Abstract
Transcranial direct current stimulation (tDCS) has considerable potential as a useful method in the field of neurorehabilitation. However, the safety of tDCS for the human is primarily based on theoretical evidence related to electricity, and the safety information of applying tDCS to the human is only available from researcher's reporting. Based on tDCS studies with human and animal subjects and simulation-based studies of the safety of current stimulation in the past 20 years, this review investigated the safety of tDCS application to the human body. No severe complications have been reported in either adults or children for tDCS at an intensity of 4 mA or less, within a period of 60 minutes per day, using commonly applied 25 or 35 cm2 electrodes. According to animal studies, the amount of electricity used for tDCS is less than 5% of the amount that permanently changes brain tissue, thereby ensuring safety to a certain extent. In order to increase the efficacy of tDCS for neurorehabilitation and to minimize even trivial complications in the human screening of exclusion criteria should be conducted with detailed observations of complications.
Keywords: Transcranial Direct Current Stimulation, Safety, Neurorehabilitation
Highlights
• To date, there have been no serious side effects reported in conventional transcranial direct current stimulation (tDCS).
• Sufficient risk evaluation should be conducted before tDCS applying.
• Careful attention must be paid to safety during tDCS.
INTRODUCTION
Attempts to achieve therapeutic effects by applying electricity to the human body have long been made in the medical field. For instance, ancient practitioners of medicine such as Hippocrates, Scribonius, Largus, and Galen treated migraines using the torpedo fish, which generates strong electric currents (30 A and above) [1,2]. As it became possible for humans to generate electricity through advances in modern science in the 18th century, it became common to apply direct current to the head of patients with psychiatric diseases [3,4]. However, the use of this therapeutic modality decreased since the danger of applying strong electricity to humans exceeded any proven benefits. In the 20th century, numerous studies reported that a relatively weak current of a few milliamperes applied constantly for a certain amount of time changed cellular activity. Subsequently, attempts have been made to achieve therapeutic effects by inducing changes in brain cortical excitability using transcranial direct current stimulation (tDCS), in which direct current is applied non-invasively through electrodes attached to the scalp. Non-invasive direct current stimulation has emerged as an important method of treatment in neurorehabilitation [5,6,7,8,9,10].
Safety has always been an issue regarding treatments using electricity. After the basic scientific principles of electricity and its effects on the human were theoretically established, early researchers investigated the use of electricity at intensity levels that they believed would not be harmful to the human. These studies established an experimental basis for safe stimulation parameters of tDCS. However, actual responses to current stimulation can vary across individual bodies, and this variability poses challenges for establishing a definitive and consistent stimulation guideline. The safety of tDCS needs to be regularly scrutinized through meta-analyses and systematic reviews involving safety issues and continuous data collection from future studies. From this perspective, this review explores unintended reactions and complications of tDCS and discusses strategies to minimize adverse effects and maximize desired effects.
APPROPRIATE STRENGTH, DURATION, AND METHODS OF tDCS APPLICATION
Three main factors (intensity, duration, and electrode size) determine the total amount of electricity applied to the human brain in tDCS. Currently, the most commonly used intensity is less than 4 mA, the duration is less than 60 minutes, and electrode size is 25 cm2 (5 × 5 cm) or 35 cm2 (5 × 7 cm) [11,12,13]. In earlier studies, a lower intensity of less than 0.5 mA was applied to the motor area for a few seconds to minutes using a 25 cm2 electrode. In Priori et al. [8], direct current of 0.075–0.5 mA was applied to the motor area through 25 cm2 (5 × 5 cm) electrodes for 7 seconds. In comparison to the motor evoked potential (MEP) measured without current stimulation, the amplitude of the MEP decreased significantly and proportionally to the intensity of electricity. In that study, complications or unintended responses of tDCS were not mentioned at all. In the study of Nitsche et al. [9], the intensity of the stimulus was increased to 0.2–1.0 mA, and the duration was also increased to 1–5 minutes. That study also did not address complications in detail, but concluded that tDCS is a useful method to control brain excitability painlessly.
tDCS studies increased explosively during the 10 years after the study of Nitsche et al. [9], and the parameters of electricity stimuli used in studies became established. The intensity was usually 1–2 mA (maximum 4 mA), duration was 20 minutes (maximum 40 minutes), and the electrode size was either 25 cm2 (5 × 5 cm) or 35 cm2 (5 × 7 cm). In 2011, Brunoni et al. [12] published a systematic review on the adverse effects of tDCS, synthesizing data from a decade's worth of studies on this issue. This study reviewed adverse effects and safety in 209 tDCS studies published between 1998 and 2010 that met the eligibility criteria. Of those studies, 117 (56%) mentioned adverse effects during treatment, whereas 92 (44%) did not mention adverse effects at all. All 117 studies that mentioned adverse effects used active stimulation, and 82 of those 117 studies also included sham stimulation. The most frequently reported adverse effect was itching, which was reported in 46 of the 117 (39.3%) studies that used active stimulation. Among the 82 studies that used sham stimulation, 27 studies (32.9%) reported itching. The percentage was higher when active stimulation was given, but the difference was not statistically significant. The second most frequent adverse effect was tingling, reported in 22.2% of studies with active stimulation and 18.3% of studies with sham stimulation. The third most frequent adverse effect was headache, reported in 14.8% and 16.2% of active stimulation studies and sham stimulation studies, respectively. The percentage was higher in sham stimulation studies, but the difference was not statistically significant. The last main adverse effect reported was burning, reported in 8.7% of studies with active stimulation and 10% of studies with sham simulation. Other discomfort was reported in 10.4% of active stimulation studies and 13.4% of sham stimulation studies, demonstrating a slightly higher frequency in the sham stimulation group. Other than these reversable minor adverse effects, no severe adverse effects that were irrecoverable or required professional treatment were reported.
In principle, the abovementioned adverse effects could occur due to the effect of electricity itself, but given that the percentage of patients reporting adverse effects was similar in the sham stimulation groups, it can be inferred that the tDCS procedure itself, such as attaching the electrodes on the scalp and securing electrodes on the head using compression bandages, can cause adverse effects. With the amount of electricity used for tDCS applied to the human brain, it was theoretically expected that no severe adverse effects would occur, and the results were in line with this expectation. In their systematic review, Brunoni et al. [12] analyzed studies that used less than or equal to 1.5 mA and more than 1.5 mA separately. Twenty-nine of the 82 (35.4%) studies with a current intensity of less than or equal to 1.5 mA reported itching, while 17 of the 35 (48.6%) studies with current intensity exceeding 1.5 mA reported itching. The proportion was higher when the intensity was greater, but the difference was not statistically significant. In contrast, proportion of tingling reported was higher when the intensity was lower, with tingling reported in 20 of the 82 (24.4%) studies that used less than or equal to 1.5 mA and 6 of the 35 (17.1%) studies that used a current intensity exceeding 1.5 mA. This difference was also not statistically significant; therefore, no meaningful differences according to electricity intensity were found.
Animal studies were conducted before tDCS was applied to the human body, and have continued subsequently to ensure safety more definitively and to improve efficacy. In 2009, Liebetanz et al. [14] studied histological changes in the rat cerebrum with increasing amounts of electricity. A charge density of more than 52,400 C/m2 caused irreversible histological changes. The charge density when 4 mA is applied using a 35 cm2 electrode for 30 minutes is roughly 2,057 C/m2. Therefore, since the amount of electricity used on humans is approximately 4% of the amount that can damage the brain tissue of rats, it is inferred that the procedure is acceptably safe [14,15]. However, there are limits to applying results from animal studies to humans, so continued research is needed to ensure safety. A report found that cathodal tDCS was helpful in an animal model of acute cerebral infarction. However, other studies reported that in the hyper-acute period (1 day or less), there were negative effects such as anodal tDCS expanding the area of infarction and the blood-brain barrier being destroyed or, at the least, there were no positive effects. More conclusive research is required to apply tDCS to patients with acute cerebral infarction [16,17,18].
Studies investigating the safety of tDCS and aiming to suggest guidelines have continued, and in 2017, Antal and many other researchers [13] published a large amount of study data. However, even in their study, clear safety guidelines about the intensity and duration of stimulation were not presented; instead, only the safety of currently used parameters based on animal studies (including the research of Liebetanz et al. [14] discussed above) was explained. Only minor adverse effects were reported, with a similar frequency as reported by Brunoni et al. [12], and no severe adverse effects directly related to tDCS were described. A potential severe adverse effect of tDCS is seizure, which can be caused by any procedure that stimulates the central nervous system. Therefore, it is theoretically possible for tDCS to cause seizures. However, in studies published from 2000 to 2016, only one case of seizure was reported. The patient had epilepsy, and it was reported that there was no evidence of a causal relationship between tDCS and the seizure [19]. There is a high risk that tDCS can cause a manic switch in patients with bipolar disorder; for this reason, patients' history must be understood well. Antal et al. [13] presented a few detailed recommendations for the application of tDCS. When attaching sponge-like electrodes, saline solution rather than tap water should be used. Abrading the skin area before attaching the electrodes is not a meaningful step; instead, just a light cleaning is suggested. To prevent severe damage to the skin, close attention should always be paid to the attachment of the electrodes.
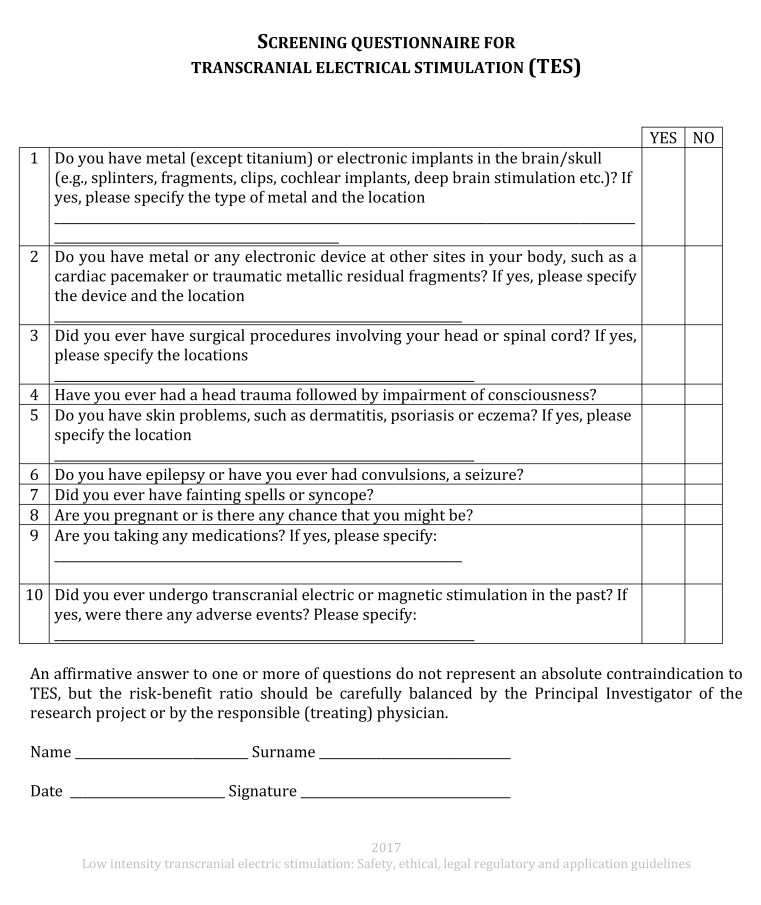
Although tDCS is not theoretically expected to have more adverse effects on pregnant than non-pregnant women, but no proper studies have yet been conducted, so additional studies to confirm its safety are necessary. When tDCS is indicated, the benefit-risk ratio should be examined closely. Moreover, it has been reported that there was no major difference in safety when tDCS was combined with other equipment such as electroencephalography, electromyography, magnetoencephalography, and MRI compared to when tDCS is used alone. In their systematic review, Antal et al. [13] emphasizes that in order to minimize adverse effects when using tDCS, a structured pre-survey is very important. A form based on the consensus of related research teams is provided on the Göttingen University research center's website; the use of this form is recommended (Fig. 1).
Fig. 1. Screening questionnaire for TES from http://www.neurologie.uni-goettingen.de/downloads.html.
TES, transcranial electrical stimulation.
SAFETY IN CHILDREN
Systematic research on safety related to children or infants is difficult to find in animal studies. Anderson et al. [20] in 2017 used a hypoxia-ischemia model in 7-day-old rats and conducted tDCS on the 14th day after damage (in 21-day-old rats). Muscle strength and physical capacity improved in the tDCS group compared to the comparison group; however, their study did not review safety specifically. In contrast, tDCS studies with human children started a long time ago. In an early study, Bogdanov et al. [21] reported that hyperkinesis was reduced after conducting transcranial electrical stimulation using a 6.0 cm2 electrode, which is much smaller than what is commonly used in current practice, with a current intensity of 0.2–0.8 mA among 21 children with cerebral palsy (age range, 6 to 18 years). Their study did not mention adverse effects. In the study of Alon et al. [22], electrical stimulation of 0.5 mA using 11.34 cm2 electrodes was given to 7 children with cerebral palsy (age range, 2.5 to 7.5 years), and there were no particular adverse effects in any participating children. Subsequently, studies with children using similar parameters to those used in current clinical practice have been conducted. Krishnan et al. [23] analyzed tDCS studies with children and reported that children's adverse effects were no more severe than those of adults. However, particularly thorough safety tests should be conducted of electrical stimulation in children. Multiple studies using computational electrical current modeling reported that when using the same parameters, electricity transmission can be 2 to 7 times stronger in children than in adults [24,25,26]. Based on these studies, it is recommended that the intensity of electrical stimulation in children should not exceed 1 mA.
In 2020, the Canadian researchers Zewdie et al. [27] published the results of a large-scale prospective study that tracked the safety of tDCS (1 mA intensity for 20 minutes) in child participants for 10 years (from 2009 to 2018). In total, 92 children from ages 6 to 18 (mean age 14) were included, and there were no cases of severe adverse effects. Headache, neck pain, unpleasant tingling, light-headedness, itching and burning, and mild nausea were reported, which were not substantially different from the adverse effects of tDCS reported in other studies. The current literature suggests that the adverse effects of tDCS are not different between children and adults. However, considering that children's brains are continuing to develop and it is possible that tDCS can have unknown effects on children's brains distinct from its effects on adults' brains, further studies should investigate this issue. It is also suggested that the intensity of the electrical stimulus should not exceed 1 mA, keeping in mind that children's brains are more receptive of electrical stimuli than adults' brains, as mentioned before.
SAFETY OF EXTRACEPHALIC ELECTRODE MONTAGE
An important technical aspect of conducting tDCS is the electrode montage. The most commonly used technique has been intracephalic montage, wherein both the active electrode and reference electrode are attached to the scalp. However, some studies have attached the active electrode to the scalp above the brain target area and the reference electrode on extracephalic areas such as the arm or chest. When 2 sets of electrodes are used to provide stimulation, it is difficult to attach 2 active electrodes and 2 reference electrodes on the scalp simultaneously. Thus, some studies have used a montage where the reference electrodes are attached to an extracephalic area [28,29,30]. In relation to safety, the theoretical issue of an extracephalic montage is that as the current flows to narrow areas in the brain such as the brain stem, it can affect the cardiopulmonary center and the autonomic center, among others. Therefore, clinical studies and computer simulation studies on the safety of extracephalic montage have been conducted. The computer simulation study by Im et al. [31] calculated the current density in the brainstem after placing the active electrode on the left primary motor cortex and the reference electrode on the right temporal lobe, right supraorbital region, right deltoid, left deltoid, under the chin, or on the right buccinator muscle. Regardless of where the reference was attached, the calculated current density in the brainstem was not statistically significantly different.
Noetscher et al. [32] conducted a study using similar methods. When the reference electrode was attached on the arm, the electric density was greater in the white matter, a deeper area in the brain, than the density measured with an intracephalic montage, but there was no difference in the brainstem. No severe adverse effects have been reported in studies using extracephalic montage in humans. In a study by Chang et al. [33] of patients with schizophrenia, symptoms improved after delivering 20 minutes of 2 mA stimulation twice a day for 5 weeks with anodal electrodes attached to either side of the prefrontal cortex and cathodal electrodes on either side of the forearms. Safety was evaluated by measuring blood pressure, respiratory rate, heart rate, and heart rate variability, and no meaningful changes or adverse effects were observed. Synthesizing the results from extant studies, it can be concluded that extracephalic montage can be used safely when necessary.
SAFETY OF IMPLANTED DEVICES
Since tDCS applies electricity to the human body artificially, in principle, it should not be conducted when an electrical device is implanted in the body. However, Iannone et al. [34] conducted 15 sessions of 30-minute cerebellar tDCS at 2 mA intensity with a 35 cm2 electrode in patients who had deep brain stimulators (DBSs) in the subthalamic nucleus for the treatment of generalized dystonia. The DBSs were turned off while tDCS stimulation was delivered. It was reported that symptoms improved, and no malfunction of the DBS devices occurred. Roncero et al. [35] delivered 2 mA for 30 minutes with a 35 cm2 anodal electrode attached to the dorsolateral prefrontal region and a cathodal electrode on the opposite arm to 7 older adults (aged 77 to 92) with pacemakers, and reported no damage after stimulation. However, only a few such attempts have been made; therefore, in principle, tDCS should not be conducted when a metal or electrical device is implanted in the body.
CONCLUSION
tDCS has long been used in the medical field for a very long time. Given the long history of applying electricity to the human, theoretical knowledge of the effects of electricity on the human is thought to be sufficient. Basic scientific research on tDCS has been conducted, and adverse effects or unintended phenomena have been regularly reported, analyzed, and organized. The safety of the commonly used parameters of less than 4 mA intensity using a 25 or 35 cm2 electrode for less than 60 minutes per day has been relatively securely established on the basis of numerous studies. Nonetheless, the safety of tDCS has been established through passively reported information; therefore, careful attention must be paid to safety continuously while applying tDCS If efforts are made to minimize even trivial adverse effects by conducting sufficient pre-surveys of tDCS recipients, tDCS will secure a place as an effective treatment method in neurorehabilitation.
Footnotes
Conflict of Interest: The author has no potential conflicts of interest to disclose.
References
- 1.Cambiaghi M, Sconocchia S. Scribonius Largus (probably before 1CE-after 48CE) J Neurol. 2018;265:2466–2468. doi: 10.1007/s00415-018-8739-5. [DOI] [PubMed] [Google Scholar]
- 2.Tsoucalas G, Karamanou M, Lymperi M, Gennimata V, Androutsos G. The “torpedo” effect in medicine. Int Marit Health. 2014;65:65–67. doi: 10.5603/IMH.2014.0015. [DOI] [PubMed] [Google Scholar]
- 3.Aldini G. Essai théorique et expérimental sur le galvanisme: avec une série d'expériences faites en présence des Commissaires de l'Institut national de France et en divers amphithéatres anatomiques de Londres. Paris: De l'Imprimerie de Fournier fils; 1804. [Google Scholar]
- 4.Cambiaghi M, Parent A. From Aldini's galvanization of human bodies to the Modern Prometheus. Medicina Hist. 2018;2:27–37. [Google Scholar]
- 5.Terzuolo CA, Bullock TH. Measurement of imposed voltage gradient adequate to modulate neuronal firing. Proc Natl Acad Sci U S A. 1956;42:687–694. doi: 10.1073/pnas.42.9.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lolas F. Brain polarization: behavioral and therapeutic effects. Biol Psychiatry. 1977;12:37–47. [PubMed] [Google Scholar]
- 7.Elbert T, Lutzenberger W, Rockstroh B, Birbaumer N. The influence of low-level transcortical DC-currents on response speed in humans. Int J Neurosci. 1981;14:101–114. doi: 10.3109/00207458108985821. [DOI] [PubMed] [Google Scholar]
- 8.Priori A, Berardelli A, Rona S, Accornero N, Manfredi M. Polarization of the human motor cortex through the scalp. Neuroreport. 1998;9:2257–2260. doi: 10.1097/00001756-199807130-00020. [DOI] [PubMed] [Google Scholar]
- 9.Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527:633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving activities of daily living, and physical and cognitive functioning, in people after stroke. Cochrane Database Syst Rev. 2016;3:CD009645. doi: 10.1002/14651858.CD009645.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nikolin S, Huggins C, Martin D, Alonzo A, Loo CK. Safety of repeated sessions of transcranial direct current stimulation: a systematic review. Brain Stimulat. 2018;11:278–288. doi: 10.1016/j.brs.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 12.Brunoni AR, Amadera J, Berbel B, Volz MS, Rizzerio BG, Fregni F. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int J Neuropsychopharmacol. 2011;14:1133–1145. doi: 10.1017/S1461145710001690. [DOI] [PubMed] [Google Scholar]
- 13.Antal A, Alekseichuk I, Bikson M, Brockmöller J, Brunoni AR, Chen R, Cohen LG, Dowthwaite G, Ellrich J, Flöel A, Fregni F, George MS, Hamilton R, Haueisen J, Herrmann CS, Hummel FC, Lefaucheur JP, Liebetanz D, Loo CK, McCaig CD, Miniussi C, Miranda PC, Moliadze V, Nitsche MA, Nowak R, Padberg F, Pascual-Leone A, Poppendieck W, Priori A, Rossi S, Rossini PM, Rothwell J, Rueger MA, Ruffini G, Schellhorn K, Siebner HR, Ugawa Y, Wexler A, Ziemann U, Hallett M, Paulus W. Low intensity transcranial electric stimulation: safety, ethical, legal regulatory and application guidelines. Clin Neurophysiol. 2017;128:1774–1809. doi: 10.1016/j.clinph.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liebetanz D, Koch R, Mayenfels S, König F, Paulus W, Nitsche MA. Safety limits of cathodal transcranial direct current stimulation in rats. Clin Neurophysiol. 2009;120:1161–1167. doi: 10.1016/j.clinph.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 15.Chhatbar PY, George MS, Kautz SA, Feng W. Charge density, not current density, is a more comprehensive safety measure of transcranial direct current stimulation. Brain Behav Immun. 2017;66:414–415. doi: 10.1016/j.bbi.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoon KJ, Oh BM, Kim DY. Functional improvement and neuroplastic effects of anodal transcranial direct current stimulation (tDCS) delivered 1 day vs. 1 week after cerebral ischemia in rats. Brain Res. 2012;1452:61–72. doi: 10.1016/j.brainres.2012.02.062. [DOI] [PubMed] [Google Scholar]
- 17.Peruzzotti-Jametti L, Cambiaghi M, Bacigaluppi M, Gallizioli M, Gaude E, Mari S, Sandrone S, Cursi M, Teneud L, Comi G, Musco G, Martino G, Leocani L. Safety and efficacy of transcranial direct current stimulation in acute experimental ischemic stroke. Stroke. 2013;44:3166–3174. doi: 10.1161/STROKEAHA.113.001687. [DOI] [PubMed] [Google Scholar]
- 18.Zhang KY, Rui G, Zhang JP, Guo L, An GZ, Lin JJ, He W, Ding GR. Cathodal tDCS exerts neuroprotective effect in rat brain after acute ischemic stroke. BMC Neurosci. 2020;21:21. doi: 10.1186/s12868-020-00570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekici B. Transcranial direct current stimulation-induced seizure: analysis of a case. Clin EEG Neurosci. 2015;46:169. doi: 10.1177/1550059414540647. [DOI] [PubMed] [Google Scholar]
- 20.Anderson CL, Tessler BJ, DeMarse TB, Douglas-Escobar M, Rossignol C, Nelson R, Kasinadhuni AK, King M, Bose P, Weiss MD, Carney PR. Transcranial direct current stimulation enhances recovery from motor deficits following hypoxia-ischemia in neonatal rats. Neurol Disord Therap. 2017;1:1–5. [Google Scholar]
- 21.Bogdanov OV, Pinchuk DY, Pisar'kova EV, Shelyakin AM, Sirbiladze KT. The use of the method of transcranial micropolarization to decrease the severity hyperkineses in patients with infantile cerebral palsy. Neurosci Behav Physiol. 1994;24:442–445. doi: 10.1007/BF02359800. [DOI] [PubMed] [Google Scholar]
- 22.Alon G, Syron SC, Smith GV. Is transcranial electrical stimulation (TCES) a safe intervention for children with cerebral palsy? Neurorehabil Neural Repair. 1998;12:65–71. [Google Scholar]
- 23.Krishnan C, Santos L, Peterson MD, Ehinger M. Safety of noninvasive brain stimulation in children and adolescents. Brain Stimulat. 2015;8:76–87. doi: 10.1016/j.brs.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kessler SK, Minhas P, Woods AJ, Rosen A, Gorman C, Bikson M. Dosage considerations for transcranial direct current stimulation in children: a computational modeling study. PLoS One. 2013;8:e76112. doi: 10.1371/journal.pone.0076112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chhatbar PY, Ramakrishnan V, Kautz S, George MS, Adams RJ, Feng W. Transcranial direct current stimulation post-stroke upper extremity motor recovery studies exhibit a dose-response relationship. Brain Stimulat. 2016;9:16–26. doi: 10.1016/j.brs.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ciechanski P, Carlson HL, Yu SS, Kirton A. Modeling transcranial direct-current stimulation-induced electric fields in children and adults. Front Hum Neurosci. 2018;12:268. doi: 10.3389/fnhum.2018.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zewdie E, Ciechanski P, Kuo HC, Giuffre A, Kahl C, King R, Cole L, Godfrey H, Seeger T, Swansburg R, Damji O, Rajapakse T, Hodge J, Nelson S, Selby B, Gan L, Jadavji Z, Larson JR, MacMaster F, Yang JF, Barlow K, Gorassini M, Brunton K, Kirton A. Safety and tolerability of transcranial magnetic and direct current stimulation in children: prospective single center evidence from 3.5 million stimulations. Brain Stimulat. 2020;13:565–575. doi: 10.1016/j.brs.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 28.Park SH, Seo JH, Kim YH, Ko MH. Long-term effects of transcranial direct current stimulation combined with computer-assisted cognitive training in healthy older adults. Neuroreport. 2014;25:122–126. doi: 10.1097/WNR.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 29.Angius L, Mauger AR, Hopker J, Pascual-Leone A, Santarnecchi E, Marcora SM. Bilateral extracephalic transcranial direct current stimulation improves endurance performance in healthy individuals. Brain Stimulat. 2018;11:108–117. doi: 10.1016/j.brs.2017.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang CC, Kao YC, Chao CY, Tzeng NS, Chang HA. Examining bi-anodal transcranial direct current stimulation (tDCS) over bilateral dorsolateral prefrontal cortex coupled with bilateral extracephalic references as a treatment for negative symptoms in non-acute schizophrenia patients: a randomized, double-blind, sham-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2020;96:109715. doi: 10.1016/j.pnpbp.2019.109715. [DOI] [PubMed] [Google Scholar]
- 31.Im CH, Park JH, Shim M, Chang WH, Kim YH. Evaluation of local electric fields generated by transcranial direct current stimulation with an extracephalic reference electrode based on realistic 3D body modeling. Phys Med Biol. 2012;57:2137–2150. doi: 10.1088/0031-9155/57/8/2137. [DOI] [PubMed] [Google Scholar]
- 32.Noetscher GM, Yanamadala J, Makarov SN, Pascual-Leone A. Comparison of cephalic and extracephalic montages for transcranial direct current stimulation--a numerical study. IEEE Trans Biomed Eng. 2014;61:2488–2498. doi: 10.1109/TBME.2014.2322774. [DOI] [PubMed] [Google Scholar]
- 33.Chang CC, Kao YC, Chao CY, Tzeng NS, Chang HA. The effects of bi-anodal tDCS over the prefrontal cortex regions with extracephalic reference placement on insight levels and cardio-respiratory and autonomic functions in schizophrenia patients and exploratory biomarker analyses for treatment response. Int J Neuropsychopharmacol. 2021;24:40–53. doi: 10.1093/ijnp/pyaa063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iannone A, Allam N, Brasil-Neto JP. Safety of transcranial direct current stimulation in a patient with deep brain stimulation electrodes. Arq Neuropsiquiatr. 2019;77:174–178. doi: 10.1590/0004-282X20190019. [DOI] [PubMed] [Google Scholar]
- 35.Roncero C, Mardigyan V, Service E, Singerman J, Whittaker KC, Friedman M, Chertkow H. Investigation into the effect of transcranial direct current stimulation on cardiac pacemakers. Brain Stimulat. 2020;13:89–95. doi: 10.1016/j.brs.2019.08.010. [DOI] [PubMed] [Google Scholar]