Abstract
We determined cellular and humoral immune responses to Borrelia burgdorferi lysate and to recombinant flagellin (FlaB), OspC, and OspA in acute- and convalescent-phase samples from 39 culture-positive patients with erythema migrans and in 20 healthy control subjects. During the acute illness, a median of 4 days after the onset of erythema migrans, 51% of the patients had proliferative cellular responses and 72% had antibody responses to at least one of the borrelial antigens tested. During convalescence, at the conclusion of antibiotic therapy, 64% of the patients had proliferative cellular reactivity and 95% had antibody reactivity with at least one of the spirochetal antigens tested. In both acute- and convalescent-phase samples, cellular immune responses were found as frequently to OspA as to OspC and FlaB. Although antibody responses were also frequently seen to OspC and FlaB, only a few patients had marginal antibody reactivity with OspA. The percentage of patients with proliferative responses was similar in those with clinical evidence of localized or disseminated infection, whereas humoral reactivity was found more often in those with disseminated disease. We conclude that cellular and humoral responses to B. burgdorferi antigens are often found among patients with early Lyme disease. In contrast with the other antigens tested, cellular but not humoral reactivity was often found with OspA.
Lyme disease in the United States is caused by the tick-transmitted spirochete Borrelia burgdorferi sensu stricto (27). The illness usually begins with a characteristic, expanding skin lesion, erythema migrans (EM), which is sometimes accompanied by flu-like symptoms (24, 28). Within days to weeks, spirochetes may disseminate to other sites, particularly to the nervous system, heart, or joints. Weeks to months later, manifestations of disseminated infection may develop, such as lymphocytic meningitis, atrioventricular nodal block, or oligoarticular arthritis (27). The wide range in outcomes in untreated patients probably reflects interplay between spirochetal virulence and differences in host immune responses.
B. burgdorferi induces complex cellular and humoral immune responses to a number of spirochetal proteins in patients with Lyme disease (1, 5, 10, 12, 21, 33). During tick feeding, the spirochete up-regulates or down-regulates certain outer-surface proteins (Osp), which apparently allow the organism to adapt to and survive in markedly different arthropod and mammalian environments (9). For example, OspA, a 31-kDa lipoprotein, is prominently expressed on the spirochete's outer membrane in the mid-gut of the tick, and it is down-regulated during tick feeding and transmission to the mammalian host (22). Conversely, OspC, a 23-kDa lipoprotein, is up-regulated during tick feeding as the spirochete traverses to the tick salivary gland and to the mammalian host (26). Prominent early immune responses in Lyme disease include reactivity with OspC and the 41-kDa flagellar antigen (FlaB) of the spirochete (1, 10, 12).
In Europe, where Lyme borreliosis is caused primarily by infection with B. garinii and B. afzelii, Krause et al. determined cellular and humoral responses to whole B. burgdorferi and to recombinant OspA and FlaB in 35 patients with early- or late-stage Lyme borreliosis (19). Most patients had marked cellular immune responses to whole B. burgdorferi. In addition, the 11 patients with early Lyme disease often had T-cell responses to OspA and FlaB, but these patients lacked antibody reactivity with OspA. Such responses were detected only in a few late-stage Lyme borreliosis patients.
Cellular immune responses to live B. burgdorferi were reported previously in three of six American patients tested with early Lyme disease (7). However, the interaction of cellular and humoral immune responses has not been assessed previously in American patients with early infection. In the present study, we determined T- and B-cell responses to B. burgdorferi lysate and to recombinant B. burgdorferi antigens, FlaB, OspC, and OspA, in acute- and convalescent-phase samples from culture-positive patients with EM and in healthy control subjects.
MATERIALS AND METHODS
Patients.
During the summers of 1998 and 1999, 52 patients with EM were recruited for the study at two field sites, one in East Lyme, Conn. (V.K.S.), and the other in Wakefield, R.I. (N.D.). The study was approved by the Human Investigations Committee at New England Medical Center. The patients met the criteria of the Centers for Disease Control and Prevention that are used for the surveillance of Lyme disease (3). They had EM, which was defined as an expanding annular lesion, at least 5 cm in diameter, often with partial central clearing.
At the initial visit, the physicians at the two field sites did a clinical assessment of signs and symptoms, using a standardized questionnaire, and based on this information, they made a clinical judgement regarding whether the patient had localized or disseminated infection. Localized infection was defined as localized EM accompanied by no more than regional lymphadenopathy, fatigue, mild headache, or myalgias. Disseminated infection was defined as EM accompanied by secondary annular skin lesions, arthritis and/or arthralgia in one or a few joints, or the combination of headache and neck stiffness or facial palsy.
Collection of samples.
A 1.5-mm punch biopsy was done for culture at the leading edge of EM lesions. Each skin biopsy specimen was placed immediately in a 15-ml sterile tube containing 13 ml of modified Barbour-Stoenner-Kelly medium (BSK-H; Sigma, St. Louis, Mo.) plus ciprofloxacin (0.4 μg/ml) and rifampin (40 μg/ml). Samples were sent overnight to New England Medical Center, where the tubes were immediately incubated at 33°C. After several days of incubation, half the culture medium was replaced with fresh medium without antibiotics. The tubes were examined weekly by dark-field microscopy for motile spirochetes for 1 month. Of the 52 patients, 39 (75%) had positive cultures for B. burgdorferi from the skin biopsy samples.
At the initial visit, an acute-phase blood sample, collected in heparinized tubes, and a serum sample, collected in nonheparinized tubes, were also obtained for cellular and humoral immune studies, and the same types of specimens were collected during convalescence at the conclusion of antibiotic treatment. After overnight shipping, peripheral blood lymphocytes (PBL) were separated by the Ficoll-Hypaque method (lymphocyte separation medium; Organon Teknika, Durham N.C.). PBL were frozen in liquid nitrogen and serum samples were frozen at −70°C for subsequent determinations. In order to be certain of the diagnosis, cellular and humoral immune responses in this study were determined only in samples from the 39 culture-positive patients. For comparison, blood samples were obtained from 20 healthy control subjects in the laboratory.
B. burgdorferi antigens.
Sonicated lysates of B. burgdorferi sensu stricto proteins were made from strain G 39/40. The spirochetes were grown in BSK-H medium, harvested by centrifugation, washed with phosphate-buffered saline, sonicated and filtered, as previously described (6). Full-length, non-lipidated OspA and OspC, minus the signal peptide, were generated as recombinant fusion proteins with Escherichia coli maltose binding protein, as previously described (14, 17). Recombinant OspA was derived from B. burgdorferi strain B31, and OspC was derived from strain 297, a virulent strain isolated from a patient with Lyme meningitis. Recombinant FlaB fused with CMP-2-keto-3-deoxyoctulosonic acid synthetase (CKS) was a kind gift from John Robinson at Abbott Laboratories (Abbott Park, Ill.) (25). We have previously shown that patients rarely have cellular or humoral responses to the fusion partner maltose binding protein or CKS alone (14, 25), and therefore, these control proteins were not included in the current study.
T-cell proliferation assay.
PBL were tested for reactivity with B. burgdorferi lysate and recombinant B. burgdorferi antigens in standard proliferation assays. Briefly, 5 × 105 mononuclear cells were plated in round-bottom, 96-well plates (Costar, Cambridge, Mass.) in 200 μl of complete medium (RPMI 1640 with 10% human AB serum [Sigma], 2 mM glutamine, penicillin [100 U/ml], streptomycin [100 μg/ml], and 9.5 mM HEPES buffer [all reagents from Gibco BRL, unless noted]). In preliminary studies, optimal antigen concentrations were shown to be 25 μg/ml for B. burgdorferi lysate and 10 μg/ml for P41, OspC, and OspA antigens. After 5 days in culture with 5% CO2 at 37°C, [3H]thymidine (0.5 μCi/well) in 50 μl of complete medium was then added to each well. The cells were harvested 16 to 18 h later with an automated harvester (Packard Instruments, Meriden, Conn.), and the incorporated thymidine was detected in a liquid scintillation counter (Top Counter; Packard Instruments). In order to minimize day-to-day and patient-to-patient variation in test performance, the results are expressed throughout as a stimulation index, which represents the counts per minute obtained with antigen stimulation divided by the counts per minute in unstimulated control wells. The cutoff for a positive value was defined as 3 standard deviations (SD) above the mean value of the 20 healthy control subjects.
Serologic assays for antibody to B. burgdorferi.
The immunoglobulin M (IgM) and IgG antibody responses to B. burgdorferi lysate and recombinant borrelial antigens were measured using modifications of previously described methods (1, 6, 10). Ninety-six-well Immulon 1 plates (Dynatech Inc., Kensington, Md.) were coated with each of the antigens (1 μg/well) in coating buffer (0.05 M sodium carbonate, pH 9.6). These concentrations were shown to be in antigen excess using checkerboard dilutions of each recombinant antigen and a strongly positive patient serum sample. After incubation overnight at 4°C, the plates were washed with PBS–0.05% Tween 20 and incubated with milk buffer (5% nonfat dried milk in PBS–0.05% Tween 20) for 45 min at 37°C. After washing, 200 μl of each patient's serum sample (1:50 dilution) was plated in duplicate and incubated for 45 min at 37°C. Following another wash, the plates were incubated with alkaline phosphatase-conjugated, goat anti-human IgG (1:750; Biosource, Camarillo, Calif.) or IgM (1:500; Biosource) in milk buffer at 37°C for 45 min. The substrate was freshly prepared p-nitrophenyl phosphate. The plates were read at 405 nm when the highest concentration (1:50 dilution) of the positive control sample, which was included on each plate, reached 1.0. The cutoff for a positive value for the IgG and IgM antibody was defined as 3 SD above the mean absorbance of eight negative control samples included on the same plate. These samples were previously shown to be representative of values obtained from 50 normal control subjects (10).
The two-test approach of enzyme-linked immunosorbent assay (ELISA) and Western blotting was done on samples with a positive response to B. burgdorferi lysate by ELISA. A commercial test system (MarDx, San Diego, Calif.) was used for Western blotting, which was carried out according to the manufacturer's instructions. The results were interpreted according to the Centers for Disease Control/Association of State and Territorial Laboratory Directors' criteria (4).
Statistical analysis.
The findings among patient groups were compared by Fisher's exact test. Values obtained during acute and convalescent phases of the illness were compared by paired t test. All P values are two-tailed.
RESULTS
Clinical characteristics of patients.
The 39 culture-positive patients with EM had a median age of 50 years, and they consisted of nearly equal numbers of men and women (Table 1). About one-quarter of the patients remembered a tick bite at the site where an expanding erythema was noted a median of 9 days later. The study physicians evaluated the patients a median of 4 days (range, 1 to 21 days) after the onset of EM. On examination, the skin lesions were a median of 10 cm in diameter, and 8 patients (21%) had secondary annular skin lesions. Associated symptoms included malaise and fatigue, fever and chills, headache and neck stiffness, and arthralgias. Most of the patients were treated with doxycycline, 100 mg twice a day, but a few patients received amoxicillin, 500 mg three times a day, or cefuroxime axetil, 500 mg twice a day—in each instance for 21 to 30 days. All of the patients had the resolution of EM and associated symptoms within a median duration of 6 days after the start of antibiotic therapy. No patient experienced subsequent manifestations of the illness.
TABLE 1.
Clinical characteristics of 39 patients with EM
| Characteristic | Valuea |
|---|---|
| Median (range) age (yr) | 50 (16–78) |
| Sex | |
| Male | 21 (54) |
| Female | 18 (46) |
| Tick bite history at site of EM | 10 (26) |
| Median (range) duration from tick bite to EM (days) | 9 (1–21) |
| Median (range) size of EM lesion (cm) | 10 (5–21) |
| Secondary annular lesions | 8 (21) |
| Median (range) duration from onset of EM to treatment (days) | 4 (1–21) |
| Associated symptoms | |
| Malaise | 18 (46) |
| Fatigue | 22 (56) |
| Headache | 19 (49) |
| Neck stiffness | 17 (44) |
| Arthralgias | 18 (46) |
| Fever | 16 (41) |
| Chills | 18 (46) |
| Myalgias | 11 (28) |
| Backache | 8 (21) |
| Anorexia | 6 (15) |
| Treatment | |
| Doxycycline | 33 (85) |
| Amoxicillin | 5 (13) |
| Cefuroxine axetil | 1 (2) |
| Median (range) duration from beginning of therapy to resolution of symptoms (days) | 6 (2–21) |
Number (percent) unless otherwise indicated.
Cellular immunity.
During the acute phase of the illness, a median of 4 days after the onset of EM, PBL from 17 of the 39 patients (44%) had proliferative responses to B. burgdorferi lysate, which were at least 3 standard deviations above the mean value of 20 healthy control subjects (Table 2; Fig. 1). In addition, three patients (8%) had responses to the P41 flagellar antigen (FlaB) of the spirochete, and eight (21%) had reactivity with OspC, which are known to be prominent early responses in the infection (1, 8, 9). Moreover, eight patients (21%) had proliferative responses to OspA, a protein that is down-regulated by the spirochete during tick feeding and transmission to the mammalian host (16). Altogether, 51% of the patients had proliferative responses to one or more of these borrelial antigens in acute-phase samples.
TABLE 2.
Cellular immune response to B. burgdorferi antigens among 39 patients with EM
| Antigen | No. (%) of patients positive by proliferation assay during phase
|
P | |
|---|---|---|---|
| Acute | Convalescent | ||
| B. burgdorferi lysate | 17 (44) | 21 (54) | 0.2 |
| FlaB | 3 (8) | 14 (36) | 0.005 |
| OspC | 8 (21) | 14 (36) | 0.2 |
| OspA | 8 (21) | 17 (44) | 0.05 |
| Any of the above | 20 (51) | 25 (64) | 0.4 |
| All of the above | 1 (3) | 10 (26) | 0.003 |
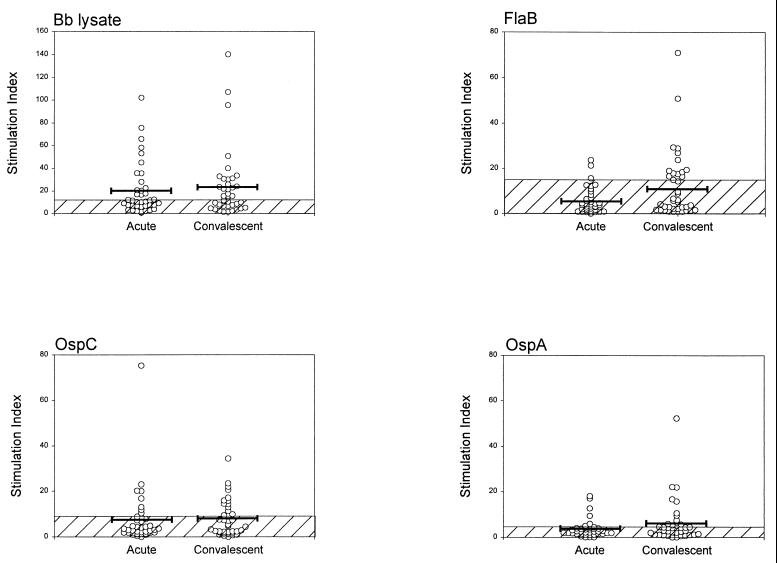
FIG. 1.
Cellular immune responses to B. burgdorferi lysate and recombinant spirochetal proteins are shown, as determined by proliferation assay. Antigen-induced proliferation (counts per minute) was divided by proliferation in the absence of antigen to obtain a stimulation index. The cross-hatched area represents the mean value plus 3 SD for 20 healthy control subjects. The bar indicates the mean value of patients' responses. The values were slightly greater in convalescent-phase samples than in acute-phase samples, but the differences were statistically significant only for FlaB (P = 0.01).
At the conclusion of antibiotic treatment, a median of 22 days after study entry, the number of patients with proliferative responses to B. burgdorferi antigens and the strength of the responses were usually greater than during the acute phase of the illness (Table 2). During convalescence, 64% of the patients had responses to at least one of the borrelial antigens tested; approximately 40% each had reactivity with FlaB, OspC, or OspA, and 26% had reactivity with all of these antigens. During both acute and convalescent phases of the illness, cellular immune responses to OspA were as frequent as those to FlaB and OspC.
Humoral immunity.
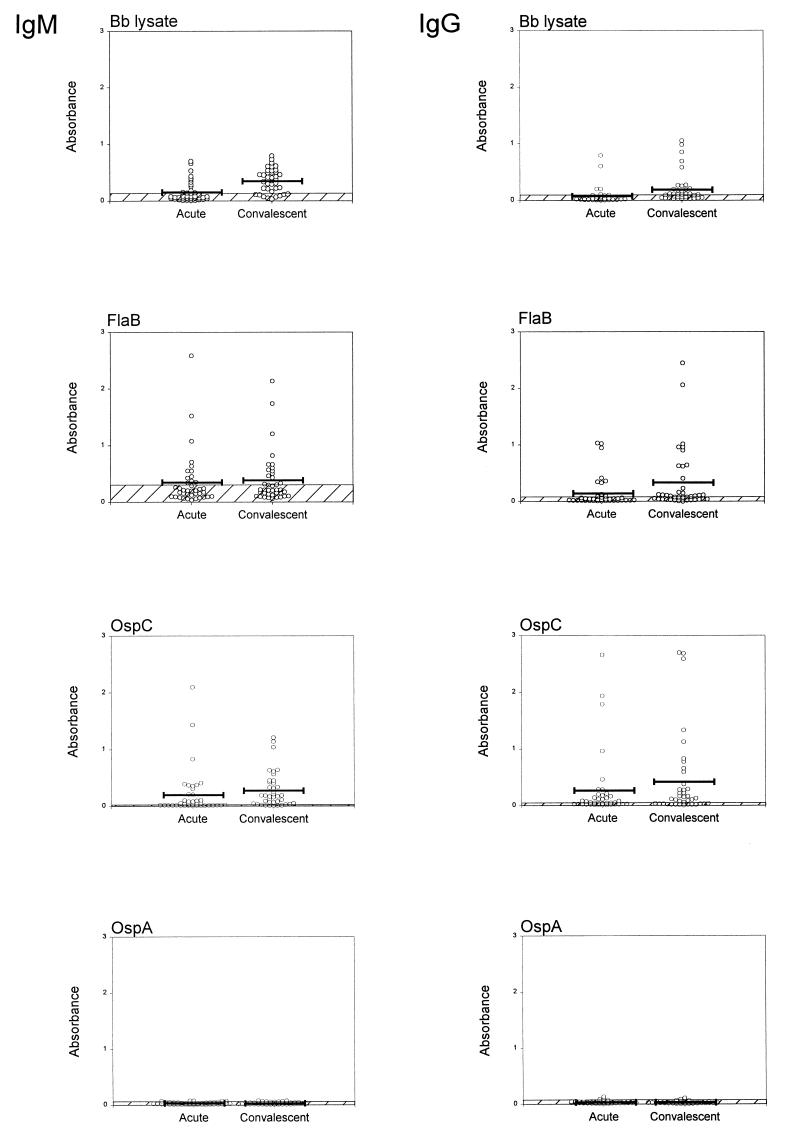
During acute infection, 16 of the 39 patients (41%) had positive antibody responses to B. burgdorferi lysate by ELISA, usually of the IgM isotype, which were at least 3 SD above the mean values of eight representative, healthy control subjects (Table 3; Fig. 2). In addition, 18 patients (46%) had responses to FlaB, and 24 (62%) had reactivity with OspC. In contrast, only six patients (15%) had IgM or IgG responses to OspA that were slightly above the cutoff value. Three to four weeks later, at the conclusion of antibiotic therapy, significantly more patients had IgM or IgG antibody responses to B. burgdorferi antigens. Altogether, 95% of the patients had such a response to one or more of the borrelial antigens tested. However, antibody reactivity with OspA did not increase either in frequency or magnitude.
TABLE 3.
Humoral immune response to B. burgdorferi antigens among 39 patients with EM
| Assay and antigen | Antibody response by ELISA during phasea
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| IgM
|
IgG
|
IgM or IgG
|
|||||||
| Acute | Conv | P | Acute | Conv | P | Acute | Conv | P | |
| ELISA | |||||||||
| B. burgdorferi lysate | 14 (36) | 30 (77) | <0.001 | 5 (13) | 23 (59) | <0.001 | 16 (41) | 36 (92) | <0.001 |
| FlaB | 12 (31) | 15 (38) | 0.6 | 10 (26) | 21 (54) | 0.02 | 18 (46) | 28 (72) | 0.04 |
| OspC | 18 (46) | 30 (77) | 0.01 | 15 (38) | 22 (56) | 0.09 | 24 (62) | 34 (87) | 0.02 |
| OspA | 3 (8) | 2 (5) | 1.0 | 3 (8) | 3 (8) | 1.0 | 6 (15) | 5 (13) | 1.0 |
| Any of the above antigens | 23 (59) | 36 (92) | 0.001 | 21 (54) | 32 (82) | 0.01 | 28 (72) | 37 (95) | 0.01 |
| Two-test approachb | 11 (26) | 26 (67) | <0.001 | 2 (5) | 4 (10) | 0.7 | 13 (33) | 29 (74) | <0.001 |
Acute- and convalescent (Conv)-phase samples of patients with EM were tested by ELISA for IgM and IgG responses to borrelial antigens. Except for P values, results are presented as number (percent) of samples testing positive.
ELISA and Western blotting.
FIG. 2.
Humoral immune responses to B. burgdorferi lysate and to recombinant spirochetal proteins are shown, determined by ELISA. The cross-hatched areas denote the mean value plus 3 SD for eight representative, healthy control subjects, whose serum samples were included on the same plate. The bar indicates the mean value of patients' responses. The values are greater in convalescent-phase samples than in acute-phase samples, but the differences were statistically significant only with B. burgdorferi lysate (P < 0.001).
Using the two-test approach of ELISA and Western blotting, 13 patients (33%) had positive IgM or IgG responses to B. burgdorferi lysate in acute-phase samples, and 29 patients (74%) had positive responses during convalescence.
Duration of infection and immune responses.
In acute-phase samples, the numbers of patients with positive cellular immune responses to B. burgdorferi lysate, FlaB, or OspC were similar in those with symptoms for <1 week or for ≥1 week (Table 4). In contrast, the percentage of patients with humoral immune responses to borrelial antigens tended to be greater in those with longer duration of disease, but antibody responses to OspA were rarely found at any time.
TABLE 4.
Cellular and humoral immune responses to B. burgdorferi antigens according to duration of acute infection
| Antigen | Resulta for patients with indicated duration of acute infection prior to sampling (days)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Proliferation assay
|
IgM ELISA
|
IgG ELISA
|
|||||||
| <7 (n = 31) | ≥7 (n = 8) | P | <7 (n = 31) | ≥7 (n = 8) | P | <7 (n = 31) | ≥7 (n = 8) | P | |
| B. burgdorferi lysate | 13 (42) | 4 (50) | 0.7 | 10 (32) | 4 (50) | 0.4 | 3 (10) | 2 (25) | 0.3 |
| FlaB | 2 (6) | 1 (13) | 0.5 | 8 (26) | 4 (50) | 0.2 | 5 (16) | 5 (63) | 0.02 |
| OspC | 7 (23) | 1 (13) | 1.0 | 12 (39) | 6 (75) | 0.1 | 11 (35) | 4 (50) | 0.7 |
| OspA | 8 (26) | 0 (0) | 0.2 | 2 (6) | 1 (13) | 0.5 | 3 (10) | 0 (0) | 1.0 |
Except for P values, results are presented as number (percent) of samples testing positive.
Localized versus disseminated infection.
Of the 39 patients, 13 had a clinical picture of localized infection, and 26 had clinical evidence of disseminated disease. The 13 patients with infection apparently localized to the skin usually had no other symptoms. In contrast, 8 of the 26 patients (31%) with clinical evidence of disseminated infection had secondary annular skin lesions, and most of the 26 patients had headache and neck stiffness or arthralgias, which were usually accompanied by malaise and fatigue. Patients with localized or disseminated infection had a similar median duration of EM prior to evaluation by the study physicians—3 days for the group with localized infection and 4 days for the group with disseminated infection.
In both the acute and convalescent phases of the illness, the percentage of patients with proliferative responses to B. burgdorferi lysate or recombinant borrelial antigens was similar in those with clinical evidence of localized or disseminated infection (Table 5). In contrast, humoral immune reactivity with each of the spirochetal antigens tested tended to be greater among those with disseminated infection, particularly during convalescence. At that time, 81 and 96% of patients had antibody responses to FlaB or OspC, respectively, compared with 54 and 69% of those with localized disease, which were differences of possible statistical significance.
TABLE 5.
Cellular and humoral immune responses to B. burgdorferi antigens according to localized or disseminated infection
| Antigen | Result for patients with indicated infectiona
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proliferation assay
|
IgM or IgG antibody response
|
|||||||||||
| Acute
|
Convalescent
|
Acute
|
Convalescent
|
|||||||||
| Local (n = 13) | Dissem (n = 26) | P | Local (n = 13) | Dissem (n = 26) | P | Local (n = 13) | Dissem (n = 26) | P | Local (n = 13) | Dissem (n = 26) | P | |
| B. burgdorferi lysate | 5 (38) | 12 (46) | 0.7 | 9 (31) | 12 (46) | 0.3 | 4 (31) | 12 (46) | 0.5 | 11 (85) | 25 (96) | 0.3 |
| FlaB | 3 (23) | 0 (0) | 0.03 | 6 (46) | 8 (31) | 0.5 | 6 (46) | 12 (46) | 1.0 | 7 (54) | 21 (81) | 0.1 |
| OspC | 4 (31) | 4 (15) | 0.4 | 6 (46) | 8 (31) | 0.5 | 7 (54) | 17 (65) | 0.5 | 9 (69) | 25 (96) | 0.04 |
| OspA | 3 (23) | 5 (19) | 1.0 | 7 (54) | 10 (38) | 0.5 | 3 (23) | 3 (12) | 0.4 | 0 (0) | 5 (19) | 0.1 |
Acute- and convalescent-phase samples from patients with localized infection (Local) or disseminated infection (Dissem) were tested by the indicated assays. Except for P values, results are presented as number (percent) of samples testing positive.
Correlation of cellular and humoral immune responses.
Cellular immune responses to B. burgdorferi did not correlate with humoral immune reactivity. During both acute and convalescent phases of the illness, the numbers of patients with antibody reactivity were greater than the numbers with cellular immune responses (Tables 2 and 3). Moreover, there were patients with weak cellular reactivity and strong humoral responses or vice versa (data not shown). Overall, cellular reactivity with OspA was as frequent and as strong as the cellular responses to FlaB and OspC. In contrast, patients often had antibody reactivity with FlaB and OspC, but only a few had slight antibody responses to OspA.
DISCUSSION
In this study of patients with culture-positive EM, cellular and humoral immune responses to B. burgdorferi antigens were often found among patients with early Lyme disease. In acute-phase samples, 51% of the patients had proliferative cellular immune responses and 72% had antibody responses, defined as values at least 3 SD above the mean values of healthy control subjects. Because spirochetal killing and antigen processing continue for some time after initial antibiotic treatment, the percentage of patients with positive cellular or humoral immune responses was greater during convalescence, approximately 3 weeks later, at the conclusion of antibiotic therapy. By that time, 64% of the patients had proliferative cellular reactivity and 95% had antibody reactivity, determined by ELISA, with at least one of the spirochetal antigens tested. Using the more-stringent two-test approach of ELISA and Western blotting, 74% had antibody responses during convalescence, a percentage compatible with past experience (10, 12). Since B-cell responses usually require T-cell help, the apparent greater frequency of humoral compared with cellular responses suggests that ELISA may be more sensitive for the determination of antibody responses than proliferation assay for the determination of T-cell responses. However, specific antibody diffuses freely from peripheral lymph nodes, whereas borrelia-specific T cells are presumably located preferentially in regional lymph nodes and at the site of infection in EM lesions. Thus, a humoral response may simply be easier to detect in peripheral blood than a cellular response. Alternatively, some B cells may be activated by T-cell-independent antigens.
In this study, cellular immune responses to OspA were found as frequently as those to OspC and FlaB. Although antibody responses were also frequently seen to OspC and FlaB, only a few patients had slight antibody reactivity with OspA. Dissociation of the cellular and humoral immune responses to OspA has been noted previously (19). To explain these immune findings, we postulate the following series of events. Immune cells first encounter B. burgdorferi in the skin at the site of the tick bite. EM lesions have mild-to-marked perivascular infiltrates of T cells and macrophages and, sometimes, small numbers of plasma cells (23). As a part of the innate immune response, spirochetal lipoproteins bind the CD14 molecule and toll-like receptor 2 on macrophages in EM lesions, which leads to the production of proinflammatory cytokines (16). To initiate an adaptive immune response, antigen presenting cells, including macrophages and dendritic cells, engulf spirochetes (13) and migrate via afferent lymphatics to peripheral lymph nodes where they present processed spirochetal peptides to T cells. Some spirochetes in EM lesions may express small amounts of OspA, and the presentation of small amounts of processed OspA peptides in regional lymph nodes may be enough to trigger a T-cell response. A single major histocompatibility peptide complex can trigger serially up to 200 T-cell receptors (31), and optimal T-cell stimulation may be achieved by interaction with as few as 1,500 T-cell receptors as long as costimulatory molecules are also engaged (31, 32). Borrelia-specific B cells are activated by intact B. burgdorferi antigens, which cross-link surface immunoglobulin, usually in the presence of T-cell help. In contrast with the small amounts of peptides required to activate T cells, the amount of antigen required for activation of an individual B cell is variable and depends on B-cell receptor affinity (2). Therefore, in most cases, the amounts of intact OspA draining to lymph nodes must be insufficient to cross-link immunoglobulin on the surface of B cells, and therefore, B cells are not activated.
Although it has been demonstrated that the spirochete down-regulates OspA early in the infection (22), to date it has not been possible to examine OspA expression directly later in the illness. Nevertheless, the strong cellular and humoral immune responses to OspA that develop in some patients with Lyme arthritis (1, 5, 10, 17–20, 33) suggest that the spirochete may sometimes up-regulate the expression of this protein within the inflamed joint. In genetically susceptible patients, particularly those with HLA-DRB1∗0401 or related alleles (29), cellular and humoral reactivity with OspA is associated with persistent knee swelling for months or even several years after treatment with ≥2 months of oral antibiotics or ≥1 month of intravenous antibiotics (5, 17, 18, 20, 30). It has been postulated that such treatment-resistant courses may develop within the proinflammatory milieu of the joint because of molecular mimicry between a dominant T-cell epitope of OspA and human lymphocyte function associated antigen-1 (15) or another similar autoantigen. Presumably, such responses do not develop in patients with T-cell responses to OspA early in the infection because tolerance may be broken only after prolonged exposure to this protein within the pro-inflammatory microenvironment of the joint.
In the current study, the frequency of proliferative cellular immune responses was similar among patients with localized or disseminated infection. Thus, antigen presenting cells seem to present processed spirochetal antigens to T cells in regional lymph nodes as often in patients with localized infection as in those with disseminated disease. In contrast, patients with disseminated disease more often had measurable antibody responses to borrelial antigens, particularly during convalescence. Presumably, patients with disseminated disease have more intact borrelial antigens that reach lymphatic tissue, where they induce a borrelia-specific antibody response. However, none of the responses that we measured correlated with the severity of early infection.
In the late 1980s, Dattwyler et al. described 17 patients who were treated with antibiotic therapy for EM but subsequently developed attenuated symptoms of late Lyme disease (8). Although all 17 patients were seronegative, 14 had cellular responses to B. burgdorferi by proliferation assay. Subsequent studies reported that the proliferation assay lacked either sensitivity (11) or specificity (34), depending on how the cutoff values were defined. For this reason, we do not advocate the use of this test by itself to support the diagnosis of Lyme disease. However, as performed here for patients with culture-confirmed EM, we believe that the assay gave reliable results. Although B. burgdorferi sonicate may cause mitogenic responses, PBL from many patients did not react with this preparation. Moreover, the number of patients with positive responses and the strength of the responses were usually greater in convalescent-phase samples than in acute-phase specimens, a pattern suggestive of true-positive responses.
In summary, cellular and humoral immune reactivity were often found to B. burgdorferi antigens among patients with early Lyme disease, particularly during convalescence. Although both cellular and humoral responses were frequently found to FlaB and OspC, only cellular reactivity was usually found with OspA. The dissociation of the cellular and humoral immune response to OspA, a protein that is down-regulated early in the infection, may occur because small amounts of processed peptides may trigger T cells, whereas intact antigen is required to activate B cells.
ACKNOWLEDGMENTS
We thank Marcia Pellegrino and Norma Grills for help with patient care and the collection of samples and Ronald Ste. Marie and Colleen Fitzpatrick for help with preparation of the manuscript.
This study was supported by Cooperative Agreement CCU110291 from the Centers for Disease Control and Prevention, the Mathers Foundation, the Lyme/Arthritis Research Foundation, and the Eshe Fund. A. Vaz received support from NIH training grant TAR-07570.
REFERENCES
- 1.Akin E, McHugh G L, Flavell R A, Fikrig E, Steere A C. The immunoglobulin (IgG) antibody response to OspA and OspB correlates with severe and prolonged Lyme arthritis and the IgG response to P35 correlates with mild and brief arthritis. Infect Immun. 1999;67:173–181. doi: 10.1128/iai.67.1.173-181.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Batista F D, Neuberger M S. Affinity dependence of the B cell response to antigen: a threshold, a ceiling, and the importance of off-rate. Immunity. 1998;8:751–759. doi: 10.1016/s1074-7613(00)80580-4. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Case definitions for public health surveillance. Morb Mortal Wkly Rep. 1990;39:19–21. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Recommendations for test performance and interpretation from the Second International Conference on Serologic Diagnosis of Lyme Disease. Morb Mortal Weekly Rep. 1995;44:1. [PubMed] [Google Scholar]
- 5.Chen J, Field J A, Glickstein L, Molloy P J, Huber B T, Steere A C. Association of antibiotic treatment-resistant Lyme arthritis with T cell responses to dominant epitopes of outer-surface protein A (OspA) of Borrelia burgdorferi. Arthritis Rheum. 1999;42:1813–1822. doi: 10.1002/1529-0131(199909)42:9<1813::AID-ANR4>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 6.Craft J E, Grodzicki R L, Steere A C. The antibody response in Lyme disease: evaluation of diagnostic tests. J Infect Dis. 1984;149:789–795. doi: 10.1093/infdis/149.5.789. [DOI] [PubMed] [Google Scholar]
- 7.Dattwyler R J, Thomas J A, Benach J L, Golightly M G. Cellular immune response in Lyme disease: the response to mitogens, live Borrelia burgdorferi, NK cell function, and lymphocyte subsets. Zentbl Bakteriol Hyg A. 1986;263:151–159. doi: 10.1016/s0176-6724(86)80118-3. [DOI] [PubMed] [Google Scholar]
- 8.Dattwyler R J, Volkman D J, Luft B J, Halperin J J, Thomas J, Golightly M G. Seronegative Lyme disease: dissociation of the specific T- and B-lymphocyte responses to Borrelia burgdorferi. N Engl J Med. 1988;319:1441–1446. doi: 10.1056/NEJM198812013192203. [DOI] [PubMed] [Google Scholar]
- 9.de Silva A M, Fikrig E. Arthropod- and host-specific gene expression by Borrelia burgdorferi. J Clin Investig. 1997;100:S3–S5. doi: 10.1172/JCI119169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dressler F, Whalen J A, Reinhardt B N, Steere A C. Western blotting in the serodiagnosis of Lyme disease. J Infect Dis. 1993;167:392–400. doi: 10.1093/infdis/167.2.392. [DOI] [PubMed] [Google Scholar]
- 11.Dressler F, Yoshinari N H, Steere A C. The T cell proliferative assay in the diagnosis of Lyme disease. Ann Intern Med. 1991;115:533–539. doi: 10.7326/0003-4819-115-7-533. [DOI] [PubMed] [Google Scholar]
- 12.Engstrom S M, Shoop E, Johnson R C. Immunoblot interpretation criteria for serodiagnosis of early Lyme disease. J Clin Microbiol. 1995;33:419–427. doi: 10.1128/jcm.33.2.419-427.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Filgueira L, Nestle F O, Rittig M, Joller H I, Groscurth P. Human dendritic cells process and phagocytose Borrelia burgdorferi. J Immunol. 1996;157:2998–3005. [PubMed] [Google Scholar]
- 14.Fung B P, McHugh G L, Leong J M, Steere A C. Humoral immune response to outer surface protein C of Borrelia burgdorferi in Lyme disease: role of the immunoglobulin M response in the serodiagnosis of early infection. Infect Immun. 1994;62:3213–3221. doi: 10.1128/iai.62.8.3213-3221.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gross D M, Fortshuber T, Tary-Lehmann M, Etling C, Kouichi I, Nagy Z A, Field J A, Steere A C, Huber B T. Identification of LFA-1 as a candidate autoantigen in treatment-resistant Lyme arthritis. Science. 1998;281:703–706. doi: 10.1126/science.281.5377.703. [DOI] [PubMed] [Google Scholar]
- 16.Hirschfeld M, Kirschning C J, Schwandner R, Wesche H, Weis J H, Wooten R M, Weis J J. Inflammatory signaling by Borrelia burgdorferi lipoproteins is mediated by toll-like receptor 2. J Immunol. 1999;163:2382–2386. [PubMed] [Google Scholar]
- 17.Kalish R A, Leong J M, Steere A C. Association of treatment resistant chronic Lyme arthritis with HLA-DR4 and antibody reactivity to OspA and OspB of Borrelia burgdorferi. Infect Immun. 1993;61:2774–2779. doi: 10.1128/iai.61.7.2774-2779.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalish R A, Leong J M, Steere A C. Early and late antibody responses to full-length and truncated constructs of outer-surface protein A of Borrelia burgdorferi in Lyme disease. Infect Immun. 1995;63:2228–2235. doi: 10.1128/iai.63.6.2228-2235.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krause A, Burmester G R, Rensing A, Schoerner C, Schaible U E, Simon M M, Herzer P, Kramer M D, Wallich R. Cellular immune reactivity to recombinant OspA and flagellin from Borrelia burgdorferi in patients with Lyme borreliosis. Complexity of humoral and cellular immune responses. J Clin Investig. 1992;90:1077–1084. doi: 10.1172/JCI115923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lengl-Janßen B, Strauss A F, Steere A C, Kamradt T. The T helper response in Lyme arthritis: differential expression of Borrelia burgdorferi outer surface protein A (OspA) in patients with treatment-resistant or treatment-responsive Lyme arthritis. J Exp Med. 1994;180:2069–2078. doi: 10.1084/jem.180.6.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma B, Christen C, Leung D, Vigo-Pelfrey C. Serodiagnosis of Lyme borreliosis by Western immunoblot: reactivity of various significant antibodies against Borrelia burgdorferi. J Clin Microbiol. 1992;30:370–376. doi: 10.1128/jcm.30.2.370-376.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montgomery R R, Malawista S E, Feen K J M, Bockenstedt L K. Direct demonstration of antigenic substitution of Borrelia burgdorferi ex vivo: exploration of the paradox of the early immune response to outer surface proteins A and C in Lyme disease. J Exp Med. 1996;183:261–269. doi: 10.1084/jem.183.1.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mullegger R R, McHugh G, Ruthazer R, Binder B, Kerl H, Steere A C. Differential expression of cytokine mRNA in skin specimens from patients with erythema migrans or acrodermatitis chronica atrophicans. J Investig Dermatol. 2000;115:1115–1123. doi: 10.1046/j.1523-1747.2000.00198.x. [DOI] [PubMed] [Google Scholar]
- 24.Nadelman R B, Nowakowski J, Forseter G, Goldberg N S, Bittker S, Cooper D, Aguero-Rosenfeld M, Wormser G. The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. Am J Med. 1996;100:502–508. doi: 10.1016/s0002-9343(95)99915-9. [DOI] [PubMed] [Google Scholar]
- 25.Robinson J M, Pilot-Matias T J, Pratt S D, Patel C B, Bevirt T, Hunt J C. Analysis of the humoral response to the flagellin protein of Borrelia burgdorferi: cloning of regions capable of differentiating Lyme disease from syphilis. J Clin Microbiol. 1993;31:629–635. doi: 10.1128/jcm.31.3.629-635.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwan T G, Piesman J, Golde W T, Dolan M C, Rosa P A. Induction of an outer surface protein on Borrelia burgdorferi during tick feeding. Proc Natl Acad Sci USA. 1995;92:2909–2913. doi: 10.1073/pnas.92.7.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steere A C. Lyme disease. N Engl J Med. 2001;345:115–125. doi: 10.1056/NEJM200107123450207. [DOI] [PubMed] [Google Scholar]
- 28.Steere A C, Bartenhagen N H, Craft J E, Hutchinson G J, Newman J H, Rahn D W, Sigal L H, Spieler P H, Stenn K S, Malawista S E. The early clinical manifestations of Lyme disease. Ann Intern Med. 1983;99:76–82. doi: 10.7326/0003-4819-99-1-76. [DOI] [PubMed] [Google Scholar]
- 29.Steere A C, Baxter-Lowe L A. Association of chronic, treatment-resistant Lyme arthritis with rheumatoid arthritis (RA) alleles. Arthritis Rheum. 1998;41:S81. [Google Scholar]
- 30.Steere A C, Levin R E, Molloy P J, Kalish R A, Abraham III J H, Liu N Y, Schmid C H. Treatment of Lyme arthritis. Arthritis Rheum. 1994;37:878–888. doi: 10.1002/art.1780370616. [DOI] [PubMed] [Google Scholar]
- 31.Valitutti S, Muller S, Cella M, Padovan E, Lanzavecchia A. Serial triggering of many T-cell receptors by a few peptide-MHC complexes. Nature. 1995;375:148–151. doi: 10.1038/375148a0. [DOI] [PubMed] [Google Scholar]
- 32.Viola A, Lanzavecchia A. T cell activation determined by T cell receptor number and tunable thresholds. Science. 1996;273:104–106. doi: 10.1126/science.273.5271.104. [DOI] [PubMed] [Google Scholar]
- 33.Yoshinari N H, Reinhardt B N, Steere A C. T cell responses to polypeptide fractions of Borrelia burgdorferi in patients with Lyme arthritis. Arthritis Rheum. 1991;34:707–713. doi: 10.1002/art.1780340611. [DOI] [PubMed] [Google Scholar]
- 34.Zoschke D C, Skemp A A, Defosse D L. Lymphoproliferative responses to Borrelia burgdorferi in Lyme disease. Ann Intern Med. 1991;114:285–289. doi: 10.7326/0003-4819-114-4-285. [DOI] [PubMed] [Google Scholar]