Abstract
Achilles tendinopathy (AT) is one of the most frequent overuse injuries in the ankle. The evidence base for its conservative management AT continues to evolve, but there is still a gap in the evidence for the efficacy of any modality of treatment in high-quality studies. This systematic review and meta-analysis investigated the efficacy of EE in improving pain and function in adult patients with mid-portion Achilles tendinopathy compared to other forms of exercise. A search was performed in PubMed, BIREME, SportDiscus, Cinahl, Web of Science and PEDro, in November 2022. The methodological quality was evaluated using the Risk of Bias 2 tool (RoB2) of the Cochrane collaboration, and the meta-analysis was performed using the Review Manager 5.1 program. 2024 articles were identified and eight fulfilled the inclusion criteria. RoB2 presented a final score with 62.5% of the studies presented “some concerns”, and 37.5% (five and three articles, respectively) presenting “high risk” of bias. EE was effective for the managment of AT. The only variable for which a meta-analysis was possible was pain (five articles), analysed with the visual analogue scale/numerical visual scale. The mean difference (MD) in treatment effect using EE was − 1.21 (− 2.72 to − 0.30) with a 95% of confidence interval (CI), thus identifying a significant positive effect for the improvement of pain in patients with AT in whom EE was used. EE is effective in the management of AT. The meta-analysis shows the need for appropriately powered randomized controlled trials with better design, the use of standard outcome measures and well-planned protocols for conservative management of AT.
Level of evidence: Level 1.
Registration: CRD42018118016.
Keywords: Ankle injuries, Achilles tendinopathy, Review, Physiotherapy modalities, Exercise therapy
Introduction
The Achilles tendon is one of the widest and strongest tendons in the human body. Despite this, injuries are common [1]. Achilles tendinopathy (AT) is one of the most frequent overuse injuries in the ankle and foot [2–4], and is a clinical syndrome characterized by pain, swelling and loss of function [5].
AT has an incidence of 1.85 per 1000 people in the general population [5, 6]. Most individuals with AT are active, and involved in recreational or competitive sports [7, 8]. For example, runners have an annual incidence of 10%, with a higher chance of developing AT symptoms compared to non-runners younger than 35 years [7, 9]. AT can be present in 51/100 of athletes in whom running is part of their sport [8].
Basketball, soccer, tennis and wrestling have high incidence rates of ankle injuries [10, 11]. Up to 27% of all musculoskeletal injuries in athletes' are foot and ankle injuries, with the highest incidence in female gymnastics, female soccer and male and female cross-country runners [12]. However, up to one in three sedentary individuals can develop AT [6].
Abnormal biomechanics of the lower limb may increase the risk of excessive or unusual loading of the Achilles tendon, and changes in range of motion (ROM) of the ankle and lower limb have been associated with an increased risk of AT [13]. In most AT patients, the condition improves with simple conservative interventions, the first line management option, which can be combined with a variety of other agents [14–16]. Surgery is generally undertaken when appropriately conducted conservative management has failed [17].
Conservative therapies for the management of AT include kinesiotherapy, electrotherapies, cryotherapy, dry needling, bandaging, splints[18–21]. Exercise programs are the most widely studied interventions for the management of AT, and eccentric, concentric, isometric, and isokinetic contractions have all been used, alone or in combination [15, 22–26]. In 2012, a systematic review with a meta-analysis [23] in relation to physical therapy in AT identified 23 publications: eccentric exercise (EE) was shown to be an effective intervention to manage AT [23]. More recently, other studies have shown the efficacy of EE for the management of AT [15, 16, 27–29].
In eccentric exercise, the muscle contracts while being lengthened [30]. Eccentric contractions not only produce the highest forces in the muscle compared to concentric or isometric contractions, but are also energy efficient [31]. The most frequently described protocol focuses on a progressive eccentric strengthening with increasingly heavier loads [32]. Van der plas et al. [33] evaluated EE for 3 months at 5 years of follow-up: EE is effective in increasing function and controlling pain symptoms. Roos et al. [34] concluded that EE reduces pain and improves function in AT patients, and more patients in the EE group returned to their sport after 12 weeks than the other groups.
The prognosis of AT may vary from individual to individual. Paavola et al., in a 8-year follow-up study, showed that 84% of the patients returned to their pre-disease activity levels, and 94% of the patients were asymptomatic or had only minimal pain [17].
The evidence base for conservative therapy for AT continues to evolve, but there is still a gap in the evidence for its effectiveness in high-quality studies. We performed a systematic review and meta-analysis to investigate the efficacy of EE in improving pain and function in adult patients with mid-portion Achilles tendinopathy compared to other forms of exercise.
Methods
The protocol for this review was registered in the International prospective register of systematic reviews—PROSPERO, number CRD42018118016, the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and the AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews) were used.
Searches
The search was performed in PubMed, BIREME, SportDiscus, Cinahl, Web of Science and PEDro without date restriction filter. Table 1 shows the search strategy relationship, which was adapted for use in other databases.
Table 1.
Keywords of the search strategy of the electronic databases
| Search | PubMed/sportdiscus/cinahl/web of Science | PEDro | BIREME |
|---|---|---|---|
| #1 | Achill*(.tw) | achill* | Achill* |
| #2 | Triceps surae(.tw) | tendin* | Triceps surae |
| #3 | Tendin*(.tw) | eccentric* | Tendin* |
| #4 | Heel(/) | concentric* | Heel |
| #5 | 1 OR 2 OR 3 OR 4 | exercise | Pain |
| #6 | Pain(/) | Function | |
| #7 | Function(.tw) | Physical therapy | |
| #8 | 6 OR 7 | Physiotherapy | |
| #9 | 5 AND 8 | Exercise therapy | |
| #10 | Physical therapy(.tw) | Exercise | |
| #11 | Physiotherapy(.tw) | Rehabilitation | |
| #12 | Exercise therapy(.tw) | Concentric* | |
| #13 | Exercise(/) | Eccentric* | |
| #14 | Rehabilitation(/) | Strength training | |
| #15 | Concentric*(.tw) | Strengthening | |
| #16 | Eccentric*(.tw) | Resistance training | |
| #17 | Strength training(.tw) | Randomized controlled trial | |
| #18 | Strengthening(.tw) | Controlled clinical trial | |
| #19 | Resistance training(/) | Randomized controlled trials as topic | |
| #20 | 10 OR 10 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 | Trial | |
| #21 | Randomized controlled trial(/) | Placebo | |
| #22 | Controlled clinical trial(/) | ||
| #23 | Randomized controlled trials as topic/ | ||
| #24 | Trial(.tw) | ||
| #25 | Placebo(.tw) | ||
| #26 | 21 OR 22 OR 23 OR 24 OR 25 | ||
| #27 | 9 AND 20 AND 26 | 1 ADN 2 AND 3 AND 4 AND 5 | 1 AND 2 AND 3 AND 4 AND 5 AND 6 AND 7 AND 8 AND 9 AND 10 AND 11 AND 12 13 AND 14 AND 15 AND 16 AND 17 AND 18 AND 19 AND 20 |
*Truncation (search term starting with the letters preceding the asterisk)
.tw, text word; /, Mes
Following identification of the articles which matched the inclusion and exclusion criteria, their references were manually searched to identify other possible articles to be included in the present study.
Study inclusion and exclusion criteria
As randomized clinical trials (RCT) are the gold standard to assess the effectiveness of clinical research [35], we included RCT with eccentric exercise performed in adult patients (older than 18 years) with mid-portion Achilles tendinopathy in whom a programme of eccentric exercises was compared to another conservative modality, and in whom the outcome measure was assessment of pain and/or disability. Regarding the studies selection, we were interested in identifying the effects and harms associated with an intervention. Hence, RCTs were chosen because they can provide a complete overview of the efficacy of a given intervention.
We did not include studies reporting on participants with ruptured Achilles tendon or with insertional tendinopathy. The search was limited to human studies and published in Portuguese, English or Spanish, due to the language capabilities of the researchers. In addition, review articles, expanded abstract, letters to the editor, annals of congress, editorials, dissertations and theses were excluded.
Data extraction
The following information was extracted: basic information (author, published year, country, trial design, subject characteristic, sample size, intervention duration, basic results); and outcome measures (primary—pain and function; secondary—strength and range of movement). The search was performed by two researchers independent of each other. If there was disagreement, a third reviewer was consulted for final decision. Data were exported and stored in the Zotero® program, where duplicate articles were excluded. The data were then exported to Microsoft Excel®, where articles were removed according to their titles, followed by their abstract, and then the remaining articles were read in full text. Relevant data were then extracted manually and inserted into Review Manager software (RevMan 5.3).
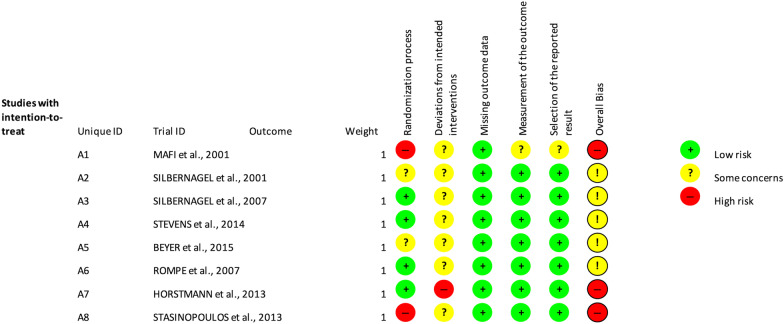
Study quality assessment
The Cochrane Collaboration risk-of-bias 2 (RoB 2) tool for randomized trials was used to assess the risk of bias in the included studies [36]. The tool is structured into five domains through which bias can be introduced. The domains cover all types of trends that may affect the results of randomized trials namely: (1) bias arising from the randomization process; (2) bias from deviations from intended interventions; (3) bias from missing outcome data; (4) bias in measurement of the outcome; (5) bias in selection of the reported result. The answer options for the questions are: yes; probably yes; probably no; no; and no information. Responses to questions provide the basis for domain-level judgments about risk of bias, and then these domain-level judgments provide the basis for a general risk of bias judgment for the outcome of the study being evaluated. The possible judgments of risk of bias are: (1) low risk of bias; (2) some concerns; and (3) high risk of bias [36].
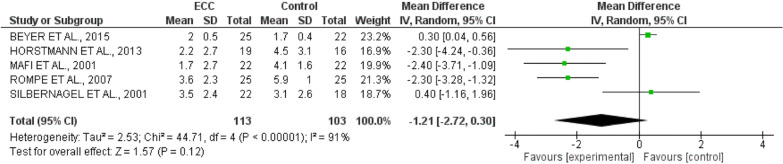
Data synthesis and presentation
A meta-analysis was performed to synthesize study data and verify the effect size of the intervention using the RevMan 5.3 program. The results of the meta-analyses are presented in a forest plot, where the left side positively represents the treatment (less than zero) and the right side negatively (greater than zero). We used for the meta-analysis an effect model with a justification of the same AT population, and a mean difference as the type of effect size. Each study is shown with its effect size and the corresponding 95% confidence interval [37, 38]. The general measure of the effect is represented by a diamond: its centre represents the overall estimate, and the width or side points indicate general confidence intervals [39]. Heterogeneity was tested by p value and I2. If p > 0.10 and I2 < 50%, the heterogeneity was considered low enough to conduct a meta-analysis with a fixed-effect model. If p < 0.10, I2 > 50%, there was a high level of heterogeneity, and a random effect model was used. Sensitivity analysis was conducted by one-by-one exclusion method for individual studies. Descriptive analysis was performed if the heterogeneity was too large (I2 > 85%).
Results
Search results
A total of 2024 articles were identified among the published articles to the time when the search was performed, with the last update in November 2022. After all stages of the review, 16 articles remained for complete analysis. Studies were excluded after the full-text screening for the following reasons: protocols [40]; comparison group without an exercise protocol [34, 41–43]; follow-up studies [33, 44]; full text not found [45]; both tendinopathy of the main body and insertional tendinopathy included in the study or not reported [46, 47]. Therefore, eight articles fulfilled the inclusion criteria. No article was identified through the manual search in the references section. A total of 8 studies were eventually included in the present study (Fig. 1). The studies were conducted in seven different countries: Sweden [48–50] and Germany [51, 52] with one each in Greece [53], Scotland [54] and Denmark [55] respectively.
Fig. 1.
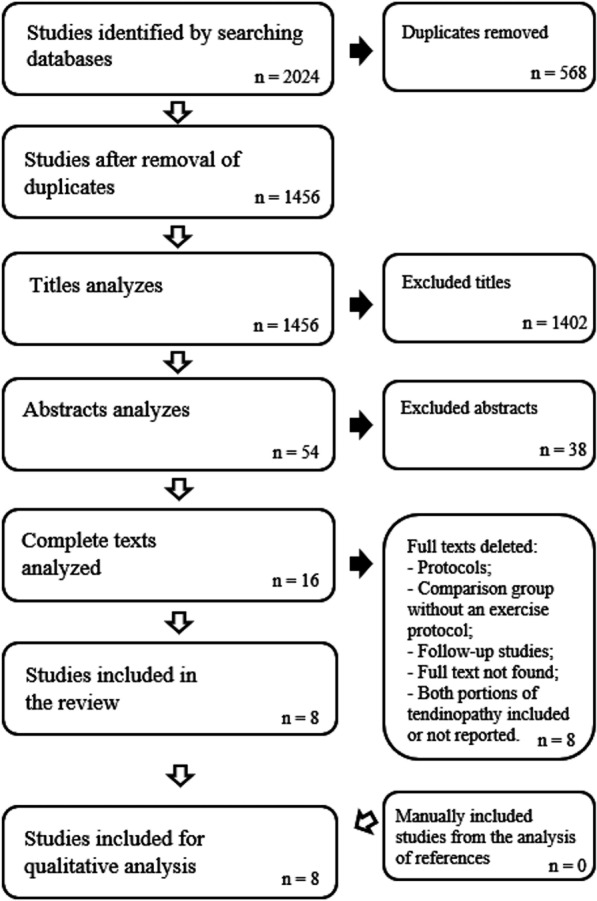
Flow chart of the literature search
Participants
The included studies reported a total of 401 Achilles tendons in 371 patients; two studies included individuals with bilateral and unilateral AT [49, 50]. Clinical examination (7/8) was the most common criterion for the diagnosis of AT [48–50, 52–55]; three studies used ultrasound [48, 51, 55], and one [55] added the VISA-A questionnaire and the VAS pain scale to complete the diagnosis. All studies included only patients with tendinopathy of the main body of the Achilles tendon. The minimum duration of symptoms was of three months. The participants' ages ranged from 19 to 77, with a mean of 46.6 years. Male participants were 54.2%, and 45.8% were females in the articles that reported the gender, with one article [53] not reporting the sex of the participants.
The samples per study group ranged from 13 to 25 participants, with a mean of 18.5 individuals in each group.
Interventions
All studies were clinical trials. Six studies included two intervention groups: one was eccentric exercise (EE), compared to another exercise modality, such as concentric exercise [48]; light training [49]; heavy slow resistance (HSR) [55]; and with another protocol of eccentric exercise [50, 53, 54]. Two articles included three groups: EE, electrotherapy and wait-and-see [51] and EE, vibration training and wait-and-see [52]. Most studies (75%) applied the intervention for 12 weeks, but Silbernagel et al. [50] extended the intervention to six months if symptoms persisted. Stevens et al. [54] undertook the intervention for 6 weeks. In addition, all articles evaluated change in pain; seven verified function/disability [49–55]; and three, patient satisfaction with treatment [48, 54, 55].
Comparison and outcome measure
Five of the eight studies used the VISA-A scale to assess pain and symptoms [50, 51, 53–55], two used functional tests (jump tests, toe-raise test, hop test, side-step test) [49, 50], one used isokinetic strength [52], and two assessed ROM [49, 50]. Only one study [53] also used the VISA-A to evaluate pain evolution. The other articles used the Visual Analogue Scale/Numerical Visual Scale (VAS/NVS). Most of the articles performed the evaluations at the beginning and at the end of the treatment, with one study undertaking follow-up at 36 weeks [53], one at 6 months [49], and three at 1-year of follow-up [50, 51, 55]. Four studies showed better outcome in the EE treatment group [48, 49, 51, 52], one article did not present statistically significant differences [55]. Among the three articles comparing two eccentric exercises protocols, one study presented better results with the Alfredson protocol [53], and two studies did not find statistically significant differences between groups [50, 54] (Table 2).
Table 2.
Source: Own author/2019
| Study | Intervention(s) | Sample size | Gender (M/F) | Age (mean) | Intervention duration (wk) | Comparison and outcome measure | Study conclusions (p value/SMD—95% CI) |
|---|---|---|---|---|---|---|---|
| Eccentric exercise vs another exercise therapy or rest/wait-and-see | |||||||
| Mafi 2001 | EE | 22 | 12/10 | 48.1 ± 9.5 | 12 | VAS | The results after treatment with EE was significantly better (p < 0.002) than the results of treatment with the concentric training regimen; Between groups comparisons of pain not presented |
| Concentric exercise | 22 | 12/10 | 48.4 ± 8.3 | ||||
| Silbernagel 2001 | Eccentric overload training; | 22 | 17/5 | 47 ± 14.7 | 12 |
VAS Jumping test; toe-raise test |
Eccentric loading had better strength and pain outcomes (p < 0.05) |
| Light training | 18 | 14/4 | 41 ± 10.2 | ||||
| Beyer 2015 | EE | 25 | 18/7 | 48 ± 2 | 12 |
VISA-A VASH VASR |
VISA-A: there was no significant interaction (p = 0.26) or difference between groups (p = 0.62). VASH and VASR there was no significant interaction (VASH, p = 0.08; VASR, p = 0.38) or difference between groups (VASH p = 0.77; VASR, p = 0.71). Similar treatments |
| HSR | 22 | 14/8 | 48 ± 2 | ||||
| Rompe 2007 | EE | 25 | 9/16 | 48.1 ± 9.9 | 12 |
1 vs 3 VISA-A VNE |
VISA-A and VNE: Patients from group 1 achieved significantly better results than patients from group 3 (p < 0.001) |
| SWT | 25 | 11/14 | 51.2 ± 10.2 | ||||
| Wait-and-see | 25 | 9/16 | 46.4 ± 11.4 | ||||
| Horstmann 2013 | Vibration training | 23 | 13/10 | 46.0 ± 6.9 | 12 |
2 vs 3 VAS Isokinetic |
Pain improvements were greater in the EE groups than in the wait-and-see group (– 27.0; 95% CI –50.9, – 3.1) |
| EE | 19 | 10/9 | 45.7 ± 8.5 | ||||
| Wait-and-see | 16 | 9/7 | 44.4 ± 7.7 | ||||
| Silbernagel 2007 | EE | 19 | 12/7 | 44 ± 8.8 | 6–52 |
VISA-A-S VAS Jump tests, strength tests, endurance test |
Both groups showed significant (p < .01) improvements on the VISA-A-S score and decrease in pain during hopping at 6 weeks and at 3, 6, and 12-month evaluations |
| EE + active | 19 | 8/11 | 48 ± 6.8 | ||||
| Stasinopoulos 2013 | Stanish protocol | 21 | NR | 48.44 ± 5.12 | 12 | VISA-A | VISA- A: there were significant differences in the magnitude of improvement between the groups at weeks 12 and 36 (p < 0.05) |
| Alfredson protocol | 20 | 48.24 ± 5.09 | |||||
| Stevens 2014 | Alfredson protocol | 15 | 6/9 | 48.2 ± 10.8 | 6 |
VISA-A VAS |
The between-group difference change score was not statistically significant at week 6 for VISA-A (ITT, p = 0.20; PP, p = 0.32) and VAS (ITT, p = 0.14; PP, p = 0.73) |
| Alfredson protocol (do-as-tolerated) | 13 | 5/8 | 49.2 ± 11.3 | ||||
SMD, standard mean difference; M, male; F, female; NR, not reported; CI, confidence interval; EE, eccentric exercise; VAS, visual analogue scale; VISA-A, Victorian Institute of Sports Assessment-Achilles; HSR, heavy slow resistance; VASH, visual analogue scale heel rises; VAS, VAS, visual analogue scale running; SWT, shock-wave therapy; VNE, visual numerical scale; VISA-A-S Victorian Institute of Sports Assessment-Achilles Swedish; ITT, intention-to-treat; PP, per-protocol
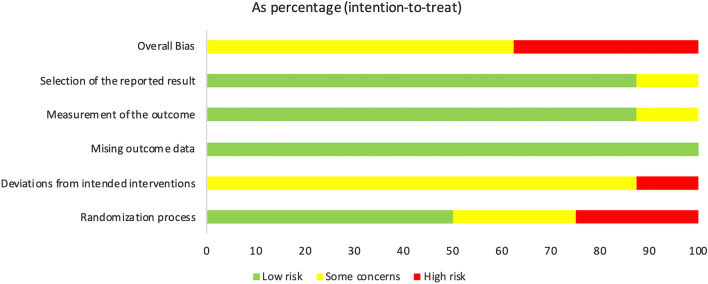
Risk of bias
Figures 2 and 3 highlight the variability between the articles included and show the general score about the methodological quality. Figure 2 shows the risk of bias for each article in each domain analysed by the program. Figure 3 shows a general comparison between low risk, some concerns and high risk in each domain.
Fig. 2.
Variability of articles in relation to fundamental methodological considerations
Fig. 3.
Methodological quality summary: analysis of the authors' judgments about each item of methodological quality for each included study
Allocation
Regarding allocation of participants, 50% of the studies presented “some concerns” or “high risk” as they did not report details about how randomization and/or allocation to the various groups were performed [48, 49, 53, 55]. Four articles had adequate allocation concealment, including central randomization methods [50–52, 54].
Blinding
No studies reported blinding of the participants, health care professionals who administered the treatment, and evaluators, presenting a low-risk score. One study did not present information about participants and health care professionals who administered the treatment [49]; the patients were aware of the treatment or no information was presented in four studies [48, 50, 53, 54]; the health care professionals who administered the treatment knew or probably knew about the treatments in six articles [48, 50–53, 55]. All except of one of them had blind evaluators [48].
Missing results data
All the articles presented the missing data reporting the reasons of exit from the study or exclusion from the intervention, being judged with low risk of bias.
Evaluation of results
Seven of the eight studies presented evaluation of appropriate results, with “low risk”. Only one study presented “some concerns” [48] for non-blinding the evaluators. None of the selected articles showed “high risk” of bias.
Selection of the reported result
Only two articles did not provide evidence of previous protocols published in study databases [49, 52], and one article presented only data for the intervention group [48]. This one study, however, did not present the statistical analysis performed, being thus judged with “some concern”.
Overall bias
Regarding the final score of risk of bias assessment, 62.5% of the studies presented “some concerns”, and 37.5% presented “high risk” of bias.
Meta-analysis
Only a meta-analysis with pain data was performed including a total of five studies. All of them used VAS/NVS to measure pain, and compared the EE with another conservative treatment (Fig. 4). The analysis of heterogeneity resulted in the I2 value of 91%, showing heterogeneity between the studies. A meta-analysis with I2 higher than 75% should use the Random Effect Model. The Mean Difference (MD) found in the treatment effect was − 1.21 (− 2.72 to − 0.30), with 95% confidence interval, with a significant positive effect for the treatment of pain in Achilles tendinopathy with eccentric exercise, with the result in favour of EE compared to CG or other exercises in pain improvement.
Fig. 4.
Meta-analysis for pain intervention with EE
Discussion
The present systematic review and meta-analysis investigated the efficacy of EE in improving pain and function in adult patients with mid-portion Achilles tendinopathy compared to other forms of exercises. The present systematic review and meta-analysis showed that EE is effective in improving disability and pain in AT patients. In the eight studies evaluating the effect of pain and disability of EE with another type of exercise, four presented favourable EE results for pain [48, 49, 51, 52], and one presented similar results between interventions [55]. Regarding the effect on disability, two articles were in favour of EE [49, 51].
The Victorian Institute of Sport Assessment-Achilles questionnaire (VISA-A) was the most commonly used outcome instrument (used in five of eight investigations) in the studies assessing disability. This questionnaire is used as an outcome measure in both research studies and in the clinical setting, and it evaluates function, activity limitation or participation restriction, in addition to documenting pain and stiffness [15]. Two studies used functional tests, the hop and heel-raise endurance tests being the most common. These tests should be used as part of the evaluation, are useful to assess progress during rehabilitation, and are often used to detect changes over time [15, 56]. Among the studies that evaluated pain, the visual analogue scale/numerical visual scale were the most commonly used (seven of eight). One study [53] used the VISA-A questionnaire to evaluate pain and function. Visual scale values can be used to track the progression of pain in a single patient, or to compare pain among patients with similar conditions [57]. While there is conflicting evidence regarding the advantage of EVA/NVS compared to other pain recording methods, it is still commonly used in clinical and home settings [58, 59].
EEs improve muscle function, possibly through their favourable effects on neural impulse and other health-related factors, and do not produce clinically relevant adverse effects [60–62]. EE may promote the formation of appropriately oriented collagen fibers in the tendon, which may facilitate remodelling of the tendon [63]. A meta-analysis [23] supports the use of EE for AT, and additional benefits can be produced when EE is used in conjunction with laser therapy.
Eccentric exercises have been tested against concentric exercise; rest/wait-and-see; light training; heavy slow resistance; or another eccentric exercise protocol. There is a wide variation between the trials regarding interventions, methods, times of evaluation of the results, and selection of the reported results.
One study investigated EE and concentric exercise. This study [48] found improvement in pain and function/return to activity in both groups, with the EE producing significantly better results. Mafi et al. [48] suggested that EE produced significantly better results than concentric exercises because of the energy efficiency of eccentric exercises on the calf muscles, with comparable muscle force developed at lower loads on the tendon during movement. In addition, EE may produce changes in the metabolism of neural transmission in the tendon, inducing alterations in the perception of pain. This corroborates Yu et al.’s [46] report that EE is more effective than concentric exercises in reducing pain, increasing muscle strength and endurance, and improving function. However, the small sample does not allow generalization of the results [64].
Two studies compared EE with rest/wait-and-see. Rompe et al. [51] verified improvement in pain and function of the EE group, which, despite not presenting a statistical difference, showed considerably better results than the control group. They report a successful outcome in the EE group of 50 to 60% of patients, reporting that eccentric training is inexpensive, although it is technique dependent. The wait-and-see protocol was the most convenient and easy intervention to implement, but also the least effective [51]. Horstmann et al. [52] showed significant improvement in the EE group compared to the control group, in addition to a significant reduction in pain on palpation of the EE group. While interventions improved pain two cm proximal to the insertion of the Achilles tendon in the calcaneus, only EE reduced pain at the musculotendinous junction as well. They reported that pain reductions following eccentric training correlated with reduction in neovascularization in patients with tendinopathy, although such changes in vascularization were not actually observed.
As in several studies with active versus rest/wait-and-see treatment, individuals receiving active treatment may have higher expectations about the effects of treatment, and testing different intensity exercises against a rest/wait- and-see can lead to bias in the conclusions [65, 66].
Silbernagel et al. [49] compared light training (eccentric plus concentric) and EE, and verified improvement in palpation, walking and activity pain, as well as improvement in functional tests and ROM for the EE group, with no statistically significant difference between the groups. The reason for improvement in the experimental group may be multifactorial, in addition to being explained by the different components of the treatment protocol used by the experimental group, such as the information provided, the exercise program, and the pain monitoring model. The authors also report that the exercise load has to be relatively high for better results [49]. Beyer et al. [55] presented a comparison of the EE and HSR groups. Both interventions showed significant gains in improving physical activity and pain, but without statistical difference between groups: the treatments are similar to each other, although patient satisfaction tended to be higher after 12 weeks with HSR (100%) than EE (80%). This may explain why these two studies [49, 55] are more towards the right side of the forest graph. Silbernagel et al. [49] further state that the experimental group had an increase in pain in the first weeks of treatment, and that this may resulted from the increased load. Both treatments improved symptoms and physical activity level equally well in patients with chronic midportion AT [55]. Eccentric and concentric contractions produce similar collagen expression, which may indicate that fibroblasts are similarly affected. Furthermore, training with concentric and eccentric contractions can produce similar tendon changes. The authors state that they cannot answer the question regarding the mode of contraction, but both treatments promoted similar results. Kongsgaard et al. [67] compared EE and HSR for patellar tendinopathy, with similar results between the interventions: it is possible that the combination of eccentric and concentric exercise may explain the advantageous effects of HSR [67].
Three studies compared EE with EE. The first [50] applied the same treatment protocol, but only one group was released for physical activity. Both groups presented improvement in pain and function during the evaluations, with no statistically significant differences between the groups. The study demonstrated no negative effects in patients who continued physical activity (such as running and jumping) when using pain monitoring during rehabilitation and believe that important factors in tendon improvement are intensity and type of load. The underlying effects of exercise are not fully understood, but the mechanical load on the tendons seems to be important both in the healing process and in the increase in tendon strength. The second study [53] compared Alfredson’s and Stanish’s protocols. The former reduced pain and improved function to a greater extent than the latter. The protocol developed by Alfredson et al. [32] is a program of eccentric exercises to treat the AT, while the uninjured limb is used to return (concentrically) to the initial position. The protocol recommends the completion of 180 eccentric repetitions per day, and has been widely adopted in research and clinical practice [32, 40]. Stanish et al.’s [68] protocol for the management of AT includes eccentric and static stretching exercises and is based on three principles. (1) length; (2) load; and (3) contraction velocity. According to the study authors [53], the protocol by Alfredson et al. [32] reduced pain and improved function more efficiently because patients exercised both calf muscles (gastrocnemius and soleus) only eccentrically, with more series and with more repetitions every day for the same treatment period [53]. In addition, the load of EE in the Alfredson’s protocol was increased according to the patients' symptoms, and the exercises were performed at low speed, which is supposed to allow suitable tissue adaptation [53].
The third study applied only the Alfredson protocol [54]. One group was asked to perform 180 repetitions, and the other performed until tolerated. A statistically significant difference was found for improvement in function in each group at three weeks and for pain in the “do-as-tolerated” group; statistically significant differences between the groups in improvement of function were evident at week three, but by six weeks there was no statistical differences between the groups for pain and function. Regarding the outcomes, given the limits of the scoring systems used, the "do-as-tolerated" regime can equal or even exceed the standard protocol. In addition, defining a dosage may be important for rehabilitation, suggesting that a clinical predictor based on worsening symptoms may be used by patients who have demonstrated optimal clinical improvements. This may be a potential benefit to improve self-efficacy, which has been associated with positive results for the treatment of musculoskeletal conditions [54]. However, as the exercises were only performed for a period of 6 weeks, and the follow-up measurements in the medium and long term (> 6 weeks) were not presented, these conclusions should be interpreted with caution.
This systematic review and meta-analysis focused only on studies comparing EE with another type of exercise or control group (rest/wait-and-see). One of the most interesting findings lies on the favourable results produced by this type of exercise, suggesting that EE should be an integral component of AT management. Also, the rest/wait-and-see approaches do not provide any significant benefits when compared to EE. In addition, controlled tendon loading can continue during the intervention, though further studies are needed to determine which activities are beneficial, and their frequency and intensity are recommended.
The present review has identified several characteristics that should be adopted for future clinical trials. With "some concerns" and "high risk" through the risk of bias, new randomized clinical trials should be performed and adhere to the recommendations of CONSORT [69]. In addition, specific, valid and reliable outcome measures should be used [15], facilitating comparisons between different studies and when performing systematic reviews and meta-analyses.
We are aware of the limitation of the present investigation. Only one meta-analysis was performed, namely on pain, since it was not possible to group more than two studies for disability analysis. It is necessary to collate a larger number of studies to achieve greater statistical power [70]. In addition, there is a substantial need for studies with larger sample size, greater details of the sample and the proposed interventions, as well as better methodological modalities and a planned design. Another limitation would be that half of the selected articles presented at least some risk of bias in relation to randomization. Ultimately, most of the articles analysed present some concerns such as heterogeneity of the study population, and lack of reporting of training compliance data or high risk of bias.
Conclusion
The available evidence supports the use of EE in the management of AT. Continuous load on the Achilles tendon does not adversely affect the results of pain and function, suggesting the possibility of practising some physical activities during the intervention. Some authors report that EE and HSR produce similar results, but more studies are needed to confirm this. Also, the rest/wait-and-see approaches probably do not play a role in the management of AT.
Acknowledgements
We like to thank the Postgraduate Program of the Santa Catarina State (PROMOP) that was supported this work and the professors Dra. Fabiana Flores Sperandio and Dr. Alexandre Marcio Marcolino.
Abbreviations
- ROM
Range of motion
- AT
Achilles tendinopathy
- EE
Eccentric exercise
- RoB2
Risk of Bias 2
- MD
Mean difference
- CI
Confidence interval
- HSR
Heavy slow resistance
Author contributions
RO: conceptualisation, writing, revision; FM: revision; DAP writing; TTS supervision; LFN revision; LSS supervision; NM revision. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external source of funding was used.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Diego Ailton Prudêncio, Email: diegoprudencio1@hotmail.com.
Nicola Maffulli, Email: n.maffulli@qmul.ac.uk.
Filippo Migliorini, Email: migliorini.md@gmail.com.
Thiago Teixeira Serafim, Email: thiagotserafim@outlook.com.
Luis Felipe Nunes, Email: lipefelipenunes@gmail.com.
Luciana Sayuri Sanada, Email: luciana.sanada@udesc.br.
Rodrigo Okubo, Email: rodrigo.okubo@udesc.br.
References
- 1.Egger AC, Berkowitz MJ. Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017;10:72–80. doi: 10.1007/s12178-017-9386-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li H-Y, Hua Y-H. Achilles tendinopathy: current concepts about the basic science and clinical treatments. Biomed Res Int. 2016;2016:1–9. doi: 10.1155/2016/6492597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sobhani S, Dekker R, Postema K, Dijkstra PU. Epidemiology of ankle and foot overuse injuries in sports: a systematic review. Scand J Med Sci Sport. 2013;23:669–686. doi: 10.1111/j.1600-0838.2012.01509.x. [DOI] [PubMed] [Google Scholar]
- 4.Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. Muscles Ligaments Tendons J. 2011;1:134–137. [PMC free article] [PubMed] [Google Scholar]
- 5.van Dijk CN, van Sterkenburg MN, Wiegerinck JI, et al. Terminology for Achilles tendon related disorders. Knee Surg Sports Traumatol Arthrosc. 2011;19:835–841. doi: 10.1007/s00167-010-1374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Jonge S, Van Den Berg C, De Vos RJ, et al. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med. 2011;45:1026–1028. doi: 10.1136/bjsports-2011-090342. [DOI] [PubMed] [Google Scholar]
- 7.Kujala UM, Sarna S, Kaprio J. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med. 2005;15:133–135. doi: 10.1097/01.jsm.0000165347.55638.23. [DOI] [PubMed] [Google Scholar]
- 8.Janssen I, van der Worp H, Hensing S, Zwerver J. Investigating Achilles and patellar tendinopathy prevalence in elite athletics. Res Sports Med. 2018;26:1–12. doi: 10.1080/15438627.2017.1393748. [DOI] [PubMed] [Google Scholar]
- 9.Lopes AD, Carlos L, Junior H, et al. What are the main running-related musculoskeletal injuries? A systematic review. Sports Med. 2012;42:891–905. doi: 10.1007/BF03262301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sport Med. 2014;44:123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 11.Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45:553–558. doi: 10.1136/bjsm.2009.060582. [DOI] [PubMed] [Google Scholar]
- 12.Hunt KJ, Hurwit D, Robell K, et al. Incidence and epidemiology of foot and ankle injuries in elite collegiate athletes. Am J Sports Med. 2016;45:426–433. doi: 10.1177/0363546516666815. [DOI] [PubMed] [Google Scholar]
- 13.Mahieu NN, Witvrouw E, Stevens V, et al. Intrinsic risk factors for the development of Achilles tendon overuse injury: a prospective study. Am J Sports Med. 2006 doi: 10.1177/0363546505279918. [DOI] [PubMed] [Google Scholar]
- 14.Mayer F, Hirschmu A, Mu S, et al. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Spots Med. 2007 doi: 10.1136/bjsm.2006.031732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin RL, Chimenti R, Cuddeford T, et al. Achilles pain, stiffness, and muscle power deficits : midportion achilles tendinopathy revision 2018 clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section. J Orthop Sports Phys Ther. 2018 doi: 10.2519/jospt.2018.0302. [DOI] [PubMed] [Google Scholar]
- 16.Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009;19:54–64. doi: 10.1097/JSM.0b013e31818ef090. [DOI] [PubMed] [Google Scholar]
- 17.Paavola M, Kannus P, Paakkala T, et al. Long-term prognosis of patients with Achilles tendinopathy: an observational 8-year follow-up study. Am J Sports Med. 2000;28:634–642. doi: 10.1177/03635465000280050301. [DOI] [PubMed] [Google Scholar]
- 18.Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med. 2018;52:387–407. doi: 10.1136/bjsports-2016-097347. [DOI] [PubMed] [Google Scholar]
- 19.Longo UG, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc. 2018;26:16–30. doi: 10.1097/JSA.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 20.Murphy M, Travers M, Gibson W, et al. Rate of improvement of pain and function in mid-portion Achilles tendinopathy with loading protocols: a systematic review and longitudinal meta-analysis. Sport Med. 2018;4201706273:1–17. doi: 10.1007/s40279-018-0932-2. [DOI] [PubMed] [Google Scholar]
- 21.Wheeler PC, Mahadevan D, Bhatt R, Bhatia M. A comparison of two different high-volume image-guided injection procedures for patients with chronic noninsertional achilles tendinopathy: a pragmatic retrospective cohort study. J Foot Ankle Surg. 2016 doi: 10.1053/j.jfas.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 22.Carcia CR, Martin RL, Wukich DK. Achilles pain, stiffness, and muscle power deficits: Achilles tendinitis. J Orthop Sport Phys Ther. 2010;40:A1–A26. doi: 10.2519/jospt.2010.0305. [DOI] [PubMed] [Google Scholar]
- 23.Sussmilch-Leitch S, Collins N, Bialocerkowski A, et al. Physical therapies for Achilles tendinopathy: systematic review and meta-analysis (provisional abstract) J Foot Ankle Res. 2012;5:1–16. doi: 10.1186/1757-1146-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gatz M, Betsch M, Tingart M, et al. Effect of a 12-week eccentric and isometric training in Achilles tendinopathy on the gastrocnemius muscle: An ultrasound shear wave elastography study. Muscles Ligaments Tendons J. 2020;10:92–99. doi: 10.32098/mltj.01.2020.12. [DOI] [Google Scholar]
- 25.Maffulli N, Walley G, Sayana M, et al. Eccentric calf muscle training in athletic patients with Achilles tendinopathy. Disabil Rehabil. 2008;30:1677–1684. doi: 10.1080/09638280701786427. [DOI] [PubMed] [Google Scholar]
- 26.Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10:52–58. doi: 10.1016/j.jsams.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 27.Wilson F, Walshe M, Owyer T, et al. Exercise, orthoses and splinting for treating Achilles tendinopathy: a systematic review with meta-analysis. Br J Sports Med. 2018 doi: 10.1136/bjsports-2017-098913. [DOI] [PubMed] [Google Scholar]
- 28.Tumilty S, Mani R, Baxter GD. Photobiomodulation and eccentric exercise for Achilles tendinopathy: a randomized controlled trial. Lasers Med Sci. 2016;31:127–135. doi: 10.1007/s10103-015-1840-4. [DOI] [PubMed] [Google Scholar]
- 29.Verrall G, Schofield S, Brustad T, Physio D. Chronic Achilles tendinopathy treated with eccentric stretching program. Foot Ankle Int. 2011 doi: 10.3113/FAI.2011.0843. [DOI] [PubMed] [Google Scholar]
- 30.Abbott B, Bigland B, Ritchie J. The cost of negative work. J Physiol. 1952;117:380–390. doi: 10.1113/jphysiol.1952.sp004755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bigland-Ritchie B, Woods JJ. Integrated electromyogram and oxygen uptake during positive and negative work. J Physiol. 1976;260:267–277. doi: 10.1113/jphysiol.1976.sp011515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic achilles tendinosis. Am J Sports Med. 1998;26:360–366. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 33.Van Der Plas A, De Jonge S, De Vos RJ, et al. A 5-year follow-up study of Alfredson ’ s heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med. 2011 doi: 10.1136/bjsports-2011-090035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roos EM, Engström M, Lagerquist A, Söderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy—a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004 doi: 10.1111/j.1600-0838.2004.00378.x. [DOI] [PubMed] [Google Scholar]
- 35.Spieth PM, Kubasch AS, Isabel Penzlin A, et al. Randomized controlled trials—a matter of design. Neuropsy Dis Treat. 2016;12:1341–1349. doi: 10.2147/NDT.S101938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JPT, Savovic J, Page MJ, Sterne JAC. Revised cochrane risk-of-bias tool for randomized trials (RoB 2). RoB 2.o Dev Gr. 2019.
- 37.Uman LS. Information management for the busy practitioner: systematic reviews and meta-analyses. J Am Acad Child Adolesc Psychiatry. 2011;20:57–59. doi: 10.1016/j.revmed.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haidich AB. Meta-analysis in medical research. Hippokratia. 2010;14:29–37. doi: 10.5005/jp/books/10519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lester J. The use of meta-analysis and forest plots to examine and display data in oncology research. J Adv Pract Oncol. 2014;5:465–470. [PMC free article] [PubMed] [Google Scholar]
- 40.Habets B, van Cingel REH, Backx FJG, Huisstede BMA. Alfredson versus Silbernagel exercise therapy in chronic midportion Achilles tendinopathy: study protocol for a randomized controlled trial. BMC Musculoskelet Disord. 2017;18:296. doi: 10.1186/s12891-017-1656-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mccormack JR, Underwood FB, Slaven EJ, Cappaert TA. Eccentric exercise versus eccentric exercise and soft tissue treatment (Astym) in the management of insertional Achilles tendinopathy: a randomized controlled trial. Sports Health. 2016 doi: 10.1177/1941738116631498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Vos RJ, Weir A, Visser RJ, et al. The additional value of a night splint to eccentric exercises in chronic midportion Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2007;41:1–6. doi: 10.1136/bjsm.2006.032532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nørregaard J, Larsen CC, Bieler T, Langberg H. Eccentric exercise in treatment of Achilles tendinopathy. Scand J Med Sci Sport. 2007;17:133–138. doi: 10.1111/j.1600-0838.2006.00545.x. [DOI] [PubMed] [Google Scholar]
- 44.Grävare Silbernagel K, Brorsson A, Lundberg M. The majority of patients with Achilles tendinopathy recover fully when treated with exercise alone: a 5-year follow-up. Am J Sports Med. 2011;39:607–613. doi: 10.1177/0363546510384789. [DOI] [PubMed] [Google Scholar]
- 45.Roos E, Engstrom M, Lagerquist A, et al. Eccentric calf-muscle exercises reduce pain and functional limitations due to Achilles tendinosis. A prospective, randomized clinical trial with one-year follow-up. Arthritis Rheum. J. 2001.
- 46.Yu J, Park D, Lee G. Effect of eccentric strengthening on pain muscle strength, endurance, and functional fitness factors in male patients with Achilles tendinopathy. Am J Phys Med Rehabil. 2013;92:68–76. doi: 10.1097/PHM.0b013e31826eda63. [DOI] [PubMed] [Google Scholar]
- 47.Ram R, Meeuwisse W, Patel C, et al. The limited effectiveness of a home-based eccentric training for treatment of Achilles tendinopathy. Clin Investig Med. 2013;36:197. doi: 10.25011/cim.v36i4.19953. [DOI] [PubMed] [Google Scholar]
- 48.Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sport Traumatol Arthrosc. 2001;9:42–47. doi: 10.1007/s001670000148. [DOI] [PubMed] [Google Scholar]
- 49.Silbernagel KG, Thomeé R, Thomeé P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain—a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. 2001;11:197–206. doi: 10.1034/j.1600-0838.2001.110402.x. [DOI] [PubMed] [Google Scholar]
- 50.Silbernagel KG, Eriksson B, Thomeé R, Karlsson J. Continued sports activity, using a pain- monitoring model, during rehabilitation in patients with Achilles tendinopathy a randomized controlled study. Am J Sports Med. 2007 doi: 10.1177/0363546506298279. [DOI] [PubMed] [Google Scholar]
- 51.Rompe JD, Nafe B, Furia J, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med. 2007 doi: 10.1177/0363546506295940. [DOI] [PubMed] [Google Scholar]
- 52.Horstmann T, Jud HM, Fröhlich V, et al. Whole-body vibration versus eccentric training or a wait-and-see approach for chronic Achilles tendinopathy: a randomized clinical trial. J Orthep Sports Phys Ther. 2013;43:794–803. doi: 10.2519/jospt.2013.4762. [DOI] [PubMed] [Google Scholar]
- 53.Stasinopoulos D, Manias P. Comparing two eccentric exercise programmes for the management of Achilles tendinopathy. a pilot trial. J Bodyw Mov Ther. 2013;17:309–315. doi: 10.1016/j.jbmt.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 54.Stevens M, Tan C. Effectiveness of the Alfredson protocol compared with a lower repetition-volume protocol for midportion Achilles tendinopathy: a randomized controlled trial. J Orthep Sports Phys Ther. 2014;44:59–67. doi: 10.2519/jospt.2014.4720. [DOI] [PubMed] [Google Scholar]
- 55.Beyer R, Kongsgaard M, Kjær BH, et al. Heavy slow resistance versus eccentric training as treatment for achilles tendinopathy: a randomized controlled trial. Am J Sports Med. 2015 doi: 10.1177/0363546515584760. [DOI] [PubMed] [Google Scholar]
- 56.Macdermid JC, Silbernagel KG. Outcome evaluation in tendinopathy: foundations of assessment and a summary of selected measures. J Orthep Sport Phys Ther. 2015;45:950–964. doi: 10.2519/jospt.2015.6054. [DOI] [PubMed] [Google Scholar]
- 57.Delgado DA, Lambert BS, Boutris N, et al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018 doi: 10.5435/JAAOSGlobal-D-17-00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Younger J, McCue R, Mackey S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep. 2009;13:39–43. doi: 10.1007/s11916-009-0009-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jamison NR, Gracely RH, Raymond SA, et al. Comparative study of electronic vs. paper VAS ratings: a randomized, crossover trial using healthy volunteers. Pain. 2002;99:341–347. doi: 10.1016/S0304-3959(02)00178-1. [DOI] [PubMed] [Google Scholar]
- 60.Paschalis V, Nikolaidis MG, Giakas G, et al. Beneficial changes in energy expenditure and lipid profile after eccentric exercise in overweight and lean women. Scand J Med Sci Sport. 2010;20:103–111. doi: 10.1111/j.1600-0838.2009.00920.x. [DOI] [PubMed] [Google Scholar]
- 61.Paschalis V, Nikolaidis MG, Theodorou AA, et al. The effects of eccentric exercise on muscle function and proprioception of individuals being overweight and underweight. J Strength Cond Res. 2013;27:2542–2551. doi: 10.1519/JSC.0b013e31827fc9a6. [DOI] [PubMed] [Google Scholar]
- 62.Hody S, Croisier J, Bury T, Rogister B. Eccentric muscle contractions: risks and benefits. Front Physiol. 2019;10:1–18. doi: 10.3389/fphys.2019.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maffulli N, Longo UG, Kadakia A, Spiezia F. Achilles tendinopathy. Foot Ankle Surg. 2019;26:112–126. doi: 10.1097/JSA.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 64.Niesen-Vertommen SL, Taunton JE, Clement DB, Mosher RE. The effect of eccentric versus concentric exercise in the management of Achilles tendonitis. Clin J Sports Med. 1992;2:109–113. doi: 10.1097/00042752-199204000-00006. [DOI] [Google Scholar]
- 65.Peterson M, Butler S, Eriksson M, Svrdsudd K. A randomized controlled trial of exercise versus wait-list in chronic tennis elbow (lateral epicondylosis) Ups J Med Sci. 2011;116:269–279. doi: 10.3109/03009734.2011.600476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oberste M, Hartig P, Bloch W, et al. Control group paradigms in studies investigating acute effects of exercise on cognitive performance—an experiment on expectation-driven placebo effects. Front Hum Neurosci. 2017;11:1–10. doi: 10.3389/fnhum.2017.00600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kongsgaard M, Kovanen V, Aagaard P, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sport. 2009;19:790–802. doi: 10.1111/j.1600-0838.2009.00949.x. [DOI] [PubMed] [Google Scholar]
- 68.Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986;2085:65–68. [PubMed] [Google Scholar]
- 69.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Clin Oral Investig. 2001;357:1191–1194. doi: 10.1016/S0140-6736(00)04337-3. [DOI] [PubMed] [Google Scholar]
- 70.Cohn LD, Decker BJ. How meta-analysis increases statistical power. Psychol Methods. 2003;8:243–253. doi: 10.1037/1082-989X.8.3.243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.