Abstract
Objectives
The aims were to explore the nature of methods/techniques applied to improve adherence to physical activity (PA) and exercise in people with inflammatory arthritis and to identify whether studies were theory based and/or used behaviour change techniques (BCTs).
Methods
Searches were undertaken of English language articles within four databases: Embase, Medline, PsycINFO and Cochrane. Articles were included if they assessed adherence to a PA and/or exercise intervention. A narrative synthesis of the findings is reported.
Results
Of 1909 studies screened, 18 studies met inclusion criteria. Adherence was most frequently included as a secondary outcome. Reporting of adherence measures was poor, in that 13 studies did not use a validated measure of adherence, with only three validated measures being identified. The majority of studies were not theory driven (n = 13), although the health belief model was the most used theoretical framework (n = 5). Only two studies mentioned both theory and BCTs. Four studies reported components that were mapped onto BCTs, with goal setting being the most prevalent.
Conclusion
This scoping review found that adherence to PA and/or exercise interventions was rarely the focus of research, despite its importance in maintaining health in people with inflammatory arthritis. Where research has been conducted in this area, serious shortcomings were revealed, in that psychological theory, evidence-based BCTs derived from theory and valid adherence measures were not used to inform intervention design and target adherence, meaning that interventions were suboptimal. These results suggest that there is considerable room for improvement and that more high-quality research is required to investigate determinants of adherence and develop impactful interventions.
Keywords: adherence, exercise, measurement, musculoskeletal, physical activity, scoping review
Key messages.
Adherence to physical activity and exercise interventions is rarely the focus of research, despite the importance of this to maintaining health in people with inflammatory arthritis.
Most studies do not use psychological theory and evidence-based behaviour change techniques to inform intervention design.
Reporting of intervention components is poor, and most studies do not use validated measures of adherence.
Introduction
Physical activity (PA) and exercise (defined as planned, purposeful PA, designed to improve or maintain physical fitness) are key management strategies for people with inflammatory arthritis (including SpA, RA and PsA). People with inflammatory arthritis are advised to complete ≥150 min of moderate-intensity PA per week, with strengthening and flexibility exercises twice a week [1–3], but adherence to this guidance is often low [4–6]. The World Health Organization (WHO) defines adherence as ‘the extent to which a person’s behaviour corresponds with agreed recommendations from a healthcare provider’ [7]. However, this definition has been refined for exercise adherence by Frost et al. [8] as ‘the extent to which individuals undertake a prescribed behaviour accurately and at the agreed frequency, intensity and duration’. Adherence to PA and exercise can be difficult to measure, and much of the evidence base does not assess adherence as a primary outcome, but only as a secondary outcome [9].
There are particular barriers to participation in PA and exercise for people with inflammatory arthritis, and many spend the majority of their time engaged in sedentary behaviour, meaning that non-adherence is a significant challenge [10–12]. Patients’ perceptions of facilitators and barriers to PA and exercise need to be understood better, and interventions need to be more tailored to address individual determinants of this behaviour [13]. Recent research suggests barriers and facilitators in people with inflammatory arthritis are related to psychological status, social support, disease level and environmental factors [14]. However, a more in-depth understanding of adherence to PA and exercise is required, because there was poor adherence to this even among those who had high adherence to medication [15].
Several studies have been designed to address this problem using interventions such as exercise prescription, patient education and behavioural counselling. However, systematic reviews of interventions have revealed variable levels of success, with limited exploration of the methods/techniques used to assess adherence [16–19]. Furthermore, it is difficult to determine which aspects of these interventions were effective or how and why they might have worked, because most have not applied theory or tested fidelity [20]. Poor reporting of intervention design makes it difficult to draw conclusions about the effectiveness of theory or to assess whether the correct theory was chosen [21]. Few studies have described using evidence-based behaviour change techniques (BCTs) [22], and psychological theory has not been used to inform selection of behavioural change targets [23, 24].
Many interventions to increase PA and exercise in people with inflammatory arthritis have demonstrated limited application of psychological theory and/or poor reporting, making it difficult to draw conclusions about the best strategies to use [20]. A scoping review, defined as ‘a form of knowledge synthesis that addresses an exploratory research question aimed at mapping key concepts, types of evidence, and gaps in research related to a defined area or field by systematically searching, selecting and synthesizing existing knowledge’ [25], is therefore appropriate for inflammatory arthritis, because this can examine how research is conducted on a certain topic or field, identify key characteristics or factors related to a concept and analyse knowledge gaps [26].
The objectives of this scoping review were to explore the nature of techniques/methods applied to improve adherence to PA and/or exercise in people with inflammatory arthritis and to identify whether studies were theory based and/or used BCTs.
Methods
The PRISMA Extension for Scoping Reviews (Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)-ScR) [27, 28] was followed and reported accordingly (see Supplementary Table S1, available at Rheumatology Advances in Practice online). A protocol for this scoping review has not been published because it was not eligible for registration on Prospero.
Search strategy
Search terms included adapted MeSH, keyword and wild card terms located in the title or abstract that reflected disease and outcome (e.g. adherence/compliance to physical activity/exercise) taken from two previous systematic reviews on a similar topic of interest [19, 29] (see Supplementary Data S2, available at Rheumatology Advances in Practice online, for full search strategy). Studies were retrieved by searching electronic databases [MEDLINE, PsychINFO, EMBASE, and Cochrane Central Register of Controlled Trials (CENTRAL)]. Databases were searched from conception to 18 January 2022. All search results (titles and abstracts) were exported into Rayyan software to be stored during the screening process.
Eligibility criteria
Articles were included if they assessed adherence to a PA and/or exercise intervention. A full list of inclusion and exclusion criteria for study inclusion is shown in Table 1 using the population, intervention, comparison, outcome(s) and study design framework.
Table 1.
Eligibility criteria for considering studies for this review
| Parameter | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population |
|
|
| Intervention |
|
No physical activity or exercise intervention clearly described |
| Comparison | Not applicable: studies with or without comparison groups included | |
| Outcomes |
|
|
| Study design | Randomized controlled trials, quasi-experimental trials, prospective cohort studies, retrospective cohort analyses and before–after trials that reported baseline and follow-up measurements of adherence to physical activity and/or exercise or physical activity/exercise levels in at least two groups, including qualitative |
|
Data collection and analysis
Selection of studies
Primary screening was undertaken by the first coder (H.C.), with a random sample of 10% of studies cross-checked by a second coder (M.S.) at the screening stage, which resulted in a 0.90 kappa level of agreement (strong) between the two coders (3) because there were only four discrepancies. Raters discussed discrepancies and reached agreement on the final studies included for the review.
Data extraction and analysis
With the use of a study-specific data extraction table, information about each study (e.g. author, year of publication, country, study design), patient population, description of the intervention, details of adherence assessment (e.g. adherence measurement, validation and study outcome type) and involvement of theory or BCTs were extracted by the first coder (H.C.). A random sample of 10% of studies were extracted by a second coder (M.S.). Only published data have been extracted, with no further data requests or confirmation from study authors undertaken.
A narrative synthesis is presented to describe the methodology used to assess adherence to PA and/or exercise interventions with descriptive statistics [31, 32]. Depending on the studies meeting inclusion, a mapping of the theory used and BCTs was also undertaken [22]. Given that the required data concerned methodology and reporting, there was no differentiation in how the data from either qualitative and quantitative studies were dealt with. A quality assessment or critical appraisal was not conducted, because the aim of this scoping review was to examine how research is conducted on adherence to PA and/or exercise interventions, to identify key characteristics or factors related to adherence assessment and to analyse knowledge gaps [31].
Results
Study selection
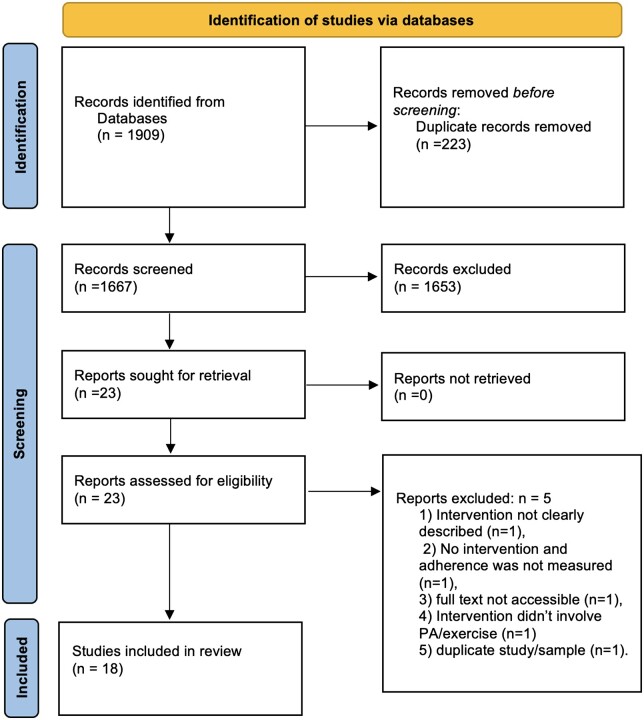
Combined searches yielded a total of 1909 citations, of which 1676 remained after removal of duplicates, with 23 studies meeting inclusion at the title/abstract screening stage (Fig. 1). At full-text screening and data extraction, 18 achieved final inclusion, with five studies being excluded for the following reasons: intervention not clearly described (n = 1); no intervention, and adherence was not measured (n = 1); full text not accessible (n = 1); intervention did not involve PA/exercise (n = 1); and duplicate study/sample (n = 1).
Figure 1.
PRISMA flowchart
Study characteristics
As shown in Table 2, the majority of included studies investigated RA (n = 12, 66.7%), mainly from Europe and UK (n = 13, 72.2%), with all studies published between 1999 and 2022. A variety of study designs were used, but the most common were randomized controlled trials or cross-over trials (n = 4, 22.2%). The sample size ranged from 14 to 328, with a median size of 42.5, with most studies (n = 14, 77.8%) representing a female majority of participants and with average age ranging from 21.54 to 63.6 years.
Table 2.
Characteristics of included studies (n = 18)
| Reference | Year | Country | Musculoskeletal population | Study type | Sample size | Age (years) | Female [n (%)] |
|---|---|---|---|---|---|---|---|
| [33] | 2014 | The Netherlands | Broad musculoskeletal (JIA, FM, RA, SpA and SLE) | Feasibility study | 19 | 21.54 (range 17–25) | 16 (84.2) |
| [34]a | 2021 | Norway and Sweden | SpA | RCT (secondary analysis) | 100 | 46.2 (range 23–69) | 53 (53) |
| [35]a | 2020 | Sweden | SpA | Qualitative analysis following RCT | 14 | 53 (range 24–63) | 5 (35.7) |
| [36] | 2014 | Italy | PsA | Observational cohort study | 30 | 50.8 (s.d. 9.5) | 12 (40) |
| [37] | 2009 | The Netherlands | RA | Observational study as long-term follow-up of RCT | 71 | 56 (IQR 15) | 61 (86) |
| [38]a | 2004 | UK | RA | Follow-up of cross-over trial | 127 | Not reported | 97 (76.4) |
| [39]a | 1999 | UK | RA | Single-blind cross-over trial | 35 | 55.17 (range 33–69) | 29 (82.9) |
| [40]a | 1999 | UK | RA | Repeated measures, cohort design | 21 | 48.95 (range 22–70) | 17 (81) |
| [41] | 2007 | France | RA | RCT | 208 | 54.7 (s.d. 13.1) | 185 (88.9) |
| [42] | 2017 | USA | OA or RA | Qualitative analysis following pilot study | 30 | 50 (range 32–69) | 28 (93) |
| [43] | 2001 | Canada | RA | Pre–post experimental design | 10 | 54 (s.d. 10) | 10 (100) |
| [44]a | 2017 | UK | RA | Qualitative analysis following RCT | 14 | 61.4 (range 44–82) | 9 (64.3) |
| [45] | 2013 | Switzerland | SpA | RCT | 106 | 48.85 (s.d. 12.16) | 38 (35.8) |
| [46] | 2015 | Sweden | RA | Observational cohort study | 220 | 59 (s.d. 8.8.) | 178 (81) |
| [47] | 2020 | China | SpA | Cross-sectional study | 259 | 33 (s.d. 17) | 69 (26.6) |
| [48] | 2022 | USA | RA | Pilot RCT | 50 | 56.1 (s.d. 11) | 46 (92) |
| [49] | 2017 | New Zealand | RA | Assessor‐blinded, two‐arm pilot RCT | 26 | 54 (range 29–73) | 25 (96) |
| [50]a | 2017 | UK | RA | RCT, follow-up | 328 | 63.6 (s.d. 10.9) | 248 (75.6) |
Same research group/study but difference in samples and reporting.
IQR: interquartile range; RCT: randomized controlled trial; SpA: spondyloarthritis (axial or ankloysing).
Synthesis of results from individual studies
Details of interventions, adherence assessments, theory and BCTs for each included study are presented in Table 3. A wide range of 14 interventions were described across the 18 studies, with most following physiotherapist- or occupational therapist-supervised moderate- to high-intensity exercise programmes (n = 5, 35.7%) or using predominantly education-based programmes (n = 4, 28.6%). Only one intervention was delivered exclusively online [32], with other interventions incorporating dance-based exercise [43] and Nordic walking [45] as PA and/or exercise.
Table 3.
Details of interventions, adherence assessments, theory and behaviour change techniques from included studies (n = 19)
| Reference | Intervention | Adherence measurement | Measure validated | Type of outcome | Associated behaviour change techniques | Theory involved |
|---|---|---|---|---|---|---|
| [33] | Online programme consisting of three e-Health applications, including a chat section, home exercises and a discussion board | Adherence to the programme was measured after completing the programmes by describing how many people had completed the whole course. Also, each participant’s presence during the chats on the discussion board and finishing the exercises of the online programme were measured (frequencies reported) | No | Secondary outcome | Goal setting (unspecified) | No |
| [34]a | Three-month physiotherapist-supervised high-intensity exercise programme | Exercise adherence was recorded by the physiotherapist as attendance at the supervised sessions and as accomplishment of the individual session of personal choice by inspection of the pulse watch. Exercise adherence was also self-reported by the participants in a personal exercise diary to enhance motivation. Reported as the percentage who followed ≥80% of the prescribed exercise protocol | No | Secondary outcome | No | Health beliefs model, because exercise health beliefs were the primary outcome |
| [35]a | Three-month physiotherapy supervised high-intensity exercise programme | Reported as the percentage who followed ≥80% of the prescribed exercise protocol | No | Secondary outcome | No | No |
| [36] | Exercise programme delivered by a single physiotherapist, with leaflets to facilitate correct performance of the exercises | Self-reported rates of adherence to a home-based programme of exercises (percentage) | No | Feasibility outcome | No | No |
| [37] | Two-year supervised high-intensity exercise programme | At 18 months of follow-up, all participants completed a 10-item questionnaire comprising questions on frequency, intensity and compliance with exercises, and the reasons for not continuing the participation in the RAPIT group and choice of an alternative if applicable. Patients reporting participation in extended RAPIT groups or other classes were asked to give the name of their supervisor, and their participation was checked with the lists of participants available from the providers | No | Primary outcome | No | No |
| [38]a | The JP group education programme consisted of four weekly 2-h sessions, plus an optional home visit within 2 weeks of the end of the programme. It was led by an experienced rheumatology occupational therapist covering RA, drug treatments, diet, exercise, pain management, relaxation and joint protection | Joint protection behaviour assessment: performances of 20 tasks when making a hot drink and snack meal were assessed as incorrect, partly correct or correct joint protection methods, with scores converted to percentages. A higher score indicates increased adherence | Yes | Primary outcome | No | Educational, behavioural, motor learning and self-efficacy enhancing strategies to increase adherence |
| [39]a | The JP group education programme consisted of four weekly 2-h sessions, plus an optional home visit within 2 weeks of the end of the programme. It was led by an experienced rheumatology occupational therapist covering RA, drug treatments, diet, exercise, pain management, relaxation and joint protection | Joint protection behaviour assessment: performances of 20 tasks when making a hot drink and snack meal were assessed as incorrect, partly correct or correct joint protection methods, with scores converted to percentages. A higher score indicates increased adherence | Yes | Primary outcome | Instruction on how to perform the behaviour, demonstration of the behaviour, feedback on behaviour, problem-solving, habit formation, goal setting (behaviour), behavioural contract and social support (unspecified), credible source (an experienced rheumatology therapist delivered intervention), information about health consequences, verbal persuasion about capability, behaviour practice/rehearsal, self-monitoring of behaviour | Group education programme was developed using the health belief model and self-efficacy theory |
| [40]a | The JP group education programme consisted of four weekly 2-h sessions, plus an optional home visit within 2 weeks of the end of the programme. It was led by an experienced rheumatology occupational therapist covering RA, drug treatments, diet, exercise, pain management, relaxation and joint protection | Joint protection behaviour assessment: performances of 20 tasks when making a hot drink and snack meal were assessed as incorrect, partly correct or correct joint protection methods, with scores converted to percentages. A higher score indicates increased adherence | Yes | Primary outcome | Instruction on how to perform the behaviour, demonstration of the behaviour, feedback on behaviour and problem-solving, behaviour practice/rehearsal, habit formation, information about health consequences | No |
| [41] | The active group received a multidisciplinary education programme, including training in home-based exercises and guidelines for leisure physical activity. The control group received a booklet added to usual medical care |
|
No | Primary outcome | No | No |
| [42] | Eight-week group hatha yoga programme | Number completing intervention (not necessarily attending all sessions) | No | Feasibility outcome | No | No |
| [43] | The dance-based exercise programme was developed and led by a physical fitness instructor in collaboration with an occupational therapist and a physical therapist. Each training session included four phases, all taking place to musical arrangements: warm-up, aerobic exercise, recovery and cool-down. The dance-based exercise period was made up of slow movements, creating a rhythmic pattern that involved all joints | Compliance measured as rate of participation in sessions (descriptive) | No | Feasibility outcome | No | No |
| [44]a | Individually tailored moderate- to high-intensity strengthening and stretching exercises over five sessions with an occupational therapist or physiotherapist |
|
No | Secondary outcome | Goal setting (unspecified) and behavioural contract | Educational behavioural model based on the health beliefs model |
| [45] | The training group performed a 12-week supervised Nordic walking training for 30 min twice a week using individually monitored, moderate-intensity heart rate levels | Based on the physiotherapists’ protocols for group adherence and on the participants’ diaries, the percentage who performed at least three training units per week (i.e. two Nordic walking training sessions and one additional unsupervised cardiovascular training unit) | No | Feasibility outcome | No | No |
| [46] | Three main components constituted the intervention programme: (i) at least moderate-intensity physical activity for ≥30 min on most days of the week; (ii) at least two weekly 45 min circuit training sessions, including both muscle strength training (50–80% of one repetition maximum, 3–10 repetitions) and aerobic exercises (60–85% of maximal heart rate); and (iii) biweekly support group meetings | Two text messages were sent once each week to collect data on the number of days during the past week that participants performed circuit training sessions and on how many additional days of the past week they performed at least moderate-intensity physical activity for ≥30 min. Support group meeting attendance was registered by the coaches. Participants were categorized into adherers and non-adherers based on 50, 70 and 90% participation in circuit training sessions, total HEPA and support group meetings, respectively | Yes (EMA) | Secondary outcome | No | No |
| [47] | Educated with the types of back exercise and the importance of adhering to standard exercise therapy by rheumatologists | Exercising for ≥30 min per day and performing back exercise on ≥5 days per week were defined as adherence to the standard exercise therapy | Yes | Secondary outcome | No | No |
| [48] | Twelve-session group programme covering pain coping skills, lifestyle behavioural weight loss plus supervised exercise sessions three times per week | Descriptive statistics (percentage) | No | Feasibility outcome | No | No |
| [49] | An 8‐week programme of group and home yoga practice. Group practice consisted of once‐weekly 75‐min yoga classes, conducted by a qualified yoga instructor and class assistant. Home practice consisted of a 20‐min guided relaxation, based on the relaxation technique practised in the group sessions. A CD, recorded by the yoga instructor, was provided. Participants were asked to practise three times per week, at a time and day of their choice | Protocol adherence (a priori level of 6/8 group classes and 16/24 home classes acceptable). Adherence to home practice in the previous week was reported verbally to the yoga instructor at the beginning of each session, and barriers and adherers to home practice were discussed among the group | No | Feasibility outcome | No | No |
| [50]a | Individually tailored moderate- to high-intensity strengthening and stretching exercises over five sessions with an occupational therapist or physiotherapist | To assess adherence to the exercise programme, all participants were asked to report how often they performed hand exercises for their RA (frequency, percentage) | No | Secondary outcome | No | Educational behavioural model based on the health beliefs model |
Same research group/study but difference in samples and reporting.
Adherence was most frequently included as a secondary outcome (n = 7, 38.9%), with only five studies reporting it as their primary outcome (27.8%). Most studies used the term adherence, with three studies using the term compliance (16.6%). Reporting of adherence measures was poor, with most studies not using a validated measure of adherence (n = 13, 72.2%), typically using a study-specific measure (n = 9, 69.2%) or simply presenting a descriptive statistic (usually a percentage or frequency) of those completing the intervention/course (n = 4, 30.8%), often only in the Discussion. The validated measures of adherence were as follows: joint protection behaviour assessment [38–40]; using ecological momentary assessment to capture frequency data alongside group attendance [46]; and a definition of adherence to standard exercise therapy stated as exercising for ≥30 min per day and performing back exercise on ≥5 days per week based on previous literature [47].
The majority of studies were not theory driven (n = 13, 72.2%); however, of those five that mentioned theory, all used the health belief model as the theoretical framework, either explicitly mentioned, alluded to or in conjunction with self-efficacy theory. Only two studies mentioned both theory and BCTs (10.5%) [39, 44]. Four studies in total (21%) mentioned components that can be mapped onto BCTs [33, 39, 40, 44], although they did not use the terminology of BCTs, ranging from 1 to 13 BCTs (median = 4.5) across studies, with goal setting the most common (n = 3, 75%).
It is important to note that three studies/interventions were exemplified across seven papers [34, 35, 38–40, 44, 50], with some papers representing follow-up (both qualitatively and quantitatively). This is particularly significant given that Hammond et al. [38–40] assessed adherence in a more theory-driven and rigorous way, with the use of BCTs to inform their intervention, compared with the rest of the literature. However, the level of detail in reporting was inconsistent across publications for the same/similar studies, particularly regarding theory usage, reporting of BCTs and interventions.
Discussion
Summary of evidence
Eighteen studies met inclusion criteria and had data extracted and analysed as part of this scoping review. A narrative synthesis was completed to describe the methodology used to assess adherence to PA and/or exercise interventions using descriptive statistics. Interestingly, adherence was reported as a primary outcome in only five studies and was most frequently included as a secondary outcome. Although the term adherence was used most commonly, reporting of adherence measures was poor, with most studies not using validated measures of adherence. In addition, many studies did not underpin interventions with theory, and the five that did all used the health belief model, sometimes in combination with self-efficacy theory. Four studies mentioned components that could be mapped onto BCTs [33, 39, 40, 44], although they did not always apply proper BCT terminology, ranging from 1 to 13 BCTs across studies. Goal setting was the most commonly used BCT, but only one paper [39] specified that goal-setting behaviour was used, whereas two others [33, 44] did not specify whether goal-setting behaviour or outcome was used. However, there was inconsistent reporting of this across publications, even within the same or similar studies, particularly regarding theory usage and reporting of BCTs and intervention components.
The scoping review reported similar shortcomings to Fenton et al. [20], because limited application of psychological theory and/or poor reporting made it difficult to draw conclusions about the best strategies to use to increase adherence to PA and exercise in people with inflammatory arthritis. However, this scoping review has added to the existing literature and advanced understanding by finding that psychological theory and evidence-based BCTs derived from theory have not been engaged to inform intervention design and target adherence. Furthermore, the included research did not distinguish between the initiation and maintenance of PA or exercise, which might be influenced by different determinants, and importantly, most studies did not use a validated measure of adherence.
Implications of the scoping review
There are implications of this review for both researchers and clinicians. It is clear that researchers need to design interventions that are theory based, then to identify the specific BCTs impacting on PA- or exercise-adherent behaviour in order to change this behaviour, if they are to be effective [51]. There is also potential to improve future studies by using valid and reliable measures of adherence as primary or secondary outcomes; for example, the exercise adherence rating scale (EARS) [24, 52]. This measure has been widely validated, used across different populations and translated into several languages [53–55]. Clinicians could be trained to use effective BCTs [56] and could also use brief measures, such as the EARS, to improve and assess the success of their treatment, because adherence to PA and exercise is an important issue for people with inflammatory arthritis [11, 15].
Strengths and limitations
An important strength of this scoping review was that it followed the PRISMA Extension for Scoping Reviews (PRISMA-ScR) process [27, 28]. In addition, to check for accuracy, a random sample of 10% of studies was extracted by a second coder (M.S.). One of the limitations of this scoping review is that no quality appraisal of studies was completed. However, this was not relevant to the aims of this scoping review, which was designed purely to examine how research was conducted on adherence to PA and/or exercise interventions, to identify key characteristics or factors related to adherence assessment and to analyse knowledge gaps [26]. It is also possible that some relevant research was not assessed, because only English language papers and published data were included, with no further data requests or confirmation from study authors undertaken. A further limitation is that a librarian or information specialist was not consulted when developing the search strategy, and therefore some key terms might have been missed, although this is unlikely given the authors’ experiential knowledge.
Conclusions
This scoping review found that adherence to PA and/or exercise interventions was rarely the focus of research studies, despite the importance of PA and/or exercise to maintaining health in people with inflammatory arthritis. Where research has been conducted in this area, serious shortcomings were revealed, because in many studies psychological theory and evidence-based BCTs derived from theory were not used to inform intervention design and target adherence, meaning that interventions were suboptimal. Furthermore, reporting of intervention components and choice of adherence measures was poor, with most studies not using validated measures of adherence. These results suggest that there is considerable room for improvement in this area and that more high-quality research is required to investigate the determinants of PA and/or exercise adherence and develop targeted interventions to enhance it in people living with inflammatory arthritis. Researchers and clinicians should use valid and reliable measures and carry out theory-informed research that targets adherence accurately using appropriate BCTs, in order to improve the outcome and provide better support for people living with inflammatory arthritis.
Supplementary Material
Contributor Information
Hema Chaplin, Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK.
Mandeep Sekhon, Population Health Research Institute, St George’s, University of London, London, UK.
Emma Godfrey, Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK; Department of Physiotherapy, Faculty of Life Sciences and Medicine, King’s College London, London, UK.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
Data availability statement
The secondary data generated that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Van Der Heijde D, Ramiro S, Landewé R. et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–91. [DOI] [PubMed] [Google Scholar]
- 2. Osthoff AK, Niedermann K, Braun J. et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis 2018;77:1251–60. [DOI] [PubMed] [Google Scholar]
- 3. Bull FC, Al-Ansari SS, Biddle S. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020;54:1451–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pedersen BK, Saltin B.. Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 2015;25:1–72. [DOI] [PubMed] [Google Scholar]
- 5. O'Dwyer T, Rafferty T, O'Shea F, Gissane C, Wilson F.. Physical activity guidelines: is the message getting through to adults with rheumatic conditions? Rheumatology 2014;53:1812–7. [DOI] [PubMed] [Google Scholar]
- 6. Bell K, Hendry G, Steultjens M.. Physical activity and sedentary behavior in people with inflammatory joint disease: a cross‐sectional study. Arthritis Care Res 2022;74:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Physical activity. 2018. https://www.who.int/news-room/fact-sheets/detail/physical-activity (23 February 2018, date last accessed).
- 8. Frost R, Levati S, McClurg D, Brady M, Williams B.. What adherence measures should be used in trials of home-based rehabilitation interventions? A systematic review of the validity, reliability, and acceptability of measures. Arch Phys Med Rehabil 2017;98:1241–56.e45. [DOI] [PubMed] [Google Scholar]
- 9. Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL.. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J 2013;13:1940–50. [DOI] [PubMed] [Google Scholar]
- 10. Meade LB, Bearne LM, Godfrey EL.. “It’s important to buy in to the new lifestyle”: barriers and facilitators of exercise adherence in a population with persistent musculoskeletal pain. Disabil Rehabil 2021;43:468–78. [DOI] [PubMed] [Google Scholar]
- 11. Manning VL, Hurley MV, Scott DL, Bearne LM.. Are patients meeting the updated physical activity guidelines? Physical activity participation, recommendation, and preferences among inner-city adults with rheumatic diseases. J Clin Rheumatol 2012;18:399–404. [DOI] [PubMed] [Google Scholar]
- 12. Baxter S, Smith C, Treharne G, Stebbings S, Hale L.. What are the perceived barriers, facilitators and attitudes to exercise for women with rheumatoid arthritis? A qualitative study. Disabil Rehabil 2016;38:773–80. [DOI] [PubMed] [Google Scholar]
- 13. Swärdh E, Opava CH, Nygård L, Lindquist I.. Understanding exercise promotion in rheumatic diseases: a qualitative study among physical therapists. Physiother Theor Pract 2021;37:963–72. [DOI] [PubMed] [Google Scholar]
- 14. Davergne T, Tekaya R, Sellam J. et al. Influence of perceived barriers and facilitators for physical activity on physical activity levels in patients with rheumatoid arthritis or spondyloarthritis: a cross-sectional study of 150 patients. BMC Musculoskelet Disord 2021;22:915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davergne T, Tekaya R, Deprouw C. et al. To apply the recent EULAR recommendations, more knowledge on adherence patterns to medication and to physical activity is needed. Joint Bone Spine 2021;88:105137. [DOI] [PubMed] [Google Scholar]
- 16. Cramp F, Berry J, Gardiner M, Smith F, Stephens D.. Health behaviour change interventions for the promotion of physical activity in rheumatoid arthritis: a systematic review. Musculoskelet Care 2013;11:238–47. [DOI] [PubMed] [Google Scholar]
- 17. Larkin L, Gallagher S, Cramp F. et al. Behaviour change interventions to promote physical activity in rheumatoid arthritis: a systematic review. Rheumatol Int 2015;35:1631–40. [DOI] [PubMed] [Google Scholar]
- 18. Demmelmaier I, Iversen MD.. How are behavioral theories used in interventions to promote physical activity in rheumatoid arthritis? A systematic review. Arthritis Care Res 2018;70:185–96. [DOI] [PubMed] [Google Scholar]
- 19. Sekhon M, White C, Godfrey E. et al. Effectiveness of web-based and mobile health interventions designed to enhance adherence to physical activity for people with inflammatory arthritis: a systematic review. Rheumatol Adv Pract 2021;5:rkab016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fenton SA, Duda JL, van Zanten JJ, Metsios GS, Kitas GD.. Theory-informed interventions to promote physical activity and reduce sedentary behaviour in rheumatoid arthritis: a critical review of the literature. Mediterr J Rheumatol 2020;31:19–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Michie S, Johnston M, Abraham C. et al. ; “Psychological Theory” Group. Making psychological theory useful for implementing evidence based practice: a consensus approach. BMJ Qual Saf 2005;14:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Michie S, Richardson M, Johnston M. et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. [DOI] [PubMed] [Google Scholar]
- 23. Knittle K, Maes S, De Gucht V.. Psychological interventions for rheumatoid arthritis: Examining the role of self‐regulation with a systematic review and meta‐analysis of randomized controlled trials. Arthritis Care Res 2010;62:1460–72. [DOI] [PubMed] [Google Scholar]
- 24. Meade LB, Bearne LM, Godfrey EL.. Comprehension and face validity of the Exercise Adherence Rating Scale in patients with persistent musculoskeletal pain. Musculoskelet Care 2018;16:409–12. [DOI] [PubMed] [Google Scholar]
- 25. Colquhoun HL, Levac D, O'Brien KK. et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291–4. [DOI] [PubMed] [Google Scholar]
- 26. Munn Z, Peters MDJ, Stern C. et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liberati A, Altman DG, Tetzlaff J. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tricco AC, Lillie E, Zarin W. et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. [DOI] [PubMed] [Google Scholar]
- 29. Meade LB, Bearne LM, Sweeney LH, Alageel SH, Godfrey EL.. Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: systematic review. Br J Health Psychol 2019;24:10–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Michie S, van Stralen MM, West R.. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A.. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Pol 2005;10:45–53. [DOI] [PubMed] [Google Scholar]
- 32. Grant MJ, Booth A.. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J 2009;26:91–108. [DOI] [PubMed] [Google Scholar]
- 33. Ammerlaan J, van Os-Medendorp H, Scholtus L. et al. Feasibility of an online and a face-to-face version of a self-management program for young adults with a rheumatic disease: experiences of young adults and peer leaders. Pediatr Rheumatol 2014;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bilberg A, Dagfinrud H, Sveaas SH.. Supervised intensive exercise for strengthening exercise health beliefs in patients with axial spondyloarthritis: a multicentre randomized controlled trial. Arthritis Care Res 2022;74:1196–204. [DOI] [PubMed] [Google Scholar]
- 35. Bilberg A, Sveaas SH, Dagfinrud H, Mannerkorpi K.. How do patients with axial spondyloarthritis experience high‐intensity exercise? ACR Open Rheumatol 2020;2:207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chimenti MS, Triggianese P, Conigliaro P. et al. Self‐reported adherence to a home‐based exercise program among patients affected by psoriatic arthritis with minimal disease activity. Drug Dev Res 2014;75:S57–9. [DOI] [PubMed] [Google Scholar]
- 37. de Jong Z, Munneke M, Kroon HM. et al. Long-term follow-up of a high-intensity exercise program in patients with rheumatoid arthritis. Clin Rheumatol 2009;28:663–71. [DOI] [PubMed] [Google Scholar]
- 38. Hammond A, Freeman K.. The long-term outcomes from a randomized controlled trial of an educational–behavioural joint protection programme for people with rheumatoid arthritis. Clin Rehabil 2004;18:520–8. [DOI] [PubMed] [Google Scholar]
- 39. Hammond A, Lincoln N, Sutcliffe L.. A crossover trial evaluating an educational-behavioural joint protection programme for people with rheumatoid arthritis. Patient Educ Couns 1999;37:19–32. [DOI] [PubMed] [Google Scholar]
- 40. Hammond A, Lincoln N.. The effect of a joint protection education programme for people with rheumatoid arthritis. Clin Rehabil 1999;13:392–400. [DOI] [PubMed] [Google Scholar]
- 41. Mayoux-Benhamou A, Giraudet-Le Quintrec J-S, Ravaud P. et al. Influence of patient education on exercise compliance in rheumatoid arthritis: a prospective 12-month randomized controlled trial. J Rheumatol 2008;35:216–23. [PubMed] [Google Scholar]
- 42. Middleton KR, Ward MM, Haaz Moonaz S. et al. Feasibility and assessment of outcome measures for yoga as self-care for minorities with arthritis: a pilot study. Pilot Feasibil Stud 2018;4:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Moffet H, Noreau L, Parent E, Drolet M.. Feasibility of an eight-week dance-based exercise program and its effects on locomotor ability of persons with functional class III rheumatoid arthritis. Arthritis Care Res 2000;13:100–11. [DOI] [PubMed] [Google Scholar]
- 44. Nichols VP, Williamson E, Toye F, Lamb SE.. A longitudinal, qualitative study exploring sustained adherence to a hand exercise programme for rheumatoid arthritis evaluated in the SARAH trial. Disabil Rehabil 2017;39:1856–63. [DOI] [PubMed] [Google Scholar]
- 45. Niedermann K, Sidelnikov E, Muggli C. et al. Effect of cardiovascular training on fitness and perceived disease activity in people with ankylosing spondylitis. Arthritis Care Res 2013;65:1844–52. [DOI] [PubMed] [Google Scholar]
- 46. Nordgren B, Fridén C, Demmelmaier I. et al. ; PARA Study Group. An outsourced health-enhancing physical activity programme for people with rheumatoid arthritis: exploration of adherence and response. Rheumatology 2015;54:1065–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sang Y, Dong C, Fu T. et al. Associated factors with adherence to standard exercise therapy and health-related quality of life in Chinese patients with ankylosing spondylitis. Modern Rheumatology 2020;30:149–54. [DOI] [PubMed] [Google Scholar]
- 48. Somers TJ, Blumenthal JA, Dorfman CS. et al. Effects of a weight and pain management program in patients with rheumatoid arthritis with obesity: a randomized controlled pilot investigation. J Clin Rheumatol 2022;28:7–13. [DOI] [PubMed] [Google Scholar]
- 49. Ward L, Stebbings S, Athens J, Cherkin D, Baxter GD.. Yoga for the management of pain and sleep in rheumatoid arthritis: a pilot randomized controlled trial. Musculoskelet Care 2018;16:39–47. [DOI] [PubMed] [Google Scholar]
- 50. Williamson E, McConkey C, Heine P. et al. Hand exercises for patients with rheumatoid arthritis: an extended follow-up of the SARAH randomised controlled trial. BMJ Open 2017;7:e013121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bartholomew LK, Markham CM, Ruiter RAC. et al. Planning health promotion programs: an intervention mapping approach . 4 edn. San Francisco: Jossey-Bass, 2016. [Google Scholar]
- 52. Newman-Beinart NA, Norton S, Dowling D. et al. The development and initial psychometric evaluation of a measure assessing adherence to prescribed exercise: the Exercise Adherence Rating Scale (EARS). Physiotherapy 2017;103:180–5. [DOI] [PubMed] [Google Scholar]
- 53. Takasaki H, Kawazoe S, Miki T, Chiba H, Godfrey E.. Development and validity assessment of a Japanese version of the Exercise Adherence Rating Scale in participants with musculoskeletal disorders. Health Qual Life Outcomes 2021;19:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. De Lira MR, De Oliveira AS, França RA. et al. The Brazilian Portuguese version of the Exercise Adherence Rating Scale (EARS-Br) showed acceptable reliability, validity and responsiveness in chronic low back pain. BMC Musculoskelet Disord 2020;21:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Adhikari SP, Dev R, Shrestha JN.. Cross-cultural adaptation, validity, and reliability of the Nepali version of the Exercise Adherence Rating Scale: a methodological study. Health Qual Life Outcomes 2020;18:328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hendry G, Bearne L, Foster N. et al. Gait rehabilitation for foot and ankle impairments in early rheumatoid arthritis: a feasibility study of a new gait rehabilitation programme (GREAT Strides). Pilot Feasibil Stud 2022;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The secondary data generated that support the findings of this study are available from the corresponding author upon reasonable request.