Abstract
Background
Over time, surgical management for conditions involving the long head of the biceps tendon (LHBT) has evolved. Some techniques, such as keyhole tenodesis proposes bicortical drilling, however, carries an axillary nerve injury risk. The goal of our cadaveric study was to see if we could keep a safe zone between the point of exit of keyhole tenodesis of biceps and axillary nerve.
Methodology
The study was performed on ten shoulders from five fresh frozen cadavers. Between the lower border of the transverse humeral ligament (THL) and the superior margin of the pectoralis major insertion at the lowest limit of the bicipital groove, a beath pin was driven through with the help of the modified tip aimer tibial jig procured from the anterior cruciate ligament reconstruction (ACL) set, which was fixed at an arc of 45°. The distance between the axillary nerve and beath pin at the exit point was measured.
Results
The biceps tendon musculotendinous junction was followed all the way to the inferiorly and biceps tendon was found in the groove. The average distance from the axillary nerve to the exit point of the beath pin was 17.7 mm (range 14.4–20.9 mm, 95% CI).
Conclusion
The axillary nerve is not injured during bicortical drilling when keyhole tenodesis of biceps is performed at the distal limit of the groove of biceps. The area in the biciptal groove between inferior margin of THL and superior border of pectoralis major insertion is safe area for biceps tenodesis.
Keywords: Axillary nerve injury, Biceps tenodesis, Safe distance, Bicipital groove, Keyhole technique, Beath pin, ACL jig, Transverse humeral ligament, Bicortical drilling, Tenotomy
Introduction
Long head of biceps tendon (LHBT) has a very constrained path in bicipital groove, and it is surrounded by synovial sheath. Pathologies involving the LHBT have been identified as separate entities or as part of a rotator cuff injury. According to immunohistochemistry studies, the LHBT contains extensive sympathetic and sensory neural network. Hence any pathogenesis contributes to pain and dysfunction [1]. Treatment for biceps tendon pathologies has evolved along with its indication over the years. Operative intervention is often indicated when there is a partial tear [2, 3], subluxation of tendon, Superior Labral Anterior Posterior lesion involving the LHBT [4], hypertrophied intraarticular portion of the LHBT (hourglass biceps) [5, 6], and Habermeyer Type 4 Biceps lesion [6].
Tenotomy of LHBT is typically indicated in patients over the age of 55–60, who do not engage in heavy manual labor, and who are obese. The benefits of biceps tenotomy include a faster return to activities and less post-operative stiffness. This procedure also had its share of complications, including excessive biceps tendon retraction, which resulted in deformity known as the "Popeye Sign," as well as biceps muscle fatigue. Although supination weakness is uncommon in younger patients, it is undesirable to operate in the dominant extremity [7, 8]. The aforementioned complications paved the way for the development of tenodesis of LHBT, which was recommended in young athletes or those who want to avoid deformity. Tenodesis involves attaching the tendon to the cortex with a suture anchor [9] or through a bone tunnel with an interference screw [10].
However, studies have shown that tenodesis of biceps by bicortical drilling is associated with risk of axillary nerve injury [11–15]. The arthroscopic keyhole biceps tenodesis technique was found to be safe, cost-effective, and implant-free [16, 17]. Supra pectoralis arthroscopic biceps tenodesis has the advantage over open procedures in that it avoids a separate axillary incision (which is required for subpectoral biceps tenodesis), allowing inspection of the entire bicipital groove and the LHBT up to the musculotendinous junction, as well as addressing other associated shoulder abnormalities such as tear in rotator cuff, labrum, impingement.
The current study's goal was to measure the distance between the exit point of beath pin used for drilling keyhole tenodesis and axillary nerve. We hypothesized that with the help of a specific guide, a relatively safe distance could be maintained during keyhole tenodesis.
Materials and Methods
The cadaveric study was done in the department of anatomy at our institute. The specimen was acquired from the torso of three men and two female cadavers. These were fresh frozen cadavers which were stored at − 1 7°C and thawed 2 days prior to the experimental study. An equal distribution of side-specific dissection was maintained (Right-Sided vs. Left Sided). The age of the cadavers was not in record as these were unclaimed bodies.
The average height of an Indian male and female was 162–164 cm and 150–152 cm respectively [18, 19]. Studies have shown that distance between nerve and tunnel exit is closer in shorter individual. However, gender does not appear to affect the tendon length [20].
Surgical Dissection
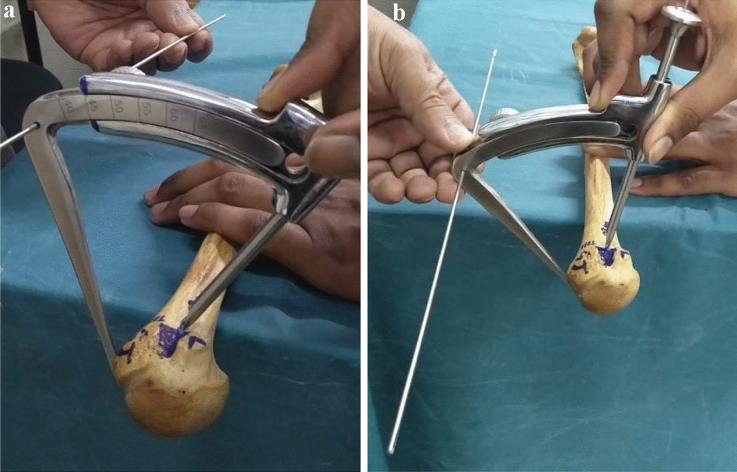
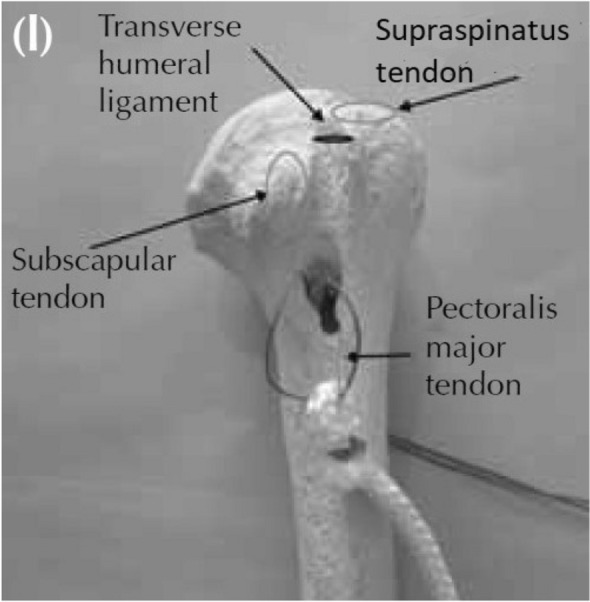
The cadaver was put in a standard lateral position with the involved limb in neutral rotation by the side of the body, simulating the position used in an operating room. The deltopectoral approach was used for the anatomical dissection. The axillary nerve was found traversing at the inferior border of the subscapularis. The anterior deltoid was reflected out, leading to the isolation of the LHBT passing through the bicipital groove [21]. The THL was identified and divided. The LHBT was traced to the superior glenoid tubercle. The LHBT tenotomy was done and the groove was cleared of THL and soft tissues, exposing the "half pipe zone" of the bicipital groove. In the groove for drilling the beath pin, a point between the lower border of THL and the upper margin of pectoralis major was identified (Fig. 1). The keyhole biceps tenodesis technique described by Rajkumar et al. in their papers [16, 17, 21] was then used (Fig. 2). The trocar is placed in the groove at the designated point and parallel to the long axis of the humerus using the modified tip aimer tibial Jig (from the ACL set). The jig and trocar were used to locate the beathpin's entry point. The jig modification aids in maintaining a parallel alignment to the long axis of the arm throughout the procedure (Fig. 3b).
Fig. 1.
A saw bone model indicating the surface landmark for entry of the beathpin
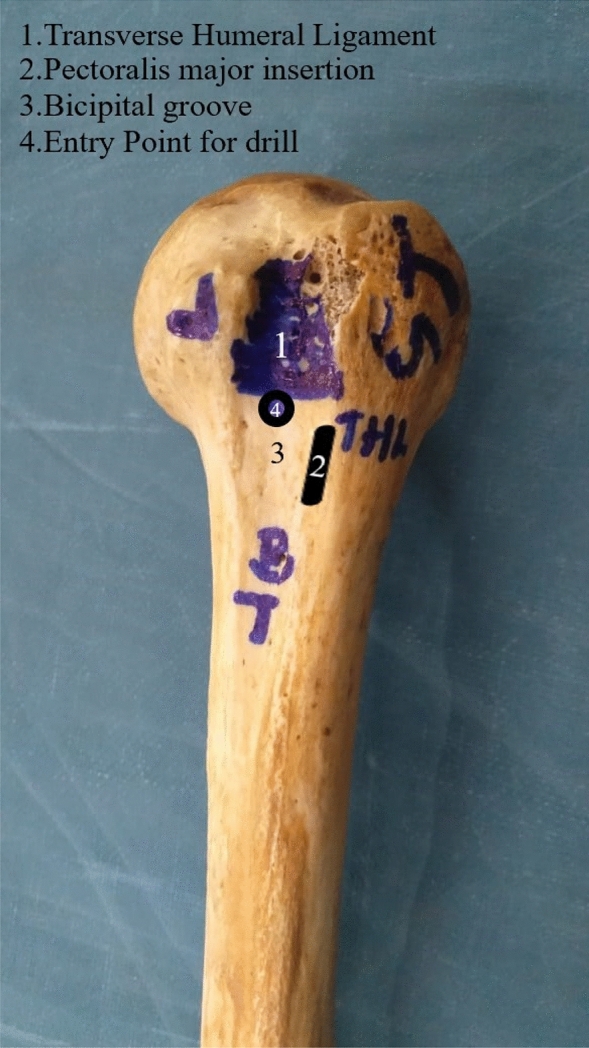
Fig. 2.
A saw bone model simulating the keyhole proximal biceps tendon tenodesis2
Fig. 3.
a A modified tibial jig fixed at an arc of 45°. b The pin parallel to the arm
After that, a 2.4 mm beath pin is drilled bicortical through the bicipital groove at the designated landmark [21]. The drilling was done at a 10° cephalad angle to the long axis of the arm. The jig’s positioning determines the drilling’s medio-lateral direction. The deltoid's posterior fibers were reflected laterally, and the axillary nerve was traced deep to the inferior border of the teres minor and marked with a marker pin. The distance between the axillary nerve and the exit point was measured with a digital caliper (Mitotoyo series 700, Mitotoyo, Kawasaki, Japan) calibrated to 0.1 mm (accuracy 0.2 mm) (Fig. 4). The nature of the study entailed a single investigator to measure the above parameters [16].
Fig. 4.
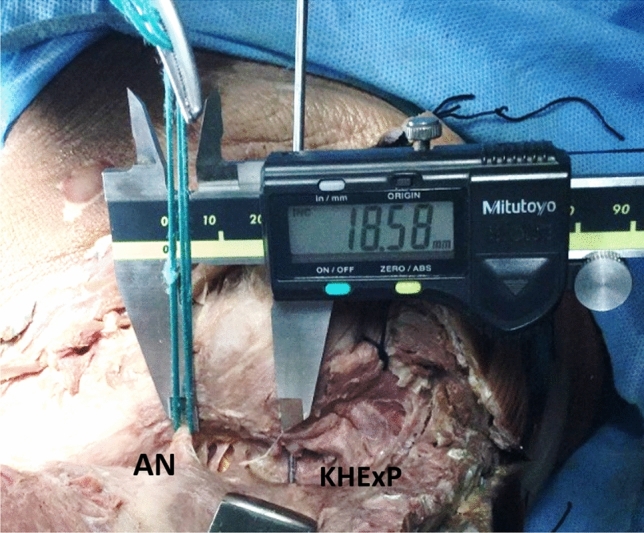
Distance between the axillary nerve (AN) and keyhole exit point (KHExP) was measured with a digital caliper
The keyhole tenodesis performed as described [16]. The tendon of biceps is looped and sutured to form a plug 2–2.5 cm from musculotendinous junction with vicryl No 2. A No. 2 polysorb should be introduced into the loop prior to suturing, and the suture's two limbs are used as traction sutures. Graft sizers, which are commonly used in knee ligament reconstructions, are used to measure the tendon and plug size. Using acron reamer of appopriate diameter the pilot hole is created to depth of 25–30 mm. This unicortical drilling aids in fracture prevention. The beath pin remains in place. To drill a second hole, a 5 mm offset guide is placed distal to pilot hole and beath pin is passed. 4.5 mm cannulated drill bit is introduced over the second beath pin and near cortex is drilled. A Kerrison Rongeur is used to remove the bony bridge between the two holes, and a keyhole is created (Fig. 2). The initial beath pin (left in situ) is then used to pull a doubled monofilament No. 2 loop through the pilot hole, allowing the two limbs to exit posteriorly. The traction suture's two limbs are then threaded through the monofilament loop and shuttled to the posterior aspect of the proximal arm via the pilot hole. The limb is given new traction. Two limbs of traction sutures are pulled and simultaneously the tendon is negotiated through the keyhole with the help of suture manipulator. A sudden ‘snap' is felt as the tendon plug gets locked into the keyhole. After the tendon plug has been locked, the traction suture is removed.
Statistics
All measurements were calculated with a 95% confidence interval and provided as mean with standard deviation (Table 1).
Table 1.
Distance between the axillary nerve and the keyhole exit point with statistical analysis
| Cadaver | Side | Gender | Distance between axillary nerve and the keyhole exit point |
|---|---|---|---|
| 1 | Right | Male | 15.1 |
| 2 | Left | Male | 14.4 |
| 3 | Left | Male | 15.2 |
| 4 | Right | Female | 18.5 |
| 5 | Left | Female | 19.1 |
| 6 | Right | Male | 20.9 |
| 7 | Right | Male | 19.6 |
| 8 | Left | Male | 19.3 |
| 9 | Left | Female | 19.2 |
| 10 | Right | Female | 20.1 |
| N | Mean | SD | 95% CI | |
|---|---|---|---|---|
| Distance (mm) | 10 | 17.7 | 3.2 | 15.38–19.98 |
Results
Using descriptive statistics and conventional statistical procedures, the mean, standard deviation, and 95% confidence intervals of data measured in mm were determined (Table 1). The average distance from the drill hole to the axillary nerve was 17.7 mm (95% confidence interval, 15.3–19.98). In our study, no axillary nerve injuries occurred in any of the cadavers when drilling was done through this landmark. The biceps tendon’s musculotendinous junction was followed all the way to the lower margin of pectoralis major insertion. As a result, at this distance, we report a risk estimate of zero for axillary nerve injury.
Discussion
The drill was inserted at the lower limit of the groove for biceps in our keyhole technique of tenodesis of biceps. The average distance between the nerve and the exit point is 17.7 mm, indicating that there is no risk of nerve injury. This landmark for drilling has the advantage of drilling in an area where the bone quality is good regardless of the patient’s gender or age. Furthermore, most of the pain generators along the bicipital groove and behind the THL are debrided. During the keyhole biceps tenodesis, any anomaly in the bicep tendon can be inspected and treated, and the working length of the tendon is kept in reasonable tension.
Study done by Lancaster et al. showed a mean distance from the axillary nerve of 10.7 mm, 18.2 mm, and 36.2 mm when the drill entry was at the Superior limit of the pectoralis major insertion, the inferior limit of the groove, and the superior limit of the bicipital groove, respectively [13]. Ding et al. measured 25.1 mm between the nerve and the drill exit point in their series [12]. In their study, Saithna et al. measured the axillary nerve's position susceptibility (laterally and posteriorly) with respect to the drill exit point taken through the bicipital groove about 1 cm above the lower border of pectoralis major [14].
Knudsen et al. investigated the axillary nerve risk by placing a low anterolateral portal over the lower aspect of the groove, followed by an open dissection to investigate the potential damage sustained. Eleven of the 23 shoulders dissected had the cannula in contact with the nerve [22]. Sethi et al. discovered that the risk of axillary nerve injury was higher in supra pectoral biceps tenodesis than in subpectoral biceps tenodesis. However, it was noted that the entry point was superior pectoralis major margin, which differed from the one used in our study [15].
Arora et al. discovered axillary nerve contact during bicortical drilling in subpectoral biceps tenodesis in some cases [11]. Suprapectoral and subpectoral biceps tenodesis proponents argue that removing the tendon of biceps from the groove improves outcomes [23]. Lutton et al. showed the tenodesis of the tendon of biceps in the proximal part of the groove had persistent shoulder pain in about 40% of patients [24].
An interference screw is used to perform a suprapectoral BT 15 mm distal to the upper edge of the groove. The safe drilling position was discovered to be 00 vertical or 150 lateral inclinations, as opposed to 200 caudal drilling, which injures the axillary nerve or cartilage of the head of the humerus [25]. Bradbury et al. described ‘T’ shaped tenotomy of biceps at tendon and labrum junction, which allowed the biceps tendon to self-lock at the THL [26]. Kany et al. examined the outcome of keyhole biceps tenodesis at the same entry point as this study. In their follow-up, no axillary nerve injury was discovered [21].
In another study comparing interference screw and keyhole biceps tenodesis, there was high incidence of deformity & popeye sign in the interference screw group than in the keyhole group, as evidenced by radiological marker migration. The procedure has the advantage of being less expensive, implant-free, and with the ability to be revised if the keyhole fails [21]. In addition, unlike open subpectoralis biceps tenodesis, keyhole biceps tenodesis can be done arthroscopically [11, 21].
Limitations
The age of the cadavers at death could not be ascertained but its influence on the study was negligible as most biceps tenodesis procedures are done in younger individuals. Only a single position of drilling was assessed during bicortical drilling. However optimum assessment of the bicep tendon and use of a modified tip aimer ACL jig can give consistent outcome during biceps tenodesis which is different from other techniques.
Using a digital caliper manually could have variation in the readings obtained. Lancaster et al. in their paper, used Computer tomography (CT) scan to get accurate measurements which were probably one of the pitfalls in our study [9]. CT scan was not economically viable for our study.
Conclusions
The axillary nerve is not injured during bicortical drilling when keyhole biceps tenodesis is performed at the distal limit of the bicipital groove. It is possible to achieve a safe and predictable result using the jig and technique correctly, in conjunction with a good understanding of anatomy.
Acknowledgements
We thank St Johns Medical College, Bangalore for the support and help in conducting the study.
Funding
This research did not receive any specific grant from the funding agencies in the form of public, commercial or not-for profit sectors.
Data availability statement
All the individual data collected during the study will be made avaialable to all who wish to access the data following publication with no end date for any purpose after deidentification.
Declarations
Conflict of Interest
Dr. Rajkumar S. Amaravathi, Dr. Manu Jacob Abraham, Dr. Keith Behram Tamboowalla, Dr. Anoop Pilar, Dr. Jean Kany, Dr. Sunil Lakshmipura Krishnamurthy, Dr. Padmanaban Sekaran and Dr. Dan Isaac Luke declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rajkumar S. Amaravathi, Email: rajamarvathi@gmail.com
Sunil Lakshmipura Krishnamurthy, Email: sunilmurthylk@gmail.com.
References
- 1.Alpantaki K, McLaughlin D, Karagogeos D, Hadjipavlou A, Kontakis G. Sympathetic and sensory neural elements in the tendon of the long head of the biceps. Journal of Bone and Joint Surgery. American Volume. 2005;87(7):1580–1583. doi: 10.2106/JBJS.D.02840. [DOI] [PubMed] [Google Scholar]
- 2.Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. Journal of Shoulder and Elbow Surgery. 2001;10(3):247–249. doi: 10.1067/mse.2001.114259. [DOI] [PubMed] [Google Scholar]
- 3.Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the bicep tendon. Journal of Shoulder and Elbow Surgery. 1999;8(6):644–654. doi: 10.1016/s1058-2746(99)90105-2. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: Biceps tenodesis as an alternative to reinsertion. American Journal of Sports Medicine. 2009;37(5):929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Ahrens PM, Hatzidakis AM. Entrapment of the long head of the biceps tendon: The hourglass biceps—A cause of pain and locking of the shoulder. Journal of Shoulder and Elbow Surgery. 2004;13(3):249–257. doi: 10.1016/j.jse.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Hedtmann A, Fett H, Heers G. Läsionenimbereich des rotatoreintervalls und der langenbizepssehne. In: Gohlke F, Hedtmann A, editors. Schulter: Das Standardwerkfür klinik und praxis. Georg thieme Verlag; 2002. pp. 310–316. [Google Scholar]
- 7.Lo I, Burkhart S. Arthroscopic biceps tenodesis: Indications and technique. Operative Techniques in Sports Medicine. 2002;100(2):105–112. doi: 10.1053/otsm.2002.30651. [DOI] [Google Scholar]
- 8.Werner BC, Burrus MT, Miller MD, Brockmeier SF. Tenodesis of the long head of the biceps: A review of indications, techniques, and outcomes. JBJS. 2014;2(12):1–10. doi: 10.2106/JBJS.RVW.N.00020. [DOI] [PubMed] [Google Scholar]
- 9.Nord KD, Smith GB, Mauck BM. Arthroscopic biceps tenodesis using suture anchors through the subclavian portal. Arthroscopy. 2005;21(2):248–252. doi: 10.1016/j.arthro.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18(9):1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 11.Arora A, Singh A, Koonce R. Biomechanical evaluation of a unicortical button versus interference screw for subpectoral biceps tenodesis. Arthroscopy: The Journal of Arthroscopic and Related Surgery. 2013;29(4):638–644. doi: 10.1016/j.arthro.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Ding D, Meislin RJ. Nerve proximity during bicortical drilling for subpectoral biceps tenodesis: A cadaveric study. Arthroscopy. 2014;30(8):942. doi: 10.1016/j.arthro.2014.03.026. [DOI] [PubMed] [Google Scholar]
- 13.Lancaster S, Smith G, Ogunleye O, Packham I. Proximity of the axillary nerve during bicortical drilling for biceps tenodesis. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(6):1925–1930. doi: 10.1007/s00167-014-3214-z. [DOI] [PubMed] [Google Scholar]
- 14.Saithna A, Longo A, Jordan RW, Leiter J, MacDonald P, Old J. A cadaveric assessment of the risk of nerve injury during open subpectoral biceps tenodesis using a bicortical guidewire. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(9):2858–2863. doi: 10.1016/j.jse.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Sethi PM, Vadasdi K, Greene RT, Vitale MA, Duong M, Miller SR. Safety of open suprapectoral and subpectoral biceps tenodesis: An anatomic assessment of risk for neurologic injury. Journal of Shoulder and Elbow Surgery. 2015;24(1):138–142. doi: 10.1016/j.jse.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 16.Amaravathi RS, Pankappilly B, Kany J. Arthroscopic keyhole proximal biceps tenodesis: A technical note. Journal of Orthopaedic Surgery. 2011;19(3):379–383. doi: 10.1177/230949901101900326. [DOI] [PubMed] [Google Scholar]
- 17.Kany J, Guinand R, Amaravathi RS, Alassaf I. The keyhole technique for arthroscopic tenodesis of the long head of the biceps tendon In vivo prospective study with a radio-opaque marker. Orthopaedics & Traumatology: Surgery & Research. 2015;101(1):31–34. doi: 10.1016/j.otsr.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 18.Som S, Ulijaszek S, Pal M, Bharati S, Bharati P. Variation in height and BMI of adult Indians. Journal of Biosocial Science. 2014;46(1):47–65. doi: 10.1017/S002193201300014X. [DOI] [PubMed] [Google Scholar]
- 19.Hood K, Ashcraft J, Watts K, Hong S, Choi W, Heymsfield SB, Gautam RK, Thomas D. Allometric scaling of weight to height and resulting body mass index thresholds in two Asian populations. Nutrition & Diabetes. 2019;9(1):2. doi: 10.1038/s41387-018-0068-3.PMID:30683839;PMCID:PMC6347591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: Implications for restoring physiological length-tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28(10):1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 21.Kany J, Guinand R, Croutzet P, Amaravathi R, Sekaran P. Biceps tenodesis (long head): Arthroscopic keyhole technique versus arthroscopic interference screw: A prospective comparative clinical and radiographic marker study. European Journal of Orthopaedic Surgery and Traumatology. 2016;26(1):77–84. doi: 10.1007/s00590-015-1714-2. [DOI] [PubMed] [Google Scholar]
- 22.Knudsen ML, Hibbard JC, Nuckley DJ, Braman JP. The low-anterolateral portal for arthroscopic biceps tenodesis: Description of technique and cadaveric study. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(2):462–466. doi: 10.1007/s00167-013-2444-9. [DOI] [PubMed] [Google Scholar]
- 23.Sanders B, Lavery KP, Pennington S, Warner JJ. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. Journal of Shoulder and Elbow Surgery. 2012;21(1):66–71. doi: 10.1016/j.jse.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 24.Lutton DM, Gruson KI, Harrison AK, Gladstone JN, Flatow EL. Where to tenodese the biceps: Proximal or distal? Clinical Orthopaedics and Related Research. 2011;469(4):1050–1055. doi: 10.1007/s11999-010-1691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pinedo M, Calvo C, Ekdahl M, Gutierrez V. Suprapectoral biceps tenodesis with bicortical drilling procedures: Anatomic analysis of chondral and axillary nerve risk with transhumeral pin guide. Journal of Shoulder and Elbow Surgery. 2020;29(7):1435–1439. doi: 10.1016/j.jse.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Bradbury T, Dunn WR, Kuhn JE. Preventing the popeye deformity after release of the long head of the biceps tendon: An alternative technique and biomechanical evaluation. Arthroscopy. 2008;24(10):1099–1102. doi: 10.1016/j.arthro.2008.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the individual data collected during the study will be made avaialable to all who wish to access the data following publication with no end date for any purpose after deidentification.