Abstract
Background and study aims Recently, the utility of endoscopic ultrasound-guided intervention without fistula dilation (EUS-IV WoD) has been reported to prevent adverse events. We clinically evaluated cases in which EUS-IV WoD was attempted using a novel self-expandable metallic stent (SEMS); this is a fully covered, laser-cut SEMS that has a tapered and stiff tip specifically designed for a 0.025-inch guidewire and a relatively thin, 7F delivery system.
Patients and methods We retrospectively evaluated cases wherein EUS-IV WoD was attempted using the novel SEMS between March and December 2021.
Results Treatment of 11 patients by EUS-IV WoD with the novel SEMS was attempted. The technical success rate for EUS-IV was 100 % and the clinical success rate was 100 %; the success rate for EUS-IV WoD was 72.8 %. Of these, the procedural success rate for EUS-IV WoD was 100 % in EUS-biliary drainage (BD) and 57.1 % in non-EUS-BD. Early adverse events were observed in 27.3 % of patients (3/11): mild abdominal pain in two patients and moderate bleeding in one patient. The abdominal pain cases were both cases of EUS-IV WoD failure and required fistula dilation.
Conclusions The novel stent may be useful for EUS-IV WoD, especially in EUS-BD.
Introduction
Endoscopic retrograde cholangiopancreatography is considered the first choice for drainage in obstructive jaundice 1 . Endoscopic ultrasound-guided biliary drainage (EUS-BD), including EUS-guided hepaticogastrostomy (EUS-HGS) and EUS-guided choledochoduodenostomy (EUS-CDS), is a useful alternative in cases in which transpapillary drainage is not possible 2 . In addition to EUS-BD, the utility of EUS intervention (EUS-IV) has been reported for non-EUS-BD, such as gallbladder drainage (EUS-GBD), gastroenterostomy (EUS-GE), and cyst drainage (EUS-CD), as an alternative to percutaneous or surgical drainage. When performing EUS-IV, it is primarily necessary to dilate the fistula before stent placement. Consequently, during the period between fistula dilation and stent insertion, drainage contents, such as bile and cystic fluid, leak into the abdominal cavity through the dilated fistula. This may cause adverse events (AEs) such as abdominal pain, peritonitis, and abscess formation during or after the procedure. Recently, EUS-BD without fistula dilation (WoD) has been reported to prevent AEs related to fistula dilation 3 4 5 6 7 . Although various types of self-expandable metallic stents (SEMS) have been used in EUS-BD WoD, the appropriate SEMS has not been confirmed. In addition, there are no reports regarding non-EUS-BD WoD. Recently, a fully covered, laser-cut SEMS (covered BileRush Advance; Piolax, Kanagawa, Japan) was developed in consideration of EUS-IV WoD. Here, we clinically evaluated cases in which EUS-IV WoD was attempted using this novel SEMS.
Patients and methods
Patients
We retrospectively evaluated cases in which EUS-IV WoD was attempted using the covered BileRush Advance at our institution between March and December 2021. This study, performed in accordance with the principles of the Declaration of Helsinki, was approved by the Institutional Review Board of the National Cancer Center Hospital, Japan (2018-149).
Techniques
Oblique-viewing echoendoscopes (GF-UCT260, GF-UCT240; Olympus, Tokyo, Japan; EG-580UT, FUJIFILM Medical, Tokyo, Japan) and forward-viewing echoendoscopes (TGF-UC260J; Olympus) were used. Generally, an oblique-viewing echoendoscope was used in EUS-BD and forward-viewing was used in non-EUS-BD. A 19-gauge EUS fine-needle aspiration needle (EZ Shot 3 Plus; Olympus) was used as the puncture needle, and a 0.025-inch guidewire (M Through; MEDICO'S HIRATA, Osaka, Japan) was used. EUS-IV WoD was attempted in all cases after contrast medium injection. When the stent delivery system could not be inserted WoD, it was inserted after fistula dilation using a mechanical dilator (ES Dilator; ZEON Medical, Tokyo, Japan) or a 4-mm dilation balloon (REN; KANEKA, Osaka, Japan) (i. e. non-adherence to EUS-IV WoD). In non-EUS-BD, including EUS-GBD, EUS-GE, and EUS-CD, a half pigtail plastic stent (PS) (Double pit; Gadelius, Tokyo, Japan) was placed in the SEMS as an anchor for preventing AEs such as stent migration.
Novel SEMS
The covered BileRush Advance is a novel SEMS with a 7F delivery system and a stiff and tapered tip specifically designed for a 0.025-inch guidewire. This stent is a fully covered, laser-cut SEMS that is flared at both ends. The diameter of the stent is either 8 mm (flared portion, 10 mm) or 10 mm (flared portion, 12 mm). The stent length is either 6 or 8 cm ( Fig. 1 ).
Fig. 1 a.
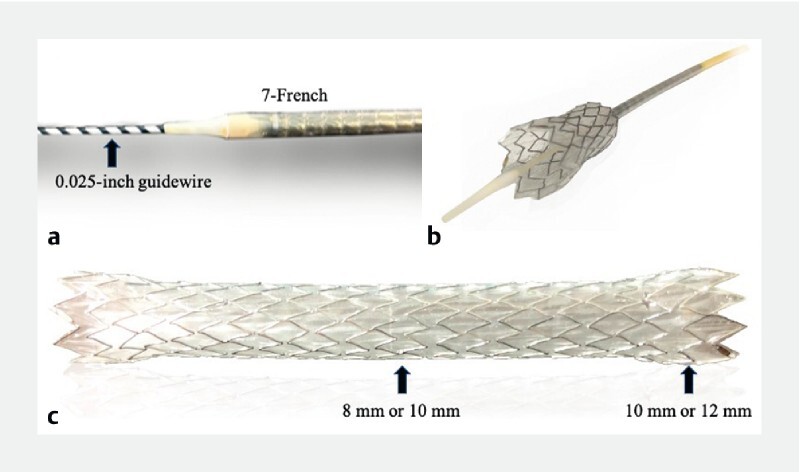
A novel stent, the covered BileRush Advance. b, c The stent has a 7F delivery and a stiff tip tapered to a 0.025-inch guidewire. The stent diameter is 8 mm (or 10 mm), with a 10-mm (or 12-mm) flared portion at both ends; the length is 6 cm or 8 cm.
Endpoints and definitions
The primary endpoint was the technical success rate of EUS-IV WoD. Secondary endpoints included the technical success rate of EUS-IV, clinical success rate, AE rate, stent patency duration, and reintervention rate. Technical success of EUS-IV WoD was defined as successful stent placement without fistula dilation. Technical success of EUS-IV was defined as successful stent placement regardless of fistula dilation. When the target was the bile duct, clinical success was defined as an improvement in the total bilirubin level to < 50 % of the value prior to the procedure or within normal limits within 14 days 8 . For all other targets, clinical success was defined as an improvement in the cause of the problems that led to the procedure. Stent patency, reintervention, and AEs were defined according to TOKYO Criteria 2014 8 . Early and late AEs were defined as AEs that occurred within 30 days and after 31 days of the procedure, respectively. The severity of AEs was classified according to the report of American Society for Gastrointestinal Endoscopy workshop 9 .
Statistical analysis
Data were analyzed using SPSS version 27.0 (IBM, Armonk, New York, United States). Continuous variables are expressed as the median (range) and categorical variables as numbers (percentage). The cumulative time to stent dysfunction was evaluated using the Kaplan-Meier method.
Results
Patient baseline characteristics
During the study period, 86 EUS-IV procedures were performed, as detailed in Fig. 2 . In total, 11 patients (age 65 years [37–76]; 45.5 % male) underwent EUS-IV WoD using the novel SEMS. The percentages of EUS-IV WoD procedures attempted with the covered BileRush Advance among all EUS-IV procedures are also detailed in Fig. 2 . The characteristics of the 11 patients are shown in Table 1 . There were no cases of moderate or severe infection, such as cholangitis.
Fig. 2 .
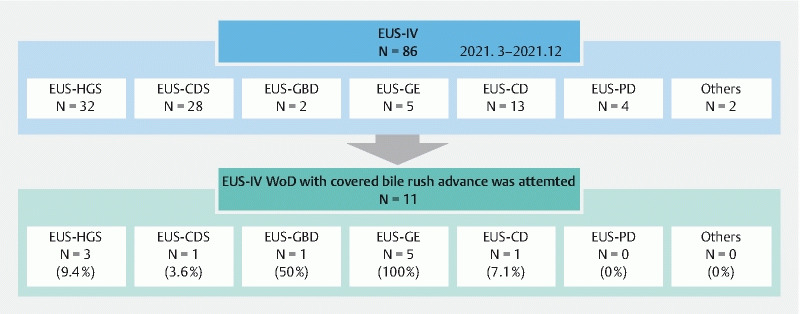
Flow diagram. Endoscopic ultrasound-guided intervention (EUS-IV) was performed on 86 patients and details of the procedure were noted. The percentages of EUS-IV without fistula dilation procedures attempted with the covered BileRush Advance among all cases of EUS-IV were 9.4 % (3/32) for EUS-guided hepaticogastrostomy, 3.6 % (1/28) for EUS-guided choledochoduodenostomy, 50 % (1/2) for EUS-gallbladder drainage, 100 % (5/5) for EUS-gastroenterostomy, and 7.7 % (1/13) for EUS-cyst drainage. EUS, endoscopic ultrasound; IV, intervention; HGS, hepaticogastrostomy; CDS, choledochoduodenostomy; GBD, gallbladder drainage; GE, gastroenterostomy; CD, cyst drainage; PD, pancreatic duct drainage; WoD, without fistula dilation
Table 1. Baseline clinical characteristics of participants.
| EUS-BD (N = 4) | Non EUS-BD (N = 7) | EUS-IV (N = 11) | |
| Median age, years (range) | 64 (47–65) | 70 (37–76) | 65 (37–76) |
| Male sex, n (%) | 3 (75 %) | 2 (28.6 %) | 5 (45.5 %) |
| Primary disease, n (%) | |||
|
4 (100 %) | 6 (85.7 %) | 10 (90.9 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
| Procedure of EUS-IV, n (%) | |||
|
3 (75 %) | 0 | 3 (27.3 %) |
|
1 (25 %) | 0 | 1 (9.1 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
|
0 | 5 (71.4 %) | 5 (45.5 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
EUS, endoscopic ultrasound; IV, intervention; HGS, hepaticogastrostomy; CDS, choledochoduodenostomy; GBD, gallbladder drainage; GE, gastroenterostomy; CD, cyst drainage.
Procedure details
Procedural details are provided in Table 2 . In the majority of patients (8 patients, 72.7 %), an 8 mm × 8-cm covered BileRush Advance was used. In non-EUS-BD cases, an anchoring PS was placed in all patients. Balloon dilation within the SEMS for placing the anchoring PS was required in three patients (42.9 %).
Table 2. Procedure details of EUS intervention.
| EUS-BD (N = 4) | Non EUS-BD (N = 7) | EUS-IV (N = 11) | |
| Scope, n (%) | |||
|
4 (100 %) | 1 (14.3 %) | 5 (45.5 %) |
|
0 | 6 (85.7 %) | 6 (54.5 %) |
| Needle, n (%) | |||
|
4 (100 %) | 7 (100 %) | 11 (100 %) |
| Guidewire, n (%) | |||
|
4 (100 %) | 7 (100 %) | 11 (100 %) |
| Covered BileRush Advance 1 , n (%) | |||
|
3 (75 %) | 5 (71.4 %) | 8 (72.7 %) |
|
1 (25 %) | 1 (14.3 %) | 2 (18.2 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
| Anchoring PS, n (%) | 0 | 7 (100 %) | 7 (63.6 %) |
|
0 | 7 (100 %) | 7 (63.6 %) |
|
0 | 3 (42.9 %) | 3 (27.3 %) |
|
0 | 4 (57.1 %) | 4 (36.4 %) |
| Necessity of dilation for placing anchoring PS 2 , n (%) | 0 | 3 (42.9 %) | 3 (27.3 %) |
EUS, endoscopic ultrasound; FNA, fine needle aspiration; PS, plastic stent.
The diameter of dilation balloon used for placing the anchoring PS was 4 mm in all cases.
The diameter of dilation balloon used for placing the anchoring PS was 4 mm in all cases.
Clinical outcomes
The clinical outcomes are provided in Table 3 . The technical and clinical success rates of EUS-IV were 100 % (11/11); the success rate of EUS-IV WoD was 72.8 % (8/11). Further, the procedural success rate of EUS-IV WoD was 100 % in EUS-BD and 57.1 % in non-EUS-BD. No AEs were observed during the procedure. However, early AEs were observed in 27.3 % (3/11) of patients, with mild abdominal pain in two patients and moderate bleeding in one patient. The cases of abdominal pain (one EUS-GE and one EUS-CD) were both cases of EUS-IV WoD failure and required fistula dilation at the time of SEMS placement. None of the patients experienced late AEs. The AE rates were 25 % (1/4), 28.6 % (2/7), 12.5 % (1/8), and 66.7 % (2/3) for EUS-BD, non-EUS-BD, EUS-IV WoD, and EUS-IV with dilation cases, respectively.
Table 3. Clinical outcomes.
| EUS-BD (N = 4) | Non EUS-BD (N = 7) | EUS-IV (N = 11) | |
| Technical success rate of EUS-IV, n (%) | 4 (100 %) | 7 (100 %) | 11 (100 %) |
| Clinical success rate, n (%) | 4 (100 %) | 7 (100 %) | 11 (100 %) |
| Technical success rate of EUS-IV WoD, n (%) | 4 (100 %) | 4 (57.1 %) | 8 (72.8 %) |
|
4 (100 %) | ||
|
3 (100 %) | ||
|
1 (100 %) | ||
|
4 (57.1 %) | ||
|
1 (100 %) | ||
|
3 (60 %) | ||
|
0 | ||
| Fistula dilation for placing SEMS, n (%) | 0 | 3 (42.9 %) | 3 (27.3 %) |
|
0 | 2 (28.6 %) | 2 (18.2 %) |
|
0 | 2 (28.6 %) | 2 (18.2 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
| Median procedural time, min (range) | 32.5 (21–90) | 45 (40–60) | 44 (21–90) |
| Adverse events during the procedure, n | 0 | 0 | 0 |
| Early adverse events, n (%) | 1 (25 %) | 2 (28.6 %) | 3 (27.3 %) |
|
0 | 2 (28.6 %) | 2 (18.2 %) |
|
1 (25 %) | 0 | 1 (9.1 %) |
| Late adverse events, n (%) | 0 | 0 | 0 |
| Reintervention | 0 | 2 (28.6 %) | 2 (18.2 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
|
0 | 1 (14.3 %) | 1 (9.1 %) |
EUS, endoscopic ultrasound; IV, intervention; WoD, without fistula dilation; BD, biliary drainage; HGS, hepaticogastrostomy; CDS, choledochoduodenostomy; GBD, gallbladder drainage; GE, gastroenterostomy; CD, cyst drainage; SEMS, self-expandable metallic stent.
Two cases of abdominal pain were observed immediately after the procedure. Both cases improved with antibiotics within 3 days.
One patient had anemia after the procedure and required 4 units of transfusion; however, endoscopic hemostasis was not required.
Details of the three cases of EUS-IV WoD failure are shown in Table 4 . All three cases were non-EUS-BD, including two EUS-GE cases and one EUS-CD case. The stent was successfully placed after fistula dilation with a mechanical dilator in the two EUS-GE cases and with a dilation balloon in the one EUS-CD case.
Table 4. Details in cases of failure of EUS intervention without fistula dilation.
| Age (yr) | Sex | Primary tumor | Procedure | Puncture site | Target | Scope | Scope position | Guidewire | Device used for fistula dilation | Procedural time (min) |
| 65 | Female | PDAC | EUS-GE | Stomach | Afferent-loop | Forward-viewing | Straight | M Through | ES dilator | 45 |
| 76 | Male | PDAC | EUS-GE | Stomach | Afferent-loop | Forward-viewing | Straight | M Through | ES dilator | 40 |
| 37 | Female | PDAC | EUS-CD | Stomach | Cyst | Oblique-viewing | Straight | M Through | REN 4 mm | 44 |
EUS, endoscopic ultrasound; PDAC, pancreatic ductal adenocarcinoma; GE, gastroenterostomy; CD, cyst drainage.
The median observation period of the 11 patients was 71 days (21–427), incidence of stent dysfunction was 9.1 % (1/11), and median time to stent dysfunction was not reached (95 % confidence interval [CI]: 110-NA) ( Fig. 3 ). The median observation period in EUS-BD was 118 days (40–427), with an incidence of recurrent biliary obstruction (RBO) of 0 % (0/4), and that in EUS-GE was 62 days (21–176), with an incidence of stent dysfunction of 20 % (1/5). The median time to stent dysfunction was 110 days (95 % CI: 110-NA).
Fig. 3 .
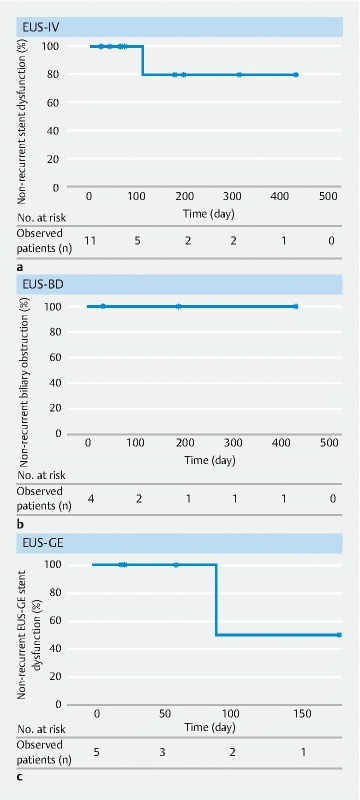
The Kaplan–Meier curve of time to reintervention. a The median observation period of all 11 cases of endoscopic ultrasound-guided intervention (EUS-IV) with the novel self-expandable metallic stents was 71 days (21–427), incidence of stent dysfunction was 9.1 % (1/11), and median time to stent dysfunction was not reached (95 % CI; 110-NA). b The median observation period for the four patients who underwent EUS-guided biliary drainage was 118 days (40–427), with an incidence of recurrent biliary obstruction of 0 % (0/4). c The median observation period for the five patients who underwent EUS-guided gastroenterostomy was 62 days (21–176), with an incidence of stent dysfunction of 20 % (1/5). The median time to stent dysfunction was 110 days (95 % CI; 110-NA). EUS, endoscopic ultrasound; IV, intervention; BD, biliary drainage; GE, gastroenterostomy.
Reintervention
Reintervention was performed in two patients. In one EUS-CD case, the stent was removed 2 months after stent placement because the cyst had disappeared. In one EUS-GE case with stent dysfunction due to stent rupture ( Fig. 4 ), stent removal was attempted but was unsuccessful; thus, two additional PSs were placed and the clinical symptoms subsequently improved.
Fig. 4.
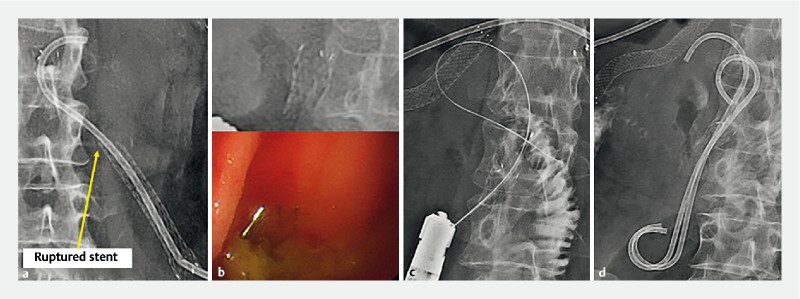
Reintervention was performed because the placed self-expandable metallic stent for endoscopic ultrasound-guided gastroenterostomy ruptured. a The ruptured stent (yellow arrow) is shown; the anchoring plastic stent maintained the fistula in an afferent-loop. b The residual stent could not be removed. c, d A guidewire was inserted into the fistula over the residual stent and two half pig-tail plastic stents were placed. Clinical improvement was achieved.
Discussion
In the present study, we analyzed cases of EUS-IV WoD using a novel fully covered laser-cut SEMS with a 7F delivery system, which was developed in consideration of EUS-IV WoD. Although there are some reports on the feasibility of EUS-BD WoD, to the best of our knowledge, there are no reports on cases of EUS-IV WoD including non-EUS-BD 3 4 5 6 7 ( Table 5 ).
Table 5. Review of literature regarding EUS intervention without fistula dilation.
| Author, year | Cases | Procedure | Outer diameter | Stent diameter | Type of stent | Stent | Success of EUS-IV WoD | Adverse events | Recurrence | |
| Koga et al, 2021 | 10 | EUS-CDS | EUS-BD | 5.9F | 8 mm | Fully covered, braided | HANARO benefit (Boston Scientific) | 90 % (9/10) | 10 % (1/10) | 30 % (3/10) |
| Ogura et al, 2021 | 14 | EUS-HGS | EUS-BD | 5.9F | 8 mm | Fully covered, braided | HANARO benefit (Boston Scientific) | 100 % (14/14) | 7.1 % (1/14) | NA |
| Maehara et al, 2020 | 6 | EUS-HGS | EUS-BD | 6F | 6 mm | Fully covered, braided | EGIS Braided6 (S&G Biotech) | 100 % (6/6) | 0 % | 33.3 % (2/6) |
| Park et al, 2015 | 16 | EUS-CDS/EUS-HGS | EUS-BD | 7F | 6 mm + flare | Partially covered, braided | DEUS (Standard Sci Tech) | 87.5 % (14/16) | 18.8 % (3/16) | 18.8 % (3/16) |
| Itonaga et al, 2019 | 20 | EUS-CDS | EUS-BD | 7.5F | 6 mm + flare | Partially covered, laser-cut | Covered BileRush (PIOLAX) | 30 % (6/20) | 5 % (1/20) | 21.1 % (4/19) |
| Present study | 11 | EUS-CDS/EUS-HGS | EUS-BD | 7F | 8 mm/10 mm + flare | Fully covered, laser-cut | Covered BileRush Advance (PIOLAX) | 100 % (4/4) | 25 % (1/4) | 0 % (0/4) |
| Non-EUS-BD | Non-EUS-BD | 57.1 % (4/7) | 28.6 % (2/7) | 14.3 % (1/7) | ||||||
EUS, endoscopic ultrasound; IV, intervention; WoD, without fistula dilation; BD, biliary drainage; HGS, hepaticogastrostomy; CDS, choledochoduodenostomy.
EUS-IV WoD is expected to prevent AEs due to drainage content leakage. In a previous study, no peritonitis was observed in the EUS-BD WoD group, whereas 12.5 % of the EUS-BD with fistula dilation group had peritonitis and intraperitoneal emphysema 3 . Another study reported no cases of peritonitis in the EUS-BD WoD group, while peritonitis was observed in 3.3 % of cases in the EUS-BD with fistula dilation group 6 . In the present study, none of the patients who underwent successful EUS-IV WoD had abdominal pain; in contrast, two of three patients who required fistula dilation had abdominal pain, suggesting that EUS-IV WoD may prevent AEs due to drainage content leakage. Therefore, EUS-IV WoD may prevent AEs associated with fistula dilation.
The stent delivery diameters for EUS-IV WoD in previous reports ranged from 5.9F to 7.5F. The success rate of EUS-BD WoD with ≤ 6F delivery systems is high 5 6 7 , whereas that of EUS-BD WoD with a 7.5F delivery system is slightly lower, at 30 % 4 . Another study reported a success rate of 88 % for EUS-BD WoD using a stent with a tapered and stiff metal tip with a 7F delivery system, similar to that in the present study 3 . Therefore, a thin delivery system (≤ 7F) and a tapered and stiff tip are critical stent-delivery factors for successful EUS-BD WoD ( Table 5 ).
In the present study, the success rate of EUS-BD WoD with a 7F delivery system was 100 %. In contrast, the success rate for non-EUS-BD WoD was slightly lower, at 57.1 %. Although there is no comparable previous report on non-EUS-BD WoD, the present results suggest that the success rate of EUS-IV WoD may be lower in non-EUS-BD than in EUS-BD. In non-EUS-BD, including EUS-CD and EUS-GE, the puncture target was not fixed intraperitoneally. This may be because mobility of the puncture target in the peritoneal cavity during insertion of the delivery prevents the transmission of force for delivery insertion ( Fig. 5 ).
Fig. 5.
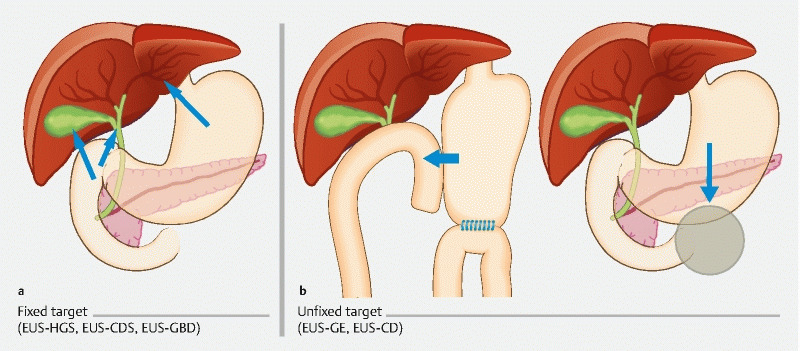
Whether the target of endoscopic ultrasound-guided intervention (EUS-IV) is intraperitoneally fixed (red arrows) or not (blue arrows) could be the determining factor for the failure of EUS-IV without fistula dilation. a The targets of EUS-HGS, EUS-CDS and EUS-GBD are fixed. b Those of EUS-GE and EUS-CD are unfixed. EUS, endoscopic ultrasound; HGS, hepaticogastrostomy; CDS, choledochoduodenostomy; GBD, gallbladder drainage; GE, gastroenterostomy; CD, cyst drainage.
Regarding stent types, although partially uncovered SEMS can prevent migration, they are more likely to be difficult to remove. In contrast, a fully covered braided SEMS can be removed at reintervention, although there is a risk of migration. In Maehara et al. 5 and Koga et al. 6 , stent migration occurred in 16.7 % and 20 % of cases of EUS-BD WoD using a fully covered braided SEMS, respectively. However, a fully covered laser-cut SEMS has been reported as useful for EUS-IV, as the fully covered design enables removal during reintervention and the laser-cut feature lessens the stent migration risk 10 . In the present study, no stent migration was observed; however, reintervention was performed in two cases. In the EUS-GE case with stent rupture, it was not possible to remove the remaining stent at the fistula site; however, the additional placement of two PSs improved the dilated afferent-loop. The cause of stent rupture may be related to the laser-cut stent material and fixation point, in addition to intestinal peristalsis. However, the usefulness of this stent in EUS-GE must be weighed against the advantages of no fistula dilation after the frequency of stent problems is further clarified with greater case accumulation. In the EUS-CD case, it was possible to remove the stent. There was no reintervention in EUS-BD cases. In addition, because this stent is a flare type, with 10 mm at both ends, there is a risk of hyperplasia when used in EUS-HGS. However, none of the three patients who underwent EUS-HGS in this study showed hyperplasia.
The median time to RBO in EUS-BD was not reached, while the median time to EUS-GE stent dysfunction was 110 days; these are relatively good results. However, there are no reports on stent patency in EUS-IV WoD for comparison. Further case accumulation is required to analyze the outcomes of stent patency after EUS-IV using the covered BileRush Advance.
The limitations of this study include its small sample size, retrospective nature, and single-center design. Therefore, further data collection is considered necessary, especially for stent patency. However, the clinical results of non-EUS-BD WoD have not been previously reported, which may be considered a novel feature of this study. In addition, in EUS-IV performed at our institution, this stent was the first choice for non-EUS-BD but was rarely selected for EUS-BD because another study was conducted in parallel. Thus, there may be a selection bias. Studies with larger sample sizes and a multicenter prospective design are required.
Conclusions
In conclusion, the covered BileRush Advance, a novel SEMS, may be useful as a stent for EUS-IV WoD, especially in EUS-BD.
Acknowledgments
This work was supported in part by The National Cancer Center Research and Development Fund (2022-A-16).
Footnotes
Competing interests The authors declare that they have no conflict of interest.
References
- 1.Moss A C, Morris E, Leyden J et al. Do the benefits of metal stents justify the costs? A systematic review and meta-analysis of trials comparing endoscopic stents for malignant biliary obstruction. Eur J Gastroenterol Hepatol. 2007;19:1119–1124. doi: 10.1097/MEG.0b013e3282f16206. [DOI] [PubMed] [Google Scholar]
- 2.Dhindsa B S, Mashiana H S, Dhaliwal A et al. EUS-guided biliary drainage: a systematic review and meta-analysis. Endosc Ultrasound. 2020;9:101–109. doi: 10.4103/eus.eus_80_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park D H, Lee T H, Paik W H et al. Feasibility and safety of a novel dedicated device for one-step EUS-guided biliary drainage: a randomized trial. J Gastroenterol Hepatol. 2015;30:1461–1466. doi: 10.1111/jgh.13027. [DOI] [PubMed] [Google Scholar]
- 4.Itonaga M, Kitano M, Hatamaru K et al. Endoscopic ultrasound-guided choledochoduodenostomy using a thin stent delivery system in patients with unresectable malignant distal biliary obstruction: a prospective multicenter study. Dig Endosc. 2019;31:291–298. doi: 10.1111/den.13300. [DOI] [PubMed] [Google Scholar]
- 5.Maehara K, Hijioka S, Nagashio Y et al. Endoscopic ultrasound-guided hepaticogastrostomy or hepaticojejunostomy without dilation using a stent with a thinner delivery system. Endosc Int Open. 2020;8:E1034–E1038. doi: 10.1055/a-1169-3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koga T, Hijioka S, Nagashio Y et al. Endoscopic ultrasound‐guided choledochoduodenostomy without fistula dilation using a stent with a 5.9‐Fr delivery system: comparison to a conventional procedure with fistula dilation. DEN Open. 2021;2:e56. doi: 10.1002/deo2.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogura T, Ueno S, Okuda A et al. Technical feasibility and safety of one-step deployment of EUS-guided hepaticogastrostomy using an 8-mm diameter metal stent with a fine-gauge stent delivery system (with video) Endosc Ultrasound. 2021;10:355–360. doi: 10.4103/EUS-D-20-00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isayama H, Hamada T, Yasuda I et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27:259–264. doi: 10.1111/den.12379. [DOI] [PubMed] [Google Scholar]
- 9.Cotton P B, Eisen G M, Aabakken L et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 10.Harai S, Hijioka S, Nagashio Y et al. Usefulness of the laser-cut, fully covered, self-expandable metallic stent for endoscopic ultrasound-guided hepaticogastrostomy. J Hepatobiliary Pancreat Sci. 2022;29:1035–1043. doi: 10.1002/jhbp.1165. [DOI] [PubMed] [Google Scholar]


