Abstract
BACKGROUND
Home blood pressure monitoring (HBPM) has a substantial role in hypertension management and control.
METHODS
Cross-sectional data for noninstitutionalized US adults 18 years and older (10,958) from the National Health and Nutrition Examination Survey (NHANES), years 2011–2014, were used to examine factors related to HBPM.
RESULTS
In 2011–2014, estimated 9.5% of US adults engaged in weekly HBPM, 7.2% engaged in monthly HBPM, 8.0% engaged in HBPM less than once a month, and 75.3% didn’t engage any HBPM. The frequency of HBPM increased with age, body mass index, and the number of health care visits (all, P < 0.05). Also, race/ethnicity (Non-Hispanic Blacks and non-Hispanic Asians), health insurance, diagnosed with diabetes, told by a health care provider to engage in HBPM, and diagnosed as hypertensive, were all associated with more frequent HBPM (P < 0.05). Adjusting for covariates, hypertensives who were aware of, treated for, and controlled engaged in more frequent HBPM compared to their respective references: unaware (odds ratio [OR] = 2.00, 95% confidence interval [CI] = 1.53–2.63), untreated (OR = 1.99, 95% CI = 1.52–2.60), and uncontrolled (OR = 1.42, 95% CI = 1.13–1.82). Hypertensive adults (aware/unaware, treated/untreated, or controlled/uncontrolled), who received providers’ recommendations to perform HBPM, were more likely to do so compared to those who did not receive recommendations (OR = 8.04, 95% CI = 6.56–9.86; OR = 7.98, 95% CI = 6.54–9.72; OR = 8.75, 95% CI = 7.18–10.67, respectively).
CONCLUSIONS
Seventeen percent of US adults engaged in monthly or more frequent HBPM and health care providers’ recommendations to engage in HBPM have a significant impact on the frequency of HBPM.
Keywords: blood pressure, home blood pressure monitoring, hypertension, NHANES
During 2011–2014, about 54.0% of adults with hypertension had their hypertension controlled. This was a significant increase from 1999 to 2000; however, no significant change was observed from 2009–2010 to 2013–2014. Moreover, 54.0% is still below the hypertension control goal of 62.1% set by Healthy People 2020.1,2
Effective blood pressure (BP) management, resulting in a reduction in BP, has been shown to greatly decrease the incidences of stroke, heart attack, and heart failure.3–6 A number of evidence-based systematic reviews of the literature suggest that home BP monitoring (HBPM) has a significant role in hypertension management by having people become aware of their BP in between physician visits and be more engaged in their overall BP management, which may lead to reducing both systolic and diastolic BP values.7,8 Also, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure describes clinical situations in which HBPM may be useful to reduce systolic and diastolic BP values and increase treatment compliance. The US Preventive Services Task Force also recommends obtaining measurements outside of the clinical setting for diagnostic confirmation before starting treatment.9,10
Using 2011–2014 NHANES data, the purpose of this study was 3-fold. First, to assess the frequency of HBPM and its association with demographic characteristics, income, health care utilization, cardiovascular risk factors, health care provider recommendation of HBPM, hypertension status, and 3 binary hypertension-related measurements: (i) hypertensive aware, (ii) hypertensive treated, and (iii) hypertensive controlled. Second, to examine whether a health care provider’s recommendation of HBPM has an impact on HBPM frequency after controlling for the effects of the 3 binary hypertension-related measurements and other covariates. Third, to evaluate whether the overall frequency of HBPM changed between 2009 and 2014.
METHODS
Survey description
The 2011–2014 NHANES was conducted by the National Center for Health Statistics (NCHS). NHANES used a complex multistage probability sample design to select participants who were representative of the entire civilian, noninstitutionalized US population. Participants were interviewed in their homes by an interviewer to obtain information on health history, health behaviors, and risk factors. Subsequently, participants underwent physical examinations at a Mobile Examination Center (MEC). The procedures to select the sample and conduct the home interview and MEC examination were previously described.11 The NCHS Research Ethics Review Board approved the NHANES protocol.
Sample
In NHANES survey cycles 2011–2014, 17,879 adults aged 18 years and older were sampled. Of those, 11,977 (67%) were interviewed in the home and 11,539 (64%) were then examined. Of those examined, 581 persons were excluded for the following reasons: 122 were pregnant, 3 missed the household HBPM questions, and 456 had missing BP data. These exclusions resulted in a final analytic sample of 10,958 (61%) participants aged 18 years and older for this study.
Definitions
Response variables.
HBPM was defined by an affirmative response to the home interview question “Did you take your blood pressure at home during the last 12 months?” Respondents who answered “yes” were then asked by the interviewer “How often did you check your blood pressure at home during the last 12 months?” They could answer the number of times per week, per month, or per year and the frequency was recorded by the number of times per year. For example, if a respondent stated that he/she took his/her BP twice a week, this was recorded as 104 (2 × 52) times a year.
Frequency of HBPM was classified as follows: respondents who answered “no” to the first question were classified as none (n = 8,180). One to 11 times in the past 12 months was categorized as less than once a month (n = 788); 12 to 51 times in the past 12 months was categorized as monthly but less than weekly and were referred to as monthly (n = 764); and 52 or more times in the past 12 months was categorized as weekly or more frequent and were referred to as weekly (n = 1,226). The 4 categories (none, less than once a month, monthly, and weekly) covered the entire frequency range and were mutually exclusive. These categories were used in our previous report.12
Covariates.
Age was categorized as 18 to 39, 40 to 59, 60 to 79, and 80 years or more. Race and Hispanic origin is self-reported and classified as Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and other. Results for the “other” category are included in the total sample analysis, but are not shown separately.
Income.
Family income to poverty ratio is the ratio of a family’s income to its appropriate poverty threshold as established by the US Department of Health and Human Services.13 Three categories of approximately equal size were used for this analyses: ≤ 1.3 (establishes income eligibility for Supplemental Nutrition Assistance Program (SNAP)), >1.3 to <3.5, and >3.5. Larger family income to poverty ratios indicate higher income.
Health insurance and health care utilization.
Availability of health insurance was defined by an affirmative response to the home interview question “Are you covered by health insurance or some other kind of healthcare plan?” Frequency of visits to a health care provider was self-reported based on the answer to the home interview question, “During the past 12 months, how many times have you seen a doctor or other healthcare professional about your health at a doctor’s office, a clinic, hospital emergency room, at home, or some other place?”.14
Risk factors.
Diabetes was defined as “diagnosed diabetic” (told by a doctor or health care provider that he/she has diabetes). Body mass index (BMI) was calculated as measured weight in kilograms over measured height in meters squared (kg/m2), and was categorized using criteria established by the National Institutes of Health as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Due to the relatively small number of participants in the underweight category, the underweight category was combined with the normal category after a sensitivity analysis showed little difference in the results when excluding the underweight category or when including it in the normal weight category.
BP-related variables.
The NHANES procedure to obtain BP is described in detail in the National Health and Nutrition Examination Survey: Physician’s Manual.15 A maximum of 3 brachial systolic and diastolic BP readings were collected for each participant in the MEC by trained physicians and followed a standard protocol measuring BP at the MEC using a Bauman true gravity mercury wall model and standard Bauman cuffs.
Participants were defined as being hypertensive if they had a systolic BP of 140 mm Hg or greater, a diastolic BP of 90 mm Hg or greater, or were currently taking prescribed medications for high BP. “Aware” of high BP among people with hypertension was defined by an affirmative response to the question, “Have you ever been told by a doctor or health professional that you have hypertension, also called high blood pressure?” “Treated” among people with hypertension was defined as currently taking prescribed medications to lower high BP. “Controlled” among people with hypertension was defined as currently taking medications to lower high BP and a systolic BP less than 140 mm Hg and diastolic BP less than 90 mm Hg.
Finally, the recommendation to use HBPM was defined as an affirmative response to the home interview question “Did a doctor or other health professional tell {you/sampled person (SP)} to take {your/his/her} blood pressure at home?”
Statistical analyses
Data analyses were conducted using SAS (version 9.3; SAS Institute, Cary, NC) and SUDAAN (version 10.1; Research Triangle Institute, Research Triangle Park, NC). All analyses used the MEC sample weights. The MEC sample weights account for the complex survey design (including oversampling), survey nonresponse, and are also poststratified to obtain nationally representative estimates of the civilian, noninstitutionalized US population.11
Taylor Series linearization was used to calculate SEs and 95% confidence intervals (CI). The independent associations of the categorical and ordinal covariates with the frequency of HBPM were examined using the Rao–Scott chi-square test. Additionally, the ordinal covariates (age groups, BMI, family income to poverty ratio, and the number of health care visits) were tested for linear association with the frequency of HBPM using the stratum-adjusted Cochran–Mantel–Haenszel test for trend (CMH).16 The CMH test for trend assumes that both row and column variables are on ordinal scales and a P-value of less than 0.05 suggests that linear relationship between the 2 variables fits the data better than no relationship.16
Three multivariate ordered logistic regression models (also called proportional odds models) were used to examine the independent association of the frequency of HBPM (none, less than once a month, monthly, and weekly) with the 3 hypertension status-related variables: (i) aware, (ii) treated, and (iii) controlled. Additionally, to examine whether the health care providers’ recommendation for HBPM affected HBPM behavior differently for different levels of BP-related measurements, interactions of “health care provider telling to take HBPM” with the 3 BP-related variables were tested in their corresponding proportional odds models among adults with hypertension. All of the models were adjusted for: sex, age group, race and Hispanic origin, family income to poverty ratio, availability of health insurance, number of visits to the health care provider, BMI categories, and diagnosed diabetes.
Of note, the assumption of the proportional odds model is that the frequency of HBPM has a natural ordering from low to high (no monitoring, less than once per month, monthly but less than weekly, weekly or more frequent) and that the effects of a covariate on the different cumulative logit functions are statistically the same. Adjusted ORs having a 95% CI, not including unity, were considered statistically significant.
Trends in the frequency of HBPM across the three 2-year survey periods, 2009–10, 2011–12, and 2013–14, were tested using the stratum-adjusted CMH.16 The stated null hypothesis was that there was no linear trend in the frequency of HBPM. Rejection of this hypothesis implied that a linear trend fit the data better than no relationship. A P-value of less than 0.05 was considered statistically significant for the test.
RESULTS
All tests are based on HBPM defined using 4 categories of frequency (none, less than once a month, monthly, and weekly). Since monthly or weekly HBPM is more clinically useful, the presentation of results from Table 1 focus on the combined monthly and weekly categories.17,18 Overall, during 2011–2014, 24.7% of adults engaged in HBPM in the past year and approximately 16.7% of adults engaged in monthly or more frequent HBPM.
Table 1.
Weighted percentages of home blood pressure monitoring (HBPM) among US adults by demographic and health characteristics, NHANES 2011–2014
| n | Frequency of home blood pressure monitoring | ||||
|---|---|---|---|---|---|
|
| |||||
| None | Less than once a month | Monthly | Weekly | ||
|
| |||||
| Percent (95% confidence interval) | |||||
|
| |||||
| Total | 10,958 | 75.3 (73.8–76.8) | 8.0 (7.0–9.0) | 7.2 (6.2–8.2) | 9.5 (8.7–10.3) |
| Sex | |||||
| Male | 5,413 | 76.0 (74.2–78.0) | 8.1 (7.0–9.1) | 7.2 (5.9–8.4) | 8.8 (7.8–9.7) |
| Female | 5,545 | 74.6 (72.9–76.3) | 7.9 (6.5–9.2) | 7.3 (6.1–8.5) | 10.2 (9.1–11.3) |
| Age group (years)*** | |||||
| 18–39 | 4,108 | 87.4 (85.9–88.9) | 6.0 (4.9–7.1) | 3.2 (2.4–4.1) | 3.4 (2.7–4.1) |
| 40–59 | 3,514 | 76.6 (74.3–78.9) | 7.9 (6.6–9.2) | 7.5 (6.0–9.1) | 7.9 (6.9–9.0) |
| 60–79 | 2,720 | 57.2 (53.9–60.5) | 11.5 (8.8–14.1) | 12.3 (10.0–14.7) | 19.0 (16.8–21.2) |
| 80 or more | 616 | 48.9 (44.9–52.9) | 7.5 (4.6–10.3) | 14.1 (11.3–16.9) | 29.5 (26.7–32.3) |
| Race/ethnicity* (age adjusted)a | |||||
| Non-Hispanic White | 4,304 | 76.1 (74.3–77.8) | 8.2 (7.0–9.6) | 7.1 (6.0–8.5) | 8.6 (7.8–9.5) |
| Non-Hispanic Black | 2,588 | 75.3 (72.3–78.1) | 8.0 (6.1–10.2) | 5.8 (4.6–7.3) | 13.2 (12.1–14.3) |
| Hispanic | 2,370 | 81.4 (78.7–84.0) | 5.6 (4.5–6.9) | 5.5 (4.5–6.8) | 7.4 (5.9–9.3) |
| Non-Hispanic Asian | 1,367 | 75.3 (72.3–78.1) | 8.0 (6.1–10.2) | 5.8 (4.6–7.3) | 11.0 (9.3–12.8) |
| Income-to-poverty ratio* | |||||
| <1.30 | 3,620 | 79.2 (76.8–81.5) | 5.7 (4.6–6.9) | 5.5 (4.2–6.7) | 9.6 (8.0–11.2) |
| 1.30–3.49 | 3,442 | 72.1 (69.6–74.6) | 8.9 (7.3–10.5) | 8.5 (6.5–10.4) | 10.5 (9.2–11.9) |
| ≥3.50 | 3,025 | 75.6 (73.6–77.6) | 9.1 (7.7–10.5) | 7.3 (5.9–8.7) | 8.0 (6.9–9.1) |
| Health insurance* | |||||
| Yes | 8,486 | 73.1 (71.4–74.7) | 8.5 (7.4–9.7) | 7.7 (6.5–9.0) | 10.7 (9.8–11.6) |
| No | 2,457 | 84.9 (83.0–86.8) | 5.6 (4.4–6.8) | 5.1 (3.8–6.3) | 4.4 (3.6–5.3) |
| Health care visits past year*** | |||||
| None | 1,774 | 86.5 (83.9–89.0) | 7.6 (5.8–9.4) | 3.5 (2.3–4.7) | 2.4 (1.6–3.2) |
| 1 –3 | 7,757 | 75.0 (73.5–76.6) | 8.2 (7.2–9.2) | 7.5 (6.4–8.6) | 9.3 (8.2–10.3) |
| ≥ 4 | 1,421 | 63.7 (59.6–67.8) | 6.9 (4.6–9.2) | 10.2 (7.5–12.9) | 19.2 (16.0–22.4) |
| Body mass index (BMI)*** | |||||
| Normal | 3,525 | 81.2 (79.0–83.5) | 7.1 (5.4–8.8) | 5.1 (3.8–6.4) | 6.5 (5.3–7.8) |
| Overweight | 3,422 | 75.3 (73.0–77.7) | 7.2 (5.8–8.6) | 8.2 (6.7–9.8) | 9.2 (8.1–10.4) |
| Obese | 3,879 | 70.5 (67.9–73.1) | 9.4 (8.1–10.7) | 8.1 (6.5–9.7) | 12.0 (10.9–13.1) |
| Diagnosed diabetes* | |||||
| Yes | 1,333 | 55.0 (51.3–58.6) | 9.4 (6.2–12.5) | 12.5 (9.3–15.7) | 23.2 (20.8–25.6) |
| No | 9,619 | 77.4 (75.9–78.9) | 7.8 (6.8–8.8) | 6.7 (5.7–7.7) | 8.1 (7.3–8.9) |
| Hypertensive* | |||||
| Yes | 3,785 | 51.0 (48.4–53.6) | 10.3 (8.6–12.1) | 14.3 (12.6–16.1) | 24.4 (22.9–25.8) |
| No | 7,173 | 86.4 (85.3–87.5) | 6.9 (6.0–7.7) | 4.0 (3.2–4.8) | 2.8 (2.2–3.3) |
| Aware among hypertensive adults* | |||||
| Yes | 3,165 | 45.9 (43.0–48.9) | 10.5 (8.6–12.4) | 15.5 (13.3–17.8) | 28.0 (26.2–29.7) |
| No | 618 | 76.6 (73.1–80.2) | 9.3 (6.3–12.4) | 8.1 (5.3–10.9) | 5.9 (3.9–7.9) |
| Treated among hypertensive adults* | |||||
| Yes | 2,856 | 43.7 (40.9–46.4) | 10.5 (8.7–12.4) | 16.3 (13.9–18.8) | 29.5 (27.4–31.5) |
| No | 927 | 73.1 (69.2–77.0) | 9.8 (6.4–13.3) | 8.2 (5.8–10.6) | 8.9 (7.1–10.8) |
| Controlled among hypertensive adults* | |||||
| Yes | 1,914 | 44.5 (40.5–48.4) | 11.1 (8.5–13.7) | 16.3 (13.4–19.3) | 28.1 (25.6–30.7) |
| No | 1,871 | 58.3 (55.6–61.1) | 9.5 (7.2–11.8) | 12.0 (10.2–13.9) | 20.1 (17.9–22.3) |
| Told to take HBPM among hypertensive adults* | |||||
| Told | 1,283 | 17.5 (14.8–20.2) | 10.9 (8.4–13.5) | 20.8 (17.5–24.1) | 50.8 (46.7–54.9) |
| Not told | 2,499 | 68.6 (65.4–71.9) | 10.1 (7.9–12.2) | 10.9 (9.3–12.6) | 10.4 (8.9–11.9) |
Frequency: none; 1–11 times in the past 12 months was considered less than once a month; 12–51 times in the past year was considered monthly; and ≥52 times in the past year was considered weekly or more frequent. Hypertension was defined as measured systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or reported currently taking prescribed medications for high blood pressure. Underweight participants are part of the “normal” weight category for body mass index.
P < 0.05, Rao–Scott chi-square test.
P < 0.05, linear trend using Cochran–Mantel–Haenszel test for trend.
Estimates are age-adjusted by the direct method to the 2000 U.S. census projected population using age groups 18–39, 40–59, 60–79, and 80 and over.
There was no statistically significant difference in the frequency of HBPM by sex. HBPM frequency was associated with age group (older subjects were more likely to perform HBPM and the frequency of HBPM increased as age increased, P <0.05 for trend). For example, only 6.6% of adults aged 18–39 years engaged in monthly or more frequent HBPM, while 43.6 of adults aged 80 years and older engaged in monthly or more frequent HBPM. After age-adjustment, self-reported race/ethnicity categories were significantly associated with the frequency of HBPM (P < 0.05), specifically 19.0% of non-Hispanic Black and 16.8% of non-Hispanic Asian adults engaged in monthly or more frequent HBPM whereas 15.7% of non-Hispanic White and 12.9% Hispanic adults engaged in such an activity. Other significant associations included: income-to poverty ratio (i.e., the middle income-to-poverty group did HBPM more often than the other groups, P <0.05 for association), health care utilization (i.e., increased health care utilization associated with more frequent HBPM, P <0.05 for linear trend), having health insurance (i.e., people with health insurance were more likely and more frequently doing HBPM, P <0.05 for association), number of health care visits (i.e., the more visits the more frequent HBPM, P <0.05 for trend). Risk factors and hypertension status were also associated with more frequent HBPM. Adults with higher BMI levels and diagnosed diabetes engaged in more frequent HBPM (i.e., the greater BMI the more frequent HBPM, P <0.05 for trend; and being diagnosed with diabetes was associated with more frequent HBPM, P <0.05 for association). Adults who were hypertensive, who were aware of, who were treated for and who had controlled hypertension, were more likely to engage in more frequent HBPM (e.g., 38.7%, 43.5%, 45.8%, and 44.4% engaged in monthly or more frequent HBPM, respectively) compared with those who were normotensive, unaware, not treated, and uncontrolled (e.g., 6.8%, 14%, 17.1%, and 32.1% engaged in monthly or more frequent HBPM, respectively; P <0.05 for association). Of note, only 34% of adults with hypertension received a recommendation from their health care providers to engage in HBPM health care and 71.6% followed the recommendation and engaged in monthly or more frequent HBPM.
After adjusting for covariates, the interactions between the health care provider recommendation for HBPM with the aforementioned hypertension groups (aware, treated, and controlled) were not statistically significant (P > 0.05 for all interactions), so we removed the interaction terms and focused on the main effects only.
Table 2 shows the results of the 3 multivariate ordered logistic regression models. Hypertensive adults who were aware of their hypertension were more likely to practice more frequent HBPM compared to those who were not aware (odds ratio [OR] = 2.00, 95% CI = 1.53–2.63), and hypertensive adults who were told by their health care providers to take home BP were more likely to engage in more frequent HBPM compared to those who were not told (OR = 8.04, 95% CI = 6.56–9.86). Similar patterns were shown in models 2 and 3. Hypertensive adults who were treated and who had controlled hypertension were more likely to engage in more frequent HBPM than those who were not treated and were not controlled (OR = 1.99, 95% CI = 1.52–2.60; OR = 1.42, 95% CI = 1.13–1.82, respectively). And similar to model 1, those who were told to perform HBPM were more likely to practice more frequent HBPM when compared to those who were not told (model 2: OR = 7.97, 95% CI = 6.54–9.72; model 3: OR = 8.75, 95% CI = 7.18–10.67).
Table 2.
Ordered logistic regressiona assessing the association of the weighted percentage of home blood pressure monitoring increased frequencyb with hypertension awareness, treatment, control, and told by health care provider to take BP at home: US adults aged ≥18 years, National Health and Nutrition Examination Survey, 2011–2014
| Model | Hypertensive categories and told to take BP at home | Adjusted odds ratio (95% confidence limit) |
|---|---|---|
|
| ||
| 1 | Hypertensive-aware | |
| Aware | 2.00 (1.52–2.63) | |
| Unaware | Reference | |
| Told | 8.04 (6.56–9.86) | |
| Not told | Reference | |
| 2 | Hypertensive-treated | |
| Treated | 1.99 (1.51–2.60) | |
| Not treated | Reference | |
| Told | 7.97 (6.54–9.72) | |
| Not told | Reference | |
| 3 | Hypertensive-controlled | |
| Controlled | 1.42 (1.11–1.82) | |
| Not controlled | Reference | |
| Told | 8.75 (7.18–10.67) | |
| Not told | Reference | |
Abbreviations: BP, blood pressure; HBPM, home blood pressure monitoring.
The association of the frequency of HBPM with told to do HBPM and the hypertension categories adjusted for demographic characteristics, family income-to-poverty ratio, availability of health insurance, health care utilization, diagnosed diabetes, and body mass index.
Frequency: none; 1–11 times in the past 12 months was considered less than once a month; 12–51 times in the past year was considered monthly; and ≥52 times in the past year was considered weekly or more frequent.
Finally, Figure 1 presents the frequency of HBPM (none, less than once a month, monthly, and weekly) across the three 2-year survey periods, the frequency of not engaging in HBPM behavior decreased by 3% from 78% in 2009–2010 to 75% in 2013–2014, whereas the frequency of engaging in monthly or more frequent HBPM increased by 2% from 15% in 2009–2010 to 17% in 2013–2014 (P < 0.05, significant for trend).
Figure 1.
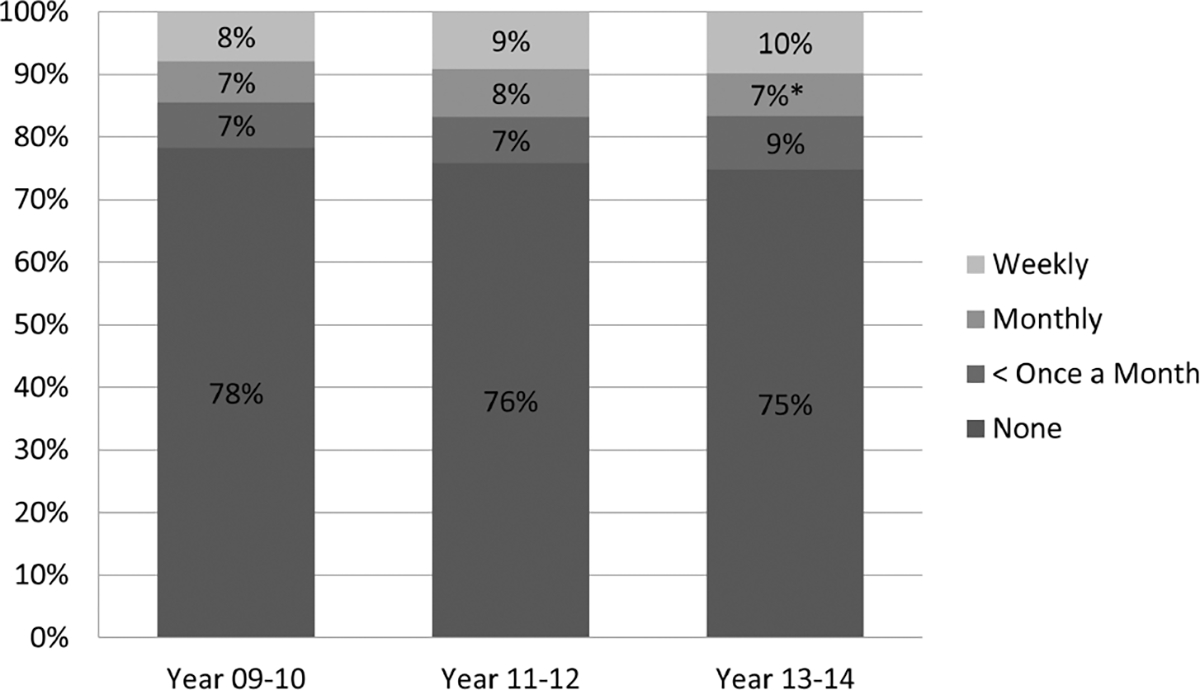
Frequency of home blood pressure monitoring among adults aged 18 years and over: NHANES 2009–2014. *Percent rounded up. The frequency of engaging in monthly or more frequent HBPM increased by 2% from 15% in 2009–2010 to 17% in 2013–2014 (P <0.05, significant for trend).
DISCUSSION
Numerous factors are associated with hypertension control, among them are demographic, income, and behavioral risk factors. This analysis suggests that HBPM is associated with those covariates. Also, health care provider recommendation to engage in HBPM may contribute to more frequent engagement in HBPM and better hypertension control. The findings in this study indicate that approximately 17% of the noninstitutionalized US population aged ≥18 years engaged in monthly or more frequent HBPM. The percentage of adults with hypertension who engaged in more frequent HBPM significantly increased with age, BMI, the number of visits to health care providers, having health insurance, being classified as hypertensive, and being aware of, treated for, and had their hypertension controlled. In addition, health care professionals’ recommendations that hypertensive adults take BP at home was significantly associated with engaging in more frequent HBPM.
Strength and limitations
This is the first NHANES study to assess the impact of health care providers recommending HBPM on the frequency of HBPM. Our results show that health care providers have a significant impact on whether or not a person with hypertension will monitor their BP at home and the frequency of HBPM, including among those aware, pharmacologically treated and controlled. A number of recent systematic reviews of the role of HBPM suggest that HBPM has a significant role in controlling both systolic and diastolic BP. Agarwal et al. reviewed 37 randomized control trials, and the findings show that compared with control (i.e., clinic BP) HBPM resulted in an average reduction of 2.63 mm Hg in systolic BP and 1.6 mm Hg in diastolic BP.7 Uhlig et al. reviewed 52 prospective studies comparing HBPM to control (i.e., clinic BP), and concluded that the combination of HBPM and communicating the results of the HBPM with the health care providers showed a statistically significant reduction in either systolic or diastolic BP at follow-up, specifically a 3.9 mm Hg reduction in systolic BP and a 2.4 mm Hg reduction in diastolic BP, compared with control.8 However, only about one-third of the adults with hypertension in our study were told by their health care provider to use HBPM.
Stergiou et al. stated, “Home blood pressure monitoring should have a primary role in diagnosis, treatment adjustment, and long-term follow-up of hypertension cases” (p.1).17 Indeed, a recent report by the American Heart Association’s (AHA), Call to Action on Use and Reimbursement for Home Blood Pressure Monitoring, made a number of recommendations, including educating persons on how to accurately obtain BP at home, to fit the person with the correct BP cuff size, to purchase only devices that were validated by international standards, and to calibrate the home BP device to the physician’s office BP device.18 Furthermore, recently, Shimbo et al. pointed out that “core clinical competency” on how to take home BP does not exist in the United States and suggest 3 areas of competency that need to be advanced: (i) standardized training on how to obtain accurate home BP, (ii) develop standardized tests to evaluate the skills, and (iii) create a program to maintain the skills.19 In contrast, the European Society of Hypertension recently provided guidelines to individuals on how and at what frequency to obtain HBPM. These guidelines should be instructive to help develop US guidelines.20
The findings in this report are subject to some limitations. First, the cross-sectional nature of our survey precludes us from assigning cause and effect to our results.
Second, misclassification of participants could occur if they provided inaccurate or incomplete information. For example, the participant may have reported that they were unaware of their hypertension, when in fact they were previously told by their health care providers that they were hypertensive. Third, “treatment” was narrowly defined as the use of medications; another treatment method included in the JNC 7 recommendations is lifestyle modifications, such as weight loss and exercise.3 Fourth, there is a limitation with the assumptions made in converting reported frequency of HBPM over the past year into number of times per year. For example, it is conceivable that a person may have started monitoring his/her BP at home in the last 6 months and reports that he/she is doing it weekly; according to our algorithm the person will be classified as engaging in HBPM 52 times a year when in reality they engaged only 26 times that year.
In conclusion, clinical BP is no longer the only approach to obtain BP values, both 24-hour ambulatory BP monitoring and HBPM are acknowledged ways to obtain BP.19–21 The results of this analysis highlight the need to better understand the factors associated with more frequent HBPM and the role of health care providers in encouraging the use of HBPM. To this end, a system similar to the International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) pioneered by Stergiou and others may be a step forward to better understand the role of home BP monitoring in monitoring the prevalence of high BP.22 Finally, new technology making it easier to integrate the HBPM data into the clinical/survey data environment, for example, cloud-based remote monitoring.23
ACKNOWLEDGMENTS
The authors would like to acknowledge Michele Chiappa for outstanding editorial help and Jeffery Hughes for computer programming help.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Office of Disease Prevention and Health Promotion Healthy people 2020. <https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke/objectives>. Accessed 1 June 2017.
- 2.Yoon SS, Fryar CD, Carroll MD. Hypertension Prevalence and Control Among Adults: United States, 2011–2014. NCHS Data Brief, No. 220. National Center for Health Statistics: Hyattsville, MD, 2015. [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 4.Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009; 338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024. [PubMed] [Google Scholar]
- 7.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension 2011; 57:29–38. [DOI] [PubMed] [Google Scholar]
- 8.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med 2013; 159:185–194. [DOI] [PubMed] [Google Scholar]
- 9.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111:697–716. [DOI] [PubMed] [Google Scholar]
- 10.Siu AL; U.S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. preventive services task force recommendation statement. Ann Intern Med 2015; 163: 778–786. [DOI] [PubMed] [Google Scholar]
- 11.Curtin LR, Mohadjer L, Dohrmann S, Montaquila JM, Kruszan-Moran D, Mirel LB, Carroll MD, Hirsch R, Schober S, Johnson CL. The National Health and Nutrition Examination Survey (NHANES) Survey: sample design, 1999–2006. Vital Health Stat 2 2012; 155:1–39. [PubMed] [Google Scholar]
- 12.Ostchega Y, Berman L, Hughes JP, Chen TC, Chiappa MM. Home blood pressure monitoring and hypertension status among US adults: the National Health and Nutrition Examination Survey (NHANES), 2009–2010. Am J Hypertens 2013; 26:1086–1092. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. Poverty Guidelines, Research, and Measurement. <https://aspe.hhs.gov/poverty-research>. Accessed 1 June 2017.
- 14.National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) Questionnaire and Exam Protocol. <http://www.cdc.gov/nchs/about/major/nhanes/questexam>. Accessed 1 June 2017.
- 15.National Health and Nutrition Examination Survey (2003). Physician Examination Procedures Manual. <http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/PE.pdf>. Accessed 1 June 2017.
- 16.Mantel N. Chi-square tests with one degree of freedom; extensions of the Mantel-Haenszel Procedure. J Am Stat Assoc 1963; 58:690–700. [Google Scholar]
- 17.Stergiou GS, Kollias A, Zeniodi M, Karpettas N, Ntineri A. Home blood pressure monitoring: primary role in hypertension management. Curr Hypertens Rep 2014; 16:462. [DOI] [PubMed] [Google Scholar]
- 18.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; American Heart Association; American Society of Hypertension; Preventive Cardiovascular Nurses Association. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008; 52:1–9. [DOI] [PubMed] [Google Scholar]
- 19.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Studies comparing ambulatory blood pressure and home blood pressure on cardiovascular disease and mortality outcomes: a systematic review. J Am Soc Hypertens 2016; 10:224–234.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O’Brien E, Ohkubo T, Padfield P, Palatini P, Pickering TG, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G; ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24:779–785. [DOI] [PubMed] [Google Scholar]
- 21.Krakoff LR. Blood pressure out of the office: its time has finally come. Am J Hypertens 2016; 29:289–295. [DOI] [PubMed] [Google Scholar]
- 22.Krakoff LR. Home blood pressure monitoring: international recognition. Hypertension 2014; 63:670–671. [DOI] [PubMed] [Google Scholar]
- 23.Consensus Document. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: current status and future directions Position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular variability. J Hypertens 2016; 34:1665–1677. [DOI] [PubMed] [Google Scholar]


