Abstract
Objective
The COVID‐19 pandemic created significant challenges in accessing and receiving treatment for individuals with eating disorders (EDs). The purpose of this study is to explore perceptions of and experiences with ED treatment during the first year of the pandemic among individuals with past and self‐reported EDs in the United States.
Methods
Online surveys were administered to adults (N = 510) with a past or current self‐reported ED at 13 timepoints between April 2020 and May 2021. Using longitudinal qualitative analysis, 5651 free‐text responses were examined to capture experiences with ED treatment and generate inferences of change over time.
Results
We categorized results into four sequential, temporal quarters and identified patterns that explained participants' perceptions of facilitators, barriers, and experiences with ED treatment over time: Quarter 1. Treatment Disruption and Reorienting Recovery; Quarter 2. Accumulating COVID‐19 Stress and Virtual Treatment Woes; Quarter 3. A Continuation of Inadequate Care; and Quarter 4. Ongoing Adaptation and Adjustment to Uncertainty. Participant experiences were marked by numerous barriers to accessing care, challenges adjusting to virtual treatment, unmet treatment needs, and beginning acceptance of telehealth.
Discussion
Our findings present a timeline to help evaluate challenges related to navigating the switch to virtual care which created significant disruption to ED recovery. Participants spent much of the first year trying to adjust to unemployment, loss of insurance, and lack of access to in‐person treatment. Future research should identify additional strategies to improve the receipt and experience of care for EDs.
Public Significance
Our findings suggest that individuals with eating disorders were significantly challenged by accumulating COVID‐19 stress, worsening symptomatology, and limited access to effective treatment during the first year of the pandemic. This knowledge can guide clinicians, treatment centers, and policy makers in addressing the behavioral health needs of individuals impacted by disordered eating amidst emergent public health crises.
Keywords: COVID‐19, eating disorder treatment, eating disorders, recovery
1. INTRODUCTION
The novel coronavirus (COVID‐19) pandemic has significantly impacted access to mental health treatment. As global healthcare systems responded to contain spread and treat critically ill cases, access to psychiatric and psychological treatment was limited (Cooper et al., 2022; Murphy et al., 2020; Weissman et al., 2020). Further, in the United States, job losses during the pandemic decreased access to employer‐provided health insurance (Banthin et al., 2020; US Department of Labor, 2022), increasing barriers to health care access and contributing to the deterioration of physical and mental health (Berkowitz & Basu, 2021; Egede et al., 2020).
Of particular interest is the lived experience of those managing eating disorders (ED) during COVID‐19. For example, individuals with EDs reported increased social isolation (Brown et al., 2021; Termorshuizen et al., 2020), changes in access to treatment (Spigel et al., 2021), and challenges with changes in routine and structure (Goode et al., 2022; Vuillier et al., 2021). Moreover, a systematic review (Devoe et al., 2022) reported a 48% increase in hospital admissions for EDs worldwide during the pandemic compared with pre‐pandemic. In fact, eating disorder symptoms have increased both among individuals with a current eating disorder and those previously in recovery (Castellini et al., 2020; Richardson et al., 2020; Termorshuizen et al., 2020). Furthermore, the pandemic created challenges for people with EDs, such as difficulty accessing food consistent with recovery meal planning, concern about worsening ED symptoms due to increased time spent in a triggering environment, and disconnect from social networks (Rodgers et al., 2020; Termorshuizen et al., 2020).
Additionally, the COVID‐19 pandemic has also furthered challenges to accessing and receiving ED treatment. The diversion of health care resources towards managing the virus, coupled with the risk of contracting COVID‐19 during in‐person treatment settings, has restricted access to treatment and shifted many care opportunities to telehealth platforms (Cooper et al., 2022). This shift may offer some potential benefits, including increased accessibility and convenience for individuals who may otherwise be unable or uncomfortable attending in‐person appointments (Barney et al., 2020; Frayn et al., 2021; Weissman et al., 2020). However, telehealth presents additional challenges to services, including confidentiality and privacy, and limited capacity to monitor weight, vital signs, and other physiological assessments (Cooper et al., 2022; Frayn et al., 2021; Matheson et al., 2020; Murphy et al., 2020). Across studies, participants report missing the structure of in‐person treatment and a general preference for the connectedness of in‐person groups (Frayn et al., 2021; Griffiths et al., 2018; Weissman et al., 2020). Indeed, with the rapid shift to teletherapy during COVID‐19, ED providers and patients navigated numerous difficulties.
Importantly, individuals with EDs also reported changes with the structure and format of ED treatment during the pandemic (Frayn et al., 2021; Vuillier et al., 2021). Early in the pandemic, whereas health services were likely re‐organizing healthcare delivery, patients reported fewer treatment sessions and reduced quality of care (Birgegard et al., 2021). Little is known, however, about their perceptions and experiences of these changes over time as the pandemic evolved. Therefore, the purpose of this study is to examine the perceptions of and experiences with ED treatment among individuals who reported a past or present ED during the first year of the COVID‐19 pandemic (April 2020–May 2021), using longitudinal qualitative analysis. Using 5651 free‐text responses, the aim of the study was to understand participant barriers, facilitators, and experiences with treatment as they unfolded over 13 different timepoints. Our hope is that this research will elucidate the challenges faced by those living with EDs and illuminate opportunities for improving or developing treatments that meet patient needs.
2. METHODS
A longitudinal qualitative research design (Calman et al., 2013; Saldaña, 2021) was implemented to capture changes in facilitators, barriers, and experiences related to ED treatment during the first year of the pandemic. We employed an interpretivist constructivist research paradigm to explore how participants perceived available services during an unprecedented time. An interpretivist constructivist paradigm posits that learning how people understand the world, interpret their encounters, and assign meaning and values to events is essential to learning (Rubin & Rubin, 2012). Within this paradigm, the epistemological framework puts forth that human phenomena are socially constructed, rather than objectively real, and underscores the importance of subjectivity and reflexivity in examining these phenomena (Padgett, 2016). Therefore, we relied on the researcher and participant perspectives to co‐create findings or reality. Ethical approval was granted by the University of North Carolina Biomedical Institutional Review Board (IRB #20‐0964).
2.1. Positionality and reflexivity
We began by reflecting on our own positionality given that our analytic lens is informed by our backgrounds and relationship to this work. The data analysis team consisted of undergraduate and graduate students (BA, HW, KO, TN, AM) and was led by SG. SG identifies as a Latinx cis‐gender woman. BA identifies as a Ghanaian‐American nonbinary person. HW, KO, TN, and AM identify as White, cisgender women. To avoid bias, and to ensure thoughtful engagement with the data and reflexive processes throughout analysis, regular consultations occurred with SG and RG (Black, cis‐gender woman and study lead). The research team was mindful of their personal and professional experiences with EDs and the COVID‐19 pandemic throughout their examination of the data, and engaged in continual reflection of their own power, positionality, identities, and experiences as they intersected with the research process and data analysis.
2.2. Participants and procedures
Participants with self‐reported EDs were recruited between April and May 2020 to complete an online study at 13 monthly time points about their experiences with EDs during the COVID‐19 pandemic. Recruitment channels included social media (e.g., Facebook, Twitter, Instagram), the University of North Carolina at Chapel Hill Exchanges blog, and emails to participants from ongoing studies through the UNC Center of Excellence for Eating Disorders who had consented to recontact. Participants were enrolled and consented during the study period from April 8, 2020, through May 6, 2021. By the end of April 2020, there were more than 1 million COVID‐19 cases in the United States (US). Early responses in March/April 2020 included social distancing and quarantines to slow the spread of the disease. The first vaccines were authorized for use in December 2020, and Americans were widely encouraged to vaccinate in early 2021.
Given our interpretivist constructivist research paradigm and epistemological framework, we used a dialectic methodology to capture participants' perceptions and experiences with the phenomenon. Participants were asked to complete an online survey (details have been described elsewhere; Termorshuizen et al., 2020), which included four free‐text questions (Table 1) assessing the following: (a) positive changes in their ED; (b) ED‐related treatment needs; (c) other ED‐related concerns not queried elsewhere in the survey; and (d) positive changes in their lives due to the COVID‐19 pandemic. Only the free‐text responses were analyzed for the purposes of this study. The surveys were administered at baseline and approximately once per month on 12 occasions over a 1‐year period using Qualtrics software, which limited responses to one per IP address and prevented search engines from finding the survey. No compensation was offered for participation in this study except for entry into a raffle for an electronic tablet at 12 months.
TABLE 1.
Baseline free‐text response survey questions
| Survey Questions |
|---|
| In the past 2 weeks, have you experienced any positive changes in your eating disorder symptoms? |
| In the last 2 weeks, what other eating‐disorder related concerns have you had that are not listed above? |
| In the last 2 weeks, what have been your greatest needs with regards to eating disorder treatment or support? |
| Has the COVID‐19 situation led to any positive changes in your life? |
2.3. Data analysis
We conducted longitudinal qualitative analysis and used inductive and iterative techniques to identify patterns, changes over time, and critical moments among participants, as guided by Saldaña (2021). Upon data collection completion, and prior to coding, we reviewed all free‐text responses (N = 5651) from the 13 timepoints to synthesize and organize responses (n = 727) into coinciding tables that captured participants' facilitators, barriers, and experiences with ED‐related treatment. The tables were then divided into four quarters to reflect changes in annual seasons and to help make meaning of changes over time: Quarter 1 (Baseline, Months 1 and 2); Quarter 2 (Months 3–5); Quarter 3 (Months 6–8); and Quarter 4 (Months 9–12). Due to sample attrition, survey responses were not linked across time within each participant. We then conducted line‐by‐line coding for a nuanced, data‐driven analysis (Saldaña, 2021). The codebook was developed in an iterative and cyclical process which involved grouping similarly coded data into categories based on shared characteristics (Saldaña, 2021). Any areas of disagreement were discussed in team meetings until consensus was reached, with an emphasis on staying close to the participants' words to find balance between participants' meaning and researchers' interpretation.
Using qualitative longitudinal analysis, we then synthesized data, including identified codes, into a series of matrices for comparative analysis and interpretation of research observations to assess change over time (see Table 2; Saldaña, 2021). Two teams of two or three researchers completed matrices for all quarters. In several large team meetings, each of the seven descriptive cells and matrix for each quarter were chronologically compared with the comparable cells and matrices from the other quarters until consensus on findings was reached.
TABLE 2.
Overview of seven descriptive categories in the summary matrices
| Category | Summary |
|---|---|
| 1. Increase and Emerge | Qualitative summary observations that answer what increases or emerges in participants' perceptions of and experiences with eating disorder (ED) treatment through time? |
| 2. Cumulative | Summary observations that answer what is cumulative in participants' perceptions of and experiences with ED treatment through time? |
| 3. Surges, Epiphanies, and Turning Points | Summary observations that answer what kind of surges, epiphanies, or turning points occur in participants' perceptions of and experiences ED treatment through time? |
| 4. Decrease and Cease | Summary observations that answer what decreases or ceases in participants' perceptions of and experiences ED treatment through time? |
| 5. Constant and Consistent | Summary observations that answer what remains constant or consistent in participants' perceptions of and experiences ED treatment through time? |
| 6. Idiosyncratic | Summary observations that answer what is idiosyncratic in participants' perceptions of and experiences with ED treatment through time? |
| 7. Missing | Summary observations that answer what is missing from participants' perceptions of and experiences with ED treatment through time? |
Note: Qualitative longitudinal analysis was guided by Saldaña (2021).
To enhance trustworthiness and reduce bias, researchers performed negative case analysis (Padgett, 2016). Negative case analysis includes frequently reviewing data to ensure researchers are critically self‐reflective, seeking alternative explanations, and upholding the integrity of unique cases that may disprove preliminary notions or may be identified as anomalies (Morrow, 2005; Padgett, 2016; Patton, 2002). Researchers also engaged in audit trailing which included documenting detailed self‐reflective and analytic memos and iterations of the codebook (Padgett, 2016). Memos were discussed in team meetings and enabled researchers to be interpretative and reflective about how their own power and worldviews shaped their understanding of these data. Though this study was not without limitations, including sample attrition and data not being linked across time within person, the resulting data provided sufficient depth and breadth to examine themes that were generated in each quarter (Johnson et al., 2020).
3. RESULTS
Table 3 presents the demographic characteristics of the sample. At baseline, 510 participants completed the survey, and 94% (n = 479) left at least one‐free text response. On average, participants were 30.6 (±9.3) years of age, cisgender female (97%), and White (94%) with a current or past self‐reported ED. Participants reported a lifetime history of anorexia nervosa (62%), bulimia nervosa (35%), and binge‐eating disorder (31%). Table 4 depicts the number of free‐text responses received, and the number of respondents who participated in the baseline and each follow‐up survey. Though there was significant attrition between baseline and the 1‐year follow‐up (71%), describing the experiences and perceptions of treatment among participants across timepoints held relevance.
TABLE 3.
Demographics of study participants (n = 510)
| Characteristic | Participants mean (SD) or n (%) |
|---|---|
| Age | 30.61 (9.37) |
| 16–21 | 63 (12%) |
| 22–29 | 230 (45%) |
| 30–39 | 133 (26%) |
| 40–49 | 57 (11%) |
| 50+ | 27 (5%) |
| Biological sex | |
| Female | 495 (97%) |
| Male | 14 (3%) |
| Intersex | <5 (<1%) |
| Gender identity | |
| Female | 484 (95%) |
| Male | 13 (3%) |
| Nonbinary/gender fluid/other | 14 (2%) |
| Region | |
| South | 151 (30%) |
| Northeast | 120 (23%) |
| West | 109 (21%) |
| Midwest | 96 (19%) |
| Lifetime eating disorders a | |
| AN | 318 (62%) |
| BN | 178 (35%) |
| BED | 156 (31%) |
| Atypical AN | 100 (20%) |
| OSFED/EDNOS | 122 (24%) |
| Purging disorder | 38 (7%) |
| ARFID | 34 (7%) |
| Night‐eating disorder | 20 (4%) |
| Currently have an ED | 474 (93%) |
Percentages add to over 100 as participants could indicate more than one lifetime eating disorder.
TABLE 4.
Study participants and respondents to free‐text questions at each time point
| Time point | Total # of sample participants | % of baseline participants | Total # of respondents to free‐text question(s) | % of cohort to respond to free‐text question(s) | Total # of free text responses |
|---|---|---|---|---|---|
| Baseline | 510 | 100 | 479 | 93.9 | 1224 |
| Month 1 | 359 | 70.4 | 324 | 90.3 | 857 |
| Month 2 | 296 | 58.0 | 269 | 90.9 | 690 |
| Month 3 | 247 | 48.4 | 220 | 89.1 | 588 |
| Month 4 | 129 | 25.3 | 114 | 88.4 | 274 |
| Month 5 | 115 | 22.6 | 110 | 95.7 | 278 |
| Month 6 | 103 | 20.2 | 95 | 92.2 | 235 |
| Month 7 | 97 | 19.0 | 86 | 88.7 | 206 |
| Month 8 | 98 | 19.2 | 92 | 93.9 | 213 |
| Month 9 | 106 | 20.8 | 85 | 80.2 | 217 |
| Month 10 | 96 | 18.8 | 88 | 91.7 | 220 |
| Month 11 | 76 | 14.9 | 73 | 96.1 | 178 |
| Month 12 | 146 | 28.6 | 115 | 78.8 | 471 |
The participants' rich and descriptive free‐text responses form the basis for the model explaining the perceptions and experiences reported in the first year of the COVID‐19 pandemic (see Figure 1). The model describes the experience of transitioning through four different quarters of the pandemic: Quarter 1. Treatment Disruption and Reorienting Recovery; Quarter 2. Accumulating COVID‐19 Stress and Virtual Treatment Woes; Quarter 3. A Continuation of Inadequate Care; and Quarter 4. Ongoing Adaptation and Adjustment to Uncertainty. Descriptions of each quarter are presented below, along with representative quotations to further elucidate the participant experience.
FIGURE 1.
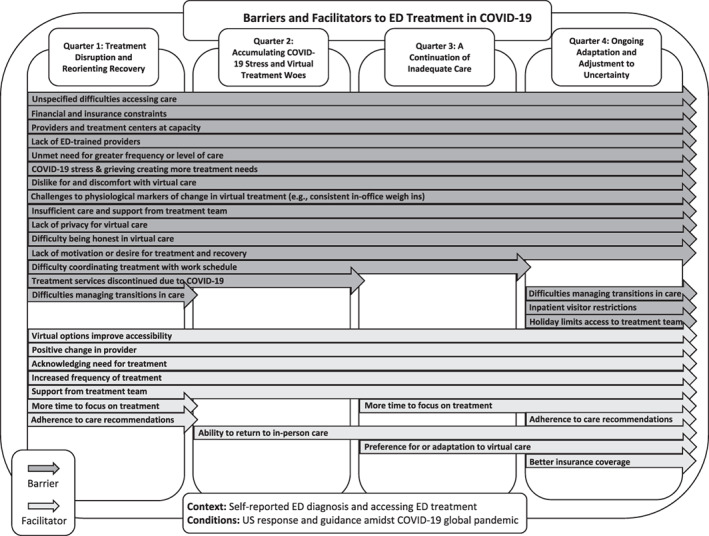
Barriers and facilitators to ED treatment in COVID‐19
3.1. Quarter 1: Treatment disruption and reorienting recovery
The first quarter was marked by several barriers to effective treatment related to widespread stay‐at‐home guidance, including lack of face‐to‐face contact, inconsistent internet access, and difficulties navigating insurance coverage. Though idiosyncratic in nature, some participants reported having positive experiences at this time, including increased time to focus on treatment and increased accessibility of telehealth. Still, participants faced numerous challenges regarding their ED treatment. One participant described their experience in this manner:
My need for eating disorder [treatment] has increased as my symptoms have increased during this time. On the other hand, my income has significantly decreased as my hours at work have been severely reduced. This puts me in a position where I cannot afford to resume treatment for my symptoms even with my insurance.
Participants also struggled with the effects of job loss and pandemic‐related economic and occupational shifts. As individuals shifted to remote work, reduced hours, and/or faced unemployment, responses also described challenges navigating insurance coverage, highlighting the numerous barriers to accessing treatment during this time.
With the massive overhaul toward virtual delivery of ED treatment services because of the COVID‐19 pandemic, participants described numerous insufficiencies in care beyond just limited access. Identified challenges with virtual treatment included the lack of face‐to‐face contact with providers, difficulties maintaining recovery without the support of providers who could track physiological markers of change (e.g., in‐office weigh‐ins), changes in treatment providers due to shifts in insurance or treatment needs, and treatment centers and providers being at capacity. Additionally, many participants reported a preference for in‐person care and discomfort receiving care virtually, inconsistent internet access, and living conditions that were not conducive to their treatment and recovery (e.g., a lack of private space to complete appointments, difficulty being honest in virtual care).
Participants also described how the pandemic resulted in discontinuities in treatment. One participant explained:
My treatment team (therapist, dietitian, and eating disorder recovery coach) all discontinued services with me after the first week in May because I did not agree to go to a residential program (dual diagnosis for OCD and ED). I was too afraid to travel because of COVID. So, I am now doing recovery on my own and it is incredibly hard not to have any support at all.
With COVID cancellations and shifts to telehealth, a gap emerged between participants' need for greater frequency or level of care and the limited availability of adequate treatment services. Participant reports consistently highlighted this dilemma, detailing difficulties managing care transitions, insufficient support from treatment teams, and increased needs due to stressors and barriers brought on by the COVID‐19 pandemic.
Despite several challenges, there were some positive therapeutic and treatment experiences. With widespread stay‐at‐home guidelines and shifts to remote work, participants reported more time to focus on treatment and recognition that they needed more support. For example, one participant stated, “[I have] More time to focus on treatment and recovery without quite as much pressure to ‘get back on track’ with ‘normal’ life.” With this additional focus on treatment, participants also described a willingness to adhere to treatment recommendations that facilitated their recovery and improved their overall treatment experience. Still, others mentioned increased frequency of therapeutic sessions or level of care, positive changes in and support from treatment teams, and, for those with quality internet access, virtual options increased treatment accessibility. These positive experiences were inconsistent, however, and contrasted with the consistent barriers reported by participants throughout the quarter.
3.2. Quarter 2: Accumulating COVID‐19 stress and virtual treatment woes
Negative perceptions and experiences with ED treatment continued throughout quarter two, with participants reiterating many of the same barriers to treatment from quarter one including COVID‐related cancellations to treatment services, lack of motivation for recovery, and financial instability. There was an increase from quarter one in mentions of the insufficiencies of virtual care. Positive experiences remained idiosyncratic in nature throughout this quarter.
Participants continued to express stress surrounding the COVID‐19 pandemic. One participant described:
I've hit a point where the social distancing is playing a role in my mental health. I miss what was my previous normal and I feel grieving that has added another layer to the complicated onion that is ED treatment.
The accumulating grief from social distancing and lack of normal access to known supports due to the pandemic created challenges for participants; this inability to engage left participants feeling isolated and “desperately needing more support.” Additionally, participants identified numerous difficulties accessing treatment due to job loss, insurance changes, financial instability, employment‐related scheduling conflicts, a lack of ED specialists, and treatment centers and providers being at capacity. Simultaneously, they noted insufficiencies in their current care that hindered progress in recovery. Identified inadequacies in treatment included not feeling validated by therapists, lack of support when transitioning to a lower level of care, a preference for in‐person treatment, and limited accountability and structure often inherent in virtual care. Further, the absence of in‐person visits continued to present challenges to tracking markers of physiological change. For example, one participant stated:
It's been challenging not having someone monitor my weight and keep me on track, but I'm avoiding buying a scale and self‐weighing because I know I would obsess over it.
These emerging repercussions of lack of face‐to‐face care led to surges in participants expressing a need for more frequent and effective ED care. The challenges of surviving during COVID‐19 continued to accumulate leading participants to voice continuing concerns with virtual treatment and the lack of support available to them. Despite these challenges, some participants were able to access necessary care via new virtual options, transitioning to different providers, and increasing frequency of appointments. One participant described, “I am switching dietitians to someone I am hopefully more comfortable with,” and another mentioned, “I am currently in a virtual PHP program. It has been nice to have that added support but it isn't the same as in‐person.” It is unknown if participants continued to have more time to focus on treatment, as seen in all other quarters, or if participants experienced a loss in available time here, as this information was missing from quarter two. Additionally, some participants were able to return to in‐person care for the first time since the onset of the pandemic, a development which was positively perceived by many. Thus, even while participants shared myriad difficulties with treatment, they were still making efforts to identify treatment options that worked for them and remain focused on their recovery.
3.3. Quarter 3: A continuation of inadequate care
Participant responses during quarter three were very similar to those in quarter two, with continued statements of negative perceptions and experiences with treatment such as difficulties accessing treatment due to financial, employment, and insurance constraints, and insufficient virtual care given its challenges to privacy, honesty, and accountability. Positive experiences continued in the same context as previous quarters. As seen in previous quarters, participants indicated that their current treatment was inadequate. One participant summarizes their experience in this manner:
I need a higher level of care, but my treatment team is not able to offer me additional support until then. Treatment centers are full with waiting lists lasting weeks. I am afraid to go to a hospital for medical stabilization due to COVID‐19, hospitals at capacity, and short on staff.
This gap in treatment availability was a constant concern for participants throughout the course of this study. A lack of ED‐trained professionals, particularly in rural areas, combined with the high demand for care at this time left many participants without the support they needed. In the context of this absence of care, participants experienced surges in symptomatology and a lack of growth in recovery.
Moreover, as participants worked from home and some participants' children began virtual learning, home obligations emerged as a barrier to treatment due to scheduling issues and a lack of privacy with family at home. Relatedly, one participant reported “need[ing] a higher level of care” but being unwilling to “go with [their] 3 kids home doing school virtually.” Here, it is evident how COVID‐related changes not only affected access to care but presented challenges to ED recovery as well.
Finally, though participants continued to express a desire for in‐person care and ongoing dissatisfaction surrounding virtual treatment, increasing reports on positive experiences with virtual treatment were also received. For the first time, participants mentioned a preference for or adaption to virtual care, describing “enjoy[ing] the online treatment” and “having some success in online EMDR therapy.” Relatedly, quarter three was first to indicate some initial signs of participants beginning to feel optimistic for their mental health again. One participant mentioned that they are “in partial treatment … and [they] are doing better” and another remarked, “I have had some significant breakthroughs in therapy.” These reports indicate a turning point for participants as they began to experience improvements in care.
3.4. Quarter 4: Ongoing adaptation and adjustment to uncertainty
Quarter four ushered in continued statements on the barriers and negative perceptions of ED treatment. Consistent with previous quarters, needing a higher level of care or more support from treatment teams was mentioned in multiple capacities, including a desire for more appointments, more intensive treatment, and more support during transitions in levels of care or between providers. Unlike previous quarters, however, participants identified COVID‐19 visitor restrictions in residential care facilities as a barrier to accessing a higher level of care. For example, one participant left inpatient treatment early due to homesickness while another was hesitant to attend inpatient treatment because they “[did]n't want to leave [their] family with no visitation allowed at residential.” Further, observed federal holidays were also a unique barrier to treatment during this quarter. Participants described not meeting with their therapist and struggling more with ED behaviors due to the holidays.
What most differentiated quarter four from the previous quarters, however, was the first instance of notably positive perceptions and experiences with ED treatment and recovery. Along with continued reports of having more time to focus on treatment, willingness to comply with treatment recommendations, and ability to access increased frequency or improved quality of care, more participants reported managing their care well and feeling satisfied with the treatment they were receiving, with some even describing a growing preference for virtual care. One participant explained that virtual treatment “reduced stress and increased accessibility” and another said, “I have a very strong team with an RD [registered dietitian] that specializes in eating disorders, a PCP that knows me well and a therapist that is super helpful.” Additionally, after a year of challenges navigating insurance coverage in relation to ED treatment, changes to insurance policies that increased telehealth coverage were mentioned as facilitators to accessing necessary ED care. While many still struggled to access the treatment they needed, these insurance changes expanded opportunities for some participants to access more frequent and higher levels of care.
Finally, it was noteworthy that participants began to feel a sense of hope, with one participant saying, “I have seen my therapist weekly and I have been feeling hopeful. It feels like this pandemic won't really be forever.”
4. DISCUSSION
In this study, participants with past or present EDs described their perceptions and experiences with treatment in the context of COVID‐19 over four quarters, noting experiences with treatment disruption, accumulating COVID‐19 stress and virtual treatment challenges, inadequate care, and ongoing adaptation and adjustment to uncertainty. Indeed, each quarter brought reminders of the continued challenges COVID‐19 was posing to individuals with past or present EDs. Though participants reported adjusting to the new realities of virtual care by the end of the first year of the pandemic, experiences with virtual treatment challenges persisted. Clearly, COVID‐19 has left an undeniable mark on the landscape of treatment for ED; understanding the nature and nuances of these challenges remains critical.
Aligning with previous research, participants in this study consistently reported challenges with treatment during the first year of the COVID‐19 pandemic. For example, in one study comprised of young adults and adolescents reporting ED, nearly 47% of participants had to discontinue some aspect of their treatment (Spigel et al., 2021). Further, among a sample of participants with anorexia nervosa, the percentage of those receiving in‐person outpatient psychotherapy decreased from 88% to 55%, having weights obtained by a clinician from nearly 50% to 31% (Schlegl et al., 2020). The results of this study provide additional context on the experience of these changes, with participants describing challenges accessing treatment providers and/or adjusting to the new requirements of virtual care. Certainly, the transition to virtual care brought conflicting reviews from patients (Weissman & Hay, 2022), with participants expressing more aversion in the beginning of the pandemic and moving towards adjustment as the realities of living with COVID‐19 continued.
Though participants in this study expressed problems with adjusting to virtual treatment, by the end of the first‐year participants began to express more positive experiences. This finding is promising given the co‐occurring limitations and benefits of telehealth. As noted in prior research, as online treatment options expanded for the safety of patients and providers, gaps in technology accessibility were also apparent (Frayn et al., 2021; Weissman et al., 2020). Furthermore, though telehealth brought greater access and improved convenience and safety to some, challenges have been reported with a lower sense of interpersonal connection, and increased body surveillance (Brothwood et al., 2021; Brownstone et al., 2022; Frayn et al., 2021). In fact, in a recent qualitative study understanding the experiences of cisgender folks with self‐reported disordered eating during COVID‐19, participants identifying as BIPOC, and in larger bodies, were more likely to report challenges with body surveillance and vulnerability in virtual settings compared with White, medium body, straight participants (Brownstone et al., 2022). However, despite these challenges, there is support that virtual treatment can yield positive outcomes over time (Raykos et al., 2021; Steiger et al., 2022), similar to what has been reported in this study.
4.1. Implications for clinical practice
The COVID‐19 pandemic has provided significant lessons to guide the future of ED treatment. Certainly, providers will need to be mindful of the exacerbated ED symptoms that may be experienced because of COVID‐19. Of note, though preference for in‐person treatment has been reported (Lewis et al., 2021; Weissman et al., 2020), providers may need to be aware of clients' increasing comfort with telehealth. In fact, maintaining a telehealth option may be particularly useful for clients who feel stigma around accessing in‐person ED treatment, do not have the flexibility to attend in‐person sessions, and/or may prefer to receive treatment in a familiar setting where they may feel more comfortable. However, when offering clinical services via telehealth, providers may need to be mindful of the challenges of not being able to witness clients' body language, limited privacy, particularly if a client may be at home, logistical/technical concerns, and the perception that teletherapy is impersonal, compared with in‐person treatment. Furthermore, providers may also need to recognize the increased possibility of weight manipulation.
The implications of this study also highlight the challenges COVID‐19 posed to those in recovery. Indeed, participants noted experiences of disruption throughout the first year, often influenced by cancellations in treatment, shifts to telehealth, lack of a private space to complete appointments, and lack of motivation. Previous recommendations have highlighted the potential benefit of using smartphone apps that promote recovery‐focused tools for self‐monitoring and positive coping skills, as well as use of group support and/or meal support offered virtually (Cooper et al., 2022). Extending these offerings in clinical settings may further augment existing treatment structures, and work to mitigate the challenges COVID‐19 has posed to recovery.
Finally, although the current study assessed the impact of COVID‐19 on treatment experiences among those with eating disorders, it is important to note that many of the issues described by participants are not unique to the pandemic. A lack of eating disorder specialist providers, long wait times, and difficulties navigating insurance have been longstanding issues for individuals seeking care for an eating disorder. Our data are not granular enough to determine any causal and/or temporal relationships; however, one reasonable hypothesis is that the issues regarding access to care that existed prior to the pandemic were exacerbated by pandemic‐related circumstances. Indeed, in many ways, the pandemic has shone a light on longstanding challenges in the American system of mental healthcare.
4.2. Limitations
We acknowledge several limitations that may affect the interpretation of this research. First, the sample was comprised of predominately White and cisgender women; thus, the results of this study do not reflect the experiences of other racial and ethnic groups, and of those who have a different gender identity. As such, future research should examine experiences of those with minoritized identities who were not accessed via recruitment for this study. Additionally, most participants in this study reported a previous diagnosis of anorexia nervosa; this may increase bias in reporting of participant experiences. Also, though this study was able to query participants at multiple time points, we were unable to match responses to specific participants and track individual‐level change at all four quarters due to missing data. Further, due to the experience of significant attrition, it is unclear whether these results fully describe the experience of the full sample, or only those who remained. Possible reasons for this attrition may be that participants may have found it burdensome to complete a survey monthly. Additionally, participants may have adjusted to managing their ED symptoms after time and may not have been experiencing the same distress and fear as they were at the beginning of the pandemic. It is also possible that those with the most severe experiences in COVID‐19 and with treatment chose not to continue completing the surveys. Although we anticipated a one‐year follow‐up to be an adequate duration, in retrospect, with pandemic‐related disruptions continuing to occur, a longer period of observation would have been desirable.
5. CONCLUSION
In summary, the first year of the global COVID‐19 pandemic significantly challenged individuals with past or present EDs in the U.S. Rich qualitative information provided greater insight into the experience of participants, isolated areas of change over time, and underscored the importance of continuing to evolve virtual care in a way that adequately replaces in‐person care for situations in which face‐to‐face options are untenable.
AUTHOR CONTRIBUTIONS
Rachel Goode: Conceptualization; supervision; writing – original draft. Sarah Godoy: Data curation; formal analysis; supervision; writing – original draft; writing – review and editing. Hannah Wolfe: Formal analysis; writing – original draft; writing – review and editing. Katie Olson: Formal analysis; writing – original draft; writing – review and editing. Bridgette Agbozo: Formal analysis; writing – original draft; writing – review and editing. Abigail Mueller: Formal analysis; writing – original draft. Taylor Noem: Formal analysis; writing – original draft. Hannah Malian: Writing – review and editing. Christine Marie Peat: Conceptualization; writing – review and editing. Hunna J Watson: Data curation; writing – review and editing. Laura M. Thornton: Data curation; writing – review and editing. Rebecca Gwira: Writing – original draft. Cynthia Marie Bulik: Conceptualization; writing – original draft.
CONFLICT OF INTEREST
CM Peat reports: Equip Health (Clinical Advisory Board), CM Bulik reports: Shire (grant recipient, Scientific Advisory Board member); Lundbeckfonden (grant recipient); Pearson (author, royalty recipient); Equip Health Inc. (Clinical Advisory Board).
ETHICS STATEMENT
Ethical permission was granted by the University of North Carolina Biomedical Institutional Review Board for the United States (IRB number 20‐0964). Participants signed online consent forms.
ACKNOWLEDGMENTS
Dr. Bulik acknowledges support from National Institute of Mental Health (R01MH120170; R01MH124871; R01MH119084; R01MH118278); Brain and Behavior Research Foundation Distinguished Investigator Grant; Swedish Research Council (Vetenskapsrådet, award: 538‐2013‐8864); Lundbeckfonden (Grant no. R276‐2018‐4581). Dr. Peat acknowledges support from HRSA (1‐D40‐HP45688) and AHRQ (EPC VI RFTO #45). Dr. Goode acknowledges support from NIDDK (K23DK129832). Dr. Goode, Peat, and Bulik acknowledge support from the Substance Abuse and Mental Health Administration (H79 SM081924).
Goode, R. W. , Godoy, S. M. , Wolfe, H. , Olson, K. , Agbozo, B. , Mueller, A. , Noem, T. , Malian, H. , Peat, C. M. , Watson, H. , Thornton, L. M. , Gwira, R. , & Bulik, C. M. (2023). Perceptions and experiences with eating disorder treatment in the first year of COVID‐19: A longitudinal qualitative analysis. International Journal of Eating Disorders, 56(1), 247–256. 10.1002/eat.23888
Action Editor: Ruth Striegel Weissman
Funding information Lundbeckfonden, Grant/Award Number: R276‐2018‐4581; National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: K23129832; National Institute of Mental Health, Grant/Award Numbers: R01MH118278, R01MH119084, R01MH124871; Substance Abuse and Mental Health Services Administration, Grant/Award Number: H79SM081924; Vetenskapsrådet, Grant/Award Number: 538‐2013‐8864
DATA AVAILABILITY STATEMENT
The data analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- Banthin, J. , Simpson, M. , Buettgens, M. , Blumberg, L. J. , & Wang, R. (2020). Changes in health insurance coverage due to the COVID‐19 recession: Preliminary estimates using microsimulation (pp. 1–9). Urban Institute. [Google Scholar]
- Barney, A. , Buckelew, S. , Mesheriakova, V. , & Raymond‐Flesch, M. (2020). The COVID‐19 pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. The Journal of Adolescent Health, 67(2), 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz, S. A. , & Basu, S. (2021). Unemployment insurance, health‐related social needs, health care access, and mental health during the COVID‐19 pandemic. JAMA Internal Medicine, 181(5), 699–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birgegard, A. , Abbaspour, A. , Borg, S. , Clinton, D. , Mantilla, E. F. , Savva, A. , Termorshuizen, J. D. , & Bulik, C. M. (2021). Longitudinal experiences and impact of the COVID‐19 pandemic among people with past or current eating disorders in Sweden. Eating Disorders, 30(6), 602–617. [DOI] [PubMed] [Google Scholar]
- Brothwood, P. L. , Baudinet, J. , Stewart, C. S. , & Simic, M. (2021). Moving online: Young people and parents' experiences of adolescent eating disorder day programme treatment during the COVID‐19 pandemic. Journal of Eating Disorders, 9(1), 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. , Opitz, M. C. , Peebles, A. I. , Sharpe, H. , Duffy, F. , & Newman, E. (2021). A qualitative exploration of the impact of COVID‐19 on individuals with eating disorders in the UK. Appetite, 156, 104977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownstone, L. M. , Greene, A. K. , Kelly, D. A. , Maloul, E. K. , Norling, H. N. , Rockholm, R. H. , & Izaguirre, C. M. (2022). Are people thinking I'm a vector…because I'm fat?: Cisgender experiences of body, eating, and identity during COVID‐19. Body Image, 40, 256–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calman, L. , Brunton, L. , & Molassiotis, A. (2013. Dec). Developing longitudinal qualitative designs: Lessons learned and recommendations for health services research. BMC Medical Research Methodology, 13(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellini, G. , Cassioli, E. , Rossi, E. , Innocenti, M. , Gironi, V. , Sanfilippo, G. , Felciai, F. , Monteleone, A. M. , & Ricca, V. (2020). The impact of COVID‐19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. The International Journal of Eating Disorders, 53(11), 1855–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, M. , Reilly, E. E. , Siegel, J. A. , Coniglio, K. , Sadeh‐Sharvit, S. , Pisetsky, E. M. , & Anderson, L. M. (2022). Eating disorders during the COVID‐19 pandemic and quarantine: An overview of risks and recommendations for treatment and early intervention. Eating Disorders, 30(1), 54–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devoe, J. D. , Han, A. , Anderson, A. , Katzman, D. K. , Patten, S. B. , Soumbasis, A. , Flanagan, J. , Paslakis, G. , Vyver, E. , Marcoux, G. , & Dimitropoulos, G. (2022). The impact of the COVID‐19 pandemic on eating disorders: A systematic review. The International Journal of Eating Disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede, L. E. , Ruggiero, K. J. , & Frueh, B. C. (2020). Ensuring mental health access for vulnerable populations in COVID era. Journal of Psychiatric Research, 129, 147–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayn, M. , Fojtu, C. , & Juarascio, A. (2021). COVID‐19 and binge eating: Patient perceptions of eating disorder symptoms, tele‐therapy, and treatment implications. Current Psychology, 40(12), 6249–6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode, R. W. , Malian, H. , Samuel‐Hodge, C. , Noem, T. , Coan, D. , Takgbajouah, M. , Bahena, L. , & Bulik, C. M. (2022). The impact of COVID‐19 on black women who binge‐eat: A qualitative study. Eating and Weight Disorders, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths, S. , Rossell, S. L. , Mitchison, D. , Murray, S. B. , & Mond, J. M. (2018). Pathways into treatment for eating disorders: A quantitative examination of treatment barriers and treatment attitudes. Eating Disorders, 26(6), 556–574. [DOI] [PubMed] [Google Scholar]
- Johnson, J. L. , Adkins, D. , & Chauvin, S. (2020). A review of the quality indicators of rigor in qualitative research. American Journal of Pharmaceutical Education, 84(1), 7120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, Y. D. , Elran‐Barak, R. , Grundman‐Shem Tov, R. , & Zubery, E. (2021). The abrupt transition from face‐to‐face to online treatment for eating disorders: A pilot examination of patients' perspectives during the COVID‐19 lockdown. Journal of Eating Disorders, 9(1), 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson, B. E. , Bohon, C. , & Lock, J. (2020). Family‐based treatment via videoconference: Clinical recommendations for treatment providers during COVID‐19 and beyond. The International Journal of Eating Disorders, 53(7), 1142–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow, S. L. (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52(2), 250–260. [Google Scholar]
- Murphy, R. , Calugi, S. , Cooper, Z. , & Dalle, G. R. (2020). Challenges and opportunities for enhanced cognitive behaviour therapy (CBT‐E) in light of COVID‐19. Cognitive Behaviour Therapy, 13, e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett, D. K. (2016). Qualitative methods in social work research. SAGE Publications. [Google Scholar]
- Patton, M. Q. (2002). Qualitative research & evaluation methods. SAGE Publications. [Google Scholar]
- Raykos, B. C. , Erceg‐Hurn, D. M. , Hill, J. , Campbell, B. N. C. , & McEvoy, P. M. (2021). Positive outcomes from integrating telehealth into routine clinical practice for eating disorders during COVID‐19. The International Journal of Eating Disorders, 54(9), 1689–1695. [DOI] [PubMed] [Google Scholar]
- Richardson, C. , Patton, M. , Phillips, S. , & Paslakis, G. (2020). The impact of the COVID‐19 pandemic on help‐seeking behaviors in individuals suffering from eating disorders and their caregivers. General Hospital Psychiatry, 67, 136–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , Linardon, J. , Courtet, P. , & Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. The International Journal of Eating Disorders, 53(7), 1166–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, H. J. , & Rubin, I. S. (2012). Qualitative interviewing: The art of hearing data (3rd ed.). Sage Publications. [Google Scholar]
- Saldaña, J. (2021). The coding manual for qualitative researchers (pp. 1–440). Arizona State University. [Google Scholar]
- Schlegl, S. , Maier, J. , Meule, A. , & Voderholzer, U. (2020). Eating disorders in times of the COVID‐19 pandemic‐results from an online survey of patients with anorexia nervosa. The International Journal of Eating Disorders, 53(11), 1791–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spigel, R. , Lin, J. A. , Milliren, C. E. , Freizinger, M. , Vitagliano, J. A. , Woods, E. R. , Forman, S. F. , & Richmond, T. K. (2021). Access to care and worsening eating disorder symptomatology in youth during the COVID‐19 pandemic. Journal of Eating Disorders, 9(1), 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger, H. , Booij, L. , Crescenzi, O. , Oliverio, S. , Singer, I. , Thaler, L. , St‐Hilaire, A. , & Israel, M. (2022). In‐person versus virtual therapy in outpatient eating‐disorder treatment: A COVID‐19 inspired study. The International Journal of Eating Disorders, 55(1), 145–150. [DOI] [PubMed] [Google Scholar]
- Termorshuizen, J. D. , Watson, H. J. , Thornton, L. M. , Borg, S. , Flatt, R. E. , MacDermod, C. M. , Harper, L. E. , van Furth, E. F. , Peat, C. M. , & Bulik, C. M. (2020). Early impact of COVID‐19 on individuals with self‐reported eating disorders: A survey of ~1,000 individuals in the United States and The Netherlands. The International Journal of Eating Disorders, 53(11), 1780–1790. [DOI] [PubMed] [Google Scholar]
- US Department of Labor . (2022). Unemployment insurance weekly claims (p. 9). DOL. [Google Scholar]
- Vuillier, L. , May, L. , Greville‐Harris, M. , Surman, R. , & Moseley, R. L. (2021). The impact of the COVID‐19 pandemic on individuals with eating disorders: The role of emotion regulation and exploration of online treatment experiences. Journal of Eating Disorders, 9(1), 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, R. S. , Bauer, S. , & Thomas, J. J. (2020). Access to evidence‐based care for eating disorders during the COVID‐19 crisis. The International Journal of Eating Disorders, 53(5), 369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, R. S. , & Hay, P. (2022). People's lived experience with an eating disorder during the COVID‐19 pandemic: A joint virtual issue of research published in leading eating disorder journals. The International Journal of Eating Disorders, 55(2), 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed during the current study are available from the corresponding author on reasonable request.


