Abstract
Acquired brain injury (ABI) is a leading cause of serious long-term disability resulting in substantial economic costs for post-ABI care. This study was conducted to estimate the socioeconomic burden of persons with ABI in Korea. We used a prevalence-based approach and societal perspective to estimate the direct medical, non-medical costs and indirect costs of ABI, including stroke, traumatic brain injury (TBI), and non-traumatic ABI (anoxia, brain tumor, encephalitis, meningitis, hydrocephalus, and other brain disorders) from 2015 to 2017. The study population included patients with ABI over 20 years of age and analyzed according to insurance types encompassing National Health Insurance and automobile insurance. The socioeconomic burden of ABI was 4.67, 5.18, and 5.73 trillion KRW (approximately 4,162, 4,612, and 5,106 million USD) from 2015 to 2017 and around 0.3% of Korea's GDP annually. Estimating by disease, the socioeconomic cost was 72.4% for stroke, 18.6% for TBI, and 9.0% for non-traumatic ABI. Calculated by cost component, medical costs and non-medical costs showed a slight increase every year. Through this study, establishment of rehabilitation systems maximizing the health and quality of life for injured persons remain the key public health strategy for ABI to reduce socioeconomic burden and financial policies to support patients should be needed.
Keywords: Brain Injuries; Stroke; Brain Injuries, Traumatic; Cost of Illness
HIGHLIGHTS
• This study was conducted to estimate the socioeconomic burden of acquired brain injury (ABI) in Korea.
• The socioeconomic burden of ABI was approximately 5 trillion KRW annually.
• The socioeconomic cost was 72% for stroke, 18% for traumatic brain injury (TBI), and 9% for non-traumatic ABI.
• Calculated by cost component, medical cost and non-medical cost increased slightly.
INTRODUCTION
Acquired brain injury (ABI) embraces a range of conditions involving rapid onset of brain injury, including trauma due to head injury, vascular event such as stroke, cerebral anoxia, toxic or metabolic insult such as hypoglycemia, and infection or inflammation [1,2,3,4]. It can result in serious long-term disability and severely reduce a survivor's quality of life. That is why extensive medical resources have been invested in order to find an effective treatment and prevent complications [5,6,7]. Consequently, patients with ABI face not only physical and mental problems, but also other problems, including economic burden, which make it difficult to maintain a regular lifestyle.
Estimates of the economic burden for ABI are available from previous studies [1,8,9,10,11,12]. In Korea, Kim et al. estimated the economic burden of brain disorders including stroke, traumatic brain injury (TBI), parkinsonism, and brain tumor from the individual and societal perspectives [8]. They revealed that, individual cost was 164 million KRW per patient and annual social burden was 9.9 trillion KRW after brain injury. Another study in Canada reported that ABI direct medical costs were ranged from $32,132 to $38,018 per patient, amounting to a total of $120.7 to $368.7 million per year [1]. In terms of stroke, the total annual economic burden due to stroke amounted to 4,148.8 billion KRW, with hemorrhagic stroke and cerebral infarction accounting for 2,201.6 and 1,947.2 billion KRW, respectively [9]. In the United States, stroke-related costs of $103.5 billion per year are incurred [10], while in the United Kingdom, stroke costs amounted to £8.9 billion per year, and direct medical expenses accounted for 5.5% of the total medical expenses of the National Health Service [11]. By expanding the scope to include other brain disorders, the economic burden of brain disease was found to cost €134 billion, exceeding half of the total economic burden [12].
As such, research on the overall impact of the socioeconomic burden of ABI on patients, caregivers, and society as a whole is scarce compared to the research interest on its physical and mental burden [13]. In particular, since previous studies of economic burden mainly focused on some diseases of ABI or calculated some components such as medical expenses, it is necessary to confirm the overall socioeconomic cost of the ABI. Because ABI consistently occurs in population groups that are capable of performing economic activities, it is necessary to establish a health care policy targeting this specific disease by identifying the medical costs and productive losses of ABIs. However, the studies to be used as evidence for this purpose are obviously lacking. In addition, since the cost incurred to patients and families may vary depending on the culture and economic conditions of each country, a study on Korean patients is necessary to establish a health care policy in Korea. Therefore, this study attempts to determine both the direct and indirect burden to patients and their families by estimating the socioeconomic costs of patients with ABI. In particular, by considering sex and age, this study intends to understand social losses caused by diseases from various perspectives.
MATERIALS AND METHODS
Framework of socioeconomic burden
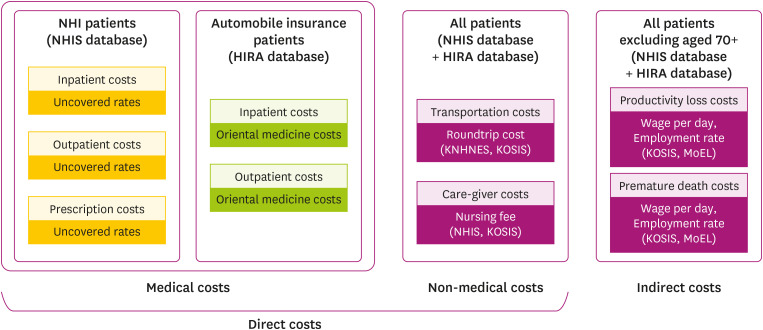
The socioeconomic burden of ABI consists of direct and indirect costs (Fig. 1) [14]. The former consists of medical and non-medical costs, while the latter consists of morbidity costs due to productivity loss and costs due to premature death. Medical costs refer to costs incurred to treat ABI; those incurred at medical institutions are termed “official medical costs,” while those constituting the purchase of general medicines, health supplements, medical devices, and orthoses for the purpose of preventing and treating diseases are termed “informal medical costs.” Non-medical costs include transportation and caregiver costs: the former are incurred when visiting a medical institution for treatment, while the latter are incurred in arranging for care from a family member or a professional caregiver while a patient is admitted to the hospital for treatment. Indirect costs constitute the cost of productivity loss, which is defined as the cost associated with the patient's own impairment or loss of labor capacity due to disease, or loss of economic productivity due to premature death due to disease.
Fig. 1. The concept of socioeconomic burden.
NHI, National Health Insurance; NHIS, National Health Insurance Service; HIRA, Health Insurance Review & Assessment Service; KNHNES, Korea National Health and Nutrition Examination Survey; KOSIS, Korean Statistical Information Service; MoEL, Ministry of Employment and Labor.
Before calculating the socioeconomic burden, the analysis perspective can be applied in various ways depending on the purpose of the study. In this study, all burdens arising from the disease were considered by applying the societal perspective. A prevalence-based approach was adopted to calculate the cost of medical use incurred during disease treatment by including all patients—without distinction—with prevailing ABI as well as newly diagnosed patients at any one time. That is, from 2015 to 2017, the socioeconomic burden was calculated by using the medical cost and medical use information measured for each year.
Study population and data source
The study population comprised patients with ABI over the age of 20 selected from 2015 to 2017. This study aimed to calculate the socioeconomic burden caused by diseases in Korea accurately by considering the medical use of patients with both National Health Insurance (NHI) and automobile insurance. ABI was defined as stroke, TBI, and non-traumatic ABI. Non-traumatic ABI was classified into anoxia, brain tumor, encephalitis, meningitis, hydrocephalus, and other brain injuries using the criteria of the Ontario Neurotrauma Foundation (ONF) in Canada (Supplementary Table 1) [15,16]. The definition of ABI among automobile insurance was applied slightly differently from that of NHI, but the disease group was excluded because car accidents were judged to have not affected the incidence and prevalence of brain tumor. In the claim data for each insurance type, if there is an ABI to a primary or secondary diagnosis, it was defined as the relevant disease. If the secondary diagnosis comprised several ABI disease codes, it was defined as a disease according to the proportion of patients by the disease group. That is, the diseases were sorted in the order of the largest number of patients or episodes and defined as the relevant disease. For example, if patient A had brain tumor and encephalitis codes in the secondary diagnosis, and did not have ABI in the primary diagnosis, this patient was defined as a brain tumor patient. The proportion of patients by disease group is presented in the Supplementary Table 2.
Various data sources were used to calculate the socioeconomic burden. The databases used in this study included the National Health Insurance Service (NHIS) database and the automobile insurance claim database from the Health Insurance Review & Assessment Service (HIRA) according to the patient's insurance type. Unlike the NHIS database, automobile insurance claim data can be used to confirm whether medical information is available at oriental medical institutions. This was included in the analysis. However, most of the automobile insurance were TBI patients, with other diseases generally making up a small proportion; therefore, it is difficult to estimate the non-medical and indirect costs of diseases other than TBI. Therefore, other data sources for calculating the socioeconomic burden were selected by referring to previous studies. The data source used and the scope of analysis of the study are shown in Fig. 1 and Supplementary Table 3.
Cost analysis
Direct costs
The direct costs of ABI were classified into medical and non-medical costs, calculated using the following equation:
| x = Age group (20–29,30–39,40–49,50–59,60–69,70+) |
| y = Sex (1 = male; 2 = female) |
| z = Type of medical institution (1 = medicine; 2 = oriental medicine) |
| α = Inpatients uncovered rate; β = Outpatients uncovered rate; γ = Prescription uncovered rate |
| In = Inpatient medical costs; Out = Outpatient medical costs; Drug = Prescription medical cost |
Medical costs were calculated by varying the formula according to each patient's insurance type and were examined separately by sex and age; the uncovered rate was calculated by reflecting the results of the 2017 Medical Expenses Survey [17].
The following formula was used to estimate non-medical costs:
| x = Age group (20–29,30–39,40–49,50–59,60–69,70+) |
| y = Sex (1 = male; 2 = female) |
| InP = Number of inpatients; OutP = Number of outpatients |
| InC = Number of hospitalizations; OutC = Number of outpatients visits |
| InR = Roundtrip transportation costs for hospitalization; OutR = Roundtrip transportation costs for outpatients visit |
| InL = Length of stay |
Non-medical costs were also separately estimated by sex and age. Round-trip transportation costs and daily nursing fees for hospital visits were considered to be costs between 2015 and 2017, reflecting the consumer price index of the corresponding item in the results of the Korea National Health & Nutrition Examination Survey (KNHANES) results in 2005 [18] and the Nursing Service Survey in 2013 [19], respectively. In Korea, traditionally, care of inpatients is performed by family members or professional caregivers. However, due to Middle East respiratory syndrome-related coronavirus (MERS), the perception of infection control in hospitals has changed, and nurses have begun taking care of patients [20]. Currently, only few hospitals are piloting a comprehensive nursing care service in which nurses perform nursing and care of inpatients. Nevertheless, there are still many factors that need to be addressed before the policy is implemented in Korean medical institutions. In this study, caregiver costs were estimated and included in the non-medical cost, in consideration of the traditional hospital environment in Korea.
Indirect costs
To estimate the indirect costs, the total production loss calculation method based on the human capital approach, used in many previous studies, was employed [14]. This method calculates the productivity cost as a result of the total lost time using hourly wages and taking into account the production time of the patient lost due to the disease. In other words, assuming that the patient's medical time is his or her production time or time spent at work, the basic wage for this period is substituted to confirm the monetary value of the lost production time. When using this method, it is assumed that patients over 70 years of age do not actually participate in economic activities; thus, the indirect costs of patients in this age group were excluded from the calculation. The formula used to calculate the indirect cost is as follows:
| x = Age group (20–29,30–39,40–49,50–59,60–69) |
| y = Sex (1 = male; 2 = female) |
| ω = discount rate (5%) |
| InL = Length of stay; OutL = Number of outpatient visits |
| EmRate = Employment rate |
| NumD = Number of deaths |
Indirect costs were also estimated separately by sex and age. The employment rate used for indirect costs was obtained from the Economically Active Population Survey data provided by Statistics Korea, while the average annual and daily wages were based on the Ministry of Employment and Labor's survey report on labor conditions by employment type. The discount rate used in calculating the indirect cost was calculated by applying a 5% discount in the same way as has been done in previous studies. All analyses used SAS 9.4 and the Microsoft Excel program.
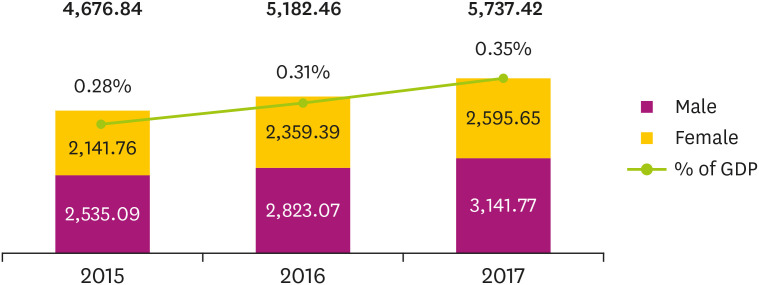
RESULTS
From 2015 to 2017, the socioeconomic burden caused by ABI was 4.67, 5.18, and 5.73 trillion KRW, and when converted into USD, these values amount to 4,162, 4,612, and 5,106 million USD, respectively. (Table 1, Fig. 2) Comparing the size of the socioeconomic burden of ABI in term of Korea's annual GDP reveals that the burden in 2015, 2016, and 2017 comprised approximately 0.28, 0.31, and 0.35% of the GDP, respectively. The socioeconomic burden of ABI for male patients was 2.53, 2.82, and 3.14 trillion KRW, resulting in an average annual cost of 2.83 trillion KRW. Female patients also showed a similar trend, and from 2015 to 2017, the burden was 2.14, 2.35, and 2.59 trillion KRW, resulting in an average annual burden of 2.36 trillion KRW. When socioeconomic burden was compared based on sex and age group, socioeconomic costs were higher for male patients of most age groups than for female patients, while the cost of the female patient group was approximately 1.5 times higher than that of the male patient group in the age group of 70 years or older.
Table 1. The socioeconomic burden of acquired brain injury in 2015–2017 (unit: 1 billion KRW).
| Age group | Total | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | |
| 20–29 | 109.94 | 114.43 | 117.74 | 114.03 | 70.39 | 73.96 | 76.68 | 73.68 | 39.55 | 40.47 | 41.06 | 40.36 |
| 30–39 | 192.96 | 205.97 | 203.09 | 200.67 | 123.94 | 130.97 | 129.33 | 128.08 | 69.02 | 75.00 | 73.76 | 72.59 |
| 40–49 | 449.62 | 471.50 | 490.18 | 470.43 | 293.39 | 309.36 | 325.59 | 309.45 | 156.23 | 162.14 | 164.59 | 160.99 |
| 50–59 | 937.48 | 1,018.01 | 1,086.12 | 1,013.87 | 631.88 | 688.02 | 738.55 | 686.15 | 305.60 | 329.99 | 347.57 | 327.72 |
| 60–69 | 941.54 | 1,072.82 | 1,200.17 | 1,071.51 | 608.45 | 699.79 | 789.79 | 699.34 | 333.09 | 373.03 | 410.38 | 372.17 |
| 70+ | 2,045.30 | 2,299.72 | 2,640.12 | 2,328.38 | 807.04 | 920.95 | 1,081.82 | 936.60 | 1,238.26 | 1,378.77 | 1,558.30 | 1,391.78 |
| Total | 4,676.84 | 5,182.46 | 5,737.42 | 5,198.91 | 2,535.09 | 2,823.07 | 3,141.77 | 2,833.31 | 2,141.76 | 2,359.39 | 2,595.65 | 2,365.60 |
| Total (1 million USD) | 4,162.39 | 4,612.39 | 5,106.30 | 4,627.03 | 2,256.23 | 2,512.53 | 2,796.17 | 2,521.64 | 1,906.16 | 2,099.86 | 2,310.13 | 2,105.39 |
1 KRW = $0.00089.
Fig. 2. The socioeconomic burden of ABI in 2015–2017.
Table 2 shows the results of confirming the socioeconomic burden by cost component. Medical and non-medical costs tended to increase slightly every year. In terms of sex, medical cost accounted for the largest share of the total burden for both male and female patients, followed by non-medical costs and indirect costs. The direct costs, combining medical and non-medical costs, accounted for about 94% (among males) and 97% (among females) of the total burden. When only medical expenses were considered, these values were 74% (among male) and 72% (among females) of the total burden. While both medical and non-medical costs increased with age in both sexes, indirect costs accounted for the highest proportion for both men and women in their 40s and 50s. (Supplementary Tables 4, 5, 6).
Table 2. The socioeconomic burden of acquired brain injury by cost component in 2015–2017 (Unit: 1 billion KRW).
| Cost components | Total | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | ||
| Medical costs | |||||||||||||
| 20–29 | 82.31 | 86.24 | 90.32 | 86.29 | 52.32 | 54.57 | 57.73 | 54.88 | 29.99 | 31.67 | 32.59 | 31.42 | |
| 30–39 | 134.58 | 144.66 | 143.34 | 140.86 | 86.65 | 92.56 | 91.37 | 90.19 | 47.93 | 52.10 | 51.97 | 50.67 | |
| 40–49 | 317.60 | 333.88 | 348.94 | 333.47 | 207.69 | 219.79 | 232.47 | 219.98 | 109.91 | 114.09 | 116.47 | 113.49 | |
| 50–59 | 668.67 | 730.95 | 779.36 | 726.33 | 450.33 | 492.40 | 529.00 | 490.58 | 218.34 | 238.55 | 250.36 | 235.75 | |
| 60–69 | 710.94 | 813.50 | 911.70 | 812.05 | 456.38 | 526.52 | 595.08 | 525.99 | 254.56 | 286.99 | 316.62 | 286.06 | |
| 70+ | 1,470.81 | 1,664.43 | 1,923.33 | 1,686.19 | 622.14 | 714.14 | 841.80 | 726.03 | 848.67 | 950.29 | 1,081.53 | 960.16 | |
| Total | 3,384.92 | 3,773.67 | 4,196.99 | 3,785.19 | 1,875.51 | 2,099.98 | 2,347.45 | 2,107.65 | 1,509.41 | 1,673.68 | 1,849.53 | 1,677.54 | |
| Non-medical costs | |||||||||||||
| 20–29 | 23.44 | 23.59 | 22.61 | 23.21 | 13.89 | 14.78 | 14.14 | 14.27 | 9.55 | 8.81 | 8.47 | 8.94 | |
| 30–39 | 36.65 | 37.28 | 35.39 | 36.44 | 22.48 | 22.23 | 21.71 | 22.14 | 14.17 | 15.05 | 13.68 | 14.30 | |
| 40–49 | 83.87 | 86.18 | 87.90 | 85.99 | 53.67 | 55.24 | 57.20 | 55.37 | 30.20 | 30.94 | 30.70 | 30.62 | |
| 50–59 | 187.78 | 197.63 | 209.71 | 198.38 | 126.09 | 134.11 | 142.88 | 134.36 | 61.70 | 63.52 | 66.84 | 64.02 | |
| 60–69 | 195.75 | 218.35 | 242.00 | 218.70 | 126.73 | 143.13 | 160.41 | 143.42 | 69.01 | 75.22 | 81.60 | 75.28 | |
| 70+ | 512.92 | 567.95 | 644.98 | 575.28 | 184.90 | 206.81 | 240.02 | 210.58 | 328.02 | 361.14 | 404.96 | 364.71 | |
| Total | 1,040.42 | 1,130.98 | 1,242.60 | 1,138.00 | 527.76 | 576.30 | 636.35 | 580.14 | 512.66 | 554.68 | 606.24 | 557.86 | |
| Indirect costs | |||||||||||||
| 20–29 | 7.64 | 8.25 | 8.55 | 8.15 | 4.18 | 4.61 | 4.80 | 4.53 | 3.46 | 3.64 | 3.75 | 3.62 | |
| 30–39 | 21.73 | 24.03 | 24.36 | 23.37 | 14.82 | 16.18 | 16.25 | 15.75 | 6.91 | 7.85 | 8.11 | 7.62 | |
| 40–49 | 48.15 | 51.44 | 53.34 | 50.98 | 32.03 | 34.34 | 35.92 | 34.10 | 16.11 | 17.10 | 17.42 | 16.88 | |
| 50–59 | 81.02 | 89.43 | 97.05 | 89.17 | 55.45 | 61.51 | 66.68 | 61.21 | 25.57 | 27.92 | 30.37 | 27.95 | |
| 60–69 | 34.86 | 40.97 | 46.47 | 40.76 | 25.34 | 30.14 | 34.30 | 29.93 | 9.52 | 10.82 | 12.17 | 10.83 | |
| Total | 193.39 | 214.11 | 229.77 | 212.43 | 131.82 | 146.78 | 157.96 | 145.52 | 61.57 | 67.34 | 71.81 | 66.91 | |
Among the ABIs, the results calculated by classifying the disease into strokes, TBI, and non-traumatic ABIs are shown in Table 3. The socioeconomic burden caused by stroke was the highest for both male and female patients and comprised 70.4% (males) and 74.9% (females) of the total socioeconomic burden of ABI, respectively. In addition, the socioeconomic cost of stroke increased with age for both males and females; particularly for female patients over the age of 70 years, it accounts for approximately 66% of the socioeconomic cost of stroke for the total female patients. The socioeconomic burden of TBI was higher in the elderly patient group for both males and females, but the cost for each age group was not extremely concentrated in the elderly population as in the case of stroke. The socioeconomic cost of non-traumatic ABI was the highest among male patients in their 50s and females who were in their 70s and older (Supplementary Tables 7, 8, 9).
Table 3. The socioeconomic burden of acquired brain injury by disease in 2015–2017 (Unit: 1 billion KRW).
| Diseases | Total | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | ||
| Stroke | |||||||||||||
| 20–29 | 16.94 | 18.17 | 18.81 | 17.97 | 10.26 | 11.14 | 11.38 | 10.93 | 6.68 | 7.03 | 7.43 | 7.05 | |
| 30–39 | 65.67 | 75.38 | 72.60 | 71.22 | 45.28 | 51.22 | 48.38 | 48.29 | 20.40 | 24.17 | 24.22 | 22.93 | |
| 40–49 | 250.60 | 264.03 | 283.03 | 265.88 | 175.93 | 186.68 | 200.88 | 187.83 | 74.67 | 77.35 | 82.14 | 78.05 | |
| 50–59 | 624.50 | 683.28 | 736.42 | 681.40 | 442.50 | 484.33 | 525.19 | 484.00 | 182.00 | 198.95 | 211.23 | 197.40 | |
| 60–69 | 696.24 | 793.86 | 884.03 | 791.38 | 455.38 | 524.43 | 592.67 | 524.16 | 240.86 | 269.43 | 291.36 | 267.22 | |
| 70+ | 1,667.39 | 1,868.77 | 2,140.89 | 1,892.35 | 640.45 | 729.10 | 851.04 | 740.20 | 1,026.94 | 1,139.67 | 1,289.85 | 1,152.15 | |
| Total | 3,321.34 | 3,703.50 | 4,135.78 | 3,720.21 | 1,769.79 | 1,986.89 | 2,229.54 | 1,995.41 | 1,551.55 | 1,716.61 | 1,906.24 | 1,724.80 | |
| TBI | |||||||||||||
| 20–29 | 72.00 | 71.32 | 75.11 | 72.81 | 46.81 | 46.99 | 48.88 | 47.56 | 25.19 | 24.33 | 26.22 | 25.25 | |
| 30–39 | 86.90 | 86.66 | 90.25 | 87.93 | 56.82 | 56.50 | 59.84 | 57.72 | 30.08 | 30.16 | 30.40 | 30.22 | |
| 40–49 | 136.65 | 136.04 | 139.57 | 137.42 | 85.06 | 86.06 | 88.79 | 86.64 | 51.59 | 49.98 | 50.78 | 50.78 | |
| 50–59 | 208.48 | 214.39 | 227.79 | 216.89 | 132.33 | 138.25 | 147.02 | 139.20 | 76.15 | 76.13 | 80.77 | 77.68 | |
| 60–69 | 160.79 | 179.32 | 202.02 | 180.71 | 105.71 | 120.46 | 133.33 | 119.83 | 55.08 | 58.86 | 68.69 | 60.88 | |
| 70+ | 224.24 | 253.37 | 298.92 | 258.84 | 124.58 | 141.37 | 169.83 | 145.26 | 99.67 | 112.00 | 129.09 | 113.58 | |
| Total | 889.07 | 941.10 | 1,033.64 | 954.60 | 551.31 | 589.63 | 647.69 | 596.21 | 337.76 | 351.47 | 385.95 | 358.39 | |
| Non-TBI | |||||||||||||
| 20–29 | 24.45 | 28.58 | 27.57 | 26.87 | 13.32 | 15.83 | 16.42 | 15.19 | 11.13 | 12.76 | 11.15 | 11.68 | |
| 30–39 | 40.39 | 43.93 | 40.24 | 41.52 | 21.85 | 23.26 | 21.11 | 22.07 | 18.54 | 20.67 | 19.13 | 19.45 | |
| 40–49 | 62.38 | 71.43 | 67.59 | 67.13 | 32.40 | 36.63 | 35.92 | 34.98 | 29.98 | 34.81 | 31.67 | 32.15 | |
| 50–59 | 104.50 | 120.35 | 121.91 | 115.59 | 57.04 | 65.44 | 66.35 | 62.94 | 47.46 | 54.90 | 55.56 | 52.64 | |
| 60–69 | 84.51 | 99.63 | 114.12 | 99.42 | 47.36 | 54.91 | 63.79 | 55.35 | 37.16 | 44.73 | 50.33 | 44.07 | |
| 70+ | 92.09 | 110.24 | 128.50 | 110.28 | 42.01 | 50.48 | 60.95 | 51.15 | 50.08 | 59.76 | 67.55 | 59.13 | |
| Total | 408.33 | 474.16 | 499.93 | 460.81 | 213.99 | 246.54 | 264.54 | 241.69 | 194.34 | 227.62 | 235.40 | 219.12 | |
TBI, traumatic brain injury.
The socioeconomic costs of ABIs were calculated according to insurance type, and the results are shown in Table 4. In the case of NHI, from 2015 to 2017, the costs of male patients were 2.28, 2.56, and 2.87 trillion KRW each year, while the costs for female patients were 1.87, 2.09, and 2.31 trillion KRW each year. The socioeconomic burden of automobile insurance increased equally for both men and women every year, with costs for men reaching 254.8, 259.7, and 270.8 billion KRW from 2015 to 2017, respectively, and costs for women reaching 201.0, 201.1, and 211.0 billion KRW, respectively, over the same period. In the case of NHI, the socioeconomic burden increased with age for both men and women, with the burden of patients over 70 years of age being about 10 times higher than that of patients in their 20s. However, automobile insurance showed a slightly different trend: the socioeconomic burden of automobile insurance patients was the highest among men and women in their 50s (the middle-aged group) (Supplementary Tables 10, 11, 12, 13, 14, 15, 16, 17, 18).
Table 4. The socioeconomic burden of acquired brain injury by insurance type in 2015–2017 (Unit: 1 billion KRW).
| Insurance type | Total | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | 2015 | 2016 | 2017 | Annual average | ||
| NHI | |||||||||||||
| 20–29 | 67.71 | 73.01 | 75.10 | 71.94 | 42.56 | 45.96 | 48.07 | 45.53 | 25.15 | 27.05 | 27.03 | 26.41 | |
| 30–39 | 138.18 | 152.07 | 148.82 | 146.36 | 90.37 | 97.73 | 95.85 | 94.65 | 47.81 | 54.34 | 52.98 | 51.71 | |
| 40–49 | 370.49 | 395.33 | 413.98 | 393.27 | 249.98 | 267.30 | 283.49 | 266.93 | 120.51 | 128.02 | 130.48 | 126.34 | |
| 50–59 | 829.10 | 911.00 | 978.20 | 906.10 | 574.31 | 631.23 | 681.33 | 628.96 | 254.79 | 279.78 | 296.86 | 277.14 | |
| 60–69 | 863.43 | 989.52 | 1,110.11 | 987.69 | 564.93 | 653.19 | 739.89 | 652.67 | 298.50 | 336.32 | 370.22 | 335.01 | |
| 70+ | 1,893.91 | 2,136.93 | 2,461.26 | 2,164.04 | 758.10 | 867.87 | 1,022.29 | 882.75 | 1,135.81 | 1,269.07 | 1,438.97 | 1,281.28 | |
| Total | 4,162.83 | 4,657.86 | 5,187.47 | 4,669.39 | 2,280.26 | 2,563.29 | 2,870.93 | 2,571.49 | 1,882.57 | 2,094.57 | 2,316.54 | 2,097.90 | |
| Automobile insurance | |||||||||||||
| 20–29 | 45.69 | 45.06 | 46.38 | 45.71 | 27.83 | 27.99 | 28.61 | 28.15 | 17.86 | 17.07 | 17.77 | 17.57 | |
| 30–39 | 54.78 | 53.91 | 54.26 | 54.32 | 33.57 | 33.24 | 33.48 | 33.43 | 21.21 | 20.66 | 20.78 | 20.89 | |
| 40–49 | 79.13 | 76.18 | 76.20 | 77.17 | 43.41 | 42.06 | 42.10 | 42.52 | 35.72 | 34.12 | 34.10 | 34.65 | |
| 50–59 | 108.37 | 107.01 | 107.93 | 107.77 | 57.57 | 56.80 | 57.22 | 57.20 | 50.81 | 50.22 | 50.70 | 50.58 | |
| 60–69 | 78.11 | 83.30 | 90.07 | 83.83 | 43.52 | 46.60 | 49.90 | 46.67 | 34.59 | 36.70 | 40.16 | 37.15 | |
| 70+ | 89.82 | 95.45 | 107.05 | 97.44 | 48.94 | 53.09 | 59.53 | 53.85 | 40.88 | 42.36 | 47.52 | 43.59 | |
| Total | 455.90 | 460.91 | 481.88 | 466.23 | 254.83 | 259.78 | 270.84 | 261.82 | 201.07 | 201.13 | 211.05 | 204.42 | |
NHI, National Health Insurance
DISCUSSION
In this study, the socioeconomic burden of ABI in Korea was calculated based on direct and indirect costs and the results are summarized as follows. From 2015 to 2017, the socioeconomic burden of ABI were 4.67, 5.18, and 5.73 trillion KRW, respectively. Male ABI patients incurred costs ranging from approximately 2.53 to 3.14 trillion KRW, while female ABI patients incurred costs ranging from 2.14 to 2.59 trillion KRW. In terms of specific components of the socioeconomic burden, medical costs totaled 3.38, 3.77, and 4.19 trillion KRW, while non-medical costs totaled 1.04, 1.13, 1.24 trillion KRW, respectively. Indirect costs were estimated to be 0.19, 0.21, and 0.22 trillion KRW, respectively, with the proportion of medical expenses being considerably large. In terms of diseases, strokes accounted for more than half of the total socioeconomic burden, and by type of insurance, the socioeconomic cost of health insurance patients was about 10 times that of automobile insurance. Several points of discussion can be confirmed through the analysis of these results.
The study results revealed that the socioeconomic burden of ABI is higher in male patients than in females in most age groups except for those over the age of 70 years. This is thought to be due to the higher incidence of ABI in male patients and the higher cost burden due to the larger number of patients. A previous study has reported that male patients are more likely to develop ABIs such as TBI due to external factors such as traffic accidents or violence than are females, and the socioeconomic burden is also estimated to be high as a result. A previous study confirmed the burden of the TBI disease mechanism, which revealed that the years of potential life lost and productivity loss as a result of TBI due to factors such as car accidents, pistol injuries, falls, and motorcycle accidents are approximately thrice as higher in males than in females [21]. A similar trend could be confirmed by the results of this study; further studies, based on our results should closely examine why the socioeconomic burden of male patients is higher than that of female patients. With regard to indirect costs, the burden of male patients was much higher than that of females, which also affects the incidence of diseases; however, the main cause is believed to be due to the differences in male and female employment rates [22].
In this study, the socioeconomic burden of ABI was found to incur a cost of 4–5 trillion KRW each year, accounting for approximately 0.3% of Korea's GDP. Upon comparing the present study with other studies on socioeconomic burden, the following differences can be identified. A study comparing the socioeconomic cost of TBI to different countries' GDP in 2016 revealed that it constituted approximately 0.815%, 0.351%, and 0.328% of the GDP of the United States, Australia, and the United Kingdom, respectively [23]. Considering that Korea's ABI socioeconomic cost accounts for approximately 0.3% of GDP per year, the economic burden of other countries is relatively higher than that of Korea. Unlike this study, in a study that calculated the socioeconomic burden according to the disease outbreak mechanism, the socioeconomic burden caused by road injury was found to be 0.106% of the GDP for high-income countries, 0.120% for low-income countries, and 0.138%–0·144% for middle-income countries [24]. Comparing these results with the socioeconomic burden of automobile insurance patients in Korea revealed that the overall burden is higher than that of Korea. In Korea, the government pays about 70% of the total medical expenditures through the NHI, and patients and their families pay the rest. However, various policies are being implemented to reduce the economic burden on patients and their families by bolstering stronger coverage for chronic diseases or rare diseases, and the government pays up to 100% of medical expenses for such diseases [25]. Among the ABIs defined in this study, stroke and brain tumor are included in Korea's strong covered medical services; it may therefore be possible to solve the economic difficulties experienced by patients and their families to some extent. Nevertheless, considering the study finding that medical costs account for a very large share of the socioeconomic burden of ABI, direct medical expense support policies should continue to be guaranteed for patients and their families. Also, the support policy for patients and their families needs to be established more carefully because unpredictable enormous medical expenses such as uncovered medical expenses may occur, or income may be lost due to disease. In addition, research on calculating the socioeconomic burden of diseases can not only provide evidence of the support system for patients and their families after the disease diagnosis, but also establish of a system to prevent further incidence of the disease, improve related infrastructure, and change public perception. Therefore, it is necessary to consider ways to alleviate the burden on patients by continuously conducting these studies.
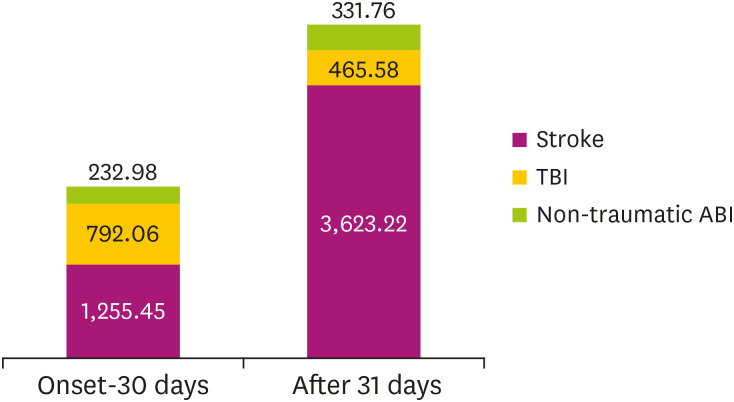
The socioeconomic cost of strokes is excessively high, showing a sharp increase in the patient group over 50 years old. This is also closely related to the incidence of diseases. In Korea, 1.71% of adults over the age of 19 have suffered strokes, which afflict 232 individuals per 100,000 population every year [26]. Thus, it is one of the chronic diseases that requires constant management. This study revealed that the socioeconomic burden of stroke increased by about 11% every year between 2015 and 2017 from 3.32 to 4.13 trillion KRW, and the socioeconomic burden of middle-aged patients over 50 years old was about eight times higher than that of patients in their 20s and 40s. Therefore, it is necessary to not only reexamine the stroke prevention and management policy for middle-aged and older patients in order to prepare a suitable medical policy but also reorganize rehabilitation care plans after the stroke, which is necessary for patients in this age group. Medical costs account for a much larger share of the socioeconomic burden of ABI compared to other components. Fig. 3 shows the classification of medical expenses by defining the acute phase as the 30 days from the onset of the disease and the convalescent phase as the period after that. ABI's medical costs accounted for approximately 30% of the total medical costs within 30 days after disease onset, that is, in the acute phase. When classified by disease, stroke has relatively high medical costs in the convalescent phase and TBI in the acute phase. The relatively large amount of acute medical costs for TBI patients might be explained by the fact that the most necessary rehabilitation medical services during the convalescent phase are inadequate. Therefore, from the standpoint of rehabilitation medicine, it is necessary to provide systematic rehabilitation medical guidelines for TBI patients after the acute stage to provide the timely rehabilitation medical care necessary in the convalescent phase.
Fig. 3. The medical costs between acute and convalescent phase.
TBI, traumatic brain injury.
Examining the results of calculating the socioeconomic burden by insurance type reveals that the socioeconomic burden of NHI increases with age, whereas it is the highest among patients in their 50s for automobile insurance. Considering that the number of driver's license holders by age in Korea is the highest among those in their 40s and 50s, it is believed that automobile insurance patients suffer ABIs caused by external factors such as accidents rather than aging in determining the occurrence or severity of diseases. Therefore, it is necessary to systematically establish a health care policy adapted to automobile insurance patients taking these characteristics into account. It is also necessary to improve the emergency medical system immediately after the accident in order to reduce the severity of the disease or the treatment period, and various preventive policies that can prevent accidents should be formulated.
In this study, ABIs caused by various external factors were studied. Because of their characteristics, the psychological burden of the patient and family should also be considered. In general, to calculate the psychological burden of a disease, the pain, grief, and suffering (PGS) cost is used, which converts the mental pain, sadness, or stress caused by a traffic accident into a monetary value. In the case of brain damage, it is necessary to determine the extent of psychological pain experienced by patients and their families to formulate a mental healthcare policy and to understand them more objectively. According to the research results of the Korea Transport Institute, the PGS cost caused by traffic accidents in 2016 was about 19 trillion KRW [27,28]. If this is applied to our study, it can be assumed that a psychological burden of 19 trillion KRW occurs every year. This is about 2.3 times higher than the calculated socioeconomic burden of this study. Therefore, ABI patients require not only economic support but also medical support and policies for mental health.
This study was the first study in Korea to calculate the socioeconomic burden by focusing on ABIs. It was able to confirm the burden of patients with brain damage, considering even data on automobile insurance claims that have been difficult to access in other studies. In addition, by calculating the socioeconomic burden trend over three years, it was confirmed that the burden on patients and families increased every year. These findings can provide the basic data necessary for policy recommendations to prepare for the economic problems for patients and their families. Nevertheless, there are some limitations to the study.
In this study, socioeconomic burden was calculated for patients with various insurance types, and different data sources were used for this purpose. However, due to the characteristics of the data, it was only possible to confirm whether or not patients in the automobile insurance patient group utilized oriental medical institutions. Therefore, it was not possible to confirm the use of oriental medical institutions through NHIS database. Considering that the outpatient utilization rate of oriental medical institutions for NHI, confirmed mainly by frequent outpatient diseases in a previous study is 7.4% and the outpatient utilization rate using both medicine and oriental medical institutions is 20.8% [29], the actual medical cost incurred in the medical field is considered to be higher than the medical cost calculated in this study.
Since automobile insurance developed diseases due to car accidents, the disease group except for TBI includes a relatively small proportion of patients compared to that of the NHI. Moreover, with regard to the non-traumatic ABI group, the cause of disease was not established. Thus, the socioeconomic burden was calculated considering the characteristics of the disease. Moreover, in the case of automobile insurance, the proportion of non-traumatic ABI patients was too low and was excluded from the calculation of the indirect cost. Therefore, the estimated socioeconomic burden may be slightly less than the actual socioeconomic burden.
Since this study focused on productivity loss in calculating indirect costs, the indirect costs for premature death were not estimated in the patient group over 70 years of age [14]. However, if the indirect cost of death is calculated by focusing on death, it can be calculated even for the patient group over 70 years old and will be higher than the current socioeconomic burden.
ABIs often cause permanent disability and require rehabilitation service. Therefore, although the cost of medical equipment and orthoses, which are the most important factors in rehabilitation, should be considered in calculating the burden, it could not be calculated due to the lack of accessibility to the data. If these factors are considered, medical costs may be higher than the current estimated cost.
Contrary to the limitations presented above, patients in car accidents often suffer damage to various parts of the body. In this study, since ABI was identified according to the International Classification of Diseases, 10th Revision (ICD-10) disease classification, injury occurring in other organs was not considered. Therefore, it is likely that the socioeconomic burden of automobile insurance may be overestimated by including the cost of damage to organs other than the brain. In future studies, it will be necessary to estimate the burden taking into account the complexity, such as accompanying injuries.
In this study, the socioeconomic burden of ABI was calculated to amount to about 5 trillion KRW annually, accounting for about 0.3% of Korea's GDP. In addition, medical and non-medical costs increased slightly every year, so the burden on patients and their families could also be expected to increase every year. Based on the results of this study, it is necessary to establish and improve on the policy to support medical expenses in order to alleviate the economic burden of patients with ABI and their families. Also, since ABI is a disease that causes permanent disabilities and one that is difficult to cure, it is necessary to establish an emergency medical system for preventing trauma, to prepare a strategy to organically link with rehabilitation service, and to establish a systematic plan for rehabilitation treatment. Establishing a support system for adapting to daily life after returning home and to society to resume economic activities after treatment is necessary for patients to live the same life as before being diagnosed with the disease. Future research will be necessary to calculate the burden of ABI as a result of various causes such as falls and traffic accidents.
Footnotes
Funding: This study was supported by a grant from the Korean Society for NeuroRehabilitation 2020. This work was supported by National Research Foundation of Korea (NRF) grant funded by the Korea government (grand number: NRF-2017R1A2B3005912).
Conflict of Interest: The corresponding author of this manuscript is an editor of Brain & NeuroRehabilitation. The corresponding author did not engage in any part of the review and decision-making process for this manuscript. The other authors have no potential conflicts of interest to disclose.
SUPPLEMENTARY MATERIALS
ICD-10 codes for acquired brain injury-related diseases
Number of patients with acquired brain injury for 3 years by insurance type
Resource and source of cost data
The medical costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)
References
- 1.Chen A, Bushmeneva K, Zagorski B, Colantonio A, Parsons D, Wodchis WP. Direct cost associated with acquired brain injury in Ontario. BMC Neurol. 2012;12:76. doi: 10.1186/1471-2377-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grace JJ, Kinsella EL, Muldoon OT, Fortune DG. Post-traumatic growth following acquired brain injury: a systematic review and meta-analysis. Front Psychol. 2015;6:1162. doi: 10.3389/fpsyg.2015.01162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fleminger S, Ponsford J. Long term outcome after traumatic brain injury. BMJ. 2005;331:1419–1420. doi: 10.1136/bmj.331.7530.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradt J, Magee WL, Dileo C, Wheeler BL, McGilloway E. Music therapy for acquired brain injury. Cochrane Database Syst Rev. 2010;7:CD006787. doi: 10.1002/14651858.CD006787.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Rees L, Marshall S, Hartridge C, Mackie D, Weiser M, Erabi Group Cognitive interventions post acquired brain injury. Brain Inj. 2007;21:161–200. doi: 10.1080/02699050701201813. [DOI] [PubMed] [Google Scholar]
- 6.Olver JH, Ponsford JL, Curran CA. Outcome following traumatic brain injury: a comparison between 2 and 5 years after injury. Brain Inj. 1996;10:841–848. doi: 10.1080/026990596123945. [DOI] [PubMed] [Google Scholar]
- 7.Thornhill S, Teasdale GM, Murray GD, McEwen J, Roy CW, Penny KI. Disability in young people and adults one year after head injury: prospective cohort study. BMJ. 2000;320:1631–1635. doi: 10.1136/bmj.320.7250.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim K, Leigh J, Oh BM, Jung SH, Lee KM, Park SW, Chun MH, Jung HY, Kim I, Kim SH, Han TR. The cost of brain disorder: individual and social cost. Brain Neurorehabil. 2010;3:86–93. [Google Scholar]
- 9.Kim HJ, Kim YA, Seo HY, Kim EJ, Yoon SJ, Oh IH. The economic burden of stroke in 2010 in Korea. J Korean Med Assoc. 2012;55:1226–1236. [Google Scholar]
- 10.Girotra T, Lekoubou A, Bishu K, Ovbiagele B. The true cost of stroke: assessment of direct and indirect cost of stroke among all age groups in United States of America from 2003 to 2014. Stroke. 2019;50(Suppl 1):A73. [Google Scholar]
- 11.McGregor K, Pentland B. Head injury rehabilitation in the U.K.: an economic perspective. Soc Sci Med. 1997;45:295–303. doi: 10.1016/s0277-9536(96)00345-0. [DOI] [PubMed] [Google Scholar]
- 12.Fineberg NA, Haddad PM, Carpenter L, Gannon B, Sharpe R, Young AH, Joyce E, Rowe J, Wellsted D, Nutt DJ, Sahakian BJ. The size, burden and cost of disorders of the brain in the UK. J Psychopharmacol. 2013;27:761–770. doi: 10.1177/0269881113495118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. Clinicoecon Outcomes Res. 2013;5:281–287. doi: 10.2147/CEOR.S44625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim y, Shin S, Park J, Jung Y, Kim J, Lee T, et al. Costing methods in healthcare. Seoul: National Evidence-based Healthcare Collaborating Agency; 2013. [Google Scholar]
- 15.Colantonio A, Chan V, Zagorski B, Parsons D, Vander Laan R. Ontario acquired brain injury (ABI) dataset project phase III: highlights: number of episodes of care and causes of brain injury. Toronto: Acquired Brain Injury Research Lab.; 2012. [Google Scholar]
- 16.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36:1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1. [DOI] [PubMed] [Google Scholar]
- 17.National Health Insurance Service (NHIS) 2017 Survey on the benefit coverage rate of National Health Insurance. Wonju: National Health Insurance Service; 2018. [Google Scholar]
- 18.Korea Centers for Disease Control Prevention. The third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005. Cheongwon: Korea Centers for Disease Control and Prevention; 2005. [Google Scholar]
- 19.National Health Insurance Service (NHIS) Nursing service survey: Ministry of Health and Welfare (MoHW) Wonju: National Health Insurance Service; 2013. [Google Scholar]
- 20.Kim Y. Nurses' experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control. 2018;46:781–787. doi: 10.1016/j.ajic.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kayani NA, Homan S, Yun S, Zhu BP. Health and economic burden of traumatic brain injury: Missouri, 2001–2005. Public Health Rep. 2009;124:551–560. doi: 10.1177/003335490912400412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Statistics Korea. Economically active population survey. [accessed on 30 May 2021]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1DA7001S&vw_cd=MT_ZTITLE&list_id=B11&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE.
- 23.Parsonage M. Traumatic brain injury and offending: an economic analysis. London: Centre for Mental Health; 2016. [Google Scholar]
- 24.Chen S, Kuhn M, Prettner K, Bloom DE. The global macroeconomic burden of road injuries: estimates and projections for 166 countries. Lancet Planet Health. 2019;3:e390–e398. doi: 10.1016/S2542-5196(19)30170-6. [DOI] [PubMed] [Google Scholar]
- 25.Park EC. Moon Jae-in Government's plan for benefit expansion in National Health Insurance. Health Policy Manag. 2017;27:191–198. [Google Scholar]
- 26.Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, Kim WJ, Kim EG, Kim JG, Kim JM, Kim JT, Kim C, Nah HW, Park KY, Park MS, Park JM, Park JH, Park TH, Park HK, Seo WK, Seo JH, Song TJ, Ahn SH, Oh MS, Oh HG, Yu S, Lee KJ, Lee KB, Lee K, Lee SH, Lee SJ, Jang MU, Chung JW, Cho YJ, Choi KH, Choi JC, Hong KS, Hwang YH, Kim SE, Lee JS, Choi J, Kim MS, Kim YJ, Seok J, Jang S, Han S, Han HW, Hong JH, Yun H, Lee J, Bae HJ. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke. 2019;21:42–59. doi: 10.5853/jos.2018.03125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shim J, Yu J, Park J, Park B. Estimation of transport accident costs in 2016. Sejong: The Korea Transport Institute; 2018. [Google Scholar]
- 28.Shim J, Sung N, Yoo J, Park J, Cho H, Shim G, et al. Development of estimation methodology for traffic accident costs in Korea. Sejong: The Korea Transport Institute; 2013. [Google Scholar]
- 29.Park YS, Kim JS. Analysis of the current status outpatient utilization of medical and Korean traditional medical institutions: focuse on outpatient frequent outpatient diseases. J Korean Med Assoc. 2017;60:912–919. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ICD-10 codes for acquired brain injury-related diseases
Number of patients with acquired brain injury for 3 years by insurance type
Resource and source of cost data
The medical costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury by disease in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury by insurance type in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury among NHI patients by disease in 2015–2017 (Unit: 1 million KRW)
The medical costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)
The non-medical costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)
The indirect costs of acquired brain injury among automobile insurance patients by disease in 2015–2017 (Unit: 1 million KRW)