Abstract
Background and aims
The Short Gambling Harm Screen (SGHS) is currently the most frequently applied dedicated measure of gambling-related harm (GRH), though concerns relating to scale validity have been expressed. The current study aimed to address criticisms that several SGHS items do not depict genuine harms that may occur as a result of gambling, causing the scale to overestimate harm. Specifically, we aimed to test convergence between the SGHS and its constituent items with: (1) wellbeing, and (2) psychological distress.
Methods
To test criterion validity of both the scale and the items, retrospective analyses of survey data from 2,704 Australian adults (36% non-gamblers; 64% gamblers) were conducted. Subjective wellbeing and psychological distress scores, captured using the Personal Wellbeing Index (PWI) and the Kessler-6 Psychological Distress Scale (K6), respectively, were used as external (non-gambling) benchmarks. A total of 428 (16%) respondents scored at least 1 on the SGHS.
Results
Monotonic decreases and increases, corresponding to poorer personal wellbeing and higher psychological distress, were found with each additional SGHS score increase. Gamblers endorsing a single SGHS item reported lower wellbeing and higher psychological distress than both non-gamblers and gamblers who scored zero on the SGHS.
Discussion and conclusion
These results show that the SGHS is a valid measure of GRH and contradict suggestions that low scores on the SGHS do not indicate true harm. The SGHS represents a valid and innovative short screening tool to measure GRH in population prevalence studies.
Keywords: gambling, gambling harm, validation, SGHS, wellbeing, psychological distress
Introduction
Gambling is a common pastime in many jurisdictions (Browne et al., 2019; Rockloff et al., 2020; Salonen, Hellman, Latvala, & Castrén, 2018; Welte, Barnes, Tidwell, Hoffman, & Wieczorek, 2014) and is associated with a spectrum of negative consequences. These negative consequences are often referred to as gambling-related harm (GRH). GRH includes harm to relationships, finances, physical and mental health, school and job performance, and involvement in criminal activities (Langham et al., 2016). GRH is not exclusive to those classified as problem gamblers, impacting those who are considered at high, moderate, and low risk of having problems with gambling (Abbott et al., 2018; Browne, Greer, Rawat, & Rockloff, 2017; Langham et al., 2016). A population study of GRH in Victoria, Australia, found that 15% of the burden of disease from gambling came from those classified as problem gamblers, whereas over 50% of the burden of disease could be attributable to low-risk gamblers (Browne et al., 2016). These findings illustrate the risk in relying on problem gambler prevalence as a measure of gambling harm in the population. Accurately measuring GRH in the community is important as, until recently, policy and prevention has focussed almost exclusively on problem gamblers (Abbott et al., 2018), largely ignoring many of the of the individuals, families, and communities being harmed by gambling.
Measuring harm from gambling at a population-level is essential for providing policymakers with accurate data to improve public health outcomes. The Short Gambling Harm Screen (SGHS; Browne, Goodwin, & Rockloff, 2018) is a brief 10-item screen of GRH developed from a 72-item pool of harms (Langham et al., 2016). The screen's brevity facilitates inclusion in population and general research studies and is currently the most frequently applied dedicated measure of GRH. The Problem Gambling Severity Index (PGSI; Ferris & Wynne, 2001) is a commonly used proxy measures of gambling harm but, rather than capturing harms, is a population-level diagnostic screen for problem gambling, measuring symptoms of addiction such as chasing losses (Browne, Greer, et al., 2017). Other measures, such as the 107-item Gambling Effects Scale (GES), capture detailed information about harms experienced, but are currently not practical or available to use as a short screening tool suitable for population prevalence studies (Blaszczynski et al., 2015; Browne, Rawat, Tulloch, Murray-Boyle, & Rockloff, 2021).
The SGHS consists of 10 binary-scored items, each depicting a unique harm that can result from gambling consumption. Total scores on the screen can theoretically be used to estimate a respondent's underlying degree of GRH via conversion to corresponding health utility values (Browne et al., 2018), a way to measure health-related quality of life (HRQoL). HRQoL scores facilitate the direct comparison of impact on self-rated quality of life between diverse health conditions, based on the Global Burden of Disease model (Murray & Lopez, 1996). More research is needed to investigate standard health utility indices and other conversion procedures (e.g., weighting) for converting SGHS scores to HRQoL scores (Browne, Greer, et al., 2017a; 2017b, 2018). Despite this, the SGHS has typically been used to estimate the quantum of GRH a population or sub-population experiences at a given point in time.
A recent review of gambling harm literature has shown that the SGHS has been increasingly incorporated into academic and non-academic research methods for the purpose of estimating GRH in a population (Browne et al., 2021). However, given the relative short track-record of the SGHS, there are concerns about the screen's validity. Proponents of the SGHS have pointed to favourable psychometric features, such as high sensitivity, reliability, and unidimensionality, as evidence of its appropriateness for measuring GRH (Browne et al., 2017a, 2017b, 2018, 2021). Additionally, a recent study probing the screen's validity showed higher SGHS scores predicted a greater variety and severity of other gambling harms that are not part of the scale, as well as more severe problem gambling risk-categorisation (Murray Boyle, Browne, Rockloff, & Flenady, 2021).
Nevertheless, concerns have been expressed that some SGHS item content may not be severe enough to indicate genuine harms (Delfabbro, King, & Georgiou, 2020, 2021). Delfabbro, Georgiou, and King (2021) suggest that around half of the screen's constituent items may be better characterised as ‘opportunity costs’ or ‘substitutions of activities.’ That is, endorsement of these items may reflect rational trade-offs for the entertainment benefits of gambling. This trade-off argument raises concerns that the inclusion of these items in the SGHS may, therefore, inflate estimates of harm in the population. Consequently, an over-estimation of harm may lead to misallocation of resources that could be better allocated to individuals at-risk of, or currently experiencing, problem gambling (Delfabbro et al., 2020; Delfabbro & King, 2020).
Lacking a ‘gold standard’ measure of harm, one viable alternative is to validate the SGHS against criteria which are reliably associated with health utility. By definition, any item or screen intended to capture harm should also predict some degree of decrement to individuals' subjective sense of health and wellbeing (Fayers & Hays, 2000). Moreover, if the item or screen is associated with significant decrements to this benchmark, the argument that the measure is an invalid indicator of harm becomes very difficult to maintain. Similar validation approaches have been used to support other measures of consumption-derived harm, such as those for alcohol (Bondy & Lange, 2000) and e-cigarettes (Persoskie, Nguyen, Kaufman, & Tworek, 2017). Even within the field of gambling studies, exploring the relationship between gambling measures and health and wellbeing has a strong precedent. A recent study explored the convergence between scores on the PGSI and various chronic health outcomes (Browne et al., 2017; Rockloff et al., 2020). The PGSI shares similarity with the SGHS to the extent they both capture problems associated with gambling, though the two scales differ in purpose (Ferris & Wynne, 2001; Murray Boyle et al., 2021). The authors noted that different PGSI risk-categories had health state valuations comparable with various chronic illnesses or other health issues (e.g., problem gambler status was comparable with that of having a migraine disorder). Though this prior study was not intended as a validation of the PGSI, it contextualised gambling problems within a broader public health framework focused on reducing population-level morbidity.
The current study aimed to apply a similar approach to assessing the criterion validity of the SGHS. Specifically, we aimed to test convergence between the SGHS and its constituent items with: (1) wellbeing, and (2) psychological distress. Both outcomes are reasonably assumed to be associated with changes to health utility. However, the former incorporates multiple attributes (e.g., health, safety) (Cummins et al., 2001; International Wellbeing Group (IWG), 2013), while the latter is ‘mental’ suffering and, thus, is more specific in scope (Furukawa, Kessler, Slade, & Andrews, 2003; Wittchen, 2010).
Current study
As the SGHS is designed so that more item endorsements indicate increased harm, we expected higher SGHS scores to predict both lower wellbeing and higher psychological distress. Furthermore, if all the screen's constituent items are valid indicators of harm – rather than having negligible impact or reflecting rational opportunity costs – then endorsement of each SGHS item should be associated with poorer outcomes.
Given that critics have suggested that up to half of the SGHS's items may not be genuinely harmful, a low score would most likely include one or more of these items. If this critique should prove to be valid, we would expect to see a dilution effect, with relatively higher rates of endorsement of those specific items considered not genuinely harmful, as well as similar wellbeing scores in those respondents scoring one (1) on the SGHS as those scoring zero (0). Conversely, if gamblers who had not endorsed any SGHS items reported lower wellbeing than non-gamblers, this may suggest the SGHS is ‘missing’ some substantial harm associated with gambling, i.e., poor scale sensitivity.
Methods
Participants
Retrospective analyses of 2018–19 Victorian Population Gambling and Health Study (Rockloff et al., 2020) data were conducted to address the research questions. Telephone surveys of adult Victorians (n = 10,638) had been conducted between 2018–19 to collect a population-representative sample. Participants were sampled for the original study proportional to Australian Bureau of Statistics' Estimated Resident Population (ABS-ERP) demographic data for Victoria. As the filtered dataset used for the principal analyses, detailed below, did not have systematically varying demographic proportions to the original dataset, no cases were weighted in the current study.
To reduce the average time to complete the interviews, only a subset of people completed some parts of the survey. Participants who had not completed both the Kessler-6 Psychological Distress Scale (K6) and the Personal Wellbeing Index (PWI) were removed for the present analyses. The final dataset (n = 2,704) included 1,742 respondents who had gambled at least once in the twelve months prior to being surveyed (gamblers; 64%) and 962 who had not gambled during this period (non-gamblers; 36%).
Demographics
Participant age in years and gender (male/female/other) were collected from the sample dataset. Respondents were split evenly between two genders (male = 1,365, 50%) with an average age (M ≈ 53) somewhat higher than the median Australian adult (M = 45). Raw age values were recoded into four range categories (Age; 18–34; 35–49; 50–64; 65+). See Table 1 for the demographic breakdown.
Table 1.
SGHS items. Nominal harm category (Financial, Emotional/Psychological, Relationship), prevalence among all gamblers, percentage of male endorsers and mean age for each item displayed
| Demographic Variable | Category | n | % |
| Gambler Type | |||
| Non-Gambler | 962 | 35.6 | |
| Gambler, no SGHS endorsements | 1,314 | 48.6 | |
| Gambler, at least 1 SGHS endorsement | 428 | 15.8 | |
| Reduction of available spending money (Spend) | Financial | 239 | 13.7 |
| Reduction of your savings (Sav) | Financial | 186 | 10.7 |
| Less spending on recreational expenses… (Rec) | Financial | 129 | 7.4 |
| Had regrets…about your gambling (Regrets) | Psychological | 189 | 10.9 |
| Felt ashamed of your gambling (Shame) | Psychological | 124 | 7.1 |
| Sold personal items (Items) | Financial | 18 | 1.0 |
| Increased credit card debt (Credit) | Financial | 36 | 2.1 |
| Spent less time with people you care about (Time) | Relationship | 66 | 3.8 |
| Felt distressed about your gambling (Distress) | Psychological | 93 | 5.3 |
| Felt like a failure (Failure) | Psychological | 92 | 5.3 |
| Age | |||
| 18–34 | 625 | 23.2 | |
| 35–49 | 504 | 18.7 | |
| 50–64 | 700 | 25.9 | |
| 65+ | 875 | 32.3 | |
| Gender | |||
| Male | 1,365 | 50.5 | |
Measures
Short gambling harm screen
The SGHS consists of 10 binary-scored items, representing a range of possible gambling-related harms that are relatively common amongst frequent gamblers (Browne et al., 2018; Langham et al., 2016). Respondents were asked to endorse any items (e.g., Felt like a failure) attributable to their gambling that occurred within the 12 months prior to completing the survey. Each endorsement was scored as one and added to yield a SGHS score with a maximum of 10. Only participants who had gambled in the last 12 months were prompted to answer SGHS questions. Respondents were required to click yes or no to each item before proceeding, and therefore there was no missing data for this measure. Around one in four gamblers in the survey (n = 428, 16%) had endorsed at least one harm item (see Table 1).
Benchmark: Personal Wellbeing Index (PWI)
The SGHS items were tested against two distinct benchmarks: wellbeing, measured by the PWI, and psychological distress, measured by the K6. The PWI is an 8-item scale probing satisfaction with various aspects of wellbeing, e.g., health, relationships, safety (IWG, 2013). The PWI is a reliable and valid measure of wellbeing, reporting both strong unidimensionality and item (Pearson) differentiation among items (Cummins et al., 2001). It has been used in the context of gambling research previously (e.g., Blackman, Browne, Rockloff, Hing, & Russell, 2019) and was, therefore, considered a good predictor of latent wellbeing. Respondents completing the index rated their current satisfaction with each aspect of wellbeing from 0 (not at all satisfied) to 10 (completely satisfied). Ratings for each item were totalled and divided by the maximum scale score (80). This provided an estimate of respondents' perceived wellbeing as a percentage of their maximum ‘potential’ wellbeing.
Benchmark: Kessler 6 (K6)
Unlike the PWI, the Kessler-10 (K10) is primarily a diagnostic screen for acute psychological distress (IWD, 2013). The K6 is a 6-item truncation of the K10 and has been validated as a measure of population-level psychological distress with a variety of domestic and international cohorts (Furukawa et al., 2003; Wittchen, 2010). Each K6 item represents a different predictor of psychological distress, e.g., nervousness, hopelessness, worthlessness (see Furukawa et al., 2003). Respondents in the current study were required to estimate how frequently they experienced each predictor with a score from 0 (None of the time) to 4 (All of the time). Scores were added to a total K6 score that ranged from 0 to 24. In non-clinical populations, scores on this scale have a strong positive skew, with a long tail of infrequent and extreme manifestations of psychological distress.
Statistical analysis
First, to determine whether endorsement of each SGHS item led to the expected differences in wellbeing and psychological distress, mean PWI and K6 scores were compared between endorsers and non-endorsers of each SGHS item. Ten (10) one-tailed t-tests (one for each SGHS item) were conducted for each dependent variable. Bonferroni adjustments were applied to correct the alpha value and reduce the risks for inflation of type-I errors (α = 0.01, pcrit = 0.005).
Secondly, to test whether the SGHS total score predicted lower wellbeing and increased psychological distress, Spearman correlations were conducted between the SGHS and the outcome measures. To further probe changes as accumulations of SGHS endorsements increased, average scores at each SGHS value were compared for both outcomes. SGHS scores ranging from 7 to 10 were binned into a single category (7+) due to the low prevalence of these scores. PWI and K6 scores for non-gamblers (Non-G), and gamblers (1, 2, 3, 4, 5, 6, 7+) were then compared against gamblers who had the minimum SGHS score (0). T-tests were conducted for these comparisons using Bonferroni adjustments (α = 0.01).
Ethics
This study was conducted in accordance with the Declaration of Helsinki and approved by the Central Queensland Human Research Ethics Committee (21134). The current study analysed this retrospective data in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments.
Results
Effect of individual ‘substitution’ item endorsements
Table 2 shows mean (M) and standard error (SE) estimates of PWI and K6 scores in the current study for gamblers. Non-gamblers were excluded from this analysis. Separate averages were calculated for respondents who did and did not endorse each SGHS item. Scores on both the PWI and K6 differed significantly between endorsers and non-endorsers of every item.
Table 2.
Mean K6 and PWI scores for endorsers (0) and non-endorsers (1) of each SGHS item. Relative and statistical differences between endorsers' and non-endorsers’ average scores shown
| SGHS Items/Benchmark | M (SE) Endorsers |
M(SE) Non-endorsers |
ΔM ± 95 CI | t |
| Personal Wellbeing Index (PWI) | ||||
| Spend | 69.8 (1.1) | 78.9 (0.3) | −9.1 ± 2.3% | −8.73* |
| Sav | 68.7 (1.3) | 78.7 (0.3) | −10.0 ± 2.7% | −8.58* |
| Rec | 65.2 (1.7) | 78.6 (0.3) | −13.4 ± 3.4% | −9.88* |
| Regrets | 68.3 (1.4) | 78.8 (0.3) | −10.5 ± 2.7% | −9.11* |
| Shame | 65.8 (1.7) | 78.6 (0.3) | −12.8 ± 3.4% | −9.24* |
| Items | 54.8 (5.1) | 77.9 (0.3) | −23.1 ± 10.1% | −6.44* |
| Credit | 66.5 (3.2) | 77.9 (0.3) | −11.3 ± 6.4% | −4.44* |
| Time | 62.2 (2.6) | 78.3 (0.3) | −16.1 ± 5.2% | −8.63* |
| Distress | 59.9 (2.2) | 78.6 (0.3) | −18.7 ± 4.3% | −11.94* |
| Failure | 62.1 (2.1) | 78.5 (0.3) | −16.4 ± 4.1% | −10.29* |
| Kessler-6 Psychological Distress Scale (K6) | ||||
| Spend | 4.1 (0.1) | 6.7 (0.3) | 2.6 ± 0.7 | 8.62* |
| Sav | 4.2 (0.1) | 6.6 (0.4) | 2.3 ± 0.8 | 6.86* |
| Rec | 4.2 (0.1) | 8.1 (0.5) | 3.6 ± 1.0 | 9.87* |
| Regrets | 4.1 (0.1) | 7.2 (0.4) | 3.1 ± 0.8 | 9.21* |
| Shame | 4.2 (0.1) | 8.4 (0.5) | 4.2 ± 1.0 | 10.39* |
| Items | 4.4 (0.1) | 11.1 (1.3) | 6.6 ± 2.7 | 6.29* |
| Credit | 4.4 (0.1) | 8.7 (0.9) | 4.3 ± 1.9 | 5.75* |
| Time | 4.3 (0.1) | 8.5 (0.7) | 4.2 ± 1.4 | 7.51* |
| Distress | 4.2 (0.1) | 9.8 (0.6) | 5.6 ± 1.1 | 12.29* |
| Failure | 4.2 (0.1) | 9.3 (0.5) | 5.1 ± 1.2 | 10.88* |
*P < 0.001.
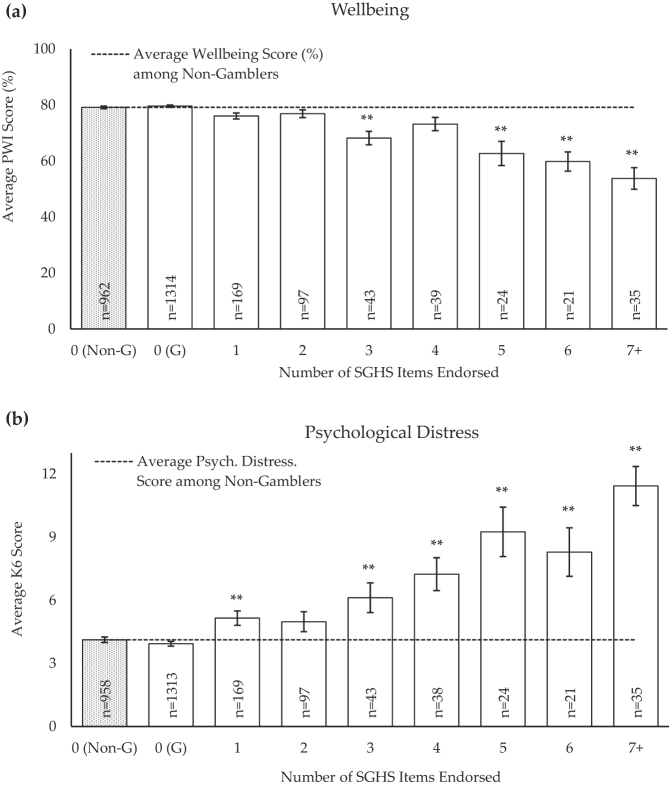
As expected, average wellbeing was reliably lower among endorsers than non-endorsers for every item (−0.09 > Δ > −0.23; Max. Error: SE = 5.1, P < 0.001), while psychological distress was consistently higher among endorsers (63.3% < Δ < 98.6%; Max. Error: SE = 1.3, P < 0.001). Endorsing any single SGHS item was associated with a decrement to overall wellbeing of between 9 and 23%, as well as an increase in psychological distress of 3–6 points on the K6 scale, depending on the item. As shown in Fig. 1, these differences were statistically significant in all cases, even inclusive of ‘milder’ harm symptoms such as reduction of available spending money, savings, and spending on recreational activities (Spend, Sav, Rec).
Fig. 1.
PWI (a) and K6 (b) means and standard errors among Non-Gamblers (Non-G) and respondents with various SGHS scores [0, 1, 2, 3, 4, 5, 6, 7+]. **P < 0.004 (αcrit = 0.996)
Effect of multiple ‘substitution’ item endorsements
Wellbeing
Table 2 shows gamblers endorsing zero SGHS items reported similar average wellbeing (0 = 79.59%, SE0 = 0.4) as non-gamblers (NG = 79.14%, SENG = 0.5; t (92,274) = −0.74, P < 0.460, ns). However, wellbeing decreased with endorsement of each item in the SGHS, with progressively lower wellbeing with more items selected (see Fig. 1a). In summary, there was a negative linear relationship between the SGHS total score and the PWI (Spearman r = −0.23, P < 0.001).
Psychological distress
Similarly to the PWI, there was no difference in average K6 score between gamblers who did not endorse any SGHS items (0 = 3.93, SE = 0.11) and non-gamblers (NG = 4.12, SE = 0.13; t (1,534) = 0.38, P = 0.704, ns). Figure 1b shows psychological distress increased as more subscale items were endorsed. Moreover, there was a positive linear association between the two scales (Spearman r = 0.24, P < 0.001; see Table 2).
Discussion
The current study sought to validate the SGHS and each of its items against two external benchmarks of harm: wellbeing and psychological distress. We found that all 10 items individually predicted both benchmarks in the directions expected: wellbeing was lower and psychological distress was higher among endorsers of each item. For the scale as a whole, higher SGHS scores were associated with progressively worse scores on both outcomes. Psychological distress increased, however, with a greater magnitude than wellbeing decreased. This is likely due to the PWI capturing a broader range of outcomes than the K6, which specifically only captures psychological distress. Taken together, these results suggest that endorsement of any SGHS item predicts some degree of imputed harm, and upon multiple endorsements, these items become incrementally better predictors of decrements to wellbeing.
Notably, gamblers endorsing as few as one SGHS item reported lower wellbeing than gamblers not endorsing any, as well as non-gamblers. Wellbeing did not differ significantly between gamblers who did not endorse any SGHS items and non-gamblers. These results taken together suggest that claims to the SGHS's sensitivity are supported, as well as the ability of the scale to capture some degree of harm, defined in this instance by decrement to personal wellbeing, even at the minimum positive value (i.e., +1 harm). Since both low scores, i.e., 1–2, on the SGHS and each individual item are associated with decrements to these benchmarks, the results do not support the suggestion that certain item content in the SGHS reflect only rational costs of consumption or are too mild to be meaningful. Instead, every item is associated with decrements to wellbeing and increases in psychological distress.
The differences in mean K6 and PWI scores are comparable to the differences seen in other studies that use these measures. For example, a study examining the outcomes of a psychological interventions in a vulnerable population (men who have sex with men) reported mean reduction in K6 scores of 4.0 and a mean increase in PWI score of 11.8. The PWI differences we observed are in the order of 10–20 points, and for the K6, two to six points. This comparison illustrates that the changes we observed in psychological distress and wellbeing are comparable to those seen in the wider literature in response to significant events, lending weight to the effect sizes observed.
The results from the current study support previous work validating the SGHS. Endorsing one or more SGHS items has been demonstrated to be associated with lower wellbeing in a multi-jurisdictional online sample of 1,524 past year gamblers (Browne et al., 2018). A similar pattern was observed in this study as in the current study, with a generally linear negative relationship between the number of harms endorsed on the SGHS and personal wellbeing score. The current findings also support the recent wider conceptualisation of harm from gambling manifesting in a decrement to health and wellbeing (Browne, Rawat, et al., 2017; Langham et al., 2016).
The current study has major implications for the detection of GRH in the community. Until recently, the main measures used to quantify harm from gambling in population studies have been problem gambling diagnostic screens (e.g., Abbott, Bellringer, Garrett, & Mundy-McPherson, 2014; Billi, Stone, Marden, & Yeung, 2014; Public Health Agency of Sweden, 2016). The current study demonstrates the validity of the SGHS and its application for use as a more accurate measure of population-level harm from gambling. Adopting a public health approach to gambling has been advocated since the 1990s (Korn & Shaffer, 1999) and the SGHS operationalises this shift in focus from problem gambling to harms from gambling. The findings from the current study also have implications clinically in the early detection of harmful gambling. Current diagnostic screens, such as the PGSI, currently categorise individuals according to their risk of having a gambling problem, meaning that those categorised at low risk are likely treated similarly to those at no risk, i.e., receive no treatment. As the current study has demonstrated that each endorsement of an individual harm on the SGHS is associated with a reduction in wellbeing and an increase in psychological distress, using the SGHS in a primary care setting would facilitate immediate intervention to prevent of more harm occurring and reduce the likelihood of transition to problem gambling.
Limitations
The current research lays out a potential avenue for a standardised conversion of SGHS scores to wellbeing scores or health-utility decrements. However, a larger sample of population-representative data would help determine more precise estimates at each SGHS value, bolstering the utility and applicability of the screen. Additionally, the current study is limited by its use of data from a single jurisdiction – Victoria, Australia – with relatively high per-capita consumption of electronic gambling machines (Rockloff et al., 2020). Further research is required to determine whether the SGHS is a valid measure of GRH in jurisdictions with different preferences and availability of gambling activities. Despite these limitations, the SGHS and its constituent items have been demonstrated to be associated with external markers of harm, further bolstering claims of its validity.
Conclusion
This study supports the validity of the SGHS as a measure of gambling harm. Moreover, it shows that every item on the SGHS has positive value in predicting decrements to wellbeing and increases in psychological distress. Importantly, these measures of dysfunction have no direct questions about gambling harm or problems and, therefore, are objective benchmarks for determining the effectiveness of the scale. The study provides some additional confidence that the SGHS has distinct utility in understanding how people can suffer harm from use of gambling products, even at a level that may have previously been categorised as no or low risk.
Funding sources
No financial support was received for this study.
Authors’ contribution
CMB and MB were responsible for project conceptualisation and planning. MB was responsible for sourcing appropriate data and advising on analysis methods. CMB conducted statistical analyses and drafted the manuscript. MB and MJR provided supervision, advised on methodology, edited, and contributed to the manuscript. HBT assisted in conducting the statistical analyses and writing and editing the manuscript. All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare no conflict of interest in relation to this work. In the past three years, MB has received funding from the NZ Ministry of Health, VRGF, the Queensland Department of Health, the Tasmanian Department of Treasury and Finance, the Alberta Gambling Research Institute, the First Nations Foundation, NSW Office of Responsible Gambling and Gambling Research Australia. MJR has also received funding from these sources and has additionally received funding from the Department of Social Services (Federal), the Queensland Treasury, and the Victorian Department of Justice. HBT has received funding from VRGF, NSW Office of Responsible Gambling and Gambling Research Australia.
Contributor Information
Cailem Murray Boyle, Email: cailem.murrayboyle@cqumail.com.
Matthew Browne, Email: m.browne@cqu.edu.au.
Matthew J. Rockloff, Email: m.rockloff@cqu.edu.au.
Hannah B. Thorne, Email: h.thorne@cqu.edu.au.
References
- Abbott, M., Bellringer, M., Garrett, N., & Mundy-McPherson, S. (2014). New Zealand 2012 national gambling study: Gambling harm and problem gambling. New Zealand Ministry of Health. https://www.health.govt.nz/system/files/documents/publications/national-gambling-study-report-2.pdf. [Google Scholar]
- Abbott, M., Binde, P., Clark, L., Hodgins, D., Johnson, M., Manitowabi, D., … Williams, R. (2018). Conceptual framework of harmful gambling: An international collaboration (3rd ed.). Gambling Research Exchange Ontario (GREO). 10.33684/CFHG3.en. [DOI] [Google Scholar]
- Billi, R., Stone, C. A., Marden, P., & Yeung, K. (2014). The victorian gambling study: A longitudinal study of gambling health in Victoria, 2008–2012. Victorian Responsible Gambling Foundation. 10.11575/PRISM/9829. [DOI] [Google Scholar]
- Blackman, A., Browne, M., Rockloff, M., Hing, N., & Russell, A. (2019). Contrasting effects of gambling consumption and gambling problems on subjective wellbeing. Journal of Gambling Studies, 35, 773–792. 10.1007/s10899-019-09862-z. [DOI] [PubMed] [Google Scholar]
- Blaszczynski, A., Anjoul, F., Shannon, K., Keen, B., Pickering, D., & Wieczorek, M. (2015). Gambling harm minimisation report. NSW Government Department of Trade & Investment; Office of Liquor Gambling and Racing. https://www.responsiblegambling.nsw.gov.au/__data/assets/pdf_file/0011/878303/gambling-harm-minimisation-report.pdf. [Google Scholar]
- Bondy, S. J., & Lange, P. (2000). Measuring alcohol-related harm: Test-retest reliability of a popular measure. Substance Use & Misuse, 35(9), 1263–1275. 10.3109/10826080009147481. [DOI] [PubMed] [Google Scholar]
- Browne, M., Goodwin, B. C., & Rockloff, M. J. (2018). Validation of the Short Gambling Harm Screen (SGHS): A tool for assessment of harms from gambling. Journal of Gambling Studies, 34, 499–512. 10.1007/s10899-017-9698-y. [DOI] [PubMed] [Google Scholar]
- Browne, M., Greer, N., Rawat, V., & Rockloff, M. (2017a). A population-level metric for gambling-related harm. International Gambling Studies, 17(2), 1–14. 10.1080/14459795.2017.1304973. [DOI] [Google Scholar]
- Browne, M., Langham, E., Rawat, V., Greer, N., Li, E., Rose, J., … Best, T. (2016). Assessing gambling-related harm in Victoria: A public health perspective. Melbourne, Australia: Victoria Responsible Gambling Foundation. 10.11575/PRISM/9419. [DOI] [Google Scholar]
- Browne, M., Rawat, V., Greer, N., Langham, E., Rockloff, M., & Hanley, C. (2017b). What is the harm? Applying a public health methodology to measure the impact of gambling problems and harm on quality of life. Journal of Gambling Issues, 36. 10.4309/jgi.2017.36.2. [DOI] [Google Scholar]
- Browne, M., Rawat, V., Tulloch, C., Murray-Boyle, C., & Rockloff, M. (2021). The evolution of gambling-related harm measurement: Lessons from the last decade. International Journal of Environmental Research and Public Health, 18(9). 10.3390/ijerph18094395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne, M., Rockloff, M., Hing, N., Russell, A., Murray Boyle, C., Rawat, V., … Sproston, K. (2019). NSW gambling survey 2019. NSW Responsible Gambling Fund, NSW Government. https://www.responsiblegambling.nsw.gov.au/__data/assets/pdf_file/0008/881279/NSW-Gambling-Survey-2019-report-FINAL-AMENDED-Mar-2020.pdf. [Google Scholar]
- Cummins, R., Eckersley, R., Pallant, J., Van Vugt, J., Shelley, J., Pusey, M., & Misajon, R. (2001). Australian unity wellbeing index (report No. 1). Australian Centre on Quality of Life, Deakin University. http://acqol.deakin.edu.au/index_wellbeing/index.htm. [Google Scholar]
- Delfabbro, P., Georgiou, N., & King, D. L. (2021). Measuring gambling harm: The influence of response scaling on estimates and the distribution of harm across PGSI categories. Journal of Gambling Studies, 37(2), 583–598. 10.1007/s10899-020-09954-1. [DOI] [PubMed] [Google Scholar]
- Delfabbro, P., & King, D. L. (2020). Don’t say the “P” word: Problem gambling is more than harm. International Journal of Mental Health and Addiction, 18(3), 835–843. 10.1007/s11469-020-00274-4. [DOI] [Google Scholar]
- Delfabbro, P., King, D., & Georgiou, N. (2020). Opportunity cost and gambling: Distinguishing between competing activities and harm. Journal of Gambling Issues, 44. 10.4309/jgi.2020.44.9. [DOI] [Google Scholar]
- Fayers, P., & Hays, R. (2000). Assessing quality of life in clinical trials (2nd ed.). Oxford University Press, 2005. [Google Scholar]
- Ferris, J., & Wynne, H. (2001). The Canadian problem gambling index: Final report. Canadian. [Google Scholar]
- Furukawa, T. A., Kessler, R. C., Slade, T., & Andrews, G. (2003). The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine, 33(2), 357–362. 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- International Wellbeing Group (IWG) (2013). Personal wellbeing index – adult (PWI-A) (5th ed.). Australian Centre on Quality of Life, Deakin University. https://www.acqol.com.au/uploads/pwi-a/pwi-a-english.pdf. [Google Scholar]
- Korn, D. A., & Shaffer, H. J. (1999). Gambling and the health of the public: Adopting a public health perspective. Journal of Gambling Studies, 15(4), 289–365. 10.1023/a:1023005115932. [DOI] [PubMed] [Google Scholar]
- Langham, E., Thorne, H., Browne, M., Donaldson, P., Rose, J., & Rockloff, M. (2016). Understanding gambling related harm: A proposed definition, conceptual framework, and taxonomy of harms. BMC Public Health, 16(80). 10.1186/s12889-016-2747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray Boyle, C., Browne, M., Rockloff, M., & Flenady, T. (2021). Opportunity costs or not? Validating the short gambling harm screen against a set of “unimpeachable” negative impacts. Journal of Clinical Medicine, 10(3). https://www.mdpi.com/983860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, C. J. L., & Lopez, A. D. (Eds.), (1996). The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Harvard School of Public Health. http://apps.who.int/iris/bitstream/handle/10665/41864/0965546608_eng.pdf;jsessionid=4DC0AE9B88E7526CF09E73D6DEADC9AC?sequence=1. [Google Scholar]
- Persoskie, A., Nguyen, A. B., Kaufman, A. R., & Tworek, C. (2017). Criterion validity of measures of perceived relative harm of e-cigarettes and smokeless tobacco compared to cigarettes. Addictive Behaviors, 67, 100–105. 10.1016/j.addbeh.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Sweden (2016). Gambling and gambling problems in Sweden 2008–2010. https://www.folkhalsomyndigheten.se/contentassets/fe1d3ba6e62a40158a8188bb3b83b9c5/gambling-gambling-problems-sweden-2008-2010-16013.pdf.
- Rockloff, M., Browne, M., Hing, N., Thorne, H., Russell, A., Greer, N., … Sproston, K. (2020). Victorian population gambling and health study 2018–2019. Victorian Responsible Gambling Foundation. https://responsiblegambling.vic.gov.au/documents/759/Population_study_2018_2019_PUBLISHED_REPORT_March_2020.pdf. [Google Scholar]
- Salonen, A. H., Hellman, M., Latvala, T., & Castrén, S. (2018). Gambling participation, gambling habits, gambling-related harm, and opinions on gambling advertising in Finland in 2016. Nordisk Alkohol- & Narkotikatidskrift: NAT, 35(3), 215–234. 10.1177/1455072518765875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welte, J. W., Barnes, G. M., Tidwell, M.-C. O., Hoffman, J. H., & Wieczorek, W. F. (2014). Gambling and problem gambling in the United States: Changes between 1999 and 2013. Journal of Gambling Studies, 31(3), 695–715. 10.1007/s10899-014-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen, H.-U. (2010). Screening for serious mental illness: Methodological studies of the K6 screening scale. International Journal of Methods in Psychiatric Research, 19(Suppl 1), 1–3. 10.1002/mpr.316. [DOI] [PMC free article] [PubMed] [Google Scholar]