Abstract
The majority of U.S. adults do not receive an annual influenza vaccination. Behavioral economics tools can be harnessed to encourage health behaviors. Specifically, scheduling patients by default for a flu shot appointment leads to higher vaccination rates at a medical practice than does merely encouraging flu shot appointments. It is not known, however, whether default appointments actually increase net vaccination or merely displace vaccinations from other venues. In the current field experiment, we examined the use of default appointments in a large medical practice and established that automatically scheduled appointments increased the total vaccination rate by 10 percentage points within the practice without displacing vaccinations that patients would otherwise have received in other settings. This increased vaccination rate came at the cost of a high no-show rate. These findings point to an effective way to increase vaccination rates and may offer a cost-saving measure in the scope of accountable care organizations.
Imagine Amy and Beth. Both receive letters from their doctor’s office about flu shots. Amy’s letter simply explains that flu shots are available and that if she would like an appointment for one, she should please call the office. Beth’s letter also states that flu shots are available but adds that she has been given a flu shot appointment for next Thursday at 7:30 a.m., although she can cancel or reschedule if she wishes. Which of these two women is more likely to receive a flu shot at her doctor’s office?
The answer matters because, in the 2015–2016 flu season, only 42% of U.S. adults received an annual influenza vaccine (flu shot),1,2 even though the shots are conveniently available at many workplaces, doctors’ offices, drugstores, and walk-in clinics, often at no out-of-pocket cost. The low vaccination rate resulted in an annual economic burden estimated at $5.8 billion, a figure that includes the costs of hospitalizations, doctors’ visits, deaths, and lost workdays (see the sidebar Selected Recent Flu Vaccination Statistics). That raises an urgent question for behavioral and social scientists: Can we nudge people to get a flu shot just as we have nudged people to sign up for organ donation and retirement savings?3,4
Selected Recent Flu Vaccination Statistics.
42 Percentage of U.S. adults who were vaccinated against influenza in 2015–2016A
31 Outpatient visits per year in the United States as a result of influenza infections, in millionsB
3.1 Days spent in the hospital per year in the United States as a result of influenza infections, in millionsB
611 Life-years lost per year in the United States as a result of influenza infections, in thousandsB
59% Average efficacy of the influenza vaccine,i in relative risk reductionC
5.8 Annual cost of illness from influenza, including inpatient, outpatient, and medication costs as well as productivity losses, in billions of dollarsD
13/18 Number of cost-effectiveness analyses in a review that found influenza vaccinationi to be cost saving—that is, flu shots save both lives and moneyE
A. Centers for Disease Control and Prevention. (2016). Flu vaccination coverage, United States, 2015–16 influenza season. Retrieved from http://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm
B. Molinari, N.-A. M., Ortega-Sanchez, I. R., Messonnier, M. L., Thompson, W. W., Wortley, P. M., Weintraub, E., & Bridges, C. B. (2007). The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine, 25, 5086–5096. doi:10.1016/j.vaccine.2007.03.046
C. Osterholm, M. T., Kelley, N. S., Sommer, A., & Belongia, E. A. (2012). Efficacy and effectiveness of influenza vaccines: A systematic review and meta-analysis. Lancet: Infectious Diseases, 12, 36–44. doi:10.1016/S1473-3099(11)70295-X
D. Ozawa, S., Portnoy, A., Getaneh, H., Clark, S., Knoll, M., Bishai, D., Patwardhan, P. D. (2016). Modeling the economic burden of adult vaccine-preventable diseases in the United States. Health Affairs, 35, 2124–2132.
E. Nichol, K. L. (2003). The efficacy, effectiveness and cost-effectiveness of inactivated influenza virus vaccines. Vaccine, 21, 1769–1775. doi:10.1016/S0264-410X(03)00070-7
i. Trivalent inactivated influenza vaccine given to adults aged 18–64 years.
In the example above, Beth has a flu shot appointment by default. The default effect—meaning the tendency for people to stick with the default option, as outlined by Thaler and Sunstein in their 2008 book Nudge5—implies that she is unlikely to cancel her appointment, whereas Amy is unlikely to make an appointment. The default or opt-out effect explains, among other health-related behaviors, why European countries with a presumed consent policy that assumes citizens are willing organ donors—requiring people to explicitly opt out if they choose not to be a donor—have organ donation rates exceeding 85%, compared with organ donation rates of less than 28% among countries that use an explicit consent policy—requiring people to explicitly opt in if they choose to be a donor.3 In the hypothetical case of Beth and Amy, on the basis of prior research (see the online Supplemental Material) demonstrating that default appointments for flu shots increase uptake at single sites such as the workplace, Beth, with her default appointment, is more likely than Amy to receive a flu vaccine at her doctor’s office. Indeed, a 2010 study led by Gretchen B. Chapman6 found that such a default intervention increased flu shot uptake by 36%, from 33% among 239 university employees in the opt-in condition to 45% among the 239 in the opt-out condition. That study focused on vaccinations obtained at a single on-campus occupational health clinic.
The fact that default appointments increase flu vaccination is encouraging news6,7 (see the online Supplemental Material): Scheduling default appointments costs very little compared with large-scale educational campaigns on flu vaccination. However, before recommendations for effective policy are made, it is imperative to determine if the default appointment intervention actually increases the rate of flu vaccination and does not simply displace vaccination from one setting to another. For instance, if Beth responds to the nudge by keeping her prescheduled clinic appointment and cancels the plan she had made to get her flu shot at a neighborhood pharmacy, then the letter would not be increasing the overall vaccination rate but, instead, moving flu shots from one site to another.
Such a displacement effect has been examined in studies of the effect of menu labeling laws, which require chain restaurants to list the number of calories in each of their menu items. In a 2010 study, researchers at Yale University found that participants assigned to order from a dinner menu that both listed calories and stated the daily recommended caloric intake chose items with fewer calories than did participants who ordered from a menu containing the same items but lacking the calorie information. The researchers assessed whether the former group made up those averted calories by eating more after dinner. The total caloric intake was indeed lower when participants received both calorie labels and recommended daily caloric intake—that is, the intervention did not simply displace caloric intake until later in the day. When participants received only calorie labels and not recommended daily caloric intake, however, then the calorie savings at the meal were offset by snacking later in the day, a displacement effect.8 Researchers often cannot assess this type of displacement effect because they do not know what individuals do outside of the time frame and location of the study. Despite this difficulty, it is critical to analyze displacement effects as fully as possible to gauge the real-world impact of default interventions on behavior. In the current study, we do just that. In addition to finding an increase in vaccination rates at the medical practice as a result of scheduling default flu shot appointments, we determined that this increase did not come about merely because we displaced vaccinations from other venues.
Testing for Displacement Effects in Default Flu Shot Appointments
In the current study, we examined whether scheduling flu shot appointments by default actually increased the vaccination rate or merely displaced vaccination from other settings, such as the pharmacy or workplace, to the appointment site—in the case of our field study, a suburban New Jersey medical school faculty medical practice with a middle-class patient base diverse in terms of age and health status. We explored this issue in two ways. First, we collected records of vaccination in two settings within the medical practice: at the “flu clinic” (the target of our default manipulation), which was simply the block of time set aside four days per week during the early morning in September and October when the medical practice did nothing but flu shots, and regular doctor’s office visits that patients scheduled for another reason, such as checkups or medication checks. We examined the net effect the default manipulation had in terms of vaccinations occurring both as part of regularly scheduled doctor’s office visits and during early morning flu clinic appointments.
Second, we invited patients to complete a questionnaire on which they self-reported the site where they received a flu shot, be it at the suburban medical practice or an outside provider such as pharmacy or workplace. We examined whether the default manipulation increased the total vaccination rate or simply moved vaccinations from off-site venues to the flu clinic via the default vaccination appointments.
We randomly assigned patients who had visited the medical practice in the past 18 months (N = 886) to one of three conditions: opt in, opt out, or no information. We initiated the study at the beginning of the flu shot season (that is, the beginning of September). Patients in the opt-out condition received a letter informing them that the medical practice had prescheduled them for a flu shot during flu clinic hours at a specific early morning time and on a date sometime from late September to late October, but they could reschedule or cancel the appointment if they chose. Patients in the opt-in condition received a letter informing them that they could make an appointment during flu clinic hours if they wished. Those in the no-information condition received neither letter, but as with patients outside the study, they could, of course, make an appointment for a flu shot of their own accord during early morning flu clinic hours or receive one as part of a doctor’s office visit scheduled for another purpose. During the study, on the day before the scheduled appointment, the medical practice provided automatic reminder phone calls to all patients who had either self-made or default appointments. We tracked vaccination status through the consent forms that patients signed when they received a flu shot at the early morning flu clinic or during regular doctor’s office visits.
For all 886 patients in the study, we had data on whether they received an on-site (flu shot clinic) flu shot or a flu shot at a regular doctor’s office visit in the same practice up until March of the following year. To track flu shots received at other sites, we sent out a follow-up survey to all patients in mid-November asking them whether they had received a flu shot and, if so, where. (At the medical practice, 79% of all flu shots dispensed were given prior to mid-November, so our questionnaire responses likely miss only a small percentage of off-site vaccinations—that is, those received after the questionnaire date.) In all, 300 patients completed the follow-up survey. In addition, 278 of them consented to a medical chart review, allowing us to extract information on other health conditions they might have had.
Analyzing Default & Displacement Effects
A detailed description of analyses and results can be found in the online Supplemental Material. Here, we briefly report the main findings.
Flu Vaccination Behavior Data From Clinical Records
Because the medical practice required all patients to fill out a consent form immediately prior to receiving a flu vaccine, we had an accurate record of which participants were vaccinated at the medical practice, either during a stand-alone appointment at the special early morning flu shot clinic or during a doctor’s office visit. At the flu clinic (see Figure 1), the default opt-out intervention—giving people appointments without their asking for one—substantially increased the vaccination rate: 16% (47 out of 295) of those in the opt-out condition received a flu shot, compared with 5% (15 out of 296) in the opt-in condition and 2% (7 out of 295) in the no-letter condition. This represents a tripling of the vaccination rate or an 11% absolute increase.
Figure 1.
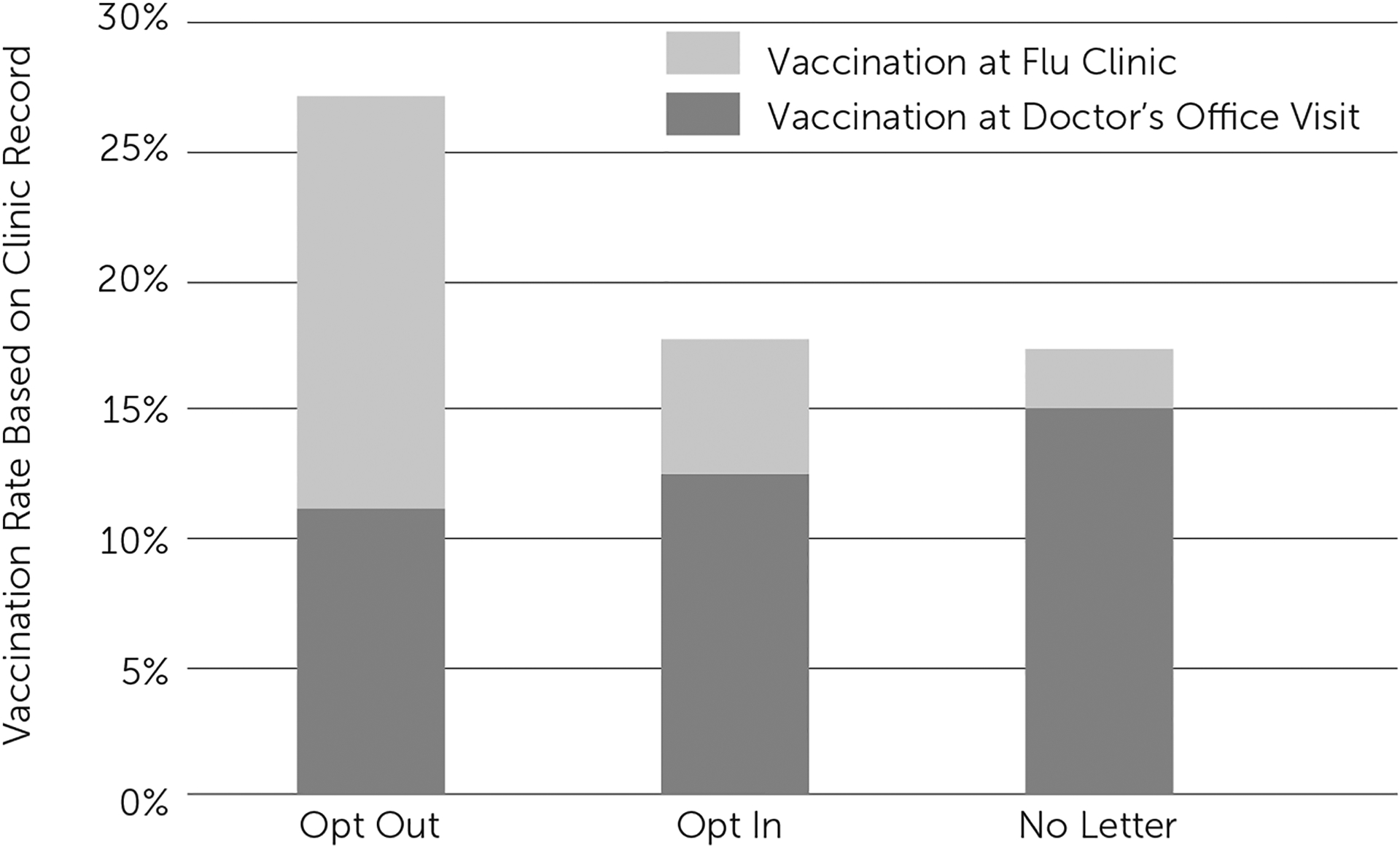
Percentage of patient participants who received a flu shot during early morning flu clinic appointments at the medical practice or at regular doctor’s office visits in the same medical practice
Vaccination data were based on the consent forms patients needed to fill out before receiving a flu shot at either site.
The size of this default effect compares favorably to the effect of offering a financial incentive for flu vaccination. In a 2016 study,9 researchers at Swarthmore College found that offering a $30 incentive to college students doubled vaccination rates from 9% to 19%, and a 2014 meta-analysis10 of the effect of patient financial incentives included two studies on vaccination, showing that incentives result in a relative increase in vaccination of approximately 32%.
It is notable that the increase in flu clinic vaccinations in the default opt-out condition did not come at the expense of doctor’s office visit vaccinations. The vaccination rate at doctor’s office visits (see dark gray section of bars in Figure 1) was 11% (33 out of 295), 13% (37 out of 296), and 15% (44 out of 295) in the opt-out, opt-in, and no-letter conditions, respectively. Although the vaccination rate in the opt-out condition seems slightly lower than the rate in the other conditions, this difference was not statistically significant, as one would expect if the opt-out condition were indeed shifting flu shots from office visits to the flu clinic.
Furthermore, as shown by the height of each bar in Figure 1, the total vaccination rate—that is, vaccinations at the flu clinic and regular doctor’s office visits—was higher in the opt-out condition than in the other two conditions: 27% of those in the opt-out condition were vaccinated at either site, compared with only 18% in the opt-in condition and 17% in the no-letter condition (see Figure 1). This suggests that the manipulation did not displace vaccinations from regular office visits to the flu clinic: it caused people who would not otherwise have received a flu shot to do so. This represents a 54% relative increase and a 10% absolute increase in vaccinations within the medical practice. The effectiveness of the default opt-out intervention did not vary with patient age, with whether the patient had been vaccinated in previous years, or with the presence of comorbidities (see the online Supplemental Material).
As shown in Figure 2A, only 44%, or 131 out of 295, opt-out patients cancelled their prescheduled appointments. The other 56% either rescheduled (n = 10) or did nothing (n = 154), meaning that they still had an appointment scheduled. In contrast, very few of the patients in the opt-in (5%, or 15 out of 296) and no-letter conditions (2%, or 7 out of 295) scheduled flu clinic appointments. Consequently, the percentage of patients who had a flu clinic appointment varied markedly across conditions.
Figure 2.
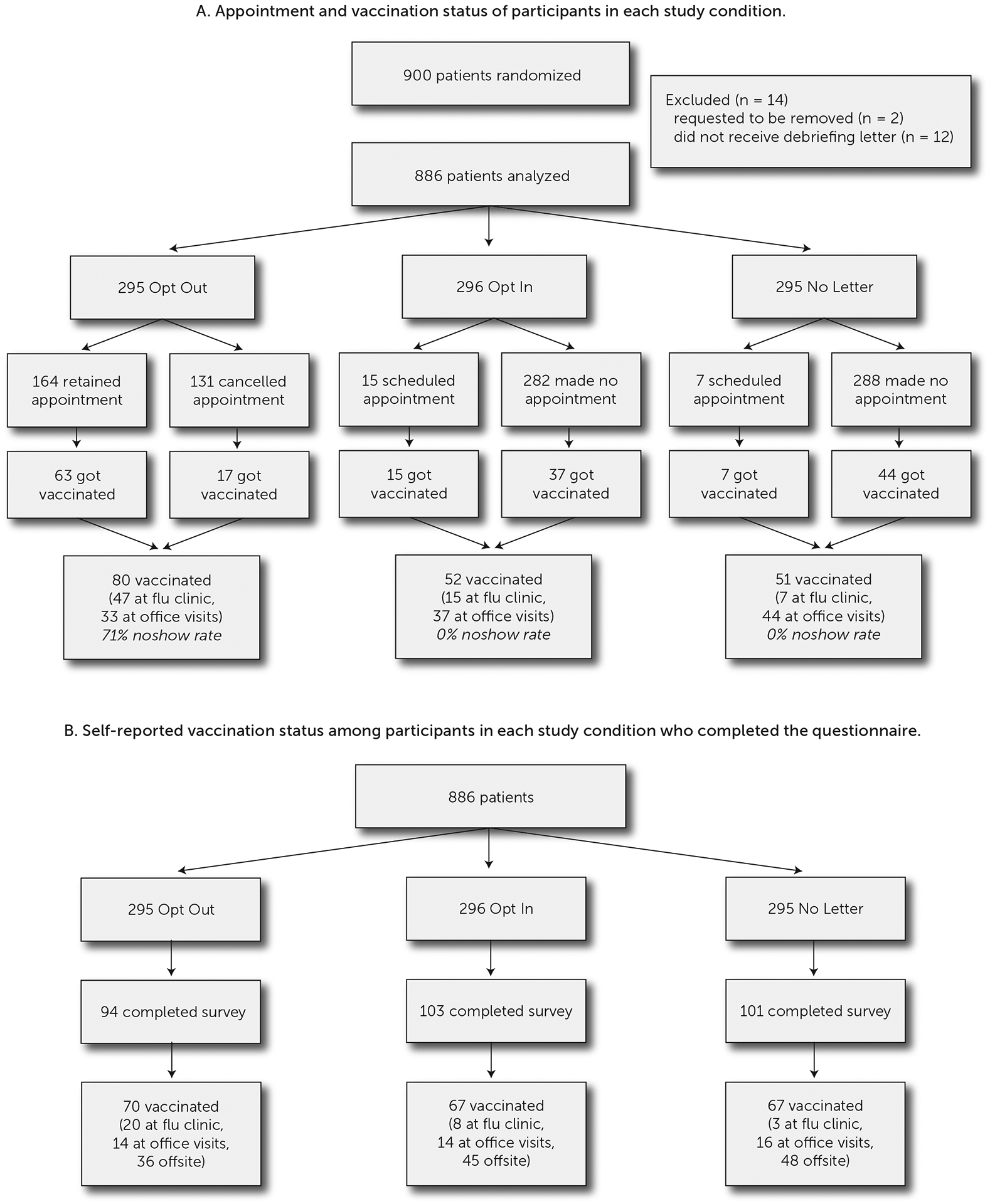
Flow of participants through the field experiment
Although participants in the opt-out condition were unlikely to cancel their appointments, more than two-thirds (71%) of them were no-shows for their default flu shot appointments, compared with a 0% no-show rate in the opt-in and no letter conditions. This very high no-show rate could place a heavy burden on a medical practice unless the practice is willing to overbook appointments.
Flu Vaccination Behavior Data From Self-Reports
On the follow-up questionnaire sent at the end of the flu shot season, 25% of participants reported receiving a flu shot at the medical practice (during either a flu clinic appointment or a doctor’s office visit) and another 43% reported receiving a flu shot elsewhere (such as in their workplace or at a pharmacy). The responses did not distinguish between vaccinations received at the early morning flu clinic and those received at a doctor’s office visit, but we were able to infer that distinction from clinic records (see the online Supplemental Material). Figure 3 shows the reported vaccination at the early morning flu clinic, doctor’s office visits at the medical practice, or elsewhere (see also Figure 2B).
Figure 3.
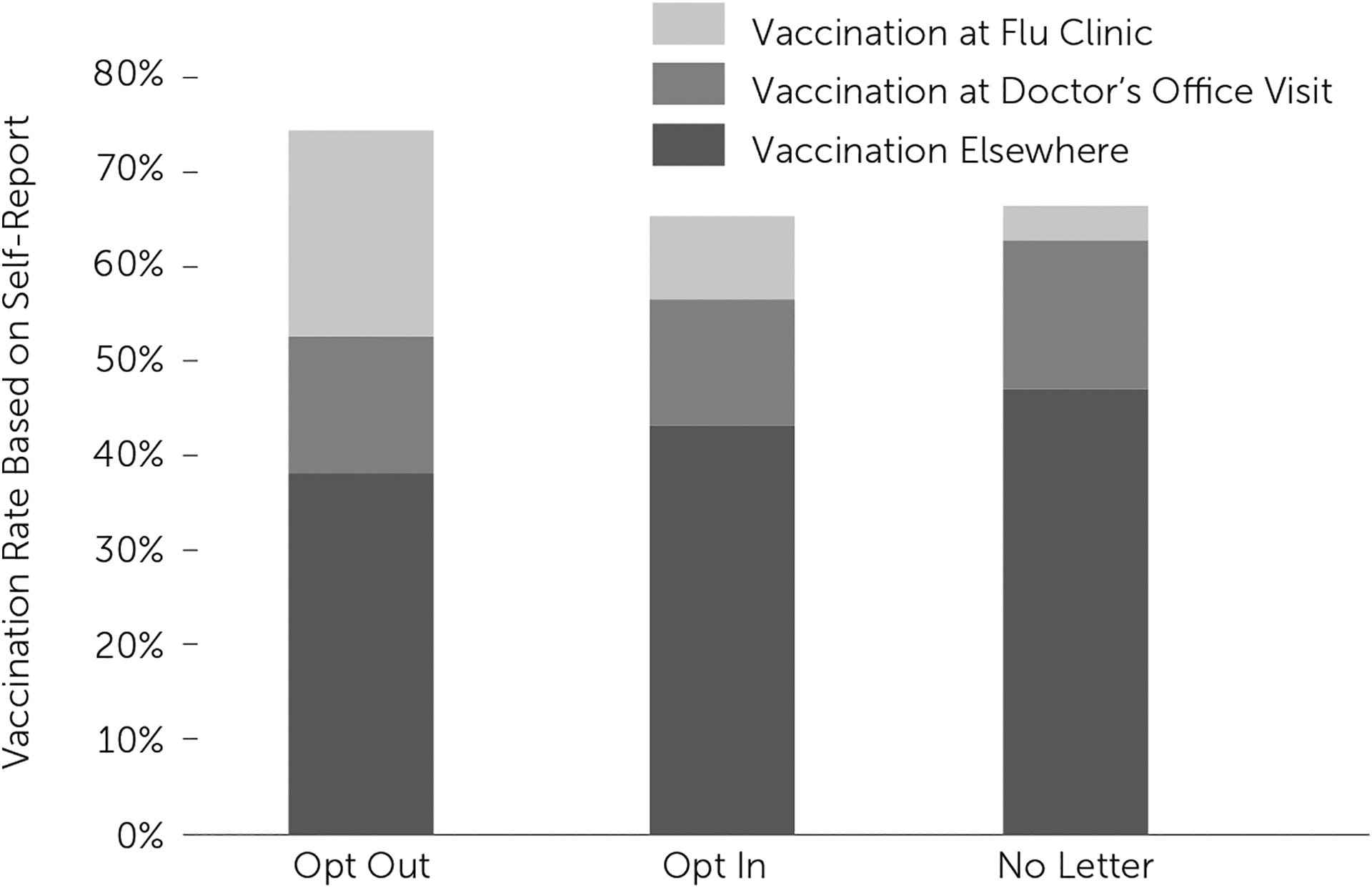
Percentage of patient participants completing the questionnaire (N = 298) who reported receiving a flu shot at the medical practice flu clinic, at regular doctor’s visits in the medical practice, or elsewhere
Default Appointments Do Not Displace Off-Site Vaccinations
Through the self-reports, we found that the default opt-out manipulation affected vaccinations received at the medical practice flu clinic: 21% (20 out of 94) of participants in the opt-out condition were vaccinated, whereas 8% (8 out of 103) and 3% (3 out of 101) in the opt-in and no-letter conditions were vaccinated, respectively.
If giving people default appointments for flu shots merely displaced vaccinations that they would have gotten somewhere else rather than increasing vaccination rates overall, then self-reports of vaccination elsewhere would decline. However, vaccination rates during doctor visits or elsewhere were similar across all three conditions (opt out, opt in and no letter): the slightly lower off-site vaccination rate in the opt-out condition as compared with the other two conditions was not statistically significant, suggesting that default opt-out appointments did not increase flu clinic vaccination rates at the expense of vaccinations elsewhere. That is, we did not find evidence of displacement.
After adding up the number of participants who reported receiving a vaccination at any location, we found a slightly higher net vaccination rate in the opt-out condition than in the other two conditions (see the online Supplemental Material for details), but the effect is not statistically significant (p = .13). The overall effect becomes significant when age and previous-year vaccination are controlled for (p = .04). Thus, we have no reliable evidence for displacement—that is, it does not appear that the opt-out intervention simply shifted vaccinations from one venue to another. In addition, the self-report questionnaire data give some indication that the opt-out intervention raised total vaccination rates.
Policy Implications
Notifying people about default flu clinic appointments that they could opt out of raised the vaccination rates at the clinic: patients in this condition, compared with patients in the opt-in and no-letter conditions, were more likely to have an appointment for a flu shot and more likely to get a flu shot at all locations. This benefit was equally likely to occur regardless of patient age, comorbidities, and previous vaccination history. It is important to note that this increase in vaccination rates was not the result of people simply getting flu shots at the flu clinic that they would otherwise have gotten at regular doctor’s office visits in the medical practice or elsewhere. If such displacement had occurred, we would have expected to see a lower rate of vaccination off-site and at doctor’s office visits in the opt-out condition than in the opt-in condition, but we found no such pattern.
Our results suggest that giving people opt-out appointments (that is, ones that they did not request but that they can cancel) is an effective way to increase vaccination rates, and this strategy does not merely shift vaccination from one venue to another. Although automatic appointments might be particularly useful for flu vaccinations, which are given each year during the same season, this policy tool might be used to encourage adherence with other types of vaccinations and other health behaviors that require an appointment. For example, pediatricians could encourage HPV vaccination (a pediatric vaccine with low uptake) by giving adolescents automatic appointments on the first available date following their 9th birthday. Dentists could automatically schedule patients for cleanings/check-ups six months after the previous cleaning/check-up, while radiology centers could automatically schedule women in their 50s for mammograms on dates two years after their previous mammogram.
It is important to point out that the benefits of default appointments that we found come with caveats. First, all patients with an appointment that they did not cancel received a phone call reminder the day before; that may have augmented the effectiveness of default appointments, which might be less effective at clinics that are unable to provide an automatic reminder call service. Another caveat is that there were many no-shows among opt-out patients: they neither cancelled nor kept the appointment they had been given. That could be quite burdensome for some clinics and pose a barrier to implementing automatically scheduled appointments. One solution could be to require that patients confirm prescheduled appointments if they wish to keep them.11 (Despite the high no-show rate, the opt-out group nevertheless had a higher vaccination rate than did the opt-in and no-letter groups, although that came at the cost of the clinic holding appointments for patients who did not keep them.)
A second limitation is that the effect of default appointments was quite localized. They increased vaccination rates at the dedicated flu clinic, because that was where the appointments were for, but they had no effect on vaccinations received at regular doctor’s office visits or off-site.
Practitioners can use these results by implementing opt-out appointments with a plan for how to handle the no-show rate. Policy-makers can facilitate the use of these findings by supporting infrastructure (such as patient scheduling software) that makes automatic appointments easier to implement. Future researchers should address whether requiring patients to confirm an automatic appointment retains the benefits of automatic appointments while reducing the no-show rate as well as ascertaining the optimal confirmation time frame. If the no-show rate can be addressed, then automatically scheduled opt-out appointments may contribute to the expansion of accountable care organizations by offering a cost-saving measure that promotes preventive care and reduces the spread of disease.
Our results have implications for the psychological mechanisms underlying the default effect. The findings suggest that the opt-out condition does not promote an overall positive attitude toward flu shots: if it did, one would expect the manipulation to increase the likelihood of vaccination at any site, not merely at the flu clinic. One proposed mechanism for the default effect is that defaults convey a social norm or policy recommendation.12 If such a mechanism underlies the current results, it must be very localized (for example, “my doctor wants me to get a flu shot at the clinic”) rather than more general (for example, “my doctor wants me to get a flu shot”). A more plausible account of the current results is that defaults have their effects because they save effort. It is easier for a patient to stick with the default appointment rather than switch to a different option; as a result, patients who have been automatically scheduled for an appointment often do not go to the trouble of canceling the appointment, whereas those without an appointment seldom exert the effort to make an appointment. Once the appointment is in place, the reminder phone call the day before brings attention to the appointment and may make many patients feel obligated to show up and get vaccinated.
Thus, we propose that vaccination appointment defaults alter what constitutes the course of least resistance, facilitating vaccination behavior without necessarily changing attitudes or perceived norms about vaccination. This type of intervention has the advantage of intervening on the behavior directly and thus being applicable to many types of patients. Such interventions that alter behavior without changing attitudes, however, also have the limitation of producing a localized effect. Sticking with the default saves effort, but the default only applies to the flu shot appointments. To be effective, the default manipulation would need to be implemented at the time and venue where the vaccination behavior was to occur. For example, a medical clinic would need to use automatically scheduled appointments every year rather than relying on an attitude change from a previous year to affect behavior in subsequent years. Making vaccination the easy course of action is an effective policy to increase vaccination rates. Automatic appointments and similarly aimed interventions, such as the recent increased availability of vaccines at retail pharmacies in the United States, likely target individuals who ordinarily would not get vaccinated because of inconvenience or complacency.13 Individuals with ideological objections to vaccination can cancel their automatically scheduled appointment or, more simply, not show up. Thus, automatically scheduled appointments both make clear the clinic’s preference for vaccination and maintain patient autonomy. Even though automatic appointments do not change attitudes, we believe their impact on increasing vaccination rates is critical to advancing public health, because vaccination protects not only the individuals immunized but also their social contacts, including those who refuse to be vaccinated.
Supplementary Material
Core Findings.
What is the issue?
New evidence suggests that scheduling patients by default for flu vaccinations does increase the net vaccination rate. In particular, there is no evidence that vaccinations are being displaced from one setting to another. Consequently, default scheduling can help reduce the $5.8 bn annual economic cost of flu, once higher no-show rates are controlled.
How can you act?
Selected interventions include:
Rolling out default scheduling into other preventative care services such as dental appointments and pediatric HPV vaccinations
Investing in research, and patient-scheduling infrastructure to reduce no-show rates
Who should take the lead?
Medical practitioners, public health policymakers, and behavioral science researchers
$5.8bn
estimated annual economic burden of flu in the US
10%
the absolute increase in vaccinated patients owing default scheduling
71%
of no-shows amongst patients with default appointments
Acknowledgments
This research was supported by National Institutes of Health Grant 1R01AG037943-01 to Gretchen B. Chapman.
Footnotes
Contributor Information
Gretchen B. Chapman, Psychology Department and Institute for Health, Healthcare Policy, and Aging Research, Rutgers University;
Meng Li, Department of Health and Behavioral Sciences, University of Colorado Denver;.
Howard Leventhal, Psychology Department and Institute for Health, Healthcare Policy, and Aging Research, Rutgers University;.
Elaine A. Leventhal, Institute for Health, Healthcare Policy, and Aging Research and Department of Medicine, Robert Wood Johnson Medical School, Rutgers University.
references
- 1.Centers for Disease Control and Prevention. (2016). Flu vaccination coverage, United States, 2015–16 influenza season. Retrieved from http://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm
- 2.Lu P, Bridges CB, Euler GL, & Singleton JA (2008). Influenza vaccination of recommended adult populations, U.S., 1989–2005. Vaccine, 26, 1786–1793. doi: 10.1016/j.vaccine.2008.01.040 [DOI] [PubMed] [Google Scholar]
- 3.Johnson EJ, & Goldstein D (2003, November 21). Do defaults save lives? Science, 302, 1338–1339. doi: 10.1126/science.1091721 [DOI] [PubMed] [Google Scholar]
- 4.Madrian BC, & Shea DF (2001). The power of suggestion: Inertia in 401(k) participation and savings behavior. Quarterly Journal of Economics, 116, 1149–1187. doi: 10.1162/003355301753265543 [DOI] [Google Scholar]
- 5.Thaler RH, & Sunstein CR (2008). Nudge: Improving decisions about health, wealth, and happiness. New Haven, CT: Yale University Press. [Google Scholar]
- 6.Chapman GB, Li M, Colby H, & Yoon H (2010). Opting in vs opting out of influenza vaccination. JAMA, 304, 43–44. doi: 10.1001/jama.2010.892 [DOI] [PubMed] [Google Scholar]
- 7.Lehmann BA, Chapman GB, Franssen FME, Kok G, & Ruiter RAC (2016). Changing the default to promote influenza vaccination among health care workers. Vaccine, 34, 1389–1392. doi: 10.1016/j.vaccine.2016.01.046 [DOI] [PubMed] [Google Scholar]
- 8.Roberto CA, Larsen PD, Agnew H, Baik J, & Brownell KD (2010). Evaluating the impact of menu labeling on food choices and intake. American Journal of Public Health, 100, 312–318. doi: 10.2105/AJPH.2009.160226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bronchetti ET, Huffman DB, & Magenheim E (2015). Attention, intentions, and follow-through in preventive health behavior: Field experimental evidence on flu vaccination. Journal of Economic Behavior & Organization, 116, 270–291. doi: 10.1016/j.jebo.2015.04.003 [DOI] [Google Scholar]
- 10.Giles EL, Robalino S, McColl E, Sniehotta FF, & Adams J (2014). The effectiveness of financial incentives for health behaviour change: Systematic review and meta-analysis. PLOS ONE, 9(3), Article e90347. doi: 10.1371/journal.pone.0090347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldstein DG, & Dinner IM (2013). A fairly mechanical method for policy innovation. In van Trijp HCM (Ed.), Encouraging sustainable behavior: Psychology and the environment (pp. 55–68). New York, NY: Psychology Press. [Google Scholar]
- 12.McKenzie CRM, Liersch MJ, & Finkelstein SR (2006). Recommendations implicit in policy defaults. Psychological Science, 17, 414–420. doi: 10.1111/j.1467-9280.2006.01721.x [DOI] [PubMed] [Google Scholar]
- 13.Betsch C, Böhm R, & Chapman GB (2015). Using behavioral insights to increase vaccination policy effectiveness. Policy Insights from the Behavioral and Brain Sciences, 2, 61–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


