Abstract
Psychiatric conditions are common in autism; however, a multitude of barriers exist in accessing community-based mental health care for autistic youth. Perhaps the first and most formidable barrier is identifying a provider that offers mental health treatment to autistic youth within the many service systems involved in supporting the autism community. These systems typically function independently of one another, contributing to the complexity of accessing services. To identify gaps caused by New York’s multi-system care model for autistic youth, and as part of a larger quality improvement initiative to advance suicide risk management in several New York City emergency departments, we conducted a telephone survey to identify outpatient mental health service availability for autistic youth with depressive symptoms or suicidal thoughts or behaviors in New York City across the state’s mental health and developmental disability systems. Results demonstrated that while a greater proportion of clinics in the mental health system compared to agencies in the developmental disability system offered outpatient mental health services to autistic youth (47.1% v. 25.0%), there is remarkably limited service availability overall. Efforts to reduce these care inequities through policy reform and improving workforce capacity are urgently needed.
Keywords: Autism Spectrum Disorder, Mental Health, Community Services, Service Systems
Lay Abstract
Autistic children and adolescents experience high rates of co-occurring mental health conditions, including depression and suicidality, which are frequently identified by stakeholders as treatment priorities. Unfortunately, accessing community-based mental health care is often difficult for autistic youth and their families. The first obstacle families confront is finding a provider that offers mental health treatment to autistic youth within the many service systems involved in supporting the autism community. The mental health and developmental disability systems are two of the most commonly accessed, and previous work has shown there is often confusion over which of these systems is responsible for providing mental health care to autistic individuals. In this study, we conducted a telephone survey to determine the availability of outpatient mental health services for autistic youth with depressive symptoms or suicidal thoughts or behaviors in New York City across the state’s mental health and developmental disability systems. Results showed that while a greater percentage of clinics in the mental health system compared to in the developmental disability system offered outpatient mental health services to autistic youth (47.1% v. 25.0%), many more did not offer care to autistic youth and there were very few options overall. Therefore, it is important that changes to policy are made to increase the availability of services and that mental health care providers’ knowledge and confidence in working with autistic youth are improved.
Autistic individuals experience high rates of co-occurring mental health (MH) conditions (Lake et al., 2014; Simonoff et al., 2008), including depression and suicidal thoughts or behaviors (Kõlves et al., 2021; Menezes et al., 2018), which have been associated with poorer outcomes in a range of areas including education, employment, independence, and quality of life (Adams & Young, 2020). Although traditional MH services are often insufficient to meet the unique needs of autistic youth, service utilization for MH concerns is high in this population. Autistic youth are nine times more likely to present to the emergency department with a psychiatric concern (Kalb et al., 2012), and they represent 10–14% of psychiatrically referred youth, making up, on average, over 20% of outpatient MH therapists’ caseloads (Brookman-Frazee et al., 2020). There has been a growing evidence base supporting interventions for MH challenges in autistic individuals (Dickson et al., 2021; Lake et al., 2014; Maddox & Gaus, 2019). These interventions are either new treatments designed specifically for use with autistic individuals or adaptations of existing evidence-based interventions for MH conditions in other groups. Adaptation is the more common approach and typically involves modifying or adding specific components to the intervention (e.g., using visual supports, increasing caregiver involvement, altering language) to improve fit for the autism population (Dickson et al., 2021; Maddox et al., 2021).
Unfortunately, despite the increase in evidence-based treatments for MH problems in autistic youth, the recognition of MH problems as treatment priorities by autistic individuals and their families (Benevides et al., 2020; McConachie et al., 2018), and the fact that the advisory committee responsible for overseeing federal activities related to autism (the Interagency Autism Coordinating Committee) has identified improving access to and implementation of evidence-based treatments in community settings as a priority (Cervantes et al., 2021), accessibility to quality MH services remains limited (Dickson et al., 2021; Wood et al., 2015) and barriers to care are numerous (Cantor et al., 2020). There is a shortage of MH clinicians trained to work with autistic individuals (Wood et al., 2015), particularly in community MH settings. Those clinicians that are specialized in autism are often employed in university settings, work in urban areas, and/or do not accept insurance, restricting accessibility (Maddox et al., 2021). Community MH clinicians often lack education in autism, which may lead to misperceptions of the presentation and support needs of autistic individuals (Camm-Crosbie et al., 2019; Maddox et al., 2020). Clinicians endorse low levels of confidence and competence in treating autistic individuals and are often unprepared to assess MH difficulties and adapt their treatment to better support autistic individuals in therapy (Adams & Young, 2020; Brookman-Frazee, Baker-Ericzén, et al., 2012; Brookman-Frazee, Drahota, et al., 2012; Brookman-Frazee et al., 2020; Camm-Crosbie et al., 2019; Lake et al., 2014; Maddox et al., 2020). Further, especially without adaptation, social communication challenges inherent to autism may lead to misunderstandings (Adams & Young, 2020; Camm-Crosbie et al., 2019) and reduce treatment effectiveness and acceptability. There are common organizational barriers as well, such as lack of funding, long waitlists, and high staff turnover rates (Brookman-Frazee, Baker-Ericzén, et al., 2012; Camm-Crosbie et al., 2019).
However, the first, and perhaps the most formidable, barrier a family may confront in accessing quality MH care is identifying a community provider that accepts autistic youth as patients. Cantor and colleagues (2020) were the first to examine the availability and distribution of MH facilities that serve autistic youth across the US. Of the over 8,000 facilities contacted, approximately 43% reported providing care for autistic youth (Cantor et al., 2020). When examining outpatient MH facilities exclusively, about 50% offered care to autistic youth, and several county- (e.g., socioeconomic status, rurality) and facility-level (e.g., public v. private, acceptance of Medicaid as payment) characteristics were associated with offering this care (Cantor et al., 2021). While a number of factors likely contribute (e.g., workforce distribution), the complexity of multi-system care and the lack of coordination between MH and developmental disability (DD) systems are two of the most likely explanations for these findings.
Autistic individuals are often served by multiple service systems, each with different functions (e.g., DD, medical, MH, special education), and coordinating services among these systems is difficult (Anderson & Butt, 2018; Brookman-Frazee et al., 2020). While there is variation across states, state DD and MH systems are typically not integrated. This can lead to autistic individuals being “shuttled” between systems. For instance, clinics in the MH system may not accept autistic individuals as patients, because they do not specialize in DDs, and therefore, the individual is referred to the DD system. However, clinics in the DD system may not provide MH services because they focus primarily on addressing disability and promoting independence, and the individual may then be referred back to the MH system (Adams & Young, 2020; Anderson & Butt, 2018; Maddox et al., 2020, 2021; Maddox & Gaus, 2019). Further, those who most often present for outpatient MH services, i.e., autistic youth without cognitive impairments experiencing co-occurring MH challenges, may not be eligible for state DD services, as substantial deficits in intellectual and/or adaptive functioning are often necessary to qualify for DD services, leaving these youth without access to MH services in either system (Brookman-Frazee, Baker-Ericzén, et al., 2012; Brookman-Frazee, Drahota, et al., 2012; Brookman-Frazee et al., 2020; Lake et al., 2014).
Given the challenge of accessing MH services for autistic youth, this study examined the availability of public outpatient MH treatment programs in the five boroughs of New York City for autistic youth with co-occurring MH concerns, namely depressive symptoms and suicidal thoughts or behaviors, within the state DD and MH systems. This study extends the work of Cantor and colleagues (2020, 2021), which highlighted the lack of MH services available for autistic youth across the US, by evaluating MH service availability in New York City through the New York State (NYS) Office of Mental Health (OMH) system as compared to MH services available in New York City through the NYS Office for Persons With Developmental Disabilities (OPWDD) system. This study aimed to identify gaps caused by New York’s multi-system care model for autistic youth. It was conducted within the context of a quality improvement initiative to develop a resource list, inclusive of outpatient MH clinics that accept autistic youth as patients, to provide to emergency department clinicians as part of a larger NIMH-funded effort to enhance universal youth suicide risk screening and management in several pediatric emergency department settings. Because the larger initiative focuses on improving care exclusively in youth serving settings, we evaluated only MH service availability for children and adolescents. It is important to focus on youth, as access to MH treatment in childhood is imperative for improving outcomes in adulthood and there are vast differences in the US adult and child service systems.
Method
The DD System
The NYS OPWDD provides and coordinates services for children and adults with DDs, including autism, with the goal of promoting greater independence to live and participate in the community (NYS OPWDD, n.d.-a). To receive OPWDD services, an individual must have a DD diagnosis and must have had the disability before age 22; the disability must be expected to be permanent and must affect the individual’s ability to live independently. Many individuals who qualify for OPWDD services score: (1) in the intellectual disability range on intelligence testing (i.e., IQ<70) and in the low range on two or more adaptive domains, or (2) in the broad average range on intelligence testing (IQ>70) and in the low range on three or more adaptive domains (Advocates for Children of New York, Inc., 2020). Those who qualify may receive a range of publicly funded services in Article 16 Clinics, which are OPWDD-certified treatment facilities that serve primarily individuals with DDs and their caregivers. Services offered at OPWDD-certified clinics focus on habilitation with the goal of improving or limiting disabling conditions or illnesses through provision of interdisciplinary assessment and therapeutic services. These services frequently include psychology, social work, rehabilitation counseling, occupational and physical therapy, speech and language pathology, nutrition, and nursing; audiology, dentistry, podiatry, and medicine are also available at some OPWDD-certified clinics (NYS OPWDD, n.d.-b).
Identifying OPWDD-Certified Clinics.
A list of OPWDD-certified clinics was downloaded from the OPWDD website (NYS OPWDD, n.d.-b). This list was dated 03/19/2021, was inclusive of agencies across NYS, and consisted of the following data: agency and program ID, agency name, agency and program address, agency phone number, name and email address of the executive director, and location of satellite sites, if applicable. Of the 66 agencies on the full list, 20 agencies were located across the New York City boroughs. The list was exported into a database. Because the list included only contact information for the agency and given the wide range of services beyond MH treatment that may be available at OPWDD-certified clinics, callers used agency phone numbers to inquire about the availability of MH treatment services across agency programs and sites. Upon making calls, it became clear that listed agency phone numbers were sometimes inaccurate or were not always the most appropriate (e.g., the number was to a director’s line while the agency had a separate line for referrals and service inquiries). In these cases, we were either referred or transferred to a better contact or we identified the correct contact through a Google search.
The MH System
The NYS OMH aims to promote the MH of children and adults in NYS. The OMH both operates a number of psychiatric centers and provides certification and oversight for more than 4,500 programs that are operated by local governments and nonprofit agencies across NYS (NYS OMH, n.d.-a). OMH-certified programs are referred to as Article 31 clinics. Child and adolescent MH treatment services provided by OMH-certified clinics are focused on identifying emotional health needs and providing treatment and support to encourage recovery from MH conditions (NYS OMH, n.d.-b). Outpatient clinic services can include psychiatric assessment and individual, family, or group psychotherapy, among others (NYS OMH, 2021).
Identifying OMH-Certified Child and Adolescent Clinics.
The authors used the OMH’s “Find a Mental Health Program” tool available on their website and conducted an advanced search for OMH-certified clinics across New York City (Counties: Bronx, New York, Kings, Queens, Richmond) that provide outpatient MH clinic services (Program Category: Outpatient; Program Subcategory: Clinic treatment) for children and adolescents (Population Served). The search resulted in 172 programs across boroughs. Results were exported into a database which included both program and agency phone number among other variables (e.g., program name, agency name, sponsor name, address). Callers used program phone numbers when both agency and program phone numbers were available, because policies may have differed across programs within an agency and because caregivers seeking treatment services for their child may be more likely to call programs directly. Similar to the OPWDD list, there were several phone numbers that were not accurate in the OMH results (e.g., went to a different department within the agency). In those cases, the contact information was obtained through a Google search.
Procedures
This effort was approved by the NYU Langone Health institutional review board. Three authors (PC, GC, & DS) called each program and/or agency responsible for overseeing individual programs following a standardized protocol and script. For OPWDD-certified clinics, callers were instructed to say, “My team and I are building a resource list for families of autistic kids and teens who have depressive symptoms or suicidal thoughts or behaviors and are seeking outpatient MH treatment. Does your agency offer this type of treatment?” If the agency reported offering MH treatment to autistic youth, callers followed up by asking which of the agency’s sites offer MH treatment and if the agency accepts children and adolescents with an autism diagnosis who have not been deemed eligible for OPWDD services. For OMH-certified clinics, callers were instructed to say, “My team and I are building a resource list for families of autistic kids and teens who have depressive symptoms or suicidal thoughts or behaviors and are seeking outpatient MH treatment. Does your clinic accept children and adolescents with an autism diagnosis as patients for this type of treatment?” If the clinic responded that they offer care to autistic youth in some cases, the callers followed up by asking under what parameters would autistic youth be accepted as patients. If the clinic indicated that they did not offer services to autistic youth, the callers recorded the response of the program, such as whether they provided a reason for not accepting autistic patients.
If there was no answer at a program or agency, callers left detailed voicemail messages that included their name, phone number, and primary reason for calling. If the program/agency did not return their call, callers waited approximately 48 hours before a subsequent call attempt. Replicating Olin et al. (2016), three separate call attempts were made if the caller was unable to speak with anyone at the program. In cases where the person they reached referred the caller to someone else in the program or reported that they would get back to the caller about the inquiry, the caller made up to five separate call attempts. There were few cases where the person the callers reached recommended emailing another person to obtain needed information. In these few cases, an identical procedure was used. Up to three email attempts were made if the caller did not receive a response from the program on the first inquiry. If referred to someone else or told that they would follow up with the caller, up to five email attempts were made. Because this effort took place during the COVID-19 pandemic, and programs still had many staff working from home, flexibility in contact modalities was important. Initial contact attempts were completed from August 9 to September 15, 2021. To attempt to capture responses from as many clinics as possible and because staffing patterns may be different between Summer and Fall months, calls to clinics that failed to respond in the first round (n=17) were repeated from October 7 to October 26, 2021, using the same procedures.
The first author trained the two other callers to conduct calls and record information in the database. To ensure fidelity to the protocol, the first author observed calls made by other callers to approximately 10% of the agencies and/or programs they were assigned. Following data collection, we coded qualitative data and identified recurring themes in the responses provided by clinics (i.e., the parameters in which autistic youth were accepted as patients, the unprompted rationale sometimes provided for not offering care to autistic youth). This involved first familiarizing ourselves with the data collected, then generating and assigning codes, including identifying, defining, and applying broader categories to related codes. These data were coded by two authors (PC & GC). Agreement was 94%; disagreement was resolved through discussions that resulted in consensus. Data were then analyzed descriptively. A Chi-Square test was used to examine differences in the availability of outpatient MH services for autistic youth across MH and DD systems.
Community Involvement
This study was motivated by barriers identified by autistic youth and their caregivers and by emergency department clinicians in an ongoing qualitative study on suicide-related care for autistic youth. There was no community involvement in the current study.
Results
We successfully contacted all 20 of the OPWDD-certified agencies and 165 of the 172 OMH-certified clinics (95.9%), representing a total response rate of 96.4%. The seven OMH-certified clinics we could not reach were located in Brooklyn (n=2), the Bronx (n=2), and Manhattan (n=3). Further, ten of the OMH-certified clinics we reached reported that they served only patients 18 years or older and were therefore removed from the sample of OMH-certified child and adolescent MH clinics.
The DD System
Five OPWDD-certified agencies (25%) reported offering outpatient MH services to autistic children and adolescents with depressive symptoms or suicidal thoughts or behaviors across a total of 11 sites located in the Bronx (n=2), Brooklyn (n=3), Manhattan (n=3), Queens (n=2), and Staten Island (n=1). Three of these five agencies reported providing services exclusively to youth who receive OPWDD services. Only two agencies, which provide outpatient MH services at sites in Brooklyn (n=1), Manhattan (n=1), and Staten Island (n=1), reported offering care to autistic youth regardless of OPWDD eligibility status (Figure 1). The other 15 agencies reported that they did not have MH services or that they had MH services but did not accept autistic youth as patients (e.g., offered MH services to adults only, did not work with youth on the autism spectrum).
Figure 1.
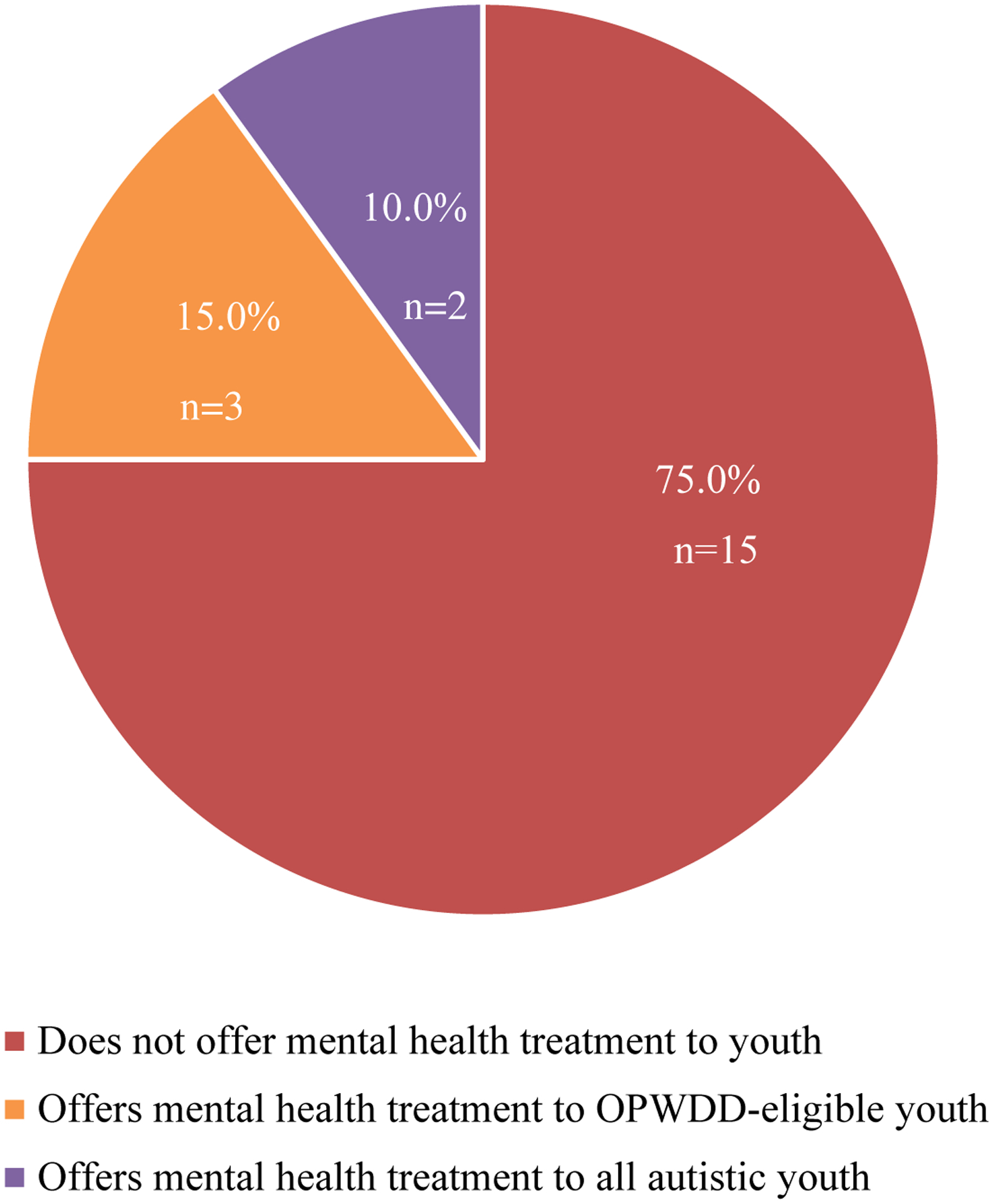
Mental Health Service Availability in the DD System
The MH System
A greater proportion of OMH-certified child and adolescent clinics compared to OPWDD-certified agencies offered outpatient MH treatment to autistic youth with depressive symptoms or suicidal thoughts or behaviors in at least some cases, although the difference was not statistically significant (47.1% v. 25.0%), X2(1)=3.5, p=0.06. More than half of the responding OMH-certified clinics (n=82; 52.9%) reported that they did not offer services to autistic children and adolescents. Thirty-one clinics (20.0%) reported that they offer treatment to autistic youth, and 42 (27.1%) reported that they offer services to autistic youth in some cases (Figure 2). There was some variability in service availability across boroughs. Of the 73 clinics within the MH system across New York City that reported offering services to some or all autistic youth, 27.4% (n=20) were located in Brooklyn, 27.4% (n=20) were located in Manhattan, 24.7% (n=18) were located in the Bronx, 16.4% (n=12) were located in Queens, and 4.1% (n=3) were located in Staten Island.
Figure 2.
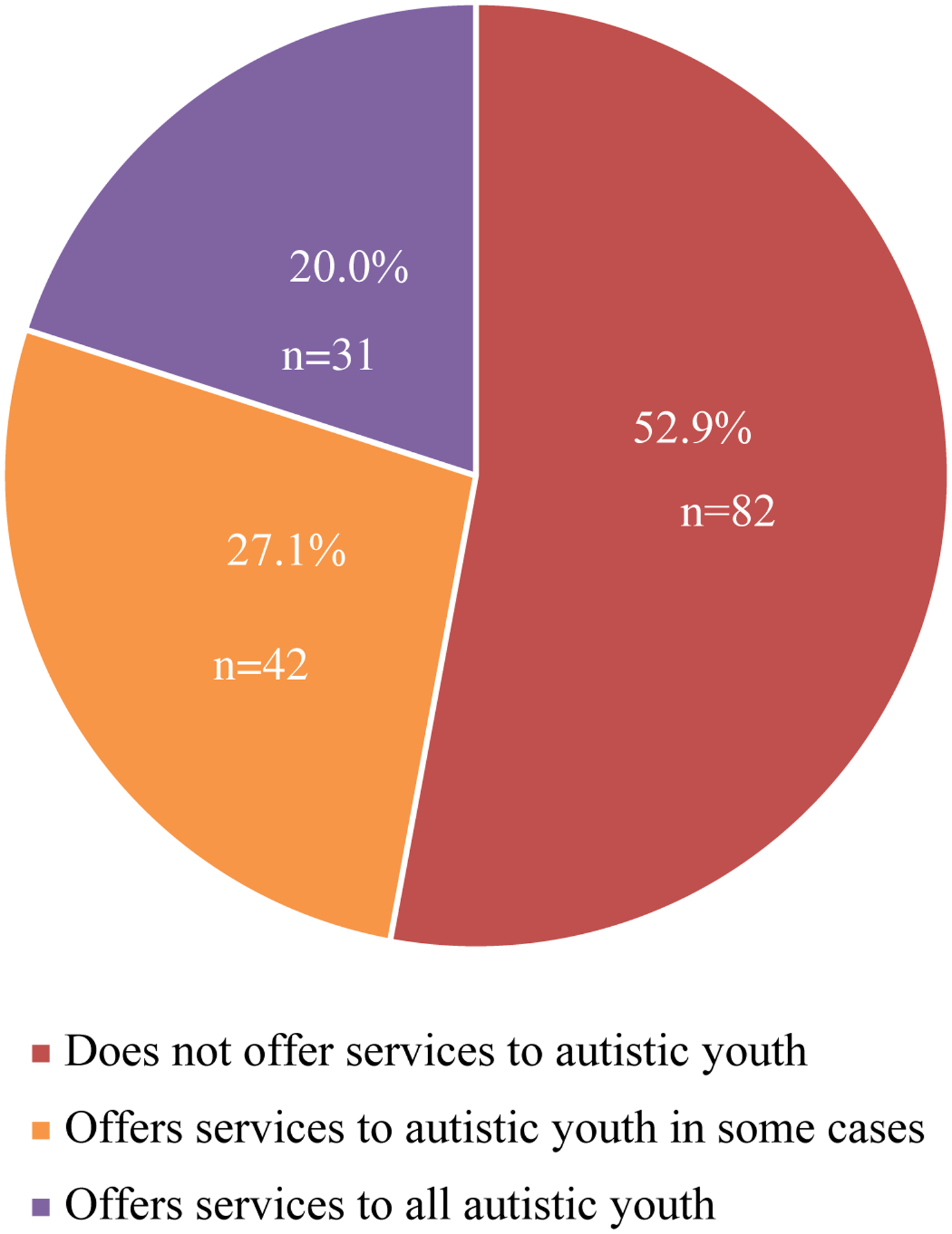
Mental Health Service Availability in the MH System
Thirty-eight clinics provided a rationale for not offering treatment to autistic youth. The majority (76.3%) reported that they do not have clinicians specialized in autism or programs targeted to the autism population. Nearly 24% of clinics reported that they were not licensed or credentialed to see autistic patients. Eleven clinics referred the caller to a clinic or agency specialized in DDs, oftentimes an OPWDD-certified agency that provides services exclusively to OPWDD-eligible youth.
When responders indicated that their clinic offers services to autistic youth in some cases, the most common response to the follow-up inquiry about the parameters under which autistic youth are accepted was vague (e.g., dependent on each individual case or left up to the discretion of individual clinicians; 38.1% of clinics that provided a response). Another 21.4% reported that acceptance of patients with an autism diagnosis was dependent on functioning level but did not define this further (e.g., youth must be “high functioning,” youth must have “mild forms” of autism). Nearly 15% of the clinics cited verbal ability as an indicator of youth eligibility, 4.8% named IQ as an indicator, and 4.8% of clinics reported offering services to autistic youth when their autism diagnosis was secondary to a MH concern. Finally, several clinic-specific factors limited their utility as referral sites for all autistic youth. Age of youth served was restricted in 19.0% of clinics (e.g., accepting only young children, accepting only adolescents). Nearly 12% of clinics provided services only to specialized populations (e.g., youth involved with the criminal justice system, students attending a particular school associated with a school-based clinic). One clinic reported that they provide only outpatient family therapy for autistic youth.
Discussion
Even in New York City, often considered a resource rich area (Center for Disease Control and Prevention, 2021), there are remarkably few clinics that offer MH care to autistic youth with depressive symptoms or suicidal thoughts or behaviors. In fact, results of this examination of community-based outpatient MH service availability for autistic youth replicated the national-level estimate found in Cantor et al. (2021)’s study. Less than 50% of clinics within the MH system accepted autistic youth with these MH concerns as patients, and only a quarter of the agencies within the DD system offered outpatient MH treatment to some or all autistic youth. Because a goal of this project was to build a referral list for emergency department clinicians, as part of a larger effort to enhance universal youth suicide risk screening and management in several emergency department settings, this lack of service availability has serious implications for their care. Clinicians that serve autistic youth in psychiatric crisis within emergency departments are often left with no or very limited options for referral at discharge (Cervantes et al., 2022). Because it is well documented that barriers to accessing outpatient services increase the probability of recurring MH crises in the future, this lack of MH service availability for autistic youth is a substantial issue.
Comparing outpatient MH service availability across systems, a greater proportion of clinics in the MH system compared to agencies in the DD system offered outpatient MH services to autistic youth with depressive symptoms or suicidal thoughts or behaviors. This finding makes conceptual sense, as the goals of the MH system are to address emotional and behavioral health concerns whereas the goals of the DD system are to address disability and promote independence and community participation. However, as described in previous literature (Maddox et al., 2021), among providers, there is often confusion over which system is responsible for providing MH care. In fact, callers in this study experienced some of the “shuttling” often described by autistic individuals and their caregivers (Maddox et al., 2020; Maddox & Gaus, 2019). Several clinics within the MH system referred the callers to agencies within the DD system for assistance building the referral list. Improved integration of the MH and DD systems is necessary to reduce this “shuttling,” clarify roles and responsibilities in the provision of autism services, and ideally, provide collaboration and support to improve care (Lake et al., 2014; Maddox & Gaus, 2019). Further, MH and DD systems are not the only systems involved in youth MH care; the role of the education system in addressing MH concerns within the context of autism is relevant and generally is covered under the Individuals with Disabilities Education Act. Efforts to improve coordination across all three systems are urgently needed.
Most clinics that provided a rationale for not accepting autistic youth as patients noted that it was because the clinic did not have clinicians with expertise in autism or specialized programs for the autism population. This is notable as evidence-based treatments for MH conditions within the context of autism are typically adaptations of evidence-based treatments developed for use with the general population (Dickson et al., 2021; Maddox et al., 2021; Schwartzman et al., 2021). Therefore, many non-specialized clinicians, including those employed within settings that deny services to autistic youth, may have the skills to provide MH care in the context of autism (Lake et al., 2014), particularly with additional training and implementation support. As such, courses on autism should be included in the education of future MH providers as well as in the training and continuing education of practicing clinicians to provide information on autism and instruction on recommendations for care and adaptations for existing practices (Maddox & Gaus, 2019). Supporting the need for additional education, previous research has shown that these clinicians are highly motivated to receive more targeted autism training (Brookman-Frazee, Drahota, et al., 2012). Following training, providing ongoing implementation support is important. This training and implementation support could be an outcome of improving integration between the MH and DD systems, whereby the DD system can offer their expertise to assist in preparing community MH providers to better serve the autism community (Lake et al., 2014). Academic-policy partnerships would also be useful for supporting clinics within the MH system to serve autistic children and adolescents. For instance, there is a longstanding partnership between researchers, policymakers, providers, and family support specialists in NYS focused on improving child MH services, which has been successful at disseminating evidence-based practices to many public MH clinicians and evaluating the implementation and dissemination of such practice for youth psychiatric concerns broadly (Hoagwood et al., 2014). Increasing training and support specific to autism would increase the competence and confidence of community MH clinicians, thereby improving the quality of care. In addition, several clinics reported that they do not offer care to autistic youth with depressive symptoms or suicidal thoughts or behaviors because they were not licensed or credentialed to treat autistic children and adolescents, perhaps representing different interpretations of the OMH and OPWDD certification processes and conditions. This could be addressed by having policymakers delineate the certification processes for the two systems to make it easier for clinics and, importantly, families to know under what circumstances to access MH care from which of the two systems. The current complexity of multiple systems certainly contributes to this inequity in MH care access.
When agencies in the DD system and clinics in the MH system reported offering MH treatment to autistic youth with depressive symptoms or suicidal thoughts or behaviors, they were more likely to accept autistic youth as patients only under certain conditions. Three of the five OPWDD agencies that had outpatient MH services for autistic youth reported that only autistic youth who receive OPWDD services were eligible to receive these services. As mentioned, it is possible that those most likely to seek outpatient services for MH concerns, i.e., autistic youth without cognitive impairments, may be least likely to qualify for services from the DD system, as significant deficits in IQ and/or adaptive domains are often necessary (Brookman-Frazee, Baker-Ericzén, et al., 2012; Brookman-Frazee, Drahota, et al., 2012; Brookman-Frazee et al., 2020; Lake et al., 2014). These youth without access to DD services experience an even more limited MH service landscape. Arguably, many individuals without co-occurring intellectual deficits would benefit from services and supports to improve community participation as well (e.g., employment, independence); therefore, echoing recommendations made by previous researchers (Lake et al., 2014), DD systems should re-evaluate their eligibility criteria for autistic individuals. Similarly, it was more common for clinics in the MH system to report that they offered care to autistic youth with depressive symptoms or suicidal thoughts or behaviors in some cases. However, the reported parameters under which autistic youth would be accepted as patients were often vague. This then creates the possibility for unstandardized determination of eligibility, where decisions are made case-by-case and parameters may vary between cases. This may also delay care for autistic youth, as clinics may request additional input, assessment, or documentation (e.g., requiring updated diagnostic reports) as they work to determine eligibility. Therefore, particularly in the context of increasing training and support for providers, there is also a critical need for community MH clinics to review their eligibility criteria for autistic youth (Lake et al., 2014).
There are limitations to this study. First, the quality of services provided to autistic patients at the clinics that reported offering outpatient MH treatment in some or all cases is unknown. In fact, several clinics within the MH system that accepted some or all autistic youth as patients noted that while they could be added to the referral list, their clinicians were not necessarily specialized in autism. We also focused exclusively on community-based programs. Cantor et al. (2021) found that private clinics were more likely to accept autistic youth as patients, and we are aware that there are a number of private clinics in New York City that offer MH services to autistic youth with co-occurring MH conditions, such as depression and suicidality. However, these clinics were excluded to evaluate the public service systems and because affordability presents as a major barrier to accessing private clinics. Beyond disparities that exist between families of autistic youth who can and cannot access private MH services, and because it has been well documented that racial/ethnic minority groups have less access to MH care, are less likely to obtain care, and often receive lower quality care (McGuire & Miranda, 2008), it should also be noted that we expect there to be additional challenges in accessing MH services for autistic youth and their families from BIPOC communities in New York City that require attention. Further, we examined only service availability for children and adolescents, and results may differ for autistic adult populations. Additionally, callers inquired about the clinic or agency’s general policy related to accepting autistic youth as patients and not the current availability of treatment for autistic youth. These calls were made during the COVID-19 pandemic, and many responders indicated that they were not currently accepting new patients or had extensive waitlists. It is important to note however that within this context, when service systems may be overwhelmed and services are limited for all youth, the availability of MH treatment is even more restricted for the autism community, who at baseline are excluded from more than half of the clinics within the MH system, despite having high rates of co-occurring MH symptoms (Lake et al., 2014; Simonoff et al., 2008). Further, because suicide risk is the focus of the larger initiative, our inquiry was specific to autistic youth with depressive symptoms or suicidal thoughts or behaviors. While no clinic reported that type of MH concern was exclusionary, responses may have differed if we inquired about autistic youth with MH concerns generally or with a different MH diagnosis (e.g., anxiety), particularly given that previous findings show that MH clinicians have low self-efficacy working with autistic individuals at risk for suicide (Jager-Hyman et al., 2020). Finally, we relied on the knowledge of the person who answered our phone call or email, and it is possible that not all responders were fully aware of clinic or agency policies on autism. However, these responders would likely be a caregivers’ first contact as well, as we used contact information posted on the MH and DD systems’ websites or on individual clinic or agency websites when necessary, so the information we received would likely represent what would be relayed to caregivers or youth trying to access services as well.
Despite these limitations, this study adds to emerging literature (Cantor et al., 2020, 2021) documenting the markedly limited MH service availability for autistic youth. This was true across both MH and DD systems. As most children and adolescents are served within community-based settings, state MH and DD systems should clarify roles and responsibilities across these systems. State policy can be reviewed to ensure that MH services are available to these youth who are currently falling through the cracks. Targeted training of MH and DD providers in evidence-based services is critical to address this shortage of services. Implementation supports will be needed to ensure that providers have the skills and knowledge about how to coordinate care across these systems. Finally, continued adaptation of evidence-based MH interventions for autistic individuals that can be feasibly implemented by non-specialized community MH clinicians is essential (Adams & Young, 2020; Camm-Crosbie et al., 2019; Wood et al., 2015), particularly in regard to suicide prevention strategies (Jager-Hyman et al., 2020; Schwartzman et al., 2021). Wide-scale adaptation and implementation of evidence-based services have been accomplished for other populations (e.g., youth with trauma; individuals experiencing first-episode psychosis). Such an effort is needed for autistic youth. Unfortunately, the limited autism research funding that has been allocated to services research, and specifically to dissemination and implementation and policy projects (Cervantes et al., 2021), presents a barrier. However, with a concerted and focused investment in building services, expanding service capacity, and ensuring workforce competencies to deliver high quality, evidence-based care, advancement is within reach.
Acknowledgements:
This study was funded by the Organization for Autism Research (OAR) and the National Institute of Mental Health (P50MH113662). The authors thank OAR and the NIMH for their support but acknowledge that the findings and conclusions are those of the authors and do not necessarily reflect the opinions of OAR or the NIMH.
References
- Adams D, & Young K (2020). A systematic review of the perceived barriers and facilitators to accessing psychological treatment for mental health problems in individuals on the autism spectrum. Review Journal of Autism and Developmental Disorders. 10.1007/s40489-020-00226-7 [DOI] [Google Scholar]
- Advocates for Children of New York, Inc. (2020). Applying for OPWDD. https://www.advocatesforchildren.org/sites/default/files/library/applying_for_opwdd.pdf?pt=1
- Anderson C, & Butt C (2018). Young adults on the autism spectrum: The struggle for appropriate services. Journal of Autism and Developmental Disorders, 48(11), 3912–3925. 10.1007/s10803-018-3673-z [DOI] [PubMed] [Google Scholar]
- Benevides TW, Shore SM, Palmer K, Duncan P, Plank A, Andresen M-L, Caplan R, Cook B, Gassner D, Hector BL, Morgan L, Nebeker L, Purkis Y, Rankowski B, Wittig K, & Coughlin SS (2020). Listening to the autistic voice: Mental health priorities to guide research and practice in autism from a stakeholder-driven project. Autism, 24(4), 822–833. 10.1177/1362361320908410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Baker-Ericzén M, Stadnick N, & Taylor R (2012). Parent perspectives on community mental health services for children with autism spectrum disorders. Journal of Child and Family Studies, 21(4), 533–544. 10.1007/s10826-011-9506-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Drahota A, Chlebowski C, Koenig Y, Williams KN, Hill B, & McPherson J (2020). Designing autism spectrum disorder interventions for community implementation. In White SW, Maddox BB, & Mazefsky CA (Eds.), The Oxford Handbook of Autism and Co-Occurring Psychiatric Conditions. Oxford University Press. 10.1093/oxfordhb/9780190910761.013.21 [DOI] [Google Scholar]
- Brookman-Frazee L, Drahota A, Stadnick N, & Palinkas LA (2012). Therapist perspectives on community mental health services for children with autism spectrum disorders. Administration and Policy in Mental Health and Mental Health Services Research, 39(5), 365–373. 10.1007/s10488-011-0355-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camm-Crosbie L, Bradley L, Shaw R, Baron-Cohen S, & Cassidy S (2019). ‘People like me don’t get support’: Autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism, 23(6), 1431–1441. 10.1177/1362361318816053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor J, McBain RK, Kofner A, Stein BD, & Yu H (2020). Fewer than half of US mental health treatment facilities provide services for children with autism spectrum disorder: Results from a survey of US mental health treatment facilities on the availability of behavioral health care services for children with autism spectrum disorder. Health Affairs, 39(6), 968–974. 10.1377/hlthaff.2019.01557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor J, McBain RK, Kofner A, Stein BD, & Yu H (2021). Where are US outpatient mental health facilities that serve children with autism spectrum disorder? A national snapshot of geographic disparities. Autism, 13623613211024046. 10.1177/13623613211024046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (2021, March 22). Behavioral health services in New York. https://www.cdc.gov/childrensmentalhealth/stateprofiles-providers/new-york/index.html
- Cervantes PE, Li A, Sullivan KA, Seag DEM, Baroni A, & Horwitz SM (2022). Assessing and managing suicide risk in autistic youth: Findings from a clinician survey in a pediatric psychiatric emergency setting. Journal of Autism and Developmental Disorders. 10.1007/s10803-022-05448-8 [DOI] [PubMed] [Google Scholar]
- Cervantes PE, Matheis M, Estabillo J, Seag DEM, Nelson KL, Peth-Pierce R, Hoagwood KE, & Horwitz SM (2021). Trends over a decade in NIH funding for autism spectrum disorder services research. Journal of Autism and Developmental Disorders, 51(8), 2751–2763. 10.1007/s10803-020-04746-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson KS, Lind T, Jobin A, Kinnear M, Lok H, & Brookman-Frazee L (2021). A systematic review of mental health interventions for ASD: Characterizing interventions, intervention adaptations, and implementation outcomes. Administration and Policy in Mental Health and Mental Health Services Research, 48(5), 857–883. 10.1007/s10488-021-01133-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoagwood KE, Olin SS, Horwitz S, McKay M, Cleek A, Gleacher A, Lewandowski E, Nadeem E, Acri M, Chor KHB, Kuppinger A, Burton G, Weiss D, Frank S, Finnerty M, Bradbury DM, Woodlock KM, & Hogan M (2014). Scaling up evidence-based practices for children and families in New York State: Toward evidence-based policies on implementation for state mental health systems. Journal of Clinical Child & Adolescent Psychology, 43(2), 145–157. 10.1080/15374416.2013.869749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager-Hyman S, Maddox BB, Crabbe SR, & Mandell DS (2020). Mental health clinicians’ screening and intervention practices to reduce suicide risk in autistic adolescents and adults. Journal of Autism and Developmental Disorders, 50(10), 3450–3461. 10.1007/s10803-020-04441-3 [DOI] [PubMed] [Google Scholar]
- Kalb L, Stuart E, Freedman B, Zablotsky B, & Vasa R (2012). Psychiatric-related emergency department visits among children with an autism spectrum disorder. Pediatric Emergency Care, 28(12), 1269–1276. 10.1097/PEC.0b013e3182767d96 [DOI] [PubMed] [Google Scholar]
- Kõlves K, Fitzgerald C, Nordentoft M, Wood SJ, & Erlangsen A (2021). Assessment of suicidal behaviors among individuals with autism spectrum disorder in Denmark. JAMA Network Open, 4(1), e2033565–e2033565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake JK, Perry A, & Lunsky Y (2014). Mental health services for individuals with high functioning autism spectrum disorder. Autism Research and Treatment, 2014, e502420. 10.1155/2014/502420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox BB, Crabbe S, Beidas RS, Brookman-Frazee L, Cannuscio CC, Miller JS, Nicolaidis C, & Mandell DS (2020). “I wouldn’t know where to start”: Perspectives from clinicians, agency leaders, and autistic adults on improving community mental health services for autistic adults. Autism, 24(4), 919–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox BB, Dickson KS, Stadnick NA, Mandell DS, & Brookman-Frazee L (2021). Mental health services for autistic individuals across the lifespan: Recent advances and current gaps. Current Psychiatry Reports, 23(10), 66. 10.1007/s11920-021-01278-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox BB, & Gaus VL (2019). Community mental health services for autistic adults: Good news and bad news. Autism in Adulthood, 1(1), 15–19. 10.1089/aut.2018.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConachie H, Livingstone N, Morris C, Beresford B, Le Couteur A, Gringras P, Garland D, Jones G, Macdonald G, Williams K, & Parr JR (2018). Parents suggest which indicators of progress and outcomes should be measured in young children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(4), 1041–1051. 10.1007/s10803-017-3282-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire TG, & Miranda J (2008). New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs (Project Hope), 27(2), 393–403. 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menezes M, Robinson L, Sanchez MJ, & Cook B (2018). Depression in youth with autism spectrum disorders: A systematic review of studies published between 2012 and 2016. Review Journal of Autism and Developmental Disorders, 5(4), 370–389. 10.1007/s40489-018-0146-4 [DOI] [Google Scholar]
- NYS OMH. (n.d.-a). About OMH. Retrieved November 5, 2021, from https://omh.ny.gov/omhweb/about/
- NYS OMH. (n.d.-b). Information for Children, Teens and Their Families. Retrieved November 5, 2021, from https://omh.ny.gov/omhweb/childservice/
- NYS OMH. (2021). New York State Office of Mental Health 14 NYCRR Part 599 Clinic Treatment Programs Interpretive/Implementation Guidance. https://omh.ny.gov/omhweb/clinic_restructuring/part599/part-599.pdf
- NYS OPWDD. (n.d.-a). About Us. Office for People With Developmental Disabilities. Retrieved November 5, 2021, from https://opwdd.ny.gov/about-us
- NYS OPWDD. (n.d.-b). Article 16 Clinics. Office for People With Developmental Disabilities. Retrieved November 5, 2021, from https://opwdd.ny.gov/providers/article-16-clinics
- Olin SS, O’Connor BC, Storfer-Isser A, Clark LJ, Perkins M, Hudson Scholle S, Whitmyre ED, Hoagwood K, & Horwitz SM (2016). Access to care for youth in a state mental health system: A simulated patient approach. Journal of the American Academy of Child & Adolescent Psychiatry, 55(5), 392–399. 10.1016/j.jaac.2016.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartzman JM, Smith JR, & Bettis AH (2021). Safety planning for suicidality in autism: Obstacles, potential solutions, and future directions. Pediatrics, 148(6), e2021052958. 10.1542/peds.2021-052958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, & Baird G (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929. 10.1097/CHI.0b013e318179964f [DOI] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Klebanoff S, & Brookman-Frazee L (2015). Toward the implementation of evidence-based interventions for youth with autism spectrum disorders in schools and community agencies. Behavior Therapy, 46(1), 83–95. 10.1016/j.beth.2014.07.003 [DOI] [PubMed] [Google Scholar]


