Abstract
Objective.
Home healthcare agencies (HHAs) are skilled care providers for Medicare home health beneficiaries in the United States. Rural HHAs face different challenges than their urban counterparts in delivering care, e.g., longer distances to travel to patient homes leading to higher fuel/travel costs and fewer number of visits in a day, impacting the quality of home healthcare for rural beneficiaries. We review evidence on differences in care outcomes provided by urban and rural HHAs.
Design.
Systematic review guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and using the Newcastle-Ottawa Scale (NOS) for quality appraisal.
Setting.
Care provided by urban and rural HHAs.
Methods.
We conducted a systematic search for English-language peer-reviewed articles after 2010 on differences in urban and rural care provided by U.S. HHAs. We screened 876 studies, conducted full-text abstraction and NOS quality review on 36 articles and excluded two for poor study quality.
Results.
Twelve studies were included; 7 focused on patient-level analyses and 5 were HHA-level. Nine studies were cross-sectional and 3 used cohorts. Urban and rural differences were measured primarily using a binary variable. All studies controlled for agency-level characteristics, and two-thirds also controlled for patient characteristics. Rural beneficiaries, compared to urban, had lower home healthcare utilization (4 of 5 studies) and fewer visits for physical therapy and/or rehabilitation (3 of 5 studies). Rural agencies had lower quality of HHA services (3 of 4 studies). Rural patients, compared to urban, visited the emergency room more often (2 of 2 studies) and were more likely to be hospitalized (2 of 2 studies), whereas urban heart failure patients were more likely to have 30-day preventable hospitalizations (1 study).
Conclusion and Implications.
This review highlights similar urban/rural disparities in home healthcare quality and utilization as identified in previous decades. Variables used to measure the access to and quality of care by HHAs varied so consensus was limited. Articles that utilized more granular measures of rurality (rather than binary measures) revealed additional differences. These findings point to the need for consistent and refined measures of rurality in studies examining urban and rural differences in care from HHAs.
Keywords: urban, rural, home health care, home health agencies, quality of care
Introduction
Home health care agencies (HHAs) are the primary providers for skilled care delivered in the home setting to Medicare beneficiaries in the United States (U.S.). These beneficiaries can receive up to 6 types of professional care: skilled nursing care, physical therapy, speech therapy, occupational therapy, medical social services, and home health aide services.1 This includes skilled care provided by nurses, social workers, physical therapists, occupational therapists, or speech therapists as well as both basic and instrumental activities of daily living (ADL and IADL) such as bathing, dressing, and housekeeping provided by a personal care attendant or home health aide.
The majority of Medicare beneficiaries live in areas served by at least one HHA.2 When providing care in rural areas with low concentrations of patients, HHAs face different challenges than urban HHAs, such as longer distances to travel to patient homes.3, 4 This leads to fewer number of visits in a day due to increased travel times, as well as higher fuel and travel costs for rural HHAs. Additionally, for HHA clinicians, reimbursement for fuel and travel costs vary between rural HHAs, which decreases overall clinician take-home pay and impacts staffing levels at HHAs with lower reimbursements. As a result, some rural beneficiaries have difficulty receiving any home health care, specialty services, and/or the appropriate amount of required services.5–8 Concerns about access to home health care for rural beneficiaries exist despite both historical and current incentive payments for HHAs to encourage provision of care to rural beneficiaries.4, 9
Prior evidence suggests there are not only urban and rural differences in access to home health care but also differences in the quality of home health care that is delivered.6, 7, 10 Rural home health patients were hospitalized and received emergent care significantly more often than urban patients.10 Functional outcomes based on ADL and IADL measures consistently favored urban patients. Home health care utilization (i.e., visits by provider type) differed by service-use for rural and urban patients, due in part by patient and agency characteristics and availability of home health resources (e.g., lack of physical therapists in rural communities).6, 7, 10 Direct home health care minutes per visit differed between rural and urban HHAs (i.e., rural patients had fewer minutes).10
Despite the evidence acknowledging disadvantages in care provided by HHAs for older adults in rural areas, no literature review in the last decade has focused specifically on the differences in care provided by urban and rural HHAs to older adults living at home. We sought to examine the current evidence on differences in care provided by urban and rural HHAs.
Methods
We reviewed articles on differences in care provided in urban and rural HHAs in the U.S. We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.11, 12
Search strategy.
In consultation with a senior medical librarian, we used a structured search strategy in PubMed and the Cumulative Index of Nursing and Allied Health Literature (CINAHL) to identify English-language, peer-reviewed articles published from January 2010 to April 2021 on care provided by urban and rural HHAs in the U.S. Supplemental Table 1 outlines the search strategy. Briefly, we identified articles using the National Library of Medicine’s Medical Subject Headings (MeSH), keywords and Boolean operators with at least (1) one home health care keyword, (2) one urban/rural keyword, and (3) one quality of care keyword (e.g., quality of care and care experiences).
Article Screening.
We reviewed titles and abstracts of 876 identified articles. After an initial period of double coding to establish consistency across reviewers (DQ, AC, JK, DB), remaining abstracts were independently reviewed by two reviewers to determine eligibility. Reviewers discussed discrepancies during regular meetings and resolved disagreement to reach consensus on inclusion. Included abstracts were reviewed by all authors. Reviewers confirmed inclusion of articles at the title and abstract stage.
Abstraction.
We undertook a full review of 36 articles. During this phase, we reviewed references of included articles to identify any additional potential articles. Reviewers abstracted specific information into a standardized data abstraction instrument: study aim; time frame; type of study; study design; statistical approach; variables controlled for in analysis; type of care; sample size; sample description; study population descriptions; HHA characteristics; main outcome(s) measured; secondary outcome(s) (if any); description of urban/rural variable; relevant rural vs. urban findings; relevant HHA findings; issues reported as possibly affecting HHA care; issues reported related to urbanicity/rurality; study limitations related to urbanicity/rurality or HHA care. To ensure reviewers employed a similar approach, articles (N=8) were selected for double-review and discussion. After discussion and training meetings, each reviewer independently abstracted 6-10 of the remaining articles. After all articles were abstracted, each article was reviewed by a second reviewer to ensure accuracy of abstracted content and the team discussed issues or discrepancies, where needed, to gain consensus.
Quality Assessment and Risk of Bias.
During full-text review, we also assessed study quality of the included articles using the Newcastle-Ottawa Scale (NOS). The NOS is an 8-item checklist that examines cohort and case-control studies (nonrandomized studies) in three areas awarding stars for ‘high study quality’ characteristics: 1) selection (4 items each worth 1 star); 2) comparability (1 item worth maximum 2 stars); and 3) assessment of outcomes/ascertainment of exposure (3 items each worth 1 star). Scores range from 0-9. Using the Agency for Health care Research and Quality (AHRQ)-developed thresholds, the scores translate into an overall rating of good, fair or poor study quality. Good study quality includes three to four stars for selection, one to two stars for comparability, and two to three stars for outcome/exposure. Fair study quality includes two stars for selection, one to two stars for comparability, and two or three stars for outcome/exposure. Poor study quality includes zero to one star for selection, zero stars for comparability, or zero to one star for outcome/exposure. Two of three researchers (DQ, AC, JK) independently scored each article and study quality rating results were discussed as a team to gain consensus. Supplemental Table 2 reports study quality scores.
Data Synthesis.
We examined the articles across study type, setting, data used, outcomes, urban/rural measures. We then synthesized the findings according to the quality outcomes.
Results
The database search and expert suggestions identified 876 articles. As shown in Figure 1, articles were initially excluded if the title and abstract indicated the research: did not include care provided by HHAs (N=206); included only urban or only rural HHA care (N=44); were not studying home health care in the U.S. (N=581); or were not empirical studies (e.g., commentaries; N=9). Full article review of 36 articles excluded an additional 22 articles because the study: did not specifically examine care provided by HHAs (N=16); included only urban or only rural care (N=2)4, 13; were not studying U.S. home health care (N=2); or were not empirical studies (e.g., commentaries; N=2). Based on the NOS quality rating, two articles were rated as “poor” study quality, possibly introducing bias, and were ultimately excluded. Ten studies were rated as “good” and two rated as “fair.” Altogether, 12 articles were included in our synthesis.14–25
Figure 1.
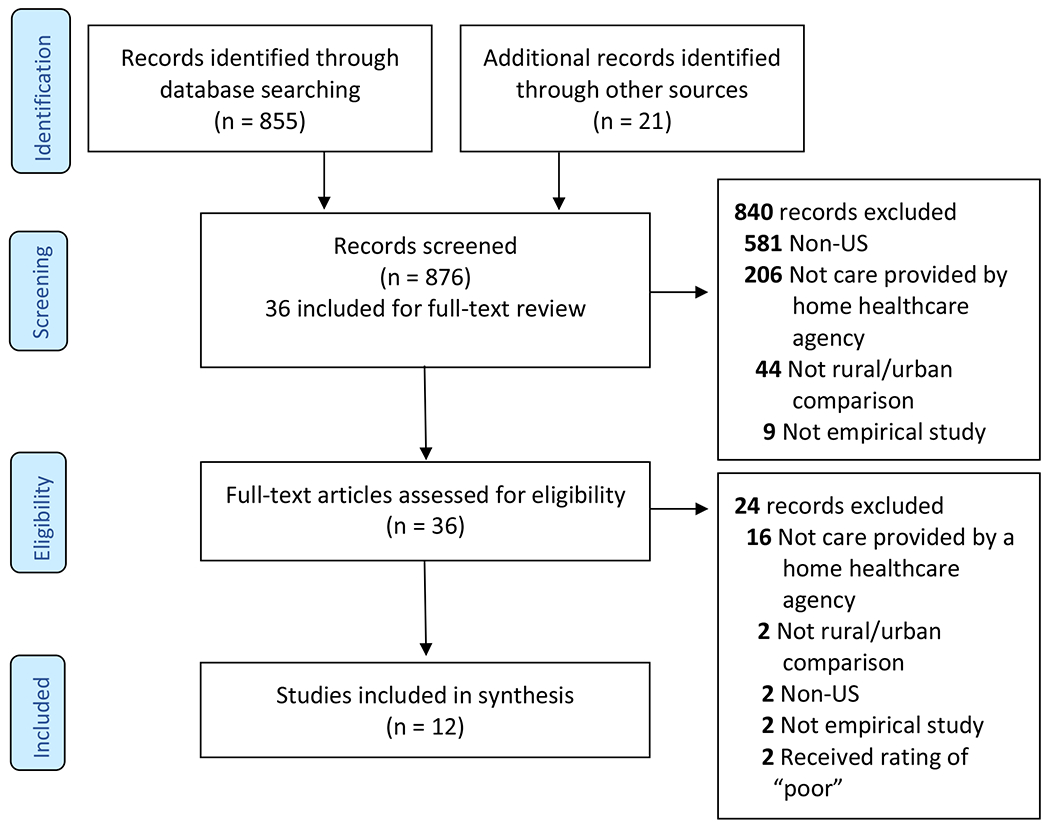
PRISMA Flow Diagram
Studies.
Table 1 describes the study type, methods, population, data source and measures. Of the twelve studies, three19, 21, 23 were cohort studies and the remaining nine14–18, 20, 22, 24, 25 were cross-sectional studies. All study settings were U.S. HHAs with Medicare beneficiaries, with 5 studies that focused analyses at the HHA-level15, 20, 22, 24, 25 and the remaining 7 focused at the patient-level. Specifically, studies included Medicare beneficiaries with heart failure,14 stroke19 or Alzheimer’s Disease and Related Dementia (ADRD),23 after total knee arthroplasty,17 who received rehabilitation care,19, 22 or were enrolled in fee-for-service plans.21, 22 The studies also included utilization outcomes (hospital admission, emergency room visits,20 intensive care unit [ICU] readmissions).18 One study only included HHAs that subscribed to a specific electronic medical record software.16
Table 1.
Methods, Population and Measures for Included Studies
| Design & Statistical Approach | Population Characteristics | Urban/Rural Measures | Home Health (HH) Quality Measures and Data Sources |
|---|---|---|---|
| Chen 2016 | |||
| • Case control • Multivariable logistic regression to examine the impact of rurality on the 30-day preventable readmission, illness severity, and risk of mortality in Home Health (HH) Medicare beneficiaries with heart failure. • Estimated odds ratio and 95% confidence intervals. |
• 51,667 post-acute home health care episodes, and 4,862 post-acute home health care episodes that had 30-day preventable readmission among heart failure HH beneficiaries. • About 83% are from urban areas, 2% remote rural areas, 4% adjacent rural areas, and 11% micropolitan areas. • About 43% were aged 85 and older, 83% were Caucasian, more than 90% required assistance in medication management or ADL, and 93% had shortness of breath. • About 51% of the index admissions were at the extreme/major level of illness severity, and 49% extreme/major level of risk of mortality. |
• Urban influence codes (UIC) from Area Health Resources File (AHRF) to distinguish between urban/rural: remote rural areas (codes from 9 to 12); adjacent rural areas (codes 4, 6 and 7); micropolitan areas (codes 3, 5, and 8); and urban areas (codes 1 and 2). | • 3 HH quality measures include: (1) a 30-day preventable readmission; (2) the extreme/major level of illness severity for a 30-day preventable readmission; and (3) the extreme/major level of risk of mortality for a 30-day preventable readmission. • 2009 MBSF, MedPAR, OASIS and Home Health Agency Research Identifiable File for patient-level data, and Area Health Resource Files (AHRF) for Home Health Agency (HHA)-level data. |
| Chen 2020 | |||
| • Case control • An analysis of variance (ANOVA) to compare quality measures between urban agencies and the 3 rural agencies. The number of beneficiaries without a low-utilization payment episode as a weight for estimation. • Weighted least squares regression models to compare urban HHAs and HHAs in each of the 3 rural categories accounting for patient, agency, and community characteristics. • P-value < 0.05 • Coefficient and 95% confidence intervals. |
• 12,155 Home Health Agencies (HHA)s from the Public Use File (PUF) data. After merged with other data, 10,202 observations were included. • 651 HHAs located in high utilization rural areas were clustered in the southern region with an average of 320 beneficiaries per year. • 977 HHAs located in all other rural areas were clustered in the northeast region with an average of 247 beneficiaries per year. • Only 80 HHAs located in low population density areas were clustered in the north central region and Alaska with an average caseload of 80 beneficiaries per year. |
• CMS grouped U.S. counties into urban and 3 rural categories: high utilization, low population density, and all other rural areas (as defined by the Bipartisan Budget Act Act of 2018). | • 7 quality measures of HHAs include: (1) hospitalizations; (2) Emergency Department (ED) visits; (3) a patient-experience star rating; (4) Activities of Daily Living (ADL) improvement; (5) pain management improvement; (6) harm prevention; and (7) treating wounds. • Quality measures were directly extracted or calculated from Home Health Compare. • 2015 Home Health Compare, HHA PUF, Provider of Services (POS), AHRF, and Medicare HH PPS rates and wage index. |
| Cotton 2017 | |||
| • Case control • Bivariate logistic regression models with any controlled medication as the binary dependent variable to determine predictor variables. • Multivariable logistic regression models to examine associations between each class of controlled medication and retained predictor variables. • P-value < 0.05 • Odds ratio and 95% confidence intervals |
• 132 HHAs that subscribed to Brightree, LLC located across 32 states, serving an average of 333 patients per year. • 87,780 Medicare patients (age ≥ 65) episodes using OASIS between 2013-2014. • 63.3% female, 33.2% were aged 86 and older, 87.5% White, and 11.1% Black. |
• Compared rural versus metropolitan. Article did not specify the source or how to classify rural vs metropolitan was made however, it could only be through Medicare claims or agency level data about the location of the home health agency from the Brighttree system. | • Frequency of use and factors related to opioid analgesics, benzodiazepines, and non-benzodiazepine hypnotics in HH patients. • 2013-2014 OASIS and electronic health records from 132 HHAs. |
| Falvey 2018 | |||
| • Case control • Multivariable linear regression models to examine relationships between PT utilization and improvement in activities of daily living (ADLs). • Negative binomial regression models to determine factors associated with PT utilization. • P-value < 0.05 • Adjusted mean difference and 95% confidence intervals. |
• 5,967 HH Medicare beneficiaries after total knee arthroplasty in 2012. • 17.2% HHAs were located in rural areas, 53.1% were for-profit, 44.3% were located in South. • 83.2% age between 65 and 84 years, 67.8% female, 89% Caucasian, and the mean duration of home health care was 20.8 days. |
• Rurality was defined in the POS file by a binary indicator of whether the area in which the HHA was located was metropolitan (urban) or not (rural) based on the 2010 Core Based Statistical Area (CBSA) designation. | • Improvements in ADL function after PT utilization in HH settings. • The number of PT visits utilized during the HH episode. • 2012 MedPAR, POS, Organization for the Advancement of Structured Information Systems (OASIS) and Medicare HHA claims. |
| Falvey 2020 | |||
| • Case control • A zero-inflated negative binomial regression model to estimate the bivariate association of each candidate variable on episode rehabilitation visits. • A multivariable model to estimate the proportional difference in rehabilitation visits for each level of variable. • P-value < 0.05 • Adjusted risk ratios and 95% confidence intervals. |
3,176 Medicare beneficiaries using HH services who were discharged from an Intensive Care Unit( ICU) and stayed ICU longer than 24 hours. 24.3% were rural residence. 35% aged between 65 and 75, 82.2% White, 22.3% Medicaid beneficiaries, and 46.3% had 6-10 hospital length of stay. |
• Patient level residence was captured by mapping state and county code of residence to Medicare’s Core-Based Statistical Areas (CBSAs) from 2012. | • Number of rehabilitation visits received per patient within the first home health care episode (up to 60 days). • Factors associated with the number of rehabilitation visits received among ICU survivors during the HH episode. • 2012 OASIS, MedPAR, Master Beneficiary Summary File (MBSF) and Medicare HHA claims. |
| Iyer 2016 | |||
| • Cohort • Bivariate analysis using chi-square tests and t-tests to examine urban/rural differences. • A logistic random effects regression model to examine potential predictors of HH service delivery by rehabilitation specialist, controlling for beneficiary and county-level variables. • P-value < 0.05 • Adjusted odds ratios and 95% confidence intervals. |
• 214,146 observations from 6,767 unique beneficiaries with stroke and 9,367 unique HH episodes from 2007 HH claims data. 6,005 beneficiaries who received rehabilitation care were included as a subset. • 19.3% were rural beneficiaries. • About two thirds were female, and one third were aged 85 years or older, about 60% had 3 or more comorbidities. |
• Urban influence codes (UIC) from 2011 Area Health Resources File (AHRF) to identify rurality of the beneficiaries’ residence: rural areas (codes from 3 to 12) and urban areas (codes 1 and 2). | • Intensity of home health services, as defined by the number of visits and service delivery by rehabilitation specialists among Medicare beneficiaries with stroke. • 2009 Medicare HHA claims. |
| Koru 2018 | |||
| • Case control • Used regression trees to develop linear and logistic regression models to examine clinical practices most associated with HHA adverse outcomes (hospital admissions; ER visits), controlling for agency-level variables, such as process measures and agency characteristics. • Variable importance scores were generated in R (rpart package). |
• 12,255 Medicare-certified HHAs in 2014 Home Health Compare; after removing HHAs missing utilization outcome variables (i.e., with less than 20 patients), 9,164 observations remained. • 21.5% of HHAs served rural areas. • Most urban HHAs were larger agencies (annual visit counts ≥6,882). |
• Rural-Urban Commuting Area (RUCA) codes provided levels of rurality using the suggested Categorization Scheme A (level 1 = urban; levels 2-4 = rural, very rural, and extremely rural). | • Home health adverse outcomes as defined by average hospital admission rate and ER visit rate among urban and rural HHAs. • 2014 Home Health Compare. |
| Mroz 2018 | |||
| • Case control Multivariable and multilevel regression models were used to examine associations between organizational characteristics of HHAs and quality outcomes among Medicare beneficiaries with rehabilitation-sensitive conditions. • Maximum likelihood estimation and the Huber-White-Sandwich method were used to estimate parameters and parameter variations. • P-value < 0.05 |
• 9,250 Medicare-certified HHAs offering physical, occupational or speech therapy in 2009. • From those HHAs, 1,006,562 fee-for-service beneficiaries (aged 65+) were included if admitted with a primary diagnosis of a rehabilitation-sensitive condition and discharged alive (but not to hospice or against medical advice) from an “index” home health episode between January 1 to December 31, 2009. • Most agencies were located in urban areas (78.1%). |
• Defined by a binary indicator of whether the area in which the HHA was located was metropolitan (urban) or not (rural) based on the 2003 Rural-Urban Continuum Code (RUCC) categories. | • Discharge to community, institutional admission (hospital, SNF or IRF) from HH episode and 30-day institutional admission after discharge. • 2009 OASIS, POS, AHRF, Geographic Variation Public Use File (GV-PUF) and Medicare HHA claims. |
| Mroz 2020 | |||
| • Cohort • Calculated unadjusted averages of home health utilization by location and used hierarchical linear regression to explore differences in U.S. home health utilization among urban and rural-dwelling Medicare beneficiaries. • Used generalized estimating equation (GEE) to account for clustering. • P-value < 0.10 |
• 3,115 counties with fee-for-service Medicare beneficiaries receiving home health care services in 2013. • 37.3% of those included were located in metropolitan counties; 32.7% were in micropolitan counties adjacent to a metropolitan area; 8.6% were in micropolitan counties not adjacent to a metropolitan area; 11.9% were in non-core counties adjacent to a micropolitan area; and, 9.5% were in non-core counties not adjacent to any metro or micro area. |
• 2013 UICs from AHRF were categorized into 5 urban/rural categories: 1) metropolitan; (2) micropolitan or non-core adjacent to a large or small metropolitan area; (3) micropolitan not adjacent to a metropolitan area; (4) non-core adjacent to micropolitan area; and, (5) non-core not adjacent to a metropolitan or micropolitan area. | • Home health care utilization at the county level, as defined by: percentage of beneficiaries using HH services, and HH episodes and visits per 1,000 beneficiaries. • 2013 OASIS, 2013 OASIS, MedPAR, MDS, Medicare claims (home health agency, inpatient and skilled nursing facility), GV-PUF, AHRF and the 2015 U.S. Department of Agriculture Economic Research Service (USDA ERS) county typology file. |
| Rahman 2020 | |||
| • Cohort • Descriptive statistics and linear regression models were used to retrospectively analyze acute and post-acute care use, as well as survival and health outcomes, among rural and urban Medicare beneficiaries with Alzheimer’s Disease and Related Dementia (ADRD) in the 6 years after diagnosis (study period: January 1, 2009, to December 31, 2016). • P-value < 0.05 |
• 555,333 Medicare beneficiaries who had an ADRD flag with a date of diagnosis in 2010. • 76.5% of beneficiaries lived in metropolitan counties. |
• Beneficiary county of residence was obtained from MBSF. • Rural-Urban Commuting Area (RUCA) codes from AHRF were assigned to the counties using 3 levels of rurality: metropolitan (codes 1-3), micropolitan (codes 4-7), and rural (codes 8-9). |
• Survival and health care utilization, as defined by: percentage of survived days per month after initial ADRD diagnosis spent in the community with and without HH services. • 2009-2016 MBSF, OASIS, Minimum Data Set (MDS), Medicare claims (inpatient, skilled nursing facility, home health agency, hospice, and outpatient), AHRF and Social Deprivation Index (SDI) data. |
| Shang 2021 | |||
| • Case-control • Descriptive statistics were computed to assess infection prevention and control- related policies, infrastructure, and procedures in U.S. HHAs prior to the SARS-CoV-2 pandemic, by urban/rural location • P-value < 0.05 |
• 1,506 U.S. (including D.C. and Puerto Rico) Medicare-certified HHAs with active provider status from the June 2018 Provider of Services file. • Complete responses from 536 HHAs were obtained (35.6% response rate). • Most of the responding HHAs were located in urban areas and in the South Census region. |
• Rurality was defined in the POS file by a binary indicator of whether the area in which the HHA was located was metropolitan (urban) or not (rural) based on the 2010 Core Based Statistical Area (CBSA) designation. | • Infection prevention and control-related policies, infrastructure, and procedures, as a function of quality of care • Cross-sectional survey data (from November 9, 2018 through December 31, 2019), June 2018 POS file, and July 2018 Home Health Compare and HHCAHPS datasets. |
| Smith 2017 | |||
| • Case control • Descriptive, multivariate, and factor analyses were conducted to examine the effects of provider characteristics on HHA performance on HHCAHPS patient experience of care and OASIS process measures. • P-value < 0.05 |
• 7,826 HHAs were included after excluding those with missing information on any of the dependent or independent variables. • Most (78.0%) HHAs were located in urban areas. |
• Rurality was defined in the POS file by a binary indicator of whether the area in which the HHA was located was metropolitan (urban) or not (rural) based on the 2010 CBSA designation. | • Composite indices from 5 Patient Experience measures in HHCAHPS and 10 process measures in OASIS (removed influenza and pneumococcal vaccination and timely initiation of care) • June 2013 POS, and HHCAHPS and OASIS data from July 2012 through June 2013. |
NOTE: ADRD stands for Alzheimer’s Disease and Related Dementia; AHRF indicates Area Health Resource Files; CBSA indicates Medicare Core-Based Statistical Areas (CBSA) codes; GV-PUF indicates Geographic Variation Public Use File; HHA indicated Home Health Agency, HCAHPS indicated Hospital Consumer Assessment of Health care Providers and Systems (CAHPS) survey; HHCAHPS indicates the Home Health CAHPS survey; MBSF indicates Master Beneficiary Summary File; MDS indicates Minimum Data Set; OASIS stands for Organization for the Advancement of Structured Information Systems (formerly SGML Open); POS indicates Provider of Services; PUF indicates Public Use File; Rural-Urban Commuting Area (RUCA); UIC indicates Urban influence codes.
Data Sources.
Data used for outcomes ranged from January 1, 2009 to December 31, 2018. The included cohort studies analyzed the following data sources to determine home health care outcomes: 2009 Medicare HHA claims (intensity of HHA services19); 2013 Geographic Variation Public Use File (home health care utilization21); and 2009-2016 Master Beneficiary Summary File, Medicare HHA claims and the Outcome and Assessment Information Set (OASIS) to identify days survived after an ADRD diagnosis spent in community with and without home health care services.23
The included case-control studies determined home health care outcomes by analyzing the following data sources: 2009 Medicare Provider Analysis and Review data (MedPAR) for 30-day preventable readmissions14; 2009 OASIS and Medicare HHA claims for discharge to community and institutional admissions22; 2012 OASIS, MedPAR and Medicare HHA claims for physical therapy visits and ADL improvement during home health episodes following a total knee arthroplasty 17, 18; electronic medical records from 2013-2014 for controlled medications16; 2014 Home Health Compare for hospitalizations and emergency department visits 20; 2015 Home Health Compare for hospitalizations, emergency department visits, Patient Experience Star Rating, ADL improvement, pain management improvement, harm prevention, treating wounds15; July 2012 to June 2013 Home Health Care Consumer Assessment of Health Providers and Systems and OASIS for composite indices of five Patient Experience and 10 OASIS process measures25; and 2018-2019 survey data for infection prevention and control-related policies, infrastructure, and procedures24.
Urban/Rural Measures.
Studies used different classifications to determine location of urban and rural HHAs; the majority of studies (N=7) used a binary variable16–19, 22, 24, 25 for urban versus rural, whereas three used four categories,14, 15, 20 one study used three categories,23 and one used five categories21 for rurality variables. Three of the seven studies that used binary variables for urban and rural classifications17, 24, 25 obtained the information from the Provider of Services (POS); in POS, each county is classified based on the urban/rural designations of the associated Core Based Statistical Area (CBSA26) from the Census Bureau. Four studies used CBSAs27 to indicate rurality of Medicare patient residence, three used the Rural-Urban Continuum Codes (RUCC),28 and two used the Urban Influence Code (UIC)29 from the Area Health Resource File (AHRF),30 but each study defined urbanicity and rurality differently. For example, Rahman et al., 2020 used three categories using RUCC codes (metropolitan, micropolitan, and rural), whereas Koru et al., 2018 used four categories using RUCC codes (rural, very rural, and extremely rural, and urban). Using the UIC from the AHRF, Chen et al., 2016 used 4 categories (remote rural areas, adjacent rural areas, micropolitan rural areas, and urban areas), whereas Mroz et al., 2020 used five categories (metropolitan, micropolitan or non-core adjacent to a large or small metropolitan area, micropolitan not adjacent to a metropolitan area, non-core adjacent to micropolitan area, and non-core not adjacent to a metropolitan or micropolitan area). Lastly, Chen et al., 2020 used CMS-grouped U.S. counties31: high utilization, low population density, all other rural areas, and urban areas and Cotton et al., 2017 used the agency location (rural versus metropolitan) with unspecified source.16
Study Sample and Analyses.
Study samples ranged from 132 to 10,202 HHAs and the percent urban ranged roughly from 70% to 83%.14 For those studies using patient-level data, the samples ranged from 3,176 to 1,006,562 Medicare beneficiaries.
Half of the studies (N=6) employed regression analysis of outcomes (with no specific details about the regression analysis),15, 17, 18, 21–23 two used logistic regression analysis,14, 19 one conducted both logistic and multivariate regression analysis across different outcomes,16 one used logistic regression and regression trees,20 and one used descriptive statistics only24. Two-thirds of the studies (N=8)14, 16–19, 21–23 controlled for both patient and agency-level characteristics, whereas the other one third (N=4)15, 20, 24, 25 controlled only for agency-level characteristics. Each of the articles determined significance using p-value <0.05 or less.
Home Health Quality and Access Metrics.
Included studies reviewed five broad categories of quality metrics: home health care utilization, emergency room visits, hospitalization, other care processes and quality of patient care experience. Table 2 provides an overview of each study’s results by these categories of quality metrics and whether the analysis was at the patient or agency level. Supplemental Table 3 provides an in-depth discussion of the results of each study. Next, the results by category are outlined.
Table 2.
Differences in Rural and Urban Home Health Care Agency Quality Metrics
| Patient-Level Quality Metrics | |||||||
|---|---|---|---|---|---|---|---|
| Study | Home Health Care Utilization | Emergency Room Visits | Hospitalizations | Other Care Process | Quality of Patient Care Experience | ||
| Chen 2016 | Urban heart failure patients were more likely to have 30-day preventable hospitalizations. | Rural agencies had lower patient-experience ratings, lower harm prevention scores and lower improvement in activities of daily living. | |||||
| Cotton 2017 |
Mixed results: Rural patients more likely to receive controlled medications. No differences for benzodiazepine and hypnotics. |
||||||
| Falvey 2018 | Rural patients had lower physical therapy utilization after total knee arthroplasty. | ||||||
| Falvey 2020 | Rural patients had fewer rehabilitation visits after a stay in an intensive care unit. | ||||||
| Iyer 2016 | Mixed results: Rural patients received fewer rehabilitation specialists visits. Rural patients received fewer physical therapy visits. No difference in the number of visits after stroke. | ||||||
| Koru 2018 | Rural patients had more ER visits. | Rural patients had more hospitalizations. | |||||
| Rahman 2020 | Rural patients with Alzheimer Disease and Related Dementia had fewer home health care days. | ||||||
| Agency-Level Quality Metrics | |||||||
| Study | Home Health Care Utilization | Emergency Room Visits | Hospitalizations | Other Care Process | Quality of Patient Care Experience | ||
| Chen 2020 | Rural agency patients had more ER visits. | Rural agencies had lower patient-experience ratings, lower harm prevention scores and lower improvement in activities of daily living. | |||||
| Mroz 2018 | Rural agencies more likely to have patients admitted to hospitals. | ||||||
| Mroz 2020 | Rural agencies had smaller percentages of patients utilize home health care services. | ||||||
| Shang 2021 | Mixed results: Urban agencies less likely to provide staff vaccinations on-site or for free and more likely to use cultures to determine infections. Rural agencies more likely to have infection prevention and control policies for patients with central lines. | ||||||
| Smith 2017 | Urban agencies less likely to be top performers. | ||||||
Note: Bold indicates worse access, processes or outcomes. Italics indicates better access, processes or outcomes. Underlined indicates mixed results.
Home health care utilization.
Five studies17–19, 21, 23 examined home health care utilization, which was measured several ways, including: percentage of Medicare beneficiaries using home health care services, the number of home health care visits and episodes (per beneficiary), number of rehabilitation visits delivered (per episode and up to 60 days), types of services delivered by rehabilitation specialists and physical therapists, and percentage of survived days (per month) after initial ADRD diagnosis spent in the community with and without home health care services. Four studies (of 5),17–19, 21 all using older data (pre-2015), consistently found that after controlling for individual and agency-level covariates, rural beneficiaries had significantly lower home health care utilization rates and physical therapy utilization rates. Compared to those in urban areas, rural patients had 6% fewer home health rehabilitation visits after ICU stays, 11% lower physical therapy utilization after total knee arthroplasty, 5.7% fewer visits from rehabilitation specialists. There were no differences found in the number of providers caring for stroke patients across home health care episodes, except for physical therapy services among rural patients were 1.6% lower. In the fifth study25 of stroke patients, also using older data, rural Medicare beneficiaries received fewer visits from rehabilitation specialists, as well as fewer physical therapy visits, but there were no differences in the overall number of visits after risk adjustment.19
Emergency Room Visits.
Two studies focused on emergency room visit rates. Koru et al., 201820 conducted a patient level analysis and Chen et al., 202015 aggregated the data to the agency level. Both found rural patients had more emergency room visits after controlling for confounding variables.
Hospitalizations.
Three studies focused on hospitalizations,20 30-day institutional admissions after discharge,22 and 30-day preventable hospital readmissions (with and without level of illness severity or risk of mortality)14. The results were mixed. Using relatively contemporary data (2015), one study found that rural heart failure patients had significantly lower 30-day preventable readmissions (compared to urban patients) and also that rural patients were less likely to have high illness severity at the 30-day preventable readmission.14 The other two studies that were not limited to a single diagnosis found that rural patients were more likely to be hospitalized after risk adjustment.20, 22
Other Care Processes.
Two studies used unique metrics to determine the quality of HHA services provided. Cotton and colleagues16 were interested in the frequency of use and factors related to opioid analgesics, benzodiazepines, and non-benzodiazepine hypnotics in home health care patients. Shang et al., 202124 looked at infection prevention and control (IPC)-related policies, infrastructure, and procedures as a function of HHA quality. In both of these studies, the results were mixed depending on the outcome variable. Specifically, patients from rural agencies were more likely to receive any class of controlled medications or opioids but there was no difference in benzodiazepine and hypnotics.16 Also, rural agencies outperformed urban agencies in some IPC policies and practices, such as: higher proportions of full-time IPC personnel and patient vaccinations.24
Quality of Patient Care Experience.
Two studies15, 25 used quality measures directly related to the Patient Experience and Quality of Patient Care Star Ratings from Home Health Compare. However, one of these studies removed the measures of influenza and pneumococcal vaccination and timely initiation of care from their analyses25; two of these measures were part of the Quality of Patient Care Star Rating when the quality data were reported. These investigators found that urbanicity was predictive of slightly lower quality for both patient experience of care and care process. Another study15 that assessed several patient experience quality metrics found that rural home health agencies had significantly lower patient-experience star ratings, poorer ADL improvement, and worse harm prevention composite scores compared to urban agencies.
Discussion
This systematic review extends and synthesizes the most current evidence available about differences in the access to and quality of home health care in rural and urban areas across the nation. Quality health services should be effective, safe, patient/family-centered, timely, equitable, integrated, and efficient.32 In this review, we found evidence on access to home health care (i.e., utilization), as well as the effectiveness of the care (i.e., emergency room visits, hospitalizations and other care processes) and its patient/family-centeredness (i.e., quality of patient care experience). Home health care utilization continues to be lower for rural patients compared to those living in urban areas, after controlling for both patient and agency characteristics. This finding supports previous evidence that rural HHAs delivering care have challenges maintaining staffing levels and rural patients do not have the same access to home health care services.4, 7, 33, 34 Rural patients also had more emergency room visits. However, evidence on differences in hospitalizations and rehospitalizations is mixed as is the evidence on other outcomes (e.g., patient experience) and processes (e.g., infection prevention) measured. Nevertheless, our review is aligned with earlier evidence that there are urban and rural differences in access and quality of home health care6, 7, 10 and those differences continue to persist.
Most of the reviewed studies were cross-sectional or cohort studies that used national datasets to examine differences in home health care related to location (i.e., urban versus rural). These datasets and designs capture nationwide trends, which is important. However, the CMS Innovation Center has an ongoing demonstration project to deliver primary care in the home (i.e., the Independence at Home Demonstration).35 Developing other demonstration projects that promote rural patients access to quality home health care services is warranted.
Earlier evidence from the 1990s documented that rural home health care patients were hospitalized and received emergent care significantly more often than urban patients,10 whereas current evidence on urban/rural differences is mixed concerning hospitalizations and admissions but confirms the higher likelihood of emergency room visits for rural compared to urban Medicare beneficiaries. This reduction in disparities related to place of residence is likely due to recent CMS initiatives such as rural add-on payments provided intermittently since 2001,36 Home Health Value-Based Purchasing (HHVBP) implemented in 2016, Patient-Driven Groupings Model (PDGM) in 2020, and other care quality initiatives aimed at improving HHA coverage and reducing preventable hospitalizations. Specifically, rural-add-on payments have been directed at services and care provided to home health care patients living in rural and marginalized communities. These incentives have been intermittently applied to home health episodes provided in rural areas.36 Research on rural add-on payments from 2002-2017 suggests that higher payments (5-10%) make a significant difference in rural HHA coverage, whereas lower payments (3% or less) do not significantly affect HHA utilization in rural areas.15, 21 Unfortunately for HHAs and rural patients, the most recent payment incentives enacted through the Bipartisan Budget Act of 2018 will gradually phase out from 2020 to 2022, and no rural add-ons will be paid to HHAs in 2023 unless new legislation is enacted.21 Given the prior market response, it is possible that without rural add-on payments, access to home health care for patients living in rural areas will be negatively impacted and rural patients’ health will suffer.
Additionally, very few recent studies examine urban and rural differences in the overall quality of home health care and patient experiences. The lack of past and present evidence can partially be explained by how hard it is to measure home health care quality and experience adequately across urban and rural settings. HHAs often provide services to both urban and rural beneficiaries.4 The AHRF provides county-level data about the number of home health care providers servicing each county. Currently, there are no publicly available datasets with information on agency-level coverage areas, but Home Health Compare does ask users to enter in their zip code, city or state to reveal a list of agencies in their area. However, this information does not guarantee that the agency coverage area overlaps with patient place of residence. For that reason, it is challenging for researchers to map patient place of residence (i.e., zip code, county) to the coverage area of an agency; patient zip code is only available through Medicare data.37 Researchers conducting prospective intervention trials or qualitative inquiries, of course, should not have these problems.
Furthermore, measurement of rurality continues to be commonly dichotomized as urban versus rural, even though funders have encouraged the use of more descriptive, refined categories to capture rural diversity. Furthermore, more refined measures exist (such as Medicare CBSA codes18 for residence, UIC from AHRF,19 Rural-Urban Continuum Codes,22); in 2007, Vanderboom and Madigan urged the use of more refined measurement of rurality.38 Our review included only a few articles in the last 10 years that used a non-binary, more refined variable for rurality to compare urban and rural differences. This emphasizes the continuing need for home health care researchers to use refined categories to better uncover and address health disparities and vulnerable populations. Use of broad rurality categories likely contributed to the mixed results found in this review.
Our study has limitations. First, as is common in systematic reviews that use a search range including year, our review includes articles based on older data; specifically, our review includes some data from 2009 and up through 2018. Studies in which important urban and rural comparisons were not the main focus may have been missed, and therefore were not apparent in either the title or abstract. Also, no studies were identified that reported null findings for urban and rural differences which may suggest publication bias. Furthermore, the identified literature on rural and urban differences in care provided by HHAs was sparse (with 12 included studies), and as such, the evidence is emerging. With the number of relevant studies being small, it limits the strength of our conclusions, but highlights the need for more research.
Conclusions and Implications
Our study importantly identifies articles that focus on urban and rural comparisons related to services and care provided by HHAs. Our review identifies several gaps in the evidence that need further study. The variables used to measure the access to and quality of care by HHAs varied so there was no consensus for any given quality of care metric. Instead, our review helped paint a detailed, descriptive picture of care quality outcomes provided by rural HHAs compared to those in urban areas. The variables used to assess urban and rural location of the HHAs were also not consistent, but those articles that utilized more granular measures of rural location revealed more differences. We recommend that the more granular measures of rurality are used in future research. Additionally, while disparities in rehospitalizations related to place of residence have narrowed in recent years, it is unknown if those improvements will endure once CMS initiatives, like rural add-on payments, lapse or are reduced in intensity. With the changes that are occurring, future evaluation of these policy changes are recommended. Additionally, with the difficulties in measuring the quality of home health care and the patient experience, we recommend that consistent metrics be developed as well as prospective intervention trials and qualitative inquiries be conducted to better examine these issues. Lastly, access to home health care services is important for rural patients with chronic conditions or disability; CMS should better support quality home health care services for rural patients. Furthermore, clinicians seeing rural patients should advocate for the services needed.
Supplementary Material
Acknowledgements:
We acknowledge the library staff that assisted with conducting the search and retrieval of articles.
Funding:
This work was supported by the National Institutes of Health: National Institute of Nursing Research and the Office of the Director (R01NR016865) and the Alliance for Home Health Quality and Innovation (AHHQI).
Footnotes
Conflicts of interest: All authors declare there are no conflicts of interest.
References
- 1.Centers for Medicare and Medicaid Services. Home Health Services. Centers for Medicare and Medicaid Services. Accessed December 1, 2021. https://www.medicare.gov/coverage/home-health-services [PubMed]
- 2.Medicare Payment and Advisory Commission (MedPAC). Report to Congress: Medicare Payment Policy, Chapter 9: Home Health Care Services. 2019. Accessed December 15, 2021. https://www.medpac.gov/document/http-www-medpac-gov-docs-default-source-reports-mar20_medpac_ch9_sec-pdf/
- 3.Nelson JA, Stover Gingerich b. Rural Health: Access to Care and Services. Home Health Care Management & Practice. 2010;22(5):339–343. [Google Scholar]
- 4.Skillman S, Patterson D, Coulthard C, Mroz T. Access to rural home health services: views from the field. Final Report #152. Seattle, WA: WWAMI Rural Health Research Center, University of Washington. 2016. [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. Report to Congress: Medicare home health study: An investigation on access to care and payment for vulnerable patient populations. Washington, DC: L&M Policy Research. 2021. Accessed January 06, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/Downloads/HH-Report-to-Congress.pdf [Google Scholar]
- 6.Probst J, Towne S, Mitchell J, Bennett K, Chen R. Home health care agency availability in rural counties. Columbia, SC: South Carolina Rural Health Research Center, Rural and Minority Health Research Center. 2014. [Google Scholar]
- 7.Sutton JP. Patterns of post-acute utilization in rural and urban communities: Home health, skilled nursing, and inpatient medical rehabilitation. Bethesda, MD: NORC Walsh Center for Rural Health Analysis. 2005. [Google Scholar]
- 8.Toth M, Holmes M, Van Houtven C, Toles M, Weinberger M, Silberman P. Rural Medicare Beneficiaries Have Fewer Follow-up Visits and Greater Emergency Department Use Postdischarge. Med Care. Sep 2015;53(9):800–8. doi: 10.1097/MLR.0000000000000401 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services. Medicare and Medicaid Programs; CY 2019 Home Health Prospective Payment System Rate Update and CY 2020 Case-Mix Adjustment Methodology Refinements; Home Health Value-Based Purchasing Model; Home Health Quality Reporting Requirements; Home Infusion Therapy Requirements; and Training Requirements for Surveyors of National Accrediting Organizations. Final rule with comment period. Fed Regist. Nov 13 2018;83(219):56406–638. [PubMed] [Google Scholar]
- 10.Shaughnessy PW, Schlenker RE, Crisler KS, Arnold AG, Powell MC, Beaudry JM. Home care: moving forward with continuous quality improvement. J Aging Soc Policy. 1996;7(3–4):149–67. doi: 10.1300/J031v07n03_09 [DOI] [PubMed] [Google Scholar]
- 11.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. Jul 21 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. Jul 21 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bronson WH, Kingery MT, Hutzler L, et al. Lack of Cost Savings for Lumbar Spine Fusions After Bundled Payments for Care Improvement Initiative. Spine. 2018;44(4):298–304. [DOI] [PubMed] [Google Scholar]
- 14.Chen HF, Carlson E, Popoola T, Suzuki S. The Impact of Rurality on 30-Day Preventable Readmission, Illness Severity, and Risk of Mortality for Heart Failure Medicare Home Health Beneficiaries. J Rural Health. Spring 2016;32(2):176–87. doi: 10.1111/jrh.12142 [DOI] [PubMed] [Google Scholar]
- 15.Chen HF, Landes RD, Schuldt RF, Tilford JM. Quality Performance of Rural and Urban Home Health Agencies: Implications for Rural Add-On Payment Policies. J Rural Health. Jun 2020;36(3):423–432. doi: 10.1111/jrh.12415 [DOI] [PubMed] [Google Scholar]
- 16.Cotton BP, Lohman MC, Brooks JM, et al. Prevalence of and Factors Related to Prescription Opioids, Benzodiazepines, and Hypnotics Among Medicare Home Health Recipients. Home Healthc Now. Jun 2017;35(6):304–313. doi: 10.1097/NHH.0000000000000553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falvey JR, Bade MJ, Forster JE, et al. Home-Health-Care Physical Therapy Improves Early Functional Recovery of Medicare Beneficiaries After Total Knee Arthroplasty. J Bone Joint Surg Am. Oct 17 2018;100(20):1728–1734. doi: 10.2106/JBJS.17.01667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falvey JR, Murphy TE, Gill TM, Stevens-Lapsley JE, Ferrante LE. Home Health Rehabilitation Utilization Among Medicare Beneficiaries Following Critical Illness. J Am Geriatr Soc. Jul 2020;68(7):1512–1519. doi: 10.1111/jgs.16412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iyer M, Bhavsar GP, Bennett KJ, Probst JC. Disparities in home health service providers among Medicare beneficiaries with stroke. Home Health Care Serv Q. Jan-Mar 2016;35(1):25–38. doi: 10.1080/01621424.2016.1175991 [DOI] [PubMed] [Google Scholar]
- 20.Koru G, Parameshwarappa P, Alhuwail D, Aifan A. Facilitating Focused Process Improvement Efforts in Home Health Agencies to Improve Utilization Outcomes Effectively and Efficiently. Home Health Care Management & Practice. 2018;30(3):122–129. [Google Scholar]
- 21.Mroz T, Garberson L, Wong J, et al. Variation in Use of Home Health Care among Fee-for-Service Medicare Beneficiaries by Rural-Urban Status and Geographic Region: Assessing the Potential for Unmet Need. Policy Brief #169. Seattle, WA: WWAMI Rural Health Research Center, University of Washington. 2020. [Google Scholar]
- 22.Mroz TM, Meadow A, Colantuoni E, Leff B, Wolff JL. Home Health Agency Characteristics and Quality Outcomes for Medicare Beneficiaries With Rehabilitation-Sensitive Conditions. Arch Phys Med Rehabil. Jun 2018;99(6):1090–1098 e4. doi: 10.1016/j.apmr.2017.08.483 [DOI] [PubMed] [Google Scholar]
- 23.Rahman M, White EM, Thomas KS, Jutkowitz E. Assessment of Rural-Urban Differences in Health Care Use and Survival Among Medicare Beneficiaries With Alzheimer Disease and Related Dementia. JAMA Netw Open. Oct 1 2020;3(10):e2022111. doi: 10.1001/jamanetworkopen.2020.22111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shang J, Chastain AM, Perera UGE, et al. The state of infection prevention and control at home health agencies in the United States prior to COVID-19: A cross-sectional study. Int J Nurs Stud. Mar 2021;115:103841. doi: 10.1016/j.ijnurstu.2020.103841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith LM, Anderson WL, Lines LM, et al. Patient experience and process measures of quality of care at home health agencies: Factors associated with high performance. Home Health Care Serv Q. Jan-Mar 2017;36(1):29–45. doi: 10.1080/01621424.2017.1320698 [DOI] [PubMed] [Google Scholar]
- 26.Data.gov. Provider of Services File - Hospital & Non-Hospital Facilities. Centers for Medicare & Medicaid Services. Accessed August 2, 2022. https://catalog.data.gov/dataset/provider-of-services-file-hospital-non-hospital-facilities-f216f [Google Scholar]
- 27.United States Census Bureau. Within Metropolitan and Micropolitan. United States Census Bureau. Accessed August 2, 2022. https://www.census.gov/programs-surveys/metro-micro/about.html [Google Scholar]
- 28.USDA Economic Research Service. Rural-Urban Continuum Codes. U.S. Department of Agriculture. Accessed August 2, 2022. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx [Google Scholar]
- 29.USDA Economic Research Service. Urban Influence Codes. U.S. Department of Agriculture. Accessed August 2, 2022. https://www.ers.usda.gov/data-products/urban-influence-codes.aspx [Google Scholar]
- 30.Health Resources & Services Administration. Area Health Resources Files. Health Resources & Services Administration. Accessed August 2, 20222. https://data.hrsa.gov/topics/health-workforce/ahrf [Google Scholar]
- 31.Centers for Medicare & Medicaid Services. CY 2019 Medicare Home Health Prospective Payment System (HH PPS) rates and wage index for calendar year (CY) 2019. Centers for Medicare & Medicaid Services. Accessed August 2, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/Home-Health-Prospective-Payment-System-Regulations-and-Notices-Items/CMS-1689-P?DLPage=1&DLEntries=10&DLSort=2&DLSortDir=descending [Google Scholar]
- 32.Rabiner DJ, Arcury TA, Howard HA, Copeland KA. The perceived availability, quality, and cost of long-term care services in America. J Aging Soc Policy. 1997;9(3):43–65. doi: 10.1300/J031v09n03_03 [DOI] [PubMed] [Google Scholar]
- 33.Davitt JK, Choi S. The impact of policy on nursing and allied health services. Lessons from the Medicare Home Health Benefit. Res Gerontol Nurs. Jan 2008;1(1):4–13. doi: 10.3928/19404921-20080101-03 [DOI] [PubMed] [Google Scholar]
- 34.Brassard A Removing Barriers to Advanced Practice Registered Nurse Care: Home Health and Hospice Services. Vol. 66. 2012. Insight on the Issues. Accessed January 8, 2022. http://campaignforaction.org/sites/default/files/Removing-Barriers-Home-Hospice.pdf [Google Scholar]
- 35.Centers for Medicare and Medicaid Services. Synthesis of Evaluation Results across 21 Models, 2012–2020. 2021. Baltimore MD: Centers for Medicare and Medicaid Services Innovation Center. Accessed August 5, 2022. https://innovation.cms.gov/data-and-reports/2022/wp-eval-synthesis-21models [Google Scholar]
- 36.Mroz TM, Patterson DG, Frogner BK. The Impact Of Medicare’s Rural Add-On Payments On Supply Of Home Health Agencies Serving Rural Counties. Health Aff (Millwood). Jun 2020;39(6):949–957. doi: 10.1377/hlthaff.2019.00952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Medicare Payment and Advisory Commission (MedPAC). Report to Congress: Medicare Payment Policy, Chapter 8: Home Health Care Services. 2021. Accessed March 21, 2022. https://www.medpac.gov/wp-content/uploads/2021/10/mar21_medpac_report_ch8_sec.pdf [Google Scholar]
- 38.Vanderboom CP, Madigan EA. Federal definitions of rurality and the impact on nursing research. Res Nurs Health. Apr 2007;30(2):175–84. doi: 10.1002/nur.20194 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


