Abstract
Background:
Mothers of infants hospitalized in the Neonatal Intensive Care Unit (NICU) may experience a variety of psychological problems such as anxiety, depression, and stress. This study investigated the effect of midwife-based Listening Visit (LV) on stress, anxiety, and depression among mothers of premature infants in the NICU.
Materials and Methods:
This randomized clinical trial study was performed on 60 mothers of premature neonates who were admitted to the NICU of Taleghani Maternity Hospital between February and April 2018 in Arak, Iran. They were selected through simple random sampling. For the intervention group (n = 30), six counseling sessions were held twice a week. The control group (n = 30) did not receive any intervention. The mean values of stress, anxiety, and depression were measured before and 4 and 8 weeks after the intervention. Data were gathered using the Depression, Anxiety, Stress Scale-21 (DASS-21). The t-test and Chi-square test were used to analyze the data.
Results:
The mean scores of anxiety (F(2, 98) = 19.92, p < 0.001), stress (F(2, 98) = 43.94, p< 0.001), and depression (F(2, 98) = 42.95, p< 0.001) significantly reduced after 4 and 8 weeks of intervention in the LV group.
Conclusions:
LVs delivered by midwives can be effective in improving anxiety, stress, and depression in mothers of preterm infants in the NICU. Implementation of LV in the NICU resolves a recognized need and highlights the importance of psychological screening, and monitoring and support services for these mothers.
Keywords: Anxiety, counseling, depression, intensive care units, midwifery, neonatal, stress
Introduction
Anxiety and depression are negative and unpleasant emotions that are accompanied with stress, worry, and fear. These can occur throughout pregnancy because of uncertainties about maternal health during and after delivery, the time and place of birth, the baby's health, and the parental role. Previous studies have reported that 25% and 10%–15% of women experience anxiety and depression in the third trimester, respectively.[1,2] These issues increase with the birth of a preterm infant; a study conducted in Kenya reported increased levels of acute stress and high levels of anxiety in mothers of preterm infants in Neonatal Intensive Care Units (NICUs). These mothers had higher postpartum depression (77.6%) and anxiety (75%) levels compared to mothers of healthy full-term infants (22.4% depression and 25% anxiety).[2]
This is due to the fact that mothers of preterm infants in NICUs spend most of their time in the hospital and neglect their emotional health; even when screening detects signs of depression or anxiety, they often prioritize the needs of their hospitalized infants over their need for counseling. Therefore, the mothers probably do not give precedence to counseling sessions with a mental health professional. The basic need of this population of women is access to on-site treatment.[3,4] Relying on mental health professionals to provide therapies is likely to identify some of the barriers that prevent many women from receiving care, such as lack of trust or access, stigma, cost, and discomfort. In contrast, Listening Visit (LV) can be effectively delivered by reliable and accessible health providers in a convenient location, usually at no extra cost to women, and therefore, removing some treatment barriers. LV is an empirically supported nurse-delivered intervention that emphasizes communication building and identifies mother's problems through active reflexive listening and participatory problem-solving.[5] LV delivered by a nurse in the NICU can provide mothers who experience mild to moderate emotional distress with an appropriate first-line treatment approach without stigmatization.[6] A previous study showed that the mean stress score of NICU mothers significantly declined, but the mean stress score of fathers did not change after LV intervention.[7]
The main technique of this intervention is a two-part indirect counseling session; in the first part, the client's problem is detected, and in the second part, a suitable solution is presented to solve the problem after examining it and reflecting on it.[8] The intervention was first introduced in the 1980s by Jeni Holden and John Kax, a team of British psychologists/psychiatrists, as part of a program in which health-care providers were trained to diagnose and treat maternal depression in the UK. In the USA, LVs have been as effective in reducing depression and improving women's postpartum life satisfaction in community-based home visits as visits in the NICU.[9]
However, emotional distress is often undetected, and even when it is diagnosed, mothers are not always able to access emotional support outside the NICU setting. LV implementation in the setting could remove this limitation.[5,6] Mehdizadeh and Abbasi[10] quoted from Valizadeh et al. in Iran and Muk et al. in China that the nursing emotional support provided to mothers of preterm infants in the NICU was less than expected. The mothers expected more nursing emotional support than they received, and the nursing emotional support received by parents was insufficient.[10] The results of another study in Iran showed that the scores for support received were much lower than those in other countries and emotional support was considered as the most neglected field. The highest gap related to this field was between requested and received support, particularly in Iran.[11] Due to the growing trend of preterm birth, its resulting high mortality and morbidity, and the consequent maternal mental health issues,[12] and considering the lack of a study in this regard in Iran, the present study was conducted with the aim to evaluate the effect of midwife-based LV on stress, anxiety, and depression among mothers of premature infants hospitalized in the NICU.
Materials and Methods
The present randomized clinical trial study (IRCT20190301042875N1) was conducted on 60 mothers of premature infants in the NICU at the maternity hospital in the city of Arak, Iran, between February and April 2018. The convenience sampling method was used. A sample size of 54 individuals was necessary to show the differences between groups based on the Depression, Anxiety, Stress Scale-21 (DASS-21), which was calculated according to the sample size formula used in interventional studies. Considering p1 = 0.52, p2 = 0.48, 95% Confidence Interval (CI), and power test of 80%, 30 women were considered for each group. This number was increased to 60 subjects considering the probability of a 10% loss of subjects. The inclusion criteria for the mothers were age >18 years, lack of a previous premature infant with history of hospitalization in the NICU, lack of experience in caring for premature infants, absence of any underlying diseases affecting daily activities (such as rheumatoid arthritis, fractures or trauma to limbs, stage 3 [or higher] cardiovascular disease, orthopnea, and respiratory problems), absence of obvious psychological problems requiring medication (according to their personal statements), and lack of consumption of psychiatric drugs or drug addiction. The inclusion criteria for the infants were age 26–36 weeks, birth weight <2500 g, singleton birth, absence of congenital anomalies, and being in their first week of NICU hospitalization. The study exclusion criteria included diagnosis of grade 3 (or higher) Intraventricular Hemorrhage (IVH), death and early discharge of the infant, reluctance of mothers to continue participating in the study, sudden incidence of an acute debilitating disease, change of residence, and inability to communicate.
After selecting the subjects, ensuring that they met the inclusion criteria, and obtaining informed consent, the participants were randomly assigned to one of the two groups of intervention (n = 30) and control (n = 30) using a computer-generated randomization sequence of four blocks with an allocation ratio of 1. Data were gathered using a two-part questionnaire. The first part of the questionnaire was a demographic characteristics form for the mothers and their infants and was completed as a self-report by the mothers. This part included nine questions in the fields of age, job, residence, educational level, parity, mode of delivery, newborn's weight, Apgar score, and sex. The second part of the questionnaire was DASS-21.
DASS-21 is a standard self-report instrument that measures anxiety, depression, and stress. This questionnaire includes 21 questions in the three dimensions of anxiety, depression, and stress, each of which contains seven items (anxiety [items 2, 4, 7, 9, 15, 19, and 20], depression [items 3, 5, 10, 13, 16, 17, and 21], and stress [items 1, 6, 8, 11, 12, 14, and 18]). The items are scored based on a 4-point Likert scale ranging from 3 to 0 (always = 3, sometimes = 2, slightly = 1, none = 0). Thus, the score of each subscale is 0–21 and the overall score of the questionnaire is 0–63, with higher scores indicating more anxiety, depression, and stress. In one study, the validity of the depression, anxiety, and stress dimensions of the questionnaire were reported to be 0.72, 0.79, and 0.80 using Cronbach's alpha, respectively.[13] DASS-21 was completed by the participants in both groups before and 4 and 8 weeks after the intervention. In the intervention group, six group sessions of midwife-based LV (45–60 min) were held twice a week in a hospital class. A summary of the sessions held for the intervention group is presented in [Table 1].[3,9] No intervention was performed in the control group. To hide the assignment, random sequences were stored securely and separately from the participating database and were not accessible to researchers. It was not possible to blind researchers and participants due to the nature of the intervention. Data were analyzed using the Statistical Package for Social Sciences (SPSS) software (version 21; IBM Corp., Armonk, NY, USA). Descriptive statistics including mean (standard deviation [SD]) and inferential statistical tests such as paired t-test and repeated measures analysis of variance (ANOVA) were used for the main outcomes. An independent t-test was employed to compare infant's weight and age. χ2 test was used for the sex and Apgar score of the infants and the level of education, residence, parity, and employment status of the mothers.
Table 1.
Content of Listening Visits (LV) sessions
| Sessions | Content |
|---|---|
| First session | Greetings and introductions, description of the project goals, starting friendly talks and building trust between the clients and researcher, completion of the informed consent form and questionnaire |
| Second session | Summary of the previous session, answering questions of participants regarding uncertainties about the last session, focus and interaction around experiencing the birth of a premature infant, gradual change of focus to the needs and concerns, expansion of the treatment relationship, and making a more intimate relationship |
| Third session | Questions and answers about previous sessions and discussion on recent concerns, helping the mother explain her thoughts, feelings, and concerns through active reflexive listening by the consultant LV midwife |
| Fourth session | Summary of the past sessions, identifying problems, presenting solutions, and developing a practical plan for responding to issues and problems through participatory solution |
| Fifth session | Summary of previous sessions and feedback, review of the progress of the current sessions and identifying the next step, discussion on long-term goals and next steps by the midwifery LV counselor and mother |
| Sixth session | Reviewing the progress and celebrating the successes by the LV midwife and mother, assessment of the need for further mental health, termination of intervention, and therapeutic relationship |
LV=listening visit
Ethical considerations
This study was approved by the Research Ethics Committee of Arak University of Medical Sciences, Iran (IR.AMU.REC.1397.263). Date of registration: 2019-05-13. To comply with ethical standards, a research and ethics license was obtained from Arak University of Medical Sciences, the participants were provided with sufficient information, informed consent was obtained, and the principles of truthfulness and confidentiality were considered throughout the research process.
Results
Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) flow chart of the study. During the period we were considering, 109 individuals took part in the current study, 60 of whom met the inclusion criteria. Therefore, these 60 individuals were randomly assigned to the intervention (n = 30) or control (n = 30) group [Figure 1]. The results showed that participants of the intervention and control groups were homogeneous in terms of demographic characteristics and no significant difference was observed between them (p > 0.05). The mean (SD) age of mothers in the LV and control groups were 29.73 (5.30) and 31.62 (6.50) years, respectively [Table 2].
Figure 1.
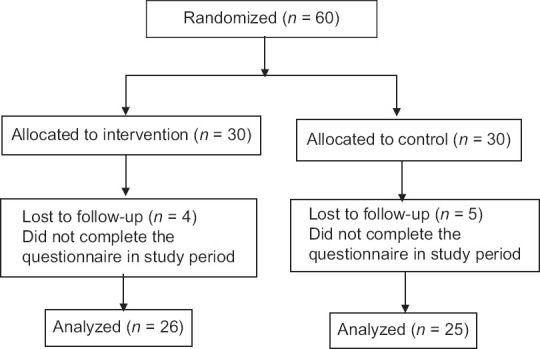
CONSORT diagram of the progress through the phases of a two-group parallel randomized trial
Table 2.
Demographic characteristics in the intervention and control groups at baseline (n=51)
| Intervention mean (SD) n=26 | Control mean (SD) n=25 | p | |
|---|---|---|---|
| Age (years) | 29.73 (5.30) | 31.62 (6.50) | 0.20a |
| Mean (SD) | |||
| Newborn's weight (g) | 1642.8 (426.9) | 1703.1 (526.1) | 0.66a |
| Mean (SD) | |||
| Apgar score (min), mean (SD) | |||
| First | 6.91 (2.10) | 7.12 (1.60) | |
| Fifth | 8.20 (1.60) | 8.32 (1.30) | 0.57a |
| n (%) | n (%) | ||
| Job | |||
| Housewife | 24 (92.26) | 25 (100) | 0.52b |
| Employee | 2 (7.74) | 0 (0.0) | |
| Residence | |||
| Urban | 20 (76.86) | 17 (68.0) | 0.55b |
| Rural | 6 (23.14) | 8 (32.0) | |
| Education level | |||
| Elementary | 10 (38.51) | 12 (48) | |
| Diploma | 9 (34.59) | 11 (44.0) | 0.53b |
| Academic | 7 (26.90) | 2 (8.0) | |
| Sex | |||
| Male | 16 (61.53) | 14 (56.0) | 0.19b |
| Female | 10 (38.47) | 11 (44.0) | |
| Mode of delivery | |||
| Cesarean | 21 (80.82) | 23 (92.0) | 0.25b |
| Vaginal | 5 (19.18) | 2 (8.0) | |
| Parity | |||
| 1-2 | 24 (92.31) | 21 (84.0) | 0.65b |
| ≥3 | 2 (7.69) | 4 (16.0) | |
SD=standard deviation. aIndependent t-test. bChi-square test
Based on the results, the effect of group and time interaction on anxiety was significant. The mean scores of anxiety differed between the study groups at different stages of the study. In the LV group, anxiety decreased 4 weeks after the intervention and continued to decrease in the eighth week after the intervention, but in the control group, this difference was not significant (F(2,98) = 19.92, p < 0.001). According to post hoc test, in the LV group, the mean scores of anxiety were significant 4 and 8 weeks after the intervention (p < 0.001). The effect of group and time interaction on stress was significant. The mean scores of stress differed between the study groups at different stages of the study. Considering the fact that the range of the stress score is 0–21 and higher scores are indicative of higher stress levels, the results showed that in the LV group, the stress level was lower after the intervention, while the stress level had increased in the control group. Comparison of mean stress level before and 4 and 8 weeks after the intervention in the LV group showed a significant difference; but in the control group, this difference was not significant (F(2, 98) = 43.94, p < 0.001). According to the post hoc test, in the LV group, the mean scores of stress were significant 8 weeks after the intervention (p < 0.001). The effect of group and time interaction on depression was significant. The mean score of depression differed between the study groups at different stages of the study. According to paired t-test, the mean score of depression was significant in the LV group compared to the control group before and 4 and 8 weeks after the intervention (F(2,98) = 42.95, p < 0.001). Based on the post hoc test, in the LV group, the mean scores of depression were significant 4 and 8 weeks after the intervention (p < 0.001) [Table 3].
Table 3.
Mean score of the DASS at three stages of the study in the intervention and control groups
| Study group variables | Mean (SD) |
F (pa) |
|||
|---|---|---|---|---|---|
| Intervention | Control | Group (between groups) | Time (within groups) | Time × group (within groups) | |
| Anxiety | |||||
| Before intervention | 9.19 (6.01) | 6.20 (4.83) | 1.69 (0.190) | 22.41 (0.001) | 19.92 (0.001) |
| 4 weeks after intervention | 3.61 (4.37) | 7.08 (6.91) | |||
| 8 weeks after intervention | 1.19 (2.29) | 5.64 (5.70) | |||
| Stress | |||||
| Before intervention | 12.15 (3.17) | 10.36 (4.78) | 12.14 (0.001) | 13.81 (0.001) | 43.94 (0.001) |
| 4 weeks after intervention | 8.50 (4.05) | 11.84 (3.64) | |||
| 8 weeks after intervention | 4.80 (3.23) | 12.44 (3.44) | |||
| Depression | |||||
| Before intervention | 9.96 (5.62) | 8.32 (5.87) | 8.44 (0.005) | 15.81 (0.001) | 42.95 (0.001) |
| 4 weeks after intervention | 4.76 (3.90) | 10.16 (5.36) | |||
| 8 weeks after intervention | 2.61 (2.99) | 9.96 (5.66) | |||
ANOVA=analysis of variance, DASS=Depression, Anxiety, Stress Scale. aRepeated measures ANOVA
Discussion
The present study was conducted to investigate the effect of midwife-based LV on stress, anxiety, and depression among mothers of premature infants in the NICU. The results showed statistically and clinically significant improvements in anxiety, stress, and depression of mothers of preterm infants in the NICU with LV delivered by midwives. This improvement was sustained until the 2-month post-LV follow-up.
Brock et al.[14] reported significant improvement in depressive symptoms of postpartum mothers 8 weeks after the LV intervention by nurses. Their results revealed the stability of LV delivered by nurses. Another study showed that six sessions of LV for mothers of NICU infants significantly improved maternal depression, anxiety, and mental health. The majority of participants benefited from these sessions and mothers' mental health improved 8 weeks after the intervention as well as our study.[3] Moreover, McCabe et al.,[5] in a meta-analysis, showed that considering the advantages afforded by how, where, and who delivers this treatment, LV can be considered as a first-line intervention in a step-by-step care manner for mothers with mild to moderate depression symptoms. LV counseling with the aid of the problem-solving skill can decrease depression in mothers of preterm infants.[9] The findings of these studies are in line with the present study findings. Chourasia et al.[15] examined the effect of counseling on the stress levels of NICU mothers. Like previous studies, interns (medical trainees) provided mothers with precise medical information on their neonates and their developmental states. The entire process lasted 30–45 min. They compared maternal stress before the intervention (6–8 days after the infant was admitted to the NICU) to that after the intervention (48 h after counseling). They showed that supportive counseling was effective in reducing stress of mothers with premature infants in the NICU. In our study, LV also had a supporting role that could reduce the mothers' stress. The findings of Chourasia et al.'s[15] research may be in line with our results; however, in our study, mothers received six counseling sessions with midwives and follow-up was 4 and 8 weeks after the intervention.
In contrast to the present study, Turner et al.[16] explored women's experiences of health visitor-provided LV as a treatment for postpartum depression with in-depth interviews. All the women reported the visits as helpful, but insufficient to manage their depression. Therefore, LV was less useful in women with a previous history of depression and in those whose depression was not attributed to postpartum events.[16] This may be due to the sample size; the sample size of their study was 22 individuals and the sample size of the present study was 60 individuals. As the sample size increases, the validation of the study will improve and generalization to the target population will be influenced.[17] Differences in the study approach can be considered as the other potential cause of the differences in results. The design of the study by Turner et al.[16] was qualitative with in-depth interviews, but our study design was interventional. Qualitative studies are the prerequisite of quantitative studies.[18]
Turan et al.[7] examined the effect of LV on reducing the stress of parents of premature infants admitted to the NICU. An approximately 30-min training program on their infants and the NICU was held for parents in the intervention group within the first week of the infant's admission to the NICU. The parents in the control group only received the routine unit procedures. The parents' stress scores were measured after the 10th day of NICU admission using the Parental Stressor Scale: Neonatal Intensive Care Unit (PSS: NICU) in both groups. The difference between the two groups in terms of the mothers' mean stress score was found to be statistically significant. However, the difference between the two groups in terms of the fathers' mean stress score was not significant. The findings of this study are not consistent with those of our study. The reasons for this difference may be the target population (parents vs. mothers), the scale (PSS: NICU vs. DASS-21), number and duration of sessions (one, 30 min vs. six, 45–60 min), and follow-up time (10th day vs. 4 and 8 weeks) after the intervention.
A strength of the study was that social stigma is often associated with mental health professionals/therapists; however, midwives often have a trusting relationship as a primary caregiver and are preferably positioned to provide stigma-free support. Moreover, midwives are physically available to mothers who do not want to leave their baby's bed. Finally, compared to most mental health professionals, midwives have significant medical knowledge that increases their understanding of mothers' concerns about their infants with medical problems and helps them in answering maternal medical questions. Due to time limitations, follow-up was performed 8 weeks after the intervention; it is recommended that mothers who answer DASS-21 be followed for a longer time. The mean weight of the neonates was between 1600 and 1700 g, and neonates weighting less than 1500 g were not included in the study. It is suggested that future studies comprehensively assess the demographic characteristics of preterm infants in the NICU.
Conclusion
LVs delivered by midwives can be effective in improving anxiety, stress, and depression in mothers of preterm infants in the NICU. This approach utilizes readily available and very reliable midwives to address maternal mental health problems.
Financial support and sponsorship
Nil.
Conflicts of interest
Nothing to declare.
Acknowledgements
The authors would like to thank the women for their willingness to participate to this study. This study was approved by the research committee of Arak University of Medical Sciences (approved code: 3111).
References
- 1.Vakilian K, Ghaemmaghami M, Sheikhganbari N, Shabani F, Vahedi M. Reducing labor anxiety with auriculotherapy: A randomized clinical trial study. Chin J Integr Med. 2022;28:440–4. doi: 10.1007/s11655-021-3452-0. [DOI] [PubMed] [Google Scholar]
- 2.Mutua J, Kigamwa P, Ng'ang'a P, Tele A, Kumar M. A comparative study of postpartum anxiety and depression in mothers with pre-term births in Kenya. J Affect Disord Rep. 2020;2:100043.. [Google Scholar]
- 3.Segre LS, Chuffo-Siewert R, Brock RL, O'Hara MW. Emotional distress in mothers of preterm hospitalized infants: A feasibility trial of nurse-delivered treatment. J Perinatol. 2013;33:924–8. doi: 10.1038/jp.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Segre LS, Orengo-Aguayo RE, Siewert RC. Depression management by NICU nurses: Mothers' views. Clin Nurs Res. 2015;25:273–90. doi: 10.1177/1054773815592596. [DOI] [PubMed] [Google Scholar]
- 5.McCabe JE, Wickberg B, Deberg J, Davila RC, Segre LS. Listening visits for maternal depression: A meta-analysis. Arch Womens Ment Health. 2021;24:595–603. doi: 10.1007/s00737-020-01101-4. [DOI] [PubMed] [Google Scholar]
- 6.Davila RC, Segre LS. A nurse-based model of psychosocial support for emotionally distressed mothers of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2018;47:114–21. doi: 10.1016/j.jogn.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Turan T, Başbakkal Z, Şenay Ö. Effect of nursing interventions on stressors of parents of premature infants in neonatal intensive care unit. J Clin Nurs. 2008;17:2856–66. doi: 10.1111/j.1365-2702.2008.02307.x. [DOI] [PubMed] [Google Scholar]
- 8.Scheiber FA, Segre LS, O'Hara MW, Taylor D, Brock RL. Maternal depression and breastfeeding in home visitation. Child Youth Serv Rev. 2020;119:105490.. doi: 10.1016/j.childyouth.2020.105490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siewert RC, Cline M, Segre LS. Implementation of an innovative nurse-delivered depression intervention for mothers of NICU infants. Adv Neonatal Care. 2015;15:104–11. doi: 10.1097/ANC.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehdizadeh S, Abbasi S, M PB. Nursing support and premature s infants in neonatal intensive care units: The views of mothers. Payesh. 2017;2:231–8. [Google Scholar]
- 11.Mousavi SS, Chaman R, Khosravi A, Mohagheghi P, Mousavi SA, Keramat A. The needs of parents of preterm infants in Iran and a comparison with those in other countries: A systematic review and meta-analysis. Iran J Pediatr. 2016;26:e4396.. doi: 10.5812/ijp.4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seiiedi-Biarag L, Mirghafourvand M, Esmaeilpour K, Hasanpour S. A randomized controlled clinical trial of the effect of supportive counseling on mental health in Iranian mothers of premature infants. BMC Pregnancy Childbirth. 2021;21:6.. doi: 10.1186/s12884-020-03502-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohammadbeigi A, Khavasi M, Golitaleb M, Jodaki K. The effect of peer group education on anxiety, stress, and depression in older adults living in nursing homes. Iran J Nurs Midwifery Res. 2021;26:252–7. doi: 10.4103/ijnmr.IJNMR_40_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brock RL, O'hara MW, Segre LS. Depression treatment by non-mental-health providers: Incremental evidence for the effectiveness of listening visits. Am J Community Psychol. 2017;59:172–83. doi: 10.1002/ajcp.12129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chourasia N, Surianarayanan P, Bethou A, Bhat V. Stressors of NICU mothers and the effect of counseling-experience from a tertiary care teaching hospital, India. J Matern Fetal Neonatal Med. 2013;26:616–8. doi: 10.3109/14767058.2012.743522. [DOI] [PubMed] [Google Scholar]
- 16.Turner KM, Chew-Graham C, Folkes L, Sharp D. Women's experiences of health visitor delivered listening visits as a treatment for postnatal depression: A qualitative study. Patient Educ Couns. 2018;78:234–9. doi: 10.1016/j.pec.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Polit Denise F, Tatano BC. 10th. Philadelphia: Lippincott, Williams & Wilkins; 2018. Essentials of Nursing Research: Appraising Evidence for Nursing Practice. [Google Scholar]
- 18.Rutberg S, Bouikidis CD. Focusing on the fundamentals: A simplistic differentiation between qualitative and quantitative research. Nephrol Nurs J. 2018;45:209–13. [PubMed] [Google Scholar]


