Abstract
Objective:
To conduct a pilot randomized controlled trial of eHealth Mindful Movement and Breathing (eMMB) compared to an empathic attention control (AC).
Participants:
Women undergoing surgery for a suspected gynecologic malignancy.
Methods:
eMMB is a brief yoga intervention delivered remotely during the perioperative timeframe. We assessed feasibility and participants completed assessments (baseline, weeks 2 and 4 postoperatively). We summarized feasibility, participant characteristics, and outcomes by intervention group and time.
Findings:
Forty-three percent of eligible patients approached participated (n=31). Adherence to the interventions was 77%. Percent of participants to complete outcomes was 81% at Week 2 and 84% at Week 4 (>70%; retention was the primary feasibility indicator). Average reductions in the primary outcome of pain intensity were larger in the eMMB group than AC group (Week 2 d=−0.38; Week 4 d=−0.46).
Implications:
This pilot study of eMMB supported feasibility and improvements in pain intensity that warrant a future efficacy study.
Keywords: Yoga, mindfulness, pain, depression, gynecologic surgery
Introduction
Over 100,000 women are diagnosed with gynecologic cancers in the United States each year and many require major abdominal surgery (1). Most (64%) of these women experience pain (2), and inadequate pain control remains among the most common reasons for hospital admission after surgery (3). In addition, many women report postoperative sleep disturbances (39-70%; 2, 4) and psychological distress (20%; 2, 5) both of which are associated with pain (2, 6). There are likely bidirectional relationships among pain, sleep disturbances and psychological distress (4). Such acute postoperative symptoms are important to address because they predict persistent symptoms (4, 7) and a reduced quality of life (8). Therefore, interventions to simultaneously improve postoperative pain, sleep disturbances, and psychological distress are needed to improve immediate and longer-term outcomes.
Women who have had surgery and been diagnosed with cancer are particularly vulnerable to chronic pain (9). While treatment of acute pain decreases the likelihood of chronic pain (9, 10), even post-treatment, the prevalence of chronic pain is estimated to be 30-35% among cancer survivors, approximately double the prevalence in the general population (11, 12). There is sufficient research supporting the recommendation for a multimodal approach that includes non-pharmacologic interventions (exercise and meditation; 10, 13) in clinical guidelines for the general treatment of chronic pain in cancer survivors and postoperative pain. Yet, there are insufficient data specific to postoperative care for gynecologic cancer surgery, so clinical guidelines for this patient group do not include non-pharmacologic approaches to pain management (14). Randomized controlled efficacy studies of non-pharmacological interventions are needed to inform consistent guidelines for optimal multimodal pain management in women undergoing gynecologic cancer surgery.
Yoga is a non-pharmacological intervention that could comprehensively improve the biobehavioral aspects of pain and associated symptoms (i.e., sleep disturbances, psychological distress). The core components of yoga are movements, meditation, and breathing practices (15). Evidence supports the efficacy of yoga as an intervention for reducing pain (16), sleep disturbances (17), and psychological distress (18), in a variety of populations including cancer survivors (19).
There is limited research investigating the efficacy of yoga delivered individually or within a surgical context. Initial studies that have included components of yoga delivered perioperatively have found reductions in pain (20), psychological distress (anxiety; 21), and postoperative length of hospital stay (20, 22). It is possible that yoga may further support other goals of postoperative care (e.g., early postoperative mobilization) and therefore help reduce other surgical management outcomes (e.g., length of stay). The multiple components of yoga may also add to benefits of other perioperative non-pharmacological interventions (e.g., relaxation; 23, 24).
Therefore, we conducted a pilot randomized controlled trial of an eHealth Mindful Movement and Breathing (eMMB) yoga intervention (25) compared to an empathic attention control (AC) among women undergoing surgery for a suspected gynecologic malignancy. Our primary objective was to assess feasibility (i.e., recruitment, adherence, retention). Our secondary objectives included assessing descriptive data on proposed outcomes (i.e., pain, sleep disturbances, psychological distress) and adverse events.
Methods
Participants and Trial Design
Participants were recruited at a private urban academic cancer center from December 2018-March 2020 (ended early due to COVID-19). Participants seen at this cancer center receive care concordant with clinical guidelines for pharmacologic pain management (14). Adult females ≥18 years of age were included if they were scheduled for an abdominal gynecological surgery to remove a suspected malignancy (i.e. uterine, ovarian), had an Eastern Cooperative Oncology Group (ECOG) performance status of ≤1, were cognitively able to complete assessments as judged by the study team, and were able to understand, read and write English. Women were excluded if they had any psychotic disorder, or a diagnosed sleep disorder (including untreated obstructive sleep apnea, periodic limb movement disorder, or restless leg syndrome). This trial was approved by the Wake Forest University Health Sciences Institutional Review Board (IRB00052655) and registered with clinicaltrials.gov (NCT03681405).
To identify participants, the research staff screened appointment lists and communicated with attending physicians regarding patients’ potential eligibility for the trial. Participants completed informed consent and baseline assessments either electronically (via REDCap) or in person before surgery. After participants provided informed consent, they were randomized to the eMMB or AC. Randomization (1:1) was computer-generated, stratified by cancer type (ovarian or uterine) and invasiveness of the planned surgical procedure type (i.e., laparotomy or minimally invasive), and concealed by the study biostatistician. Study team members did not know group assignment when discussing consent and were made aware of group assignments after participants provided informed consent.
Most follow-up assessments were completed remotely via a REDCap survey link. The staff member who collected primary outcome data in the clinical setting (that was not collected remotely) was blinded to group assignment. Participants were told that they could be randomly assigned to one of two different supportive treatments with a general description of what they would involve (i.e., counseling, gentle movement, writing, and/or relaxation strategies) and no indication of which was hypothesized to be more efficacious. They were also asked not to discuss study procedures with their treating surgeon, medical staff, or research personnel. Thus, participants and healthcare providers were also blinded to perceived active group assignment.
Study Interventions
eHealth Mindful Movement and Breathing (eMMB).
We called our yoga intervention “Mindful Movement and Breathing (MMB)” based on participant feedback in preliminary work to describe the gentle movements that can be done in a bed (26). The remotely-delivered eMMB intervention was developed through an iterative process that included a feasibility study to refine delivery strategies, which were primarily self-directed (25). eMMB taught awareness meditation, movement, breathing, and relaxation. The movements were adapted to be taught in a bed and chosen to be appropriate following surgery. Instructors were accredited and experienced at teaching patients with medical conditions.
Participants were asked to watch a 20-minute eMMB video via loaned tablet or email link at least once before surgery. Instructors called participants before surgery to answer any questions and offer additional guidance upon request throughout the study. The instructor also met with the participant (who was either in the hospital room or at home) via a synchronous videoconference or telephone call for approximately 30 minutes the day following surgery. During this time, instructors discussed any questions, guided eMMB, and encouraged self-directed practice. Participants were asked to continue the use of the eMMB video daily for at least two weeks following surgery.
Attention Control (AC).
As recommended for the study of mind-body practices (27) and used in previous studies (28), empathic attention was employed to attempt to control for the added attention, efficacy expectations of, and self-directed practice frequency in the active intervention. In addition, the interventionist asked patients to write brief daily entries once before surgery and daily for two weeks following surgery. Participants were given the option to complete diaries on paper or through the REDCap application on study tablets (accessible offline). The AC interventionist called participants before surgery and offered additional caring attention upon request at any time throughout the study. The interventionist also met with the participant via a synchronous videoconferencing or telephone session following surgery for approximately 30 minutes to provide caring attention. The AC was delivered by individuals with experience working in a medical setting who were trained to create and maintain relationships by using techniques such as active listening, reflection statements, and avoiding negative judgments. Interventionists used standardized instructions to prompt patients as adapted from previous studies (29, 30): “What were some of the events or circumstances that affected you in the past two weeks?” The instructions for two weeks of daily diary entries (to match the time practicing the intervention) were the same with reference to the past day and this additional sentence: “Think back over the past day and write down on the lines below up to five events that had an impact on you” (29).
Treatment Fidelity.
A number of steps were taken to ensure treatment fidelity (31). The study team trained interventionists in delivery of eMMB and AC during an initial session. The interventionists completed an initial written test to confirm understanding, documented the synchronous videoconference or phone session with a checklist, and audio recorded this session for all participants. Twenty percent of recordings were randomly selected for review by an investigator who observed the sessions, completed the same checklist, and discussed any discrepancies with the protocol in ongoing meetings that reinforced the initial training (yoga therapist AW reviewed eMMB sessions, clinical psychologist SCD reviewed AC sessions).
Measures
Study process variables were tracked to assess feasibility (e.g., recruitment, adherence, assessment completion) and adverse events. Patient-reported assessments were collected at four time points: before surgery (baseline), one day after surgery, two weeks after surgery and four weeks after surgery. Assessments were completed either while participants were at home or on site for standard care.
Process Variables.
The recruitment proportion was defined as the number who agreed to participate among those who were eligible and we aimed to enroll at least 50% of eligible patients. Adherence was assessed through completion of the synchronous session with the instructor. Number of days participants used the self-directed intervention was assessed retrospectively (in the past week) at postoperative week 2. We considered adequate adherence to the protocol if 70% of participants completed the planned synchronous session and 3 or more days of self-directed intervention activity reported in the week assessed. Any additional contact with the interventionists was also tracked. Assessment completion/retention was assessed with the percent completion of planned assessments at weeks 2 and 4 indicating that participants were retained in the study. We designated a priori that an adequate retention rate of at least 70% at week 2 was our primary indicator of feasibility as informed by our prior feasibility work (26).
Patient-Reported Outcome Measures.
Pain was assessed with the Patient Reported Outcomes Measurement Information System (PROMIS) measure of pain intensity, which was selected for the primary outcome (at 2 weeks) in the planned future study and adapted for assessing pain on a numeric rating scale from 0 (no pain) to 10 (worst imaginable pain) “in the last day” (32). We measured pain interference, the impact of pain on daily life activities, with the 6-item PROMIS measure (32). Items are summed, converted to a standardized T-score, and higher T-scores on this and all PROMIS measures indicates more of the construct measured. The affective dimension of pain “in the last day” was assessed with one item on a scale from 0 (not bad at all) to 10 (the most unpleasant feeling possible for me) (28, 33). Sleep disturbance was assessed with a PROMIS Sleep Disturbance short-form (34) adapted for daily use. We measured psychological distress “in the last day” with the PROMIS Depression and Anxiety adapted short-forms (32).
Adverse events.
Each interventionist monitored any adverse events experienced during the synchronous session. In addition, interventionists asked participants if they experienced any problems during self-directed practice. Participants also completed two 100 mm Visual Analogue Scale (VAS) items assessing pain intensity and psychological distress with the instructions to report their experience “right now,” immediately before and after the synchronous intervention to detect any acute adverse events (26). Any reported worsening was discussed in real-time with participants and documented. Adverse events were labeled according to severity and likelihood that they were related to study interventions according to the NCI Common Terminology Criteria for Adverse Events version 4.0. Only adverse events possibly related to the study intervention or procedures were captured with the exception of unexpected serious adverse events, which were also documented and reported.
Demographic and Clinical Data.
Age, race/ethnicity, relationship status, education level, ability to pay monthly bills, smoking status, distance traveled for care, medical history, internet use, and previous use of mind-body practices (including yoga) or psychological services were self-reported at baseline. Cancer site, type of surgery, stage, recurrence status, performance status, comorbid chronic pain and anxiety/depression, height, weight, and prescription medications for pain were abstracted from medical charts at baseline. Time to mobilization and length of stay were abstracted four weeks postoperatively.
Analyses.
We employed a contemporary approach to assess feasibility, variability of outcomes, and adverse events to inform a future efficacy study (rather than reporting underpowered hypothesis tests; 35). The original target sample size (N=44) was based on estimating the parameters of interest within +/− 15% using a two-sided 95% confidence interval. With the COVID-19 pandemic, recruitment was stopped at the institution and we re-examined our target sample size, ultimately deciding that n=31 provided reasonable 95% CI for the rates (within +/−18%). Power calculations for a subsequent larger study will be based on clinically meaningful differences between the groups on the primary outcome of pain intensity (36).
Data were cleaned prior to study unblinding and databases were locked prior to analysis by group. We calculated 95% confidence intervals (CI) for each of the feasibility measures (i.e., recruitment, adherence, and retention rates) to determine the range of estimates that were consistent with our data. Enrolled participants were compared to eligible participants who were both not approached and actively declined participation on key variables using chi-square tests and ANOVA, using a two-tailed alpha of 0.05. For our remaining analyses by intervention group, we did not employ statistical testing, but rather quantified variability with confidence intervals and effect sizes. Descriptive analyses included summaries of demographic and clinical characteristics and outcomes by intervention group and time. The distributions of continuous variables were examined to determine the presence of outliers and whether transformations were necessary for analysis. We computed Cohen’s d effect sizes and used the following guidelines for interpretation: 0.2, small effect; 0.5, medium effect; 0.8, large effect (37). T-tests were used to evaluate difference between groups on changes in pain and distress from before to after the synchronous intervention session. SAS (v9.4, Cary, NC) was used for statistical analyses.
Results
Enrollment occurred from October 2018-March 2020. Overall, 231 patients were screened for this study (Figure 1: Study Flow Diagram). Of these, n=107 were deemed eligible, and n=31 or 29% (95% CI: 21%-39%) of those eligible agreed to participate. Of the 73 patients approached about study participation, 42% (31/73; 95% CI: 31%-55%) agreed to participate. Additionally, we found that the proportion of eligible patients agreeing to participate increased to 53% (9 enrolled/17 approached; 95% CI: 28-77%) during a time period towards the end of recruitment when we focused on approaching more participants in person in the clinic rather than by telephone. We also aimed to improve recruitment by mailing study information materials to patients who did not have an in-person appointment before surgery. We found no significant differences with respect to age, ethnicity, race, cancer type, or surgery type among eligible patients who enrolled (n=31), eligible patients who actively declined enrollment after being approached (n=42), or eligible patients not approached due to logistical barriers to study coordination (n=34; Supplementary Table 1).
Figure 1.
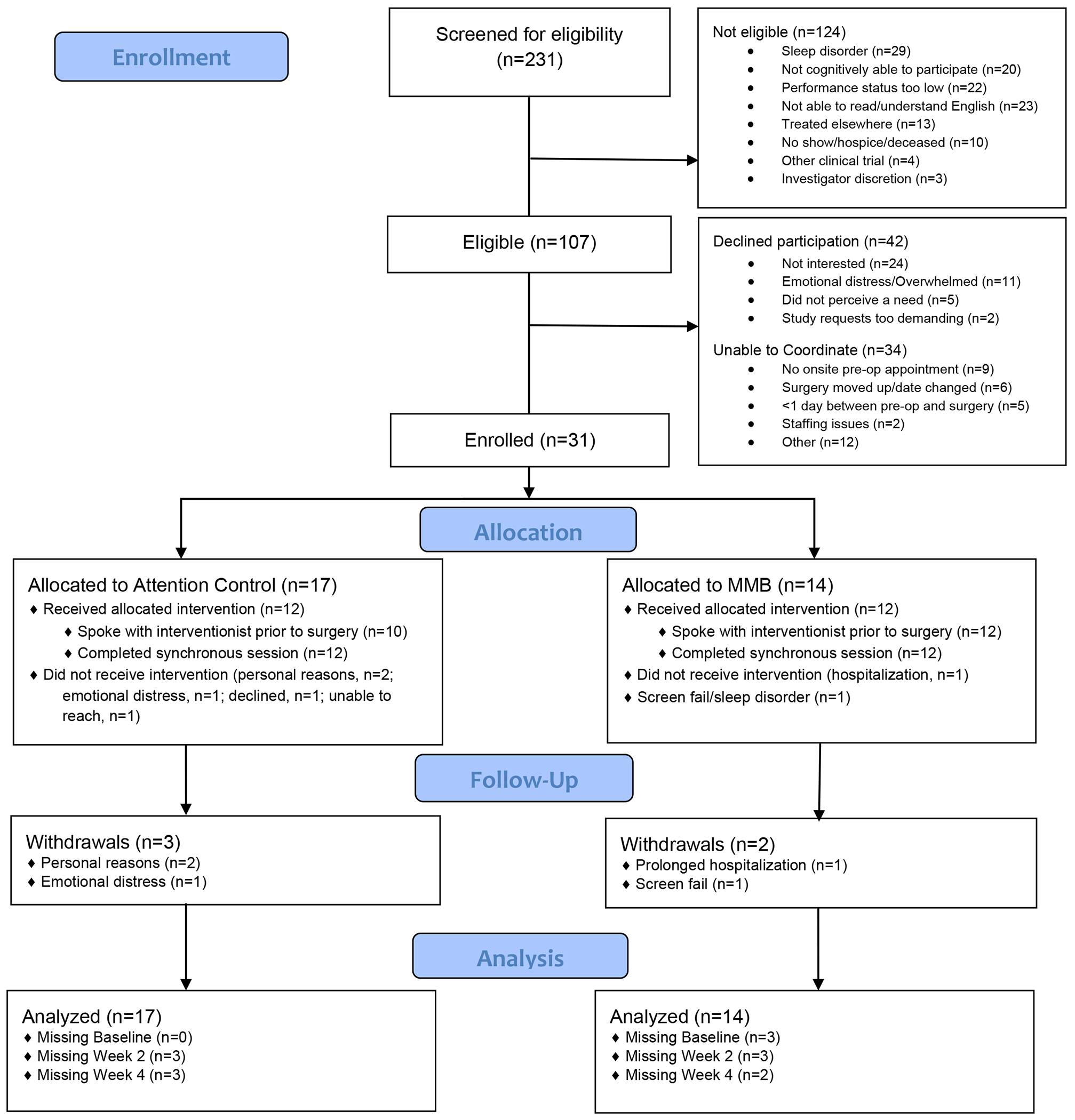
Study Flow Diagram
Enrolled participants (n=31; eMMB n=14, AC n=17) were on average 59.7 (SD=11.2) years of age at enrollment. All but one participant (97%) were White, and the suspected cancer type was relatively evenly divided (uterine 53%; ovarian 47%; Table 1). At follow-up chart review, 52% had a confirmed uterine mass (16 participants; 13 malignant, 3 benign), 42% had a confirmed ovarian mass (13 participants; 7 malignant, 6 benign), one enrolled participant with suspected ovarian cancer actually had an ovarian mass that turned out to be a metastasis from breast cancer, and one was not classified (ineligibility detected after randomization due to a sleep disorder documented during the clinic visit).
Table 1.
Participant Baseline Characteristics
| Total Sample (n=30) b | Mindful Movement and Breathing (n=13) | Attention Control (n=17) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Characteristics | N | % | N | % | N | % |
| Ethnicity | ||||||
| Not Hispanic or Latino | 30 | 100.0% | 13 | 100.0% | 17 | 100.0% |
| Race | ||||||
| Black or African American | 1 | 3.3% | 0 | 0.0% | 1 | 5.9% |
| White | 29 | 96.7% | 13 | 100% | 16 | 94.1% |
| Relationship | ||||||
| Currently married/living with partner | 18 | 60.0% | 8 | 61.5% | 10 | 58.8% |
| Separated/divorced | 4 | 13.3% | 0 | 0% | 4 | 23.5% |
| Widowed | 5 | 16.7% | 3 | 23.1% | 2 | 11.8% |
| Never married | 0 | 0.0% | 0 | 0% | 0 | 0.0% |
| Unknown | 3 | 10.0% | 2 | 15.4% | 1 | 5.9% |
| Education | ||||||
| High school or equivalent | 5 | 16.7% | 2 | 15.4% | 3 | 17.7% |
| Technical/vocational school/some college | 13 | 43.3% | 5 | 38.5% | 8 | 47.1% |
| College graduate | 6 | 20.0% | 2 | 15.4% | 4 | 23.5% |
| Post graduate degree | 3 | 10.0% | 2 | 15.4% | 1 | 5.9% |
| Unknown | 3 | 10.0% | 2 | 15.4% | 1 | 5.9% |
| How difficult to pay monthly bills | ||||||
| Very difficult/somewhat difficult | 11 | 36.7% | 3 | 23.1% | 8 | 47.1% |
| Not very difficult | 9 | 30.0% | 5 | 38.5% | 4 | 23.5% |
| Not at all difficult | 7 | 23.3% | 3 | 23.5% | 4 | 23.5% |
| Unknown | 3 | 10.0% | 2 | 15.4% | 1 | 5.9% |
| Smoke cigarettes | ||||||
| Not at all | 23 | 76.7% | 10 | 76.9% | 13 | 76.5% |
| Some days | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Every day | 4 | 13.3% | 1 | 7.7% | 3 | 17.7% |
| Unknown | 3 | 10.0% | 2 | 15.4% | 1 | 5.9% |
| Use internet (yes) | 27 | 90.0% | 11 | 84.6% | 16 | 94.1% |
| Suspected cancer sitea | ||||||
| Ovarian | 14 | 46.7% | 6 | 46.2% | 8 | 47.1% |
| Uterine | 16 | 53.3% | 7 | 53.9% | 9 | 52.9% |
| Stage (Summary)a | ||||||
| I | 15 | 50.0% | 8 | 61.5% | 7 | 41.2% |
| II | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| III | 5 | 16.7% | 3 | 23.1% | 2 | 11.8% |
| IV | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Benign | 10 | 33.3% | 2 | 15.4% | 8 | 47.1% |
| Recurrent disease (yes)a | 1 | 3.3% | 0 | 0.0% | 1 | 5.9% |
| Surgery typea | ||||||
| Laparotomy | 12 | 40.0% | 5 | 38.5% | 7 | 41.2% |
| Minimally Invasive | 18 | 60.0% | 8 | 61.5% | 10 | 58.8% |
| ECOG performance statusa | ||||||
| 0 | 15 | 50.0% | 4 | 30.8% | 11 | 64.7% |
| 1 | 15 | 50.0% | 9 | 69.2% | 6 | 35.3% |
| Use of medication for pain (yes)a | 22 | 73.3% | 8 | 61.5% | 14 | 82.4% |
| Comorbid chronic pain (yes)a | 12 | 40.0% | 6 | 46.2% | 6 | 35.3% |
| History of anxiety/depression (yes)a | 15 | 50.0% | 5 | 38.5% | 10 | 58.8% |
| Psychological services (last 2 weeks) | 1 | 3.3% | 0 | 0.0% | 1 | 5.9% |
| Mind-body practices (last 2 weeks) | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Yoga (last 2 weeks) | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Mean | SD | Mean | SD | Mean | SD | |
|
| ||||||
| Age | 59.7 | 11.2 | 60.6 | 0.13 | 58.9 | 0.10 |
| Body mass index (BMI)a | 33.7 | 10.3 | 29.8 | 0.06 | 36.7 | 0.12 |
| Distance travelled to clinic (minutes) | 53.7 | 23.8 | 62.5 | 29.4 | 48.1 | 18.4 |
From medical chart review.
It was not possible to report baseline data from one person who was withdrawn due to a screen failure.
Adherence to the synchronous session with an interventionist was 77% overall (95% CI: 58-90%), and 77% of participants also completed at least 3 days of postoperative self-directed practice in the week assessed. It was possible for interventionists to reach most (71%) participants by telephone before surgery (eMMB n=12; AC n=10). Participants did not initiate additional contact with interventionists. Eighty-one percent of participants (n=25; 95% CI: 63-93%) completed assessments at Week 2 and 84% (n=26; 95% CI: 66-95%) at Week 4. None of the above-reported proportions differed significantly by assigned intervention. Only three participants chose to use study tablets (9.6%; most used their own devices or paper AC diaries).
The effect sizes for reduction in pain intensity showed a greater small to moderate improvement in the eMMB group than AC group (Week 2 d= −0.38; Week 4 d= −0.46; Table 2). There were also clinically important within-group changes for pain intensity in the eMMB group (greater than 1.74; [38]) such that the reduction for the eMMB group (Week 2: −52%; Week 4: −70%) was larger than for the AC group (Week 2: −23%; Week 4 −37%). Further, there were clinically important larger average reductions in depressive symptoms in eMMB than AC at both time points (estimates of minimally important differences for PROMIS measures range from 2.0-5.0; [39]). Other differences in outcomes at Week 4 favored eMMB (affective pain, pain interference). Yet at both time points, reductions in anxiety were larger in the AC group and not different by group for sleep disturbances, with clinically meaningful within group improvements for both groups (sleep only at clinically meaningful at Week 2; [39]). Time to mobilization (n=27, mean difference=−0.33, SD=0.83 days) and length of stay (n=27, mean difference=−0.15, SD=1.44 days) were feasible to ascertain from medical charts and slightly shorter in the eMMB group than AC group (as indicated by the negative mean difference values).
Table 2.
Description of study outcomes by group
| Measures | Baseline | Week 2 | |||||
|---|---|---|---|---|---|---|---|
| eMMB Mean (SD) | AC Mean (SD) | eMMB Change Mean (SD) | AC Change Mean (SD) | Difference in Change Scores (SD) | Cohen’s d for difference | ||
| n=11 | n=17 | n=10a | n=14 | n=24 | |||
| Pain Intensity (Range: 0–10) | 3.63 (3.47) | 3.11 (3.41) | −1.9 (3.57) | −0.71 (2.67) | −1.19 (3.07) | −0.38 | |
|
| |||||||
| Affective Pain (Range: 0–10) | 3.09 (3.53) | 3.06 (3.75) | −1.00 (3.89) | −0.71 (3.67) | −0.29 (3.76) | −0.08 | |
|
| |||||||
| Pain Interference (PROMIS; Range: 0–100) | 53.38 (11.22) | 55.02 (10.93) | 0.08 (13.88) | −0.93 (12.79) | 1.01 (13.25) | 0.06 | |
|
| |||||||
| Depressive Symptoms (PROMIS; Range: 0–100) | 51.43 (11.07) | 50.42 (8.51) | −7.38 (8.60) | −3.78 (9.98) | −3.60 (9.44) | −0.39 | |
|
| |||||||
| Anxiety (PROMIS; Range: 0–100) | 53.47 (12.29) | 55.49 (8.40) | −7.36 (7.83) | −9.66 (13.73) | 2.30 (11.68) | 0.21 | |
|
| |||||||
| Sleep Disturbance (PROMIS; Range: 0–100) | 49.65 (11.78) | 52.46 (10.33) | −3.42 (9.03) | −2.92 (8.26) | −0.50 (8.58) | −0.06 | |
| Measures | Week 4 | |||
|---|---|---|---|---|
| eMMB Change Mean (SD) | AC Change Mean (SD) | Difference in Change Scores (SD) | Cohen’s d for difference | |
| n=11a | n=14 | n=26 | ||
| Pain Intensity (Range: 0–10) | −2.55 (3.08) | −1.14 (3.03) | −1.41 (3.05) | −0.46 |
|
| ||||
| Affective Pain (Range: 0–10) | −2.00 (3.13) | −1.07 (2.92) | −0.93 (3.01) | −0.31 |
|
| ||||
| Pain Interference (PROMIS; Range: 0–100) | −5.92 (10.82) | −4.00 (12.27) | −1.92 (11.67) | −0.17 |
|
| ||||
| Depressive Symptoms (PROMIS; Range: 0–100) | −6.58 (8.06) | −3.75 (5.47) | −2.83 (6.72) | −0.41 |
|
| ||||
| Anxiety (PROMIS; Range: 0–100) | −5.86 (9.70) | −7.90 (11.64) | 2.04 (10.84) | 0.19 |
|
| ||||
| Sleep Disturbance (PROMIS; Range: 0–100) | −1.53 (8.15) | −1.90 (7.74) | 0.37 (7.92) | 0.05 |
Note. eMMB = eHealth Mindful Movement and Breathing, AC = Attention Control.
Patient-Reported Outcomes Measurement Information System (PROMIS) measures are standardized scores such that mean values generally center around 50 with standard deviations of 10. We also computed Cohen’s d.
An additional difference score was not calculated due to an unusable baseline survey noted as missing in Figure 1.
No adverse events were reported throughout the study. Five participants (eMMB n=2; AC n=3) reported small increases in pain and 3 participants reported increases in distress from immediately before to after the synchronous session with the interventionist. When these changes were discussed with study staff, participants stated they did not feel worse than they did before the intervention. Therefore, these small differences may have been due to the high sensitivity of the VAS scale or increased awareness of symptoms. There was no indication that the interventions caused participants any harm. Overall, the eMMB group showed larger decreases than AC in immediate changes for both pain (d= −0.9) and distress (d= −1.3; Table 3).
Table 3.
Assessments of pain and distress immediately pre-post synchronous sessions with interventionists
| Pain | |||||||
|---|---|---|---|---|---|---|---|
| Group | N | Before | N | After | Change Score | Difference Between Group Change Scores | Cohen’s |
| M (SD) | M (SD) | M (SD) | M (SD) | d | |||
| eMMB | 10 | 46.70 (20.40) | 10 | 28.50 (24.30) | −18.20 (21.96) | −14.87 (15.11) | −0.94 |
| AC | 13 | 32.08 (19.10) | 12 | 28.08 (19.92) | −3.33 (4.54) | ||
| Distress | |||||||
| Group | N | Before | N | After | Change Score | Difference Between Group Change Scores | Cohen’s |
| M (SD) | M (SD) | M (SD) | M (SD) | d | |||
|
| |||||||
| eMMB | 10 | 17.00 (13.46) | 11 | 5.82 (12.40) | −10.60 (8.71) | −9.02 (6.79) | −1.29 |
| AC | 13 | 8.69 (19.48) | 12 | 7.83 (18.98) | −1.59 (4.68) | ||
Notes. Pain and distress were assessed with 100mm Visual Analogue Scale items. We also computed Cohen’s d effect sizes.
eMMB = eHealth Mindful Movement and Breathing, AC = Attention Control.
Discussion
We demonstrate the feasibility of an eMMB intervention to improve postoperative pain in patients undergoing gynecologic cancer surgery. Participants showed that it was possible to complete assessments and adhere to the interventions. The proportion of eligible patients recruited in this pilot was lower than proposed, although increased after approaching more participants in person rather than by phone, and the confidence interval for those recruited who were approached included the target rate of 50%. The proportion of eligible patients agreeing to participate was comparable to and proportion of those retained is above those reported for other psychosocial interventions in patients with cancer (40). It is possible that the shorter follow-up timeframe (2 and 4 weeks rather than 6-10 weeks) may account for the improved retention.
We found clinically important improvements in pain intensity in the eMMB group and pain intensity is the proposed primary outcome for a future efficacy study. Further, participants randomized to eMMB showed larger reductions in depressive symptoms than those randomized to AC. Anxiety and sleep disturbances were considerably reduced in both groups, which may be partially due to relief from completing surgery. The clinically important differences in outcomes evident in this study were additive to guideline-concordant care that included pharmacologic pain management (14).
No adverse events related to study interventions were reported, which provides preliminary support for the interventions’ safety. There were large effects of eMMB on decreases in pain and distress immediately after the synchronous eMMB session as compared to AC. These changes were similar in magnitude to our prior feasibility studies (25, 26), suggesting that eMMB leads to an experience of acute pain and distress relief and was not perceived as harmful.
The next step for this research is conducting a fully-powered efficacy study of eMMB. This future study will build upon research showing promising effects of yoga for reducing pain, psychological distress, sleep disturbances, and postoperative length of stay (19–22), while also overcoming methodological challenges of these initial studies (e.g., addressing barriers to participation, using validated measures of pain, including all components of yoga without other approaches). We aim to inform clinical guidelines for multimodal pain management specific to gynecologic cancer surgery, which currently do not include non-pharmacological approaches (14).
Study Limitations
Although there were no significant differences between patients who chose to enroll in the study compared to those who declined, recruiting from a clinic with more representation of racial and ethnic minorities in a larger study would increase generalizability of results. Estimates of effects on outcomes should be interpreted with the consideration that this study was designed to assess feasibility and thus these results may not be stable due to the small sample. The sample was also smaller than initially designed due to the pandemic, yet results were still informative and promising. Further detail regarding type of pain medication used should be considered in future analyses since it may influence results.
Conclusions
In summary, this pilot study supported feasibility and larger improvements in pain intensity and depressive symptoms in eMMB versus AC. These results along with the need for additional data to inform the inclusion of non-pharmacological approaches in multimodal clinical practice guidelines for pain management specific to gynecologic oncology surgery warrant a future efficacy study of eMMB. eMMB may be an optimal non-pharmacological intervention for supporting the management of pain, depressive symptoms, and other clinical outcomes of women undergoing surgery for suspected gynecologic malignancies.
Supplementary Material
Acknowledgements.
The authors gratefully acknowledge the study participants, referring healthcare providers and study team for their contributions.
Funding Details.
Research reported in this publication was supported by the National Center for Complementary & Integrative Health of the National Institutes of Health under Award Number R34AT009546 (Principal Investigator: SJS) and in part by the Wake Forest Baptist Comprehensive Cancer Center’s National Cancer Institute Cancer Center Support Grant (P30CA012197). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We also have a grant under review to extend this work with the National Institutes of Health.
Footnotes
Link to Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT03681405
Disclosure Statement. The authors report there are no competing interests to declare.
References
- 1.American Cancer Society. Cancer Facts and Figures 2020. Atlanta, GA: American Cancer Society; 2020. [Google Scholar]
- 2.Liu S, Ercolano E, Siefert ML, et al. Patterns of symptoms in women after gynecologic surgery. Oncol Nurs Forum 2010;37:133–40. [DOI] [PubMed] [Google Scholar]
- 3.Keil DS, Schiff LD, Carey ET, et al. Predictors of admission after the implementation of an Enhanced Recovery After Surgery pathway for minimally invasive gynecologic surgery. Anesth Analg 2019;129:776–83. [DOI] [PubMed] [Google Scholar]
- 4.Clevenger L, Schrepf A, Degeest K, et al. Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer 2013;119:3234–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsushita T, Murata H, Matsushima E, et al. Emotional state and coping style among gynecologic patients undergoing surgery. Psychiatry Clin Neurosci 2007;61:84–93. [DOI] [PubMed] [Google Scholar]
- 6.Honerlaw KR, Rumble ME, Rose SL, et al. Biopsychosocial predictors of pain among women recovering from surgery for endometrial cancer. Gynecol Oncol 2016;140:301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jim HS, Andrykowski MA, Munster PN, et al. Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Ann Behav Med 2007;34:200–8. [DOI] [PubMed] [Google Scholar]
- 8.Vaz AF, Pinto-Neto AM, Conde DM, et al. Quality of life of women with gynecologic cancer: associated factors. Arch Gynecol Obstet 2007;276:583–9. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 10.Paice JA, Portenoy R, Lacchetti C, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 2016;34:3325–45. [DOI] [PubMed] [Google Scholar]
- 11.van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437–49. [DOI] [PubMed] [Google Scholar]
- 12.Sanford NN, Sher DJ, Butler SS, et al. Prevalence of chronic pain among cancer survivors in the United States, 2010–2017. Cancer 2019;125:4310–8. [DOI] [PubMed] [Google Scholar]
- 13.Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: A clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016;17:131–57. [DOI] [PubMed] [Google Scholar]
- 14.Nelson G, Bakkum-Gamez J, Kalogera E, et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS) Society recommendations-2019 update. Int J Gynecol Cancer 2019;29:651–68. [DOI] [PubMed] [Google Scholar]
- 15.Yoga: What You Need To Know. Available from: https://www.nccih.nih.gov/health/yoga-what-you-need-to-know. Accessed November 22, 2021.
- 16.Posadzki P, Ernst E, Terry R, et al. Is yoga effective for pain? A systematic review of randomized clinical trials. Complement Ther Med 2011;19:281–7. [DOI] [PubMed] [Google Scholar]
- 17.Sarris J, Byrne GJ. A systematic review of insomnia and complementary medicine. Sleep Med Rev 2011;15:99–106. [DOI] [PubMed] [Google Scholar]
- 18.Saeed SA, Antonacci DJ, Bloch RM. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Physician 2010;81:981–6. [PubMed] [Google Scholar]
- 19.Danhauer SC, Addington EL, Cohen L, et al. Yoga for symptom management in oncology: A review of the evidence base and future directions for research. Cancer 2019. 15;125:1979–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khan AZ, Pillai GG. From 200 BC to 2015 AD: an integration of robotic surgery and Ayurveda/Yoga. J Thorac Dis 2016;8:S84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kovačič T, Zagoričnik M, Kovačič M. Impact of relaxation training according to the Yoga In Daily Life® system on anxiety after breast cancer surgery. J Complement Integr Med 2013;10. [DOI] [PubMed] [Google Scholar]
- 22.Rao RM, Nagendra HR, Raghuram N, et al. Influence of yoga on postoperative outcomes and wound healing in early operable breast cancer patients undergoing surgery. Int J Yoga 2008;1:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Astin JA. Mind-body therapies for the management of pain. Clin J Pain 2004;20:27–32. [DOI] [PubMed] [Google Scholar]
- 24.Good M, Anderson GC, Stanton-Hicks M, et al. Relaxation and music reduce pain after gynecologic surgery. Pain Manag Nurs 2002;3:61–70. [DOI] [PubMed] [Google Scholar]
- 25.Sohl SJ, Tooze JA, Wheeler A, et al. Iterative adaptation process for eHealth Mindful Movement and Breathing to improve gynecologic cancer surgery outcomes. Psychooncology 2019;28:1774–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sohl SJ, Avis NE, Stanbery K, et al. Feasibility of a brief yoga intervention for improving acute pain and distress post gynecologic surgery. Int J Yoga Ther 2016;26:43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. Am Psychol 2015;70:581–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montgomery GH, Bovbjerg DH, Schnur JB, et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J Natl Cancer Inst 2007;99:1304–12. [DOI] [PubMed] [Google Scholar]
- 29.Emmons RA, McCullough ME. Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol 2003;84:377–89. [DOI] [PubMed] [Google Scholar]
- 30.Lang EV, Laser E, Lutgendorf SK, Logan HL, et al. Empathic attention and self-hypnotic relaxation for interventional radiological procedures. Iowa City, IA; 1996. [Google Scholar]
- 31.Borrelli B, Sepinwall D, Ernst D, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol 2005;73:852–60. [DOI] [PubMed] [Google Scholar]
- 32.Stone AA, Broderick JE, Junghaenel DU, et al. PROMIS(®) fatigue, pain intensity, pain interference, pain behavior, physical function, depression, anxiety, and anger scales demonstrate ecological validity. J Clin Epidemiol 2015; 74:194–206. [DOI] [PubMed] [Google Scholar]
- 33.Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19. [DOI] [PubMed] [Google Scholar]
- 34.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care 2007;45:S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kistin C, Silverstein M. Pilot studies: A critical but potentially misused component of interventional research. JAMA 2015;314:1561–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leon AC. Implications of clinical trial design on sample size requirements. Schizophr Bull 2008;34:664–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 38.Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58. [DOI] [PubMed] [Google Scholar]
- 39.Kroenke K, Stump TE, Kean J, et al. PROMIS 4-item measures and numeric rating scales efficiently assess SPADE symptoms compared with legacy measures. J Clin Epidemiol 2019;115:116–24. [DOI] [PubMed] [Google Scholar]
- 40.Hanvey GA, Padron A, Kacel EL, et al. Accrual and retention of diverse patients in psychosocial cancer clinical trials. J Clin Transl Sci. 2022;6: e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


