Abstract
We report two cases of pulmonary collapse that simulated pneumothorax on computed tomographic images and were caused by rapid complete bronchial obstruction. One patient was a 77-year-old woman with sudden dyspnea, and the other was an 83-year-old woman with sudden dyspnea who was infected with influenza A virus. Chest computed tomography revealed lobular complete atelectasis with an almost complete expansion of the other lobes of the right lung. Some air space in the right pleural cavity was also observed. Both cases were diagnosed as “pneumothorax” by primary doctors. We noted the disappearance of air density in the lumen of the right bronchus in both cases. We performed bronchoscopy before thoracic drainage and removed the obstruction. Immediately, the obstructed pulmonary lobes expanded, and the air space in the pleural cavity disappeared without thoracic drainage. In the literature, this pneumothorax-like pulmonary collapse is called as “pneumothorax ex vacuo.”
Keywords list: Bronchoscopy, Pneumothorax ex vacuo, Pulmonary collapse
Abbreviations: PEV, pneumothorax ex vacuo
Highlights
-
•
Pneumothorax ex vacuo patients may be diagnosed with typical closed pneumothorax.
-
•
Two cases here illustrate pulmonary collapse due to a rapid complete bronchial obstruction.
-
•
Diagnosed as pneumothorax, the cases were later discovered as pneumothorax ex vacuo.
-
•
Bronchoscopy is more effective than thoracic drainage in treating this condition.
1. Introduction
Pneumothorax is a common disease defined by air in the pleural cavity, resulting in a partial or total collapse of the lung. In the case of a closed pneumothorax, air in the pleural cavity enters from the lung via the visceral pleura fistula or, with an open pneumothorax from outside the chest wall. Thoracic drainage or surgery is usually required to treat moderate or severe pulmonary collapse.
Conversely, pneumothorax ex vacuo (PEV) is characterized by collapsed lung and air space in the pleural cavity due to rapid bronchial obstruction, which does not present with visceral pleural fistula or an open injury of the chest cavity [1]. Therefore, thoracic drainage is an ineffective treatment.
Bronchial obstruction is usually characterized by the disappearance of air density in the lumen of the bronchus, partial or complete pulmonary collapse, mediastinal shift to the affected side, and absence of air space in the affected pleural cavity. However, it is a rare condition where bronchial obstruction and air space in the pleural cavity exist together, explaining the few reports on PEV. We report two cases of PEV that were successfully treated with bronchoscopy alone.
2. Narrative
2.1. Case 1
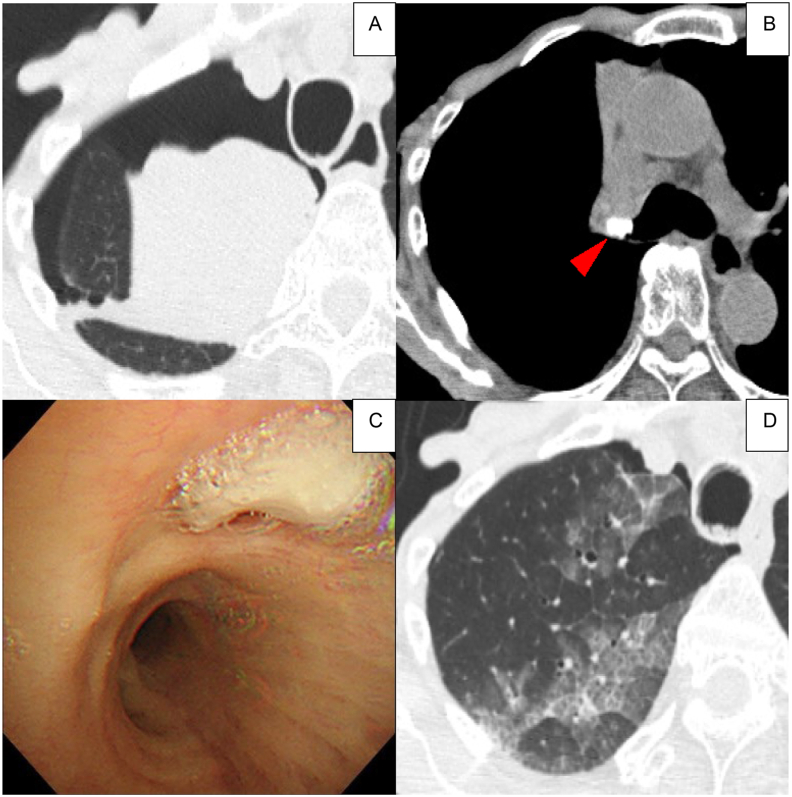
A 77-year-old woman presented with a sudden worsening of her respiratory status. Chest computed tomography (CT) showed a complete pulmonary collapse of the upper lobe of the right lung, an almost complete expansion of the middle and lower lobes, and a mediastinal shift to the affected side. An air space in the right pleural cavity appeared around the atelectasis of the upper lobe. She was diagnosed with pneumothorax by her primary doctor. A calcified mass, which was suggestive of a foreign body, was observed in the lumen of the right upper bronchus (Fig. 1). Bronchoscopy revealed obstruction of the bronchial lumen of the right upper lobe bronchus by grains of rice. The foreign body was extracted from the bronchial lumen. The day after removal of the rice grains, chest CT showed that the right upper pulmonary lobe had expanded completely, with some pulmonary edema. The air space in the pleural cavity disappeared and the mediastinal shift improved. The pneumothorax of the right pleural cavity improved without thoracic drainage.
Fig. 1.
case 1
The upper lobe of the right lung is completely collapsed, but the middle and lower lobes are almost completely expanded, and an air space in the right pleural cavity has appeared around the atelectasis of the upper lobe (A). A calcified mass (red arrowhead), which is suggestive of a foreign body, is observed in the lumen of the right upper bronchus (B). Bronchoscopy reveals obstruction of the bronchial lumen of the upper lobe bronchus by the rice grains (C). After removal of the rice grains, the right upper pulmonary lobe has expanded completely, with some pulmonary edema (D). . (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
2.2. Case 2
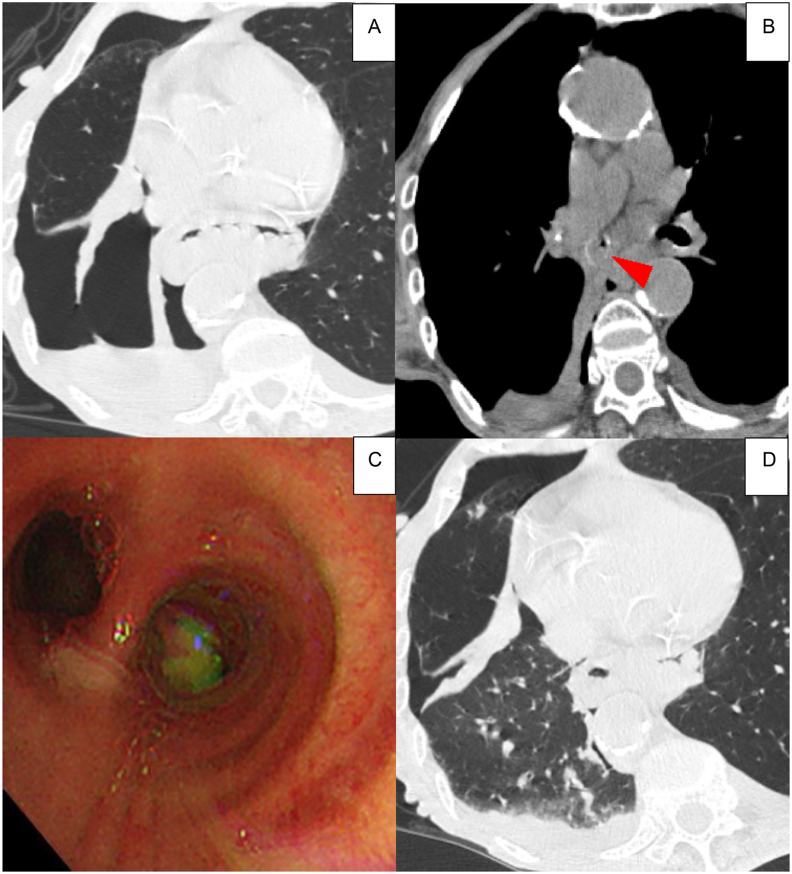
An 83-year-old woman presented with a sudden worsening of her respiratory status. A rapid diagnostic test using nasopharyngeal swabs confirmed that she was infected with the influenza A virus. She was diagnosed with right pneumothorax by her primary doctor. Chest CT revealed a complete pulmonary collapse of the middle and lower lobes of the right lung, an almost complete expansion of the upper lobe, and a mediastinal shift to the affected side (Fig. 2). An air space appeared in the right pleural cavity. The right intermediate bronchial trunk was obstructed by viscous sputum, which was removed using bronchoscopy. Chest CT was performed on the same day after the bronchoscopic removal of the sputum. It showed that the atelectasis of the middle and lower lobes had improved, and air space in the right pleural cavity had disappeared without thoracic drainage.
Fig. 2.
case 2
The middle and lower lobes of the right lung are completely collapsed, but the upper lobe is almost completely expanded, and an air space in the right pleural cavity has appeared around the collapsed lobes (A). The right intermediate bronchial trunk is obstructed by sputum (red arrowhead) (B). Bronchoscopy reveals obstruction of the bronchial lumen by viscous sputum (C). After the bronchoscopic removal of sputum, atelectasis of the middle and lower lobes improves, and the air space in the right pleural cavity almost disappears (D). . (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
PEV is a closed pneumothorax that occurs due to acute pulmonary collapse caused by a sudden bronchial obstruction without a visceral pleural fistula [2]. However, it only occurs under very specific conditions, and PEV has been reported in the literature in a few cases. The mechanism has not been sufficiently clarified until now.
This report suggests the following clinical lessons: 1) air space in a pleural cavity can be caused by acute bronchial obstruction even without air supply via visceral pleural fistula, and 2) bronchoscopy prioritized over thoracic drainage might be effective in treating this condition.
First, sudden lobar bronchial obstruction by a foreign body may result in total pulmonary collapse and the appearance of air space in the affected pleural cavity. Although both patients were diagnosed with “pneumothorax” by their primary doctors, the actual cause of the collapsed lung was not the same as typical closed pneumothorax. The rationale for this decision is as follows.
(ⅰ) In the usual pneumothorax, the mediastinum and diaphragm are shifted to the sound side, whereas in the two cases, they were shifted to the affected side. This condition suggests pathology unlike a typical closed pneumothorax (Table 1). Cho Y–K et al. reported encouraging results; they used 10 rabbits to create a model of acute bronchial obstruction, and herniations on the affected side were observed in eight rabbits [3].
(ⅱ) On the affected side, expansion of the other lobes was almost completely preserved. In a typical closed pneumothorax condition, in which the pleural cavity is over pressurized by air, the other lobes should be poorly expanded. Florman S et al. stated that the most critical point is that PEV is limited to the pleural cavity between the collapsed lobe and chest wall and does not extend to the other remaining inflated lobes [4].
(ⅲ) Despite the rapid improvement in pulmonary collapse, there was no evidence of subcutaneous or mediastinal emphysema. If a large amount of air has accumulated in the pleural cavity, then, without thoracic drainage, the accumulated air would be seen as subcutaneous or mediastinal emphysema. In these two cases, chest CT was rechecked a short time after the collapse had improved, but there were no findings of subcutaneous or mediastinal emphysema.
(ⅳ) Bronchial obstruction is usually revealed as “partial or complete pulmonary atelectasis; ” however, there is no air space in the affected pleural cavity. A possible mechanism against the hyper-negative pressure caused by pulmonary collapse might be a mediastinal shift, a diaphragmatic elevation, and an over-expansion of the other lobes, avoiding the appearance of air space in the pleural cavity. However, under the very special condition of acute pulmonary collapse, these compensatory mechanisms may not be sufficiently effective, resulting in the appearance of air space in the pleural cavity.
Table 1.
Characteristics of CT findings.
| Diagnosis | usual closed pneumothorax | PEV |
|---|---|---|
| air space in the pleural cavity | + | + |
| bronchial obstruction | – | + |
| mediastinum or diaphragm shift | sound side | affected side |
| expansion of the other lobes | poorly | almost completely |
| subcutaneous or mediastinum emphysema | either | – |
PEV; pneumothorax ex vacuo.
Second, bronchoscopy is more effective than thoracic drainage and observation. In the two cases presented here, bronchoscopic removal of the bronchial obstruction was performed without thoracic drainage, and the air space in the pleural cavity disappeared. If PEV had been misdiagnosed as a typical closed pneumothorax and thoracic drainage had been performed, it is likely that the over-negative pressure would have drawn external air into the pleural cavity, resulting in indistinguishability from a typical closed pneumothorax case.
In the special condition of PEV, acute pulmonary collapse increases the negative intrapleural pressure surrounding the collapsed lobe. Therefore, it is considered that the affected pleural cavity is filled with gas originating from the ambient tissues and blood [5]. However, the density and pressure of the gas in the affected pleural cavity may still be lower than those in the atmosphere. As a result, it has been reported that drainage is normally not necessary as a treatment strategy for PEV and that a ‘wait-and-see’ policy can be successful in these patients as the pneumothorax will slowly resolve [6]. Although it is not clear how long it will take to improve with the ‘wait-and-see’ policy, Cho Y–K et al. also reported in the rabbit model experiment mentioned above, that the pneumothorax resolved completely in all rabbits during the 2-week follow-up [3].
On the other hand, Richard W. Light stated that, in terms of respiratory physiology, the pressure in the pleural cavity must be more negative than −60 cmH2O for air to be drawn out of the tissues and accumulate in the pleural cavity. He then questioned whether such an over-negative pressure could actually occur in the pleural cavity [7].
This is the first report to compare CT findings before and after PEV treatment. Since neither case showed subcutaneous nor mediastinal emphysema on post-treatment CT, it is unlikely that there was a large amount of air in the affected pleural cavity. Slow bronchial obstruction can usually produce no air space in the affected pleural cavity; however, these very special conditions of acute pulmonary collapse might result in the appearance of air space in the pleural cavity. Under these conditions, it is more reasonable to assume that the affected pleural cavity was in a state of hyper-negative pressure compared to the atmosphere, similar to a vacuum. If this condition had continued, the air space in the pleural cavity would have gradually disappeared because of the usual compensatory mechanisms. However, in our cases, we removed the bronchial obstruction by bronchoscopy at a stage before the compensatory mechanism set in, and the pulmonary collapse improved quickly.
Thus, for acute pulmonary collapse with bronchial obstruction, especially with mediastinal shift to the affected side and expansion of the other lung lobes, aggressive bronchoscopic removal of bronchial obstruction should be considered, because it may be a more appropriate treatment for PEV than thoracic drainage or “wait-and-see” policy.
In conclusion, as there are only a few reports on PEV, it may have been latent in some patients who were misdiagnosed with typical closed pneumothorax and underwent thoracic drainage. We need to be aware of this condition so that we can diagnose correctly and give appropriate treatment.
Summary conflicts of interest statement
The authors have no conflicts of interest to declare.
Funding information
None of the authors have any funding to disclose.
Notation of prior abstract publication/presentation
Not applicable.
Author contributions
D.H. drafted the manuscript; D.H., T.S., T.A., and G.S. performed bronchoscopy and systemic management during hospitalization; R.K. revised the manuscript; all authors have read and approved the final manuscript.
Financial/nonfinancial disclosures
None declared.
We would like to thank Editage (www.editage.jp) for English language editing.
Handling Editor: DR AC Amit Chopra
References
- 1.Woodring J.H., Baker M.D., Stark P. Pneumothorax ex vacuo. Chest. 1996;110(4):1102–1105. doi: 10.1378/chest.110.4.1102. [DOI] [PubMed] [Google Scholar]
- 2.Valipour A., Slebos D.J., de Oliveira H.G., et al. Expert statement: pneumothorax associated with endoscopic valve therapy for emphysema--potential mechanisms, treatment algorithm, and case examples. Respiration. 2014;87(6):513–521. doi: 10.1159/000360642. [DOI] [PubMed] [Google Scholar]
- 3.Cho Y.K., Shin J.H., Oh Y.M., et al. Experimental lung collapse following deployment of a self-expandable bronchial occluder in a rabbit model. Br. J. Radiol. 2012;85(1014):e146–e152. doi: 10.1259/bjr/40247893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Florman S., Young B., Allmon J.C., et al. Traumatic pneumothorax ex vacuo. J. Trauma. 2001;50(1):147–148. doi: 10.1097/00005373-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 5.van Dijk M., Sue R., Criner G.J., et al. Expert statement: pneumothorax associated with one-way valve therapy for emphysema: 2020 update. Respiration. 2021;100(10):969–978. doi: 10.1159/000516326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koster T.D., Klooster K., Ten Hacken N.H.T., et al. Endobronchial valve therapy for severe emphysema: an overview of valve-related complications and its management. Expet Rev. Respir. Med. 2020;14(12):1235–1247. doi: 10.1080/17476348.2020.1813571. [DOI] [PubMed] [Google Scholar]
- 7.Light R.W. sixth ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2013. Pleural Diseases; pp. 8–18. [Google Scholar]