Abstract
Background
COVID-19 had a significant impact on Emergency Departments (ED) with early data suggesting an initial decline in avoidable ED visits. However, the sustained impact over time is unclear. In this study, we analyzed ED discharges over a two-year time period after the COVID-19 pandemic began and compared it with a control time period pre-pandemic to evaluate the difference in ED visit categories, including total, avoidable, and unavoidable visits.
Methods
This was a retrospective, cross-sectional study assessing the distribution of visits with ED discharges from two hospitals within a health system over a three-year time period (1/1/2019–12/31/2021). Visits were categorized using the expanded NYU-EDA algorithm modified to include COVID-19-related visits. Categories included: Emergent - Not Preventable/Avoidable, Emergent – Preventable/Avoidable, Emergent - Primary Care Treatable, Non-Emergent, Mental Health, Alcohol, Substance Abuse, Injury, and COVID-19. Chi-square testing was conducted to investigate differences within the time period before COVID-19 (1/1/2019–12/31/2019) and both initial (1/1/2020–12/31/2020) and delayed (1/1/2021–12/31/2021) COVID-19 time frames and ED visit categories, as well as post hoc testing using Fisher's exact tests with Bonferroni correction. ANOVA with post hoc Bonferroni testing was used to determine differences based on daily census for each ED visit category.
Results
A total of 228,010 ED discharges (Hospital #1 = 126,858; Hospital #2 = 101,152) met our inclusion criteria over the three-year period. There was a significant difference in the distribution of NYU-EDA categories between the two time periods (pre-COVID-19 versus during COVID-19) for the combined hospitals (p < 0.001), Hospital #1 (p < 0.001), and Hospital #2 (p < 0.001). When examining daily ED discharges, there was a decline in all categories from 2019 to 2020 except for “Emergent - Not Preventable/Avoidable” which remained stable and “Substance Abuse” which increased. From 2020 to 2021, there were no differences in ED avoidable visits. However, there were increases in discharged visits related to “Injuries”, “Alcohol”, and “Mental health” and a decrease in “COVID-19”.
Conclusion
Our study identified a sustained decline in discharged avoidable ED visits during the two years following the beginning of the COVID-19 pandemic, which was partially offset by the increase in COVID-19 visits. This work can help inform ED and healthcare systems in resource allocation, hospital staffing, and financial planning during future COVID-19 resurgences and pandemics.
Keywords: COVID-19, Avoidable visits, Emergency departments, Administration
1. Introduction
The coronavirus disease of 2019 (COVID-19) had a profound impact on healthcare systems worldwide [1]. As of December 2022, there have been 655 million cases worldwide with over 6.6 million deaths [2]. This has led to a large influx of patients presenting to hospitals with initial and delayed sequelae of COVID-19. However, this was counterbalanced by state and local initiatives, such as stay-at-home orders and emphasis on outpatient testing, as well as hospital-based efforts to conserve resources for the critically ill patients (e.g., cancellation of elective procedures) [3]. Moreover, patients may have feared potential exposure to COVID-19, prompting them to avoid necessary medical care [4].
The Emergency Department (ED) is often at the front lines, serving as a primary point of entry for patients with acute conditions and those being admitted to the hospital, as well as a safety net for individuals with limited access to outpatient care. While this serves a critical role for society, increasing volumes and length-of-stay can tax already limited resources [5]. Studies conducted prior to COVID-19 have reported that approximately one-third of all ED visits are non-urgent or avoidable, wherein a patient could be evaluated and treated outside the ED setting (e.g., physician's office, retail clinic, urgent care, virtual care) [6]. In fact, one study reported that seeking care outside of the ED in these settings could save approximately $4.4 billion in healthcare costs per year [7].
Early data on COVID-19 demonstrated an acute reduction in total ED visits [[8], [9], [10], [11], [12]]. This decline was most notable for non-urgent visits [13,14]. However, these data were primarily limited to early in the pandemic period, with limited understanding of the impact on avoidable ED visits over time. This is particularly relevant given the increased understanding of COVID-19, changes in public health measures, and access to vaccination. As such, there is a need to better understand the trend in both avoidable and unavoidable ED visits over a longer time period in order to inform stakeholders and healthcare policymakers when developing interventions to reduce avoidable ED visits and improve the efficiency of care during COVID-19 and beyond.
In this study, we sought to analyze ED discharges for a two-year time period after the COVID-19 pandemic began and compare it with a control time period pre-pandemic to evaluate the initial (January to December 2020) and delayed (January to December 2021) impact on total, avoidable, and unavoidable ED visits across two hospitals in a single health system.
2. Methods
This was a retrospective, cross-sectional study assessing the distribution of ED discharges across two hospitals in a health system with arrival dates between January 1, 2019 to December 31, 2021. We followed best practices in observational research and adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [15]. The study was conducted using data from two separate hospitals in Illinois. Hospital #1 (Rush University Medical Center [RUMC]) is a 707-bed urban tertiary care hospital in Chicago, IL with an annual ED volume of 70,000 patients per year. Hospital #2 (Rush Oak Park Hospital [ROPH]) is an 87-bed urban primary hospital in Oak Park, IL with an annual ED volume of 50,000 patients per year. Both hospitals have an established, shared enterprise data warehouse (EDW), which is managed by Rush. The EDW is maintained as a long-term data mart for patient medical, financial, and administrative data. This single source EDW supports all clinical, research, and operational data needs for the organization. The Rush University Medical Center institutional review board evaluated this project and approved it with a waiver of informed consent. There was no funding for this study.
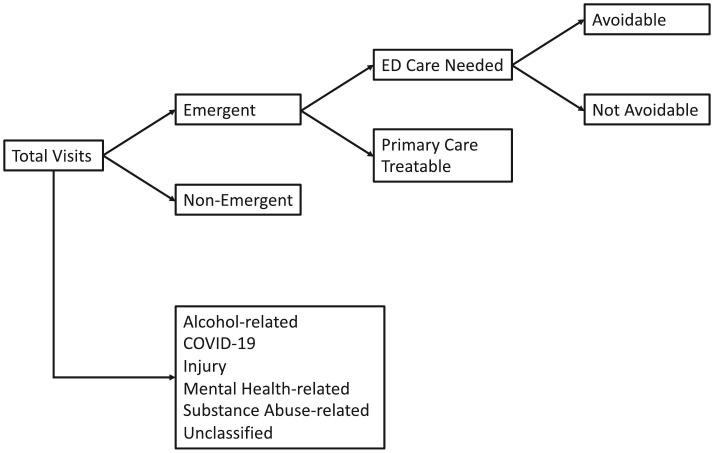
This study utilized data for all patients who were discharged from the ED. Patients of all ages were included. The urgency of a visit was categorized using the New York University Emergency Department Algorithm (NYU-EDA) [[16], [17], [18]], and was modified to include a breakout for COVID-19 related visits. The NYU-EDA (Fig. 1 ) consists of four severity categories (Emergent – Not Preventable/Avoidable, Emergent – Preventable/Avoidable, Emergent – Primary Care Treatable, and Non-Emergent) and four expanded categories (Mental Health, Alcohol, Substance Abuse, and Injury) [16]. The primary ICD-10 diagnosis codes were used to assign patients to either one of the four expanded categories or assign them to probabilities of being in each of the four severity categories (summing to a total of 100% across the 4 severity categories). For this study, visits were classified as one of the NYU-EDA categories by assigning the category if the probability for a given category was >50% according to the criteria set forth by Ballard et al. [18]. If an individual visit did not map to a specific category with >50% probability, they were assigned a default grouping of “Unclassified”. We also added an additional group for COVID-19, as this did not exist at the time when the NYU-EDA algorithm was created. These consisted of the following four ICD-10 codes: U07.1, Z11.52, Z20.822, and Z86.16. Consequently, 10 total categories were included in the analysis (Emergent – Not Preventable/Avoidable, Emergent – Preventable/Avoidable, Emergent – Primary Care Treatable, Non-Emergent, Mental Health, Alcohol, Substance Abuse, Injury, COVID-19, and Unclassified). In addition to total volumes, we also captured the daily census data for the study population to compare each category of ED visit by hospital.
Fig. 1.
Schematic diagram of NYU-EDA model. Adapted fromhttps://wagner.nyu.edu/faculty/billings/nyued-background.
Descriptive statistics (count and proportion) for ED visit categories and daily census by each category of ED visit were computed for the time period before COVID-19 (1/1/2019–12/31/2019) and both the initial (1/1/2020–12/31/2020) and delayed (1/1/2021–12/31/2021) COVID-19 time frames. Chi-square tests were conducted to investigate overall differences in NYU-EDA categories (dependent variable) in the pre and during COVID-19 time frames (independent variable). For each hospital and the combined data for both hospitals, we performed Fisher's exact tests with a Bonferroni correction [19]. Based upon 30 comparisons between observed and expected counts per combination of NYU-EDA categories and COVID-19 time frames, the corrected p-value was p < 0.00167 (0.05/30). To analyze the differences between each time frame (2019, 2020, and 2021) and daily census by each NYU-EDA category, ANOVA with post hoc Bonferroni tests were used. The analysis was performed for the combined data for both hospitals. We also reported data for each individual hospital. All statistical tests utilized significance levels of 5% except for post hoc Bonferroni tests. We also conducted a sensitivity analysis removing the COVID-19 category. All data analyses were conducted using Python, Microsoft Excel, and SPSS (Version 26).
3. Results
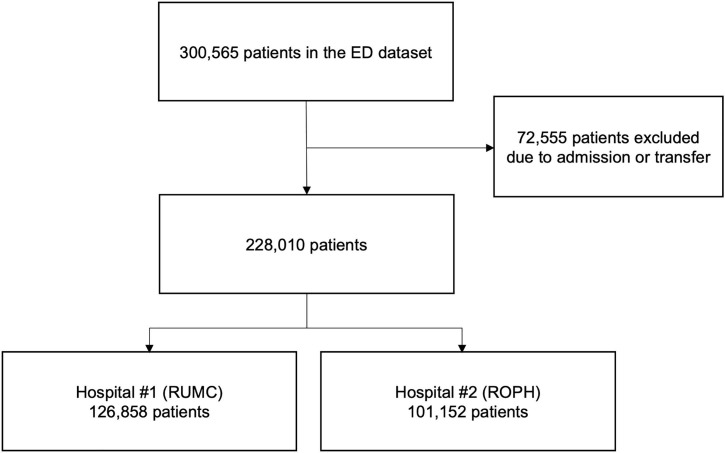
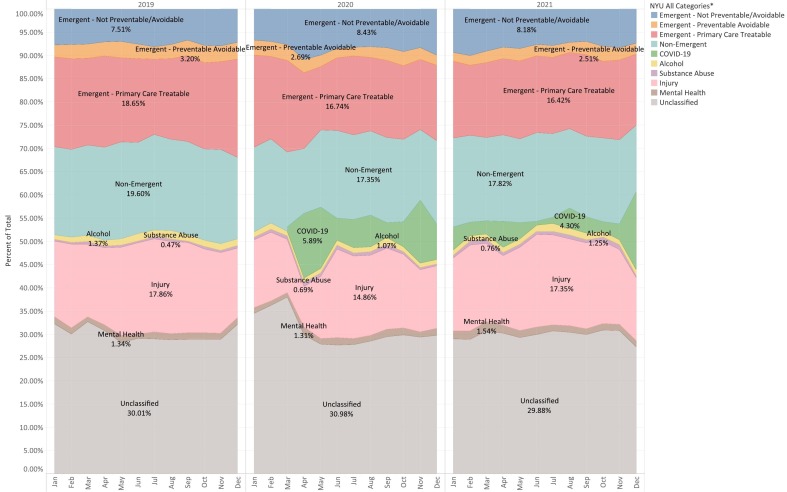
Over the three-year study period, 228,010 outpatient ED discharges were identified (RUMC = 126,858; ROPH = 101,152; Fig. 2). Of these, it was possible to classify 158,972 (70%) using the modified NYU-EDA criteria. Table 1 provides the distribution of ED visits by year for 2019, 2020, and 2021 for each category of ED visit. The monthly changes in each ED visit category from 2019 to 2021 are displayed in Fig. 3 and Supplemental Fig. 1, Supplemental Fig. 2.
Fig. 2.
Flow Diagram.
Table 1.
Descriptive and bivariate analysis for discharged ED visit categories from 2019 to 2021.
| Urgency of ED Visit Categories | Pre and During COVID- 19 Time Frame |
Chi-square test | |||
|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | ||
| HOSPITAL #1 (RUMC) | |||||
| Emergent - Not Preventable/Avoidable | 4003 (8.62%)⁎ | 4095 (9.79%)⁎ | 3771 (9.78%)⁎ | 11,869 (9.36%) | χ2 = 3789.605 df = 18 p < 0.001 |
| Emergent - Preventable Avoidable | 1335 (2.87%)⁎ | 993 (2.37%) | 884 (2.29%)⁎ | 3212 (2.53%) | |
| Emergent - Primary Care Treatable | 8350 (17.97%)⁎ | 6567 (15.7%)⁎ | 5837 (15.14%)⁎ | 20,754 (16.36%) | |
| Non-Emergent | 9030 (19.43%)⁎ | 7051 (16.86%)⁎ | 7012 (18.18%) | 23,093 (18.2%) | |
| Injury | 7811 (16.81%)⁎ | 5651 (13.51%)⁎ | 6108 (15.84%) | 19,570 (15.43%) | |
| Alcohol | 636 (1.37%) | 402 (0.96%)⁎ | 545 (1.41%)⁎ | 1583 (1.25%) | |
| Mental Health | 734 (1.58%) | 600 (1.43%) | 680 (1.76%)⁎ | 2014 (1.59%) | |
| Substance Abuse | 210 (0.45%)⁎ | 265 (0.63%) | 275 (0.71%)⁎ | 750 (0.59%) | |
| COVID-19 | 0 (0%)⁎ | 3134 (7.49%)⁎ | 1808 (4.69%)⁎ | 4942 (3.9%) | |
| Unclassified | 14,355 (30.89%) | 13,075 (31.26%) | 11,641 (30.19%) | 39,071 (30.8%) | |
| Total | 46,464 (100%) | 41,833 (100%) | 38,561 (100%) | 126,858 (100%) | |
| HOSPITAL #2 (ROPH) | |||||
| Emergent - Not Preventable/Avoidable | 2055 (6%)⁎ | 2104 (6.64%) | 2264 (6.42%) | 6423 (6.35%) | χ2 = 1604.257 df = 18 p < 0.001 |
| Emergent - Preventable Avoidable | 1246 (3.64%)⁎ | 984 (3.11%) | 969 (2.75%)⁎ | 3199 (3.16%) | |
| Emergent - Primary Care Treatable | 6702 (19.58%)⁎ | 5736 (18.11%) | 6278 (17.81%)⁎ | 18,716 (18.5%) | |
| Non-Emergent | 6787 (19.83%)⁎ | 5701 (18%) | 6143 (17.43%)⁎ | 18,631 (18.42%) | |
| Injury | 6598 (19.28%)⁎ | 5270 (16.64%)⁎ | 6694 (18.99%)⁎ | 18,562 (18.35%) | |
| Alcohol | 467 (1.36%) | 383 (1.21%) | 379 (1.08%) | 1229 (1.22%) | |
| Mental Health | 351 (1.03%) | 364 (1.15%) | 453 (1.29%) | 1168 (1.15%) | |
| Substance Abuse | 166 (0.48%)⁎ | 242 (0.76%) | 288 (0.82%)⁎ | 696 (0.69%) | |
| COVID-19 | 0 (0%)⁎ | 1198 (3.78%)⁎ | 1363 (3.87%)⁎ | 2561 (2.53%) | |
| Unclassified | 9857 (28.8%)⁎ | 9698 (30.61%)⁎ | 10,412 (29.54%) | 29,967 (29.63%) | |
| Total | 34,229 (100%) | 31,680 (100%) | 35,243 (100%) | 101,152 (100%) | |
| COMBINED HOSPITALS #1 and #2 | |||||
| Emergent - Not Preventable/Avoidable | 6058 (7.51%)⁎ | 6199 (8.43%)⁎ | 6035 (8.18%) | 18,292 (8.02%) | χ2 = 5115.204 df = 18 p < 0.001 |
| Emergent - Preventable Avoidable | 2581 (3.2%)⁎ | 1977 (2.69%) | 1853 (2.51%)⁎ | 6411 (2.81%) | |
| Emergent - Primary Care Treatable | 15,052 (18.65%)⁎ | 12,303 (16.74%)⁎ | 12,115 (16.42%)⁎ | 39,470 (17.31%) | |
| Non-Emergent | 15,817 (19.6%)⁎ | 12,752 (17.35%)⁎ | 13,155 (17.82%)⁎ | 41,724 (18.3%) | |
| Injury | 14,409 (17.86%)⁎ | 10,921 (14.86%)⁎ | 12,802 (17.35%)⁎ | 38,132 (16.72%) | |
| Alcohol | 1103 (1.37%)⁎ | 785 (1.07%)⁎ | 924 (1.25%) | 2812 (1.23%) | |
| Mental Health | 1085 (1.34%) | 964 (1.31%) | 1133 (1.54%)⁎ | 3182 (1.4%) | |
| Substance Abuse | 376 (0.47%)⁎ | 507 (0.69%) | 563 (0.76%)⁎ | 1446 (0.63%) | |
| COVID-19 | 0 (0%)⁎ | 4332 (5.89%)⁎ | 3171 (4.3%)⁎ | 7503 (3.29%) | |
| Unclassified | 24,212 (30.01%) | 22,773 (30.98%)⁎ | 22,053 (29.88%) | 69,038 (30.28%) | |
| Total | 80,693 (100%) | 73,513 (100%) | 73,804 (100%) | 228,010 (100%) | |
RUMC, Rush University Medical Center; ROPH, Rush Oak Park Hospital.
, represents significant p values for post-hoc analysis between observed and expected values using Fisher's Exact test with Bonferroni correction.
Fig. 3.
Monthly distribution of ED visit categories from 2019 to 2021 across both hospitals.
As shown in Table 1, the “Non-Emergent” ED visits category decreased from 15,817 (19.6% of ED visits) to 12,752 (17.4%) between 2019 and 2020 and remained at a lower level in 2021 (13,155 [17.8%]). Similarly, the “Emergent – Primary Care Treatable” ED visit category also decreased from 15,052 (18.7%) to 12,303 (16.7%) between 2019 and 2020 and remained at a lower level in 2021 (12,115 [16.4%]). The “Emergent – Not Preventable/Avoidable” ED visit category slightly increased between 2019 (6058 [7.5%]) and 2020 (6199 [8.4%]) and the proportion remained elevated in 2021 (6035 [8.2%]). The “Injury” ED visit category remained similar for 2019 (14,409 [17.9%]) and 2021 (12,802 [17.4%]) but dropped in 2020 (10,921 [14.9%]). The “Mental Health” and “Substance Abuse” ED visit categories either remained the same or increased during the COVID-19 period as compared to 2019. The “Unclassified” categories remained similar prior to and during the COVID-19 time frame.
For RUMC, the “Non-Emergent” ED visit category dropped during 2020 (7051 [16.9%]) as compared to 2019 (9030 [19.4%]) but started to return to pre-pandemic levels during 2021 (7012 [18.2%]). In addition, for RUMC, the percentage in the “Emergent – Not Preventable/Avoidable” ED visit category increased in 2020 (4095 [9.8%]) and 2021(3771 [9.8%]) as compared to 2019 (4003 [8.6%]). For ROPH, the proportion of “Substance Abuse” and “Mental Health” ED visit categories increased during the COVID-19 pandemic as compared to the pre-pandemic time frame. There was a significant association identified between the time period (pre-COVID-19 versus during COVID-19) and the ED visit category for the combined hospitals (p < 0.001), RUMC (p < 0.001), and ROPH (p < 0.001). This finding remained significant in the sensitivity analysis removing the COVID-19 category. Based on Fisher's exact test with Bonferroni-correction, “Non-Emergent”, “Emergent – Primary Care Treatable”, and “COVID -19” ED visits were significantly different than expected ED visits for all COVID-19 time frames for the combined hospitals (Table 1). Similarly, “Emergent - Not Preventable/Avoidable”, “Emergent – Primary Care Treatable”, and “COVID -19” ED visits were significantly different than expected ED visits for all COVID-19 time frame for RUMC while for ROPH “Injury”, and “COVID-19” ED visits were significantly different than expected ED visits for all COVID-19 time frames.
Compared with 2019, the daily ED census for the combined hospitals significantly dropped during COVID-19 by 20.2 and 18.9 ED visits in 2020 and 2021, respectively (p < 0.001; Table 2 ). There was a statistically significant decline in all categories from 2019 to 2020 except for “Substance Abuse” (statistically significant increase) and “Emergent – Not Preventable/Avoidable” (no difference). Similarly, all categories had a statistically significant decline from 2019 to 2021, except for “Substance Abuse” (statistically significant increase), “Mental Health” (no difference), and “Emergent – Not Preventable/Avoidable” (no difference). In contrast, only a few differences were statistically significant from 2020 to 2021, which included increases in “Injuries”, “Alcohol”, and “Mental Health” and a decrease in “COVID-19” related visits. There were no significant differences in ED avoidable visits between 2020 and 2021.
Table 2.
Descriptive and bivariate analysis for daily census of ED visit categories from 2019 to 2021.
| Urgency of ED Visit Categories | Pre and During COVID- 19 Time Frame |
ANOVA Test | Comparison |
|||||
|---|---|---|---|---|---|---|---|---|
| 2019 (mean ± SD) |
2020 (mean ± SD) |
2021 (mean ± SD) |
Total (mean ± SD) |
2019 vs 2020 | 2019 vs 2021 | 2020 vs 2021 | ||
| HOSPITAL# 1 (RUMC) | ||||||||
| Emergent - Not Preventable/Avoidable | 10.97 ± 3.43 | 11.19 ± 3.48 | 10.33 ± 3.22 | 10.83 ± 3.39 | f = 6.34 df = 2 p = 0.0018 | p = 1 | p=0.0335* | p=0.0019* |
| Emergent - Preventable Avoidable | 3.66 ± 1.93 | 2.71 ± 1.81 | 2.42 ± 1.59 | 2.93 ± 1.86 | f = 47.98 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.0821 |
| Emergent - Primary Care Treatable | 22.88 ± 5.49 | 17.94 ± 6.09 | 15.99 ± 4.54 | 18.94 ± 6.14 | f = 156.87 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| Non-Emergent | 24.74 ± 5.39 | 19.27 ± 5.54 | 19.21 ± 5.29 | 21.07 ± 5.99 | f = 126.03 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 1 |
| Injury | 21.4 ± 5.05 | 15.44 ± 6.1 | 16.73 ± 5.14 | 17.86 ± 6.02 | f = 120.86 df = 2 p < 0.001 | p<0.001* | p<0.001* | p=0.0041* |
| Alcohol | 1.74 ± 1.63 | 1.1 ± 1.13 | 1.49 ± 1.36 | 1.44 ± 1.41 | f = 20.06 df = 2 p < 0.001 | p<0.001* | p=0.0459* | p<0.001* |
| Mental Health | 2.01 ± 1.46 | 1.64 ± 1.23 | 1.86 ± 1.4 | 1.84 ± 1.37 | f = 6.87 df = 2 p = 0.0011 | p<0.001* | p = 0.43 | p = 0.0808 |
| Substance Abuse | 0.58 ± 0.77 | 0.72 ± 0.85 | 0.75 ± 0.9 | 0.68 ± 0.84 | f = 4.74 df = 2 p = 0.009 | p=0.05* | p=0.0126* | p = 1 |
| COVID-19 | 0 ± 0 | 8.56 ± 7.93 | 4.95 ± 6.25 | 4.51 ± 6.8 | f = 198.57 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| Unclassified | 39.33 ± 7.35 | 35.72 ± 9.87 | 31.9 ± 7.2 | 35.65 ± 8.77 | f = 74.4 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| Total | 127.3 ± 13.67 | 114.3 ± 18.31 | 105.65 ± 14.95 | 115.75 ± 18.09 | f = 174.38 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| HOSPITAL# 2 (ROPH) | ||||||||
| Emergent - Not Preventable/Avoidable | 5.63 ± 2.5 | 5.75 ± 2.66 | 6.2 ± 2.41 | 5.86 ± 2.54 | f = 5.22 df = 2 p = 0.0055 | p = 1 | p=0.0068* | p=0.0459* |
| Emergent - Preventable Avoidable | 3.41 ± 1.96 | 2.69 ± 1.78 | 2.65 ± 1.66 | 2.92 ± 1.84 | f = 20.52 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 1 |
| Emergent - Primary Care Treatable | 18.36 ± 5.43 | 15.67 ± 6.24 | 17.2 ± 5.27 | 17.08 ± 5.76 | f = 20.74 df = 2 p < 0.001 | p<0.001* | p=0.0171* | p<0.001* |
| Non-Emergent | 18.59 ± 4.75 | 15.58 ± 5.82 | 16.83 ± 4.72 | 17 ± 5.26 | f = 32.03 df = 2 p < 0.001 | p<0.001* | p<0.001* | p=0.0029* |
| Injury | 18.08 ± 5.2 | 14.4 ± 5.81 | 18.34 ± 5.85 | 16.94 ± 5.9 | f = 56.04 df = 2 p < 0.001 | p<0.001* | p = 1 | p<0.001* |
| Alcohol | 1.28 ± 1.19 | 1.05 ± 1.11 | 1.04 ± 1.11 | 1.12 ± 1.14 | f = 5.32 df = 2 p = 0.005 | p=0.0168* | p=0.0125* | p = 1 |
| Mental Health | 0.96 ± 1.04 | 0.99 ± 1.12 | 1.24 ± 1.19 | 1.07 ± 1.12 | f = 6.83 df = 2 p = 0.0011 | p = 1 | p=0.0022* | p=0.0087* |
| Substance Abuse | 0.45 ± 0.66 | 0.66 ± 0.84 | 0.79 ± 0.96 | 0.64 ± 0.84 | f = 14.99 df = 2 p < 0.001 | p=0.0025* | p<0.001* | p = 0.1143 |
| COVID-19 | 0 ± 0 | 3.27 ± 3.71 | 3.73 ± 4.54 | 2.34 ± 3.77 | f = 132.27 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.197 |
| Unclassified | 27.01 ± 6.51 | 26.5 ± 10.19 | 28.53 ± 6.68 | 27.34 ± 8.01 | f = 6.4 df = 2 p = 0.0017 | p = 1 | p=0.0304* | p=0.0018* |
| Total | 93.78 ± 14.43 | 86.56 ± 21.98 | 96.56 ± 15.47 | 92.29 ± 18.1 | f = 31.37 df = 2 p < 0.001 | p<0.001* | p = 0.1002 | p<0.001* |
| COMBINED HOSPITALS #1 & #2 | ||||||||
| Emergent - Not Preventable/Avoidable | 16.6 ± 4.25 | 16.94 ± 4.52 | 16.53 ± 4.11 | 16.69 ± 4.29 | f = 0.93 df = 2 p = 0.3944 | p = 0.8546 | p = 1 | p = 0.6149 |
| Emergent - Preventable Avoidable | 7.07 ± 2.92 | 5.4 ± 2.85 | 5.08 ± 2.42 | 5.85 ± 2.87 | f = 55.72 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.3273 |
| Emergent - Primary Care Treatable | 41.24 ± 8.19 | 33.61 ± 10.15 | 33.19 ± 7.58 | 36.01 ± 9.45 | f = 98.74 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 1 |
| Non-Emergent | 43.33 ± 7.7 | 34.84 ± 9.31 | 36.04 ± 7.87 | 38.07 ± 9.13 | f = 111.28 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.1552 |
| Injury | 39.48 ± 7.96 | 29.84 ± 10.13 | 35.07 ± 8.8 | 34.79 ± 9.83 | f = 104.83 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| Alcohol | 3.02 ± 2.11 | 2.14 ± 1.7 | 2.53 ± 1.84 | 2.57 ± 1.92 | f = 19.82 df = 2 p < 0.001 | p<0.001* | p=0.0014* | p=0.0171* |
| Mental Health | 2.97 ± 1.84 | 2.63 ± 1.59 | 3.1 ± 1.88 | 2.9 ± 1.78 | f = 6.85 df = 2 p = 0.0011 | p = 0.0297 | p = 0.949 | p=0.001* |
| Substance Abuse | 1.03 ± 1.01 | 1.39 ± 1.19 | 1.54 ± 1.34 | 1.32 ± 1.21 | f = 17.78 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.2226 |
| COVID-19 | 0 ± 0 | 11.84 ± 10.47 | 8.69 ± 10.03 | 6.85 ± 9.75 | f = 195.74 df = 2 p < 0.001 | p<0.001* | p<0.001* | p<0.001* |
| Unclassified | 66.33 ± 10.75 | 62.22 ± 17.28 | 60.42 ± 10.99 | 62.99 ± 13.57 | f = 18.79 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 0.2054 |
| Total | 221.08 ± 22.63 | 200.86 ± 35.19 | 202.21 ± 25.37 | 208.04 ± 29.69 | f = 58.49 df = 2 p < 0.001 | p<0.001* | p<0.001* | p = 1 |
SD, standard deviation.
4. Discussion
This was a novel study analyzing the impact of COVID-19 on avoidable ED discharged visits over a three-year time period. While prior research has focused on the acute time period immediately after COVID-19 first occurred [13,14], we were able to build on this by evaluating the longer-term trends (nearly two years after the pandemic started). We were also able to expand on the limited literature by adding data from a large healthcare system across two hospitals, as well as the direct impact of COVID-19 diagnoses.
Similar to previous research [13,14], we found an overall decrease in both total ED visits and avoidable ED visits in the immediate post-pandemic period which was both clinically and statistically significant. This decrease began in February and March 2020, three months after the first case of COVID-19 and coinciding with when the World Health Organization officially declared COVID-19 a pandemic on March 11, 2020 [20]. These trends continued into the post-pandemic period through 2021. While both total ED visits and avoidable ED visits increased slightly in comparison to their trough levels, they ultimately settled at volumes significantly lower than their pre-pandemic counterparts.
The initial decline may be attributed to multiple factors including city-wide legislative efforts and community outreach. The city of Chicago enacted its first, city-wide guidance in an attempt to minimize the spread of COVID-19 on March 12, 2020 [21]. In addition to encouraging patrons to stay at home, this guidance resulted in the cancellation of many large-scale events and public gatherings. In addition, the mayor enacted an executive order on March 19, 2020 for those with COVID-19 or similar symptoms to stay at home [21]. In the month of March alone, there were 20 televised press conferences covering the risk of COVID-19 and its continued spread, as well as reiterating and expanding on Rush's efforts to limit the spread of the virus [22]. In addition to preventing public gatherings that may have resulted in future ED visits, these efforts may have persuaded patients to delay ED evaluation for what they considered to be less significant medical conditions.
Regarding the continued, longer-term decreased volumes in both total ED visits and avoidable ED visits, several potential explanations exist. In the time since the COVID-19 pandemic began, boarding and ED wait times have continued to increase [23]. This may have resulted in patients leaving without being seen by a clinician (particularly in light of potential concern for exposure to COVID-19 in crowded waiting rooms), or alternatively seeking evaluation at urgent care or outpatient appointments. In addition, telehealth services were continuously being deployed and expanded during the post-pandemic period which may have contributed to both a decline in total ED visits as well as helping identify patients that did not immediately require ED evaluation [24]. Moreover, the continued presence of COVID-19 along with new variants may also explain the lack of a rebound in total ED visits and it is possible that this may change as the impact of COVID-19 declines over time. While the present study does not allow us to identify the exact reasons for the findings, this suggests a potential role for healthcare policymakers to continue interventions (e.g., telemedicine, urgent care centers) that had been launched during COVID-19, as well as to expand primary care access in order to further reduce avoidable ED visits – particularly during times of staffing shortages and increased ED boarding.
COVID-19 related ED visits became trackable starting in March 2020 after COVID-19 specific ICD-10 codes were created. The initial surge in COVID-19 related ED visits from March through May 2020 correlates closely with the decrease in avoidable ED visits over this period. The initial COVID-19 surge was the first time the majority of the public had faced a pandemic. It follows that the public was understandably cautious when dealing with possible COVID-19 exposures and/or symptoms as epidemiologic data were limited. During this initial phase of relative uncertainty, it is possible that many patients defaulted to ED evaluation for any potential COVID-19 related ailment, regardless of severity. Subsequent surges of COVID-19 related ED visits in December 2020 and December 2021 were also associated with decreases in avoidable ED visits, albeit to a lesser magnitude. The surge in COVID-19 related visits in December 2020 aligns with national data on COVID-19 severity, as the highest number of COVID-19 related deaths were reported over the three-month period spanning from November 2020 through January 2021 [25]. It is possible that patient caution and reluctance to come to the ED for non-critical conditions may have reached an apex during this period, potentially explaining the reduction in avoidable ED visits.
We also compared findings between two different hospitals in the same healthcare system. RUMC is a large, tertiary care academic medical center located in Chicago, IL, while ROPH is a smaller, community hospital located in Oak Park, IL. Both hospitals experienced a decrease in avoidable ED visits from 2019 to 2021. As a percentage of total ED visits in 2020, RUMC realized a more significant drop in avoidable ED visits in addition to a significantly greater amount of COVID-19 related visits. This may be attributable to RUMC being designated as the primary COVID-19 response facility in Chicago [26]. With this designation came many televised ads, articles, and increased public awareness of RUMC's role in Chicago's COVID-19 response. As many COVID-19 patients were transferred and routed to RUMC, this may have resulted in patients without COVID-19 related concerns avoiding the facility altogether. As a result, many patients may have sought care at other locations, including smaller, affiliated community hospitals such as ROPH.
Interestingly, the reduction in avoidable ED visits was partially offset by the increase in COVID-19 related visits. While there does not currently exist a stratification of avoidable versus unavoidable visits for COVID-19 visits, increased access to home testing and outpatient oral medications may reduce the need for ED-based care of milder COVID-19 cases. Future research is needed to better understand which COVID-19 presentations are potentially avoidable and to develop decision tools for guiding the need for ED-based care.
5. Limitations
There are several important limitations to consider in this study. First, this was a retrospective study of a single healthcare system within one region. While we had a large number of patients and intentionally included different hospital types (i.e., a large tertiary care and smaller community hospital) in this study, it remains possible this may not reflect the experience of other healthcare systems or other regions. Additionally, the data do not allow us to determine whether patients visited other healthcare systems within the region or if patients went untreated. Similar to prior work [14], we utilized data among discharged patients, which may not reflect all patients presenting to the ED. Moreover, the NYU-EDA algorithm uses dichotomous indicators and may not fully reflect all visits. While we were able to successfully classify 70% of all visits based on our data, some important information about patterns of ED utilization may have been obscured in unclassified diagnoses. Further, the addition of COVID-19 codes was not present in the original NYU-EDA algorithm. While we attempted to account for this by adding it as a new category, further research is needed to determine the role of COVID-19 codes in avoidable ED visits. The NYU-EDA algorithm, while one of the most commonly utilized tools for assessing avoidable visits, does have some inherent limitations and, consequently, may not fully reflect avoidable visits. Among these are limited external validity data and the possibility that the criteria are less representative of current clinical patterns (e.g., aging populations with more severe illnesses) based on the algorithm being developed 20 years prior [27]. Finally, this study was limited to the first two years after COVID-19 began and longer-term studies will still be needed to assess the implications on avoidable ED visits further downstream.
6. Conclusion
Our study found a sustained decline in avoidable ED discharged visits during the two years following the beginning of the COVID-19 pandemic. These data provide a nuanced understanding of ED utilization during the COVID-19 pandemic. Moving forward, these analyses can provide a foundation as we continue to evaluate the longer-term impact of COVID-19 on ED utilization. In addition, these findings may serve as a framework for comparisons across larger regions and/or multiple healthcare systems. Furthermore, this research may help prepare EDs and healthcare systems in resource allocation, hospital staffing, and financial planning during future COVID-19 resurgences and pandemics.
The following are the supplementary data related to this article.
Monthly distribution of ED visit categories from 2019 to 2021 for Hospital #1 only.
Monthly distribution of ED visit categories from 2019 to 2021 for Hospital #2 only.
Disclosures/funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We have no disclosures to declare.
Meetings
None.
IRB
Approved.
CRediT authorship contribution statement
Michael Gottlieb: Writing – review & editing, Writing – original draft, Supervision, Project administration, Methodology, Investigation, Conceptualization. Ryan Schipfer: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Shital Shah: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Dennis McKinney: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Conceptualization. Paul Casey: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Conceptualization. Brian Stein: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Data curation, Conceptualization. Brian Stein: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Data curation, Conceptualization. Doug Thompson: Writing – review & editing, Writing – original draft, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization.
Declaration of Competing Interest
None.
Acknowledgements
None.
References
- 1.Fuchs V.R. Health care policy after the COVID-19 pandemic. JAMA. 2020;324(3):233–234. doi: 10.1001/jama.2020.10777. [DOI] [PubMed] [Google Scholar]
- 2.Johns Hopkins University and Medicine Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html Available at. Last accessed: December 22, 2022.
- 3.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 4.Wong L.E., Hawkins J.E., Langness S., et al. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catalyst. 2020 May 14 doi: 10.1056/CAT.20.0193. [DOI] [Google Scholar]
- 5.American College of Emergency Physicians Emergency Medicine Practice Committee Emergency department crowding: high impact solutions. https://www.acep.org/globalassets/sites/acep/media/crowding/empc_crowding-ip_092016.pdf Available at. Last accessed: December 22, 2022.
- 6.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 7.Weinick R.M., Burns R.M., Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood) 2010;29(9):1630–1636. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baum A., Schwartz M.D. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeffery M.M., D’Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kruizinga M.D., Peeters D., van Veen M., et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021;180(7):2271–2279. doi: 10.1007/s00431-021-04015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rennert-May E., Leal J., Thanh N.X., et al. The impact of COVID-19 on hospital admissions and emergency department visits: a population-based study. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252441. Published 2021 Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tuominen J., Hällberg V., Oksala N., Palomäki A., Lukkarinen T., Roine A. NYU-EDA in modelling the effect of COVID-19 on patient volumes in a Finnish emergency department. BMC Emerg Med. 2020;20(1):97. doi: 10.1186/s12873-020-00392-1. Published 2020 Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giannouchos T.V., Biskupiak J., Moss M.J., Brixner D., Andreyeva E., Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. 2021;40:20–26. doi: 10.1016/j.ajem.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Elm E., Altman D.G., Egger M., et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 16.New York University NYU-EDA background. https://wagner.nyu.edu/faculty/billings/nyued-background Available at:
- 17.Gandhi S.O., Sabik L. Emergency department visit classification using the NYU algorithm. Am J Manag Care. 2014;20(4):315–320. [PubMed] [Google Scholar]
- 18.Ballard D.W., Price M., Fung V., et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48(1):58–63. doi: 10.1097/MLR.0b013e3181bd49ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shan G., Gerstenberger S. Fisher’s exact approach for post hoc analysis of a chi-squared test. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0188709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. March 11, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Last accessed: December 22, 2022.
- 21.Buchanan A. State of Illinois and City of Chicago issue New Guidance to Minimize COVID-19 Spread. March 12, 2020. https://www.chicago.gov/city/en/depts/cdph/provdrs/health_protection_and_response/news/2020/march/state-of-illinois-and-city-of-chicago-issue-new-guidance-to-mini.html
- 22.City of Chicago Press Room. 2022. https://www.chicago.gov/city/en/sites/covid-19/home/press-releases.html Last accessed: December 22, 2022.
- 23.Lucero A., Sokol K., Hyun J., et al. Worsening of emergency department length of stay during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021;2(3) doi: 10.1002/emp2.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah M., Patel K., Popa D., et al. Use of telemedicine to expedite and expand care during COVID-19. West J Emerg Med. 2021;22(5):1028–1031. doi: 10.5811/westjem.2021.4.51317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention Provisional Death Counts for Coronavirus Disease 2019 (COVID-19) https://www.cdc.gov/nchs/nvss/vsrr/COVID19/index.htm Available at. Last accessed: December 22, 2022.
- 26.St. Clair S. Rush University Medical Center was built for a moment like this. Take a look inside the calm at the center of Chicago's coronavirus storm. Chicago Tribune. April 9 2020. https://www.chicagotribune.com/coronavirus/ct-coronavirus-rush-university-medical-center-chicago-20200409-4odjgtv6h5eohjcnaqhsi3if2e-story.html Available at.
- 27.Lowe R.A. Updating the emergency department algorithm: one patch is not enough. Health Serv Res. 2017;52(4):1257–1263. doi: 10.1111/1475-6773.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Monthly distribution of ED visit categories from 2019 to 2021 for Hospital #1 only.
Monthly distribution of ED visit categories from 2019 to 2021 for Hospital #2 only.