According to the American Psychiatric Association, mental illnesses represent conditions where the emotions, thinking, or behavior of patients are altered. Given the close association between mental illness and stress, an imbalance of neurotransmitters is often a driver for the pathophysiologic changes observed [1]. For example, patients with mental illnesses have been reported to have a higher prevalence of cardiovascular disease, which may be partially due to lifestyle-based risk factors [2, 3]. It has been found that both mental illnesses and their associated risk factors, including delays in care and medications, contribute to other postoperative outcomes such as a higher readmission rate, more non-fatal cardiac events, repeat cardiac procedures, and overall higher mortality rates [4, 5]. When mentally ill patients are considered for surgery, their cardiac status is difficult to optimize because of the additional complications. Additionally, patients with cardiovascular disease often have concomitant conditions such as renal failure and diabetes [6]. Because of these comorbidities, it is difficult to attribute any post-surgical complications purely to a mental illness diagnosis without additional statistical analysis. However, publications reporting preoperative risk factors have passed over the influence of mental illness diagnoses on clinical outcomes and resource utilization.
Given the paucity of articles identified using traditional search techniques, a very broad MEDLINE (PubMed) database search combined with manual screening of all articles was undertaken. For the 81 relevant articles found with multivariable risk models predicting new-onset atrial fibrillation, a wide variety of patient risk factors were reported; however, only 2 even considered the potential influence of mental illness. Katznelson et al. [7] prospectively observed 107 coronary artery bypass graft (CABG) patients to identify if preoperative depression was associated with new postoperative arrhythmias. Arrhythmias were assessed based on postoperative Holter monitoring. Comparing depressed versus non-depressed CABG patients, the new postoperative arrhythmias rates were not different (37.9% vs 35.9%: P = 0.50). Upon multivariable analysis, older age – but not depression – was identified as the most important risk factor impacting new onset of arrhythmias [7].
In Australia, Tully et al. [8] studied 226 CABG patients. By the fifth day post-surgery, 56 (24.8%) of the CABG patients developed new-onset postoperative atrial fibrillation (POAF). Arrhythmias were detected via Holter monitor and daily electrocardiograms. Psychological assessments were based upon the three Depression Anxiety Stress Scales (DASS) where clinically relevant symptoms were identified for depression, anxiety, and stress. Although baseline psychological assessments did not predict POAF, patients’ postoperative DASS-identified anxiety had increased POAF odds (OR 1.09; 95% CI 1.00, 1.18; P < 0.05) [8].
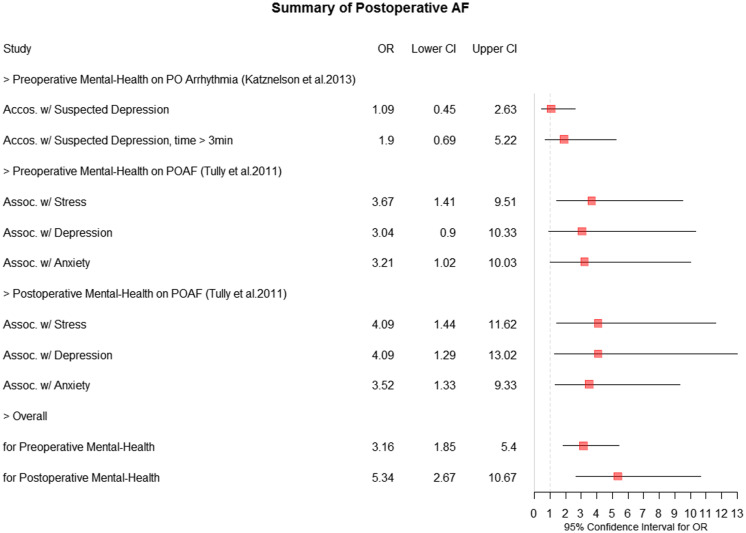
To summarize the correlation of preoperative and postoperative mental illness with postoperative atrial fibrillation, odds ratios were identified through a forest plot (Fig. 1). The forest plot supports that patients who developed atrial fibrillation were more likely to have mental illness compared to the non-atrial fibrillation group.
Fig. 1.
Forest plot summary of postoperative atrial fibrillation (AF). CI = confidence interval, PO = postoperative, POAF = postoperative atrial fibrillation.
In general, mentally ill patients have been under-represented in research but are overall shown to receive less medical care and suffer from more complications [9]. In fact, cardiovascular disease is the leading cause of death in patients with severe mental illnesses. One of the major reasons for this is related to the higher prevalence of smoking, obesity, lack of exercise, and alcohol consumption in these patients [10]. Patients with less medical care are also less likely to undertake testing such as cholesterol screening, which is related to higher rates of undiagnosed cardiovascular disease [9]. Gender and ethnicity may also play a role. Studies showed females are more likely to be diagnosed with a mental illness and cardiac conditions are associated with anxiety and depression among groups such as Caribbean Blacks [11, 12]. Unfortunately, even taking antidepressant and antipsychotic medications can have cardiovascular side effects and symptoms that need to be considered while prescribing [13]. These medications can alter signaling pathways and lead to arrhythmias, especially in patients with other risk factors [14].
Given the potential for a mental illness impact, it is disconcerting that large [e.g., the Society of Thoracic Surgeons (STS)], adult cardiac surgical databases do not gather enough data regarding cardiac surgery patients’ preoperative mental illness. Further, there is little known about how to manage cardiac surgical patients’ psychiatric medications peri- and postoperatively. Of note, medications such as anti-depressants are potent cytochrome inhibitors, risking postoperative drug-drug interactions [15, 16]. Thus, “at risk” mentally ill cardiac surgical patients provide a unique challenge to cardiac treatment selection, perioperative care management, as well as to cardiac research enrollment decisions. Finding innovative, patient-centered approaches to engaging more actively mentally ill patients with concomitant cardiac disease to participate in future research investigations now appears warranted to improve this vulnerable patient population’s overall cardiovascular health and quality of life.
Acknowledgements
Sincere gratitude is provided to Mrs. Jessica Koos and Mrs. Jamie Saragossi for their expert librarian assistance.
Supported by Stony Brook Medicine's Scholarly Concentration Program Research Track, Cancer Center, and General T. F. Cheng endowment (Dr. Tannous - PI).
Availability of data and materials
Not applicable.
Disclosure
The authors have no conflicts of interest to declare.
References
- 1. Parekh R. What Is Mental Illness? American Psychiatric Association, World Health Organization World Health Report. 2018. [Google Scholar]
- 2. Hawes MR, Roth KB, Wang X, Stefancic A, Weatherly C, Cabassa LJ. Ideal cardiovascular health in racially and ethnically diverse people with serious mental illness. Journal of Health Care for the Poor and Underserved 2020; 31(4): 1669–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGrath JJ, Wray NR, Pedersen CB, Mortensen PB, Greve AN, Petersen L. The association between family history of mental disorders and general cognitive ability. Translational Psychiatry 2014; 4(7): e412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pignay-Demaria V, Lespérance F, Demaria RG, Frasure-Smith N, Perrault LP. Depression and anxiety and outcomes of coronary artery bypass surgery. The Annals of Thoracic Surgery 2003; 75(1): 314–321. [DOI] [PubMed] [Google Scholar]
- 5. Jang HY, Kim J.H, Song Y.-K et al. Antidepressant use and the risk of major adverse cardiovascular events in patients without known cardiovascular disease: a retrospective cohort study. Frontiers in Pharmacology 2020; 11: 594474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Luscher TF. Heart failure and comorbidities: Renal failure, diabetes, atrial fibrillation, and inflammation. European Heart Journal 2015; 36(23): 1415–1417. [DOI] [PubMed] [Google Scholar]
- 7. Katznelson R, Scott Beattie W, Djaiani GN, Machina M, Lavi R, Rao V, Lavi S. Untreated preoperative depression is not associated with postoperative Arrhythmias IN CABG patients. Canadian Journal of Anesthesia 2013; 61(1): 12–18. [DOI] [PubMed] [Google Scholar]
- 8. Tully PJ, Bennetts JS, Baker RA, McGavigan AD, Turnbull DA, Winefield HR. Anxiety, depression, and stress as risk factors for atrial fibrillation after cardiac surgery. Heart & Lung 2011; 40(1): 4–11. [DOI] [PubMed] [Google Scholar]
- 9. Ward M. Increasing psychiatrists’ role in addressing the cardiovascular health of patients with severe mental illness. FOCUS 2021; 19(1): 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Davidson S, Judd F, Jolley D, Hocking B, Thompson S, Hyland B. Cardiovascular risk factors for people with mental illness. Australian & New Zealand Journal of Psychiatry 2001; 35(2): 196–202. [DOI] [PubMed] [Google Scholar]
- 11. Eaton NR, Keyes KM, Krueger RF, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. Journal of Abnormal Psychology 2012; 121(1): 282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Assari S. Race and ethnic differences in additive and multiplicative effects of depression and anxiety on cardiovascular risk. International Journal of Preventive Medicine 2016; 7(1): 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yekehtaz H, Farokhnia M, Akhondzadeh S. Cardiovascular considerations in antidepressant therapy: An evidence-based review. The Journal of Tehran University Heart Center 2013; 28(8): 169–176. [PMC free article] [PubMed] [Google Scholar]
- 14. Yamaguchi T, Sumida TS, Nomura S, et al. Cardiac dopamine D1 receptor triggers ventricular arrhythmia in chronic heart failure. Nature Communications 2020; 11(1): 4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Low Y, Setia S, Lima G. Drug–drug interactions involving antidepressants: Focus on desvenlafaxine. Neuropsychiatric Disease and Treatment 2018; 14: 567–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ebrahimi R, Shroyer AL, Dennis P, Currier J, Lendvai Wischik D. Music can reduce the need for pharmacologic conscious sedation during invasive coronary angiography. The Journal of Invasive Cardiology 2020; 32(11): 440–444. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.