Abstract
Background
Malalignments of the lower extremity are common reasons for orthopedic consultation because it may lead to osteoarthritis in adulthood. An accurate and reliable radiological assessment of lower limb alignment in children and adolescents is essential for clinical decision-making on treatment of limb deformities and for regular control after a surgical intervention.
Objective
First, does the analysis of full-length standing anteroposterior radiographs show a good intra- and interobserver reliability? Second, which parameter is most susceptible to observer-dependent errors? Third, what is the Standard Error of Measurement (SEM95%) of the absolute femoral and tibial length?
Methods
Two observers evaluated digital radiographs of 144 legs from 36 children and adolescents with pathological valgus alignment before a temporary hemiepiphysiodesis and before implant removal. Parameters included Mechanical Femorotibial Angle (MFA), Mechanical Axis Deviation (MAD), mechanical Lateral Distal Femoral Angle (mLDFA), mechanical Medial Proximal Tibial Angle (mMPTA), mechanical Lateral Proximal Femoral Angle (mLPFA), mechanical Lateral Distal Tibial Angle (mLDTA), Joint Line Convergence Angle (JLCA), femur length, tibial length. Intra- and interobserver reliability (ICC2,1), SEM95% and proportional errors were calculated.
Results
The intra- and interobserver reliability for almost all measurements was found to be good to excellent (Intra-ICC2,1: 0.849–0.999; Inter-ICC2,1: 0.864–0.996). The SEM95% of both observers was found to be ± 1.39° (MFA), ± 3.31 mm (MAD), ± 1.06° (mLDFA) and ± 1.29° (mMPTA). The proportional error of MAD and MFA is comparable (47.29% vs. 46.33%). The relevant knee joint surface angles show a lower proportional error for mLDFA (42.40%) than for mMPTA (51.60%). JLCA has a proportional error of 138%. Furthermore, the SEM95% for the absolute values of the femoral and tibial length was 4.53 mm for the femur and 3.12 mm for the tibia.
Conclusions
In conclusion, a precise malalignment measurement and the knowledge about SEM95% of the respective parameters are crucial for correct surgical or nonsurgical treatment. The susceptibility to error must be considered when interpreting malalignment analysis and must be considered when planning a surgical intervention. The results of the present study elucidate that MAD and MFA are equally susceptible to observer-dependent errors. This study shows good to excellent intra- and interobserver ICCs for all leg alignment parameters and joint surface angles, except for JLCA.
Trial registration: This study was registered with DRKS (German Clinical Trials Register) under the number DRKS00015053.
Level of evidence
I, Diagnostic Study.
Keywords: Lower limb deformities, Leg axis, Genu valgum, Radiological assessment, Reliability, Pediatric orthopedic, Guiding growth
Background
Osteoarthritis (OA) of the knee is a common cause for knee pain, reduced joint motion and consecutive muscle weakness leading to physical inactivity, reduction in quality of life, disability and eventually a total joint replacement [1]. Varus or valgus malalignment of the lower extremity has a major impact on the development and progression of knee OA [2]. The valgus deformity leads to increased load on the lateral compartment of the knee joint and the varus malalignment increases the load on the medial compartment [3–6].
To prevent the development of OA, growth control should be considered in children with severe axial deviation in the frontal plane. For children and adolescents, there is a wide range of normal values concerning axis deviation of the lower limb, which need to be differentiated from pathological and pre-arthritic deformities prior to surgical intervention [7]. As a surgical treatment, temporary hemiepiphysiodesis (THE) of the distal femur or proximal tibia using tension band plates, depending on the location of the pathologic joint surface angles, has become established for axis correction of children and adolescents [8, 9]. However, the exact patient age for the best possible correction and the lowest probability of rebound remains unclear. Furthermore, there is a lack of defined parameters for the indication of THE. The definition of parameters like the Mechanical Axis Deviation (MAD) or the Mechanical Femorotibial Angle (MFA) is complicated by the interindividual variation during growth, the uncertainty of when MAD leads to pathological joint moments and pressure loads as well as the determination method and the associated susceptibility to errors [4, 5, 10, 11].
Malalignment of the lower extremity is one of the most common reasons for an orthopedic consultation. An accurate and reliable radiological assessment of lower limb alignment is essential for clinical decision-making on treatment of limb deformities and for regular control after a surgical intervention [8, 12]. The full-length standing anteroposterior radiograph of both legs is the gold standard for assessment of lower limb alignment in frontal plane [13]. Most commonly the indication for a THE is set when the physiological mechanical bearing line (MAD) deviates more than 10 mm lateral or 15 mm medial to the center of the knee [14], which is approximately 3° deviation of the physiological MFA. Furthermore, knowledge of the joint surface angles and the Joint Line Convergence Angle (JLCA) is important to assess on which bones the guided growth intervention should be performed. In addition, an estimate of the residual growth can be made based on the absolute lengths of the femur or tibia in relation to age and sex and thus the correction potential of the guided growth intervention can be determined [15–17].
To the best of our knowledge no study has shown which parameter or combination of parameters is more reliable for setting the indication for a THE in children and adolescents. Therefore, we first aim to elucidate if the analysis of a full-length standing anteroposterior radiograph of both legs shows a good intra- and interobserver reliability concerning lower limb alignment measurements in the frontal plane. A misjudgment or incorrect determination may result in a delayed or unnecessary indication for THE and thus in an incorrect manipulation of the leg axis. Second, it is important to clarify which of the investigated alignment parameters is less prone to observer-dependent errors in determining lower limb alignment. Third, as mentioned earlier, the correct and reproducible measurement of the absolute tibial and femoral length is essential to estimate the growth potential. Therefore, the measurement error of the absolute femoral and tibial length needs to be elaborated.
Methods
Patients
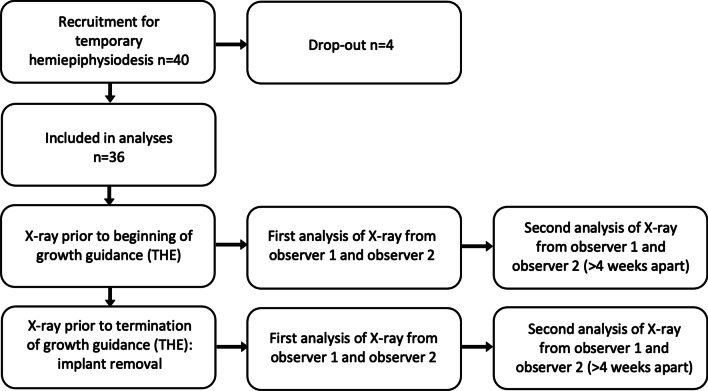
Patients older than 8 years of age who showed an intermalleolar distance of more than 10 cm received an anterior–posterior-full length X-ray of both legs in the standing position for objective assessment of the leg axis [7]. From the 40 patients recruited, four patients were excluded from this study due to unusable radiographs. This homogenous cohort finally consists of 36 patients (median age of 12.81 years at baseline; Table 1) with an idiopathic pathological valgus alignment of at least one knee according to the MAD of the lower limb were recruited between September 2014 and October 2021 on a voluntary basis. Patients were included if the MAD deviates more than 10 mm lateral [14] and were planned to receive THE of one or both knees [3, 12, 18]. The tension band plates used in this study were the Eight-Plates (Orthofix, Lewisville, TX, USA) or Pedi-Plates (Orthopediatrics Inc., Warsaw, IN, USA). The aim of this growth guidance technique is to straighten the leg axis. After a successful operation by means of THE is an MFA of 0° (± 2°) or an MAD of 0 mm (± 6 mm). All patients were analyzed twice, directly before guided growth intervention (72 legs) and at the time of implant removal (the same 72 legs). Accordingly, patients were deliberately measured both at a time when a lower limb malalignment was present and with corrected leg alignment to test the reliability during the entire treatment period (see Fig. 1). In total 144 legs/data sets could be evaluated.
Table 1.
Patient characteristics (n = 36)
| Time of Investigation | Age (range) in years | Height (range) in cm | Weight (range) in kg | BMI (range) in kg/m2 |
|---|---|---|---|---|
| Implantation of tension band plates using THE | 12.81 (10.50–15.38) | 165.89 (145.20–182.90) | 63.49 (31.80–89.30) | 22.86 (14.95–29.29) |
| Removal of tension band plates using THE | 13.72 (11.32–16.35) | 171.83 (150.60–187.40) | 71.25 (33.80–94.50) | 23.88 (14.90–32.79) |
Table 1 shows the anthropometric data of the collective at the time of implantation and removal of tension band plates using the temporary hemiepiphysiodesis (THE). Values are presented as median and interquartile range in parenthesis
Fig. 1.
Diagram of the prospective study design. THE—temporary hemiepiphysiodesis
Exclusion criteria were: rheumatoid arthritis, anterior cruciate ligament deficiency, neuromuscular disorders, achondroplasia or hypochondroplasia, sagittal plane deformities (genu pro- and recurvatum), flexion contractures in the hip or knee joint, leg length discrepancy of more than 10 mm, avascular necrosis of the femoral head or knee condyles, history of major trauma or sport injury of the lower extremity, knee surgery within 12 months prior to inclusion in this study, chronic joint infections or previously received intraarticular corticosteroid injections.
Radiographic malalignment analysis
The standardized, scalable, digital long leg X-rays were taken in an anterior–posterior orientation. A 25.4-mm (1 inch)-diameter metal ball was placed between the legs at the level to the bones next to the joint line of the knees and used as a reference for determining the individual magnification factor. The radiographic measurements were performed with a commercially available templating program, TraumaCad® (version 2.3.4.1; Voyant Health, Petach-Tikva, Israel). Criteria for a valid full leg length anteroposterior radiographic image were [18]: patient standing in an upright, weight-bearing position, both legs parallel to each other a shoulder width apart, fully extended knees, patellae centered over the femoral condyles pointing straight forward in order to avoid rotational errors [19, 20].
Definitions of the angles measured are described below (Fig. 2):
Fig. 2.
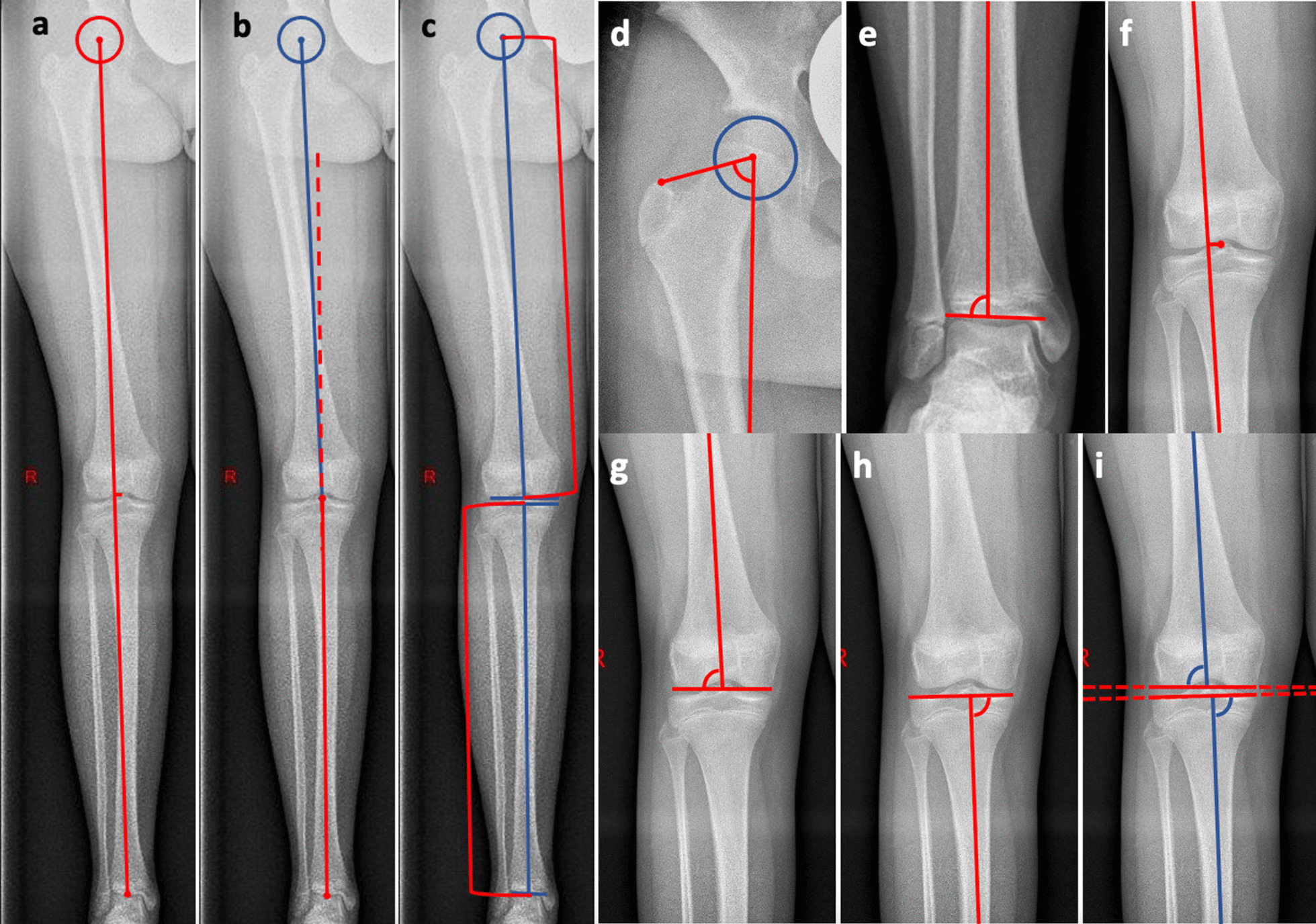
Left (Image a–c) full-length standing anterior–posterior radiograph of the right leg; a – d center of the hip (circle); a Mechanical axis of the limb and Mechanical Axis Deviation (MAD) (red lines); b Mechanical Femorotibial Angle (MFA) between mechanical femur line (blue line) and mechanical tibia line (red line); c length of the femur and tibia (red brackets); d mLPFA mechanical Lateral Proximal Femur Angle; e mLDTA mechanical Lateral Distal Tibia Angle; f detailed magnification from image a, Mechanical axis of the limb and MAD; g mLDFA mechanical Lateral Distal Femur Angle; h mMPTA mechanical Medial Proximal Tibia Angle; i JLCA Joint Line Convergence Angle [18]
Malalignment analysis was performed due to the principles described by Paley et. al [12, 18]: The radiographic Mechanical Femorotibial Angle (MFA) is defined as the angle formed by the line from the center of the hip to the center of the knee (mechanical femur line) and the line from the center of the knee to the center of the ankle (mechanical tibia line) (Fig. 2b) [21]. To find the center of the hip, an auxiliary circle around the femoral head was needed. The center point of the circle was determined as center of the hip. The center of the knee joint was defined as the midpoint between the center of the intercondylar region and the center of the eminentia intercondylaris. The center of the ankle was determined as the midpoint of the talar dome. Neutral alignment was defined as 0°, varus malalignment as positive angles and valgus malalignment as negative angles.
The Mechanical Axis Deviation (MAD) is defined as the distance between the center of the knee and the mechanical axis of the limb (Fig. 2a–f). Medial deviation (varus) is depicted as positive and lateral deviation (valgus) as negative values.
The mechanical Lateral Distal Femoral Angle (mLDFA) shows the angle between the mechanical femoral axis and the tangent through the most convex points of each femoral condyle (Fig. 2g).
The mechanical Medial Proximal Tibial Angle (mMPTA) depicts the angle between the mechanical tibial axis and the line along the subchondral bone from the tibial plateau (Fig. 2h).
The mechanical Lateral Proximal Femoral Angle (mLPFA) shows the angle between the mechanical femoral axis and the line from the tip of the greater trochanter to the center of the hip (Fig. 2d).
The mechanical Lateral Distal Tibial Angle (mLDTA) is defined as the angle between the mechanical axis of the tibia and the line through the medial and lateral talus shoulder (Fig. 2e).
The Joint Line Convergence Angle (JLCA) depicts the angle between the tangent of the most convex points of each femoral condyle and the line along the subchondral bone from the tibial plateau (Fig. 2i).
The length of the femur describes the distance between the center of the femoral head and the center of a line connecting the two most distal points of the medial and lateral femoral condyle (Fig. 2c) [22].
The length of the tibia describes the distance between the center of a line connecting the two most proximal points of the medial and lateral proximal tibial plateau and the center of a line.
To assess intra- and interobserver reliability, radiographs for each patient were blinded and templated twice by two independent and experienced observers (SB, MB) familiar with the templating software. The two observers are orthopedic residents with special focus on pediatric orthopedics and more than five years of experience analyzing lower limb alignments. To avoid recollection bias, the second evaluations from the same set of measurements were repeated at least 4 weeks apart, blinded to the measurements provided previously.
Statistical analysis
To evaluate the reliability of the measurements, the intra- and interobserver intraclass correlation coefficient (ICC2,1) was calculated. An important advantage of ICC2,1 is that the coefficient can detect bias by the order in which pairs of data are compared and is therefore preferable to other correlation coefficients [23, 24]. For interobserver ICC2,1 the results of the first measurement of observer one are compared with the results of the first measurement of observer two. One-way random tests with absolute agreement were used for each observer to estimate intraobserver ICCs and two-way random tests with absolute agreement per set of measurements for each parameter were used to determine interobserver ICCs. ICC2,1 values < 0.70 indicate poor, 0.70 to 0.79 fair, 0.80 to 0.89 good, and 0.90 to 1.00 excellent reliability [23, 24].
The Shapiro–Wilk test was used to test normal distribution of the analyzed parameters. Differences between observers were tested with Wilcoxon test (nonparametric dependent variables) or paired t-test (parametric dependent variables). To assess the observer-dependent errors, we calculated the Standard Error of Measurements (SEM95%) from the interobserver ICC2,1.
The SEM estimates the distribution of repeated measurements with the same instrument around their "true" value. It quantifies the precision of individual scores on tests and provides an absolute index of reliability, in contrast to ICC, which is a relative measure of reliability [25]. The SEM is directly related to the reliability of a test, i.e., the greater the SEM, the lower the reliability of the test. The range of the SEM95% (e.g., MAD SEM95% = ± 3.31 mm → SEM95%Range = 6.62 mm) was divided by the range of the respective norm values considered as acceptable (e.g., MADAcptRange 15 mm to 1 mm = 14 mm). This proportional error shows for which parameter, the SEM95% is proportionately lowest or highest.
Statistical data analysis was performed with SPSS (version 26, IBM Corporation, New York, NY, USA). The significance level for all statistical tests was set at p ≤ 0.05. The following data were presented as mean and standard deviation (parametric variables) or median ± 25–75 percentiles (nonparametric variables).
The level of evidence of this study is a Level I, Diagnostic Study.
Results
From September 2014 to October 2021, full-length standing anteroposterior radiographs of the legs at two different time points (implantation of tension band plates and removal of tension band plates) from 72 legs of 36 children and adolescents (16 girls and 20 boys) were included in this study. All the children and adolescents had a valgus malalignment on both sides. Table 1 shows the anthropometric data such as age, height, weight, and BMI of the collective at the time of implantation and at the time of removal of the tension band plates.
Does the analysis of a full-length standing anteroposterior radiograph of the lower limb show a good intra- and interobserver reliability concerning lower limb alignment measurements?
The values MFA, MAD, mLPFA, mLDFA, mMPTA, mLDTA, JLCA, length of femur, and length of tibia were measured twice on 144 legs by each observer (Table 2). For both observers, the intraobserver ICC2,1 (Table 3) in alignment analysis was good to excellent and likewise high, ranging from 0.849 to 0.999. In contrast, fair results were only found for intraobserver ICC2,1 in analysis of JLCA (0.607–0.676).
Table 2.
Lower limb measurement parameters (N = 144)
| Measures | Observer one | Observer two | p Value | ||
|---|---|---|---|---|---|
| Mean ± SD (range) | Median (25 – 75 percentiles) | Mean ± SD (range) | Median (25 – 75 percentiles) | ||
| MFA (°) | − 2 (− 5 to 0) | − 3 (− 5 to − 1) | p < 0.001 | ||
| MAD (mm) |
− 8.69 ± 11.17 (− 38 to 22) |
-9.01 ± 10.60 (− 37 to 22) |
p = 0.013 | ||
| mLPFA (°) | 88 (85–91) | 88 (85–92) | p = 0.173 | ||
| mLDFA (°) | 86 (84–89) | 86 (84–89) | p < 0.001 | ||
| mMPTA (°) | 90 (89–92) | 90 (89–91) | p < 0.001 | ||
| mLDTA (°) | 87 (84–89) | 87 (85–89) | p < 0.001 | ||
| JLCA (°) | 2 (1–2) | 1 (1–2) | p < 0.001 | ||
| length of femur (mm) | 474.24 ± 36.58 (387–572) | 474.20 ± 36.28 (390–570) | p = 0.067 | ||
| length of tibia (mm) | 379.5 (359–402) | 378 (358–401) | p < 0.001 | ||
Table 2 shows the mean measures from both analyses of both observers (SD = standard deviation) and the median with 25–75 percentiles
MFA Mechanical Femorotibial Angle; MAD Mechanical Axis Deviation; negative values of MFA and MAD show valgus malalignment; mLPFA mechanical Lateral Proximal Femur Angle; mLDFA mechanical Lateral Distal Femur Angle; mMPTA mechanical Medial Proximal Tibia Angle; mLDTA mechanical Lateral Distal Tibia Angle; JLCA Joint Line Convergence Angle, length of the femur and tibia. Parametric values: MAD and femur length; nonparametric values: MFA, mLPFA, mLDFA, mMPTA, mLDTA, JLCA and tibia length.
Table 3.
Intraobserver reliability: Intraclass correlation coefficient ICC2,1 (95% confidence interval in parenthesis)
| Measures | Observer one | Observer two |
|---|---|---|
| Intraobserver-ICC2,1 | Intraobserver-ICC2,1 | |
| MFA (°) | 0.974 (0.963–0.981) | 0.982 (0.972–0.989) |
| MAD (mm) | 0.994 (0.992–0.996) | 0.995 (0.993–0.996) |
| mLPFA (°) | 0.977 (0.967–0.984) | 0.961 (0.946–0.972) |
| mLDFA (°) | 0.972 (0.962–0.980) | 0.981 (0.974–0.987) |
| mMPTA (°) | 0.889 (0.845–0.920) | 0.949 (0.929–0.963) |
| mLDTA (°) | 0.849 (0.796–0.889) | 0.902 (0.866–0.929) |
| JLCA (°) | 0.607 (0.492–0.701) | 0.676 (0.612–0.757) |
| Femur length (mm) | 0.997 (0.996–0.998) | 0.999 (0.999–0.999) |
| Tibia length (mm) | 0.997 (0.996–0.998) | 0.996 (0.994–0.997) |
Table 3 shows the intraobserver-ICC2,1 from both observers
MFA Mechanical Femorotibial Angle, MAD Mechanical Axis Deviation, mLPFA mechanical Lateral Proximal Femur Angle, mLDFA mechanical Lateral Distal Femur Angle, mMPTA mechanical Medial Proximal Tibia Angle, mLDTA mechanical Lateral Distal Tibia Angle, JLCA Joint Line Convergence Angle, length of the femur and tibia.
Interobserver ICC2,1 (Table 4) for alignment parameters (MFA, MAD, mLPFA, mLDFA, mMPTA, mLDTA, femur length and tibia length) ranged from 0.864 to 0.996. Similar to intraobserver findings, interobserver ICC2,1 analysis of JLCA was slightly out of line and showed fair results (0.488). It is also shown that the intraobserver ICC2,1 and interobserver ICC2,1 are slightly lower for the joint surface angles at the tibia than for the joint surface angles at the femur.
Table 4.
Standard values and the accepted range of each lower limb parameter [12, 18], interobserver-ICC2,1, Standard Error of Measurement (SEM) and proportional error
| Measures | Standard value | Accepted range | Interobserver-ICC2,1 | SEM95% | SEM95%Range | Proportional error in % |
|---|---|---|---|---|---|---|
| MFA (°) | 1.3 ± 3 | 6 | 0.949 (0.859–0.975) | ± 1.39 | 2.78 | 46.33 |
| MAD (mm) | 8 ± 7 | 14 | 0.976 (0.966–0.983) | ± 3.31 | 6.62 | 47.29 |
| mLPFA (°) | 90 ± 5 | 10 | 0.974 (0.964–0.981) | ± 1.69 | 3.38 | 33.80 |
| mLDFA (°) | 88 ± 2.5 | 5 | 0.969 (0.954–0.979) | ± 1.06 | 2.12 | 42.40 |
| mMPTA (°) | 87 ± 2.5 | 5 | 0.864 (0.816–0.901) | ± 1.29 | 2.58 | 51.60 |
| mLDTA (°) | 89 ± 3 | 6 | 0.876 (0.831–0.909) | ± 2.17 | 4.34 | 72.33 |
| JLCA (°) | 1 ± 1 | 2 | 0.488 (0.350–0.605) | ± 1.38 | 2.76 | 138.00 |
| Femur length (mm) | N/A | N/A | 0.996 (0.994–0.997) | ± 4.53 | N/A | N/A |
| Tibia length (mm) | N/A | N/A | 0.994 (0.990–0.998) | ± 3.12 | N/A | N/A |
Interobserver-ICC2,1 (95% confidence interval in parenthesis) with Standard Error of Measurement (SEM) with a 95% confidence interval. For interobserver-ICC2,1 first measurement results of observer 1 were compared with first measurement results of observer 2
MFA Mechanical Femorotibial Angle; MAD Mechanical Axis Deviation; mLPFA mechanical Lateral Proximal Femur Angle; mLDFA mechanical Lateral Distal Femur Angle; mMPTA mechanical Medial Proximal Tibia Angle; mLDTA mechanical Lateral Distal Tibia Angle; JLCA Joint Line Convergence Angle, length of the femur and tibia
For values of femur length and tibia length there are no standard values and therefore no accepted ranges, SEM95%Range or proportional errors are not applicable (N/A)
Which parameter is most susceptible to observer-dependent errors in determining lower limb alignment?
As shown in Table 2, the mean MFA was −2.40° (SD ± 3.13°) for observer one and −2.81° (SD ± 3.12°) for observer two. The MAD values averaged -8.69 mm (SD ± 11.17 mm) for observer one and −9.01 mm (SD ± 10.60 mm) for observer two. The other mean values for observer one and observer two are shown in Table 2.
The mLDFA, mMPTA, mLDTA, JLCA, MFA, MAD and tibia length measurements of observer one and observer two were significant different (p < 0.05). No significant difference between both observers was found for femur length (p = 0.067) and mLPFA (p = 0.173).
To assess the observer-dependent errors, the SEM95% was calculated (Table 4). The SEM95% of both observers was found to be ± 1.39° for MFA, ± 3.31 mm for MAD, ± 1.69° for mLPFA, ± 1.06° for mLDFA, ± 1.29° for mMPTA, ± 2.17° for mLDTA and ± 1.38° for JLCA with a 95% confidence interval. In order to determine for which parameter the SEM95% is proportionately lowest/highest, we divided the range of the respective SEM95% (SEM95%Range) by the range of the different values considered acceptable (accepted range). The results (proportional error) are shown in Table 4. The proportional error of MAD was slightly higher, but comparable to the proportional error of MFA (47.29% vs. 46.33%). Looking at the relevant joint surface angles at the knee joint, we noticed that the proportional errors for the femur (mLPFA 33.80% and mLDFA 42.40%) are lower than for the tibia (mMPTA 51.60% and mLDTA 72.33%). JLCA shows the highest proportional error of 138%. Consistent to the results from the intraobserver- and interobserver ICC2,1, the SEMs and the proportional errors are also larger for the articular surface angles at the tibia than at the femur.
What is the SEM95% of the determination of the absolute femoral and tibial length, which are needed for the estimation of the existing correction potential for each bone?
The mean femur length was 474.24 mm (SD ± 36.58 mm) for observer one and 474.20 mm (SD ± 36.28 mm) for observer two. The mean tibia length was 379.80 mm (SD ± 29.85 mm) for observer one and 378.38 mm (SD ± 29.67 mm) for observer two. The statistical analysis did detect significant differences between the measurements of those two observers for the tibia length (p < 0.001), but not for the femur length (p = 0.067) (Table 2). The SEM95% for the absolute values of the femoral and tibial length were ± 4.53 mm (femur) and ± 3.12 mm (tibia) (Table 4). If the SEM95% of the respective bone is related to its absolute length, it can be shown that the SEM95% of ± 4.53 mm for the femur is about 1.92% of the length of the femur, and ± 3.12 mm for the tibia is about 1.64% of the length of the tibia in this collective.
Discussion
The digital measurement of biometric parameters as well as the preoperative planning of orthopedic interventions was shown to have good to excellent reliability, e.g., for Cobb angle in scoliosis [26, 27], planning of hip prostheses [28, 29] or leg axis determinations in long-leg X-rays [30–33]. The correct and reliable analysis of static parameters of the lower extremity is essential for an adequate treatment of pediatric orthopedic diseases. In addition to the clinical appearance, these measurements play a significant role in determining the indication for guided growth intervention of the lower limb using THE. In the present study the intra- and interobserver reliability for almost all lower limb alignment measurements in full-length standing anteroposterior radiographs of the frontal plane were found to be good to excellent.
Our study is the first that investigates all relevant malalignment parameters in the frontal plane in children and adolescents regarding intra- and interobserver reliability, SEM95% and proportional errors in order to make the best possible and the least error-prone decision on the indication and timing of THE, on postoperative follow-up and on the right time for removal of the tension band plates after completion of growth guidance.
According to the study of Specogna et al. [34], reliability of repeated lower limb frontal plane alignment measures is high for planning a high tibial osteotomy with OA affecting the medial compartment of the knee due to varus malalignment (MFA Intra-ICC2,1 = 0.98; 95% CI = 0.97 − 0.99, Inter-ICC2,1 = 0.98; 95% CI = 0.91–0.99; MAD Intra-ICC2,1 = 0.98; 95% CI = 0.97 − 0.99, Inter-ICC2,1 = 0.97; 95% CI = 0.90–0.99). Specogna et al. [34] elucidated that the estimates of error for the measurements of MFA need to be considered with ± 1.50° and for the MAD ± 4.3 mm. These findings are largely consistent with the results of our investigation. In contrast to our findings, the mentioned study investigated MFA and MAD on radiographs collected from adult patients (mean age 44 (21–65) years). When analyzing leg axis on skeletally immature patients, Gordon et al. [31] were able to show that intra- and interobserver reliabilities for each of the measurements (mLDFA, mMPTA and MAD) were ≥ 0.90 (0.90–0.99) in children (mean age 11.2 (7.1–14.7) years) with neutral alignment and both varus or valgus malalignment regardless of the level of observer experience. Gordon et al. [31] pointed out that the overall mean interobserver differences were ± 1.4° for the mLDTA, ± 1.6° for the mMPTA and ± 3.1 mm for the MAD measurement. In a similar study, Schmale et al. [32] have shown that the intraobserver ICC values ranged from 0.27 to 0.94 for the mLDFA and from 0.88 to 0.97 for the mMPTA in patients with open distal femur and proximal tibia physes at the time of a transphyseal anterior cruciate ligament reconstruction. Furthermore, the reliability (interobserver ICC: MAD 0.92, mLDFA 0.86 and mMPTA 0.98) of leg axis measurements were rated as good to excellent. Nowicki et al. [33] evaluated the MAD, mLDFA, mMPTA and JLCA of pediatric lower extremities (mean age 13.5 years) with neutral, varus or valgus (mal)alignment but not the MFA and they did not calculate the SEM95% for all relevant parameters. They could also show comparable values for the intraobserver ICC of the four measurement parameters: 0.756–0.990 for mLDFA, 0.489–0.958 for mMPTA, 0.831–0.927 for JLCA and 0.974–0.993 for MAD. Interobserver ICC values of 0.732–0.977 could be presented for the respective parameters. Feldman et al. [35] came to a similar conclusion that planning guiding treatment on those digital radiograph measurements is reliable and reproducible with intraobserver ICC of 0.77 (0.65–0.86) for mMPTA and mLDTA 0.80 (0.77–0.84). In this study, however, only the relevant joint surface angles of the tibia were comparable to our finding, because they chose to measure and analyze the anatomical angles instead of the mechanical angles. Furthermore, MAD and MFA were not investigated as well. Table 5 shows a summary of all the studies just mentioned. This is to illustrate the investigated parameters and the respective differences in our manuscript.
Table 5.
Summary of the results of the leg axis and joint angle analyses of different studies investigating intra- and interobserver reliability and Standard Error of Measurements of lower limb radiographs
| Parameters | Specogna et al.[34] | Gordon et al.[31] | Schmale et al.[32] | Nowicki et al.[33] | Feldman et al.[35] |
|---|---|---|---|---|---|
| N = 42 | N = 56 | N = 15 | N = 32 | N = 60 | |
| MFA | |||||
| Intra ICC | 0.98 (0.97–0.99) | N/A | N/A | N/A | N/A |
| Inter ICC | 0.98 (0.91–0.99) | N/A | N/A | N/A | N/A |
| SEM | 1.50 | N/A | N/A | N/A | N/A |
| MAD | |||||
| Intra ICC | 0.98 (0.97–0.99) | 0.99 (0.99–0.99) | 0.93–0.99 (0.84–1.00) | 0.974–0.993 (0.946–0.996) | N/A |
| Inter ICC | 0.97 (0.90–0.99) | 0.99 (0.99–0.99) | 0.92 (0.81–0.97) | 0.977 (0.964–0.987) | N/A |
| SEM | 4.3 | 3.1 | N/A | N/A | N/A |
| mMPTA | |||||
| Intra ICC | N/A | 0.99 (0.99–0.99) | 0.88–0.97 (0.73–0.99) | 0.489–0.958 (0.183–0.979) | 0.78 (0.65–0.86) |
| Inter ICC | N/A | 0.98 (0.97–0.98) | 0.98 (0.94–0.97) | 0.778 (0.670–0.869) | 0.77 |
| SEM | N/A | 1.6 | N/A | N/A | N/A |
| mLDFA | |||||
| Intra ICC | N/A | 0.96 (0.95–0.97) | 0.27–0.94 (-0.16–0.97) | 0.756–0.990 (0.545–0.995) | 0.80 (0.77–0.84) |
| Inter ICC | N/A | 0.91 (0.90–0.92) | 0.86 (0.68–0.95) | 0.732 (0.423–0.877) | 0.70 |
| SEM | N/A | 1.4 | N/A | N/A | N/A |
| mLPFA | |||||
| Intra ICC | N/A | N/A | N/A | N/A | N/A |
| Inter ICC | N/A | N/A | N/A | N/A | N/A |
| SEM | N/A | N/A | N/A | N/A | N/A |
| mLDFA | |||||
| Intra ICC | N/A | N/A | N/A | N/A | N/A |
| Inter ICC | N/A | N/A | N/A | N/A | N/A |
| SEM | N/A | N/A | N/A | N/A | N/A |
| JLCA | |||||
| Intra ICC | N/A | N/A | N/A | 0.831–0.927 (0.659–0.964) | N/A |
| Inter ICC | N/A | N/A | N/A | 0.812 (0.678–0.899) | N/A |
| SEM | N/A | N/A | N/A | N/A | N/A |
Intra ICC Intraobserver reliability using the intraclass correlation coefficient; Inter ICC Interobserver reliability using the intraclass correlation coefficient; SEM Standard Error of Measurement; MFA Mechanical Femorotibial Angle; MAD Mechanical Axis Deviation; mLPFA mechanical Lateral Proximal Femur Angle; mLDFA mechanical Lateral Distal Femur Angle; mMPTA mechanical Medial Proximal Tibia Angle; mLDTA mechanical Lateral Distal Tibia Angle; JLCA Joint Line Convergence Angle
When looking at the results of the present study, it becomes obvious that nearly all ICCs represent good to excellent correlations. Only the intra- and interobserver ICCs for JLCA are out of line and provide solely poor correlations. At a closer look at the standard values of the JLCA (1 ± 1°), it becomes apparent that a planning discrepancy of 1.38° in two successive examinations of two different observers of the same X-ray results in a relatively large discrepancy (proportional error = 138%; Table 4). This might explain why even small measurement inaccuracies become noticeable in a relatively smaller ICC. In accordance with objective 1, it can be concluded that the reliability of the individual parameters is good, except of the JLCA.
Furthermore, it was investigated which parameter is most susceptible to observer-dependent errors in determining lower limb alignment in the frontal plane. To date, there are no clear criteria for the indication of THE. The growth of the child and the development of the leg axis in children and adolescents show a high physiological range in younger patients and a typical course. While children under 2 years of age show a physiological varus alignment, a valgus leg axis develops until about 7 years of age. With advancing skeletal maturation (about 8 to 10 years of age), the range decreases significantly, which is also reflected in a decrease in the spontaneous correction of the existing leg axis deformities [36]. The results of this study refer to children aged 10 years and older, in whom the spontaneous correction potential is already reduced. Radtke et al. [8] indicate a THE of the knee at a MAD of > 10 mm, regardless of whether the deviation is medial or lateral. They were not using the MFA for indication. The same applies to other studies. Gupta et al. [37] considered a MAD of 3 mm both medial and lateral as a normal value and described a deviation of the MFA lateral to the lateral intercondyloid tubercle as valgus malalignment and a deviation medial to the medial intercondyloid tubercle as varus malalignment. In contrast, Stevens et al. [38] divide the knee joint in an anteroposterior radiograph into three zones lateral and three zones medial, mirrored at the knee joint center. Here, neither the MFA nor the MAD is directly considered. They see an indication for a THE in the case of a deviation of the mechanical bearing line in zones 2 and 3 [38].
Regarding the results of the present study, we can postulate that the SEM95% of MFA, MAD, mLPFA, mLDFA, mMPTA and mLDTA are likewise high. Thus, the results suggest that if a MFA measurement of 3° valgus is assumed, an SEM95% of ± 1.39° means that the actual value will range between 1.61° (non-pathologic) and 4.39° (pathologic) valgus. In addition, a MAD measurement of −10 mm lateral to the center of the knee with a SEM95% of ± 3.31 mm means that the actual value ranges between −6.69 mm (non-pathologic) and -13.31 mm (pathologic) valgus. This susceptibility to error must be taken into account not only for leg alignment parameters but also for joint surface angles when interpreting malalignment analysis and must be considered when planning a surgical intervention. An inaccurate and wrong interpreted malalignment analysis may result in an incorrect diagnosis, which in turn leads to an unnecessary indication for surgical therapy. Furthermore, it could lead to termination of the guided growth intervention by a removal of the tension band plates at the wrong point of time. Considering the SEM95% of the MAD and the MFA, a wrong interpretation could also be an explanation for the high rebound rates of up to nearly 50% [39]. Therefore, it must be discussed whether an overcorrection of the leg axis with a minimum of 1.39° MFA and 3.31 mm MAD should be aimed to prevent the common phenomenon of rebound by taking the respective SEM95% into account. This slight overcorrection is already recommended by several authors [40, 41]. Thus, a precise malalignment measurement and the knowledge about the presented SEM95% of the respective parameters is crucial for a correct surgical or nonsurgical treatment. In addition, we were able to show that by measuring the MAD and MFA, the SEM95% are comparable (proportional error = 47.29% vs. 46.33%, respectively). Hereby, we consider the MAD and MFA to be equally (im)precise parameters for the determination of an axial malalignment and initiation of a growth-guiding therapy. In order to decide on which bones to perform growth guidance, mLDFA and mMPTA show distinct observer-dependent differences. The proportional error for mLDFA is lower at 42.2% than for mMPTA at 51.60%.
In addition to the observer-dependent errors, the radiological acquisition technique also influences the result of the respective angles [13, 42, 43]. When taking the full-leg radiograph, the patellae of the extended legs have to be aligned frontally (not the feet) so that the femoral condyles are positioned parallel to the frontal plane. Rotation of the leg at the time the image is taken should be avoided, as should flexion of the knee joint. In the case of increased internal rotation of the knee joints, the leg axis appears more valgus; in the case of external rotation, it appears correspondingly more varus [13]. In our study cohort, an internal quality assessment was performed first by the executing radiology assistants and subsequently by the two analyzing observers. All included patients showed qualitatively unobjectionable radiographs.
Furthermore, SEM95% of tibial and femoral length was determined. Those values are essential for a proper estimation of residual growth and correction potential using the multiplier method according to Paley [15, 16, 44]. The multiplier method need an exact determination of the bone length (either tibia or femur) to give a precise information about the correction potential. We could show that the ICCs of the length determination were good and the SEM95% were relatively high with ± 4.53 mm for the femur and ± 3.12 mm for the tibia. Since the femur length shows no significant difference in the measurement of two different examiners, the measurement method for determining the center of the femoral head with the aid of a circle around the femoral head with the determination of the most distal points of the two femoral condyles does not seem to be examiner-dependent and could be seen as precise when analyzing the residual growth and correction potential with the multiplier method. Due to the slightly lower SEM95% in determining the tibial length, which were 1.64% of the total tibia length and ± 1.96% of the total femur length, the tibial length can be considered as precise as well. Again, it is important to know the error and include it in the analysis in predicting growth potential for each bone.
One limitation of this study is that it did not aim to identify differences in the experience of the two examiners. However, Vaishya et al. [45] showed that more experienced examiners tend to perform more precise measurements. Other studies (e.g., Gordon et al. [31]) did not find any experience-dependent differences in intra- or interobserver reliability with excellent agreement for all observers. In accordance with Vaishya et al. [45], we consider the measured values of this study to be highly reliable and reproducible and may not be improved with further experience of the observers.
In conclusion, a precise malalignment measurement and the knowledge about the presented SEM95% of the respective parameters are crucial for a correct surgical or nonsurgical treatment. The susceptibility to error must be included when interpreting malalignment analysis and must be considered when planning a surgical intervention. The ICC and SEM95% values in this study indicate how reproducible, reliable and precise radiological assessment of variables are obtained from an X-ray. In general, with any individual measurement, it should be understood that a measurement can never be determined exactly but is always subject to a certain measurement error or measurement inaccuracy. The same applies to anatomical standard values, which also have their physiological range. The results of this study elucidate that MAD and MFA show no different susceptibility to observer-dependent errors. In addition, due to no significant difference in determining the femoral length between two different observers and a lower SEM95% for tibial length by two different observers, both femoral and tibial length may be considered precise when analyzing the residual growth and correction potential for the respective bone, for instance, with the multiplier method. This study shows good to excellent intra- and interobserver ICCs for all leg alignment parameters and joint surface angles, except for JLCA. Furthermore, according to the SEM95% and proportional errors the determination of joint surface angels of the femur seems to be more precise than for the tibia. In unclear or borderline cases with marginal MAD and MFA, instrumented gait analysis and the determination of dynamic joint loading [4, 5, 11] should be included to determine whether surgical or nonsurgical treatment should be preferred.
Acknowledgements
Not applicable.
Abbreviations
- OA
Osteoarthritis
- THE
Temporary hemiepiphysiodesis
- SEM
Standard Error of Measurement
- MAD
Mechanical Axis Deviation
- MFA
Mechanical Femorotibial Angle
- JLCA
Joint Line Convergence Angle
- mLPFA
Mechanical Lateral Proximal Femur Angle
- mLDFA
Mechanical Lateral Distal Femur Angle
- mMPTA
Mechanical Medial Proximal Tibia Angle
- mLDTA
Mechanical Lateral Distal Tibia Angle
- ICC
Intraclass correlation coefficient
- SD
Standard deviation
Author contributions
SB, MB, JH, FS and AM were involved in the conception; SB, MB, and FS designed the work; SB and MB contributed to the acquisition and analysis; SB, MB, JH and FS assisted in the acquisition, analysis; SB and MB contributed to writing—original draft preparation; SB, MB, JH, FS and AM helped in writing—review and editing. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The institution of one or more of the authors (SB, MB, JH, FS, AM) has received funding from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation). Project number: 403837822. This study was registered with DRKS (German Clinical Trials Register) under the number DRKS00015053. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript or in the decision to publish the results.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Goethe University Frankfurt (protocol code: 182/16). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sebastian Braun and Marco Brenneis have contributed equally to this work and share first authorship
Andrea Meurer and Felix Stief have contributed equally to this work and share last authorship
Contributor Information
Sebastian Braun, Email: sebastian.braun@kgu.de.
Marco Brenneis, Email: marco.brenneis@kgu.de.
Jana Holder, Email: jana.holder@plus.ac.at.
Andrea Meurer, Email: andrea.meurer@kgu.de.
Felix Stief, Email: felix.stief@kgu.de.
References
- 1.Sharma L. Osteoarthritis of the Knee. N Engl J Med. 2021;384(1):51–59. doi: 10.1056/NEJMcp1903768. [DOI] [PubMed] [Google Scholar]
- 2.Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review Arthritis Rheum. 2009;61(4):459–467. doi: 10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- 3.Farr S, Kranzl A, Pablik E, Kaipel M, Ganger R. Functional and radiographic consideration of lower limb malalignment in children and adolescents with idiopathic genu valgum. J Orthop Res. 2014;32(10):1362–1370. doi: 10.1002/jor.22684. [DOI] [PubMed] [Google Scholar]
- 4.Böhm H, Stief F, Sander K, Hösl M, Döderlein L. Correction of static axial alignment in children with knee varus or valgus deformities through guided growth: Does it also correct dynamic frontal plane moments during walking? Gait Posture. 2015;42(3):394–397. doi: 10.1016/j.gaitpost.2015.06.186. [DOI] [PubMed] [Google Scholar]
- 5.Holder J, Feja Z, van Drongelen S, Adolf S, Böhm H, Meurer A, et al. Effect of guided growth intervention on static leg alignment and dynamic knee contact forces during gait. Gait Posture. 2020;78:80–88. doi: 10.1016/j.gaitpost.2020.03.012. [DOI] [PubMed] [Google Scholar]
- 6.Stief F, Böhm H, Schwirtz A, Dussa CU, Döderlein L. Dynamic loading of the knee and hip joint and compensatory strategies in children and adolescents with varus malalignment. Gait Posture. 2011;33(3):490–495. doi: 10.1016/j.gaitpost.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Vogt B, Schiedel F, Rödl R. Guided growth in children and adolescents. Correction of leg length discrepancies and leg axis deformities. Orthopade. 2014;43(3):267–84. doi: 10.1007/s00132-014-2270-x. [DOI] [PubMed] [Google Scholar]
- 8.Radtke K, Goede F, Schweidtmann K, Schwamberger T, Calliess T, Fregien B, et al. Temporary hemiepiphysiodesis for correcting idiopathic and pathologic deformities of the knee: a retrospective analysis of 355 cases. Knee. 2020;27(3):723–730. doi: 10.1016/j.knee.2020.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Hosseinzadeh P, Ross DR, Walker JL, Talwalkar VR, Iwinski HJ, Milbrandt TA. Three methods of guided growth for pediatric lower extremity angular deformity correction. Iowa Orthop J. 2016;36:123–127. [PMC free article] [PubMed] [Google Scholar]
- 10.Stief F, Feja Z, Holder J, van Drongelen S, Adolf S, Braun S, et al. Non-invasive determination of frontal plane lower limb alignment using motion capture technique—An alternative for full-length radiographs in young patients treated by a temporary hemiepiphysiodesis? Gait Posture. 2020;79:26–32. doi: 10.1016/j.gaitpost.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Stief F, Holder J, Böhm H, Meurer A. Dynamic analysis of joint loading due to leg axis deformity in the frontal plane: relevance of instrumented gait analysis. Orthopade. 2021;50(7):528–537. doi: 10.1007/s00132-021-04121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paley D, Pfeil J. Principles of deformity correction around the knee. Orthopade. 2000;29(1):18–38. doi: 10.1007/s001320050004. [DOI] [PubMed] [Google Scholar]
- 13.Radtke K, Gómez Dammeier B, Braun S. Radiographic analysis of limb malalignment in the frontal plane. Orthopade. 2021;50(7):520–527. doi: 10.1007/s00132-021-04125-5. [DOI] [PubMed] [Google Scholar]
- 14.Schnurr C, König DP. Achsfehlstellungen Knie. Orthopädie und Unfallchirurgie Essentials. 2. Stuttgart: Georg Thieme; 2013. [Google Scholar]
- 15.Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82(10):1432–1446. doi: 10.2106/00004623-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Birch JG, Makarov MR, Sanders JO, Podeszwa DA, Honcharuk EM, Esparza M, et al. Lower-extremity segment-length prediction accuracy of the Sanders multiplier, Paley multiplier, and White-Menelaus formula. J Bone Joint Surg Am. 2021;103(18):1713–1717. doi: 10.2106/jbjs.20.01923. [DOI] [PubMed] [Google Scholar]
- 17.Sanders JO, Howell J, Qiu X. Comparison of the Paley method using chronological age with use of skeletal maturity for predicting mature limb length in children. J Bone Joint Surg Am. 2011;93(11):1051–1056. doi: 10.2106/jbjs.J.00384. [DOI] [PubMed] [Google Scholar]
- 18.Paley D. Normal Lower Limb Alignment and Joint Orientation. Principles of Deformity Correction. Berlin, Heidelberg: Springer; 2002. [Google Scholar]
- 19.Hunt MA, Fowler PJ, Birmingham TB, Jenkyn TR, Giffin JR. Foot rotational effects on radiographic measures of lower limb alignment. Can J Surg. 2006;49(6):401–406. [PMC free article] [PubMed] [Google Scholar]
- 20.Jamali AA, Meehan JP, Moroski NM, Anderson MJ, Lamba R, Parise C. Do small changes in rotation affect measurements of lower extremity limb alignment? J Orthop Surg Res. 2017;12(1):77. doi: 10.1186/s13018-017-0571-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–749. doi: 10.2106/00004623-198769050-00016. [DOI] [PubMed] [Google Scholar]
- 22.Reina-Bueno M, Lafuente-Sotillos G, Castillo-Lopez JM, Gomez-Aguilar E, Munuera-Martinez PV. Radiographic assessment of lower-limb discrepancy. J Am Podiatr Med Assoc. 2017;107(5):393–398. doi: 10.7547/15-204. [DOI] [PubMed] [Google Scholar]
- 23.Streiner D. Health measurement scales: a practical guide to their development and use. Aust N Z J Public Health. 2016;40(3):294–5. doi: 10.1111/1753-6405.12484. [DOI] [PubMed] [Google Scholar]
- 24.Gamble P, de Beer J, Petruccelli D, Winemaker M. The accuracy of digital templating in uncemented total hip arthroplasty. J Arthroplasty. 2010;25(4):529–532. doi: 10.1016/j.arth.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 25.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. doi: 10.1519/15184.1. [DOI] [PubMed] [Google Scholar]
- 26.Mok JM, Berven SH, Diab M, Hackbarth M, Hu SS, Deviren V. Comparison of observer variation in conventional and three digital radiographic methods used in the evaluation of patients with adolescent idiopathic scoliosis. Spine. 2008;33(6):681–686. doi: 10.1097/BRS.0b013e318166aa8d. [DOI] [PubMed] [Google Scholar]
- 27.Wills BP, Auerbach JD, Zhu X, Caird MS, Horn BD, Flynn JM, et al. Comparison of Cobb angle measurement of scoliosis radiographs with preselected end vertebrae: traditional versus digital acquisition. Spine. 2007;32(1):98–105. doi: 10.1097/01.brs.0000251086.84420.d1. [DOI] [PubMed] [Google Scholar]
- 28.Shaarani SR, McHugh G, Collins DA. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties: a single surgeon series. J Arthroplasty. 2013;28(2):331–337. doi: 10.1016/j.arth.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 29.Brenneis M, Braun S, van Drongelen S, Fey B, Tarhan T, Stief F, et al. Accuracy of preoperative templating in total hip arthroplasty with special focus on stem morphology: a randomized comparison between common digital and three-dimensional planning using biplanar radiographs. J Arthroplasty. 2021;36(3):1149–1155. doi: 10.1016/j.arth.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Sled EA, Sheehy LM, Felson DT, Costigan PA, Lam M, Cooke TD. Reliability of lower limb alignment measures using an established landmark-based method with a customized computer software program. Rheumatol Int. 2011;31(1):71–77. doi: 10.1007/s00296-009-1236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gordon JE, Chen RC, Dobbs MB, Luhmann SJ, Rich MM, Schoenecker PL. Interobserver and intraobserver reliability in the evaluation of mechanical axis deviation. J Pediatr Orthop. 2009;29(3):281–284. doi: 10.1097/BPO.0b013e31819b9188. [DOI] [PubMed] [Google Scholar]
- 32.Schmale GA, Bayomy AF, O'Brien AO, Bompadre V. The reliability of full-length lower limb radiographic alignment measurements in skeletally immature youth. J Child Orthop. 2019;13(1):67–72. doi: 10.1302/1863-2548.13.180087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nowicki PD, Vanderhave KL, Farley FA, Kuhns LR, Dahl W, Caird MS. Reliability of digital radiographs for pediatric lower extremity alignment. J Pediatr Orthop. 2012;32(6):631–635. doi: 10.1097/BPO.0b013e3182694e07. [DOI] [PubMed] [Google Scholar]
- 34.Specogna AV, Birmingham TB, DaSilva JJ, Milner JS, Kerr J, Hunt MA, et al. Reliability of lower limb frontal plane alignment measurements using plain radiographs and digitized images. J Knee Surg. 2004;17(4):203–210. doi: 10.1055/s-0030-1248222. [DOI] [PubMed] [Google Scholar]
- 35.Feldman DS, Henderson ER, Levine HB, Schrank PL, Koval KJ, Patel RJ, et al. Interobserver and intraobserver reliability in lower-limb deformity correction measurements. J Pediatr Orthop. 2007;27(2):204–208. doi: 10.1097/01.bpb.0000242441.96434.6f. [DOI] [PubMed] [Google Scholar]
- 36.Ehnert M, Stief F, Meurer A. Axial deformities of the lower extremity in the frontal plane: from physiological development to pathological and possible long-term consequences. Orthopade. 2021;50(7):511–519. doi: 10.1007/s00132-021-04124-6. [DOI] [PubMed] [Google Scholar]
- 37.Gupta P, Gupta V, Patil B, Verma V. Angular deformities of lower limb in children: Correction for whom, when and how? J Clin Orthop Trauma. 2020;11(2):196–201. doi: 10.1016/j.jcot.2020.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stevens PM, Maguire M, Dales MD, Robins AJ. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19(5):645–649. doi: 10.1097/01241398-199909000-00018. [DOI] [PubMed] [Google Scholar]
- 39.Stief F, Holder J, Böhm H, Meurer A. Prevalence and predictors of rebound deformity in the frontal plane: a literature review. Orthopade. 2021;50(7):548–558. doi: 10.1007/s00132-021-04118-4. [DOI] [PubMed] [Google Scholar]
- 40.Saran N, Rathjen KE. Guided growth for the correction of pediatric lower limb angular deformity. J Am Acad Orthop Surg. 2010;18(9):528–536. doi: 10.5435/00124635-201009000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27(3):253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 42.Marques Luís N, Varatojo R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021;6(6):487–494. doi: 10.1302/2058-5241.6.210015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Radtke K, Becher C, Noll Y, Ostermeier S. Effect of limb rotation on radiographic alignment in total knee arthroplasties. Arch Orthop Trauma Surg. 2010;130(4):451–457. doi: 10.1007/s00402-009-0999-1. [DOI] [PubMed] [Google Scholar]
- 44.Whitaker AT, Vuillermin C. Lower extremity growth and deformity. Curr Rev Musculoskelet Med. 2016;9(4):454–461. doi: 10.1007/s12178-016-9373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vaishya R, Vijay V, Birla VP, Agarwal AK. Inter-observer variability and its correlation to experience in measurement of lower limb mechanical axis on long leg radiographs. J Clin Orthop Trauma. 2016;7(4):260–264. doi: 10.1016/j.jcot.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.