Abstract
COVID‐19 pandemic presents an unheralded opportunity to better understand trajectories of posttraumatic stress disorder (PTSD) symptoms across a prolonged period of social disruption and stress. We tracked PTSD symptoms among trauma‐exposed individuals in the United States and sought to identify population‐based variability in PTSD symptom trajectories and understand what, if any, early pandemic experiences predicted membership in one trajectory versus others. As part of a longitudinal study of U.S. residents during the pandemic, participants who reported at least one potentially traumatic experience in their lifetime (N = 1,206) at Wave 1 (April 2020) were included in the current study. PTSD symptoms were assessed using the PCL‐5 at four time points extending to July 2021. Latent growth mixture modeling was used to identify heterogeneous symptom trajectories. Trajectory membership was regressed on experiences from the early stage of the pandemic as measured using the Epidemic‐Pandemic Impacts Inventory in a model that controlled for variables with documented associations to PTSD trajectories, including age, sex, income, and trauma history. Four trajectories were identified, categorized as resilient (73.0%), recurring (13.3%), recovering (8.3%), and chronic (5.5%). Emotional and physical health problems and positive changes associated with the early phase of the pandemic were each significant predictors of trajectory membership over and above all other variables in the model. Predictors primarily differentiated the resilient trajectory from each of the other three trajectories. Distinct PTSD symptom trajectories during the COVID‐19 pandemic suggest a need for targeted efforts to help individuals at most risk for ongoing distress.
The coronavirus disease 2019 (COVID‐19) pandemic and social turmoil of 2020 had wide‐ranging effects on the overall well‐being of the U.S. population. Economic repercussions, social isolation, and widespread uncertainties contributed to a range of emotional and psychological responses, including fear, anxiety, traumatic stress, and depression (Cénat et al., 2021; McGinty et al., 2020; Nochaiwong et al., 2021). Individuals with preexisting mental health concerns, such as posttraumatic stress disorder (PTSD), were found to be disproportionately at risk of experiencing harm related to the COVID‐19 pandemic (Asmundson et al., 2020; Pinkham et al., 2020).
Much attention has been drawn to the pathological sequelae of trauma, such as PTSD, depression, and substance misuse (Hien et al., 2021), yet research has consistently shown that following traumatic adversity, most individuals maintain or regain a normative level of functioning (Bonanno, 2004, 2005). Examining this heterogeneity in population responses is critical for ensuring responsive prevention, treatment, and recovery supports that adequately address trauma‐related dysfunction. Research that produces summary data (i.e., does not consider the relative vulnerability and resilience of subgroups) is unable to sensitively guide policy and implementation decisions, such as where and how limited resources should be deployed and to what target subpopulations. Complementing variable‐centered analyses, person‐centered methods that assume the existence of multiple, meaningfully different subpopulations can facilitate answering these questions. In the wake of traumatic events, person‐centered analyses can quantify the number and prevalence of subgroups, characterize each distinct group based on symptom severity and longitudinal trajectory, and assist in identifying factors that are associated with membership in each group.
To date, research (Foster et al., 2019; Lowe et al., 2021; van Zuiden et al., 2022) converges upon a set of longitudinal posttrauma trajectories, typically ranging in number from three to five. These include variations on four typologies: a chronically elevated state of distress, a resilient response where minimal distress is noted, a delayed stress response, and a recovery course of progressive improvement (Galatzer‐Levy et al., 2018). In longitudinal modeling studies conducted prior to COVID‐19, female sex assigned at birth, younger age, lower income level, and lower educational attainment were associated with a higher likelihood of membership in a posttrauma trajectory characterized by higher levels of distress (Bonanno et al., 2007; Lowe et al., 2021). These associations have been understood as functions of relative resource scarcity (Hobfoll, 1989, 2002), such as limited access to environmental and social resources that may buffer individuals from harm related to overwhelming stress.
The COVID‐19 pandemic has been described as an extreme event—a population‐wide, chronic, and potentially traumatic stressor. PTSD‐related distress during the COVID‐19 pandemic has resembled prior trajectory models during a brief (i.e., 6‐week) observation period (Lin et al., 2021) and across 3 months (McPherson et al., 2021). The five distinct COVID‐related PTSD and anxiety–depression trajectories found across a 4‐month period in a nationally representative sample of U.K. residents (Shevlin, Butter, McBride, Murphy, Gibson‐Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, & Bentall, 2021), and extended to 1‐year follow‐up (Shevlin, Butter, McBride, Murphy, Gibson‐Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, Vallieres, & Bentall, 2021) echo previously observed trajectories of resilience, improvement, and deterioration described in shorter investigations. Similarly, studies of populations that faced specific, concentrated doses of traumatic stress before or during the pandemic (i.e., military veterans and health care workers) have also revealed multiple, distinct PTSD symptom profiles during the pandemic that mirror the sustaining, improving, and worsening patterns observed in earlier work (Dufour et al., 2021; Kalaitzaki & Rovithis 2021; Marvaldi et al., 2021; Solomon et al., 2021; Zhou & Wu, 2022). Data on the year‐plus time frame and chronicity of the COVID‐19 pandemic, as well as the longitudinal responses among the broader population of individuals with prior trauma exposure, are now necessary.
The current study set out to answer two questions about the progression of PTSD symptoms in the U.S. population during the COVID‐19 pandemic. First, we aimed to model the 16‐month time course of PTSD symptoms, as assessed using the criteria in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM‐5; American Psychiatric Association [APA], 2013), in a sample of U.S. residents, testing the hypothesis that population heterogeneity would reveal significantly different PTSD symptom trajectories rather than a single mean trajectory. Second, we assessed whether early pandemic experiences were associated with trajectory membership. Based on variously replicated findings of PTSD symptom trajectories (Armenta et al., 2019; Bonanno et al., 2012; Cheng et al., 2019; Galatzer‐Levy et al., 2018; Solomon et al., 2012), we hypothesized that the identified trajectories would characterize longitudinal severity in our sample along the lines of minimal, chronic, improving, and deteriorating PTSD symptoms. In our examination of associations between early pandemic experiences and trajectories, we controlled for key variables that have demonstrated associations with PTSD trajectories in studies conducted prior to COVID‐19, including female sex assigned at birth, younger age, lower income level, and lower educational attainment (Bonanno et al., 2007; Lowe et al., 2021).
METHOD
Participants and procedure
The COVID‐Dynamic project is a longitudinal, internet‐based study developed to assess the psychosocial impacts of the COVID‐19 pandemic among a sample of U.S. residents. Details about participant recruitment, enrollment criteria, assessment schedule, and testing procedures are available elsewhere (Rusch et al., in press). This study was deemed exempt by the California Institute of Technology Institutional Review Board.
This study employed data collected during four waves that took place between April 4, 2020, and July 24, 2021. The inclusion criteria for this study were (a) participation in the baseline Life Events Checklist for DSM‐5 (LEC‐5; Weathers, Blake, et al., 2013) and PTSD Checklist for DSM‐5 (PCL‐5; Weathers, Litz, et al., 2013) assessments on April 11, 2020; (b) reported lifetime experience of at least one potentially traumatic event (PTE); and (c) failure of no more than one attention check in at least half of their included waves. Meeting the DSM‐5 PTSD diagnostic criteria was not required for study participation. From the original sample of 1,797 individuals, 1,498 completed the baseline PTSD assessment, 1,222 of these participants reported having experienced at least one lifetime PTE, and 1,206 (98.7%) passed the attention check criteria. All eligible participants (N = 1,206) were included in the analyses; missing data patterns and estimation methods are reported in the data analysis section. Sample characteristics are presented in Table 1.
TABLE 1.
Descriptive statistics of the sample
| Variable | n | % | M | SD |
|---|---|---|---|---|
| Female sex assigned at birth | 628 | 52.1 | ||
| Age (years) | 39.36 | 14.09 | ||
| Hispanic or Latino ethnicity | 113 | 9.4 | ||
| Race | ||||
| White | 909 | 75.4 | ||
| Asian | 107 | 8.9 | ||
| Black or African American | 95 | 7.9 | ||
| Multiracial | 58 | 4.8 | ||
| Other or not reported | 27 | 2.2 | ||
| American Indian/Alaska Native | 8 | 0.2 | ||
| Native Hawaiian or Other Pacific Islander | 2 | 0.2 | ||
| Previous week income (USD) | ||||
| < $250 | 509 | 42.2 | ||
| $250–$499 | 195 | 16.2 | ||
| $500–$999 | 224 | 18.6 | ||
| $1,000–$1,499 | 147 | 12.2 | ||
| $1,500–$2,999 | 101 | 8.4 | ||
| ≥ $3,000 | 30 | 2.5 | ||
| Educational attainment | ||||
| Less than high school | 10 | 0.8 | ||
| High school/trade school | 134 | 10.3 | ||
| Some college | 313 | 26.0 | ||
| Associate's degree | 133 | 11.9 | ||
| Bachelor's degree | 387 | 32.1 | ||
| Some graduate school | 45 | 3.7 | ||
| Master's degree | 146 | 12.1 | ||
| Doctoral/professional degree | 37 | 3.1 | ||
| Trauma exposure b | ||||
| Transportation accident | 687 | 47.9 | ||
| Natural disaster | 620 | 51.4 | ||
| Other very stressful event or experience | 569 | 47.2 | ||
| Other unwanted/ uncomfortable sexual experience | 460 | 38.1 | ||
| Physical assault | 408 | 33.8 | ||
| Sexual assault | 228 | 18.9 | ||
| Other serious accident | 213 | 17.7 | ||
| Life‐threatening illness or injury | 176 | 14.6 | ||
| Fire/explosion | 152 | 12.6 | ||
| Assault with a weapon | 115 | 9.5 | ||
| Toxic substance exposure | 84 | 7.0 | ||
| Severe human suffering | 63 | 5.2 | ||
| Captivity | 31 | 2.6 | ||
| Serious injury/harm/death you caused to other(s) | 25 | 2.1 | ||
| Combat or war zone exposure | 21 | 1.7 | ||
| Sudden accidental death of a loved one | 21 | 1.7 | ||
| Sudden violent death of a loved one | 12 | 1.0 | ||
| Cumulative trauma types experienced | 3.22 | 2.21 | ||
| Early pandemic impact, by domain c | ||||
| Work/employment | 1.39 | 1.41 | ||
| Home life | 1.22 | 1.65 | ||
| Social/isolation | 1.09 | 0.88 | ||
| Physical/mental health | 3.84 | 2.32 | ||
| Positive change | 0.94 | 0.87 | ||
| Infection‐related items | 0.23 | 0.74 |
Note: N = 1,206.
Range: 18–83 years.
Endorsed as “happened to me” on the Life Events Checklist.
Sum score comprised of endorsed items (“yes” for the respondent or someone in their household) on the Epidemic–Pandemic Impacts Inventory
The study's prespecified aims, hypotheses, and analysis plan can be found within the COVID‐Dynamic Project in the Open Science Foundation repository (https://osf.io/phwf2/), and links to the data and analysis code are provided in the Supplementary Materials. To enhance transparency and reproducibility, we used the guidelines for reporting on latent trajectory studies (van de Schoot et al., 2017). Supplementary Table S1 contains the 21‐item checklist along with a reference to the section of the article or Supplementary Material where that item is located.
Measures
Lifetime trauma exposure
At baseline, participants completed the LEC‐5 (Weathers, Blake, et al., 2013) is used to assess self‐reported lifetime exposure to 17 PTEs . For each event type, participants report if they ever experienced the PTE and their level of exposure (i.e., “happened to me,” “witnessed it,” “learned about it,” “part of my job,” “not sure,” and “doesn't apply”). We summed all endorsed PTEs (i.e. rated as “happened to me”) to create a sum of cumulative trauma types experienced.
PTSD symptoms
The PCL‐5 (Weathers, Litz, et al., 2013) is a self‐report questionnaire that is used to assess the frequency and severity of 20 DSM‐5 PTSD symptoms during the past month. The measure has shown strong internal consistency, test–retest reliability, and convergent and discriminant validity (Belvins et al. 2015). The PCL‐5 was administered as part of the COVID‐Dynamic testing waves as included in parent‐study surveys that were distributed on April 11, 2020 (baseline); May 9, 2020; September 19, 2020; and July 24, 2021. In the trajectory analysis, these four time points are coded in weeks relative to baseline (i.e., Week 0, Week 4, Week 23, and Week 67). The mean duration, in weeks, between baseline and each subsequent time point was 4.03 (SD = 0.08) for Week 4, 23.06 (SD = 0.09) for Week 23, and 67.10 (SD = 0.14) for Week 67. Demographic information was acquired in the week prior to the baseline assessment of the current study.
Pandemic impact
The Epidemic–Pandemic Impacts Inventory (EPII; Grasso et al., 2020) is a 92‐item inventory developed by experts spanning the fields of psychology, social work, pediatrics, medicine, and anthropology (Grasso et al., 2020). Participants were asked to rate whether each pandemic‐related experience had happened to them or someone in their home. Initial support for the measure's construct validity has been demonstrated by the predictive association between distinct EPII profiles and psychosocial risk (Grasso et al., 2021). Summary results were generated by selecting the items that demonstrated bivariate associations with stress in Grasso et al. (2020), grouping items to the domains identified by Grasso et al. (2021), and creating a sum score comprising endorsed items (i.e., “yes” answer for a respondent or someone in their household) for each of the five domains: work/employment (seven items), home life (13 items), social life/isolation (five items), emotional/physical health and infection (15 items), and positive change (three items).
Demographic predictors
Four demographic predictors, measured the week before the baseline assessment, were also included in this analysis: sex at birth, age, income level in the week prior to the baseline assessment (coded as 1–6: 1 = with less than $250, 2 = $250–$499, 3 = $500–$999, 4 = $1,000–$1,499, 5 = $1,500–$2,999, 6 = $3,000 or more), and educational attainment (coded as 1–8: 1 = did not complete high school, 2 = high school or trade school, 3 = some college, 4 = associate's degree, 5 = bachelor's degree, 6 = some graduate education, 7 = master's degree, 8 = PhD or professional degree).
Data analysis
Latent growth mixture modeling (LGMM) was used to test the hypothesis that multiple heterogeneous trajectories would characterize the course of PTSD symptom severity in the sample better than a single mean trajectory. In this approach, intercepts and slopes representing initial severity and change across the assessment phase, respectively, are estimated in models with varying numbers of latent trajectories. Trajectories can be modeled with random intercepts and slopes (i.e., quadratic and/or linear) or restricted to random intercepts only or fixed effects only (i.e., latent class growth analysis), which can facilitate model convergence. We examined LGMMs, with random intercepts and slopes, with one to six trajectories and selected a final model based on sample size–adjusted Bayesian information criteria (ssaBIC), for which lower values indicate better fit; entropy, which reflects classification accuracy, where values closer to 1 indicate better fit; and the Lo–Mendell–Rubin (LMR) likelihood ratio test, with lower values indicating better fit (Jung & Wickrama, 2008). Models that showed improved fit with an additional trajectory that included a low proportion of participants (i.e., less than 5%) were rejected in favor of a more parsimonious solution (Jung & Wickrama, 2008). LGMM analyses were conducted in R with the lcmm package (Version 1.9.4). The variance–covariance matrix was constrained across trajectories to facilitate model convergence. For the multiclass models, gridSearch, with 100 repetitions and a maximum of 100 iterations in the optimization algorithm, was used to generate random starting values using information from the single‐trajectory model. Complete information about the number of random start values and final iterations included is included in the analysis outputs for each model (see Supplementary Materials).
LGMM analyses were conducted with maximum likelihood estimation, which can accommodate participants with data assumed to be missing at random (Asendorpf et al., 2014). Therefore, all eligible participants (N = 1,206) were included in the estimation of PTSD trajectories even if they had missing data from some of the collection waves. Average PCL‐5 scores were 18.17 (SD = 17.13, n = 1,206, 0.0% missing) at Week 0, 14.60 (SD = 15.31, n = 1,002, 16.9% missing) at Week 4, 11.28 (SD = 14.88, n = 734, 39.1% missing) at Week 23, and 10.58 (SD = 13.81, n = 519, 57.0% missing) at Week 67. A nonmonotonic missing data pattern was observed, and only a minority of participants (12.9%) did not complete any assessment after baseline. Baseline PCL‐5 scores did not differ between participants with missing data at Week 4 and those who completed the Week 4 assessment, Week 4 ΔM = 2.69, 95% confidence interval (CI) [−0.16, 5.54], p = .064; however, baseline PCL‐5 scores were higher among participants with missing data at subsequent assessments: Week 23 ΔM = 3.57, 95% CI [1.57, 5.57], p < .001; Week 67 ΔM = 4.76, 95% CI [2.85, 6.67], p < .001. The maximum likelihood estimation methods used in LGMM have been recommended as an effective approach to reducing bias associated with this type of systematic attrition (Aspendorf et al., 2014; Graham, 2009).
To examine predictors of trajectory membership, we used the bias‐adjusted three‐step approach (Clark & Muthen, 2016) implemented in a weighted multinomial logistic regression analysis with the nnet package (Version 7.3‐14; Ripley et al., 2016). For each participant, the LGMM analysis provided a posterior probability of membership in each latent trajectory. For the regression analysis, each participant was assigned to their most probable trajectory, which served as the dependent variable. To account for the uncertainty around trajectory membership, the posterior probabilities of trajectory membership were incorporated as weights in the regression model. The associations between predictors and specific trajectories are reported as adjusted odds ratios (aORs) and interpreted only for predictors that were significant in the multinomial logistic regression at the p < .05 level. All continuous variables were standardized such that all coefficients represent the change in the odds of trajectory membership per 1 standard deviation increase in the predictor.
RESULTS
PTSD trajectory analysis
Supplementary Table S2 shows the fit indices of the LGMM results with one through six trajectories for models that included either quadratic and linear slopes or linear slopes only. All linear and quadratic models converged and showed decreases in ssaBIC values and a significant LMR‐adjusted likelihood ratio test as the number of trajectories increased. Because these models converged, we did not examine more restricted models (e.g., LGMM with random intercepts and fixed slopes, LCGA with fixed intercepts and slopes). We focused on the quadratic models because they had slightly higher entropy and lower ssaBIC than the linear models. Although the four‐trajectory model had slightly lower entropy than the three‐trajectory model, the decrease in ssaBIC was larger than the decrease observed between the two‐ and two‐trajectory models (−119.58 vs. −103.52). The five‐trajectory model had the same entropy as the four‐trajectory model, with an additional trajectory that included only 30 participants (i.e., 2.4% of the sample). However, the five‐trajectory model showed a diminished gain in model fit (i.e., −59.51 change in ssaBIV relative to the four‐trajectory model; Masyn, 2013). Similar patterns were observed for Akaike information criterion and BIC values (see Supplementary Table S2). Therefore, we selected the four‐trajectory model.
Table 2 contains parameter estimates from the four‐trajectory model, including intercept (i.e., PCL‐5 total at Week 0) and linear slope (i.e., change in PCL‐5 total per week) as well as the proportion of participants included in each trajectory based on the highest posterior probability of trajectory assignment. Figure 1 (Panel A) illustrates the course of the trajectories across the assessment phase. The resilient trajectory was the most common (73.0%) and had the lowest estimated PCL‐5 score at baseline, a significant negative linear slope, and a significant positive quadratic slope, indicating a decreasing rate of reduction in PCL‐5 score across assessments. The recurring trajectory was the second most common (13.3%) and had an estimated PCL‐5 score that was within the diagnostic threshold at baseline, a significant negative linear slope, and a significant positive quadratic slope, as reflected in the initial decrease to below the diagnostic threshold followed by a rebound to above the diagnostic threshold in the final wave. The recovering trajectory was the third most common (8.3%) and had an estimated PCL‐5 score that was within the diagnostic threshold at baseline, like the recurring trajectory; however, unlike the recurring trajectory, the recovering trajectory had a significant positive linear slope and a significant negative quadratic slope, which were reflected in the initial increase to above the diagnostic threshold in PCL‐5 severity followed by a reduction to below the diagnostic threshold in the final wave. Finally, the chronic trajectory was the least common (5.5%) and reflected the highest PCL‐5 score at baseline, a significant negative linear slope, and a nonsignificant positive quadratic slope, as reflected by a minor decrease in severity, which remained above the diagnostic threshold throughout the assessment window. Figure 2 contains the observed values of individual participants within each model‐estimated trajectory. Trajectory plots for all the estimated LGMM models are available in the Supplementary Materials. Of note, the trajectory labels should be taken as descriptors of the estimated patterns and not as definitions of clinical phenotypes. For example, “chronic” was used to denote PTSD lasting more than 3 months in the DSM‐IV (APA, 2000) but was removed as a specifier in the DSM‐5 (APA, 2013). Here, we use the term chronic to convey clinically elevated levels of PTSD symptoms that were maintained throughout our study's 16‐month assessment window.
TABLE 2.
Parameter estimates from the four‐class latent growth mixture model
| Trajectory | Intercept | SE | Linear slope | SE | Quadratic slope | SE | n a | % |
|---|---|---|---|---|---|---|---|---|
| Resilient | 9.72*** | 0.41 | −0.28*** | 0.03 | 0.0032*** | 0.0004 | 880 | 73.0 |
| Recurring | 32.93*** | 1.52 | −1.41*** | 0.13 | 0.0214*** | 0.0018 | 160 | 13.3 |
| Recovering | 30.71*** | 1.38 | 0.55*** | 0.11 | −0.0110*** | 0.0016 | 100 | 8.3 |
| Chronic | 55.18*** | 1.63 | −0.29* | 0.14 | 0.0027 | 0.0020 | 66 | 5.5 |
Number of participants assigned to each trajectory based on the highest posterior probability of class membership.
* p < .05; *** p < .001.
FIGURE 1.
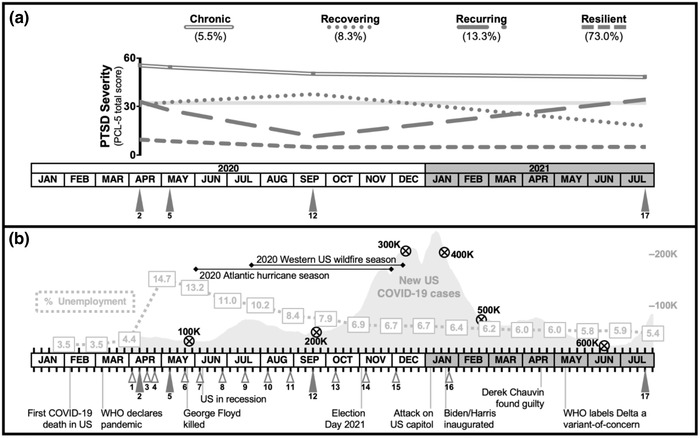
Longitudinal posttraumatic stress disorder (PTSD) trajectories from the (a) four‐trajectory model alongside a (b) timeline of U.S. unemployment rates, sociopolitical events, and COVID‐19 cases and related deaths, from January 2020 to July 2021
Note: In Panel A, the gray area between PTSD Checklist for DSM‐5 (PCL‐5) total scores of 31–33 represents the range of diagnostic thresholds that have been found in psychometric evaluations of the PCL‐5 (Morrison, et al., 2021; Bovin et al., 2016; Wortmann et al., 2016; Hoge et al., 2014). Timepoints 2, 5, 12, and 17 represent the four PTSD assessment periods.
FIGURE 2.
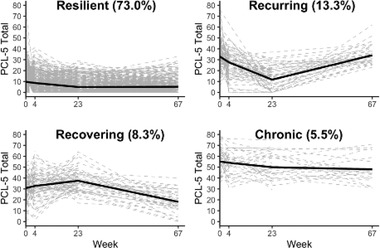
Estimated model trajectories and individual observed posttraumatic stress disorder (PTSD) trajectories
Note: Black solid lines represent the mean trajectory based on the estimated intercepts and slopes from the latent growth mixture modeling. Gray dashed lines represent individual participant trajectories based on data collected at 0, 4, 23, and 67 weeks, indicated on the x‐axis. PCL‐5 = PTSD Checklist for DSM‐5.
Predictors of trajectory membership
Table 3 shows results from the multinomial logistic regression in which trajectory membership was regressed on 10 predictors. Two of the five categories of pandemic experiences showed significant associations with trajectory membership: pandemic impact on physical and emotional health, p < .001, and positive changes associated with the pandemic, p = .001. Pairwise comparisons showed most of the significant differences were between the resilient trajectory and the other three trajectories; therefore, Table 3 shows complete results from comparisons with the resilient trajectory as the reference class. Note that the estimates reflect adjusted odds ratios, or the association between a predictor and trajectory membership after controlling for all other predictors in the model. There was a significantly higher likelihood of membership in the recurring, recovering, or chronic trajectories, relative to the resilient trajectory, among participants with more pandemic‐related physical and mental health problems at baseline. Additionally, relative to the resilient trajectory, there was a significantly higher likelihood of being in the recovering or recurring trajectories among participants with fewer pandemic‐related positive changes at baseline. Consistent with prepandemic PTSD trajectory studies, several of the variables for which we controlled were also significant in the model, including age, p < .001, and lifetime trauma exposure, p < .001. Several pairwise comparisons with alternate reference trajectories were significant for the control variables but not the pandemic‐related predictors. Lifetime exposure to more types of PTEs was associated with higher odds of membership in the chronic versus recurring trajectory, aOR = 1.58, 95% CI [1.19, 2.09], or the chronic versus recovering trajectory, aOR = 1.42, 95% CI [1.06, 1.90]. Relative to the chronic trajectory, older age was associated with higher odds of membership in the resilient, aOR = 2.21, 95% CI [1.48, 3.31]; recurring, aOR = 1.78, 95% CI [1.15, 2.76]; or recovering trajectories, aOR = 1.84, 95% CI [1.16, 2.90].
TABLE 3.
Predictors of posttraumatic stress disorder (PTSD) trajectory membership
| Trajectory | ||||||
|---|---|---|---|---|---|---|
| Recovering | Recurring | Chronic | ||||
| Predictor | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
| Early pandemic impact, by domain | ||||||
| Work/employment | 1.03 | [0.80, 1.33] | 1.13 | [0.90, 1.40] | 0.90 | [0.66, 1.23] |
| Home life | 1.02 | [0.78, 1.34] | 1.13 | [0.90, 1.41] | 1.24 | [0.93, 1.65] |
| Social/isolation | 1.05 | [0.82, 1.34] | 0.89 | [0.71, 1.11] | 0.95 | [0.71, 1.27] |
| Physical/mental health | 1.54* | [1.15, 2.06] | 2.01* | [1.55, 2.61] | 1.86* | [1.31, 2.63] |
| Positive change | 0.72* | [0.56, 0.94] | 0.69* | [0.55, 0.87] | 0.76 | [0.56, 1.04] |
| Control variables with documented associations to PTSD trajectories | ||||||
| Female sex | 1.22 | [0.75, 1.99] | 1.63* | [1.05, 2.54] | 1.69 | [0.90, 3.16] |
| Age | 0.83 | [0.64, 1.08] | 0.81 | [0.63, 1.02] | 0.45* | [0.30, 0.68] |
| Income level | 0.89 | [0.67, 1.17] | 0.87 | [0.68, 1.10] | 0.61 | [0.40, 0.94] |
| Education level | 0.83 | [0.64, 1.08] | 1.13 | [0.90, 1.42] | 0.83 | [0.59, 1.16] |
| Cumulative trauma types | 1.67* | [1.34, 2.08] | 1.50* | [1.22, 1.84] | 2.37* | [1.84, 3.04] |
Note: Adjusted odds ratios (aORs) reflect pairwise comparisons with the resilient trajectory. Continuous variables were standardized such that aORs represent the change in odds of trajectory membership per 1 standard deviation increase in the predictor, adjusted for all other predictors in the model. CI = confidence interval.
p < .05 for the pairwise comparison (uncorrected).
Post hoc analyses
Post hoc analyses, which were suggested by reviewers, were conducted to more closely examine the association between PTSD trajectories and COVID‐related illness and COVID‐related deaths of friends and loved ones. Supplementary Table S4 contains descriptive statistics of the eight individual items measured by the EPII that relate to COVID infections and deaths. Given that our examination of pandemic experiences occurred early in the pandemic (i.e., April 2020), there was a low incidence rate of the individual infection‐related items. We created a composite EPII infection variable using the same approach described in the Methods section (see Table 2 for descriptive statistics). Supplementary Table S5 contains results from the multinomial logistic regression. The EPII infection variable was not significant in the model, p = .277, and its inclusion did not meaningfully change the results (i.e., all previously significant variables remained significant in the model).
DISCUSSION
Identifying meaningful variations in how PTSD symptoms evolve is critical to both public health and personalized treatment approaches. The results established the presence, prevalence, and key early discriminating traits of four distinct courses of PTSD symptoms: resilient (73.0%), recurring (13.3%), recovering (8.3%), and chronic (5.5%). These findings offer evidence that over a 16‐month period of pandemic stress, the longitudinal patterns of traumatic stress response in individuals with prior trauma exposure were consistent with patterns evident over shorter timespans during the pandemic (Dufour et al., 2021; Kalaitzaki & Rovithis 2021; Solomon et al., 2021). Thus, for most individuals, the path forward over time is not marked with the hallmark symptoms of PTSD, including nightmares, intrusive thoughts, affective numbing, cognitive distortions (e.g., shame, guilt), or hyperarousal and irritability (Bonanno, 2004; Bryant et al., 2015). Even among study participants who experienced at least one PTE in their lifetime by early in the pandemic (April of 2020), almost three quarters reported few symptoms of PTSD during this highly stressful year (i.e., resilient trajectory) and continued to report minimal symptoms into the second summer of the pandemic, when infection and hospitalization rates were decreasing, most U.S. states had opened, and more of the population had begun to return to the workplace and the outside world.
Similar patterns have emerged among the few studies that have reported on trajectory analyses during the COVID‐19 pandemic. One recent United Kingdom–based study of the general population (Shevlin, Butter, McBride, Murphy, Gibson‐Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, & Bentall, 2021) that focused on posttraumatic symptoms over a 4‐month period early in the COVID pandemic identified five, largely parallel our findings, categorized as resilient, adaptive, vulnerable, and chronic. The authors reported a moderate‐stable fifth class, whereas other studies have reported a delayed‐onset group, neither of which was identified in our dataset. Notably, Shevlin, Butter, McBride, Murphy, Gibson‐Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, and Bentall (2021) focused on the “pandemic as the trauma” rather than conducting a formal assessment of PTE exposure encompassing events that may have occurred either within or outside both the pandemic context and study time frame. Similarly, in another COVID‐19–related, 6‐month study examining a nationally representative sample in Ireland (Hyland et al., 2021), four trajectories of response on internalizing symptoms emerged, encompassing resilient, sustained improving, worsening, and symptom trajectories, also mirroring our findings, although this study occurred before the onset of vaccine availability and was considerably briefer than our 16‐month timeframe.
The second aim of this study was to determine if early pandemic experiences were associated with PTSD symptom trajectory membership even after controlling for variables that have shown consistent associations with PTSD trajectories in prepandemic research. Among the pandemic‐related variables tested, only physical or emotional health impacts and positive changes due to the pandemic (e.g., more quality time with loved ones) had significant unique associations with specific PTSD trajectories. This provides evidence about some of the mechanisms through which the pandemic may have exacerbated PTSD symptoms, acting as an additional, corrosive stressor for individuals suffering from prior PTSD (Breslau et al., 2008).
Specifically, participants with more pandemic‐related physical and mental health problems at baseline (e.g., “increase in use of alcohol or substances,” “unable to access mental health treatment”) showed meaningfully higher odds of having a symptomatic trajectory compared to being classified into the resilient trajectory. For example, every increase of approximately two pandemic‐related physical or emotional problems (i.e., ∼1 standard deviation) was associated with twice the odds of membership in the recurring trajectory, nearly twice the odds of chronic trajectory membership, and 1.5 higher odds of membership in the recovering trajectory, even after controlling for all other factors in the model. Similar associations have been observed in other studies in which individuals infected with COVID‐19 who had longer hospitalizations or reported more maladaptive coping, hopelessness, and loneliness were at greater risk of ongoing psychological distress (Lin et al., 2021; Matalon et al., 2021; Shevlin, Butter, McBride, Murphy, Gibson‐Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, & Bentall, 2021). Given that PTSD can be chronic for many people if not treated (Resick et al., 2012), it is possible that pandemic‐related health problems, or safety precautions taken because of suspected COVID‐19 infection, may have disrupted the provision of trauma‐focused treatment or other supports that helped to manage prepandemic PTSD symptoms.
Conversely, participants with more pandemic‐related positive changes were more likely to belong to the resilient trajectory than the recurring or recovering trajectories. Given that many of the items in the EPII positive change domain have to do with social support (e.g., more quality time with family or friends, new connections with supportive people), this finding is consistent with research linking social support and resilience (Ozbay et al., 2007). Taken together, the present findings highlight the need to identify individuals who experienced both higher levels of health‐related stressors during the COVID‐19 pandemic and fewer positive changes, as they may be at risk for PTSD symptoms that persist beyond the pandemic.
Consistent with prior work, two of the sample characteristics we controlled for in our analyses showed the expected statistical associations with PTSD symptom trajectories: age (Kessler et al., 2005; Bonanno et al., 2007) and lifetime exposure to a higher number of PTE types (Solomon et al. 2021). Participants who were younger in age and those with exposure to a higher number of trauma types had a reduced likelihood of membership in the resilient trajectory compared to the other three trajectories. Although not the focus of our study, these findings allude to the rich bodies of literature documenting the contribution of developmentally sensitive periods and the cumulative burden of trauma “loads” to the progression of PTSD over time (Brewin et al., 2000).
Several study limitations should be noted. Relative to the U.S. population, the study sample overrepresented White, Asian, and non‐Hispanic/Latinx participants and underrepresented Black, multiracial, and Hispanic/Latinx participants. Due to the sample size, we did not examine the contribution of racial and ethnic identities to trajectory membership. It is well established that Black, Indigenous, and Latinx communities have disproportionately borne COVID‐19 pandemic burdens, and the mental health sequelae of these disparities merit specific and concerted attention (Nana‐Sinkam et al., 2021). Secondly, certain U.S. regions were affected by the COVID‐19 pandemic sooner than others; given the complexity of modeling these impacts, we did not factor in such indices of pandemic severity (e.g., infection, hospitalization, and mortality rates) to control for geographic differences. Our regression model controlled for cumulative types of lifetime trauma exposure assessed using the LEC‐5, which does not make a distinction between trauma that occurred in childhood or adulthood. We focused on early pandemic stressors plus strong predictive variables that have previously predicted PTSD trajectories and did not account for a host of potentially impactful contextual variables, such as preexisting and ongoing mental health conditions or treatment engagement. Although the observation period for the current study was longer than prior COVID‐19 pandemic investigations, assessments were not conducted at higher frequency time points (e.g., monthly) that might provide evidence for other, alternative trajectories and/or better inform the dynamic course of those already identified. Moreover, we cannot assume that the four trajectories identified continued on the same path, especially in the context of the delta and omicron variant COVID waves.
The present study provides support for the presence of multiple, heterogeneous temporal profiles of PTSD in the U.S. population during the COVID‐19 pandemic. Considering both the inherent variability identified in the current study and the role of COVID‐19 problems in shaping the course of PTSD symptoms are key to designing effective individual‐ and policy‐level responses, including treatment and recovery support for people who experience widespread traumatic stressors.
OPEN PRACTICES STATEMENT
This article reported on prespecified aims, hypotheses, and analytic plans (https://osf.io/phwf2/) from a preregistered broader study, the COVID‐Dynamic Project. Within the COVID‐Dynamic Project in the Open Science F repository, the Introduction to the COVID Dynamic Dataset component (https://osf.io/kex8y/) contains all assessment instruments (https://osf.io/nhm2v/) and the full COVID‐Dynamic data dictionary (https://osf.io/z8k2t/). The component specific to the current manuscript (https://osf.io/hy3aq/) contains a project‐specific dataset, data dictionary, analysis code, and output.
AUTHOR NOTE
This work was supported by grants from the National Institute of Mental Health (2P50MH094258), Caltech Chen Neuroscience Institute, Caltech Merkin Institute, Oscar M. Ruebhausen Fund at Yale Law School, Rutgers Center of Alcohol & Substance Use Studies, John Templeton Foundation, and Kay Family Foundation at Chapman University. The opinions expressed in this publication are those of the authors and do not necessarily reflect the views of the funding agencies. We have no known conflicts of interest to disclose.
COVID‐Dynamic team members associated with this work are as follows: Amber Hopkins, Dehua Liang, Uri Maoz, and Tessa Rusch. A detailed characterization of each author's contribution can be found in Supplementary Table S3.
OPEN RESEARCH BADGES
This article has earned an Open Materials badge for making publicly available the components of the research methodology needed to reproduce the reported procedure and analysis. All materials are available at https://osf.io/9vgzj/.
Supporting information
Supporting Material
Lopez‐Castro, T. , Papini, S. , Bauer, A. , Swarbrick, M. , Paul, L. K. , Nizzi, M. ‐. C. , Stanley, D. , & COVID‐Dynamic Team, and Denise Hien . (2022). Posttraumatic stress disorder symptom trajectories in a 16‐month COVID‐19 pandemic period. Journal of Traumatic Stress, 00, 1–13. 10.1002/jts.22899
REFERENCES
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed.). [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Armenta, R. F. , Walter, K. H. , Geronimo‐Hara, T. R. , Porter, B. , Stander, V. A. , & LeardMann, C. A. , for the Millennium Cohort Study Team . (2019). Longitudinal trajectories of comorbid PTSD and depression symptoms among U.S. service members and veterans. BMC Psychiatry, 19(1), 1–12. 10.1186/s12888-019-2375-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asendorpf, J. B. , van de Schoot, R. , Denissen, J. J. A. , & Hutteman, R. (2014). Reducing bias due to systematic attrition in longitudinal studies: The benefits of multiple imputation. International Journal of Behavioral Development, 38(5), 453–460. 10.1177/0165025414542713 [DOI] [Google Scholar]
- Asmundson, G. J. G. , Paluszek, M. M. , Landry, C. A. , Rachor, G. S. , McKay, D. , & Taylor, S. (2020). Do pre‐existing anxiety‐related and mood disorders differentially impact COVID‐19 stress responses and coping? Journal of Anxiety Disorders, 74, 102271. 10.1016/j.janxdis.2020.102271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A. , Weathers, F. W. , Davis, M. T. , Witte, T. K. , & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist, 59(1), 20–28. 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. (2005). Resilience in the face of potential trauma. Current Directions in Psychological Science, 14(3), 135–138. 10.1111/j.0963-7214.2005.00347.x [DOI] [Google Scholar]
- Bonanno, G. A. , Galea, S. , Bucciarelli, A. , & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682. 10.1037/0022-006X.75.5.671 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Mancini, A. D. , Horton, J. L. , Powell, T. M. , LeardMann, C. A. , Boyko, E. J. , Wells, T. S. , Hooper, T. I. , Gackstetter, G. D. , Smith, T. C. , for the Millennium Cohort Study Team . (2012). Trajectories of trauma symptoms and resilience in deployed U.S. military service members: Prospective cohort study. The British Journal of Psychiatry, 200(4), 317–323. 10.1192/bjp.bp.111.096552 [DOI] [PubMed] [Google Scholar]
- Bovin, M. J. , Marx, B. P. , Weathers, F. W. , Gallagher, M. W. , Rodriguez, P. , Schnurr, P. P. , & Keane, T. M. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL‐5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breslau, N. , Peterson, E. L. , & Schultz, L. R. (2008). A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiological study. Archives of General Psychiatry, 65(4), 431–437. 10.1001/archpsyc.65.4.431 [DOI] [PubMed] [Google Scholar]
- Brewin, C. R. , Andrews, B. , & Valentine, J. D. (2000). Meta‐analysis of risk factors for posttraumatic stress disorder in trauma‐exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. 10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Bryant, R. A. , Nickerson, A. , Creamer, M. , O'Donnell, M. , Forbes, D. , Galatzer‐Levy, I. , McFarlane, A. C. , & Silove, D. (2015). Trajectory of post‐traumatic stress following traumatic injury: 6‐year follow‐up. The British Journal of Psychiatry, 206(5), 417–423. 10.1192/bjp.bp.114.145516 [DOI] [PubMed] [Google Scholar]
- Cénat, J. M. , Blais‐Rochette, C. , Kokou‐Kpolou, C. K. , Noorishad, P.‐G. , Mukunzi, J. N. , McIntee, S.‐E. , Dalexis, R. D. , Goulet, M.‐A. , & Labelle, P. R. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Research, 295, 113599. 10.1016/j.psychres.2020.113599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, J. , Liang, Y.‐M. , Zhou, Y.‐Y. , Eli, B. , & Liu, Z.‐K. (2019). Trajectories of PTSD symptoms among children who survived the Lushan earthquake: A four‐year longitudinal study. Journal of Affective Disorders, 252, 421–427. 10.1016/j.jad.2019.04.047 [DOI] [PubMed] [Google Scholar]
- Clark, S. L. , & Muthén, B. (2016). Relating latent class analysis results to variables not included in the analysis. http://www.statmodel.com/download/relatinglca.pdf
- Dufour, M. M. , Bergeron, N. , Rabasa, A. , Guay, S. , & Geoffrion, S. (2021). Assessment of psychological distress in health‐care workers during and after the first wave of COVID‐19: A Canadian longitudinal study. The Canadian Journal of Psychiatry, 66(9), 807–814. 10.1177/07067437211025217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster, K. , Mitchell, R. , Van, C. , Young, A. , McCloughen, A. , & Curtis, K. (2019). Resilient, recovering, distressed: A longitudinal qualitative study of parent psychosocial trajectories following child critical injury. Injury, 50(10), 1605–1611. 10.1016/j.injury.2019.05.003 [DOI] [PubMed] [Google Scholar]
- Galatzer‐Levy, I. R. , Huang, S. H. , & Bonanno, G. A. (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. 10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- Graham, J. W. (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Grasso, D. J. , Briggs‐Gowan, M. J. , Carter, A. S. , Goldstein, B. L. , & Ford, J. D. (2021). Profiling COVID‐related experiences in the United States with the Epidemic–Pandemic Impacts Inventory: Linkages to psychosocial functioning. Brain and Behavior, 11(8), e02197. 10.1002/brb3.2197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso, D. J. , Briggs‐Gowan, M. J. , Ford, J. D. , & Carter, A. S. (2020). Epidemic–Pandemic Impacts Inventory (EPII). https://health.uconn.edu/psychiatry/research/family‐adversity‐and‐resilience‐research‐program/epii/
- Hien, D. A. , López‐Castro, T. , Fitzpatrick, S. , Ruglass, L. M. , Fertuck, E. A. , & Melara, R. (2021). A unifying translational framework to advance treatment research for comorbid PTSD and substance use disorders. Neuroscience & Biobehavioral Reviews, 127, 779–794. 10.1016/j.neubiorev.2021.05.022 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. (1989). Conservation of resources. A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. 10.1037//0003-066x.44.3.513 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. (2002). Social and psychological resources and adaptation. Review of General Psychology, 6(4), 307–324. 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- Hobfoll, S. E. , Mancini, A. D. , Hall, B. J. , Canetti, D. , & Bonanno, G. A. (2011). The limits of resilience: Distress following chronic political violence among Palestinians. Social Science & Medicine, 72(8), 1400–1408. 10.1016/j.socscimed.2011.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge, C. W. , Riviere, L. A. , Wilk, J. E. , Herrell, R. K. , & Weathers, F. W. (2014). The prevalence of post‐traumatic stress disorder (PTSD) in U.S. combat soldiers: A head‐to‐head comparison of DSM‐5 versus DSM‐IV‐TR symptom criteria with the PTSD checklist. The Lancet Psychiatry, 1(4), 269–277. 10.1016/S2215-0366(14)70235-4 [DOI] [PubMed] [Google Scholar]
- Hyland, P. , Vallières, F. , Daly, M. , Butter, S. , Bentall, R. P. , Fox, R. , Karatzias, T. , MacLachlan, M. , McBride, O. , Murphy, J. , Murphy, D. , Spikol, E. , & Shevlin, M. (2021). Trajectories of change in internalizing symptoms during the COVID‐19 pandemic: A longitudinal population‐based study. Journal of Affective Disorders, 295, 1024–1031. 10.1016/j.jad.2021.08.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, T. , & Wickrama, K. A. S. (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. 10.1111/j.1751-9004.2007.00054.x [DOI] [Google Scholar]
- Kalaitzaki, A. , & Rovithis, M. (2021). Secondary traumatic stress and vicarious posttraumatic growth in healthcare workers during the first COVID‐19 lockdown in Greece: The role of resilience and coping strategies. Psychiatriki, 32(1), 19–25. 10.22365/jpsych.2021.001 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Sonnega, A. , Bromet, E. , Hughes, M. , & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund, P. , Demler, O. , Jin, R. , Merikangas, K. R. , & Walters, E. E. (2005). Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Lin, T. , Yi, Z. , Zhang, S. , & Veldhuis, C. B. (2021). Predictors of psychological distress and resilience in the post–COVID‐19 era. International Journal of Behavioral Medicine, 29(4), 506–516. 10.1007/s12529-021-10036-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe, S. R. , Ratanatharathorn, A. , Lai, B. S. , van der Mei, W. , Barbano, A. C. , Bryant, R. A. , Delahanty, D. L. , Matsuoka, Y. J. , Olff, M. , Schnyder, U. , Laska, E. , Koenen, K. C. , Shalev, A. Y. , & Kessler, R. C. (2021). Posttraumatic stress disorder symptom trajectories within the first year following emergency department admissions: Pooled results from the International Consortium to Predict PTSD. Psychological Medicine, 51(7), 1129–1139. 10.1017/S0033291719004008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvaldi, M. , Mallet, J. , Dubertret, C. , Moro, M. R. , & Guessoum, S. B. (2021). Anxiety, depression, trauma‐related, and sleep disorders among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Neuroscience and Biobehavioral Reviews, 126, 252–264. 10.1016/j.neubiorev.2021.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masyn, K. E. (2013). Latent class analysis and finite mixture modeling. In Little T. D. (Ed.), The Oxford handbook of quantitative methods: Statistical analysis (pp. 551–611). Oxford University Press. [Google Scholar]
- Matalon, N. , Dorman‐Ilan, S. , Hasson‐Ohayon, I. , Hertz‐Palmor, N. , Shani, S. , Basel, D. , Gross, R. , Chen, W. , Abramovich, A. , Afek, A. , Ziv, A. , Kreiss, Y. , Pessach, I. M. , & Gothelf, D. (2021). Trajectories of post‐traumatic stress symptoms, anxiety, and depression in hospitalized COVID‐19 patients: A one‐month follow‐up. Journal of Psychosomatic Research, 143, 110399. 10.1016/j.jpsychores.2021.110399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E. E. , Presskreischer, R. , Anderson, K. E. , Han, H. , & Barry, C. L. (2020). Psychological distress and COVID‐19–related stressors reported in a longitudinal cohort of U.S. adults in April and July 2020. JAMA, 324(24), 2555–2557. 10.1001/jama.2020.21231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson, K. E. , McAloney‐Kocaman, K. , McGlinchey, E. , Faeth, P. , & Armour, C. (2021). Longitudinal analysis of the U.K. COVID‐19 Psychological Wellbeing Study: Trajectories of anxiety, depression and COVID‐19‐related stress symptomology. Psychiatry Research, 304, 114138. 10.1016/j.psychres.2021.114138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, K. , Su, S. , Keck, M. , & Beidel, D. C. (2021). Psychometric properties of the PCL‐5 in a sample of first responders. Journal of Anxiety Disorders, 77, 102339. 10.1016/j.janxdis.2020.102339 [DOI] [PubMed] [Google Scholar]
- Nana‐Sinkam, P. , Kraschnewski, J. , Sacco, R. , Chavez, J. , Fouad, M. , Gal, T. , AuYoung, M. , Namoos, A. , Winn, R. , Sheppard, V. , Corbie‐Smith, G. , & Behar‐Zusman, V. (2021). Health disparities and equity in the era of COVID‐19. Journal of Clinical and Translational Science, 5(1), E99. 10.1017/cts.2021.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nochaiwong, S. , Ruengorn, C. , Thavorn, K. , Hutton, B. , Awiphan, R. , Phosuya, C. , Ruanta, Y. , Wongpakaran, N. , & Wongpakaran, T. (2021). Global prevalence of mental health issues among the general population during the coronavirus disease–2019 pandemic: A systematic review and meta‐analysis. Scientific Reports, 11(1), 1–18. 10.1038/s41598-021-89700-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris, F. H. , Friedman, M. J. , Watson, P. J. , Byrne, C. M. , Diaz, E. , & Kaniasty, K. (2002). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry, 65(3), 207–239. 10.1521/psyc.65.3.207.20173 [DOI] [PubMed] [Google Scholar]
- Ozbay, F. , Johnson, D. C. , Dimoulas, E. , Morgan, III, C. A. , Charney, D. , & Southwick, S. (2007). Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont), 4(5), 35–40. [PMC free article] [PubMed] [Google Scholar]
- Pinkham, A. E. , Ackerman, R. A. , Depp, C. A. , Harvey, P. D. , & Moore, R. C. (2020). A Longitudinal investigation of the effects of the COVID‐19 pandemic on the mental health of individuals with pre‐existing severe mental illnesses. Psychiatry Research, 294, 113493. 10.1016/j.psychres.2020.113493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick, P. A. , Williams, L. F. , Suvak, M. K. , Monson, C. M. , & Gradus, J. L. (2012). Long‐term outcomes of cognitive–behavioral treatments for posttraumatic stress disorder among female rape survivors. Journal of Consulting and Clinical Psychology, 80(2), 201–210. 10.1037/a0026602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ripley, B. , Venables, W. , & Ripley, M. B. (2016). Package ‘nnet’ [Software program]. https://cran.r‐project.org/web/packages/nnet/nnet.pdf
- Rusch, T. , Han, Y. , Liang, D. , Hopkins, A. R. , Lawrence, C. , Maoz, U. , Paul, L. K. , Stanley, D. , and The COVID Dynamic Team . (in press). COVID‐Dynamic: A large‐scale multifaceted longitudinal study of socioemotional and behavioral change across the pandemic. Scientific Data. [DOI] [PMC free article] [PubMed]
- Shevlin, M. , Butter, S. , McBride, O. , Murphy, J. , Gibson‐Miller, J. , Hartman, T. K. , Levita, L. , Mason, L. , Martinez, A. P. , McKay, R. , Stocks, T. V. A. , Bennett, K. , Hyland, P. , & Bentall, R. P. (2021). Refuting the myth of a “tsunami” of mental ill‐health in populations affected by COVID‐19: Evidence that response to the pandemic is heterogeneous, not homogeneous. Psychological Medicine. [Advance online publication]. 10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed]
- Shevlin, M. , Butter, S. , McBride, O. , Murphy, J. , Gibson‐Miller, J. , Hartman, T. K. , Levita, L. , Mason, L. , Martinez, A. P. , McKay, R. , Stocks, T. V. A. , Bennett, K. M. , Hyland, P. , Vallieres, F. , & Bentall, R. P. (2021). Psychological responses to the COVID‐19 pandemic are heterogeneous but have stabilised over time: 1‐year longitudinal follow‐up of the COVID‐19 Psychological Research Consortium (C19PRC) study. Psychological Medicine. Advance online publication. 10.1017/S0033291721004025 [DOI] [PMC free article] [PubMed]
- Solomon, Z. , Ginzburg, K. , Ohry, A. , & Mikulincer, M. (2021). Overwhelmed by the news: A longitudinal study of prior trauma, posttraumatic stress disorder trajectories, and news watching during the COVID‐19 pandemic. Social Science & Medicine, 278, 113956. 10.1016/j.socscimed.2021.113956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon, Z. , Horesh, D. , Ein‐Dor, T. , & Ohry, A. (2012). Predictors of PTSD trajectories following captivity: A 35‐year longitudinal study. Psychiatry Research, 199(3), 188–194. 10.1016/j.psychres.2012.03.035 [DOI] [PubMed] [Google Scholar]
- van de Schoot, R. , Sijbrandij, M. , Winter, S. D. , Depaoli, S. , & Vermunt, J. K. (2017). The GRoLTS‐Checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling, 24(3), 451–467. 10.1080/10705511.2016.1247646 [DOI] [Google Scholar]
- van Zuiden, M. , Engel, S. , Karchoud, J. F. , Wise, T. J. , Sijbrandij, M. , Mouthaan, J. , Olff, M. , & van de Schoot, R. (2022). Sex‐differential PTSD symptom trajectories across one year following suspected serious injury. European Journal of Psychotraumatology, 13(1), 2031593. 10.1080/20008198.2022.2031593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W. , Blake, D. D , Schnurr, P. P. , Kaloupek, D. G. , Marx, B. P. , & Keane, T. M. (2013). The Life Events Checklist for DSM‐5 (LEC‐5). https://www.ptsd.va.gov/professional/assessment/te‐measures/life_events_checklist.asp
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The PTSD Checklist for DSM‐5 (PCL‐5). https://www.ptsd.va.gov/professional/assessment/adult‐sr/ptsd‐checklist.asp
- Wortmann, J. H. , Jordan, A. H. , Weathers, F. W. , Resick, P. A. , Dondanville, K. A. , Hall‐Clark, B. , Foa, E. B. , Young‐McCaughan, S. , Yarvis, J. S. , Hembree, E. A. , Mintz, J. , Peterson, A. L. , & Litz, B. T. (2016). Psychometric analysis of the PTSD Checklist‐5 (PCL‐5) among treatment‐seeking military service members. Psychological Assessment, 28(11), 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Zhou, X. , & Wu, X. (2022). Posttraumatic stress disorder and growth: Examination of joint trajectories in children and adolescents. Development and Psychopathology, 34(4), 1353–1365. 10.1017/S0954579421000213 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Material


