL and YSR than misophonia symptoms), it may also indicate that categorizing misophonia as an internalizing disorder is an overly simplistic conclusion.
To that end, beyond internalizing disorders, there were high rates of comorbidity with several diagnoses beyond what would be expected in a randomly selected sample, including chronic tic disorders (13%), ADHD (21%), and OCD (8%), as well as high rates of elevated autistic characteristics (8% with elevated social communication/interaction difficulties; 10% with elevated repetitive behaviors and focused interests). Rather than being linked to one specific diagnosis, it is likely that shared transdiagnostic processes across these diagnoses led to this pattern. One psychological dimension that may be implicated across these disorders is sensory dysregulation, which should be more thoroughly investigated in follow-up work (Harrison et al., 2019). Further research should seek to better understand comorbidity in misophonia, as co-occurring psychiatric diagnoses likely exist due to shared predispositions (e.g., genetics, neurobiology, behavioral patterns) as well as causal pathways (e.g., misophonia-related isolation causing depression and social anxiety).
It is worth noting that the anxiety sample reported significantly higher autistic characteristics than the misophonia sample, and further, that misophonia symptoms were not correlated with autism characteristics, consistent with a large study in adults (Jager et al., 2020). Autism features have been found to be elevated in youth with misophonia relative to non-misophonia controls in prior work (Rinaldi et al., 2022b); it is plausible that some may consider this finding reflective of some specific relationship between autism and misophonia, particularly when considering the phenomenological similarities in sound sensitivity in these syndromes, which are rarely seen in other populations. When comparing with a relevant psychiatric control in this study, the autism-misophonia connection appears less specific and further supports the notion that there may be other underlying dimensions across these conditions (e.g., emotional and sensory hyperreactivity), rather that misophonia reflecting a symptom of some other diagnosis.
A clear understanding of the clinical presentation of misophonia in youth provides a much-needed foundation for interdisciplinary work investigating the mechanisms of this disorder, which will inform innovative treatment development. For example, avoidance behavior was very commonly reported in this sample, both in anticipation of and in response to trigger noises (e.g., using headphones, avoiding family members, avoiding meals). Behavioral and emotional avoidance is considered to play a central role in the development and maintenance of mood, anxiety, and obsessive-compulsive disorders in youth, and thus has become a key treatment target of cognitive-behavioral therapies, and it is reasonable to expect it would play a similar role in misophonia (Chu, 2013; Kennedy and Ehrenreich-May, 2017).
This study had several limitations. First, participants primarily identified as White and English speaking; further work is needed to understand misophonia in culturally diverse populations. The comparison anxiety group was significantly younger and less frequently identified as White; although age-corrected scores were used in comparison analyses and the pattern of results did not change when statistically controlling for race, results should be considered within this possible limitation. Similarly, the misophonia sample was recruited predominantly from online support communities, and may reflect youth with more severe, primary misophonia, and results may be less generalizable to youth with misophonia sampled from the general population, or youth with misophonia as a secondary diagnosis. Another limitation of this study was the use of misophonia assessments with only preliminary psychometric validation; unfortunately no validated assessments were available when this study began and thus we adapted measures from the adults literature to draw conclusions. Rigorous development of psychometrically validated assessment for misophonia severity and diagnosis are needed in the future. Further, only auditory triggers were assessed in this study despite an increasing appreciation of visual triggers in the clinical presentation of misophonia (Swedo et al., 2022) Further research is also needed to understand clinical features of misophonia from interdisciplinary perspectives (e.g., audiological and neurobiological evaluations were not included in this study) and in comparison with other populations (e.g., autistic youth).
This study provided foundational data on the clinical presentation of misophonia in youth, confirming a highly impairing clinical presentation that is congruent with reports in adults while adding an important developmental perspective. Further research is needed to understand the mechanisms of this disorder to inform treatment development.
Highlights.
Misophonia was associated with substantial functional impairment in this sample
Anger/irritation, avoidance behavior, and impact to family life were nearly universal
Anxiety disorders were common (45%) as were current or past depressive disorders (46%)
Other common comorbidities were attention-deficit/hyperactivity disorder (21%) and tic disorders (13%)
Youth with misophonia had elevated internalizing symptoms and autism features relative to population norms (though less than youth with anxiety disorders)
Acknowledgements:
We thank the families who participated in this study as well as the numerous misophonia advocates who helped promote the study.
Role of the Funding Source:
Research reported in this publication was supported by a grant from the Ream Foundation/Milken Institute/Misophonia Research Fund, as well as support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number P50HD103555 for use of the Clinical and Translational Core facilities. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Ream Foundation nor the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Ream Foundation/Milken Institute/Misophonia Research Fund or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla L, 2001. Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families, Burlington, VT. [Google Scholar]
- Bastiaansen D, Koot HM, Ferdinand RF, Verhulst FC, 2004. Quality of Life in Children With Psychiatric Disorders: Self-, Parent, and Clinician Report. Journal of the American Academy of Child & Adolescent Psychiatry 43, 221–230. 10.1097/00004583-200402000-00019 [DOI] [PubMed] [Google Scholar]
- Boyle MH, Duncan L, Georgiades K, Bennett K, Gonzalez A, Van Lieshout RJ, Szatmari P, MacMillan HL, Kata A, Ferro MA, Lipman EL, Janus M, 2017. Classifying child and adolescent psychiatric disorder by problem checklists and standardized interviews. International Journal of Methods in Psychiatric Research 26, e1544. 10.1002/mpr.1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni TP, 2014. Test Review: Social Responsesiveness Scale-Second Edition (SRS-2). Journal of Psychological Assessment 32, 365–369. 10.1177/0734282913517525 [DOI] [Google Scholar]
- Cervin M, Guzick AG, Smith EEA, Clinger J, Draper IA, Goodman WK, Lijffift M, Murphy N, Schneider SC, Storch EA, under review. A psychometric evaluation of child and parent measures of pediatric misophonia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu BC, 2013. Behavioral avoidance across anxiety, depression, impulse, and conduct problems, in: Transdiagnostic Treatments for Children and Adolescents: Principles and Practice. Guilford Press. [Google Scholar]
- Claiborn JM, Dozier TH, Hart SL, Lee J, 2020. Self-identified misophonia phenomenology, impact, and clinical correlates. Psychological Thought 13, 349–375. 10.37708/psyct.v13i2.454 [DOI] [Google Scholar]
- Constantino JN, Gruber CP, 2012. Social Responsiveness Scale-Second Edition (SRS-2).
- Cusack SE, Cash TV, Vrana SR, 2018. An examination of the relationship between misophonia, anxiety sensitivity, and obsessive-compulsive symptoms. Journal of Obsessive-Compulsive and Related Disorders 18, 67–72. 10.1016/j.jocrd.2018.06.004 [DOI] [Google Scholar]
- Dover N, McGuire JF, 2021. Family-Based Cognitive Behavioral Therapy for Youth With Misophonia: A Case Report. Cognitive and Behavioral Practice. 10.1016/j.cbpra.2021.05.005 [DOI] [Google Scholar]
- Dozier TH, 2015. Counterconditioning Treatment for Misophonia. Clinical Case Studies 14, 374–387. 10.1177/1534650114566924 [DOI] [Google Scholar]
- Duncan L, Georgiades K, Wang L, Van Lieshout RJ, MacMillan HL, Ferro MA, Lipman EL, Szatmari P, Bennett K, Kata A, Janus M, Boyle MH, 2018. Psychometric evaluation of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Psychol Assess 30, 916–928. 10.1037/pas0000541 [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Yang R, Wohlberg C, 2006. Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q): Reliability and Validity. Journal of the American Academy of Child & Adolescent Psychiatry 45, 401–407. 10.1097/01.chi.0000198590.38325.81 [DOI] [PubMed] [Google Scholar]
- Erfanian M, Kartsonaki C, Keshavarz A, 2019. Misophonia and comorbid psychiatric symptoms: a preliminary study of clinical findings. Nordic Journal of Psychiatry 73, 219–228. 10.1080/08039488.2019.1609086 [DOI] [PubMed] [Google Scholar]
- George D, Mallery P, 2010. SPSS for Windows Step by Step: A Simple Guide and Reference. Pearson Education, Boston, MA. [Google Scholar]
- Golomb RG, Mouton-Odum S, 2016. Psychological Interventions for Children with Sensory Dysregulation. Guilford Publications. [Google Scholar]
- Goodman WK, 1989. The Yale-Brown Obsessive Compulsive Scale: II. Validity. Arch Gen Psychiatry 46, 1012. 10.1001/archpsyc.1989.01810110054008 [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS, 1989. The Yale-Brown Obsessive Compulsive Scale: I. Development, Use, and Reliability. Arch Gen Psychiatry 46, 1006–1011. 10.1001/archpsyc.1989.01810110048007 [DOI] [PubMed] [Google Scholar]
- Harrison LA, Kats A, Williams ME, Aziz-Zadeh L, 2019. The Importance of Sensory Processing in Mental Health: A Proposed Addition to the Research Domain Criteria (RDoC) and Suggestions for RDoC 2.0. Frontiers in Psychology 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager I, Koning P. de, Bost T, Denys D, Vulink N, 2020. Misophonia: Phenomenology, comorbidity and demographics in a large sample. PLOS ONE 15, e0231390. 10.1371/journal.pone.0231390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jastreboff PJ, Jastreboff MM, 2000. Tinnitus Retraining Therapy (TRT) as a Method for Treatment of Tinnitus and Hyperacusis Patients. Tinnitus Retraining Therapy 11, 18. [PubMed] [Google Scholar]
- Johnson M, Dozier T, 2013. Misophonia Assessment Questionnaire =.
- Kennedy SM, Ehrenreich-May J, 2017. Assessment of Emotional Avoidance in Adolescents: Psychometric Properties of a New Multidimensional Measure. J Psychopathol Behav Assess 39, 279–290. 10.1007/s10862-016-9581-7 [DOI] [Google Scholar]
- Lewin A, 2020. Misophonia Assessment Interview.
- Lewin AB, Dickinson S, Kudryk K, Karlovich AR, Harmon SL, Phillips DA, Tonarely NA, Gruen R, Small B, Ehrenreich-May J, 2021. Transdiagnostic cognitive behavioral therapy for misophonia in youth: Methods for a clinical trial and four pilot cases. Journal of Affective Disorders 291, 400–408. 10.1016/j.jad.2021.04.027 [DOI] [PubMed] [Google Scholar]
- McGuire JF, Wu MS, Storch EA, 2015. Cognitive-Behavioral Therapy for 2 Youths With Misophonia. J Clin Psychiatry 76, 3143. 10.4088/JCP.14cr09343 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J, 2010. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry 49, 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller D, Khemlani-Patel S, Neziroglu F, 2018. Cognitive-Behavioral Therapy for an Adolescent Female Presenting With Misophonia: A Case Example. Clinical Case Studies 17, 249–258. 10.1177/1534650118782650 [DOI] [Google Scholar]
- Naylor J, Caimino C, Scutt P, Hoare DJ, Baguley DM, 2021. The Prevalence and Severity of Misophonia in a UK Undergraduate Medical Student Population and Validation of the Amsterdam Misophonia Scale. Psychiatr Q 92, 609–619. 10.1007/s11126-020-09825-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascal SA, Rodina IR, Nedelcea C, 2020. A Meta-Analysis on the Efficacy of Exposure-Based Treatment in Anxiety Disorders: Implications for Disgust. Journal of Evidence-Based Psychotherapies 20, 31–49. [Google Scholar]
- Potgieter I, MacDonald C, Partridge L, Cima R, Sheldrake J, Hoare DJ, 2019. Misophonia: A scoping review of research. Journal of Clinical Psychology 75, 1203–1218. 10.1002/jclp.22771 [DOI] [PubMed] [Google Scholar]
- Ramsawh HJ, Chavira DA, 2016. Association of Childhood Anxiety Disorders and Quality of Life in a Primary Care Sample. Journal of Developmental & Behavioral Pediatrics 37, 269–276. 10.1097/DBP.0000000000000296 [DOI] [PubMed] [Google Scholar]
- Reid AM, Guzick AG, Gernand A, Olsen B, 2016. Intensive cognitive-behavioral therapy for comorbid misophonic and obsessive-compulsive symptoms: A systematic case study. Journal of Obsessive-Compulsive and Related Disorders 10, 1–9. 10.1016/j.jocrd.2016.04.009 [DOI] [Google Scholar]
- Rinaldi LJ, Simner J, Koursarou S, Ward J, 2022. Autistic traits, emotion regulation, and sensory sensitivities in children and adults with Misophonia. J Autism Dev Disord. 10.1007/s10803-022-05623-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinaldi LJ, Smees R, Ward J, Simner J, 2022. Poorer Well-Being in Children With Misophonia: Evidence From the Sussex Misophonia Scale for Adolescents. Front Psychol 13, 808379. 10.3389/fpsyg.2022.808379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MZ, Anand D, Cassiello-Robbins C, Williams ZJ, Guetta RE, Trumbull J, Kelley LD, 2021. Development and Initial Validation of the Duke Misophonia Questionnaire. Frontiers in Psychology 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MZ, McMahon K, Greenleaf AS, Cassiello-Robbins C, Guetta R, Trumbull J, Anand D, Frazer-Abel ES, Kelley L, 2022. Phenotyping misophonia: Psychiatric disorders and medical health correlates. Front Psychol 13, 941898. 10.3389/fpsyg.2022.941898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouw R, Erfanian M, 2018. A Large-Scale Study of Misophonia. Journal of Clinical Psychology 74, 453–479. 10.1002/jclp.22500 [DOI] [PubMed] [Google Scholar]
- Sarigedik E, Yurteri N, 2021. Misophonia Successfully Treated of With Fluoxetine: A Case Report. Clinical Neuropharmacology 44, 191–192. 10.1097/WNF.0000000000000465 [DOI] [PubMed] [Google Scholar]
- Schröder A, Vulink N, Denys D, 2013. Misophonia: Diagnostic Criteria for a New Psychiatric Disorder. PLOS ONE 8, e54706. 10.1371/journal.pone.0054706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, Wilkinson B, 2010. Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J Clin Psychiatry 71, 0–0. 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- Siepsiak M, Rosenthal MZ, Raj-Koziak D, Dragan W, 2022. Psychiatric and audiologic features of misophonia: Use of a clinical control group with auditory over-responsivity. J Psychosom Res 156, 110777. 10.1016/j.jpsychores.2022.110777 [DOI] [PubMed] [Google Scholar]
- Smith EEA, Guzick AG, Draper IA, Clinger J, Schneider SC, Goodman WK, Brout JJ, Lijffijt M, Storch EA, 2022. Perceptions of various treatment approaches for adults and children with misophonia. Journal of Affective Disorders 316, 76–82. 10.1016/j.jad.2022.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swedo SE, Baguley DM, Denys D, Dixon LJ, Erfanian M, Fioretti A, Jastreboff PJ, Kumar S, Rosenthal MZ, Rouw R, Schiller D, Simner J, Storch EA, Taylor S, Werff KRV, Altimus CM, Raver SM, 2022. Consensus Definition of Misophonia: A Delphi Study. Frontiers in Neuroscience 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter HJ, Bukstein OG, Abright AR, Keable H, Ramtekkar U, Ripperger-Suhler J, Rockhill C, 2020. Clinical Practice Guideline for the Assessment and Treatment of Children and Adolescents With Anxiety Disorders. Journal of the American Academy of Child & Adolescent Psychiatry 59, 1107–1124. 10.1016/j.jaac.2020.05.005 [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, Jensen-Doss A, Hawley KM, Krumholz Marchette LS, Chu BC, Weersing VR, Fordwood SR, 2017. What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist 72, 79–117. 10.1037/a0040360 [DOI] [PubMed] [Google Scholar]
- Wu MS, Pinto A, Horng B, Phares V, McGuire JF, Dedrick RF, Van Noppen B, Calvocoressi L, Storch EA, 2016. Psychometric properties of the Family Accommodation Scale for Obsessive-Compulsive Disorder-Patient Version. Psychol Assess 28, 251–262. 10.1037/pas0000165 [DOI] [PubMed] [Google Scholar]
- Zhou X, Teng T, Zhang Y, Del Giovane C, Furukawa TA, Weisz JR, Li X, Cuijpers P, Coghill D, Xiang Y, Hetrick SE, Leucht S, Qin M, Barth J, Ravindran AV, Yang L, Curry J, Fan L, Silva SG, Cipriani A, Xie P, 2020. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. The Lancet Psychiatry 7, 581–601. 10.1016/S2215-0366(20)30137-1 [DOI] [PMC free article] [PubMed] [Google Scholar]


