Abstract
Background
Malaria infection during pregnancy is a significant public health problem that puts pregnant women at risk. Interruption of transmission of asymptomatic malaria among a population remained a challenge and the host serves as a reservoir for the malaria parasite; and is also recognized as a major barrier to malaria elimination. This study aimed to assess the prevalence of asymptomatic malaria and associated factors among pregnant women in the Boset District, East Shoa Zone, Oromia, Ethiopia.
Methods
A community-based cross-sectional study was conducted to assess the prevalence of asymptomatic malaria and associated factors in pregnant women from February to March 2022. Using multistage sample techniques, 328 asymptomatic pregnant women were enrolled. Data were collected using a structured questionnaire. A rapid test and Giemsa-stained blood smear microscopy were used to diagnose Plasmodium infections. Epi info version 7 was used to code, enter, and clean data before being uploaded to SPSS version 25.0 for analysis. Bivariable and multivariable binary logistic regression were employed to find the associated factors. Variables in the multivariable model with a p-value < 0.05 were considered significantly associated with asymptomatic malaria.
Results
Of the total 328 pregnant women who participated in this study, 9(2.74%) and 10(3.05%) were confirmed to be infected with Plasmodium species by microscopy and rapid diagnostic tests, respectively. Asymptomatic malaria during pregnancy was found to be significantly associated with not using an insecticide-treated bed net [(P = 0.002, AOR: 9.61; 95% CI (2.22–41.53)], lack of consultation and health education about malaria prevention during Antenatal care attendance [(P = 0.04, AOR: 4.05; 95% CI (1.02, 16.05)], and living close stagnant water [(P = 0.02, AOR: 4.43; 95% CI (1.17,16.82)].
Conclusions
The current study showed that asymptomatic malaria is prevalent in pregnant women. Not using insecticide-treated bed nets, inadequate health education during antenatal care, and living close to stagnant water are significantly associated with malaria infection. Thus, using insecticide-treated bed nets, health education, and avoiding stagnant water from residential areas could play significant roles in preventing asymptomatic malaria among pregnant women in the study area.
Keywords: Asymptomatic Malaria, Pregnancy, Associated factors, Prevalence, Ethiopia
Background
Malaria is a disease caused by protozoan parasites of the genus Plasmodium, which are transmitted to humans by blood-feeding female Anopheles mosquitoes. Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, and Plasmodium malariae are the four human Plasmodium species [1]. Plasmodium falciparum is found in most of the tropical regions of the world and is the most dangerous of the five species in terms of both its lethality and morbidity [2].
Malaria infection during pregnancy is a significant public health problem that poses a significant risk to the pregnant woman, fetus, and newborn. In sub-Saharan Africa, malaria mainly affects children and pregnant women [3]. Although malaria is often asymptomatic in some regions of Africa during pregnancy, it nevertheless results in severe maternal anemia and low birth weight babies. Because low birth weight is so strongly correlated with a child's likelihood of surviving, successfully treating malaria during pregnancy could prevent 75,000–200,000 newborn fatalities annually [4]. Malaria during pregnancy affects the mother, fetus, and neonates [5]. It increases the risk of stillbirths, spontaneous abortion, premature delivery, and low birth weight [5, 6]. In areas with high transmission, malaria is often asymptomatic in adults. This is due to acquired immunity from constant exposure and previous childhood infections [7]. This immunity does not cover infection, but it does reduce the risk of serious illness [8]. The acquired immunity also protects pregnant women and malaria infections are often asymptomatic. However, pregnant women are still predisposed to malaria and the risk of severe symptomatic disease is higher than that of non-pregnant women [7, 8]. Infection with malaria during pregnancy has significant effects not only on the pregnant mother’s health, but also on her child’s birth outcomes. Nevertheless the acute illness due to malaria is uncommon; and the disease in many instances remains silent during pregnancy [9].
Malaria is one of the most widespread human parasitic diseases that ranks first in terms of its socio-economic and public health importance in the tropical and subtropical regions of the world, particularly in sub-Saharan African and Southeast Asian countries [2, 10]. As stated by World Health Organization (WHO), there were approximately 228 million cases of malaria worldwide, and the death toll reached 435,000 in 2018 [11].
In Ethiopia, an estimated 55.7 million people (68% of the population) are at risk of malaria, and three fourth of the landmass is considered malarious [12]. The Federal Ministry of Health (FMOH) estimates the annual cases of clinical malaria as 5–10 million, which corresponds to 12% of outpatient consultations and 10% of hospital admissions [13]. In the country, P. falciparum and P. vivax are the main species that account for about 60 and 40% of malaria cases, respectively [13], Recent reports indicate a shift in dominance from falciparum to vivax in highland areas [14].
Asymptomatic malaria is a new challenge to the national strategic plan for malaria prevention and control (2011–2015): a situation in which a human Plasmodium reservoir is maintained with individuals who are not treated because they are undiagnosed since they are asymptomatic [13]. The use of long-lasting insecticidal nets (LLINs), the administration of intermittent preventive treatment with artemisinin-based combination therapy (ACT), and adequate case management through rapid and effective therapy for malaria in pregnant women are the current strategies recommended by the WHO [15]. Currently, as part of the antenatal care (ANC) service package, WHO is working to improve access to ACT for pregnant women in all areas of moderate to high malaria transmission in Africa, but these activities are not used as ANC services to pregnant women in Ethiopia [15].
The presence of asymptomatic infections is less well-known in environments with pronounced seasonality [16]. However, in recent years such cases have also been reported from areas with low endemics such as the Amazon basin malaria, as the detection and treatment of all sources of infection is very important at this stage in Brazil, Peru [17], Colombia[18], Solomon Island [19], and Principe [20]. Any successful malaria elimination strategy depends on the ability to find and treat the asymptomatic reservoir. Globally, various studies reported the prevalence of asymptomatic malaria infection among pregnant women in both the control and eradication phases by taking into account the significance of asymptomatic malaria infection in diversified endemic regions [21].
In Ethiopia; a study on the prevalence of asymptomatic malaria in pregnant women; reported by different study groups shows a prevalence in the district of Merti, Oromia (3.6%) in 2016 [22]. Sanja (6.8%) in 2014 [23], and Arba Minch town (9.1%) in 2015 [24].
In both stable endemic regions and regions with the unstable transmission, asymptomatic malaria is frequently seen. Although acute malaria infections were given a lot of attention in many malaria-endemic regions of the world, asymptomatic malaria infection is yet to get due attention. In contrast, the asymptomatic host remained a significant barrier and challenge to the prevention, control, and eradication strategies of malaria in different countries of the world [25].
Therefore, this study aimed to assess the prevalence of asymptomatic malaria and associated factors among pregnant women in Boset District, Oromia Regional State, Ethiopia.
Methods
Study area
This study was conducted in Boset District which is located 125 kms southeast of Addis Ababa and has a total landmass of 14,050.27 square kilometres. It is one of the districts of the East Shewa Zone. The district is bordered on the south by the South Arsi Zone, the north by the North Amhara Regional State, the west by the West Adama District, and the east by the East Fentale District. The elevation of the District was 1050 m above sea level and 2500 m above mean sea level. The average annual rainfall and temperature range from 600 to 900 mm and 12 to 34 degrees Celsius, respectively. The district has three climate zones: 79 percent low-land "Kola," 20 percent mid-land "Woyinadega," and 1 percent high-land "Dega."
Study design and period
A community-based cross-sectional study was conducted from February to March 2022.
Population
Source population
The source population was all pregnant women living in the Boset district, East Shoa zone.
Study population
All pregnant women who live in selected Villages of Boset District.
Inclusion and exclusion criteria
Inclusion criteria: All pregnant women with the absence of disease symptoms/signs of malaria within the past 48 h, axillaries temperature ≤ 37.5 ℃, and permanent residents in the study area.
Exclusion criteria: Pregnant women had taken antimalarial drugs in the last 4 weeks before the study period.
Sample size determination and sampling technique
The sample size was calculated using the single population proportion sample size calculation formula, with a 95% confidence level, a 5% margin of error, and the proportion of asymptomatic malaria infection among pregnant women (P) taken as 11.2% [26]. The final calculated sample size was 328.
Key: n = sample size, P = proportion of asymptomatic malaria infection, and d = margin of error.
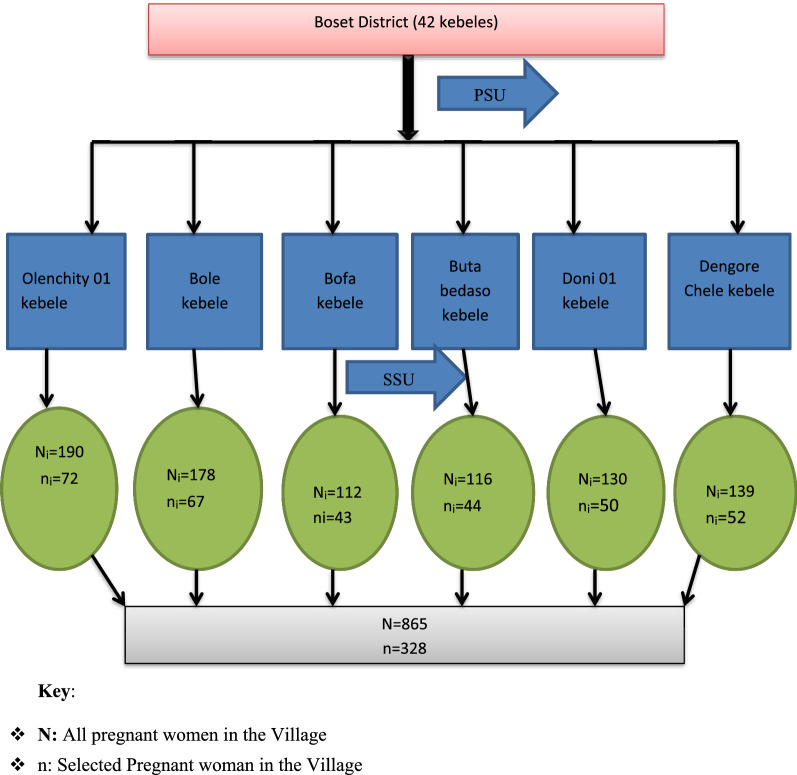
In addition, from the total 42 villages in the study area (Boset district) 6 villages were selected using the random sampling method. The above-calculated sample size was proportionally distributed to each village as per the current number of pregnant women population (Fig. 1). Then, a multistage sampling technique was employed to get each study subject during the actual data collection period.
Fig. 1.
Flow chart indicating the sampling procedure for a study conducted on asymptomatic malaria among pregnant women in Boset District, Oromia, Ethiopia, 2022. Key: N: All pregnant women in the Village. n: Selected Pregnant woman in the Village
Study variables
Dependent variable: Asymptomatic malaria among pregnant women.
Independent variable: Age, residence, gestational age, previous infection with Plasmodium, living close to stagnant water, indoor residual spray, use of insecticide-treated bed net, gravidity, ANC attendance, trimester.
Socio-demographic characteristics
Pre-tested and semi-structured questionnaires were administered by six trained Nurses and midwives interviewers to obtain data on socio-demographic characteristics and factors associated with asymptomatic malaria. They were supervised by one health professional with a qualification of BSc degree. The questionnaire was initially prepared in English and it was translated into Afan Oromo, the local language, and back into English by language experts, to check the consistency.
Blood sample collection and processing
Capillary blood samples were collected by finger pricking using a disposable lancet. Giemsa-stained blood smear microscopy and RDTs were employed for the diagnosis of asymptomatic malaria parasitaemia at Olenchity Primary Hospital, Olenchity Health Center, and Bole Health Center. Asexual Plasmodium parasite density per microlitre (μl) of blood was determined by counting the number of parasites per 200 white blood cells on a thick blood film assuming a total standard WBC count of 8000/μl. The degree of parasite density was graded as mild, moderate, and severe when the counts will be between 1–999 parasites/μl, 1000–9999/μl, and > 10,000/μl, respectively, following the method described elsewhere [27].
Operational definitions
Asymptomatic malaria: The absence of malaria-related symptoms within the past 2 days and at the time of the survey, and the presence of malaria parasites in the blood.
Residents: An individual that lives in a selected study village at least for 6 months before the start of the data collection time frame.
Data quality assurance
Quality control
Two experienced laboratory technologists individually examined the microscopic slides. Hundred microscopic fields of the thick smear were examined before concluding as negative. The discrepancy between the first and second readings was settled by a third senior laboratory technologist. The manufacturer’s instructions were strictly followed for the RDTs. Blood smear microscopy readers were blinded to the result of RDTs.
Data quality management
All laboratory materials such as rapid test kits, slides, thermometers, and sample transporting systems were checked by experienced laboratory professionals. The specimens were also checked for serial number, quality, and procedures of collection. The laboratory professionals involved in RDT and light microscopy examination were trained in malaria diagnosis and quality assurance training. The rapid test kit was checked for the expiration date, correct collection procedures, and samples as well as inbuilt control appearances. Inconsistent results of light microscopy were checked again to confirm the findings.
Data processing and analysis
Data were coded, entered into, and cleaned using Epi info version 7.2 and transferred to SPSS version 25.0 for analysis. Both descriptive and inferential statistics were employed for the analysis of data. Frequencies were used to determine the prevalence of asymptomatic Plasmodium infection in pregnant women. The Chi-square assumption was checked for all categorical independent variables. Both bi-variable and multi-variable logistic regressions were used to assess the association between outcome and explanatory variables. Factors with p-value ≤ 0.25 from the bi-variable model were included in the final model. Variables having a p-value < 0.05 from the multivariable model were considered as having a statistically significant association with the outcome. An adjusted Odds ratio with 95% CI was used as a measure of association. The model goodness of fit was assessed using the Hosmer–Lemeshow test.
Results
Socio-demographic, obstetric, and malaria prevention methods characteristics of the pregnant women
This study included a total of 328 pregnant women, with 252 (76.8%) of them living in rural areas. Participants in the study ranged in age from 16 to 36 years old, with a mean age of 25.52 ± 4.74 years. The majority of study participants were farmers 192(58.5%) and 314(95.7%) were married. About 219 (66.8%) of respondents owned at least one bed net, and 179 (54.6%) of them sleep under bed nets the previous night. Only 134 (40.9%), of the households, had indoor residual spraying (IRS) in the last 12 months. About 27.7% of the pregnant women were multigravidae, 47.3% of them were in their second trimester of pregnancy, and the majority 84.8% of them were following antenatal care (Table 1).
Table 1.
Socio-demographic characteristics and malaria prevention methods in boset district, Ethiopia, 2022
| Variables | Frequency | Percent (%) | Variables | Frequency | Percent (%) |
|---|---|---|---|---|---|
| Age groups in years | Residence | ||||
| 15–19 | 38 | 11.6 | Rural | 252 | 76.8 |
| 20–24 | 102 | 31.1 | Urban | 76 | 23.2 |
| 25–29 | 121 | 36.9 | Gravidity | ||
| 30–34 | 52 | 15.9 | Multigravidae | 91 | 27.7 |
| ≥ 35 | 15 | 4.6 | Primigravidae | 131 | 39.9 |
| Occupational status | Secondigravidae | 106 | 32.3 | ||
| Daily wage laborer | 51 | 15.5 | Gestational age | ||
| Farmer | 192 | 58.5 | 1st trimester | 104 | 31.7 |
| Government | 23 | 7.0 | 2nd trimester | 155 | 47.3 |
| Private | 48 | 14.6 | 3rd trimester | 69 | 21.0 |
| Other | 14 | 4.3 | ANC Attendance | ||
| Educational status | Yes | 278 | 84.8 | ||
| No formal education | 102 | 31.1 | No | 50 | 15.2 |
| Primary School | 125 | 38.1 | ITN Ownership | ||
| Secondary School | 74 | 22.6 | Yes | 219 | 66.8 |
| College/University | 27 | 8.2 | No | 109 | 33.2 |
| Marital Status | ITN Utilization | ||||
| Single | 2 | 0.6 | Yes | 179 | 54.6 |
| Married | 314 | 95.7 | No | 149 | 45.4 |
| Separated | 5 | 1.5 | IRS Use(past 1yrs) | ||
| Divorced | 7 | 2.1 | Yes | 134 | 40.9 |
| No | 194 | 59.1 | |||
Prevalence of malaria infection among asymptomatic pregnant women
The prevalence of asymptomatic Plasmodium infection was 9(2.74%) [95% CI (1, 4.5)] and 10(3.05%) [95% CI (1.2, 4.9)] by using microscopy and RDTs, respectively. The density of parasitaemia, as determined from the thick blood smear, ranged from 790 to 5600 parasites /μl. The geometric mean of parasite density among the 7 parasitaemic pregnant women was 3528.6/μl [95% CI (3310–3750)]. The majority of the study participants who were diagnosed with malaria cases had moderate parasitaemia 5(71.4%), while 2(28.6%) had mild parasitaemia (Table 1).
Factors associated with asymptomatic Plasmodium infection
Socio-demographic characteristics, obstetric characteristics, and other health-related factors were analyzed using bivariable binary logistic regression for the possible association. Then, gravidity, ITN utilization, ITN ownership, consultation about malaria prevention methods during ANC attendance, and Living close to stagnant water were variables that showed a possible association with Plasmodium infection at a P-value of ≤ 0.25 and fit for multivariable logistic regression analysis.
In multivariable logistic regression analysis, ITN utilization, consultation about malaria prevention methods during ANC attendance, and living close to stagnant water had a statistically significant association with asymptomatic Plasmodium species infection at P-value < 0.05 after adjusting for possible confounders. This study also found that pregnant women who did not utilize ITN had 9.61 times [AOR 9.61; 95% CI (2.22, 41.53)] higher chance of having asymptomatic Plasmodium infection than those who did. Pregnant women who lived near stagnant water had 4.43 times [AOR 4.43; 95% CI (1.17, 16.82)] greater odds of having asymptomatic Plasmodium infection than those who did not live near stagnant water. In addition, pregnant women who did not receive malaria prevention education during their ANC follow-up had a 4.05-fold higher risk of malaria infection than their counterparts [AOR: 4.05; 95% CI (1.02, 16.05)] (Table 2).
Table 2.
Bivariable and Multivariable analysis of associated factors for asymptomatic Plasmodium species infection among pregnant women at Boset district, 2022 (N = 328)
| Variables | Malaria status | COR (95% CI) | AOR (95% CI) | P-value | ||
|---|---|---|---|---|---|---|
| Negative (%) | Positive (%) | |||||
| Gravidity | Secondigravidae | 101(95.3%) | 5(4.7%) | 1 | 1 | |
| Multigravidae | 88(96.7%) | 3(3.3%) | 0.68[0.16,2.96] | 0.31[0.22,5.80] | 0.24 | |
| Primigravidae | 129(98.5%) | 2(1.5%) | 0.23[0.04,1.34] | 0.22[0.04,2.18] | 0.06 | |
| Counseling at ANC attendance | Yes | 272(97.8%) | 6(2.2%) | 1 | 1 | |
| No | 46(92%) | 4(8%) | 3.94[1.07,14.51] | 4.05[1.02,16.05] | 0.04** | |
| ITN ownership | Yes | 210(95.9%) | 9(4.1%) | 1 | 1 | |
| No | 108(99.08%) | 1(0.92%) | 0.21[0.02,1.72] | 0.16[0.02,1.43] | 0.10 | |
| ITN utilization | Yes | 176(98.3%) | 3(2.7%) | 1 | 1 | |
| No | 142(95.3%) | 7(4.7%) | 2.89[0.73,11.38] | 9.61[2.22,41.53] | 0.002** | |
| IRS use in the last year | Yes | 131(97.8%) | 3(2.2%) | 1 | 1 | |
| No | 187(96.4%) | 7(3.6%) | 1.63[0.41,6.43] | 2.70[0.65,11.17] | 0.16 | |
| Living close to stagnant water | No | 49(92.5%) | 4(7.5%) | 1 | 1 | |
| Yes | 269(97.8%) | 6(2.2%) | 3.66[0.99,13.44] | 4.43[1.17,16.82] | 0.02** | |
Discussion
This study assessed the prevalence of asymptomatic malaria infection and associated factors among pregnant women. The prevalence rates of asymptomatic Plasmodium infections among pregnant women were 2.74% [95% CI = (1.26, 5.14)] and 3.05% [95% CI = (1.47, 5.54)] using Giemsa-stained blood smear microscopy and RDT, respectively. These findings are lower when compared to the results reported previously from many similar studies conducted in different countries. For instance, the reported prevalence from the Republic of Congo was 7% [28]; the rural district surrounding Arbaminch town, Ethiopia was 9.1% [24]; the global scenario reported 10.8% [29]; the study from South-West Nigeria reported 7.7% [30]; a study from Southern Laos reported 8.3% [31], and the study from India reported 5.4% [32]. The low prevalence of asymptomatic malaria infection among pregnant women in this study could be due to the improvements in malaria control interventions in Ethiopia or the likely difference in malaria epidemiology among various study populations and areas; and the differences in climatic conditions or seasons where the data were collected from different parts of the world. In addition, the current study was conducted during the season in which the malaria prevalence rate is usually lower in the study area. This could be the possible explanation for the observed lower prevalence rate of asymptomatic malaria among pregnant women in this study.
Nevertheless, the prevalence of asymptomatic malaria infection documented in this study is comparable to the findings of the studies conducted in Bangladesh, which was reported as 2.3% among pregnant women [33], and in Merti district, Oromia, Ethiopia (3.6%) [22]. According to the findings of the current study, 77.78% of the cases were caused by P. falciparum. This result was almost in line with the study conducted in Ethiopia that reported 65–75% of malaria infections are caused by P. falciparum [34]. However, our result was higher than the study done in the Merti district, Ethiopia which was 46.2% [22]. This high proportion of P. falciparum in this study is a clear implication that there is a need for aggressive prevention and control of the disease, especially among pregnant women. Moreover, P. falciparum causes the most severe form of the disease and devastating complications not only to the mother, but also to the fetus. However, the proportion of malaria cases caused by P. falciparum in the study was lower than that of the WHO malaria 2017 report, which stated that P. falciparum was responsible for almost 99% of malaria cases [2]. The cause for these variations might be owing to significant seasonal, inter-annual, and geographical variability. Large climate changes (temperature, rainfall, and relative humidity), human habitation, and population mobility patterns could be also the possible reasons for the observed variations in prevalence rates.
In addition, the findings revealed not using ITN effectively increased the odds of developing malaria infection during pregnancy. This finding is in agreement with the findings of previous studies conducted elsewhere. For instance, the studies from Malawi [35], Arbaminch, Ethiopia [24], and Sherkole district, West Ethiopia [36], reported that using bed nets significantly reduced malaria infection. These associations could be explained by the fact that ITNs successfully minimize human-mosquito contact, which in turn helps in preventing malaria illnesses.
Furthermore, the pregnant women who lived near stagnant water were more likely to have an asymptomatic malaria infection than their counterparts. This finding is also in agreement with the findings of research that were undertaken in the West Arsi Zone, Ethiopia [37], and the Southwestern part of Ethiopia [38]. This could be because stagnant water is the ideal site for malaria vector breeding, and those who live near stagnant water are more susceptible to the disease. According to the findings of this research getting a consultation and health education about malaria prevention methods during ANC follow-up significantly reduced the risk of asymptomatic malaria infection among pregnant women. In the studies conducted in other localities of Ethiopia, similar findings were discovered [36, 39]. In general, the effective use of various malaria prevention and control measures among different population segments also play vital roles in the prevention and control of asymptomatic malaria among pregnant women.
The main limitations of the study include the inability to identify a direct temporal association between asymptomatic malaria infection and its likely risk factors because of being a cross-sectional study design; in the inability to diagnose all subjects using real-time PCR due to resources constraints; and fact that the data were collected during the season with low transmission probability which could have underestimated the prevalence of asymptomatic malaria among the study population.
Conclusions
This study showed that asymptomatic malaria is prevalent among pregnant women in the study area. Plasmodium falciparum is most prevalent species in the area. Inadequate use of ITNs, living close to stagnant water, and inadequate consultation and health education about malaria prevention methods during ANC attendance were found to be factors associated with the occurrences of asymptomatic malaria infection among pregnant women.
Thus, using insecticide-treated bed nets effectively, adequate consultation and health education on various malaria preventive measures, and avoiding stagnant water from residential areas could play significant roles in preventing asymptomatic malaria among pregnant women in Ethiopia in general and in the study area in particular.
Acknowledgements
We would like to thank all who participated actively and played positive roles in the success of this MPH project and the manuscript emanated from its main findings. Nevertheless, our special thanks go to St. Paul’s Hospital Millennium Medical College, Ethiopian Field Epidemiology Training Program coordinators, study participant Zone and District Health offices’ staff, Village leaders, Health facilities’ Nurses, Midwives, Laboratory personnel, Health Extension Workers and Study Participants for their unreserved cooperation and supports given towards the success of this study.
Abbreviations
- ACT
Artemisinin-based combination therapy
- AOR
Adjusted Odd Ratio
- ANC
Antenatal Care
- COR
Crude Odd Ratio
- CI
Confidence Interval
- EDTA
Ethylene Diamine Tetra Acetic acid
- EFETP
Ethiopian Field Epidemiology Training Program
- FMOH
Federal Ministry of Health
- IRB
Institutional Review Board
- IRS
Indoor Residual Spray
- ITN
Insecticide-Treated Net
- LLINs
Long-Lasting Insecticidal Nets
- PCR
Polymerase Chain Reaction
- PI
Principal Investigator
- RDT
Rapid Diagnostic Test
- SOP
Standard Operating Procedures
- SPSS
Statistical Package for Social Science
- SPHMMC
St. Paul’s Hospital Millennium Medical College
- WBC
White Blood Cell
- WHO
World Health Organization
Author contributions
FB designed the study, developed the proposal, participated in the data collection, performed analysis and interpretation of data, and drafted the paper. TM contributed significantly from its inception up to the manuscript preparation and its critical editing. FL contributed to the design the study, proposal writing, data analysis, and interpretation of the study. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The data upon which the result is based could be accessed as a reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board (IRB) of St. Paul’s Hospital Millennium Medical College and the permission letter was also obtained from East Shoa Zone. Then the letter was delivered to the Boset District Health office and the respective villages. The purpose and importance of the study were explained to the participants. In addition, written consent was obtained from each study participant above the age of 18. But from those study participants under the age of 18 assents or permissions were sought from their respective parents or guardians. Blood smears were taken by experienced laboratory technicians under an aseptic technique using sterile gloves and disposable sterile lancets. Codes were used to ensure the confidentiality of Laboratory results. Pregnant women with positive for malaria parasite were linked to the nearest health facilities for treatment according to the national malaria guideline.
Consent for publication
Not applicable.
Competing interests
Both authors declared that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . Guidelines for the treatment of malaria. Geneva: World Health Organization; 2015. [PubMed] [Google Scholar]
- 2.WHO . Global malaria report. Geneva: World Health Organization; 2018. [Google Scholar]
- 3.Huynh B-T, Cottrell G, Cot M, Briand V. Burden of malaria in early pregnancy: a neglected problem? Clin Infect Dis. 2015;60:598–604. doi: 10.1093/cid/ciu848. [DOI] [PubMed] [Google Scholar]
- 4.Moya-Alvarez V, Abellana R, Cot M. Pregnancy-associated malaria and malaria in infants: an old problem with present consequences. Malar J. 2014;13:271. doi: 10.1186/1475-2875-13-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jagannathan P. How does malaria in pregnancy impact malaria risk in infants? BMC Med. 2018;16:13–15. doi: 10.1186/s12916-018-1210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dellicour S, Tatem AJ, Guerra CA, Snow RW, ter Kuile FO. Quantifying the number of pregnancies at risk of malaria in 2007: a demographic study. PLoS Med. 2010;7:e1000221. doi: 10.1371/journal.pmed.1000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schantz-Dunn J, Nour NM. Malaria and pregnancy: a global health perspective. Rev Obstet Gynecol. 2009;2:186–192. [PMC free article] [PubMed] [Google Scholar]
- 8.Griffin JT, Déirdre Hollingsworth T, Reyburn H, Drakeley CJ, Riley EM, et al. Gradual acquisition of immunity to severe malaria with increasing exposure. Proc Biol Sci. 2015;282:20142657. doi: 10.1098/rspb.2014.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nzobo BJ, Ngasala BE. Kihamia CM Prevalence of asymptomatic malaria infection and use of different malaria control measures among primary school children in Morogoro municipality Tanzania. Malar J. 2015;14:491. doi: 10.1186/s12936-015-1009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hochman S, Kim K. The impact of HIV and malaria coinfection: what is known and suggested venues for further study. Interdiscip Perspect Infect Dis. 2009;2009:617954. doi: 10.1155/2009/617954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO . High burden to high impact: a targeted malaria response. Geneva: World Health Organization; 2018. [Google Scholar]
- 12.Ngondi JM, Graves PM, Gebre T, Mosher AW, Shargie EB, Emerson PM, et al. Which nets are being used: factors associated with mosquito net use in Amhara, Oromia and Southern Nations, Nationalities and Peoples’ Regions of Ethiopia. Malar J. 2011;10:92. doi: 10.1186/1475-2875-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taffese HS, Hemming-Schroeder E, Koepfli C, Tesfaye G, Lee MC, Kazura J, Yan GY, et al. Malaria epidemiology and interventions in Ethiopia from 2001 to 2016. Infect Dis Poverty. 2018;7:103. doi: 10.1186/s40249-018-0487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alemu A, Abebe G, Tsegaye W, Golassa L. Climatic variables and malaria transmission dynamics in Jimma town. South West Ethiopia Parasit Vectors. 2011;4:30. doi: 10.1186/1756-3305-4-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO . World Health Organization (WHO) Guidelines for malaria. Geneva: World Health Organization; 2021. [Google Scholar]
- 16.Cairns M, Roca-Feltrer A, Garske T, Wilson AL, Diallo D, Milligan PJ, et al. Estimating the potential public health impact of seasonal malaria chemoprevention in African children. Nat Commun. 2012;3:881. doi: 10.1038/ncomms1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Branch OL, Casapia WM, Gamboa DV, Hernandez JN, Alava FF, Roncal N, et al. Clustered local transmission and asymptomatic Plasmodium falciparum and Plasmodium vivax malaria infections in a recently emerged, hypoendemic Peruvian Amazon community. Malar J. 2005;4:27. doi: 10.1186/1475-2875-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cucunubá Z, Guerra Á, Rahirant SJ, Rivera JA, Cortés LJ, Nicholls RS. Asymptomatic Plasmodium spp. infection in Tierralta Colombia. Mem Inst Oswaldo Cruz. 2008;103:668–673. doi: 10.1590/S0074-02762008000700007. [DOI] [PubMed] [Google Scholar]
- 19.Harris I, Sharrock WW, Bain LM, Gray KA, Bobogare A, Boaz L, et al. A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J. 2010;9:254. doi: 10.1186/1475-2875-9-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee PW, Liu CT, Rampao HS, Do Rosario VE, Shaio MF. Pre-elimination of malaria on the island of Príncipe. Malar J. 2010;9:26. doi: 10.1186/1475-2875-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sturrock HJW, Hsiang MS, Cohen JM, Smith DL, Greenhouse B, Bousema T. Targeting asymptomatic malaria infections: active surveillance in control and elimination. PLoS Med. 2013;10:e1001467. doi: 10.1371/journal.pmed.1001467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Subussa BW, Eshetu T, Degefa T, Ali MM. Asymptomatic Plasmodium infection and associated factors among pregnant women in the Merti district, Oromia. Ethiopia PLoS ONE. 2021;16:e0248074. doi: 10.1371/journal.pone.0248074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Worku L, Damtie D, Endris M, Getie S, Aemero M. Asymptomatic malaria and associated risk factors among school children in Sanja Town, Northwest Ethiopia. Int Sch Res Notices. 2014 doi: 10.1155/2014/303269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nega D, Dana D, Tefera T, Eshetu T. Prevalence and predictors of asymptomatic malaria parasitemia among pregnant women in the rural surroundings of Arbaminch Town. South Ethiopia PLoS One. 2015;10:e0123630. doi: 10.1371/journal.pone.0123630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akiyama T, Pongvongsa T, Phrommala S, Taniguchi T, Inamine Y, Takeuchi R, et al. Asymptomatic malaria, growth status, and anaemia among children in Lao People’s Democratic Republic: a cross-sectional study. Malar J. 2016;15:3. doi: 10.1186/s12936-016-1548-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tilahun A, Id MY, Gelaye W, Tegegne B. Prevalence of asymptomatic Plasmodium species infection and associated factors among pregnant women attending antenatal care at Fendeka town health facilities, Jawi District, North west Ethiopia : a cross-sectional study. PLoS ONE. 2020;15:e0231477. doi: 10.1371/journal.pone.0231477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nwagha UI, Ugwu VO, Ukamaka Nwagha T, Anyaehie U. Asymptomatic Plasmodium parasitaemia in pregnant Nigerian women: almost a decade after Roll Back Malaria. Trans R Soc Trop Med Hyg. 2009;103:16–20. doi: 10.1016/j.trstmh.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 28.Francine N, Bakoua D, Fesser A, Kombo M, Vouvoungui JC, Koukouikila-Koussounda F. Characterization of asymptomatic Plasmodium falciparum infection and its risk factors in pregnant women from the Republic of Congo. Acta Trop. 2016;153:111–115. doi: 10.1016/j.actatropica.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 29.Fonseca JC, Arango EM. Asymptomatic plasmodial infection in pregnant women: a global scenario. J Vector Borne Dis. 2017;54:201–206. doi: 10.4103/0972-9062.217610. [DOI] [PubMed] [Google Scholar]
- 30.Agomo CO, Oyibo WA, Anorlu RI, Agomo PU. Prevalence of malaria in pregnant women in Lagos South-West Nigeria Korean. J Parasitol. 2009;47:179–183. doi: 10.3347/kjp.2009.47.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Briand V, Le Hesran JY, Mayxay M, Newton PN, Bertin G, Houzé S, et al. Prevalence of malaria in pregnancy in southern Laos: a cross-sectional survey. Malar J. 2016;15:436. doi: 10.1186/s12936-016-1492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sohail M, Shakeel S, Kumari S, Bharti A, Zahid F, Anwar S, et al. Prevalence of malaria infection and risk factors associated with anaemia among pregnant women in semiurban community of Hazaribag, Jharkhand India. Biomed Res Int. 2015;2015:40512. doi: 10.1155/2015/740512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khan WA, Galagan SR, Prue CS, Khyang J, Ahmed S, Ram M, et al. Asymptomatic Plasmodium falciparum malaria in pregnant women in the Chittagong Hill Districts of Bangladesh. PLoS ONE. 2014;9:e98442. doi: 10.1371/journal.pone.0098442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ayele DG, Zewotir TT, Mwambi HG. Prevalence and risk factors of malaria in Ethiopia. Malar J. 2012;11:195. doi: 10.1186/1475-2875-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boudová S, Divala T, Mawindo P, Cohee L, Kalilani-Phiri L, Thesing P, et al. The prevalence of malaria at first antenatal visit in Blantyre, Malawi declined following a universal bed net campaign. Malar J. 2015;14:422. doi: 10.1186/s12936-015-0945-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gontie GB, Wolde HF, Baraki AG. Prevalence and associated factors of malaria among pregnant women in Sherkole district, Benishangul Gumuz regional state. West Ethiopia BMC Infect Dis. 2020;20:573. doi: 10.1186/s12879-020-05289-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Golassa L, Baliraine FN, Enweji N, Erko B, Swedberg G, Aseffa A. Microscopic and molecular evidence of the presence of asymptomatic Plasmodium falciparum and Plasmodium vivax infections in an area with low, seasonal and unstable malaria transmission in Ethiopia. BMC Infect Dis. 2015;15:310. doi: 10.1186/s12879-015-1070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Degefa T, Zeynudin A, Zemene E, Aga DA, Yewhalaw D. High prevalence of gametocyte carriage among individuals with asymptomatic malaria: implications for sustaining malaria control and elimination efforts in Ethiopia. Hum Parasit Dis. 2016;8:17–25. doi: 10.4137/HPD.S34377. [DOI] [Google Scholar]
- 39.Belay M, Deressa W. Use of insecticide treated nets by pregnant women and associated factors in a pre-dominantly rural population in northern Ethiopia. Trop Med Int Health. 2008;13:1303–1313. doi: 10.1111/j.1365-3156.2008.02159.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data upon which the result is based could be accessed as a reasonable request.